1. Introduction
Total hip arthroplasty is the main salvage procedure for hip osteoarthritis in dogs. Two main types of femoral stems are available: cemented stems which offer excellent primary stability (Olmstead Citation1995) but are subject to aseptic loosening at long terms (Bergh et al. Citation2006) and cementless stems which have good long term outcomes but lack of primary stability (Kidd et al. Citation2016). Adjunction of a neutral rod through the neck of the cementless stem to the lateral cortex of the femur could offer better primary stability by reinforcing the cementless system and limiting the torsion and compression forces during osseointegration and bone healing. The aim of this study is to compare the primary stability of 3 different femoral stems.
2. Methods
2.1. Femur preparation
Eighteen femurs harvested from 9 adults cadavers (24.4 ± 4.5 kg) were randomly implanted with 3 different femoral stems: cemented (cFS), press-fit cementless (pfFS), and rod-cementless stems (r-pfFS). Before and after implantation, medio-lateral and cranio-caudal digital radiographs were performed (). To ensure the reliable positioning of the femoral stem and to have repeatable biomechanical assays, degrees of cranio-caudal and varus-valgus angulation were, respectively, calculated (Townsend et al. Citation2017).
2.2. Biomechanical assays
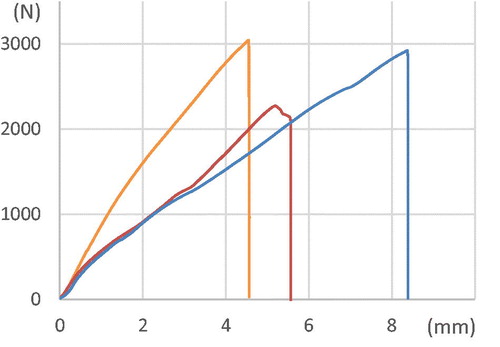
After preparation, the distal part of the femurs was potted in synthetic polyurethane resin and placed in the servohydraulic press. The load was applied on the femoral head, parallel to the longitudinal axis of the femur. They were first cyclically loaded at 75% of their live weight to study transverse displacement (0.2mm/sec for 90 cycles). Then, unidirectional load compression was performed at 0.2 mm/sec to evaluate resistance to subsidence. Force and displacement were obtained directly from the press sensors. Stress, axial load stiffness, work necessary to subsidence, strain to failure and mean strain of cyclic assays were calculated. The Force–Displacement () and Stress–Strain curves were then plotted. Non-parametric Kruskal-Wallis tests were used to compare statistical differences between the groups. Non-parametric Wilcoxon tests were used to compare paired groups. The confidence interval was fixed at 0.05.
3. Results and discussion
On the post-implantation radiographs, no growth plates has been identified. No fracture was identified in each group, PMMA cement was homogeneously distributed around the stem in the femoral shaft. Frontal (varus-valgus) and sagittal (cranio-caudal) angulation were, respectively, 2.22 ± 0.76° and 3.02 ± 1.44°. No significant difference was observed between the groups (p = 0.65 and 0.81, respectively). Proper positioning of the femoral stem is a critical aspect during surgery as well as during biomechanical assay. Indeed, if only subjective eye evaluation is made after implantation, slight differences in angulation can compromise the final result. It has been shown that a varus angulation of the femoral stem superior or equal to 5° leads to an increased risk of fracture intraoperatively because of the medial position of the proximal part of the femoral stem, which overpressures a common site of fractures, the craniomedial part of the proximal femur (Townsend et al. Citation2017).
No significant difference was observed on transverse displacement (p = 0.263) and mean strain (p = 0.244) during cyclic tests, as well as axial load stiffness (p = 0.121), work necessary to subsidence (p = 0.079). and strain to failure (p = 0.075) on subsidence assays (). Cyclic assays have been developed with the technical possibilities of the servo-hydraulic press. The aim of the test was not to imitate the immediate postoperative normal gait of the dog after surgery but rather to pre-stress the femur before the failure test. The immediate postoperative normal gait of a dog is around 1500 steps (Aper et al. Citation2003). On assays presented in this study, only 90 cycles were performed. Considering the relatively low number of cycles, the load was set at 75% dog’s respective living weight, miming the trot to increase stress on the femur. No significant difference has been shown between all groups. Those results validate the reliability of the new implant and demonstrate the same strain and displacement of the other group.
Table 1. Summarized results (mean ± standard deviation) for the subsidence and cyclic assays. Significant difference (p < 0.05) when superscripted symbols are similar. “Displ.” means displacement.
4. Conclusions
The addition of a rod on a cementless femoral stem offers significantly higher stability to compressive load parallel to the longitudinal axis of the femur compared to standard cementless stems. It is favorably comparable to femoral stems already available on the market. r-pfFS could be a valuable option to limit subsidence and micro-motion of press-fit femoral stems and thus improving prosthesis osseointegration.
Acknowledgements
The authors would like to thank Mr. Michel Porte and PorteVet® society for providing the femoral stems.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Aper RL, Litsky AS, Roe SC, Johnson KA. 2003. Effect of bone diameter and eccentric loading on fatigue life of cortical screws used with interlocking nails. Am J Vet Res. 64(5):569–573.
- Bergh MS, Gilley RS, Shofer FS, Kapatkin AS. 2006. Complications and radiographic findings following cemented total hip replacement: a retrospective evaluation of 97 dogs. Vet Comp Orthop Traumatol. 19(03):172–179.
- Kidd S, Preston C, Moore G. 2016. Complications of porous-coated press-fit cementless total hip replacement in dogs. Vet Comp Orthop Traumatol. 29(5):402–408.
- Olmstead ML. 1995. Canine cemented total hip replacements: state of the art. J Small Anim Pract. 36(9):395–399.
- Townsend S, Kim SE, Pozzi A. 2017. Effect of stem sizing and position on short-term complications with canine press fit cementless total hip arthroplasty. Vet Surg. 46(6):803–811.