Abstract
As natural teeth are lost, many older adults choose softer foods lacking in essential micronutrients and fiber, yet replacing missing teeth alone does not positively influence diet. Dietary intervention in combination with treatment to replace missing teeth is increasing, though understanding of effective intervention components is limited. This systematic review synthesized literature relating to oral rehabilitation coupled with dietary intervention in adults. The primary outcome was dietary intake; secondary outcomes pertained to oral health and dietary intervention characteristics including: theoretical basis and behavior change techniques (BCTs). MEDLINE, Web of Science, PubMed and CENTRAL were searched. Nine studies were included. Study designs were heterogeneous involving 526 participants. Narrative synthesis identified improvements in at least one aspect of participants’ oral health (i.e. biting/chewing) alongside at least one positive diet/nutrition outcome post-intervention for all studies. F/V results were pooled for three studies using meta-analysis techniques resulting in a standardized mean difference (SMD) of 0.29 [CI −0.54, 1.12], p = 0.49, but with marked heterogeneity (p = 0.0007). Few interventions were theory-based and intervention components were poorly described. Overall, narrative synthesis indicated support for dietary intervention coupled with oral rehabilitation on diet. Meta-analysis was only possible with three studies highlighting limitations. Large-scale, appropriately described trial methodologies are needed.
Trial registry: This review was prospectively registered with PROSPERO on the 11 July 2017 [CRD42017071075].
Introduction
As life expectancy grows globally, the proportion of older adults within the population is set to double between 2015 and 2050 (from 12% to 22%) (WHO Citation2018). Whilst this demographic change can be considered to be largely positive, it also brings to light significant nutritional challenges for an aging population group that are particularly vulnerable to malnutrition and age-related disease (Fávaro-Moreira et al. Citation2016). Consequently, public health dietary advice and guidelines in some countries are tailored for older adults (for example in the USA, though not in the UK) to help guide them towards the specific nutritional requirements necessary to safeguard or improve health in older age (Brownie, Muggleston, and Oliver Citation2015; Scientific Advisory Committee on Nutrition Citation2011; Lichtenstein et al. Citation2008). This advice typically includes recommendations to increase intake of a range of vitamins and minerals, decrease energy requirements and incorporate adequate fluids (British Nutrition Foundation Citation2018; United States Department of Agriculture Citation2018). However, despite these efforts to aid nutritional inadequacies, older adults still remain largely at risk to the many malnutrition-related risk factors that commonly present themselves in later life. For example, in many instances, the risk of malnourishment is exacerbated by impaired dental status and loss of natural teeth (Toniazzo et al. Citation2018). There are many factors which influence tooth loss; it is strongly associated with older age, typically caused by increased rates of dental caries, periodontal disease and dry mouth, all commonly observed in older age (Agostini et al. Citation2018; National Institute of Dental and Craniofacial Research Citation2018; Lopez et al. Citation2017). Although global prevalence of tooth loss is poorly reported, total tooth loss (i.e. being edentulous) is considered to impact up to 14% of the world’s population over 50 years of age (Slade, Akinkugbe and Sanders, Citation2014; NHS Digital Citation2011; Tyrovolas et al. Citation2016). As the loss of natural teeth has been shown to significantly reduce chewing performance and consequently, act as a significant barrier to food choice, edentulism or partial edentulism are both major risk factors for malnourishment among older adults (Kazemi et al. Citation2011). Older adults who encounter such chewing difficulties are at greater risk of having a poor quality diet, as they are less likely to opt for nutrient-dense foods that are harder to masticate such as fruit, vegetables or fiber-based foods (Brodeur et al. Citation1993; Krall, Hayes, and Garcia Citation1998; Marcenes et al. Citation2003). Instead, they are more likely to replace them with easier to chew foods, which are often lacking in key nutrients, and of a high calorie and low dietary fiber content (Watson et al. Citation2019). Whilst previous literature has demonstrated that oral rehabilitation (i.e. restoration of greater chewing function) using a variety of methods (e.g. complete dentures, partial dentures, etc.) can have a positive effect on one’s overall oral health-related quality of life (Zani et al. Citation2009; Kaushik et al. Citation2018; Ali et al. Citation2019), the evidence of a wide-ranging benefit to dietary quality from a variety of oral rehabilitation methods appears to be less commonly observed (Moynihan et al. Citation2000; Hamada et al. Citation2001; Muller, Morais and Feine, Citation2008). This research therefore suggests that replacing missing teeth alone is not predictive of positive dietary behavior change and has highlighted the need for targeted or purposeful dietary intervention alongside oral rehabilitation. This approach has been explored in a number of studies in order to address diet and nutritional challenges in this growing population group with mixed evidence of impact (Bartlett et al. Citation2013; Wöstmann et al. Citation2016). However, an increasing body of randomized controlled trial evidence supports the combination of oral rehabilitation coupled with a purposeful dietary intervention component amongst this population group (Bradbury et al. Citation2006; Amagai et al. Citation2017; Suzuki et al. Citation2017); with reported improvements in dietary intake ranging from increases in fruit and vegetables to protein. Yet, fundamental gaps in understanding remain regarding the content, design and format of these dietary interventions, and how these characteristics might link to the outcomes of such dual interventions (i.e. oral rehabilitation plus dietary intervention). Furthermore, there is a lack of clarity around the theoretical and behavior change basis of existing interventions, including the form of delivery (FoD) (i.e. who delivers the intervention, what it entails, where it is delivered, how often, etc.) and effectiveness (Dombrowski, O’Carroll, and Williams Citation2016). These intervention aspects are of known importance, as the identification of a relevant theory to guide design and evaluation is a crucial step in the development of complex dietary interventions (Craig et al. Citation2008). Furthermore, inclusion of identifiable behavior change techniques (BCTs) has been associated with greater efficacy across a range of health behavior interventions (Michie et al. Citation2008; Greaves et al. Citation2011; Lara et al. Citation2014), with hierarchically structured taxonomies of techniques (BCTs) consensually agreed for specifying intervention components (Michie et al. Citation2013). Greater understanding of the behavioral science basis of dietary interventions used in the domain of oral rehabilitation will have considerable utility in advancing the field as has happened in other domains (Olander et al. Citation2013; French et al. Citation2014; Hill, Skouteris, and Fuller-Tyszkiewicz Citation2013; Hartmann-Boyce et al. Citation2014; Hollywood et al. Citation2017; Martin, Chater, and Lorencatto Citation2013), by helping to concentrate efforts at the most effective behavioral targets to support positive change in future interventions. The objective of this systematic review was to identify, critically review and synthesize existing intervention studies where oral rehabilitation (replacement of natural missing teeth full/partial) was coupled with a purposeful dietary intervention amongst adults, and to examine the impact upon dietary intake (as measured by questionnaires/food diaries and/or biochemical markers of nutritional status e.g. vitamin C where available etc.). Secondary objectives were to investigate oral health status, dietary intervention characteristics and BCTs.
