ABSTRACT
Individuals with lower limb amputation have a high incidence of falls. Above-the-knee amputation and diabetes/vascular disease are both risk factors for falls. Microprocessor knee (MPK) technology may reduce falls in this population. The objective was to determine the association between MPKs and reduced injurious falls. A retrospective analysis of injurious falls within a large, national outcomes database was conducted. Inclusion was limited to adult K3 ambulators with unilateral, transfemoral, or knee disarticulation amputation due to diabetes/vascular disease. There were 744 out of 881 individuals that did not receive an MPK. Results showed that 16.3% of non-MPK users experienced an injurious fall compared to 7.3% of MPK users (p = .007). Not having an MPK resulted in significantly increased odds (unadjusted: OR: 2.47, 95% CI: 1.26–4.83, p = .009; adjusted for confounders: OR: 2.52, 95% CI: 1.28–4.94, p = .007) of incurring an injurious fall over a 6-month period. In conclusion, the current study found use of an MPK strongly associated with reduced injurious falls in a population of patients with amputation due to diabetes/vascular disease. The findings strongly support the use of MPK technology to mitigate fall risk, and in particular injurious falls requiring medical intervention.
Introduction
The consequences of a fall can be detrimental to a person’s health. In terms of immediate physical health, 1 out of 5 falls results in serious injury such as broken bones or head injury (Alexander et al., Citation1992; Centers for Disease Control and Prevention [CDC], Citation2020; Sterling et al., Citation2001). Falls are also the most common cause of traumatic brain injury (CDC, Citation2020; Jager et al., Citation2000), as well as the leading cause of death for Americans aged 65 and older (Burns & Kakara, Citation2018; Roubik et al., Citation2017). Additionally, fall sequelae are not limited to immediate injury. For example, only 25% of elderly individuals report a return to prior levels of independence after a fall (Ayoung-Chee et al., Citation2014; Roubik et al., Citation2017). In 2015, the total healthcare cost burden in the United States for falls was approximately $50 billion, with Medicare and Medicaid covering about 70% of the costs (Florence et al., Citation2018).
Individuals with a lower limb amputation are known to have increased risk and incidence of falling compared to the general population, with 50% incurring a fall each calendar year (Hafner & Smith, Citation2009; Miller et al., Citation2001). This is in contrast to about 30% of individuals over age 65 in the general population (Stalenhoef et al., Citation2002; Tinetti et al., Citation1988). An above-the-knee amputation (AKA), which includes amputation at the transfemoral or knee disarticulation level, is among the noted risk factors for falling among individuals with lower limb amputation (Miller et al., Citation2001). Amputation etiology and comorbid vascular health may also impact the relative risk of falls. Vascular disease results in a 73% increase in falls for elderly adults compared to their healthy counterparts (Gardner & Montgomery, Citation2001; Rand et al., Citation2015) and is the most common cause of amputation in the United States (Hunter et al., Citation2017). Unsurprisingly, a recent systematic review identified diabetes/vascular disease as a fall risk factor for individuals with lower limb amputation (Hunter et al., Citation2017).
Prostheses for individuals with AKA may include microprocessor knee (MPK) technology that is purported to provide multiple benefits to patients (Hafner & Smith, Citation2009; Hafner et al., Citation2007; Kahle et al., Citation2008; Kannenberg et al., Citation2014; Stevens & Wurdeman, Citation2019; Wong et al., Citation2015). Briefly, MPKs utilize multiple strain gauges, accelerometers, and gyroscopes to measure a person’s gait in real-time. A microprocessor embedded within the knee unit processes the signals to then regulate the resistance to flexion and extension of the knee joint. The most common methods open and close an iris for restricting hydraulic fluid or changing current to modulate viscosity of a magnetorheological fluid. As a result, the knee is a dynamic and reactive device rather than a static device relying on fluid dynamics and thus afford multiple benefits to patients (Stevens & Wurdeman, Citation2019). These benefits include reduction in number of falls, decreased frustrations, reduced perceived cognitive burden with ambulation, increased mobility, greater satisfaction, and quality of life, increased self-selected walking speed and greater metabolic efficiency (Hafner & Smith, Citation2009; Hafner et al., Citation2007; Kahle et al., Citation2008; Kannenberg et al., Citation2014; Stevens & Wurdeman, Citation2019; Wong et al., Citation2015). However, the majority of studies has tended to focus on younger, healthier individuals. In a review, Theeven et al. (Citation2013) noted only 13% of the studies had focused on patients with vascular amputation etiology.
