Abstract
Background
Clinical decision-making is a core competency of the nursing role, with nurses having to make decisions surrounding patient care and patient safety daily. With decision-making being linked to psychological outcomes, it is important to consider potential areas that may support or hinder nurses’ wellbeing whilst navigating clinical decisions.
Aim
The present study sought to investigate the relationship between clinical decision-making and moral distress, and further explore the role of personality, perfectionism, philotimo (a virtue describing the desire to do right by oneself and others, aligning with one’s sense of morality), and self-compassion.
Design
An online cross-sectional survey was conducted using Qualtrics. Associations between clinical decision-making and moral distress, burnout, personality, perfectionism, philotimo, and self-compassion were examined using univariate and multivariate statistics.
Methods
One hundred and forty-three nurses from the United Kingdom completed an online questionnaire. Eligibility criteria included individuals who had practised in the nursing profession for a minimum of six months. To ensure that all participants were practising across the United Kingdom, the eligibility criteria was made clear in the study advertisement, and the consent form. The consent form required participants to confirm that they reached these criteria to proceed with the study.
Results
Results revealed that clinical decision-making was associated with moral distress experience, and that both openness to experience, and philotimo mediated this relationship, independently. In addition to this, self-compassion was significantly associated with clinical decision-making across senior banded nursing roles, but this was non-significant for junior banded nursing roles.
Conclusion
Findings highlight the role of individual differences when looking at the impact of clinical decision-making upon nurses’ wellbeing and offers explanation for any variance in moral distress experience across nursing professionals. This research identifies fundamental differences between junior and senior nurses in relation to clinical decision-making and self-compassion that should be considered in future research.
Impact statement
This study addresses the impact of clinical decision-making on nurses’ wellbeing, and highlights the role of individual differences, particularly openness to experience and philotimo characteristics.
Plain language summary
In the nursing profession, making crucial decisions about patient care, safety, and treatment plans is a daily challenge. This study sheds light on the impact of these decisions on nurses’ wellbeing, focusing on the emotional burden of moral distress. The research reveals that nurses’ personalities play a role in determining whether they experience moral distress, identifying those at higher risk. This study also found that there were differences between junior and senior nurses in terms of being self-compassionate during these challenging moments, providing potential future solutions for some nursing staff. A larger sample of senior nurses is required to support these findings further.
Introduction
Clinical decision-making is central to the nursing role, with nurses having to utilise their clinical judgement, intuition, and higher-order cognitive skills to optimise patient care (Johansen & O'Brien, Citation2016; Manetti, Citation2018; Smith et al., Citation2008; Thompson et al., Citation2004). Concerningly, nurses report feeling alone, uncertain, and at times, like they had to go against their own conscience when navigating these decisions (Grönlund et al., Citation2015). Moral conflicts such as these have been coined ‘ethical dilemmas’ and occur when barriers prevent nurses from carrying out what they believe is the morally correct action (Haahr et al., Citation2020; Rainer et al., Citation2018). Frequent or unresolved exposure to ethical dilemmas has been linked to moral distress (Rathert et al., Citation2016).
Moral distress describes the psychological unease that arises when an individual identifies an ethically correct action to take but is constrained from implementing these in reality (British Medical Association, Citation2021). Across the nursing profession moral distress has been linked to depression, anxiety, and burnout (Petrișor et al., Citation2021; Smallwood et al., Citation2021). Burnout not only impacts individuals but also predicts greater infection rates, reduced patient safety and intention to leave the profession (Dall’Ora et al., Citation2020). Individual characteristics and values significantly influence nurses’ experience and susceptibility to moral distress (Kovanci & Akyar, Citation2022; Montoya et al., Citation2019), and it is likely that a person’s idea of morality, specifically moral judgment is a key factor in the experience of moral distress. The concept of Philotimo may therefore offer a novel understanding of moral distress, given its emphasis on social and moral virtues (Hatzimalonas, Citation2018). A person embodying philotimo is described as virtuous, dependable, respectful, self-sacrificing, and dedicated to fulfilling their obligations and duties (Hatzimalonas, Citation2018). These values are consistent with many nursing principles (Nursing & Midwifery Council, Citation2015, Citation2022), and so philotimo may add insight when exploring the role of individual differences in nurses’ decision-making.
Personality is a significant predictor of both decision-making and wellbeing, with evidence suggesting that more emotion-driven personality traits, such as neuroticism are related to increased decision-making difficulties and a lower tolerance for psychological distress (Martincin & Stead, Citation2015; Warbah et al., Citation2007). Perfectionism is a trait that has been implicated in stress and wellbeing outcomes (Smith et al., Citation2017; Smith et al., Citation2018) and is characterised by excessively high standards and critical evaluations of oneself and others. Perfectionism is a multidimensional concept, which can lead to adaptive and maladaptive outcomes (Frost et al., Citation1990; Hewitt & Flett, Citation1991; Stoeber et al., Citation2020). Maladaptive perfectionism has been linked to higher stress reactivity, depression, decision-making difficulties, and an increased reluctance to seek help for psychological distress (Chen et al., Citation2022; Ey et al., Citation2000; Flett et al., Citation2016). Crane et al. (Citation2015) found trait perfectionism to enhance individual vulnerability to distress in a veterinarian population in morally challenging events such as performing convenience euthanasia on animals. Montoya et al. (Citation2019) concluded that trait perfectionism significantly increased the risk of developing moral distress from moral conflicts. Nurses regularly face morally complex situations within their profession therefore exploring associations between perfectionism and moral distress is relevant.