Materials and methods
Protocol and registration
This systematic review was conducted and reported in line with the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement (see Supplemental File I for PRISMA checklist) (Moher et al. 2009) and also using the Cochrane Handbook for Systematic Reviews of Interventions (Higgins and Green Citation2011). This review was prospectively registered with PROSPERO on the 11 July 2017 [CRD42017071075]. An update to data extraction (regarding secondary outcomes) was added on the 12 February 2018 to include intervention BCTs and theoretical underpinnings. Cochrane Collaboration reviewing methods were followed throughout (Higgins and Green Citation2011) and being a systematic review, ethical approval was not required.
Eligibility criteria
Studies were reviewed using the participants, interventions, comparisons, outcomes and study design reporting system (PICOS). They were included if:
(Participants) they conducted oral rehabilitation (replacement of missing natural teeth – full/partial) in edentate or partially dentate adults;
(Interventions) an intentional healthy eating dietary intervention was delivered (i.e. diet-related pamphlets/leaflets, written information, face-to-face, telephone, counseling, etc.) in conjunction with oral rehabilitation as defined as replacement of missing natural teeth;
(Comparisons) comparison was made between ‘standard/usual’ dental care only versus dental care plus dietary intervention (preferred); however, no restrictions/exclusions were applied based upon presence/absence of comparator groups, i.e. before and after studies which delivered both dental care plus dietary intervention with no control/comparator group were eligible;
(Outcomes) dietary outcomes were reported (as measured by questionnaires/food diaries e.g. F/V, protein intake etc. and/or biochemical markers of nutritional status e.g. vitamin C etc.).
(Study design) all intervention study designs were considered in the preliminary inclusion of studies in order to maximize the study pool for final selection.
In addition to the PICOS criteria being satisfied, no exclusions were made based on publication date nor the length of follow-up for intervention studies given that scoping searches did not indicate an extensive range of relevant literature. Furthermore, a study was considered eligible for inclusion if it was a published article in a peer-reviewed journal (i.e. not conference proceeding/editorial), it was available in English, and it was conducted on humans.
Search strategy
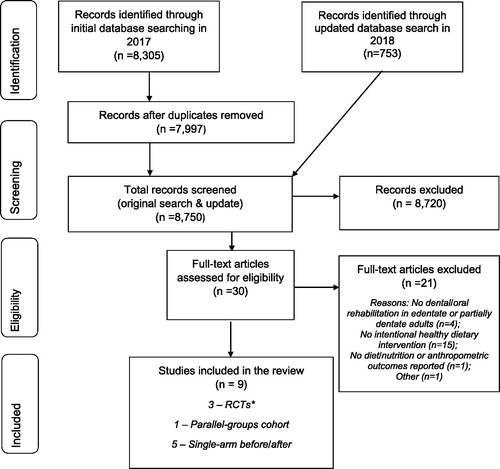
An electronic database search using MEDLINE, Web of Science, PubMed and CENTRAL (Cochrane Central Register of Controlled Trials) was used to identify eligible studies, outlined in . The search strategy was designed and set up by a team of three systematic reviewers (LM, LAM and HR). Initial online searches were performed by reviewers independently using the search terms that were carefully identified in accordance with the eligibility criteria and stated PICOS criteria. The search terms employed were either medical subject headings (MeSH) terms or key words classified under general (all fields) category. The search terms were then combined with an ‘OR’ within categories, and PICOS categories were combined using ‘AND’ to create a final logic search query.
Appropriate adaptions were made to allow search strategies to be conducted on other databases (see Supplemental File II for full search strategies for all databases). All searches were limited to only include published, English, human studies and exclude gray literature. Hand-searching reference lists of eligible studies was performed to identify studies that may not have been discovered online. Further attempts to maximize the pool of relevant studies and avoid any erroneous exclusion involved personal communications sent to selected authors identified in the review. The online search was performed on 6 July 2017; with one further search update performed by LM and VP using the same search terms on the 13 July 2018, covering the period 2017–2018. No further searches were performed after this date.
Study selection
A thorough title and abstract screening was performed by three reviewers (LM, LAM and HR) independently based upon the PICOS framework and eligibility criteria described. The search update performed in July 2018 was screened independently by LM, LAM and VP. Each reviewer created a list of studies for full text analysis. The lists were compared and studies common to both lists were shortlisted. The identified studies unique to each reviewer were then included or discarded from the full text analyses after discussion and mutual agreement. Disagreements were solved by a consensus discussion presided over by another review team member and a final list of studies was put forth for full text analysis and subsequent data extraction and analyses, only after a mutual consensus between at least two reviewers. Studies were considered eligible for the meta-analysis if they compared two groups (i.e. intervention and control) and presented dietary intake data (means) for total fruit and/or vegetable intake in grams per day across timepoints.
Review outcomes
The primary outcome for the review overall focused on dietary intake (as measured by questionnaires/food diaries and/or biochemical markers of nutritional status e.g. vitamin C) for example, including fruit and/or vegetables, fiber, protein and fatty/sugary food intakes. Secondary outcomes included general anthropometry measures where available which may serve as a proxy for health status (e.g. BMI, weight), oral/dental health status, e.g. changes in mastication abilities/perceived chewing abilities; alongside the theoretical basis to the nutritional interventions identified in the review (i.e. the processes through which the intervention is assumed to influence behavior), the BCTs used (i.e. the content of the intervention – explicitly stated or inferred), and the form of intervention delivery (FoD) (i.e. the way in which the intervention is delivered, by whom, in what setting, their expertise, etc.) (Dombrowski, O’Carroll, and Williams Citation2016). The BCTs were categorized using the BCT Taxonomy v1, an extensive taxonomy of 93 hierarchically clustered BCTs (Michie et al. Citation2013).
