1. Introduction
Thanks to the advent of CAD/CAM technology in dental practice and to the increased bonding strength of adhesives, dentists can now offer to their patient new types of restorations (inlays, onlays, overlays, veneers) with reduced dimensions, complex shapes and diverse materials (composites and ceramics) in order to preserve healthy tissues as much as possible. Dentists and/or dental technicians follow four steps to make a restoration using CAD/CAM technology (Tapie et al. Citation2015):
Intraoral scan of the patient's prepared tooth
Computer-aided design (CAD) of the prosthesis using dedicated software
Computer-aided manufacturing (CAM) and numerically controlled milling of the prosthesis.
Finishing: sandblasting and/or acid etching of the basal surface for adhesive infiltration; polishing and glazing of the external surface for aesthetic and biological requirements.
Fracture of the restoration is the first cause of clinical failure for restorations in ceramics (Pjetursson et al. Citation2007) and the second cause, after secondary caries, for restorations in composite (Opdam et al. Citation2014). Curran et al. (Citation2017) have shown that manual adjustment of the prosthesis after machining - grinding with diamond discs followed by polishing - introduced chipping damage responsible for a decrease in strength by 10 to 70% depending on the considered material. This study focuses on numerically controlled milling that may also introduce initial local damage. Lebon et al. (Citation2015) have shown that milling parameters such as the tool-material couple or the tool orientation generated different surface roughness.
The objective is to evaluate the impact of numerically controlled machining on surface topography and on flexural strength for various restorative materials and milling conditions.
2. Methods
Four restorative materials were included in this study:
Coltene Brilliant Crios composite composed of a reticulated methacrylate resin reinforced by dental glass and amorphous silica
Cerasmart composite composed of a Bis-MEPP, UDMA and DMA resin reinforced by silica and baryum glass particles
Enamic polymer infiltrated feldspathic ceramic network
LRF leucite reinforced feldspathic ceramics.
Two milling conditions were investigated:
FL: Flank milling with Lyra milling bur (grain size 78 µm ± 18 µm)
EC: End milling with Cerec milling bur (grain size 44 µm ± 10 µm)
For Coltene Brilliant Crios composite, two additional conditions were investigated: high polishing (HP) (1 µm) and flank milling with Cerec milling bur (FC). Surface roughness was estimated using Alicona focus variation microscope.
shows the number of samples subjected to 3-point bending tests and analysed using Weibull statistics. Fractography analysis was performed for Coltene groups in order to characterize fracture origins for each surface condition. Using fracture mechanics, critical flaw size is also calculated from fracture toughness and flaw location.
Table 1. Number of samples per group.
3. Results and discussion
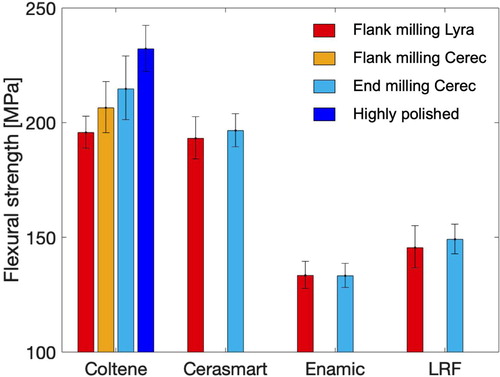
shows the flexural strength of the studied restorative materials, which ranked as follows:
Coltene > Cerasmart > LRF > Enamic.
No significant impact of milling condition was observed for Cerasmart, Enamic and LRF (difference in flexural strength < 3%). This result was expected for Enamic and Cerasmart, known for their machinability but was more surprising for LRF. Indeed, strength reduction due to chipping induced by manual grinding is evaluated between 34% and 47% for a material similar to LRF (Curran et al. Citation2017).
For Coltene Brilliant Crios, the FL group showed 8.8% lower flexural strength than the EC group, the EC group's flexural strength being already reduced by 8% compared to the HP reference group. Damage induced by flank milling with Lyra bur is greater than grinding damage generally observed on restorative composites.
Surface roughness was significantly affected by milling conditions. For Coltene Brilliant Crios, Ra parameter increased from 0.2 µm for EC condition to 1.9 µm for FL condition. Roughness measurements are in progress for the other groups.
All Coltene groups showed diverse and similar fracture origins: pores, inclusions, machining or polishing damage near the centre or at corners of the specimen. However fracture origins were more often related to machining damage for the FL group.
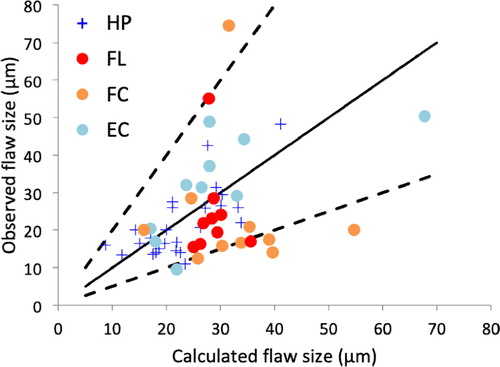
A satisfying correlation was observed between calculated and measured flaw sizes (), especially for groups with low surface roughness (EC and HP). For FL and FC groups, the measured flaw size was smaller than the calculated flaw size, suggesting an interaction between material microstructure and surface topography.
4. Conclusions
This study showed that machining parameters had little impact on the flexural strength of Cerasmart, Enamic and LRF. However, the orientation and the type of milling burs significantly affected Coltene Brilliant Crios strength. Thus, dental CAD/CAM software should adapt their machining strategy and recommendations according to the chosen restorative material.
Acknowledgements
The authors would like to thank S. Abdel-Gawad for the realization of bending tests.
References
- Curran P, Cattani-Lorente M, Wiskott HWA, Durual S, Scherrer SS. 2017. Grinding damage assessment for CAD-CAM restorative materials. Dent Mater. 33(3):294–308.
- Lebon N, Tapie L, Vennat E, Mawussi B. 2015. Influence of CAD/CAM tool and material on tool wear and roughness of dental prostheses after milling. J Prosthetic Dent. 114(2):236–247.
- Opdam NJ, van de Sande FH, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, Gaengler P, Lindberg A, Huysmans MC, van Dijken JW. 2014. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res. 93(10):943–949.
- Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CH. 2007. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res. 18(Suppl 3):73–85.
- Tapie L, Lebon N, Mawussi B, Fron Chabouis H, Duret F, Attal JP. 2015. Understanding dental CAD/CAM for restorations-the digital workflow from a mechanical engineering viewpoint. Int J Comp Dent. 18(1):21–44.