Abstract
Objectives: We investigated whether a Mediterranean-style diet (MedDiet) supplemented with fish oil can improve mental health in adults suffering depression.
Methods: Adults with self-reported depression were randomized to receive fortnightly food hampers and MedDiet cooking workshops for 3 months and fish oil supplements for 6 months, or attend social groups fortnightly for 3 months. Assessments at baseline, 3 and 6 months included mental health, quality of life (QoL) and dietary questionnaires, and blood samples for erythrocyte fatty acid analysis.
Results: n = 152 eligible adults aged 18–65 were recruited (n = 95 completed 3-month and n = 85 completed 6-month assessments). At 3 months, the MedDiet group had a higher MedDiet score (t = 3.95, P < 0.01), consumed more vegetables (t = 3.95, P < 0.01), fruit (t = 2.10, P = 0.04), nuts (t = 2.29, P = 0.02), legumes (t = 2.41, P = 0.02) wholegrains (t = 2.63, P = 0.01), and vegetable diversity (t = 3.27, P < 0.01); less unhealthy snacks (t = −2.10, P = 0.04) and red meat/chicken (t = −2.13, P = 0.04). The MedDiet group had greater reduction in depression (t = −2.24, P = 0.03) and improved mental health QoL scores (t = 2.10, P = 0.04) at 3 months. Improved diet and mental health were sustained at 6 months. Reduced depression was correlated with an increased MedDiet score (r = −0.298, P = 0.01), nuts (r = −0.264, P = 0.01), and vegetable diversity (r = −0.303, P = 0.01). Other mental health improvements had similar correlations, most notably for increased vegetable diversity and legumes. There were some correlations between increased omega-3, decreased omega-6 and improved mental health.
Discussion: This is one of the first randomized controlled trials to show that healthy dietary changes are achievable and, supplemented with fish oil, can improve mental health in people with depression.
Introduction
The world is facing a growing epidemic of non-communicable diseases. In 2012, 68% of global deaths (38 million) were attributable to non-communicable diseases, with cardiovascular diseases (CVDs) the leading cause.Citation1 The 2013 Global Burden of Disease report identified that, in both developing and developed countries, major depressive disorder now ranks as the second highest cause of years of life lost due to disability (YLD). From 1990 to 2013, YLD attributed to mental and substance abuse disorders increased by 45%, depressive disorders by 53.4% and CVDs by 89.2%,Citation2 constituting a major burden of disease worldwide with tremendous associated personal, psychosocial, and financial impacts.
It has long been known that people with CVD have a higher incidence of depression than the general population, and it is established that depression is a risk factor for developing CVD.Citation3 What is perhaps less recognized is that depression and CVD share similar underlying biological risk factors such as inflammation,Citation4–6 low levels of omega-3 polyunsaturated fatty acids (PUFAs)Citation7–9 and poor diets. Traditional Mediterranean diets, characterized by high intake of plant foods (vegetables, fruit, legumes, nuts, seeds, olives, wholegrains), extra virgin olive oil as the main culinary fat, moderate intake of fish and low intakes of confectionary, red meat, and processed food,Citation10 are emerging as protective for CVD.Citation11,Citation12
Meta-analyses of observational studies have shown that a healthy dietCitation13 and Mediterranean dietCitation14 are associated with lower risk of depression. People with mental illness have been identified as having poorer diet and other lifestyle behaviours that impact on health, and less understanding of the impact of lifestyle behaviours on health.Citation15 Randomized controlled trials (RCTs) such as the large Prevención con Dieta Mediterránea (PREDIMED) study have successfully implemented Mediterranean diets in adults with CVD risk.Citation16 Secondary analysis from the PREDIMED study showed some trends for reduced risk of depression in the MedDiet groupCitation17 but was not powered for this outcome. We are aware of only two dietary RCTs in people with depression; this studyCitation18 and another Australian study which was recently completed.Citation19
Changing established dietary behaviours is challenging, and this is attributed to factors such an obesogenic environmentCitation20 and the addictive nature of high-fat high-sugar foods.Citation21 However, there is evidence that neural reward thresholds can be changed in favour of preferring healthy over unhealthy food.Citation22 A Mediterranean diet not only has demonstrated health benefits but is also a highly palatable diet and thus more likely to become a sustainable part of a healthy lifestyle.Citation10
We aimed to investigate the impacts of a Mediterranean-style diet intervention for mental health and quality of life (QoL) in people with depression using a RCT design over 3 months with follow-up at 6 months. Owing to the particularly low levels of omega-3 PUFAs in people with mental illnessCitation23 including this sample,Citation24 we provided participants in the dietary intervention with fish oil supplements for 6 months. This paper reports the dietary changes that were achieved in a Mediterranean-style diet (MedDiet) intervention group versus a social (comparison) group, the impact on mental health, and correlations between improved mental health outcomes and changes in diet and erythrocyte (red blood cell) omega-3 and omega-6 PUFA concentrations.
Methods
The detailed study protocol is published elsewhere.Citation18 The trial was registered with the Australian New Zealand Clinical Trials Register (ACTRN12614000438651).