A recent study focused on individuals with amputation due to vascular disease (Wong et al., Citation2015). The prospective study assessed functional outcomes for patients (n = 8) using their non-MPK, then provided the patient with an MPK with repeated assessments. After the use of MPK, patients showed improvements in fear of falling, balance, timed-up-and-go score, and number of falls (Wong et al., Citation2015). The reduction in falls is consistent with other studies not focused on individuals with AKA due to diabetes/vascular disease (Burnfield et al., Citation2012; Hafner & Smith, Citation2009; Kahle et al., Citation2008; Kannenberg et al., Citation2014; Kaufman et al., Citation2018; Stevens & Wurdeman, Citation2019).
Thus, further work is warranted to better understand the ability for MPK technology to reduce falls among individuals with AKA due to diabetes/vascular disease. Therefore, the purpose of this study was to determine the influence MPK technology can have on mitigating falls for individuals with AKA due to diabetes/vascular disease. Based on previous work (Wong et al., Citation2015), it was hypothesized that those individuals that were not provided with an MPK have higher odds of incurring an injurious fall.
Methods
Study design
A retrospective cohort review of a multi-center outcomes database was performed. Outcomes are being collected as part of standard of care at clinics across the United States. The database includes multiple-assessment points, such as history of falls, mobility, satisfaction, and quality of life. For the current analysis, specifically, the unilateral AKA due to diabetes/vascular disease outcomes database was utilized with data collected through the period of April 2016 through May 2019, with focus specific to the hypothesis on the history of falls. Data is captured directly from the patient through a digital entry platform. Outcomes are captured at baseline for a new device and at various follow-up time points to track patient status. At the time of the analysis, the database included 1,857 patients. The current database review was approved and deemed exempt from patient consent by the Western Investigational Review Board (Protocol #20170059). This study conforms to all STROBE guidelines.
Included persons
Inclusion in the database is limited to adults age 18 and older, thereby restricting the current analysis to age ≥ 18 years. The database includes gender, age, and years since amputation, height, and mass. Additionally, the database is limited to AKA inclusive of transfemoral and knee disarticulation amputation levels. Inclusion is limited to English and Spanish speaking only. Inclusion was limited to K3 ambulators with comorbidities verified on file to ensure similar functional potential, health status, and eligibility for MPK (”LCD: Lower limb prostheses,” Citation2019). The K3 classification, while adopted as guidance in multiple countries, is specific to the United States healthcare system, driven by the Centers for Medicare and Medicaid Services coverage determination policies and guiding prescription and access (”LCD: Lower limb prostheses,” Citation2019). Comorbidities were used to calculate individual functional comorbidity indices (FCI) (Groll et al., Citation2005). Body mass index (BMI) was adjusted for limb loss (Tzamaloukas et al., Citation1994, Citation2000). As the nature of the study is observational, individuals must be presented to their prosthetics provider to have outcomes assessment recorded.
Assessment
As part of the routine standard of care, patients with lower limb amputation are presented with a single question with a binary response permitted, “Have you had a fall in the previous 6 months that resulted in a hospital or physician visit?” The question is not limited to when the patient is wearing the prosthesis. The decision was made to ask about injurious falls as opposed to general falls to reduce bias. In particular, this allowed anchoring the fall to a traumatic episode to enhance patient recall (Strange & Takarangi, Citation2015). In this manner, recall bias and the subsequent associated error can be minimized. Injurious falls were also of greater concern due to care and cost burden.