Data extraction and synthesis
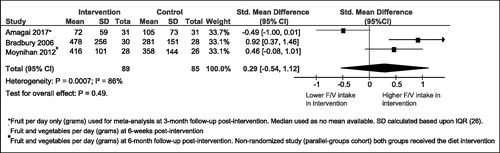
A data extraction spreadsheet was developed and independently reviewed by two researchers (LM and LAM). Generic details of the studies were coded including details of the; study design; research question; sample size; eligibility criteria; statistical analysis; control group characteristics; follow-up period; results summary; demographic data; dental/oral health status and findings; health status; diet/nutritional status, diet/nutritional measures; and any other relevant information. Intervention data was also extracted including further details on the intervention length; content; theory; FoD; delivery personnel; format; intensity; tailoring; materials used and; identifiable BCTs (Michie et al. Citation2013). A detailed assessment of bias was also given in the data extraction spreadsheet (see next section). All data was extracted from the included studies at the group-level and tabulated by two reviewers (LM and LAM). A narrative synthesis was conducted ordered by study design, given study heterogeneity. A random-effects meta-analysis model (DerSimonian and Laird Citation1986) was used to pool data on F/V intake by calculating the standardized mean difference (SMD) between intervention and control/comparator groups (where possible) using Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. A heterogeneity test was conducted and I2 calculated (Higgins and Thompson Citation2002). Median values were used for one study in the meta-analysis where means were unavailable (Amagai et al. Citation2017). In this instance, standard deviation (SD) was calculated based on interquartile range (IQR), where the width of the interquartile range was considered approximately 1.35 SDs (Higgins and Green Citation2011).
Risk of bias
Two members of the research team (LM and LAM) assessed risk of bias (RoB) using the Cochrane Handbook Risk of Bias Tool (Higgins and Green Citation2011) for randomized studies. Bias was assessed under the following domains; selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias (see Supplemental File III for full RoB breakdown for all included studies). The independent reviewers reported bias under each domain for individual studies and also assigned an overall low risk, high risk or unclear risk of bias (see , Supplemental File III). The ROBINS-I tool (Risk Of Bias In Non-randomized Studies – of Interventions) (Sterne et al. Citation2016) was used to assess the risk of bias present in non-randomized and single-arm intervention studies (see in Supplemental File III). ROBINS-I was developed in 2016 to guide judgements on potential sources of bias in non-randomized interventions across a range of domains, where the Cochrane Risk of Bias tool does not coherently fit (due to lack of randomization).
Table 1. Included studies grouped by study design: methodology and risk of bias.
Table 2. Findings’ grouped by study design: dental and diet/nutrition-related outcomes.
Results
Search results
Initial searching for studies examining the effect of oral rehabilitation coupled with dietary intervention was conducted on 6 July 2017. In total, 8,305 possible studies were retrieved and following the removal of duplicates a total of 7,997 studies remained for assessment. Of these, 27 full texts were assessed according to the predefined assessment criteria. Six studies were deemed eligible for inclusion in the review at this stage. The search was updated on the 13 July 2018 to cover the period 2017–July 2018. This search update identified a further 753 individual studies, of which three met the inclusion criteria after full text review (total full text reviews original search plus update n = 30), leaving nine studies for inclusion in the review overall. Full details of the search and review process are presented in the PRISMA flowchart including reasons for exclusion ().
Characteristics of included studies
Of the nine articles included in the review, two reported differing diet and nutrition outcomes from the same RCT leaving both articles eligible for inclusion (Amagai et al. Citation2017; Suzuki et al. Citation2017). Therefore, eight separate studies were reported upon, involving data from 526 participants. Studies predominantly aimed to improve the diet and nutritional status of edentulous older adults using complete dentures (CD) as the form of oral rehabilitation (Amagai et al. Citation2017; Bartlett et al. Citation2013; Bradbury et al. Citation2006; Moynihan et al. Citation2012; Olivier et al. Citation1995; Prakash et al. Citation2012; Suzuki et al. Citation2017;) except in two instances; one where participants were described as partially dentate (Nabeshima et al. Citation2018), and another where participants had a severely reduced dentition (Wöstmann et al. Citation2016).
Three articles reported outcomes drawn from two RCTs (Amagai et al. Citation2017; Bradbury et al. Citation2006; Suzuki et al. Citation2017); one article reported a two-cohort prospective parallel dietary intervention study (comparing the same dietary intervention across two groups with different forms of oral rehabilitation) (Moynihan et al. Citation2012), and the remaining five studies were identified as single-arm before and after intervention studies, with no control/comparator group (Bartlett et al. Citation2013; Nabeshima et al. Citation2018; Olivier et al. Citation1995; Prakash et al. Citation2012; Wöstmann et al. Citation2016). The results are presented within these differing strength of evidence categories following a short summary of study characteristics overall.
Overall summary
Participants recruited to the studies were edentulous except for those in the single-arm studies by Wöstmann et al. (Citation2016) (inclusion criteria was fewer than ten pairs of opposing natural teeth (antagonists) and required new (first-time) fixed or removable prostheses) (Wöstmann et al. Citation2016), and Nabeshima et al. (Citation2018) (participants received definitive removable partial dentures (RPDs), and had an average of 16.6 (5.5 SD) teeth remaining) (Nabeshima et al. Citation2018). One study purposefully recruited edentulous adults requiring their first set of CD (Prakash et al. Citation2012); another recruited participants who had their prosthesis made between 3 months and less than 5 years (Moynihan et al. Citation2012); and across all other studies participants were eligible if edentulous for at least one year (thus existing CD users). The majority of participants were female (one study was female-only (Olivier et al. Citation1995); in one study sex ratio was unreported (Prakash et al. Citation2012); with only the most recent studies reporting an even sex ratio (Amagai et al. Citation2017; Suzuki et al. Citation2017; Wöstmann et al. Citation2016). Age of participants ranged from 50 – 80 years (median age 72.5 years).
Sample sizes for included studies were small. In the single-arm (before/after studies) sample sizes ranged from n = 20 to n = 94 participants (Bartlett et al. Citation2013; Nabeshima et al. Citation2018; Olivier et al. Citation1995; Prakash et al. Citation2012; Wöstmann et al. Citation2016). The parallel groups cohort study (Moynihan et al. Citation2012) reported 54 completers (n = 26 in the complete (conventional) dentures group [CD] and n = 28 in the implant-supported overdentures group [IOD]), with the RCTs reporting final sample sizes of N = 62 (n = 31 intervention; n = 31 control) (Amagai et al. Citation2017; Suzuki et al. Citation2017) and N = 58 (n = 30 intervention and n = 28 control) (Bradbury et al. Citation2006); with equal attrition reported across study arms for the RCTs.