Participants
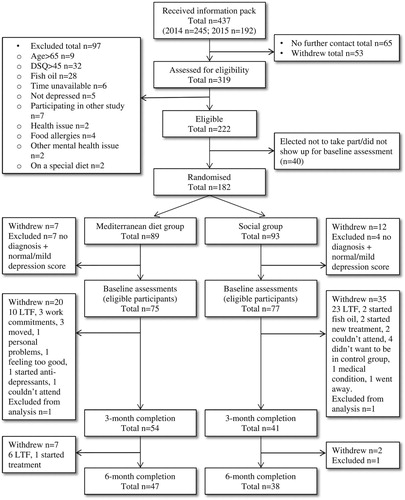
According to Cohen’s power analyses,Citation25 at least 60 people in each group are required to detect a medium effect size with 80% power (n = 120) at the usual 5% significance level. Allowing for an estimated 30% dropout rate the target sample size was n = 172. We recruited 182 adults with either GP diagnosed or self-reported depression over the previous 2 months or more (which has a moderate level of agreement with diagnosed depressionCitation26) in 2014 and 2015 via the community using newspaper advertisements, flyers, television and radio interviews, social media, and a market research agency. Of those eligible volunteers, 163 attended baseline assessments. Eleven participants retrospectively identified after baseline assessments as not having a depression diagnosis or a ‘moderate’ to ‘extremely severe’ score on the depression subscale of the Depression Anxiety Stress Scale (DASS – see below) were excluded from analyses, leaving a total sample size of 152. A CONSORT flow chart of participants through the study is provided in .
Ethics, consent, and permissions
Ethics approval was provided by the Human Research Ethics Committee of the University of South Australia (Registration no. 0000032674) and all participants provided written informed consent to take part in the study.
Procedure
Interested volunteers were screened for eligibility by phone. Inclusion criteria were age between 18 and 65 years and diagnosed or self-reported depressive symptoms over the previous 2 months or longer. People who took fish oil supplements or had a high diet quality score on an adapted dietary screening tool were excluded. If participants were receiving treatment for their depression they were asked to continue what they were doing. All participants were asked not to start any new treatment for the 6-month duration of the study. Eligible participants were sent detailed study information and a consent form via post or e-mail. On receipt of the signed consent form, they were scheduled to attend the Sansom Institute for Health Research clinic in Adelaide at the University of South Australia for baseline assessments. Before beginning baseline assessments participants were randomized by a team member not involved in screening or data collection to the MedDiet or Social group, blocked on age and gender, using the process of minimization.Citation27 Data collectors and participants were blinded to the treatment allocation until baseline assessments were completed. Investigators were blinded until after data were analyzed. Assessments were conducted at baseline, 3 and 6 months.
At baseline and 3-month assessments participants in the MedDiet group were given 3 months’ supply of fish oil capsules (2 per day, grade EPAX 1050 TB each containing 450 mg DHA and 100 EPA). All participants were scheduled for fortnightly group sessions at the university campus for three months. For the MedDiet group’s first visit they were given an interactive nutrition education session led by a dietitian, nutritionist and support study staff. For their subsequent fortnightly visits they took part in cooking workshops in a commercial kitchen at the university. Recipes focussed on simple, healthy, affordable, tasty meals using Mediterranean-style dietary principles. These had previously been trialled in cooking workshops in a pilot study with people suffering from severe mental illness, where positive dietary changes and improved cardiometabolic markers were achieved.Citation28 Following the cooking workshop, MedDiet participants were given food hampers that provided ingredients for the recipe that had been cooked, and in addition including 500 ml extra virgin olive oil, vegetables, fruit, tinned legumes, tinned tomatoes, tinned tuna and mixed nuts (almonds, walnuts, hazelnuts). They were also given a link to a website that provided recipes, resources and cooking videos, and a printed book of recipes. The comparison group attended a fortnightly ‘social’ group with nibbles provided (i.e. biscuits, cheese, dips, tea/coffee, and water/juice), held in tutorial rooms at the university to control for the social interaction component of the cooking workshops. These groups undertook a range of social activities such as playing games, sharing holiday photos, book club activities, and completing personality questionnaires. Therapeutic discussion about depressive symptoms was discouraged, although many participants formed friendships as a result of the groups (similarly to the MedDiet group during cooking workshops).
Measures
The Depression Anxiety Stress Scale (DASS-21) and the Assessment of Quality of Life (AQoL)-8D scores were the primary outcome measures. Secondary outcome measures included the Positive and Negative Affect Scale (PANAS), 14-item Mediterranean diet questionnaire, and the Simple Dietary Questionnaire (SDQ). These are described below. A sociodemographic and health behaviour questionnaire collected information on age, gender, education level (1 = completed primary school to 8 = postgraduate degree), household income, and sleeping difficulties (how many hours of sleep on average on weeknights and weekends; and whether or not they consider sleep to be a problem – yes/no/don’t know). Socioeconomic status was determined from participant postcodes using deciles of the Socio-Economic Indexes For Areas (SEIFA), a ranking of Australian neighbourhood disadvantaged and advantage, based on census data for variables such as education, income, and occupation status.Citation29
DASS-21
The DASS is a 21-item self-report scale that provides a measure of the level of negative emotional states of depression, anxiety, and stress. It is a highly reliable measure with high convergent validity and good internal consistency with a Cronbach alpha of 0.82–0.93.Citation30,Citation31 To identify degree of severity of these emotional states, DASS-21 sub-scale severity ratings were calculated based on the full DASS-42 severity ratingCitation32 – each scale is multiplied by two and divided into severity categories to yield equivalent scores ranging from 1 (normal) to 5 (extremely severe) for clinical purposes.