Analysis
Summary and descriptive statistics were calculated among the sample population. Any missing explanatory or response variables were replaced using expectation-maximization algorithms. Little’s Missing Completely at Random test was confirmed as non-significant. Differences in demographics data between MPK and non-MPK users were compared through Mann Whitney U and Pearson’s Chisquare test for continuous and categorical data, respectively. Next, unadjusted odds ratios (OR) and 95% confidence intervals (CI) were obtained using logistic regression to provide a crude association for each potential confounding variable with reported falls. Multivariate logistic regression was used to assess the MPK association with falls while adjusting for covariates. To assess confounding, each potential confounder was entered into a univariate model separately. If the variable changed the magnitude of the OR compared to the crude OR by at least 10% it would be considered a confounder and a separate model would be run retaining only those variables. A final model was also run whereby all potential confounding variables were retained and controlled as these variables have been previously mentioned as potential risk factors associated with falls (Miller et al., Citation2001). All data analyses were performed using SPSS v20.0 (Armonk, NY).
Results
After applying inclusion/exclusion criteria, 12.7% of our initial population were excluded for incomplete documentation of comorbid health conditions. This resulted in a total of 881 total patients included for analysis ( and ). Within the population of non-MPK users, a little over 16% of the sample experienced an injurious fall. This was more than double the number within the MPK users at 7%. The median age of individuals with non-MPK and those with MPK were similar (62.4 years compared to 61.9 years, respectively), as well as the percentage of individuals aged 65 years and older. There were no significant group differences in terms of demographics.
Figure 1. Individuals were extracted from the adults with unilateral above-the-knee amputation due to diabetes/vascular disease outcomes database based in the United States. For inclusion to the current analysis, individuals were restricted to the United States medicare functional classification level K3. Individuals were excluded if they did not have comorbidities verified. This resulted in exclusion of 12.7% of individuals to yield a total of 881 individuals available for analysis.
Table 1. Sample demographics. Values presented as median (interquartile range) except where percentage is noted for counts. MPK: microprocessor knee; BMI: adjusted body mass index; FCI: functional comorbidity index.
The unadjusted logit regression model was first run. Results showed individuals with an AKA that were not provided with an MPK as part of their lower limb prosthetic rehabilitation had a 2.47 times increased odds of incurring an injurious fall over a 6-month period ().
Table 2. Influence of microprocessor knees on injurious falls for individuals with diabetic/vascular amputation. MPK: microprocessor knee.
When running separate models for potential confounders, minimal change occurred to the crude OR for non-MPK versus MPK in models separately assessing age (OR: 2.49, CI: 1.27–4.90), sex (OR: 2.48, CI: 1.26–4.85), adjusted BMI (OR: 2.44, CI: 1.25–4.79), or time since amputation (OR: 2.48, CI: 1.27–4.86). Individual potential confounding variables did not affect the crude OR by more than the traditional 10% threshold.
Finally, the multivariate model was run with all potential confounding variables retained. Results from this analysis were consistent with results from individual models. In particular while accounting for age, sex, time since amputation, and adjusted BMI, it was noted that individuals that are not provided with an MPK have a 2.52 times increased odds of sustaining an injurious fall over a 6-month period compared to their counterparts that receive an MPK ( and ). In the multivariate model, age ended up being significant, with OR slightly greater than 1 at 1.02.
Figure 2. From the multivariate logistic regression model, it is possible to see the increased odds of falling for the individual with amputation due to diabetes/vascular disease when not provided an MPK regardless of factors such as age, gender, time since amputation, and BMI. MPK: microprocessor knee; BMI: adjusted body mass index.