The majority of studies identified were published within the past 10 years (Amagai et al. Citation2017; Bartlett et al. Citation2013; Moynihan et al. Citation2012; Nabeshima et al. Citation2018; Prakash et al. Citation2012; Suzuki et al. Citation2017; Wöstmann et al. Citation2016) and all studies identified reported at least one positive diet/nutritional finding. The most recent RCT conducted in Japan was published in 2017 (reported across two articles (Amagai et al. Citation2017; Suzuki et al. Citation2017)); the other RCT conducted in England was published in 2006 (Bradbury et al. Citation2006); the single-arm pilot studies drawn from India (Prakash et al. Citation2012), England (Bartlett et al. Citation2013), Germany (Wöstmann et al. Citation2016) and Japan (Nabeshima et al. Citation2018) were published in 2011, 2013, 2016 and 2018, respectively, and the parallel-groups cohort study conducted in England was published in 2012 (Moynihan et al. Citation2012). The oldest data came from a single-arm, female only study conducted in Canada, published in 1995 (Olivier et al. Citation1995).
Randomized controlled trials
Included studies
Details of the three studies (Bradbury et al. Citation2006; Amagai et al. Citation2017; Suzuki et al. Citation2017) reporting RCT evidence are given in . One RCT (reported across two articles) sought to clarify the effect of CD (replacement) treatment in combination with simple dietary advice on food intake among elderly Japanese edentulous participants (Amagai et al. Citation2017; Suzuki et al. Citation2017). The dietary intervention involved two 20 minute one-to-one sessions with a dentist and focused on simple dietary advice, with participants followed up at 3 months. The RCT by Bradbury et al. (Citation2006) aimed to evaluate the effectiveness of a theory-based, tailored nutrition intervention delivered by a trained nutritionist, to increase the F/V intake of edentulous participants receiving replacement CD and followed up after 6 weeks. Both RCTs involved delivery of two nutrition-related sessions over the intervention timeframe and primary outcomes related to weight of F/V consumed (as measured by 3-day food diaries (Bradbury et al. Citation2006); or protein intake assessed via a validated self-report questionnaire (Brief Diet History Questionnaire (Amagai et al. Citation2017; Suzuki et al. Citation2017)).
Findings: diet/nutrition outcomes
Both RCTs reported improvements in a least one area of diet/nutrient intake post-intervention based on self-reported patient outcomes, i.e. food diaries or questionnaires (see ). The RCT reported by Suzuki et al. (Citation2017) and Amagai et al. (Citation2017) was powered to detect a change in protein intake. Findings reported by Suzuki et al. focused on nutrient intakes, illustrating that protein intake in the dietary intervention group significantly increased compared with that in the denture care control group at 3-month post-treatment (p = 0.001), alongside a number of other key nutrients in a positive direction (see ), whereas Amagai et al. (Citation2017) reported on food groups. There were no reported differences in food intake between the two groups at baseline; however, at the 3-month assessment, the dietary intervention group showed significantly greater intake of chicken and fish (with bones) (in line with protein as primary outcome), and carrots and pumpkins compared to the control group (see ) (Amagai et al. Citation2017). No other food or drinks showed a significant change.
The RCT reported by Bradbury et al. (Citation2006) showed the dietary intervention group had significantly greater increases in total F/V intake and fruit (including fruit juice) than the control group (primary outcome). Energy and macronutrient intakes were not significantly different between groups at follow-up; regarding micronutrients, vitamin C and β-carotene were significantly higher in the intervention group at follow-up (see ).
Findings: dental status and oral health outcomes
Findings from the three RCTs relating to dental status and oral health are displayed in . Suzuki and colleagues report that masticatory function (measured objectively) was not significantly different between groups at baseline, but significantly increased at 3-month post-treatment compared with the baseline in both groups (Suzuki et al. Citation2017). The intervention group showed a significant increase in objectively measured shearing ability post-intervention (i.e. ability to crush a food object between teeth, in a back and forth motion), not matched by the control group, despite oral rehabilitation being matched between groups.
Amagai et al. (Citation2017) reported that at baseline and at the 3-month assessment, there was no significant difference in self-reported OHIP-EDENT-J scores between groups; however, the OHIP-EDENT-J scores significantly improved for both groups at the 3-month assessment. There were a greater number of significantly improved dimensions of OHIP-EDENT-J in the dietary intervention group than in the denture care advice control group at the 3-month assessment (Amagai et al. Citation2017). The dietary intervention group showed significant improvements in six of the seven domains; in contrast, the control group showed significant improvements in only three domains (Amagai et al. Citation2017) (see ). In the RCT reported by Bradbury et al (Citation2006), perceived chewing ability post-insertion of replacement CD (self-reported ability to bite/chew, denture fit and comfort etc.) improved significantly across both groups and was not significantly different between groups.
Findings: theoretical basis, FoD and BCTs
The Japanese RCT (Amagai et al. Citation2017; Suzuki et al. Citation2017) did not report any theoretical basis to the dietary intervention (see ); the RCT by Bradbury et al. (Citation2006) was explicitly based upon the Stages of Change model (Prochaska, DiClemente, and Norcross Citation1992) and intervention materials were designed to address optimistic bias (Weinstein Citation1980), i.e. induce discrepancy between current behavior and ideal/recommended intakes for F/V. Both RCTs followed a similar FoD (two dietary advice sessions, one at denture try-in and one at final fitting); however, dietary advice was individually-tailored based on current intake levels and delivered by a nutritionist in the RCT by Bradbury et al., whereas a dentist not involved in the clinical aspects of denture fitting delivered the dietary advice based on a uniform pamphlet in the Japanese RCT (Amagai et al. Citation2017; Suzuki et al. Citation2017). BCTs (identified from the published articles and versions of the pamphlets given to participants in each trial) differed between the two RCTs (see and Supplemental File IV). In the Japanese RCT intervention group there were five BCTs, focusing mainly on information-giving strategies regarding current dietary recommendations and the health consequences of poor diet (Amagai et al. Citation2017; Suzuki et al. Citation2017). Self-monitoring charts were also available in the pamphlet which participants may/may not have used. In the RCT by Bradbury et al. (Citation2006) eight BCTs were identified, where in addition to those BCTs in the Japanese RCT, they included problem-solving, action planning and tailored feedback based upon participants’ dietary self-monitoring (food diaries and diet questionnaire).
Table 3. Findings’ grouped by study design: theoretical basis, intervention content, form of delivery and identifiable BCTs.