Research evidence shows that maladaptive perfectionism is associated with diminished levels of self-compassion (Stoeber et al., Citation2020) suggesting a pathway for the noted adverse correlations with stress, depression and decision-making difficulties and offering a means to support wellbeing. Self-compassion has been identified as a ‘buffer’ against negative life experiences and poorer psychological health outcomes (Játiva & Cerezo, Citation2014), implicating its relevance in healthcare, where such challenges are encountered daily. Despite this, existing research is yet to examine the role of self-compassion in nurses’ clinical decision-making and moral distress experience. The present study therefore explores the role of self-compassion, perfectionism, philotimo and personality in relation to clinical decision-making, with the goal of supporting nurses’ decision-making, and mitigating any impact on wellbeing.
Methods
Design
An online cross-sectional survey was conducted using Qualtrics. The survey platform was trialled by the research team prior to data collection.
Setting and sample
This online study was conducted across the United Kingdom (UK) from October to November 2022. Non-probability volunteer and snowball sampling were utilised to recruit 143 UK nurses. This sampling strategy was selected due to its effectiveness when targeting specific populations, such as nurses, at a relatively low cost (Acharya et al., Citation2013). Participants were recruited through social media platforms (Facebook, X). Eligibility criteria included individuals who had practised in the nursing profession for a minimum of six months. With Cowin and Hengstberger-Sims (Citation2006) reporting that it takes six months for nurses to develop the confidence to apply their knowledge, this criterion ensures that participants have sufficient experience of decision-making to complete the questionnaire. The eligibility criteria were made clear in both the study advertisement and participant information sheet. All participants indicated that they were currently practising across the UK in the consent form provided prior to taking part in the study. Fritz and MacKinnon (Citation2007) suggest that 148 participants were required for the present study. The sample size fell marginally below this value due to incomplete responses (n = 16), however, 143 participants significantly exceed estimates of 115 and 116 for alpha and beta paths of the mediations at medium effect (Fritz & MacKinnon, Citation2007).
Materials
The present study utilised several questionnaires for data collection. The estimated completion time for the final survey was 30–40 min, which was made clear in the participant information sheet.
The Clinical Decision-making in Nursing Scale-40 (CDMNS-40; Jenkins, Citation1985) utilises 40 items to measure nurses’ perceptions of decision-making ability. The CDMNS-40 has four subscales: search for alternatives or options, canvassing of objectives and values, evaluating and re-evaluation of consequences, search for information and unbiased assimilation of new information. Items include ‘I consider even the remotest consequences before making a choice’. Responses range from 1 (never) to 5 (always). Higher scores indicate greater perceptions of clinical decision-making ability. Cronbach’s alpha for this study was α = .764 for the total score, α = .429 search for alternatives or options, α = .486 for canvassing of objectives and values, α = .580 for evaluating and re-evaluation of consequences, α = .293 for search for information and unbiased assimilation of new information. Each subscale demonstrated low internal consistency (Tavsancil, Citation2006) and was therefore not used in the final analysis. Instead, the sum of each item was calculated to develop a total score, which was utilised throughout all data analyses.
The Clinical Decision-making in Nursing Scale-13 (CDMNS-13; Miley et al., Citation2023) is a revised version of Jenkins's (Citation1985) scale, which utilises 13 of the original items to measure nurses' clinical decision-making ability. This shortened scale is a global clinical decision-making measure that allows for the use of more materials in a research context, thus supporting understanding of the construct. Responses range from 1 (never) to 5 (always). Higher scores indicate higher perceptions of clinical decision-making ability. Cronbach’s alpha for this study was α = .693. The CDMNS-13 has been reported in parallel to the CDMNS-40 and is presented in parentheses throughout the results section.
The Moral Distress Scale-revised (MDS-R; Hamric et al., Citation2012) utilises 21 items to assess moral distress experienced by healthcare workers. Participants are required to rate their experience of statements in terms of frequency and intensity. Statements include ‘Witness diminished patient care quality because of poor team communication’. Responses range from 0 (none) to 4 (a great extent). Higher scores indicate higher levels of moral distress. Internal consistency for this study was α = .888.
The Sussex-Oxford Compassion Scale for Self (SOCS; Gu et al., Citation2020) utilises 20 items to assess self-compassion. The SOCS has five subscales: recognising suffering, understanding the universality of suffering, feeling for the person suffering, tolerating uncomfortable feelings, acting or being motivated to act to alleviate suffering. Items include, ‘I’m good at recognising when I’m feeling distressed’. Responses range from 1 (not at all true) to 5 (always true). Higher scores indicate greater levels of self-compassion. Internal consistency for this study was α = .921, α = .850 for recognising suffering, α = .775 for understanding the universality of suffering, α = .825 for feeling for the person suffering, α = .802 for tolerating uncomfortable feelings, and α = .851 for acting or being motivated to act.