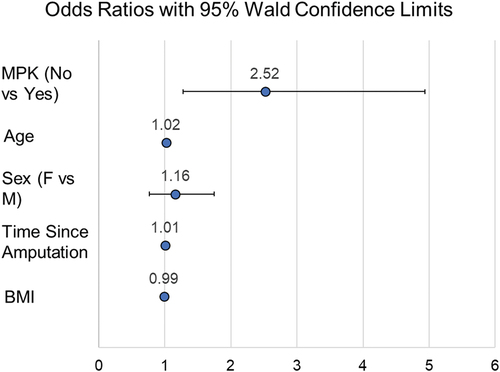
Table 3. Multivariate regression model to assess influence of microprocessor knees while accounting for age, sex, time since amputation, and adjusted body mass index. MPK: microprocessor knee; BMI: adjusted body mass index.
Discussion
While there is high awareness of the problem of falls in the elderly, less attention is given to the incidence of falling among individuals with lower limb amputation despite a nearly double incidence rate (Miller et al., Citation2001). Fortunately, the evolution of technology may bring hope for mitigating falls among lower limb prosthesis users. MPKs have in particular been noted to reduce falls among individuals with an AKA (Stevens & Wurdeman, Citation2019). However, there continues to be limited utilization among those with amputation due to diabetes/vascular disease, necessitating further evidence. These individuals are at greater risk for falls given the underlying diabetes/vascular disease (Yang et al., Citation2016). For this reason, the current study is set to determine the influence of MPK technology on reducing falls among individuals with lower limb amputation due to diabetes/vascular disease. The focus was limited to injurious falls due to the associated increased clinical and fiscal impact. Our results show that if an individual with amputation due to diabetes/vascular disease is not provided with an MPK, they are placed at 2.5 times increased odds of sustaining an injurious fall. The current study’s findings add to the existing body of the literature surrounding benefits of MPK use (Chen et al., Citation2018; Hafner et al., Citation2007; Kahle et al., Citation2008; Kannenberg et al., Citation2014; Kaufman et al., Citation2007, Citation2008, Citation2012, Citation2018; Liu et al., Citation2017; Stevens & Wurdeman, Citation2019; Wong et al., Citation2015; Wurdeman et al., Citation2018b), but extends to note specific benefits to patients with amputation due to diabetes/vascular disease.
The increased odds of an injurious fall for the non-MPK user was noted while accounting for several potential confounding variables. Age commonly reported as a fall risk factor, was significant. However, with an odds ratio of 1.02, it is questionable to state this as clinically significant versus a statistical result. Any potential effect of age, a well-cited risk factor for falls, was overshadowed by whether the individual’s prosthesis incorporated an MPK. Current results would indicate an increased risk of injurious falls is present regardless of age. Thus, the current results show the benefits of MPK technology for fall reduction for the younger population of individuals with amputation (i.e. age < 65, represented by 542 out of 881 individuals in the study, ) as well as for the older population of individuals with amputation (i.e. age ≥ 65, represented by 339 out of 881 individuals, ).
There are obvious healthcare costs associated with an injurious fall as the individual seeks medical attention (Chen et al., Citation2018; Liu et al., Citation2017). However, this should not overshadow the additional impacts of injurious falls on mortality and morbidity (Tinetti & Kumar, Citation2010; Tinetti & Williams, Citation1998). The US Centers for Disease Control reported that fall-related deaths rose ~31% from 2007 to 2016 for individuals over age 65 in the general public (Burns & Kakara, Citation2018). The number of non-fatal fall-related injuries was recently published to be about 1% of Americans over a 3 month period (Verma et al., Citation2016). This is a considerable difference compared to the ~15% of individuals within the current study that reported an injurious fall over a 6 month period. Thus, the current study would indicate the problem of falls among lower limb prosthesis users extends beyond just minor inconveniences as individuals are incurring a high rate of injuries.