Assessment of bias
RoB ratings for the RCTs varied across the domains of assessment (see and Supplemental File III). Selection bias was possible in the RCT by Bradbury et al., (Citation2006) as despite randomization, only patients already attending dental-student clinics were invited to participate. For the Japanese RCT a variety of approaches to recruitment were used including reviewing dental records, placing advertisements in geriatric magazines/websites, posters and flyers in the dental hospital (Amagai et al. Citation2017; Suzuki et al. Citation2017). Performance bias was possible in this latter RCT as the dietary advice was delivered by one of two dentists, with no detail on provided their level of dietetics/nutrition training. Detection bias was possible given the incomplete nature of blinding in both RCTs; as for example, it was reported that despite efforts to blind, participants inevitably disclosed their allocation to evaluators (Bradbury et al. Citation2006); and, that the same researchers delivering the intervention advice sessions analyzed the results (Amagai et al. Citation2017; Suzuki et al. Citation2017). Attrition bias risk was low for both RCTs, as moderate, equal attrition from study arms was reported (approximately 12% attrition in each arm (Bradbury et al. Citation2006); 11.4% attrition each arm (Amagai et al. Citation2017; Suzuki et al. Citation2017), with detail on reasons for drop-out relating to lack of interest or development of disease. Risk of reporting bias was considered high in the RCT by Bradbury et al. (Citation2006) as the trial was not registered, with no protocol available. Therefore, despite inclusion of reporting on non-significant outcomes, it is unclear as to whether the primary outcome matched original intentions. Low reporting bias was found in the Japanese RCT as the trial was registered and a published protocol detailing the primary outcome was available, which matched outcome reporting in both articles (Amagai et al. Citation2017; Suzuki et al. Citation2017).
Two-cohort prospective parallel groups studies
Included studies
Only one study (Moynihan et al. Citation2012) followed this type of design (see for methodological details). Moynihan et al. (Citation2012) sought to test the effect of tailored dietary advice (delivered by a community nutrition assistant) across two groups of participants with differing preexisting forms of oral rehabilitation (CD and IODs). The intervention design followed that of the Bradbury et al. (Citation2006) RCT; the primary outcome related to F/V intake and blood samples were included to examine plasma biomarkers of antioxidant status.
Findings: diet/nutrition outcomes
No significant difference was reported in relation to the primary outcome of F/V between-groups as both groups increased their F/V intake (grams per day) from baseline at both 3 and 6 months (trend for greater gains in g/day for the IOD group) (see ) (Moynihan et al. Citation2012). The IOD group reported a significant reduction in percentage energy obtained from saturated fat compared to the CD group at 3 months not sustained at 6 months, and although serum antioxidant levels improved for both groups, the IOD group showed significantly greater improvements at all time-points (measured by FRAP (ferric-reducing antioxidant power) and TEAC (trolox equivalent antioxidant capacity) methods) (Moynihan et al. Citation2012).
Findings: dental status and oral health outcomes
There was an overall trend for perceived chewing ability (self-reported) to be lower for the CD group versus the IOD group at baseline and 3-month follow-up; however, this difference only reached statistical significance at 6-month follow-up (Moynihan et al. Citation2012).
Findings: theoretical basis, FoD and BCTs
This dietary intervention followed the same format (though different patient group) as Bradbury et al. (Citation2006). It was explicitly based upon the Stages of Change model (Prochaska, DiClemente and Norcross Citation1992) and designed intervention materials to address optimistic bias (Weinstein Citation1980) by inducing discrepancy between current behavior and ideal/recommended intakes for F/V. Eight BCTs were identifiable and the intervention involved the production of a tailored written educational package for each participant, based upon data from their food diaries and a dietary behavior questionnaire (completed at the first session) (Moynihan et al. Citation2012) (See and Supplemental File IV).
Assessment of bias
Moynihan et al. (Citation2012) reported that females were over-represented (across both groups) and participants in the CD group were significantly older than those in the IOD group (controlled for in subsequent analyses) – although they did not differ by measures of socio-economic status. Differential attrition (attrition bias) was noted between the two groups before the dietary intervention commenced (n = 27 CD participants withdrew and n = 10 IOD participants) however, those who withdrew did not differ by age, sex or socio-economic status compared to completers. Only partial blinding was possible (nutrition assistants were told the purpose was to examine the impact of dietary advice on the diet of denture wearers’, however they were unaware of the different study groups), and as such, any impact upon the measurement of outcomes is suggested to have been equal across both groups (Moynihan et al. Citation2012) (see and Supplemental File III).
Non-controlled before and after studies
Included studies
Methodological details are given in . The five single-arm studies (Bartlett et al. Citation2013; Nabeshima et al. Citation2018; Olivier et al. Citation1995; Prakash et al. Citation2012; Wöstmann et al. Citation2016) identified differed regarding their aims: one study primarily tested the impact of a denture adhesive alongside provision of two dietary information leaflets on participants’ diets (Bartlett et al. Citation2013); one was specified as a pilot study to examine the impact of tailored dietary counseling on the diet of those undergoing (new) implant-prosthetic treatment (Wöstmann et al. Citation2016); one focused on fiber intake with the view to reducing gastrointestinal symptoms (Olivier et al. Citation1995); one focused on MNA improvements following (new) CD fabrication and brief advice on a healthy diet (Prakash et al. Citation2012); and, one aimed to investigate dietary counseling on the nutritional status of participants receiving RPDs, and to ascertain the role of occlusal support on the effects of the dietary intervention (Nabeshima et al. Citation2018).
Findings: diet/nutrition outcomes
Four of the five single-arm studies reported statistically significant improvements in primary outcomes pertaining to F/V intake, fiber intake and MNA scores (Bartlett et al. Citation2013; Nabeshima et al. Citation2018; Olivier et al. Citation1995; Prakash et al. Citation2012) (see ). Blood plasma levels of α- and β-carotene remained constant which did not support self-reported increases in vegetables in the study by Nabeshima et al. (Citation2018). Furthermore, sub-analyses conducted examining the role of OUs in dietary intake indicated that the presence of OUs was predictive of greater vegetable intake and greater odds of consuming target amounts per day (p < 0.05) (Nabeshima et al. Citation2018).
No primary outcome was specified by Wöstmann et al. (Citation2016) given it was designed as a pilot study and aimed to examine a range of blood and nutritional parameters to identify possible markers for a future large-scale study. Whilst no significant differences were observed for nutrient intake or food choice, a significant increase was noted for cholinesterase and ferritin at 6 months alongside a decrease in Vitamin A, and folic acid intake fell between 6 and 12 months, though no reasons are posited regarding these findings (Wöstmann et al. Citation2016). There was a trend for caloric reduction which did not reach statistical significance (Wöstmann et al. Citation2016).
