KEYWORDS:
1. Introduction
In healthy subjects, spinal alignment varies with variations of lung volume (Attali et al. Citation2019) and natural breathing perturbs physiologically the balance (Hamaoui et al. Citation2010). This phenomenon is illustrated by the existence of “respiratory” minimal oscillations of the center of pressure (COP). This disturbance is partially counteracted by cyclic movements of the spine, pelvis and lower limbs (Attali et al. Citation2019; Clavel et al. Citation2020b). The balance between respiratory postural perturbation and its counteraction represents the posturo-respiratory interaction (PRI) (Hamaoui et al. Citation2010). The PRI is centrally controlled as attested by its modulation along the postural chain during a cognitive load (Clavel et al. Citation2020b).
The Obstructive Sleep Apnea Syndrome (OSAS) is a frequent and severe respiratory disease characterized by recurrent obstructions of the upper airways during sleep. It is associated with a specific postural dysfunction characterized by a pathological spinal alignment with cervical hyperextension and a greater amplitude of COP displacements in medio-lateral direction related to an abnormal PRI (Clavel et al. Citation2020a). Consequently there is a need for clinicians to evaluate the PRI in these patients, to detect early the OSAS-related postural dysfunction and to prevent its consequences. Numerous tools exist to measure the PRI (Hamaoui et al. Citation2010; Clavel et al. Citation2020b). The PRI computation requires synchonized assessment of breathing and COP displacements. Clavel et al. (Citation2017) showed the necessity to use a non-invasive method to assess breathing, and developed a method based on the coupling between an optoelectronic system to assess breathing patterns and a force platform to assess the COP displacements (Clavel et al. Citation2020b). According to this observation we propose an alternative contactless and non-invasive approach using airborne ultrasound devices.
This approach offers the advantages to simultaneously assess breathing and postural variations and to be easily usable in clinical settings. This approach has also been used to measure heart beat and chest surface motion to extract breathing parameters ( Jeger-Madiot et al. Citation2017; Nierat et al. Citation2019 ).
The aim is to evaluate the performance of the ultrasonic device to assess the breathing pattern compared to that of a spirometer, as well as the calculated PRI parameters.
2. Material and methods
2.1. Material
Two identic airborne ultrasound probes working in echographic mode are oppositely aligned. Each probe is equipped with a Murata brand transducer model MA40S4S. The transducers operate in transmission reception at 40 kHz. They are connected to home-made electronics. The electrical signals sent and received by the transducers are generated and received by a digital acquisition board (Keysight Model UA2541A), at 320kSa/s. The ultrasounds are focused on the measurement surface using an eliptical mirror. The diameter of the ultrasonic spot is approximately 15 mm at 150 mm distance from the mirror. Comparison is achieved using a low-resistance pneumotachograph spirometer (M.E.C PFT Systems Pocket-Spiro, Medical Electronic Construction, Brussels, Belgium).
2.2. Method
Two healthy volunteers participated to this preliminary test and were placed between the two probes to about 150 mm each. The anterior probe at the sternum level measures both the respiratory and postural movements. The posterior probe at the T7 area level measures postural movements. The Signals of postural movement measured by the two probes are of opposite sign. Finally the sum of both signals only lead to the respiration. Breathing profile was measured during two minutes in two configurations: with the spirometer held at arm’s length; without spirometer. First, we respectively compared the volume and flow rate measured by the spirometer with the displacements and surface velocities measured by the ultrasonic probes. We deduced in parallel the respiratory rate. Then we evaluated the PRI by calculating a new parameter comparable to that of respiratory emergence (Hamaoui et al. Citation2010) which we called respiratory pseudo-emergence. It is based on the postural displacement measured at the level of the T7 area using the ultrasound probe placed behind the subject. This data will be used to replace the antero-posterior displacement of the COP - measured using a force platform - necessary for the calculation of the classical respiratory emergence parameter. The calculation of the respiratory emergence or pseudo-emergence remained otherwise the same. It is the ratio between two energies of the measured displacement: the first is calculated in the frequency band centered on the respiratory frequency at +/- 0.04 Hz and the second in the frequency band 0 − 10 Hz.
3. Results and discussion
3.1. Results
shows the respiratory volume (blue curve) obtained with the spirometer and the respiratory amplitude measured thanks to the two ultrasound probes (red curve). The two curves are correlated with a correlation coefficient of 0.88. In , the postural movement from posterior probe is shown.