The HEXACO Personality Inventory-Revised (HEXACO-PI-R; Ashton & Lee, Citation2009) utilises 60 items to assess individual personality dimensions. The HEXACO-PI-R has six subscales; honesty-humility, emotionality, extraversion, agreeableness, conscientiousness, and openness to experience. Sample items include, ‘People often call me a perfectionist’. Responses range from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate a higher prevalence of each personality dimension. Internal consistency for this study was α = .683 for honesty-humility, α = .609 for emotionality, α = .837 for extraversion, α = .737 for agreeableness, α = .708 for conscientiousness, α = .758 for openness to experience. The low reliability score observed for the honesty-humility facet of personality, alongside a low item-total correlation, indicated that item 42 was problematic. Therefore, this item was removed from the subscale to increase the internal consistency to .690. Likewise, the low reliability score observed for the emotionality subscale, alongside low item-total correlations, indicated that items 5 and 53 were problematic. We therefore removed these items from the subscale to increase the internal consistency to .695.
The Big-three Perfectionism Scale Short-form (BTPS-SF; Feher et al., Citation2019) utilises 16 items to assess individual perfectionism. The BTPS-SF has three subscales: rigid perfectionism, self-critical perfectionism, narcissistic perfectionism. Items include ‘It is important to me to be perfect in everything I attempt’. Responses range from 1 (disagree strongly) to 5 (agree strongly). Higher scores indicate greater levels of perfectionism. Internal consistency for this study was α = .918 for rigid perfectionism, α = .885 for self-critical perfectionism, and α = .800 for narcissistic perfectionism.
The Philotimo Scale (Mantzios, Citation2021) utilises 5 items to measure personality traits consistent with philotimo. Items include ‘I find it principled to help others even if I get stuck in a difficult situation’. Responses range from 1 (not at all like me) to 5 (extremely like me). Higher scores indicate greater traits of philotimo. Internal consistency for this study was α = .871.
Procedure
Participants responded to an online invitation posted on social media platforms (X, Facebook) to take part in the study. They received a short introduction to the study before being directed to Qualtrics to complete the survey. Participants were initially presented with an information sheet and consent form. Participants were asked to indicate that they had read the consent form, and further continuation of the study implied consent. Having given consent, participants were presented with a short demographic questionnaire, before being directed to the online survey. Upon completion, participants were directed to a debrief form.
Ethical approval
Ethical approval was obtained from Birmingham City University’s ethics committee (approval number, Miley/#10414/sub1/R(C)/2022/Mar/BLSSFAEC). Informed consent was obtained from all participants.
Data analysis
Data analysis was conducted using IBM SPSS 28. All surveys were screened for completeness. Any responses with missing data were excluded from the final analysis (n = 16). Descriptive statistics including means, standard deviations, and frequencies were obtained to describe sample characteristics. The relationships between all study variables were examined using Pearson’s bivariate correlations. Preliminary analyses and visual inspection of residual scatterplots suggested that the necessary assumptions for both regression and mediation analyses were met, including normality of data, linearity, homoscedasticity, independent errors, and no multicollinearity. Linear regression analyses were conducted to offer further insight into the strength of the relationships identified in correlation analyses. Given the exploratory nature of the present study, mediation analyses were deemed appropriate to develop a better understanding into the variable interactions and explore what factors influence the relationship between clinical decision-making and well-being. Mediation effects were determined using Hayes’ (Citation2017) PROCESS macro (model 4) with a bootstrap sample of 5000. Statistical significance was determined when p < .05.
Results
Descriptive statistics
The sample consisted of 143 nurses (Mdnage = 46, range: 24–64). Female participants made up 91.6% (n = 131/143) of the sample, with just 7.7% (n = 11/143) identifying as male (non-binary, n = 1/143, 0.7%). Most nurses within the sample practised full-time (Mdn = 37.5, range: 8–60) and were in a senior nursing position (62%, n = 89/143). For the present study, junior nursing roles were categorised as band 5 and included newly qualified staff and staff nurses. Senior banded nurses were categorised as band 6 and above and included senior staff nurses, advanced nurse practitioners and chief nurses. See for summary.
Table 1. Descriptive statistics.
Bivariate correlations revealed that CDMNS-40 was negatively associated with moral distress experience (r = −.233, p = .005; CDMNS-13: r = −.274, p < .001). Regarding personality, honesty-humility (r = .233, p = .005; CDMNS-13: r = .244, p = .003), conscientiousness (r = .346, p < .001; CDMNS-13: r = .314, p < .001), and openness (r = .252, p = .002; CDMNS-13: r = .209, p = .012) were significantly associated with CDMNS-40. Higher scores on these dimensions were associated with increased decision-making ability. Similarly, higher philotimo scores were associated with greater perceptions of decision-making ability (r = .385, p < .001; CDMNS-13: r = .332, p < .001). However, higher narcissistic perfectionism scores were associated with lower perceptions of decision-making ability (CDMNS-13: r = −.209, p = .012).
Interestingly, only the emotionality dimension of personality was significantly associated with moral distress experience (r = .169, p = .043), in a positive linear direction. A further inspection into nurses’ seniority revealed that self-compassion was only significantly associated with moral distress experience amongst senior nurses (r = −.317, p = .002) ().
