 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
For several years, in traumatic surgery, techniques have evolved towards minimally invasive methods. In 2013, Vendeuvre et al. published a new minimally invasive technic, named Tuberoplasty, to treat Schatzker type II fractures (Vendeuvre et al. Citation2013) (Kfuri and Schatzker Citation2018). This type of fracture corresponds to the splitting and depression of the lateral tibial plateau and mostly occurs in fall from height cases. The surgical procedure was defined to reduce the fracture with an expanding balloon and to stabilize the fracture with PMMA (PolyMethylMethAcrylate) cement injection and bi-cortical screws. As others minimally invasive methods this procedure has considerable advantages in terms of morbidity, speed of recovery and quality of fracture reduction. But the lack of direct fracture visualization requires surgeons to have thorough pre-operative planning to understand how to reduce the fracture.
The aim of this study is to show the interest of Digital Volume Correlation (DVC) to characterize the volume displacement of bone fragments during minimally invasive using the example of Tuberoplasty (Vendeuvre et al. Citation2013)
2. Methods
2.1. The specimen
One fresh frozen human specimen [Laboratory of anatomy, Université de Poitiers - n°DC-2019-3704] was prepared by conserving the proximal third part of the tibia and fibula. The soft tissues, as ligaments and muscles, were removed; meniscus and condyle were preserved. The distal extremity of the tibia and fibula were potted in rigid polyurethane resin to apply fix support. The specimen was fractured from a protocol previously developed by our team (Vendeuvre et al. Citation2018). The resulting fracture corresponds to splitting and depression of 5 mm of the lateral tibial plateau according to fractures type Schatzker II defined in the clinical classification of tibia fractures (Kfuri and Schatzker Citation2018).
2.2. Experimental protocol
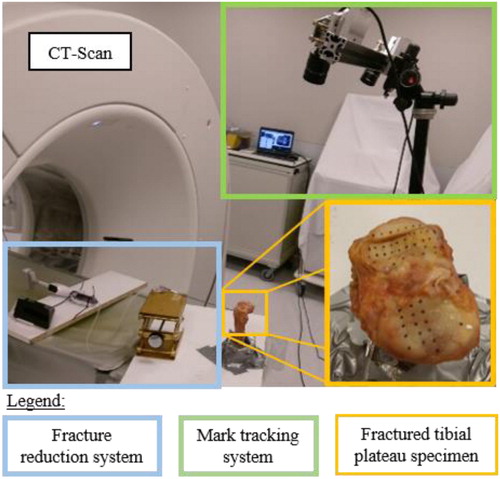
An orthopaedic surgeon practiced Tuberoplasty (Vendeuvre et al. Citation2013) on the tibia-fibula complex. Before, during (every 0.5 cm3 of water injected in the expending balloon) and after the surgical gesture, 3D images were acquired by a medical Helical X-Ray CT-scan [TOSHIBA Aquilon ONE – Resolution: (468 × 468 × 250µm3) - Reconstructed matrix size (512 × 512 × 640 voxels)]. During the surgery, the 3D displacement fields was measured on the tibial plateau surface by mark tracking method (Germaneau et al. Citation2016) ().
Figure 1. Experimental devices to perform surgery under periodic (every 0.5 cm3 of water injected in the expending balloon) CT-Scan acquisitions and mark-up tracking. (The table translation is controlled).
For this study, we selected two CT-scan images to measure the volume displacement fields within bone fragments by DVC. The first image corresponded to the unmodified fractured tibia-fibula complex (reference state) and the second 3D image corresponded to the maximal displacement of the fragments involved by ballon inflation during reduction. To reduce the amount of input data, a mask based on the segmentation of the separated fragment was created and imported in the software X-DVCorrel (Valle et al. Citation2019).
3. Results and discussion
The shows the resulting displacement field of the separated fragment in the medio-lateral direction () in the antero-posterior plan (⊥
between the first and the second 3D images in mm. The volume of the sample was
measured with
The dimensions of the parallelepiped containing the volume are
The subset size was
The displacement field of the superior surface (
from the DVC was compared with measurements obtained by mark tracking method. We found a good accuracy of the displacement fields from DVC regarding to results from 3D displacement of markers (error < 0.5 mm).
Figure 2. Displacement field in medio-lateral direction () in the antero-posterior view (⊥
of the separated fragment between the first and the second 3D images in mm.
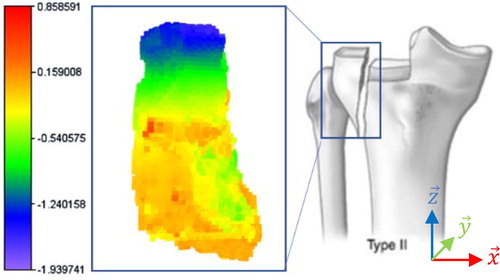
Those results offer a quantification of the volume displacements obtained during the surgical procedure on ex vivo specimen with a medical Helical X-Ray CT-Scan. The observed displacement field corresponds to the opening of the separation during the surgical procedure which is not desirable in surgical practices. But, the effect of soft tissues and the surgical clamp were not represented in this experimentation.
In the case of tibial plateau fracture surgery, restoring the tibial plateau surface according to its morphological shape by minimally invasive technic can be challenging. Those preliminary measurements are valuable for clinicians to understand the kinematic behaviour of fragments during minimally invasive surgery. These experiments are also relevant for the evaluation of the results obtains by numerical simulations of the surgical gestures.
In future work, this measurement method could be implemented with different fracture schemes and different clinical setups to characterize their influence on fracture reduction. Then, the measurement method could be used on medical in vivo images to characterize displacements fields in real conditions, with soft tissues and for others surgical procedure applications.
4. Conclusions
Those results offer a quantification of the volume displacements obtained during the surgical procedure on ex vivo specimen.
This study shows that DVC with 3D images from medical CT-Scan can help clinical practitioners to better understand the displacements of bone fragments during minimally invasive surgery.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Vendeuvre T, Babusiaux D, Brèque C, Khiami F, Steiger V, Merienne J-F, Scepi M, Gayet LE. 2013. Tuberoplasty: Minimally invasive osteosynthesis technique for tibial plateau fractures. Rev Chir Orthop Traumatol. 99(4):S47–S272.
- Kfuri M, Schatzker J. 2018. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 49(12):2252–2263.
- Vendeuvre T, Grunberg M, Germaneau A, Maloubier F, Faure J-P, Gayet L-E, Rigoard P, Brèque C. 2018. Contribution of minimally invasive bone augmentation to primary stabilization of the osteosynthesis of Schatzker type II tibial plateau fractures: Balloon vs bone tamp. Clin Biomech (Bristol, Avon). 59:27–33.
- Germaneau A, Vendeuvre T, Saget M, Doumalin P, Dupré JC, Brémand F, Hesser F, Couvertier M, Brèque C, Maxy P, et al. 2016. A novel approach for biomechanical spine analysis: Mechanical response of vertebral bone augmentation by kyphoplasty to stabilise thoracolumbar burst fractures. J Mech Behav Biomed Mater. 59:291–303.
- Valle V, Bokam P, Germaneau A, Hedan S. 2019. New development of digital volume correlation for the study of fractured materials. Exp Mech. 59(1):1–15.