One concerning observation from the current analysis is the potential prescription bias based upon etiology. Within the US, the qualification for an MPK is that an individual must be at a K3 ambulator level, notwithstanding a few third-party payer exceptions (”LCD: Lower limb prostheses,” Citation2019). There are no limitations with regard to age or comorbidities. This does not mean that age or comorbidity status may not influence K-level assignment by the rehabilitation physician and team, but within the US only the K-level status subsequently qualifies a patient for an MPK. In the current study based out of the US, we limited inclusion to 881 individuals with AKA that were designated as K3 ambulators. Importantly, AKA included both transfemoral and knee disarticulation. These surgical-level differences have not been differentiated in terms of the primary endpoint of fall risk (Miller et al., Citation2001). Furthermore, recent work comparing functional outcomes between these two surgical-level differences failed to show functional differences (Polfer et al., Citation2019). Additionally, there is no differentiation in terms of qualification for these two surgical levels. Thus, all individuals qualified for an MPK, yet only 137 individuals were provided an MPK. In the worst case, one might suggest that anyone not eligible for Medicare (i.e. age 65 and older) happens to fall into a limited percentage of private plans that have exemptions for MPK. This however, still means that there were 286 Medicare eligible patients who did not receive an MPK. Future work will need to tie in other populations to understand potential biases based on etiology. If such biases do exist, then hopefully studies such as the current one can help individuals understand the benefits of MPK technology specifically for individuals with AKA due to diabetes/vascular disease.
The current analysis is limited in its ability to quantify the types of injuries that individuals incurred. However, data from the 2008 National Health Interview Survey showed the most common non-fatal fall-related injuries were sprains and strains of joints, followed by fractures, contusions, and lacerations (Verma et al., Citation2016). This is concerning given that downtime for recovery can reduce mobility (e.g., a fracture even of the wrist can prevent the ability to don a lower limb prosthesis for 8 weeks or more). A reduction in mobility would likely further reduce quality of life beyond the immediate impact of injury (Wurdeman et al., Citation2018a). Further work is needed to determine if injurious falls among lower limb prosthesis users have similar long-term effects as in the general population, such as increased mortality and poorer quality of life (Ayoung-Chee et al., Citation2014; Hartholt et al., Citation2011).
The current study findings should be viewed in light of certain limitations. First, in addition to not tracking the type of injury associated with the individuals’ falls, there was no mechanism to track cost to allow analysis of costs incurred as a result of the fall. Second, the falls question does not differentiate between falls occurring, while the patient is wearing their prosthesis or not. This would allow more insight into the ability of the MPK to mitigate falls. It is, however, interesting to consider if the injurious falls are occurring without the MPK being worn. The implication of this would be either 1) the injurious fallers are not wearing their device as much which could speak to reduced utility, possibly consequential of a perceived reduced value of non-MPK compared to MPK in this population or 2) individuals prone to injurious falls are not being prescribed MPKs to the same degree as those that are not prone to injurious falls. Further, while the question of a fall was anchored to a traumatic event to strengthen memory recall, there is no guarantee that the trauma of a fall reached the threshold for strengthening memory in all individuals. This method also would not overcome injuries that may have resulted in a traumatic head injury with memory impairment. Thus, the combination of these would seemingly have increased the likelihood of an underestimation of injurious falls in the current sample. However, given similar demographics, there is no reason to believe any bias in such underestimation in one group or the other.
Conclusion
Falls are a major problem for individuals with lower limb amputation. Balance impairments associated with diabetes and peripheral vascular disease place individuals with this underlying amputation etiology at greater risk for falling. Within a population of nearly 900 lower limb prosthesis users with transfemoral amputation or knee disarticulation due to diabetes/vascular disease, 15% incurred an injurious fall over a 6-month period. Fortunately that rate was less than half that amount for those individuals with an MPK in their prosthesis. Ultimately, those individuals with diabetes/vascular etiology not provided an MPK face 2.5-fold increased odds of an injurious fall while accounting for age, sex, time since amputation and BMI adjusted for limb loss.