Figure 1. (a) Breathing data from spirometer (blue curve) and ultrasonic probes (red curve); (b) T7 area postural movement from ultrasonic probes.
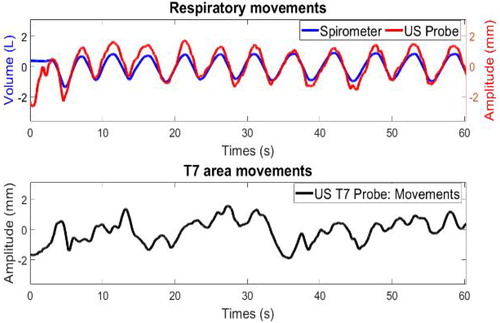
The respiratory pseudo-emergence calculation gives a value of 8.33%. This value is close to the median emergence that was computed from Clavel’s data with Vicon markers, at the T7 area level (7.02%) and at the pelvis level (8.22%).
3.2. Discussion
This study shows that the ventilation measurement is realizable with non contact ultrasonic probes and consistent with the spirometer data. The postural movement is measured with the posterior ultrasonic probe and allows finally to evaluate the PRI. We acknowledge that there was no precise control of the equidistance of the subjects compared to the probes. In addition, this pre-manipulation was carried out on only 2 subjects of fine corpulence. In order to confirm the results obtained, a more reliable prototype is in development. So, we plan to continue with different subject morphologies. Finally, the present method will be compared with simultaneous measurements by force plate and optoelectronic sensors. The proposed respiratory pseudo-emergence parameter will be then compared to the reference computation of respiratory emergence.
4. Conclusions
The aim of the study assessed the ability of the ultrasonic probes to measure ventilation by comparison with the reference spirometry method. The proposed method allows a reliable measurement of breathing. In addition, we also offer a contactless approach of a respiratory pseudo-emergence parameter to evaluate the PRI. The obtained parameters seem promising and consistent with the literature, but need to be confirmed.
Acknowledgements
We thank IUIS for integrating and funding our project into their Lighthouse Breath Innovative Technology for Medicine program.
No potential conflict of interest was reported by the author(s).
Disclosure statement
References
- Attali V, Clavel L, Rouch P, Rivals I, Rémy-Néris S, Skalli W, Sandoz B, Similowski T. 2019. Compensation of respiratory-related postural perturbation is achieved by maintenance of head-to-pelvis alignment in healthy humans. Front Physiol. 10:441. doi:10.3389/fphys.2019.00441.
- Clavel L, Attali V, Jacq O, Nierat MC, Similowski T, Rouch P, Sandoz B. 2017. Breathing through a spirometer perturbs balance. Computer Methods in Biomechanics and Biomedical Engineering. 20:41–42. doi:10.1080/10255842.2017.1382851.
- Clavel L, Attali V, Rivals I, Niérat M-C, Laveneziana P, Rouch P, Similowski T, Sandoz B. 2020b. Decreased respiratory-related postural perturbations at the cervical level under cognitive load. Eur J Appl Physiol. 120:1063–1074. doi:10.1007/s00421-020-04345-1.
- Clavel L, Rémy-Neris S, Skalli W, Rouch P, Lespert Y, Similowski T, Sandoz B, Attali V. 2020a. Cervical spine hyperextension and altered posturo-respiratory coupling in patients with obstructive sleep apnea syndrome. Front Med (Lausanne). 7:30. doi:10.3389/fmed.2020.00030.
- Hamaoui A, Gonneau E, Le Bozec S. 2010. Respiratory disturbance to posture varies according to the respiratory mode. Neurosci Lett. 475:141–144. doi:10.1016/j.neulet.2010.03.064.
- Jeger-Madiot N, Gateau J, Fink M, Ing R-K. 2017. Non-contact and through-clothing measurement of the heart rate using ultrasound vibrocardiography. Elsevier Med Eng Phys. 50:96–102. doi:10.1016/j.medengphy.2017.09.003.
- Niérat M-C, Laveneziana P, Dubé B-P, Shirkovskiy P, Ing R-K, Similowski T. 2019. Physiological validation of an airborne ultrasound based surface motion camera for a contactless characterization of breathing pattern in humans. Front Physiol. 10:680. doi:10.3389/fphys.2019.00680.
