 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
Idiopathic Scoliosis (IS) is associated with three-dimensional deformity of the spine, resulting in a considerable impact on morphology (Assaiante et al. Citation2012). Patients with IS reveal neurological defects: sensory integration disorder; visuo-spatial perceptual impairment; and motor control problem. Spinal fusion has been shown to be very effective in correcting the deformity and preventing further progression of scoliosis (Mahaudens et al. Citation2018). This surgery aims to restore normal sagittal plane alignment and reduce pain. Nevertheless, spinal fusion leads to back stiffness (Delpierre et al. Citation2019). Recently, it was depicted that the most postural stability outcomes of spinal fusion participants were comparable to controls except for significantly reduced equilibrium scores (Li et al. Citation2019). Patients with IS exhibited only tendencies of reduced direction control during the limit of stability tests. So, these tests might not be sensitive enough. In relation to neurological defects, it seems interesting to study imbalance with freely oscillating platform in case of important radius.
With retrospective approach, the purpose of this study was to determine whether patients with IS have defective dynamic equilibrium compared to asymptomatic group on freely oscillating platform with important radius. The second purpose was to evaluate trunk and pelvic stiffness during this test. The third purpose was to delineate the effects of corrective spinal fusion on dynamic equilibrium. We hypothesized that (1) patients with IS present higher CoM displacement than controls; (2) anchoring index quantifies higher back stiffness in case of patients with IS before spinal fusion in reference to controls; (3) spinal fusion increases lower back stiffness.
2. Methods
2.1. Population
The population consisted of 15 patients with scoliosis who had undergone spinal fusion (19.1 ± 8.7 years; Body Mass Index: 20.3 ± 1.1 kg/m2; Cobb angle before fusion: 44.4 ± 17.7 degrees) and 15 control subjects (20.4 ± 1.6 years; BMI: 20.3 ± 1.6 kg/m2). Individuals were excluded if they presented conditions such as musculoskeletal or neurological diseases, pain, or use of drugs. All patients were operated on by the same orthopedic surgeon. The treatment group was analyzed before and one year after surgery. The control group was composed of students who signed the informed consent form.
2.2. Material and methods
With the subject standing on a freely oscillating platform (), Anteroposterior Oscillations were recorded in the sagittal plane here. Only one position was tested in this pilot study: eyes open and feet in a parallel position on a surface defined by a rectangle.
The experimenter held the platform (while manually obscuring a marker placed on the platform, thereby preventing recording), and the subject mounted the platform and stood in the requested position. The experimenter then let go of the platform, which defined the starting point of the trial. Each subject was asked to remain in equilibrium for 10 seconds in a prescribed position. The subject’s oscillations were recorded during this time. Vertical posture was not compulsory, although foot movement was not permitted. After 10 seconds had elapsed, the experimenter again held the platform while obscuring a marker placed on the platform, which represented the end of the trial. Each subject was given one minute to rest between tests.
A 3 D motion capture system (ViconT10, Oxford, UK, 100 Hz) recorded data for 34 passive markers (14 mm) to define “Plug-in gait” model. To measure oscillations on the platform and compute its center, four markers were positioned in each upper corner. Two trials were performed for each subject. A filtering procedure with a second-order Butterworth filter (6 Hz) was applied to the markers data. Center of Mass (CoM) was extracted from Nexus and displacement of CoM was computed with Matlab. About back stiffness, four stabilization segments were analyzed according: upper back (C7-T10), lower back (T10-sacrum), right thigh, left thigh. Considering Assaiante’s method, from these four segments, the Anchoring Index (AIs) were computed: based on the standard deviation of the angular distribution between two segments (SdRel) and the standard deviation of the angular distribution between a segment and the absolute vertical reference (SdAbs) according to:
Descriptive statistics were used to report mean, standard deviation (SD), or median and quartiles, where adequate. Statistical analyses were performed using Statistica (version 13, USA). The Mann–Whitney U test was used to identify differences between scoliotic patients and healthy subjects. The Wilcoxon signed-rank test was also used to assess the influence of arthrodesis. In accordance with (Assaiante et al. Citation2012), the Wilcoxon signed-rank test was used to compare AIs with zero after a Z-transform was applied to the AI distribution such that Z = 0.5*ln((1 + x)/(1 − x)). The chosen level of significance was p ≤ 0.05.
3. Results and discussion
Cobb angle values for the scoliotic group were significantly reduced after spinal fusion (14.1 ± 17.0 degrees). About CoM, before spinal fusion, patients described higher displacements than controls and in reference to post-fusion ().
Table 1. Center of Mass displacements.
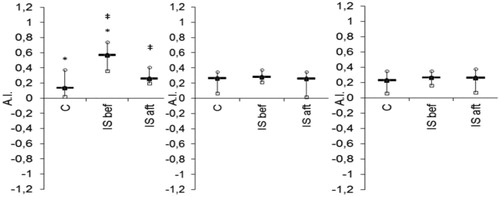
After fusion, CoM displacement presented no significant difference in comparison to controls. So, this test revealed significant result in opposition to postural control (Li et al. Citation2019). shows the segmental AIs with median and quartile values for each side. Our comparison between IS- before fusion and control-group data revealed significant differences between the upper and lower back AI values. Upper and lower back AI values differed significantly from those computed after fusion. Other AI values showed no differences between before and after fusion.
Figure 2. Anchoring Indices. Healthy subjects (C), patients with IS AI median and quartiles: before surgery (called “IS BEF”) and after surgery (called “IS AFT”). * Significant difference with controls. ‡ Significant difference between before/after surgery.
Patients with IS used specific strategies in condition of dynamic equilibrium compared to healthy controls. So, fusion induced positive impact on segmental organization without back stiffness.
4. Conclusions
This pilot study based on dynamic imbalance reveals influence of scoliosis and spinal fusion on CoM and back stiffness. Adding other conditions and oscillations (lateral) could define new sensory test with dynamic imbalance (Assaiante et al. Citation2012).
Acknowledgements
All patients included in this retrospective study. Ethics Committee of Angers for his ethical approval.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Assaiante C, Mallau S, Jouve J-L, Bollini G, Vaugoyeau M. 2012. Do adolescent idiopathic scoliosis neglect proprioceptive information in sensory integration of postural control?. PLoS One. 7(7):e40646.
- Delpierre Y, Vernet P, Surdel A. 2019. Effect of preferred walking speed on the upper body range of motion and mechanical work during gait before and after spinal fusion for patients with idiopathic scoliosis. Clin Biomech (Bristol, Avon)). 70:265–269.
- Li Y, Kakar RS, Fu YC, Walker M, Brown CN, Oswald TS, Simpson KJ. 2019. Postural control of individuals with spinal fusion for adolescent idiopathic scoliosis. Clin Biomech (Bristol, Avon)). 61:46–51.
- Mahaudens P, Dalemans F, Banse X, Mousny M, Cartiaux O, Detrembleur C. 2018. Gait in patients with adolescent idiopathic scoliosis. Effect of surgery at 10 years of follow-up. Gait Posture. 61:141–148.

