1. Introduction
One of the main requirements for a successful dental implant is its osseointegration to the cancellous peri-implant bone which is mainly controlled by the material, surface properties and micro displacements. On the other hand, the long term marginal bone loss occurs as the bone remodels in response to its local elastic strain (Klein-Nulend et al. Citation2012). The commercial offer and variety even within a single dental implant company is very wide and includes bone level, soft tissue level, tapered, straight, various diameters and lengths (). Anatomical and biomechanical characteristics are usually the determining factors for the choice of length and diameter of the implant to be placed, but the choice between bone level and soft tissue level implants is usually left to aesthetic considerations or to the clinicians’ personal preference. In this study, we use a finite element analysis to compare the strains induced on the cortical peri-implant bone of two different implant designs.
2. Methods
The left second premolar section of a mandible was reconstructed from a cone beam computed tomography. The cortical and cancellous bone was segmented and reconstructed accordingly (). The implants from the manufacturer Institut Straumann AG were modeled in CATIA V5 and have the same diameter (4.1 mm) and implantable length (10 mm). A finite element model was created in ANSYS workbench 18.1. The material properties were assigned according to . All contacts were set as bonded and quadratic tetragonal elements were used for the mesh. The mesh is refined in the implant-cortical bone interface up to an element size of 0.15 mm that showed mesh convergence.
Figure 1. (A) Implant models: Soft tissue level left and bone level right. (B) Soft tissue level implant positioned on the reconstructed mandible section.
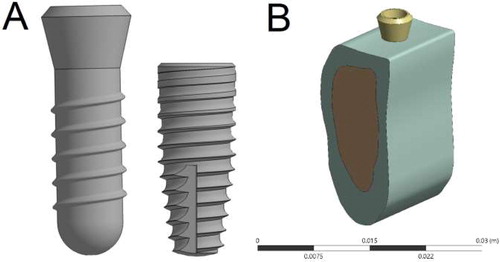
Table 1. Material properties for the finite element model.
Two load scenarios in accordance to recent studies (Peyroteo et al. Citation2019) were simulated: (1) Axial vertical load of 100 N and (2) 100 N oblique load at 20° from the vertical axis in the distal-mesial direction . The load is remotely applied 8 mm above the cortical bone level, which resembles a biting contact where the occlusal surface of the crown would lie. The distal and mesial surfaces of the bones are fixed in all six degrees of freedom. The equivalent strains at the peri-implant cortical bone were quantified and shown in milistrains (mε).
3. Results and discussion
From (axial load scenario), it can be seen that the soft tissue level implant induces higher strains on the peri-implant cortical bone at the 0 mm depth (dark red on the figure) than the bone level implant (1.2 and 0.2 mε, respectively). This is also the case in the oblique load scenario (figure not included) where, at the 0 mm depth, the soft tissue level implant induces around 4.5 mε in the mesial and 2.7 mε in the distal direction. In that same scenario, the bone level implant induces around 1 mε in the mesial and 0.5 mε in the distal direction. However, at the 1 mm depth and below, both implants generate very similar strains on the peri-implant cortical bone, around 0.35 mε in the axial load scenario and around 0.6 mε in the mesial side of the oblique load scenario.
Figure 2. Equivalent strain (mε) at the peri-implant in the 100 N axial load scenario. (A) Soft tissue level implant. (B) Bone level implant.
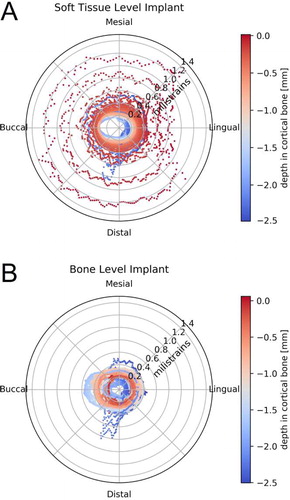
It is interesting to note the higher strain at the 2.5 mm depth (dark blue in the figure) in the distal direction for both implant designs. This peak corresponds to the location where the thread of the implants coincides with the cortical bone – cancellous bone interface. Even though the strains induced by the soft tissue level implant are higher in both load scenarios, this type of implant has shown excellent conservation of the marginal bone in clinical studies and has been used even as the control for marginal bone loss in animal trials (Heitz-Mayfield et al. Citation2013). In the clinical practice, both implants have also shown comparable long-term esthetic outcomes where the marginal bone level plays a critical role (Siebert et al. Citation2018). This could suggest, that the higher strains induced by the soft tissue level implant are still within the physiological range to preserve the marginal cortical bone and avoid resorption. Nevertheless, the values are significantly lower in the axial load condition than the 2.5 mε for the best conservation of marginal bone that patient-specific implants intend to achieve (Roy et al. Citation2018). This means that the stiffness of these implants is still higher than ideal.
4. Conclusions
The soft tissue level implant from Straumann induces 6 times higher equivalent stress on the peri-implant cortical bone at the 0 mm depth than the bone level implant of the same manufacturer. However, both implants show a similar and uniform distribution of strain below the 1 mm cortical bone depth.
Additional information
Funding
References
- Heitz-Mayfield LJA, Darby I, Heitz F, Chen S. 2013. Preservation of crestal bone by implant design. A comparative study in minipigs. Clin Oral Impl Res. 24(3):243–249.
- Klein-Nulend J, Bakker A, Bacabac R. 2012. Mechanical loading and how it affects bone cells: the role of the osteocyte cytoskeleton in maintaining our skeleton. Eur Cell Mater. 24:278–291.
- Peyroteo MMA, Gomes HIG, Belinha J, Jorge RMN. 2019. Biomechanical analysis of bone tissue after insertion of dental implants using meshless methods: stress. In: Advances in biomechanics and tissue regeneration. Elsevier; p. 393–403.
- Roy S, Dey S, Khutia N, Roy Chowdhury A, Datta S. 2018. Design of patient specific dental implant using FE analysis and computational intelligence techniques. Appl Soft Comput. 65:272–279.
- Siebert C, Rieder D, Eggert J, Wichmann M, Heckmann S. 2018. Long-term esthetic outcome of tissue-level and bone-level implants in the anterior maxilla. Int J Oral Maxillofac Implants. 33(4):905–912.
