1. Introduction
The lack of a tooth is a recurring problem due to functional and aesthetic changes and there are more and more solutions, mainly dental implants as a solution. Several factors affect the integrity of the dental implant (Nelson Citation2011), but the main cause of implant failure is peri-implantitis, which generates infection and bone loss; another critical aspect is the lack of bone integration after implantation (Kullar and Miller Citation2019).
Several studies analyze the modification of the implant surface to promote connectivity with the bones (Smeets et al. Citation2016), improving the stability of the implant with surface roughness or active coatings.
The implant stability is crucial for its success and in the long term, some studies suggest vibration analysis to predict the implant stability by measuring the assembly stiffness (Zanetti et al. Citation2018).
Bone loss around the implant is a critical aspect (Demenko et al. Citation2016) and can predict in long term the stability of fixation (Linetskiy et al. Citation2017). Some studies with finite element model has been developed to predict bone loss in proximal region of cancellous bone and the influence on implant stability, with an effect of 50 to 55% in stability, but is dependently of geometries of implant (Linetskiy et al. Citation2017).
The hypothesis of the study is the proximal bone loss at long-term induces implant failure and predict the loose. The study analysed experimentally the effect of the cancellation of the proximal bone loss around the implant and the effect of the stability of the implant.
2. Methods
The cancellous bone tested was made of open polyurethane foam with a density of D20 (where 20 is the density in pounds per cubic foot pcf) in the open cell structure and the mechanical properties are in are used to replicate bone from Sawbones®. To test the effect of bone loss in the proximal region of the cancellous bone around dental implant the bone was removed. The effect of bone loss was 0.2 mm in deep per year has been taken into account (Linetskiy et al. Citation2017). Was considered two situations, bone loss after 5 and 10 years off implantation, which is equivalent to removing 1 mm and 2 mm of bone respectively proximally. This bone loss represents a reduction of 3% and 6% of the bone support (contact area) around the implant interface in the proximal region. Three samples of each conditions were tested in a total of 9 test (intact, 5 and 10 years bone loss).
Table 1. Mechanical properties of the cancellous bone in experiments.
The implant tested, shown in , is a Branemark model at a 3: 1 scale, with 31.5 mm in length and 12 mm in diameter in Titanium alloy material. To define the geometry of the bone around the implant, a layer of 2 mm in real (representing 6 mm minimum thickness) and 40 mm long presented in was considered.
Figure 1. Representation of experimental setup. a) Bone-implant model, b) Implant position in experiments, c) Loading conditions.
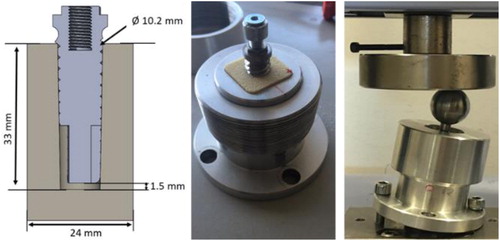
After machining the bone with a hole, the implant was self-screwed with a controlled torque at 0.9 N.m with a screw drive. The compression load done in an Instrom Machine 10KN at 14° representing the loads on the tooth (two components) in the vertical and horizontal direction (Linetskiy et al. Citation2017) presented in , applied on a sphere of a diameter of 20 mm. The test was carried out at a speed of 1 mm/minute up to 355 N in compression, maintaining this force for a total of 60 seconds before relaxation.
The experimental procedure was replicated with 3 samples under the same conditions (torque, loads and bone) and displacement and load was register.
3. Results and discussion
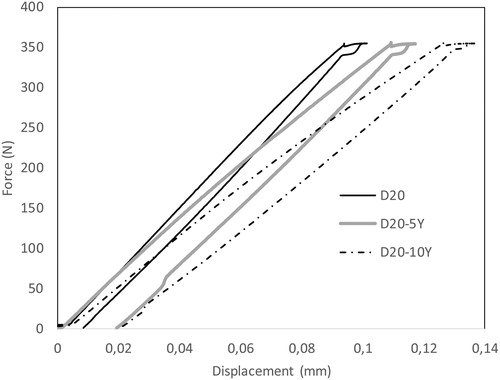
The results of the experimental tests presents a linear behaviour until the maximum load applied, but some damage generated with load-timing process. The bone loss presents some effect in linearity and presented in , where lose some linearity in loading scenario. Relatively to maximum displacement observed for the applied load (), the bone loss increase the maximum displacement of implant and for 10Years bone loss presents the maximum value (). The results show a decrease in stability with proximal bone loss; this effect is more pronounced when at long time, 10 years, the implant-bone interface loses 27% of its initial stiffness.
The results highlight the effect of bone loss, when computing the assembly stiffness the results presents a decrease of 100 N.mm−1 per year, resume of results presented in . The permanent deformation increases more in the first 5 years and presents lower values in the next years. Given the maximum displacement for the applied load, bone loss over 10 years increases.
Table 2. Implant stiffness for different bone losses.
The results highlight the effect of bone lossthe permanent deformation increases more in the first 5 years and shows lower values in the next 5 years of bone loss.
The results emphasize the importance of bone loss in the implant stability; a reduction of bone implant contact area with bone loss was 6% for 10 years in the contact area and generates 27% of implant stability loss.
4. Conclusions
The results of this experimental work describe the importance of bone loss in the implant stability. In addition, bone loss promotes the loss of the implant and can be measured by the reduction of stiffness of dental implant. Another important stiffness factor to consider will be the bone density around the implant; this will be analyzed in the following steps.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Demenko V, Linetskiy I, Linetska L, Nesvit V, Shevchenko A, Yefremov O, Weisskircher HW. 2016. Prognosis of implant longevity in terms of annual bone loss: a methodological finite element study. Comput Methods Biomech Biomed Eng. 19(2):180–187.
- Kullar AS, Miller CS. 2019. Are there contraindications for placing dental implants? Dent Clin North Am. 63(3):345–362.
- Linetskiy I, Demenko V, Linetska L, Yefremov O. 2017. Impact of annual bone loss and different bone quality on dental implant success – a finite element study. Comput Biol Med. 91:318–325.
- Nelson C. 2011. Factors affecting the success of dental implants. In: Ilser Turkyilmaz (Ed.). Implant dentistry: a rapidly evolving practice. Available from: https://www.intechopen.com/books/implant-dentistry-a-rapidly-evolving-practice/factors-affecting-the-success-of-dental-implants
- Smeets R, Stadlinger B, Schwarz F, Beck-Broichsitter B, Jung O, Precht C, Kloss F, Gröbe A, Heiland M, Ebker T. 2016. Impact of dental implant surface modifications on osseointegration. Biomed Res Int. 2016:6285620.
- Zanetti EM, Ciaramella S, Calì M, Pascoletti G, Martorelli M, Asero R. Watts DC. 2018. Modal analysis for implant stability assessment: sensitivity of this methodology for different implant designs. Dent Mater. 34(8):1235–1245.