1. Introduction
Temporomandibular joint replacement (TMJR) is recognized to solve pain and functional limitations when other less invasive strategies failed. TMJR consists in condyle osteotomy (leading to the section of the lateral pterygoid muscle) followed by the fixation of the fossa and the mandibular components. The surgery leads to immediate pain relief and a progressive increase of the mouth opening, assessed by the gap between the upper and lower incisal teeth. Other parameters were rarely considered such as the trajectories of mandibular landmarks (Wojczyńska et al. Citation2019). Our study combines the assessment of the quality of life (QoL) outcomes with quantitative functional measurements – electromyography (EMG) of the masticatory muscles and 3 D mandibular motions – in order to evaluate the mid-term effects of TMJR.
2. Methods
A national ethical committee validated the protocol and all the subjects gave their consent to participate.
2.1. Subjects
Five females (P1 to P5, 63 ± 7.6 years old), who suffered from advanced TMJ osteoarthritis, underwent unilateral TMJR. They participated in four measurements: one before and three after the surgery at 1 month, 3 months and 6 months of follow-up. 29 asymptomatic volonteers were also considered as a reference group (18 males & 11 females, 37 ± 12 years old). Inclusion criteria were a type 1 dental occlusion, and the absence of previous TMJ disorders, clicking joint, cephalalgia and tinnitus.
2.2. EMG of the masticatory muscles
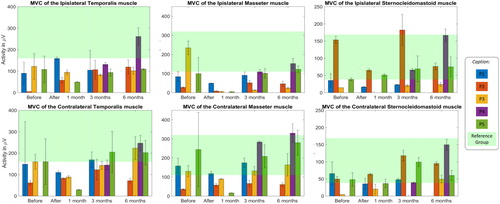
The muscular activities of the masseters (M), anterior temporalis (T) and sternocleidomastoid (SCM) muscles were recorded during the rest and the maximal volontary contraction (MVC) obtained by clenching on dental cottons or by rotating the head, following the protocol described by Sapin-de Brosses et al. (2019). The values were compared to 10 females having the patients’ morphotype among the reference group.
2.3. Mandibular kinematic measurement
The mandibular 3 D positions were recorded using the CMS-20-JMA device (Zebris GmbH, Germany) composed by a mobile transmitter unit glued on the mandibular teeth, and a receiving unit placed on the head. Cranial and mandibular landmarks were palpated while keeping the mouth closed. The 3 D coordinates of the mandibular points were then provided at each time during thirty opening-closing movements. The six mandibular degrees of freedom (DOF) were computed with an accuracy of 0.26 mm for the translations and 0.5° for the rotations (Koeppel et al. Citation2015).
3. Results and discussion
3.1. Clinical outcomes
No surgical complications occurred. The pain, rated at the maximum for 4 over the 5 patients before TMJR, was reduced to a controlled pain for all the patients one month after the surgery. The pain relief is sustainable: 4 patients had no more pain 3 months post- surgery and after on. The quality of life, rated as “poor” to “moderate” before the surgery, increased for all the patients from three months after the TMJR.
3.2. Functional recovery: muscular activities
Before the surgery, the patients had difficulty to relax due to the extreme pain, revealed by the high muscular activities for all the muscles during the rest (4 to 8 µV vs a maximum of 4 µV for the reference group). After the surgery, the activities during the rest progressively decreased and stabilized within the asymptomatic range. The MVC values were significantly smaller than for the asymptomatic women before the surgery for the suffering side, and close or within the asymptomatic range for the contralateral side (). After the surgery, the MVC activities globally increased for all the muscles and both sides. Six months after the surgery, the MVC values were in the asymptomatic range for the SCM muscles. They were smaller than the asymptomatic values for the T and M muscles for the prosthetic side, with the exception of patient P4. The difficulty to obtain patients’ maximal contraction by biting on the cottons should be noticed, due to a lack of intraoral feeling or the fear of suffering. Interestingly, patient P4 who recovered asymptomatic contractions for both sides, was the unique patient performing daily sessions of physiotherapy.
3.3. Kinematic analysis
Before the surgery, the vertical displacement of the inter-incisal point was on average limited to the half of the asymptomatic opening (18.9 ± 9.6 mm vs 39.5 ± 5.7 mm respectively). This magnitude significantly increased three months after the surgery and later on. Six months after the TMJR, mouth opening reached between 80% and 800% of the preoperative value depending on the patient, but remained lower than the asymptomatic one (average of 25.9 ± 3.5 mm).
The analysis of the six mandibular DOF provides insights into the mandibular behaviour with the prosthesis. Before the surgery, all the DOF were smaller than the asymptomatic values (), which is consistent with the limitation of the mouth opening.
Table 1. Six mandibular DOF: absolute values (average ± standard deviation) during mouth opening.
One month after TMJR, mandibular translations were nearly zero. The rotation around the intercondylar axis (IC) was divided by a factor of two and represented the third of the asymptomatic IC value. On the contrary, the frontal tilt and the axial rotation increased and were higher than the asymptomatic range. The translations increased with time but remained lower than the asymptomatic values six months after TMJR. As expected, the anterior-posterior (AP) and inferior-posterior (IS) translations were limited, due to the design of the prosthesis that ensures vertical contact between the prosthetic elements and avoids anterior luxation. The lack of translation was compensated by the mandibular tilt and axial rotation towards the prosthetic side to allow the anterior displacement of the contralateral natural condylar pole. The IC rotation increased with time and reached on average 21° six months after TMJR but was smaller than the asymptomatic rotation.
4. Conclusions
TMJ replacement leads to an immediate pain relief and a progressive increase of the mouth opening. Patients’ QoL increased with the same rate. The patients recovered moderate abilities to contract the superficial masticatory muscles after TMJR. Physiotherapy exercises are not systematically prescribed and it could be interesting to better understand their potential effects on the maximal contractions. The analysis of the 3 D mandibular motions revealed differences with the asymptomatic patterns. It is the way towards the in-deep understanding of the in situ prosthetic behaviour and improvement of the prosthetic design.
Acknowledgement
Thanks to the Fondation des Gueules Cassées which funded the study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Koeppel T, Sapin-de Brosses E, Bonnet A-S. 2015. Three dimensional functional analysis of the human mandibular movements. Comput Methods Biomech Biomed Eng. 18(sup1):1964–1965.
- Sapin-de Brosses E, Bonnet A-S, Zwetyenga N. 2019. Evolution of the activity of the masticatory muscles before and after temporomandibular joint replacement: a clinical and functional study. Comput Methods Biomech Biomed Eng. 22:S52–S54.
- Wojczyńska A, Gallo LM, Bredell M, Leiggener CS. 2019. Alterations of mandibular movement patterns after total joint replacement: a case series of long-term outcomes in patients with total alloplastic temporomandibular joint reconstructions. Int J Oral Maxillofac Surg. 48(2):225–232.