AQoL-8d
The AQoL-8D is a 35-item questionnaire that is used to measure QoL. The 35 items load onto eight dimensions, of which three represent physical domains of QoL (independent living, pain, and senses) and five represent psychological domains (happiness, self-worth, coping, relationships, mental health). These load onto two super dimensions (physical and psycho-social). The scores from each dimension can be further combined to create a total AQoL-8D utilities score for use in economic evaluation. The AQoL-8D has good validity and internal consistency with alpha coefficients of 0.89–0.96.Citation33
PANAS
The PANAS is a 20-item scale measuring positive and negative emotions. It has been validated and demonstrates reliable psychometric properties, discriminant, convergent and construct validity. The reliability (internal consistency) of the PANAS positive and negative emotions scales were previously determined to be α = 0.89 and 0.85, respectively.Citation34
Dietary questionnaires
A validated 14-item Mediterranean diet questionnaire was used to assess the level of adherence to the Mediterranean diet. Each item is scored as 0 or 1, yielding a maximum score of 14.Citation35 Higher scores on this questionnaire have been consistently associated with reduced risk of mortality from or incidence of CVD.Citation36
A SDQ measured the frequency of intake of a range of food groups including, for the purpose of this study, vegetables, fruit, legumes, wholegrain foods, takeaway foods (examples given were unhealthy options such as burgers, chips, pizza), sweetened drinks, unhealthy sweet and savoury snacks, fish, meat/chicken and nuts. For each question a picture of the food was provided and the portion size was described. For each food group, frequency of usual intake was reported using six to nine-item response scales ranging from never/don’t eat to consume seven or more serves per day. For vegetables, fruit, wholegrain foods, takeaway foods, snack foods, nuts, legumes, fish, and meat/chicken a further qualifying question presented a range of different items asking which of those had been consumed in the past 2 weeks, in order to help prompt memory about foods relevant to the previous item as well as to measure dietary diversity. For the purpose of this study diversity of fruit and vegetable consumption were measured because of the variety of bioprotective nutrients and phytonutrients provided by different fruits and vegetables.Citation37 Test–retest reliability of the SDQ over 1–2 weeks in a different sample (n = 66) ranged from r = 0.690 to r = 0.875 and validity coefficients with 24-hour recalls ranged from r = 0.256 to r = 0.569 with the majority greater than r = 0.400 (unpublished). The SDQ will be further validated against 3-day food diaries which participants from the present study completed on two week days and one weekend day at baseline.
Omega-3 fatty acids
Fasted blood samples were used to measure erythrocyte levels of n-3 PUFAs to quantify and separate the direct contribution of fish oil supplementation to any improved outcome measures. Fasted blood samples were collected in 6 ml EDTA tubes, red blood cells were separated from plasma by low-speed centrifugation and packed red blood cells were stored in 1 ml micro tubes at −80°C until analysis. Erythrocyte samples were thawed and prepared for fatty acid analysis according to Swierk et al.Citation38 using the direct transesterification procedure according to Lepage and Roy.Citation39 Samples were analysed by flame-ionization gas chromatography (model GC-17A, Shimadzu) using a 50 m × 0.25 mm internal diameter capillary column. One microlitre of the sample was auto-injected into the column, and individual fatty acids were quantified using the Shimadzu analysis software (Class-VP 7.2.1 SP1, USA). Fatty acid peaks were identified by comparison with known fatty acid standards and quantitated by comparison to the 21:0 internal standard (Nu-chek and Sigma).
Statistical analysis
Analyses were performed using IBM SPSS Version 21.0 for Windows (Chicago, IL, USA). Descriptive statistics (mean and standard deviation, M ± SD, or number/percentage for categorical variables, n/%) were used to provide baseline participant demographics, and t-tests or Chi-Square (categorical outcome) to check for differences between randomized groups. Empirical distributions were examined for continuous outcome variables to ensure that assumptions of normality are met. To analyse primary and secondary outcomes and determine the effect of the Mediterranean diet intervention, a linear mixed modelling approach with variance component structure was used to compare changes in the MedDiet and social groups over time; this process includes all data therefore allowing analysis on an intent-to-treat basis. To investigate whether changed dietary patterns were associated with any positive outcomes in mental health, changes in diet scores, omega-3 and omega-6 PUFA levels were entered into Pearson correlation analyses with changes in mental health outcome scores.
Results
Participants included in the analyses (with depression diagnosis and/or DASS depression score in the ‘moderate’ to ‘extremely severe’ range) were comprised of 105 females and 47 males aged between 18 and 65 years (M = 44 ± 13). This proportion reflects the approximate 2/1 ratio of depression incidence in women and men.Citation40 Thirty-eight per cent of participants reported a depression diagnosis and 36 per cent were taking anti-depressant medication. There was no statistically significant difference in age between those with (M = 46.5 ± 12.4) and without (M = 42.9 ± 13.2) a depression diagnosis (P = 0.095) and no significant difference in their baseline DASS depression score (22.60 ± 10.82 and 22.28 ± 8.53, respectively; P = 0.841) with both group means in the ‘extremely severe’ category (>14). Of those without a depression diagnosis, 86.4% ranked in the severe to extremely severe categories of the DASS depression scale compared with 86.0% of those with a diagnosis. Demographics and health-related data are broken down by treatment condition in . There were no statistically significant differences in demographic and health variables between groups, indicating successful randomization.
Table 1 Participant demographics and health status by treatment group (n = 152)
From the 152 eligible participants who commenced the study, 95 completed 3-month and 85 completed 6-month assessments (). Retention to 3 months was 72% for the MedDiet group and 53% for the social group (P = 0.013). Retention to 6 months (from baseline) was 63% in the MedDiet group and 49% in the social group (P = 0.068). Most volunteers who did not complete the 3-month assessments dropped out before attending their first workshop/social group. There was no statistically significant difference in severity of baseline DASS depression scores between those who completed 3-month assessments (M = 21.9 ± 8.97) and those who did not (M = 23.3 ± 10.15; P = 0.381). There was also no statistically significant difference in age, gender, SEIFA index, education, or household income between those who completed or did not complete 3 months.