Findings: dental status and oral health outcomes
Two studies reported improvements regarding ability to bite/chew etc. based upon self-reported data (Bartlett et al. Citation2013; Prakash et al. Citation2012), with only Bartlett et al. (Citation2013) specifying statistically significant improvements. Wöstmann et al. (Citation2016) reported OHRQoL improvements alongside significant improvements in objective chewing efficiency pre-to-post intervention; Olivier et al. (Citation1995) reported significant improvements in both objective and self-reported measures chewing and swallowing measures; however, scores remained below functional levels, even at final follow-up (6–9 months). Nabeshima et al. (Citation2018) reported significant improvements over time for maximal biting force (MBF) and objective masticatory performance, however perceptions of chewing ability did not improve across participants over time.
Findings: theoretical basis, FoD and BCTs
No underlying theory was reported explicitly as guiding any of the single-arm interventions (Bartlett et al. Citation2013; Nabeshima et al. Citation2018; Olivier et al. Citation1995; Prakash et al. Citation2012; Wöstmann et al. Citation2016) (see ); however, Nabeshima et al. (Citation2018) suggest their intervention was administered in accordance with a previous study by Bradbury et al. (Citation2006) which was explicitly based upon the Stages of Change and Optimistic Bias theoretical constructs. No discussion or measures pertaining to these theoretical components are present in the Nabeshima article. In two studies, a dietitian delivered the dietary intervention (one single intervention session in each) which was individually tailored based on prior food diary data (Olivier et al. Citation1995: Wöstmann et al. Citation2016). One study specified ‘a trained examiner’ delivered the intervention explicitly stating that ‘no attempt was made to provide dietary counseling’ beyond giving two pamphlets on healthy eating and asking participants to read them (Bartlett et al. Citation2013); another other study did not report who delivered the brief dietary advice, although this was conducted during CD fitting (Prakash et al. Citation2012); and in the most recent study a dentist delivered both counseling sessions (Nabeshima et al. Citation2018). Identifiable BCTs based on the published articles ranged from one (Prakash et al. Citation2012) to nine (Olivier et al. Citation1995) (see full details and Supplemental File IV). The dietary intervention by Bartlett et al. (Citation2013) contained 4 identifiable BCTs which focused on information-giving (two healthy eating pamphlets) containing information about health consequences of diet (including BMI charts) and detail on how to perform the behavior (i.e. eat healthily) with recipes included. Interventions by Wöstmann et al. (Citation2016) and Nabeshima et al. (Citation2018) each contained five BCTs with common intervention components relating to instruction on how to perform the behavior and dietary information delivered by a credible source (i.e. a health professional).
Assessment of bias
The RoB across all single-arm studies was considered high overall, with one judgement of serious bias (Wöstmann et al. Citation2016), two of moderate (Olivier et al. Citation1995; Nabeshima et al. Citation2018) and two considered critical (Bartlett et al. Citation2013; Prakash et al. Citation2012) (see Supplemental File III for detailed breakdown of categories). Given that the single-arm studies were non-randomized and as such did not have pre-registered trial protocols, it is unknown if reported primary outcomes matched original proposals. Furthermore, the study by Prakash et al. (Citation2012) was poorly reported regarding participant characteristics, intervention content, FoD, BCTs and outcomes, with limited data collection tools highlighting significant methodological uncertainties. In the study by Bartlett et al. (Citation2013), fundamental confounders exist as the authors discuss how beneficial changes in F/V intake may be associated with the use of denture adhesive or the healthy eating pamphlets, with available data unable to disentangle these effects. The pilot study by Wöstmann et al. (Citation2016) discussed a socio-economic bias in their sample in that participants were typically affluent, as there was a high cost to cover in relation to the implant-prosthetic rehabilitation, and they were more likely to be already consuming an adequate diet at baseline. The study by Olivier et al. (Citation1995) was conducted more than 20 years ago and despite a comprehensive discussion of the intervention and FoD, limitations may exist regarding interpretation of findings and generalizability of outcomes in today’s world. Nabeshima et al. (Citation2018) report discrepancies between participants’ self-reported dietary improvements and objective plasma markers, indicating the possible presence of socially-desirable reporting at follow-up.
Magnitude of F/V changes across studies
Three studies provided data pertaining to two groups (intervention and a comparator/control group) to enable a meta-analysis of F/V intake (Amagai et al. Citation2017; Bradbury et al. Citation2006; Moynihan et al. Citation2012) where a random effects model was used to calculate SMD (See ). F/V intake was, on average, higher by 0.29 SDs in the intervention group compared to the control (SMD 0.29 [−0.54, 1.12]), although the model was not statistically significant overall (p = 0.49). Findings were not consistent across studies with high heterogeneity noted (I2 = 86%, p = 0.0007); in particular, a more marked increase in F/V intake was observed in the RCT by Bradbury et al. Citation2006.
Figure 2. Forest plot showing the effect of intervention on standardized mean difference (SMD) F/V intake across a subgroup of interventions with a control/comparator group.
Further subgroups analyses by type of oral rehabilitation or by age/sex was not possible given the limited number of studies with small sample sizes, and the predominance of women participants in the studies included in the review.
Discussion
The available empirical evidence relating to this topic is limited to a small number of heterogeneous study designs with small sample sizes. Based on a narrative synthesis of data there is support for a dual intervention approach combining oral rehabilitation with a purposeful dietary intervention in order to improve dietary intake in older adults. All studies reported improvements in one aspect of oral health (i.e. biting/chewing) for the majority of participants, albeit with some slight between-group variations (discussed later), alongside at least one positive diet/nutritional post-intervention outcome, however objective plasma biomarkers did not always support self-reported dietary improvements (Nabeshima et al. Citation2018; Wöstmann et al. Citation2016). Explicit use of theory to guide dietary intervention design and/or evaluation was limited (n = 2) (Bradbury et al. Citation2006; Moynihan et al. Citation2012) and identifiable BCTs varied greatly across interventions making it difficult to discriminate effective intervention strategies. There was a focus on information-giving strategies, which are not typically associated with the most effective behavior change outcomes in this age group (Lara et al. Citation2014). Of the three studies included in the meta-analysis, two contained an identical set of eight identifiable BCTs each which successfully improved dietary outcomes (F/V) (Bradbury et al. Citation2006; Moynihan et al. Citation2012); furthermore, there was a high degree of overlap regarding BCTs between these aforementioned studies and the third study in the meta-analysis (Amagai et al. Citation2017) – with all three studies including the BCTs: self-monitoring of dietary behavior, instruction on how to perform the behavior, information on the health consequences, and delivery of the intervention from a credible source. To our knowledge, no other reviews of this nature have been conducted with this population group, and therefore it offers comprehensive insight into the impact of a dual intervention focusing on dietary intervention coupled with oral rehabilitation, alongside characterization of the behavioral science components of such interventions.
