?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.1. Introduction
1.1. Clinical context
Heart failure affects the heart’s ability to meet the oxygen needs of the organs. It concerns more than one million people in France. It can be defined by the reduced capacity of the heart to be filled with blood (diastolic dysfunction) and/or emptied (systolic dysfunction). Although systolic dysfunction is relatively easy to diagnose, the diagnosis of diastolic dysfunction is more challenging. The accessibility of echocardiography, and its ability to provide information non-invasively and in real time, makes ultrasound the preferred technique for evaluating left ventricular diastolic function. However, the diagnosis of diastolic dysfunction often remains uncertain, as the recommended ultrasound indices may lead to conflicting conclusions. Since intracardiac blood flow is very sensitive to changes in the myocardium, we hypothesized that a thorough examination of intraventricular blood flow by color Doppler echocardiography could improve the assessment of diastolic function in patients with heart failure.
1.2. Objective
During diastole, a vortex ring is created in the left ventricle downstream of the mitral valve. This vortex naturally redirects the blood flow towards the outflow tract. In healthy subjects, it facilitates the transition from filling to ejection. When filling is impaired (diastolic dysfunction), a change in blood flow occurs, which has a significant impact on the intraventricular vortex and on its properties.
Doppler echocardiography provides only one component of the velocity vectors: the component parallel to the ultrasound beam. Two-dimensional intraventricular vector flow mapping (iVFM) was introduced to construct 2-D vector velocity fields from conventional color Doppler (Garcia et al. Citation2010; Assi et al. Citation2017). We have extended the method, and present a three-dimensional mapping of intraventricular flow (3-D iVFM) by color Doppler to decipher the dynamics of the 3-D vortex ring that forms in the left ventricle during diastole. Unlike multi-angle methods (Gomez et al. Citation2015), the approach we propose is based on a single acoustic window and does not require spatio-temporal registration, making it 100% compatible with clinical needs.
2. Methods
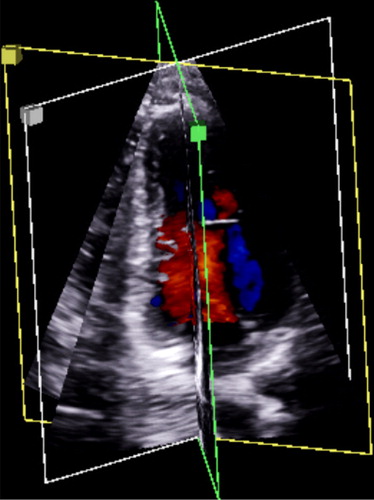
The objective of 3D-iVFM is to recover the three velocity components in the intraventricular cavity from Doppler velocities alone (i.e. from radial components only) on a limited set of planes (three planes). To provide the 3D-iVFM, we used the echocardiographic triplane mode available on clinical GE scanners (). This means that we used Doppler data from three planes separated by an azimuthal angle of 60° in the apical long-axis view, without moving the probe. The Doppler data prior to scan-conversion were retrieved using the EchoPAC software. Volumetric three-component intraventricular blood flows were estimated from the three planes of the color Doppler. The problem was written as a constrained least squares problem, which was solved by the Lagrange multiplier method. We used hemodynamic properties to constrain the problem such as mass conservation for an incompressible fluid (null-divergence) and free-slip conditions on the wall. The mathematical equation of this problem is:
with
subject to:
Figure 1. Triplane echocardiography provides three planes from the same heartbeat with high temporal and spatial resolutions.
is the objective function,
is the 3-D velocity vector,
is the radial component of the estimated velocity,
is the negative Doppler velocity (to ensure sign compatibility with the Doppler convention, which dictates positive values when blood flows towards the probe),
is a smoothing function and
is the smoothing parameter,
is the region of interest,
is the vector normal to the wall, and
is its velocity. A finite-difference discretization converted the minimization problem into a basic linear problem. Operator-dependence was minimized by using automatic model selection.
3. Results and discussion
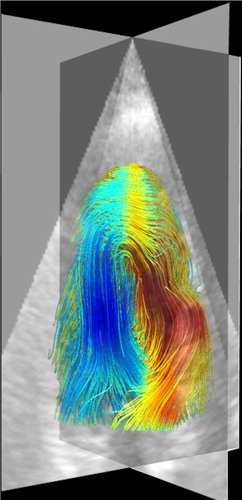
To check its well-posedness and robustness, we evaluated 3D-iVFM in silico in a spherical Hill’s vortex ring. The NRMS errors between the estimated and actual 3-D velocity vectors were between 8–20% for a wide range of Doppler noise and beam-to-flow alignment. 3D-iVFM was also tested in a healthy volunteer with triplane color Doppler (). The 3-D intraventricular vortical flow recovered by 3D-iVFM was clearly visible () and consistent with published data. These promising in silico and in vivo findings tend to show that 3D-iVFM could be an efficient clinical tool for analysis of left ventricular filling. The next step is to validate 3D-iVFM on a patient-specific model of the intraventricular blood flow (Chnafa et al. Citation2014) and compare 3D-iVFM against magnetic resonance velocimetry in patients.
4. Conclusions
3D-iVFM could be an efficient tool for a thorough clinical analysis of the 3-D intraventricular vortex. Fast and 100% clinical, 3D-iVFM could offer new echocardiographic insights into left ventricular function, especially for diastology.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Assi KC, Gay E, Chnafa C, Mendez S, Nicoud F, Abascal JFPJ, Lantelme P, Tournoux F, Garcia D. 2017. Intraventricular vector flow mapping: a Doppler-based regularized problem with automatic model selection. Phys Med Biol. 62(17):7131–7147.
- Chnafa C, Mendez S, Nicoud F. 2014. Image-based large-eddy simulation in a realistic left heart. Comput Fluids. 94:173–187.
- Garcia D, del Álamo JC, Tanné D, Yotti R, Cortina C, Bertrand É, Antoranz JC, Pérez-David E, Rieu R, Fernández-Avilés F, et al. 2010. Two-dimensional intraventricular flow mapping by digital processing conventional color-Doppler echocardiography images. IEEE Trans Med Imag. 29(10):1701–1713.
- Gomez A, de Vecchi A, Jantsch M, Shi W, Pushparajah K, Simpson JM, Smith NP, Rueckert D, Schaeffter T, Penney GP. 2015. 4D blood flow reconstruction over the entire ventricle from wall motion and blood velocity derived from ultrasound data. IEEE Trans Med Imag. 34(11):2298–2308.