Dietary changes
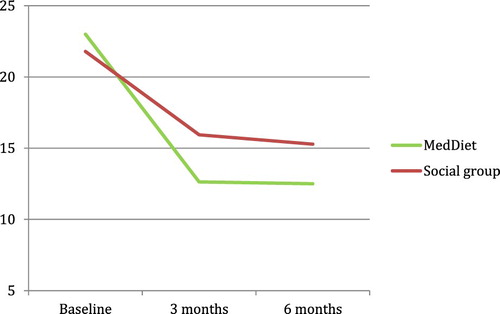
Changes in diet from baseline to 3 and 6 months in each condition are provided in . Compared to the social group, the MedDiet group reported significantly greater increase in their total Mediterranean diet scoreCitation35 from baseline to 3 months (see ), along with a significantly greater increase in consumption of vegetables, fruit, wholegrain foods, nuts and legumes, significantly lower consumption of unhealthy snacks and meat/chicken, and a greater diversity of vegetables. Both groups reported reduced sweetened drink intake which was not significantly different between the groups. These dietary changes were maintained at 6 months ().
Figure 2 Mediterranean diet scores in each group at baseline and 3 months (P < 0.001). Bars represent standard error of the mean.
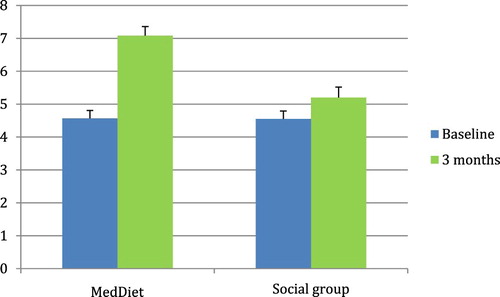
Table 2 Mediterranean diet and food group scores in Mediterranean diet (MedDiet) and Social groups at baseline, 3 and 6 months, and test of differences between groups using linear mixed modelling, n = 152 (MedDiet n = 75; social group n = 77)
Mental health outcomes
Both the MedDiet and the social group reported significantly improved mental health on all outcome measures (DASS, PANAS, and AQoL-8D subscales) over 3 months (all P < 0.001) except for the AQoL-8D pain value. Compared to the social group, the MedDiet group reported significantly greater improvement in their DASS depression score (, ), and AQoL-8D mental health score over 3 months. Depression scores improved by 45% in the MedDiet group and 26.8% in the Social group – equating to 1.68 times greater improvement in depressive symptoms in the MedDiet group. All changes were sustained at 6 months (; ).
Figure 3 DASS depression scores in each group at baseline and 3 months (P = 0.027). Bars represent standard error of the mean. Dotted line represents cut-off for ‘extremely severe depression’.
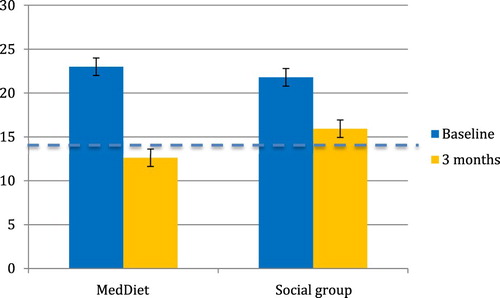
Table 3 Mental health and quality of life in Mediterranean diet (MedDiet) versus social groups at baseline, 3 and 6 months, and test of differences between groups using linear mixed modelling n = 152 (MedDiet n = 75; social group n = 77)
Correlations between dietary changes and mental health changes over 3 months
Over 3 months there were several statistically significant correlations between improved diet and better mental health, as shown in . Higher Mediterranean diet scores were significantly associated with lower depression, anxiety, negative affect and better coping and overall QoL. Higher vegetable consumption was associated with less stress and more positive emotions and happiness while higher fruit consumption was associated with less anxiety and more positive emotions and relationships. Higher intake of nuts was associated with reduced depression, anxiety and stress, and better mental health, self-worth and overall QoL. More legumes were associated with reduced anxiety, stress, negative emotions, and greater coping, psychosocial and overall QoL scores. Greater diversity of vegetables was associated with reduced depression, anxiety and negative emotions, and higher positive emotions, and along with greater diversity of fruits also with higher independent living, mental health, happiness, relationships, psychosocial and overall QoL. Reduced intake of takeaway food was associated with better pain and overall physical health QoL scores and reduced intake of unhealthy snacks was associated with improved mental health, coping and psychosocial QoL scores.
Table 4 Pearson correlations between changes in mental health and diet over 3 months (n = 95)
Correlations between erythrocyte polyunsaturated fatty acids and mental health
Correlations between changes in erythrocyte omega-3 and omega-6 PUFAs and mental health scores are shown in . Increased omega-3 PUFA eicosapentaenoic acid (EPA) was significantly associated with reduced anxiety and stress at 3 months and 6 months, and also with improved independent living, senses and physical health at 6 months. Increased omega-3 PUFA docosahexaenoic acid (DHA) was associated with reduced stress and negative emotions at 6 months. Decreased omega-6 PUFA arachidonic acid (AA) was associated with decreased stress and increased AQoL mental health, psychosocial and overall QoL at both 3 and 6 months as well as lower coping AQoL scores at 6 months. A reduced ratio of AA to EPA was associated with better pain, senses and physical health QoL scores at 6 months.