Table 2. Bivariate correlations between clinical decision-making, moral distress, self-compassion, personality, perfectionism, and philotimo (n = 143).
A regression model used CDMNS-40 as the outcome variable, and the HEXACO personality dimensions, philotimo, and perfectionism as predictors. The model was statistically significant F(10, 132) = 6.01, p < .001 and predictive capacity calculated through R2 adj. was .261. Results revealed that openness to experience (B = .176, p = .020, 95% CI: 0.47, 5.39), conscientiousness (B = .317, p < .001, 95% CI: 3.33, 10.08), and philotimo (B = .309, p < .001, 95% CI: 0.39, 1.21) demonstrated significant predictive abilities (see ). Similar findings were reported with the CDMNS-13 (see ).
Table 3. Summary of the predictive capability of personality, perfectionism, and philotimo upon scores on the CDMNS-40 (n = 143).
Table 4. Summary of the predictive capability of personality, perfectionism, and philotimo upon scores on the CDMNS-13 (n = 143).
A second regression model, utilising only the senior sample of nurses (n = 89/143) investigated the predictive capabilities of self-compassion upon moral distress. The model was statistically significant F (5, 83) = 3.41, p = .008 and predictive capacity calculated through adjusted R2 was .120. Results revealed that understanding universality of suffering (B = −6.92, p = .029, 95% CI: −13.09, −0.74) and tolerating uncomfortable feelings (B = −7.31, p = .043, 95% CI: −14.38, −0.25) demonstrated significant predictive abilities (see ).
Table 5. Summary of the predictive capability of self-compassion upon moral distress in the senior nursing sample (n = 89).
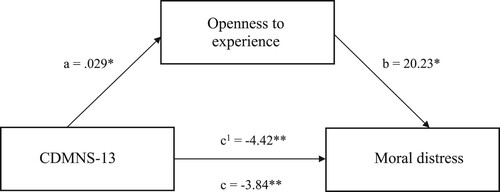
Mediation analyses examined the direct and indirect effects of clinical decision-making on moral distress via the personality dimension ‘openness to experience’. Findings suggest that CDMNS-40 had a significant direct effect on moral distress (B = −1.75, p < .001, 95% CI: −2.76, −0.738), and this remained significant when exploring this effect via openness to experience (B = .315, 95% CI: 0.033, 0.691). These results are summarised in . Similarly, the direct and indirect effects of CDMNS-40 on moral distress via philotimo were examined using mediation analyses. CDMNS-40 had a significant direct effect on moral distress (B = −1.97, p < .001, 95% CI: −3.03, −0.913), and this remained significant when exploring this effect via philotimo (B = .536, 95% CI: 0.109, 1.01). Therefore, both openness to experience and philotimo significantly mediate the relationship between CDMNS-40 and moral distress (see ). Similar findings were observed with the CDMNS-13 (see and ).
Figure 1. The mediating effect of philotimo in the relationship between CDMNS-40 and moral distress. Note: All presented effects are unstandardised; a is the effect of clinical decision-making upon philotimo; b is the effect of philotimo on moral distress; c1 is the direct effect of clinical decision-making on moral distress: c is the total effect of clinical decision-making on moral distress. * p < .05, ** p < .01. Note: MD - scores on the moral distress scale-revised.
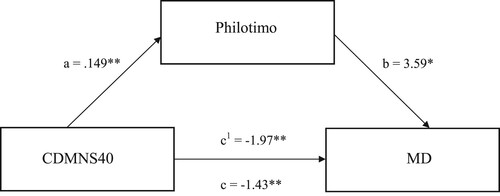
Figure 2. The mediating effect of philotimo in the relationship between CDMNS-13 and moral distress. Note: All presented effects are unstandardised; a is the effect of clinical decision-making upon philotimo; b is the effect of philotimo on moral distress; c1 is the direct effect of clinical decision-making on moral distress: c is the total effect of clinical decision-making on moral distress. * p < .05, ** p < .01.
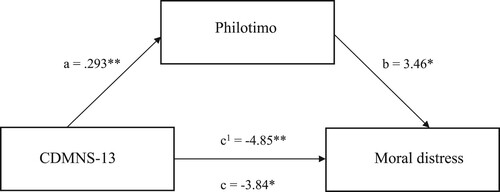
Figure 3. The mediating effect of openness to experience in the relationship between CDMNS-40 and moral distress. Note: All presented effects are unstandardised; a is the effect of clinical decision-making upon openness to experience; b is the effect of openness to experience on moral distress; c1 is the direct effect of clinical decision-making on moral distress: c is the total effect of clinical decision-making on moral distress. * p < .05, ** p < .01. Note: Openness to experience – subscale of the HEXACO-PI-R (higher scores represent higher traits of openness to experience); MD - scores on the moral distress scale-revised.