Abbreviations
AKA: above-the-knee amputation
MPK: microprocessor knee
BMI: body mass index
FCI: functional comorbidity index
OR: odds ratio
CI: confidence interval
Acknowledgments
The authors would like to thank Dwiesha England, MS, and Mandi Laurie, MS, for assistance with data identification and reduction, as well as all the clinicians that have embraced a cultural shift in the practice of orthotics and prosthetics to include the routine collection of outcome measures providing the ability to do these large aggregate analyses.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Alexander, B. H., Rivara, F. P., & Wolf, M. E. (1992). The cost and frequency of hospitalization for fall-related injuries in older adults. American Journal of Public Health, 82(7), 1020–1023. https://doi.org/10.2105/ajph.82.7.1020
- Ayoung-Chee, P., McIntyre, L., Ebel, B. E., Mack, C. D., McCormick, W., & Maier, R. V. (2014). Long-term outcomes of ground-level falls in the elderly. The Journal of Trauma and Acute Care Surgery, 76(2), 498–503; discussion 503. https://doi.org/10.1097/TA.0000000000000102
- Burnfield, J. M., Eberly, V. J., Gronely, J. K., Perry, J., Yule, W. J., & Mulroy, S. J. (2012). Impact of stance phase microprocessor-controlled knee prosthesis on ramp negotiation and community walking function in K2 level transfemoral amputees. Prosthetics and Orthotics International, 36(1), 95–104. https://doi.org/10.1177/0309364611431611
- Burns, E., & Kakara, R. (2018). Deaths from falls among persons aged >65 years - United States, 2007–2016. MMWR Morb Mortal Wkly Rep 67, 509–514. doi:10.15585/mmwr.mm6718a1
- Centers for Disease Control and Prevention. Falls among older adults: An overview. Retrieved September 21, 2020, from http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html
- Chen, C., Hanson, M., Chaturvedi, R., Mattke, S., Hillestad, R., & Liu, H. (2018). Economic benefits of microprocessor controlled prosthetic knees: A modeling study. Journal of Neuroengineering and Rehabilitation, 15(1), 62. https://doi.org/10.1186/s12984-018-0405-8
- Florence, C. S., Bergen, G., Atherly, A., Burns, E., Stevens, J., & Drake, C. (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66(4), 693–698. https://doi.org/10.1111/jgs.15304
- Gardner, A. W., & Montgomery, P. S. (2001). Impaired balance and higher prevalence of falls in subjects with intermittent claudication. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56(7), M454–8. https://doi.org/10.1093/gerona/56.7.m454
- Groll, D., To, T., Bombardier, C., & Wright, J. (2005). The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology, 58(6), 595–602. https://doi.org/10.1016/j.jclinepi.2004.10.018
- Hafner, B. J., & Smith, D. G. (2009). Differences in function and safety between medicare functional classification level-2 and -3 transfemoral amputees and influence of prosthetic knee joint control. Journal of Rehabilitation Research and Development, 46(3), 417–433. https://doi.org/10.1682/JRRD.2008.01.0007
- Hafner, B. J., Willingham, L. L., Buell, N. C., Allyn, K. J., & Smith, D. G. (2007). Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Archives of Physical Medicine and Rehabilitation, 88(2), 207–217. https://doi.org/10.1016/j.apmr.2006.10.030
- Hartholt, K. A., Van Beeck, E. F., Polinder, S., Van der Velde, N., Van Lieshout, E. M., Panneman, M. J., Van der Cammen, T. J., & Patka, P. (2011). Societal consequences of falls in the older population: Injuries, healthcare costs, and long-term reduced quality of life. Journal of Trauma, 71(3), 748–753 doi:10.1097/TA.0b013e3181f6f5e5.