Table 5 Pearson correlations between changes in mental health and erythrocyte PUFAs over 3 and 6 months
Discussion
Over three months the MedDiet intervention significantly and substantially improved the diet quality of people with self-reported depression when compared with diet changes in the social group, with higher total Mediterranean diet scores and increased intake of vegetables, fruit, wholegrains, nuts, legumes and greater diversity of vegetables, along with lower intake of unhealthy snacks and meat/chicken. These dietary improvements were sustained at 6 months. Both groups reported significantly improved mental health outcomes across all measures over 3 months which were also sustained at 6 months. The MedDiet group reported significantly greater improvements in depression and overall mental health-related QoL compared to the social group. Improvements in a range of mental health outcomes were significantly correlated with improvements in diet over 3 months, most notably for greater diversity of vegetables and fruit and intake of legumes but also including higher Mediterranean diet score, vegetables, fruit and nuts and reduced consumption of unhealthy snacks, takeaway food, and meat.
The provision of free food has previously been shown to be successful in increasing intake. For instance, the PREDIMED study provided free nuts (walnuts, almonds, and hazelnuts) or olive oil to treatment groups, and showed that these groups consumed more of these foods.Citation16 This approach is compatible with behavioural economics and ‘nudging’ principles, i.e. using the path of least resistance, setting desirable defaults, making healthy food more available.Citation41 Along with education, goal setting, and menu ideas, continued exposure to and familiarity with healthy foods such as vegetables can increase liking and preference for that food.Citation42 Furthermore, learning basic cooking skills and hands-on learning of healthy recipes is empowering and has previously been associated with healthier food choices.Citation43,Citation44 We successfully applied these strategies using the HELFIMED protocol in a pilot study for people with serious mental illnessCitation28 and now in the present study. These skills, combined with the palatability and variety offered by a Mediterranean-style diet, may help to account for the sustained improvements shown over 6 months and potentially over the longer term.
To measure the impact of fish oil supplementation on mental health we measured erythrocyte omega-3 and omega-6 PUFAs. There were a small number of correlations between decreased AA (omega-6 PUFA), increased EPA and DHA and decreased ratio of AA/EPA and improved mental health over 3 and 6 months. We have observed previously that when fish oil is consumed and erythrocyte omega-3 PUFAs increase, the omega-6 levels decrease as they are displaced from the cell membranes.Citation45–47 Increased use of olive oil may have also reduced use of vegetable oils containing omega-6 PUFAs. The ratio of omega-6 to omega-3 PUFAs in cell membranes reflects dietary intake, which has a higher omega-6 to omega-3 ratio in Western diets compared to traditional diets globallyCitation48 and in Australia.Citation49 This can contribute to a pro-inflammatory state, given the inflammatory properties of eicosanoids produced by AA and anti-inflammatory properties of eicosanoids produced by EPA.Citation48 Furthermore, given the high concentration of DHA in neural membranes and its established role in a range of critical brain functions,Citation8 low omega-3 PUFA intake has been reflected in mental health outcomesCitation50 including depression.Citation51 The present study showed no significant correlation between increased omega-3 and improved depressive symptoms, although improved depression scores were associated with a decreased ratio of AA (omega-6) to EPA (omega-3). Improved depression was also significantly correlated with increased Mediterranean diet scores. A range of essential nutrients are required for healthy brain function and they also work synergistically; therefore improving the whole diet is likely to have far greater benefit for mental health than any single nutrient alone.Citation8 An interesting trial with elderly people with mild cognitive impairment recently discovered that reduced brain atrophy, and therefore risk of developing dementia, following Vitamin B supplementation was greatest in those adults who had adequate omega-3 levels.Citation52 This supports the contention that single nutrient trials are limited.
The improved mental health that was observed in both groups may in part be attributed to the social component of the study as both groups were exposed to group workshops (either cooking or social group). Furthermore, as all participants had depression there was an element of peer support in the group dynamic in both the social group and cooking workshops (where participants also share a meal together). Peer support, and particularly group-based peer support has been shown to be effective for treating depression, with equal efficacy to psychotherapy.Citation53 Nonetheless, there was evidence of greater improvement in the MedDiet group, consistent with population studies that have reported cross-sectional and longitudinal associations between poor diet and increased risk of depression, and conversely healthier diet and decreased risk.Citation13 This was supported in our study by multiple significant correlations between improved diet and mental health. The magnitude of benefit was large, with 60% fewer persons experiencing extremely severe levels of depression, 72% of anxiety and 69% of stress in the MedDiet group. The improved mental health in both groups is noteworthy, given that the Mediterranean diet is not just about healthy food – it is also about lifestyle, and this has been factored into the Mediterranean diet pyramid by including cultural and lifestyle elements such as conviviality and culinary activities.Citation10 Indeed, the cooking workshops we conducted previously with people who have serious mental illness were the most popular of all the workshops offered at Community Residential Care centres. As participants cooked and ate together, they progressively became more socially engaged as the workshops progressed.Citation28
Nonetheless, there are also well-described biological mechanisms that support a causal underpinning to the observed relationship between diet and mental health. Dietary nutrients – including vitamins, minerals, polyunsaturated fats and amino acids – are essential for healthy brain structure and function. Nutrients are required as cofactors for hundreds of different enzymes; they support metabolic pathways, neurotransmitter synthesis, cell signalling, myelin sheath maintenance, glucose and lipid metabolism, mitochondrial function, prevention of oxidation and more.Citation54,Citation55 Furthermore, factors that underpin poor physical health like inflammation, glucose intolerance, impaired cerebral blood flow and oxidative stress, also impact on mental health.Citation6,Citation8,Citation9,Citation55,Citation56 These factors are all related to poor diet.