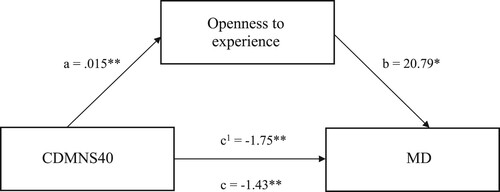
Figure 4. The mediating effect of openness to experience in the relationship between CDMNS-13 and moral distress. Note: All presented effects are unstandardised; a is the effect of clinical decision-making upon openness to experience; b is the effect of openness to experience on moral distress; c1 is the direct effect of clinical decision-making on moral distress: c is the total effect of clinical decision-making on moral distress. * p < .05, ** p < .01. Note: Openness to experience – subscale of the HEXACO-PI-R (higher scores represent higher traits of openness to experience).
Discussion
The present study sought to explore the relationship between clinical decision-making and wellbeing across the nursing population and examine the effect of personality, philotimo, and perfectionism on clinical decision-making ability. Findings indicate that clinical decision-making ability is associated with moral distress across this population, with lower perceived decision-making ability lending itself to increased moral distress experience. This confirms that decision-making is significantly associated with nurses’ wellbeing and offers potential insight as to why moral distress prevalence is elevated across nursing roles (Berhie et al., Citation2020; Mehlis et al., Citation2018).
In line with existing research into perfectionism and decision-making more broadly, narcissistic perfectionism was significantly negatively associated with nurses clinical decision-making ability (Chen et al., Citation2022; Wang et al., Citation2020). A central theme of narcissistic perfectionism is the quest for the ‘perfect self’ and that any kind of imperfection is intolerable (Flett et al., Citation2014). Given these unrealistic expectations, it is unsurprising that scoring high in these traits is associated with lower perceptions of decision-making ability, as it is not possible to reach such personal standards. The observed relationship may therefore be understood by the critical outlook upon one’s own behaviour and an inability to achieve unrealistic expectations regarding decision-making.
Regarding individual differences, the honesty-humility, openness to experience, and conscientiousness dimensions of personality were positively associated with clinical decision-making ability. These elements are deemed indicators of moral character, relating to justice, fairness, and care (Kim & Cohen, Citation2015; Međedović & Petrović, Citation2016; Ścigała et al., Citation2020; Webster et al., Citation2021). Furthermore, openness and honesty are coined as the professional standards for good medical practice (Nursing & Midwifery Council, Citation2022). It is therefore unsurprising that scoring high in these traits is associated with increased decision-making abilities. Furthermore, openness to experience significantly mediated the relationship between clinical decision-making and moral distress, suggesting that being open to new experiences, may reduce associations between moral distress and clinical decision-making. This aligns with existing literature which emphasises the positive influence of openness traits on wellbeing and self-efficacy (Audet et al., Citation2021).
Additionally, philotimo was positively associated with clinical decision-making ability, and further mediated its relationship with moral distress. Given that philotimo encompasses the virtues of respect, honesty, benevolence, and moral responsibility (Mantzios, Citation2021), the findings of the present study align with previous literature outlining the positive associations between these areas and wellbeing (Aghababaei et al., Citation2016; Aghababaei & Arji, Citation2014; Martela & Ryan, Citation2016; Weziak-Bialowolska et al., Citation2021). Recognising the significance of philotimo within the healthcare environment prompts upcoming research to explore concepts of morality and integrity to broaden the potential impact of clinical decision-making.
Contrary to expectations, self-compassion did not relate to clinical decision-making or moral distress within this study. This opposes existing literature where self-compassion has been shown to predict both decision-making competency and wellbeing (Bailis et al., Citation2021; Homan, Citation2016; McKay & Walker, Citation2021). Further inspection into this relationship revealed that self-compassion was only significantly negatively associated with moral distress experience across senior banded nurses. One possible explanation for this is level of education. Joy et al. (Citation2023) found that senior nursing roles tended to possess a greater education level, and that this allowed for greater reflection, and subsequently increased self-compassion awareness. The interaction observed within this study may therefore be understood through nurses’ education level; perhaps prompting healthcare organisations to encourage education opportunities if the benefits of self-compassion are to occur. However, self-compassion remained a non-significant moderator of the relationship between clinical decision-making and moral distress across senior roles. This may be explained by the strike action that took place within the National Health Service during the period of this study. Andrews et al. (Citation2020) found that to be self-compassionate, nurses needed a ‘stable base’ where they felt safe and secure in the workplace. The strike action evoked major changes within the healthcare system, preventing nurses from achieving this (Booth, Citation2022). The unexpected findings regarding self-compassion may be an indirect result of nurses’ industrial action.
There were two limitations to the present study. First, when observing differences between junior and senior nurses, the sample sizes did not reach desirable power estimates for further regression analyses (Cohen, Citation1992). Therefore, replicating this study with a larger sample of senior nurses is essential to provide more precise estimations of interactions, and validate the conclusions drawn. Second, the present study is cross-sectional. It is beyond the scope of cross-sectional studies to infer cause and effect; future research should utilise a more experimental design to allow inferences to be made about the role of personality and self-compassion on clinical decision-making and moral distress.
Conclusion
Findings from the present study should inform future research and practice in aiming to mitigate the impact of clinical decision-making on nurses’ wellbeing. Recognising the influence of openness to experience and philotimo characteristics on the relationship between clinical decision-making and moral distress highlights the importance of acknowledging the role of individual differences when supporting nurses with clinical decision-making. Further consideration should be applied to potential differences between junior and senior nurses. Although sample sizes were limited in the present research, key differences between these two populations regarding the relationship between clinical decision-making and self-compassion require further consideration. This study emphatically underscores the significance of individual differences, specifically openness to experience and philotimo characteristics, in understanding the impact of clinical decision-making on nurses’ wellbeing, providing crucial insights for shaping future research and enhancing practical support and education in the field.