- Hunter, S. W., Batchelor, F., Hill, K. D., Hill, A. M., Mackintosh, S., & Payne, M. (2017). Risk factors for falls in people with a lower limb amputation: A systematic review. PM & R: The Journal of Injury, Function, and Rehabilitation, 9(2), 170–180.e1. https://doi.org/10.1016/j.pmrj.2016.07.531
- Jager, T. E., Weiss, H. B., Coben, J. H., & Pepe, P. E. (2000). Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 7(2), 134–140. https://doi.org/10.1111/j.1553-2712.2000.tb00515.x
- Kahle, J. T., Highsmith, M. J., & Hubbard, S. L. (2008). Comparison of nonmicroprocessor knee mechanism versus C-leg on prosthesis evaluation questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. Journal of Rehabilitation Research and Development, 45(1), 1–14. https://doi.org/10.1682/JRRD.2007.04.0054
- Kannenberg, A., Zacharias, B., & Probsting, E. (2014). Benefits of microprocessor-controlled prosthetic knees to limited community ambulators: Systematic review. Journal of Rehabilitation Research and Development, 51(10), 1469–1496. https://doi.org/10.1682/JRRD.2014.05.0118
- Kaufman, K. R., Bernhardt, K. A., & Symms, K. (2018). Functional assessment and satisfaction of transfemoral amputees with low mobility (FASTK2): A clinical trial of microprocessor-controlled vs. non-microprocessor-controlled knees. Clinical Biomechanics (Bristol, Avon), 58, 116–122. https://doi.org/10.1016/j.clinbiomech.2018.07.012
- Kaufman, K. R., Frittoli, S., & Frigo, C. A. (2012). Gait asymmetry of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Clinical Biomechanics (Bristol, Avon), 27(5), 460–465. https://doi.org/10.1016/j.clinbiomech.2011.11.011
- Kaufman, K. R., Levine, J. A., Brey, R. H., Iverson, B. K., McCrady, S. K., Padgett, D. J., & Joyner, M. J. (2007). Gait and balance of transfemoral amputees using passive mechanical and microprocessor-controlled prosthetic knees. Gait & Posture, 26(4), 489–493. https://doi.org/10.1016/j.gaitpost.2007.07.011
- Kaufman, K. R., Levine, J. A., Brey, R. H., McCrady, S. K., Padgett, D. J., & Joyner, M. J. (2008). Energy expenditure and activity of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Archives of Physical Medicine and Rehabilitation, 89(7), 1380–1385. https://doi.org/10.1016/j.apmr.2007.11.053
- LCD: Lower limb prostheses. (2019). Centers for Medicare & Medicaid Serviceshttps://med.noridianmedicare.com/documents/2230703/7218263/Lower+Limb+Prostheses+LCD+and+PA/d3244c51-74d3-4214-a789-7481bc2e03d5
- Liu, H., Chen, C., Hanson, M., Chaturvedi, R., Mattke, S., & Hillestad, R. (2017). Economic value of advanced transfemoral prosthetics. Rand Corporation.
- Miller, W. C., Speechley, M., & Deathe, B. (2001). The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Archives of Physical Medicine and Rehabilitation, 82(8), 1031–1037. https://doi.org/10.1053/apmr.2001.24295
- Polfer, E. M., Hoyt, B. W., Bevevino, A. J., Forsberg, J. A., & Potter, B. K. (2019). Knee disarticulations versus transfemoral amputations: Functional outcomes. Journal of Orthopaedic Trauma, 33(6), 308–311. https://doi.org/10.1097/BOT.0000000000001440
- Rand, T. J., Wurdeman, S. R., Johanning, J. M., Pipinos, I. I., & Myers, S. A. (2015). Increased minimum toe clearance variability in patients with peripheral arterial disease. Medical Engineering & Physics, 37(12), 1141–1145. https://doi.org/10.1016/j.medengphy.2015.09.009
- Roubik, D., Cook, A. D., Ward, J. G., Chapple, K. M., Teperman, S., Stone, M. E., Jr, Gross, B., & Moore, F. O., 3rd. (2017). Then we all fall down: Fall mortality by trauma center level. The Journal of Surgical Research, 217, 36–44.e2. https://doi.org/10.1016/j.jss.2016.12.039