This study is potentially limited by the fact that it was only single blinded, as participants could not be blinded to their treatment allocation. The measures and diet records are self-reported which cannot rule out expectation bias. Further, we recruited people with self-reported depression which may limit the generalizability to people with diagnosed depression – although there was no significant difference in severity of depression reported at baseline between those who were diagnosed or not. Drop out levels were relatively high, and more so in the social group, which may limit the generalizability of the results. We observed that many people dropped out from the social group because they had enrolled in the study in the hope of receiving dietary and cooking education, and expressed disappointment when advised of their group allocation after baseline assessments. Depression scores, gender, age, and income were not significantly different between those who completed 3-month assessments and those who dropped out. Strengths of the study include the study design; being a RCT; participants were instructed not to change any existing therapy or start any new therapy; and the 6-month follow up. Nonetheless, longer trials are needed to assess longer-term sustainability of the dietary changes and reduced depressive symptoms. We were able to correlate reported changes in diet/PUFAs and mental health outcomes to show that improvements were related to positive dietary and/or PUFA changes. Future studies with larger sample sizes could extend this with objective measures such as biological markers of improved dietary intake (e.g. carotenoids, urinary hydroxytyrosol) and underlying mechanisms for improved symptoms such as reduced inflammation, oxidation and increased brain-derived neurotrophic factor and correlating those with improved symptoms, as well as more robust inferential analyses (linear models for repeated measures adjusting for potential confounders). Importantly, we controlled for the social aspect of the cooking workshops (and research involvement more generally) to which people with depression can respond positively. Finally, statistical analysis included all cases, instead of being limited to cases with complete assessments over time.
This study supports preliminary findings from other dietary interventions that showed evidence of reduced depression in people with high CVD risk,Citation17 metabolic syndrome,Citation57 and unexpectedly in a trial of problem solving in elderly adults at risk for depression in the dietary arm that was used as a control.Citation58 Our study is one of the first RCTs to show benefits of healthier diet for mental health in a cohort of people with depression. Another Australian study was recently published, reporting improvements in depressive symptoms of people suffering major depressive disorder, and 32.3% achieving remission over 12 weeks.Citation59 In our study, the average depression score of the MedDiet group fell below the extremely severe depression cut-off, whereas in the social group it remained in the extremely severe range. Interestingly, while our study design was group based, the latter intervention involved one-on-one dietetic counselling in the dietary arm and ‘buddying’ as a control arm, and had similar findings. More studies with larger sample sizes and objective markers are required.
Westernized societies have developed an alarming culture of increased takeaway and ultra-processed food consumption which not only has dire health consequences but has also removed people from enjoying the whole process of growing, cooking, and enjoying good wholesome food together. With the increased personal, societal and financial burden of chronic physical and mental illness, getting back to basics by promoting cooking skills and family/group meals could be such a simple yet powerful and empowering approach to healthcare and prevention.
Disclaimer statements
Contributors None.
Conflicts of interest The authors report no conflicts of interest.
Ethics approval Human Research Ethics Committee, University of South Australia, 9 April 2014.
Acknowledgments
We are grateful to all participants who took part in the study; Caitlin Moss, Thomas Butler, Haruka Ishimoto and Lucy Fairlie-Jones for their assistance with cooking workshops and social groups; Judith Lukas and the School of Pharmacy and Medical Sciences for use of the commercial kitchen. Epax, Pathway International, Cobram Estate, John West, Edgell and Simplot provided in-kind supply of fish oil capsules, extra virgin olive oil and food hamper/cooking workshop items (legumes, tuna, tinned tomatoes), respectively; Tony & Marks provided fruit, vegetables and nuts at wholesale prices. The funders played no role in the study design or publication of results.
ORCID
Natalie Parletta http://orcid.org/0000-0003-2322-5555
Dorota Zarnowiecki http://orcid.org/0000-0003-0874-7830
Amy Wilson http://orcid.org/0000-0002-3855-0281
Svetlana Bogomolova http://orcid.org/0000-0003-4449-6514
Catherine Itsiopoulos http://orcid.org/0000-0003-1397-4149
Theo Niyonsenga http://orcid.org/0000-0002-6723-0316
Sarah Blunden http://orcid.org/0000-0002-5026-1992
Leonie Segal http://orcid.org/0000-0002-6391-6791
Bernhard Baune http://orcid.org/0000-0001-6548-426X
Additional information
Funding
References
- World Health Organisation. Global status report on noncommunicable diseases. Geneva: WHO Press; 2014.