Ethics approval
Approval was obtained from Birmingham City University’s ethics committee (Approval number, Miley/#10414/sub1/R(C)/2022/Mar/BLSSFAEC). Approval letter has been submitted as a supplementary file.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Acharya, A. S., Prakash, A., Saxena, P., & Nigam, A. (2013). Sampling: Why and how of it. Indian Journal of Medical Specialties, 4, 330–333.
- Aghababaei, N., & Arji, A. (2014). Well-being and the HEXACO model of personality. Personality and Individual Differences, 56, 139–142. https://doi.org/10.1016/j.paid.2013.08.037
- Aghababaei, N., Błachnio, A., Arji, A., Chiniforoushan, M., Tekke, M., & Fazeli Mehrabadi, A. (2016). Honesty–humility and the HEXACO structure of religiosity and well-being. Current Psychology, 35, 421–426. https://doi.org/10.1007/s12144-015-9310-5
- Andrews, H., Tierney, S., & Seers, K. (2020). Needing permission: The experience of self-care and self-compassion in nursing: A constructivist grounded theory study. International Journal of Nursing Studies, 101, 5–9. https://doi.org/10.1016/j.ijnurstu.2019.103436.
- Ashton, M. C., & Lee, K. (2009). The HEXACO–60: A short measure of the major dimensions of personality. Journal of Personality Assessment, 91(4), 340–345. https://doi.org/10.1080/00223890902935878
- Audet, ÉC, Levine, S. L., Metin, E., Koestner, S., & Barcan, S. (2021). Zooming their way through university: Which Big 5 traits facilitated students’ adjustment to online courses during the COVID-19 pandemic. Personality and Individual Differences, 180, 3–4. https://doi.org/10.1016/j.paid.2021.110969.
- Bailis, D. S., Brais, N. J., Single, A. N., & Schellenberg, B. J. (2021). Self-compassion buffers impaired decision-making by potential problem gamblers in a casino setting. Journal of Gambling Studies, 37, 269–282. https://doi.org/10.1007/s10899-020-09993-8
- Berhie, A. Y., Tezera, Z. B., & Azagew, A. W. (2020). Moral distress and its associated factors among nurses in northwest Amhara regional state referral hospitals, Northwest Ethiopia. Psychology Research and Behavior Management, 161–167. https://doi.org/10.2147/PRBM.S234446
- Booth, R. (2022, Dec 15). Striking nurses need the public behind them to keep pressure on ministers. The Guardian. https://www.theguardian.com/society/2022/dec/15/striking-nurses-need-the-public-behind-them-to-keep-pressure-on-ministers.
- British Medical Association. (2021). Moral distress and moral injury, recognising and tackling it for UK doctors. https://www.bma.org.uk/media/4209/bma-moral-distress-injury-survey-report-june-2021.pdf.
- Chen, H., Pang, L., Liu, F., Fang, T., & Wen, Y. (2022). Be perfect in every respect: the mediating role of career adaptability in the relationship between perfectionism and career decision-making difficulties of college students. BMC Psychology, 10(1), 1–12. https://doi.org/10.1186/s40359-021-00711-6
- Cohen, J. (1992). A power primer: Quantitative methods in psychology. Psychological Bulletin, 112(1), 155–158. https://doi.org/10.1037/0033-2909.112.1.155.
- Cowin, L. S., & Hengstberger-Sims, C. (2006). New graduate nurse self-concept and retention: A longitudinal survey. International Journal of Nursing Studies, 43(1), 59–70. https://doi.org/10.1016/j.ijnurstu.2005.03.004
- Crane, M. F., Phillips, J. K., & Karin, E. (2015). Trait perfectionism strengthens the negative effects of moral stressors occurring in veterinary practice. Australian Veterinary Journal, 93(10), 354–360. https://doi.org/10.1111/avj.12366
- Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020). Burnout in nursing: A theoretical review. Human Resources for Health, 18, 1–17. https://doi.org/10.1186/s12960-019-0441-x
- Ey, S., Henning, K. R., & Shaw, D. L. (2000). Attitudes and factors related to seeking mental health treatment among medical and dental students. Journal of College Student Psychotherapy, 14(3), 23–39. https://doi.org/10.1300/J035v14n03_05
- Feher, A., Plouffe, R. A., Saklofske, D. H., Sherry, S. B., Smith, M. M., & Wilson, C. A. (2019). The Big three perfectionism scale-short form (BTPS-SF): development of a brief self-report measure of multidimensional perfectionism. Journal of Psychoeducational Assessment, 38(1), 37–52. https://doi.org/10.1177/0734282919878553
- Flett, G. L., Nepon, T., Hewitt, P. L., & Fitzgerald, K. (2016). Perfectionism, components of stress reactivity, and depressive symptoms. Journal of Psychopathology and Behavioral Assessment, 38(4), 645–654. https://doi.org/10.1007/s10862-016-9554-x
- Flett, G. L., Sherry, S. B., Hewitt, P. L., & Nepon, T. (2014). Understanding the narcissistic perfectionists among us: Grandiosity, vulnerability, and the quest for the perfect self. In Avi Besser (Ed.), Handbook of psychology of narcissism: Diverse perspectives (pp. 43–66). Nova Science Publishers.
- Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18(3), 233–239. https://doi.org/10.1111/j.1467-9280.2007.01882.x
- Frost, R. O., Marten, P., Lahart, C., & Rosenblate, R. (1990). The dimensions of perfectionism. Cognitive Therapy and Research, 14, 449–468. https://doi.org/10.1007/BF01172967
- Grönlund, C. E. F., Söderberg, A. I., Zingmark, K. M., Sandlund, S. M., & Dahlqvist, V. (2015). Ethically difficult situations in hemodialysis care–nurses’ narratives. Nursing Ethics, 22(6), 711–722. https://doi.org/10.1177/0969733014542677
- Gu, J., Baer, R., Cavanagh, K., Kuyken, W., & Strauss, C. (2020). Development and psychometric properties of the Sussex-Oxford compassion scales (SOCS). Assessment, 27(1), 3–20. https://doi.org/10.1177/1073191119860911
- Haahr, A., Norlyk, A., Martinsen, B., & Dreyer, P. (2020). Nurses’ experiences of ethical dilemmas: A review. Nursing Ethics, 27(1), 258–272. https://doi.org/10.1177/0969733019832941
- Hamric, A. B., Borchers, C. T., & Epstein, E. G. (2012). Development and testing of an instrument to measure moral distress in healthcare professions. AJOB Primary Research, 3(2), 1–9. https://doi.org/10.1080/21507716.2011.652337
- Hatzimalonas, M. R. (2018). Philotimo: Vices and virtues of a moral archetype. In N. Brown (Ed.), The Routledge international handbook of critical positive psychology (pp. 474–487). Routledge. https://doi.org/10.4324/9781315659794-35.
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis (second). Guilford Publications.
- Hewitt, P. L., & Flett, G. L. (1991). Perfectionism in the self and social contexts: Conceptualization, assessment, and association with psychopathology. Journal of Personality and Social Psychology, 60, 456–470. https://doi.org/10.1037/0022-3514.60.3.456
- Homan, K. J. (2016). Self-compassion and psychological well-being in older adults. Journal of Adult Development, 23, 111–119. https://doi.org/10.1007/s10804-016-9227-8
- Játiva, R., & Cerezo, M. A. (2014). The mediating role of self-compassion in the relationship between victimization and psychological maladjustment in a sample of adolescents. Child Abuse & Neglect, 38(7), 1180–1190. https://doi.org/10.1016/j.chiabu.2014.04.005
- Jenkins, H. M. (1985). A research tool for measuring perceptions of clinical decision making. Journal of Professional Nursing, 1(4), 221–229. https://doi.org/10.1016/S8755-7223(85)80159-9
- Johansen, M. L., & O'Brien, J. L. (2016). Decision making in nursing practice: A concept analysis. Nursing Forum, 51(1), 40–48. https://doi.org/10.1111/nuf.12119
- Joy, G. V., Alomari, A. M. A., Singh, K., Hassan, N., Mannethodi, K., Kunjavara, J., & Al Lenjawi, B. (2023). Nurses’ self-esteem, self-compassion and psychological resilience during COVID-19 pandemic. Nursing Open, 4406–4410. https://doi.org/10.1002/nop2.1682.
- Kim, Y., & Cohen, T. R. (2015). Moral character and workplace deviance: Recent research and current trends. Current Opinion in Psychology, 6, 134–138. https://doi.org/10.1016/j.copsyc.2015.08.002
- Kovanci, M. S., & Akyar, I. (2022). Culturally-sensitive moral distress experiences of intensive care nurses: A scoping review. Nursing Ethics, 29(6), 1476–1490. https://doi.org/10.1177/09697330221105638
- Manetti, W. (2018). Sound clinical judgment in nursing: A concept analysis. Nursing Forum, 55(1), 102–110. https://doi.org/10.1111/nuf.12303
- Mantzios, M. (2021). Pre-Socratic understandings of moral identity: The theoretical infrastructure, development, reliability and validity of the Philotimo Scale. Imagination, Cognition and Personality, 41(2), 187–206. https://doi.org/10.1177/02762366211013503
- Martela, F., & Ryan, R. M. (2016). The benefits of benevolence: Basic psychological needs, beneficence, and the enhancement of well-being. Journal of Personality, 84(6), 750–764. https://doi.org/10.1111/jopy.12215
- Martincin, K. M., & Stead, G. B. (2015). Five-factor model and difficulties in career decision making: A meta-analysis. Journal of Career Assessment, 23(1), 3–19. https://doi.org/10.1177/1069072714523081
- McKay, T., & Walker, B. R. (2021). Mindfulness, self-compassion and wellbeing. Personality and Individual Differences, 168, 1–2. https://doi.org/10.1016/j.paid.2020.110412.