- Stalenhoef, P. A., Diederiks, J. P., Knottnerus, J. A., Kester, A. D., & Crebolder, H. F. (2002). A risk model for the prediction of recurrent falls in community-dwelling elderly: A prospective cohort study. Journal of Clinical Epidemiology, 55(11), 1088–1094. https://doi.org/10.1016/S0895-4356(02)00502-4
- Sterling, D. A., O’Connor, J. A., & Bonadies, J. (2001). Geriatric falls: Injury severity is high and disproportionate to mechanism. The Journal of Trauma, 50(1), 116–119. https://doi.org/10.1097/00005373-200101000-00021
- Stevens, P. M., & Wurdeman, S. R. (2019). Prosthetic knee selection for individuals with unilateral transfemoral amputation: A clinical practice guideline. Journal of Prosthetics and Orthotics, 31(1), 2–8. https://doi.org/10.1097/JPO.0000000000000214
- Strange, D., & Takarangi, M. K. (2015). Memory distortion for traumatic events: The role of mental imagery. Frontiers in Psychiatry, 6(27)., . https://doi.org/10.3389/fpsyt.2015.00027
- Theeven, P. J., Hemmen, B., Brink, P. R., Smeets, R. J., & Seelen, H. A. (2013). Measures and procedures utilized to determine the added value of microprocessor-controlled prosthetic knee joints: A systematic review. BMC Musculoskeletal Disorders, 14(1), 333–2474-14-333. https://doi.org/10.1186/1471-2474-14-333
- Tinetti, M. E., & Kumar, C. (2010). The patient who falls: “it’s always a trade-off.” Journal of the American Medical Association, 303(3), 258–266. https://doi.org/10.1001/jama.2009.2024
- Tinetti, M. E., Speechley, M., & Ginter, S. (1988). Risk factors for falls among elderly persons living in the community. New England Journal of Medicine, 319(26), 1701–1707. https://doi.org/10.1056/NEJM198812293192604
- Tinetti, M. E., & Williams, C. S. (1998). The effect of falls and fall injuries on functioning in community-dwelling older persons. Journal of Gerontology: Medical Sciences, 53A(2), M112–M119 doi:10.1093/gerona/53a.2.m112.
- Tzamaloukas, A., Leger, A., Hill, J., & Murata, G. (2000). Body mass index in patients with amputations on peritoneal dialysis: Error of uncorrected estimates and proposed correction. Advances in Peritoneal Dialysis. Conference on Peritoneal Dialysis, 16, 138–142.
- Tzamaloukas, A., Patron, A., & Malhotra, D. (1994). Body mass index in amputees. Journal of Parenteral and Enteral Nutrition, 18(4), 355–358. https://doi.org/10.1177/014860719401800414
- Verma, S. K., Willetts, J. L., Corns, H. L., Marucci-Wellman, H. R., Lombardi, D. A., Courtney, T. K., & Haddad, J. M. (2016). Falls and fall-related injuries among community-dwelling adults in the United States. PLOS One, 11(3), e0150939. https://doi.org/10.1371/journal.pone.0150939
- Wong, C. K., Rheinstein, J., & Stern, M. A. (2015). Benefits for adults with transfemoral amputations and peripheral artery disease using microprocessor compared with nonmicroprocessor prosthetic knees. American Journal of Physical Medicine & Rehabilitation, 94(10), 804–810. https://doi.org/10.1097/PHM.0000000000000265
- Wurdeman, S. R., Stevens, P. M., & Campbell, J. H. (2018a). Mobility analysis of AmpuTees (MAAT 1): Quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthetics and Orthotics International, 42(5), 498–503. https://doi.org/10.1177/0309364617736089
- Wurdeman, S. R., Stevens, P. M., & Campbell, J. H. (2018b). Mobility analysis of amputees (MAAT 3): Matching individuals based on comorbid health reveals improved function for above-knee prosthesis users with microprocessor knee technology. Assistive Technology: The Official Journal of RESNA, 32(5) , 236–242. https://doi.org/10.1080/10400435.2018.1530701
- Yang, Y., Hu, X., Zhang, Q., & Zou, R. (2016). Diabetes mellitus and risk of falls in older adults: A systematic review and meta-analysis. Age and Ageing, 45(6), 761–767. https://doi.org/10.1093/ageing/afw140