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 2013 acute and chronic diseases and injuries in 188 countries, 1990–2103: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4
- Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry 2003;54(3):227–40. doi: 10.1016/S0006-3223(03)00587-0
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry 2010;67:446–57. doi: 10.1016/j.biopsych.2009.09.033
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med 2009;71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
- Pasco JA, Nicholson GC, Williams LJ, Jacka FN, Henry MJ, Kotowicz MA, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry 2010;197:372–7. doi: 10.1192/bjp.bp.109.076430
- Frasure-Smith N, Lespérance F, Julien P. Major depression is associated with lower omega-3 fatty acid levels in patients with recent acute coronary syndromes. Biol Psychiatry 2004;55:891–6. doi: 10.1016/j.biopsych.2004.01.021
- Parletta N, Milte CM, Meyer B. Nutritional modulation of cognitive function and mental health. J Nutr Biochem 2013;24(5):725–43. doi: 10.1016/j.jnutbio.2013.01.002
- Sinn N, Howe PRC. Mental health benefits of omega-3 fatty acids may be mediated by improvements in cerebral vascular function. Biosci Hypotheses 2008;1(2):103–8. doi: 10.1016/j.bihy.2008.02.003
- Bach-Faig A, Berry EM, Lairon D, Reguant J, Trichopoulou A, Dernini S, et al. Mediterranean diet pyramid today. Science and cultural updates. Pub Health Nutr 2011;14(12A):2274–84. doi: 10.1017/S1368980011002515
- Estruch R, Ros E, Salas-Salvado J, Covas M-I, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368(14):1279–90. doi: 10.1056/NEJMoa1200303
- Nordmann AJ, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle KR, Estruch R, et al. Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors. Am J Med 2011;124:841–51. doi: 10.1016/j.amjmed.2011.04.024
- Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr 2014;99:181–97. doi: 10.3945/ajcn.113.069880
- Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann Neurol 2013;74(4):580–91. doi: 10.1002/ana.23944
- Parletta N, Aljeesh Y, Baune BT. Health behaviours, knowledge, life satisfaction and wellbeing in people with mental illness across four countries and comparisons with normative sample. Front Psychiatry 2016. doi:10.3389/fpsyt.2016.00145.
- Zazpe I, Sanchez-Tainta A, Estruch R, Lamuela-Raventos RM, Schröder H, Salas-Salvado J, et al. A large randomised individual and group intervention conducted by registered dietitians increased adherence to Mediterranean-type diets: The PREDIMED study. J Am Diet Assoc 2008;108(7):1134–44. doi: 10.1016/j.jada.2008.04.011
- Sanchez-Villegas A, Martínez-Gonzalez MA, Estruch R, Salas-Salvadó J, Corella D, Covas M-I, et al. Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC Med 2013;11(208). doi:10.1186/741-7015-11-208.
- Zarnowiecki D, Cho J, Wilson AM, Bogomolova S, Villani A, Itsiopoulos C, et al. A 6-month randomised controlled trial investigating effects of Mediterranean-style diet and fish oil supplementation on dietary behaviour change, mental and cardiometabolic health and health-related quality of life in adults with depression (HELFIMED): study protocol. BMC Nutr 2016;2:e132. doi:10.1186/s40795-016-0095-1 doi: 10.1186/s40795-016-0095-1
- O’Neil A, Berk M, Itsiopoulos C, Castle D, Opie R, Pizzinga J, et al. A randomised, controlled trial of a dietary intervention for adults with major depression (the ‘SMILES’ trial): study protocol. BMC Psychiatry 2013;13. doi:10.1186/1471-244X-13-114):114.
- Kleinert S, Horton R. Rethinking and reframing obesity - comment. Lancet 2015. doi:10.1016/S0140-6736(15)60163-5.
- Johnson PM, Kenny PJ. Addiction-like reward dysfunction and compulsive eating in obese rats: role for dopamine D2 receptors. Nat Neurosci 2010;13(5):635–41. doi: 10.1038/nn.2519
- Deckersbach T, Das SK, Urban LE, Salinardi T, Batra P, Rodman AM, et al. Pilot randomized trial demonstrating reversal of obesity related abnormalities in reward system responsivity to food cues with a behavioural intervention. Nutr Diab 2014;4:e129. doi:10.1038/nutd.2014.26 doi: 10.1038/nutd.2014.26
- Milte C, Sinn N, Howe PRC. Polyunsaturated fatty acid status in ADHD, depression and dementia: towards an omega-3 index for mental health? Nutr Rev 2009;67(10):573–90. doi: 10.1111/j.1753-4887.2009.00229.x
- Parletta N, Zarnowiecki D, Cho J, Wilson A, Procter N, Gordon A, et al. People with schizophrenia and depression have a low omega-3 index. Prostaglandins Leukot Essent Fatty Acids 2016;110:42–7. doi: 10.1016/j.plefa.2016.05.007
- Cohen J. A power primer. Psychol Bull 1992;112(1):155–9. doi: 10.1037/0033-2909.112.1.155
- Stuart AL, Pasco JA, Jacka FN, Brennan SL, Berk M, Williams LJ. Comparison of self-report and structured clinical interview in the identification of depression. Compr Psychiatry 2014;55:866–9. doi: 10.1016/j.comppsych.2013.12.019
- Altman DG, Bland JM. Treatment allocation by minimisation. Br Med J 2005;330:843. doi: 10.1136/bmj.330.7495.843
- Bogomolova S, Zarnowiecki D, Wilson A, Fielder A, Procter N, Itsiopoulos C, et al. Dietary intervention for people with mental illness in South Australia. Health Promot Int 2016. doi:10.1093/heapro/daw055.
- Pink B. Socio-economic indexes for areas (SEIFA). Canberra: Australian Bureau of Statistics; 2011.
- Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 2005;44(2):227–39. doi: 10.1348/014466505X29657
- Crawford JR, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychol 2011;46(1):3–14. doi: 10.1111/j.1742-9544.2010.00003.x
- Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales, 2nd ed. Sydney: Psychology Foundation; 1995.