- Međedović, J., & Petrović, B. (2016). Can there be an immoral morality? Dark personality traits as predictors of moral foundations. Psihologija, 49(2), 185–197. https://doi.org/10.2298/PSI1602185M
- Mehlis, K., Bierwirth, E., Laryionava, K., Mumm, F. H., Hiddemann, W., Heußner, P., & Winkler, E. C. (2018). High prevalence of moral distress reported by oncologists and oncology nurses in end-of-life decision making. Psycho-Oncology, 27(12), 2733–2739. https://doi.org/10.1002/pon.4868
- Miley, M., Connabeer, K., Wallis, D., Egan, H., & Mantzios, M. (2023). Development and Revision of the Clinical Decision-making in Nursing Scale: A Methodological Study. SSRN. https://doi.org/10.2139/ssrn.4621063
- Montoya, A. I. A., Hazel, S., Matthew, S. M., & McArthur, M. L. (2019). Moral distress in veterinarians. Veterinary Record, 185(20), 631–631. https://doi.org/10.1136/vr.105289
- Nursing and Midwifery Council. (2022). Openness and honesty when things go wrong: the professional duty of candour. https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/openness-and-honesty-professional-duty-of-candour.pdf.
- Nursing & Midwifery Council. (2015). The Code. https://www.nmc.org.uk/standards/code/
- Petrișor, C., Breazu, C., Doroftei, M., Mărieș, I., & Popescu, C. (2021). Association of moral distress with anxiety, depression, and an intention to leave among nurses working in intensive care units during the COVID-19 pandemic. Healthcare, 9(10), 5–12. https://doi.org/10.3390/healthcare9101377.
- Rainer, J., Schneider, J. K., & Lorenz, R. A. (2018). Ethical dilemmas in nursing: An integrative review. Journal of Clinical Nursing, 27(19-20), 3446–3461. https://doi.org/10.1111/jocn.14542
- Rathert, C., May, D. R., & Chung, H. S. (2016). Nurse moral distress: A survey identifying predictors and potential interventions. International Journal of Nursing Studies, 53, 39–49. https://doi.org/10.1016/j.ijnurstu.2015.10.007
- Ścigała, K. A., Schild, C., & Zettler, I. (2020). Doing justice to creative justifications: Creativity, honesty-humility, and (un) ethical justifications. Journal of Research in Personality, 89, 9–13. https://doi.org/10.1016/j.jrp.2020.104033.
- Smallwood, N., Pascoe, A., Karimi, L., & Willis, K. (2021). Moral distress and perceived community views are associated with mental health symptoms in frontline health workers during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(16), 4–12. https://doi.org/10.3390/ijerph18168723.
- Smith, M., Higgs, J., & Ellis, E. (2008). Factors influencing clinical decision making. Clinical Reasoning in the Health Professions, 3, 94–100.
- Smith, M. M., Sherry, S. B., Chen, S., Saklofske, D. H., Mushquash, C., Flett, G. L., & Hewitt, P. L. (2017). The perniciousness of perfectionism: A meta-analytic review of the perfectionism suicide relationship. Journal of Personality, 86, 522–542. https://doi.org/10.1111/jopy.12333
- Smith, M. M., Vidovic, V., Sherry, S. B., Stewart, S. H., & Saklofske, D. H. (2018). Perfectionistic concerns confer risk for anxiety symptoms: A meta-analysis of 11 longitudinal studies. Anxiety, Stress & Coping, 31, 4–20. https://doi.org/10.1080/10615806.2017.1384466
- Stoeber, J., Lalova, A. V., & Lumley, E. J. (2020). Perfectionism, (self-) compassion, and subjective well-being: A mediation model. Personality and Individual Differences, 154, 2–4. https://doi.org/10.1016/j.paid.2019.109708.
- Tavsancil, E. (2006). Measuring attitudes and data analysis with SPSS. Nobel Publishing and Distribution.
- Thompson, C., Cullum, N., McCaughan, D., Sheldon, T., & Raynor, P. (2004). Nurses, information use, and clinical decision making—the real world potential for evidence-based decisions in nursing. Evidence-based Nursing, 7(3), 68–72. https://doi.org/10.1136/ebn.7.3.68
- Wang, D., Hou, Z. J., Ni, J., Tian, L., Zhang, X., Chi, H. Y., & Zhao, A. (2020). The effect of perfectionism on career adaptability and career decision-making difficulties. Journal of Career Development, 47(4), 469–483. https://doi.org/10.1177/0894845318803192
- Warbah, L., Sathiyaseelan, M., Vijayakumar, C., Vasantharaj, B., Russell, S., & Jacob, K. S. (2007). Psychological distress, personality, and adjustment among nursing students. Nurse Education Today, 27(6), 597–601. https://doi.org/10.1016/j.nedt.2006.09.002
- Webster, R. J., Morrone, N., Motyl, M., & Iyer, R. (2021). Using trait and moral theories to understand belief in pure evil and belief in pure good. Personality and Individual Differences, 173, 6–10. https://doi.org/10.1016/j.paid.2020.110584.
- Weziak-Bialowolska, D., Bialowolski, P., & Niemiec, R. M. (2021). Being good, doing good: The role of honesty and integrity for health. Social Science & Medicine, 291, 4–7. https://doi.org/10.1016/j.socscimed.2021.114494.