Positive diet-related primary outcomes for the intervention groups predominantly focused on F/V intake (n = 4) (Bartlett et al. Citation2013; Bradbury et al. Citation2006; Moynihan et al. Citation2012; Nabeshima et al. Citation2018). Adequate F/V intake is of particular importance for aging adults given its association with a lower risk of all-cause mortality, particularly cardiovascular mortality (Wang et al. Citation2014). Bartlett et al. (Citation2013) illustrated significant gains in F/V intake (servings increased by 1.4 servings per day (p < 0.0001) with corresponding significant increases in Vitamin C levels), although these intervention findings are confounded by the concurrent use of denture adhesive alongside the provision of healthy eating pamphlets. Moynihan et al. (Citation2012) reported gains of approximately one F/V serving per day for the IOD group at 3 months (87 g/d for IOD group) and over half a serving per day for the CD group (54 g/d for CD group) which persisted at 6 months for both groups. The lack of between-group differences is somewhat expected given that both the IOD group and the CD group received the same tailored dietary intervention (i.e. no true ‘control’ group) – what differed between-groups was the form of oral rehabilitation (IOD versus CD) (Moynihan et al. Citation2012). Nonetheless, the levels of additional F/V intake reported across these studies may confer clinically significant improvements to health (Wang et al. Citation2014). Due caution should be observed however, given the methodological uncertainties of these latter studies with greater emphasis placed upon RCT evidence (n = 3) (Amagai et al. Citation2017; Bradbury et al. Citation2006; Suzuki et al. Citation2017). Individually, the RCTs provide support for improved diet/nutrition in the intervention group; in the RCT by Bradbury et al. (Citation2006) (involving theory-based, tailored dietary advice), participants in the dietary intervention group increased their F/V intake by over 200 g/d (+209 g/d – over two portions) compared to the ‘standard denture care’ control group (+26 g/d), though follow-up was limited to 6 weeks. These gains in F/V intake far exceed those reported in the existing literature with participants who aren’t undergoing oral rehabilitation (Luszczynska et al. Citation2016) perhaps due to restoration of mastication abilities via tooth replacement, although further explanation is not offered by the authors (Bradbury et al. Citation2006). The meta-analysis conducted with three (of nine) interventions did not support a significant benefit of dietary intervention on F/V intake (p = 0.49); however, substantive limitations to the meta-analysis and marked heterogeneity leave it difficult to draw firm conclusions. For example, fruit intake alone (versus fruit and vegetables combined) was used for one study which also did not contain mean intake data, therefore median values were used (Amagai et al. Citation2017). Another study was not randomized and did not have a true comparator group (Moynihan et al. Citation2012) with both groups receiving the dietary intervention, therefore the impact of the intervention may have been diluted. Furthermore, diet/nutritional outcomes may have been confounded by oral health status in the Japanese RCT (Amagai et al. Citation2017; Suzuki et al. Citation2017); as despite both groups receiving the same oral rehabilitation, the control group (i.e. denture care advice only) reported lower levels of OHRQoL post-intervention, further illustrated by significantly lower shearing ability scores (food-crushing abilities, in a back and forth motion). The authors suggest this may have been due to floor effects in shearing ability, and that greater self-reported OHRQoL improvements in the dietary intervention group may have been noted as a result of greater awareness of eating function, brought about via the dietary advice (Suzuki et al. Citation2017). As stated, few interventions were theory-based (n = 2) or designed intervention components or outcome evaluations within a theoretical framework, yet, there was a suggestion that the greatest gains in dietary improvement (F/V intake) came from these theory-based interventions (Bradbury et al. Citation2006; Moynihan et al. Citation2012) (indicative in the meta-analysis). They employed the BCTs tailoring of dietary feedback, problem-solving, action-planning and included self-monitoring (Bradbury et al. Citation2006; Moynihan et al. Citation2012). This supports previous research from other health-behavior domains, where interventions with these aforementioned BCTs have been associated with greater effectiveness (Greaves et al. Citation2011; Hill et al. Citation2013; Lara et al. Citation2014; Martin, Chater, and Lorencatto Citation2013). Interestingly systematic review evidence highlights the beneficial role of ‘social support’ in lifestyle interventions, particularly with older adults (Greaves et al. Citation2011; Lara et al. Citation2014), yet none of the interventions in this review explicitly targeted this.
Future studies
Given the limited evidence base highlighted in this study, there is a need for large scale experimental designs to determine the effect of dietary interventions alongside oral rehabilitation. RCTs should be appropriately powered and could be undertaken on either a parallel-arm basis or as a factorial design. Furthermore, given the considerable global burden of suboptimal diets (Reynolds et al. Citation2019), future intervention studies should incorporate more comprehensive and holistic dietary assessment measures which are particularly relevant to the aging population (for example, assessing the Mediterranean diet compatibility, given its links to healthy cognitive aging (Morris et al. Citation2015) rather than examining changes in isolated dietary components (such as fruit and vegetable intake) (Berendsen et al. Citation2017; Bonaccio et al. Citation2018; Afshin et al. Citation2019). Additionally, given that not all studies in the present review included information on energy intake (kcal/per day) (n = 5 of 9) nor examined macronutrients, it was not possible to comment on a particular trend from the available data; future studies should therefore comprehensively assess macronutrient intake and energy intake in order to make an accurate assessment of the impact of any dietary intervention on overall diet quality and pattern.
Strengths and limitations of included studies
The findings of this review are limited by the quality of evidence currently available regarding robust study design. Furthermore, the majority of studies included focused on edentate participants; whilst this population group is very important, recent epidemiological evidence has demonstrated a shift towards a partially dentate older population with lower prevalence and incidence of severe tooth loss (Kassebaum et al. Citation2014). Additionally, the dietary outcomes reported from the studies included in this review mainly focused on examining changes in isolated dietary components (such as F/V or protein intake, for example) rather than looking at the impact upon overall energy intake and/or dietary patterns, a factor of known importance, particularly with regard to growing evidence for benefit of the Mediterranean diet pattern and healthy cognitive aging (Morris et al. Citation2015).