- Richardson J, Iezzi A, Khan MA, Maxwell A. Validity and reliability of the assessment of quality of life (AQoL)-8D multi-attribute utility instrument. Patient 2014;7(1):85–96. doi: 10.1007/s40271-013-0036-x
- Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 2004;43(3):245–65. doi: 10.1348/0144665031752934
- Martinez-Gonzalez MA, Garcia-Arellano A, Toledo E, Salas-Salvado J, Buil-Cosiales P, Corella D, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS ONE 2012;7(8):e43134. doi: 10.1371/journal.pone.0043134
- Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol 2014;25(1):20–6. doi: 10.1097/MOL.0000000000000044
- Slavin JL, Lloyd B. Health benefits of fruit and vegetables. Adv Nutr 2012;3:506–16. doi: 10.3945/an.112.002154
- Swierk M, Williams PG, Wilcox J, Russell KG, Meyer BJ. Validation of an Australian electronic food frequency questionnaire to measure polyunsaturated fatty acid intake. Nutrition 2011;27:641–6. doi: 10.1016/j.nut.2010.06.011
- Lepage G, Roy CC. Direct transesterification of all classes of lipids in a one-step reaction. J Lipid Res 1986;27:114–20.
- Kessler RC. Epidemiology of women and depression. J Affect Disord 2003;74(1):5–13. doi: 10.1016/S0165-0327(02)00426-3
- Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA 2007;298(20):2415–7. doi: 10.1001/jama.298.20.2415
- Cooke L. The importance of exposure for healthy eating in childhood: a review. J Hum Nutr Diet 2007;20(4):294–301. doi: 10.1111/j.1365-277X.2007.00804.x
- Hartmann C, Dohle S, Siegrist M. Importance of cooking skills for balanced food choices. Appetite 2013;65:125–31. doi: 10.1016/j.appet.2013.01.016
- Larson NI, Perry CL, Story M, Neumark-Sztainer D. Food preparation by young adults is associated with better diet quality. J Am Diet Assoc 2006;106(12):2001–7. doi: 10.1016/j.jada.2006.09.008
- Milte CM, Parletta N, Buckley J, Coates A, Young R, Howe P. Increased erythrocyte eicosapentaenoic acid and docosahexaenoic acid are associated with improved attention and behaviour in children with ADHD in a 12-month randomised controlled three-way crossover trial. J Atten Disord 2015;19(11):954–64. doi: 10.1177/1087054713510562
- Milte CM, Parletta N, Buckley JD, Coates AM, Young RM, Howe PRC. Eicosapentaenoic and docosahexaenoic acids, cognition, and behavior in children with attention deficit hyperactivity disorder: A randomized controlled trial. Nutrition 2012;28(6):670–7. doi: 10.1016/j.nut.2011.12.009
- Sinn N, Milte CM, Street SJ, Buckley JD, Coates AM, Petkov J, et al. Effects of omega-3 fatty acids, EPA v. DHA, on depressive symptoms, quality of life, memory and executive function in older adults with mild cognitive impairment: A 6-month randomised controlled trial. Br J Nutr 2012;107(11):1682–93. doi: 10.1017/S0007114511004788
- Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med 2008;233(6):674–88. doi: 10.3181/0711-MR-311
- Meyer BJ, Mann NJ, Lewis JL, Milligan GC, Sinclair AJ, Howe PRC. Dietary intakes and food sources of omega-6 and omega-3 polyunsaturated fatty acids. Lipids 2003;38:391–8. doi: 10.1007/s11745-003-1074-0
- Sinn N, Milte C, Howe PRC. Oiling the brain: A review of randomised controlled trials of omega-3 fatty acids in psychopathology across the lifespan. Nutrients 2010;2(2):128–70. doi: 10.3390/nu2020128
- Stahl LA, Begg DP, Weisinger RS, Sinclair AJ. The role of omega-3 fatty acids in mood disorders. Curr Opin Investig Drugs 2008;9(1):57–64.
- Jernerén F, Elshorbagy AK, Oulhaj A, Smith SM, Refsum H, Smith AD. Brain atrophy in cognitively imparied elderly: the importance of long-chain ω-3 fatty acids and B vitamin status in a randomized controlled trial. Am J Clin Nutr 2015. doi:10.3945/ajcn.114.103283.
- Pfeiffer PN, Heisler M, Piette JD, Rogers MAM, Valenstein M. Efficacy of peer support interventions for depression: a meta-analysis. Gen Hosp Psychiatry 2011;33(1):29–36. doi: 10.1016/j.genhosppsych.2010.10.002
- Kaplan BJ, Crawford SG, Field CJ, Simpson JSA. Vitamins, minerals and mood. Psychol Bull 2007;133(5):747–60. doi: 10.1037/0033-2909.133.5.747
- Kaplan BJ, Rucklidge JJ, Romjin A, McLeod K. The emerging field of nutritional mental health: inflammation, the microbiome, oxidative stress, and mitochondrial function. Clin Psychol Sci 2015. doi:10.1177/2167702614555413:1017.
- Agrawal R, Gomez-Pinilla F. ‘Metabolic syndrome’ in the brain: deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signalling and cognition. J Physiol 2012;590(10):2485–99. doi: 10.1113/jphysiol.2012.230078
- Perez-Cornago A, Lopez-Legarrea P, de la Iglesia R, Lahortiga F, Martinez JA, Zulet MA. Longitudinal relationship of diet and oxidative stress with depressive symptoms in patients with metabolic syndrome after following a weight loss treatment: the Resmena Project. Clin Nutr 2014;33:1061–7. doi: 10.1016/j.clnu.2013.11.011
- Stahl ST, Albert SM, Dew MA, Lockovich MH, Reynolds CF. Coaching in healthy dietary practices in at-risk older adults: a case of indicated depression prevention. Am J Psychiatry 2014;171(5):499–505. doi: 10.1176/appi.ajp.2013.13101373
- Jacka FN, O’Neil A, Itsiopoulos C, Opie R, Cotton S, Mohebbi M, et al. A randomised, controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med 2017;15:181. doi:10.1186/s12916-017-0791-y doi: 10.1186/s12916-017-0791-y