Strengths and limitations of the review
Limitations to review findings arise as dietary interventions were poorly described, lacking adequately operationalized intervention components – relating to both FoD and BCTs implemented. Therefore, it is not known if all intervention aspects have been fully accounted for. In addition, whilst there was significant overlap regarding the BCTs used in the dietary interventions (e.g. self-monitoring of dietary behavior, instruction on how to perform the behavior, information on the health consequences and delivery of the intervention from a credible source) there were also differences across studies, with certain BCTs appearing in only one study and not others (e.g. demonstration of the behavior and behavioral substitution). Furthermore, despite RCT evidence suggesting a positive impact of intervention on the diets of adults, non-significant findings on F/V intake in the meta-analysis (for a small number of studies) limits the strength of this finding. Strengths of the review include a wide variety of systematic search methods used to obtain the relevant literature and the inclusion of worldwide research. A further strength is the novel focus on the behavioral science characterization of dietary interventions within this field and the use of the 93-item BCT v1 taxonomy.
Conclusions
Based upon a narrative synthesis, the limited robust evidence available suggests moderate support for a dual intervention approach combining oral rehabilitation with purposeful dietary intervention in order to improve dietary intake in older adults, particularly in relation to increasing F/V and protein intake, in addition to oral health improvements. Greater dietary improvements were evident for the two dietary interventions based explicitly upon theory and involving the BCTs of problem-solving, self-monitoring and tailoring of dietary feedback. Findings were unclear regarding intervention delivery format and how this might link to effectiveness. Characterizing the behavioral science basis of interventions with this population group is novel and significant, as this population group are at a high-risk of poor dietary intake and inadequate nutritional status; this approach provides greater transparency in relation to intervention content, delivery and BCTs; imperative for the design of future effective interventions. Moreover, given the complex and multifactorial influences on dietary intake, this type of purposeful dietary intervention with adequate behavior change strategies embedded could help to facilitate positive dietary change in older adults or those at risk of malnutrition due to impaired dental status, before the progression of nutritional decline. From a public health perspective, these type of dietary interventions should be tested and implemented in a range of settings including within routine dental practice and within care home settings in order to maximize the public health impact.
PubMed indexing
McGowan, McCrum, Watson, Cardwell, McGuinness, Rutherford, Paice, Moore, Brocklehurst, Woodside, McKenna.
Authors’ contributions
GMK, LM, JVW, SW, LAM, CC, BM, PRB and CM designed the research; LM and LAM predominantly conducted the research; HR and VP conducted database searching and assisted with title and abstract screening; LM, LAM and CC analyzed data and performed relevant synthesis/analyzes; LM mainly wrote the article with input from LAM; GMK and LM had primary responsibility for final content; and all authors read, edited and approved the final manuscript.
| Abbreviations | ||
| BCT(s) | = | behavior change technique(s) |
| BDHQ | = | brief diet history questionnaire |
| BMI | = | body mass index |
| CD | = | complete dentures |
| CG | = | control group |
| F/V | = | fruit/vegetables |
| FoD | = | form of delivery |
| IG | = | intervention group |
| MBF | = | maximal biting force |
| MNA | = | Mini-Nutritional Assessment |
| OHIP-EDENT-J | = | oral health impact profile for edentulous adults – Japanese version |
| OHRQoL | = | oral health related quality of life |
| OU(s) | = | occlusal units |
| RCT(s) | = | randomized controlled trial(s) |
| RPDs | = | removable partial dentures |
| SMD | = | standardized mean difference |
Acknowledgements
The authors would like to thank Helen Rutherford (HR) and Victoria Paice (VP) for their valuable contributions regarding literature searching and article screening during their summer studentship placements at the Centre for Public Health, Queen’s University Belfast.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
This work was supported by a grant from the Health Service Executive (HSE) Research Awards on Ageing (ref: HaPAI/2015/GM) and the Public Health Agency R&D Office Enabling Research Award (ref: STL/5187/15).
References
- Afshin, A., P. J. Sur, K. A. Fay, L. Cornaby, G. Ferrara, J. S. Salama, E. C. Mullany, K. H. Abate, C. Abbafati, and Z. Abebe. 2019. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 393 (10184):1958–72. doi: 10.1016/S0140-6736(19)30041-8.
- Agostini, B. A., G. O. Cericato, E. R. D. Silveira, G. G. Nascimento, F. D. S. Costa, W. M. Thomson, and F. F. Demarco. 2018. How common is dry mouth? Systematic review and meta-regression analysis of prevalence estimates. Brazilian Dental Journal 29 (6):606–18. doi: 10.1590/0103-6440201802302.
- Ali, Z., S. R. Baker, S. Shahrbaf, N. Martin, and M. V. Vettore. 2019. Oral health-related quality of life after prosthodontic treatment for patients with partial edentulism: A systematic review and meta-analysis. The Journal of Prosthetic Dentistry 121 (1):59–68.e3. doi: 10.1016/j.prosdent.2018.03.003.
- Amagai, N., Y. Komagamine, M. Kanazawa, M. Iwaki, A. Jo, A. Suzuki, and A. Minakuchi. 2017. The effect of prosthetic rehabilitation and simple dietary counseling on food intake and oral health related quality of life among the edentulous individuals: A randomized controlled trial. Journal of Dentistry 65:89–94. doi: 10.1016/j.jdent.2017.07.011.
- Bartlett, D. W., B. Maggio, D. Targett, M. R. Fenlon, and J. Thomas. 2013. A preliminary investigation into the use of denture adhesives combined with dietary advice to improve diets in complete denture wearers. Journal of Dentistry 41 (2):143–7. doi: 10.1016/j.jdent.2012.10.012.
- Berendsen, A. A. M., J. H. Kang, O. van de Rest, E. J. M. Feskens, L. C. P. G. M. de Groot, and F. Grodstein. 2017. The dietary approaches to stop hypertension diet, cognitive function, and cognitive decline in American older women. Journal of the American Medical Directors Association 18 (5):427–32. doi: 10.1016/j.jamda.2016.11.026.
- Bonaccio, M., A. Di Castelnuovo, S. Costanzo, A. Gialluisi, M. Persichillo, C. Cerletti, M. B. Donati, G. de Gaetano, and L. Iacoviello. 2018. Mediterranean diet and mortality in the elderly: A prospective cohort study and a meta-analysis. British Journal of Nutrition 120 (8):841–54. doi: 10.1017/S0007114518002179.
- Bradbury, J., J. M. Thomason, N. J. Jepson, A. W. Walls, P. F. Allen, and P. J. Moynihan. 2006. Nutrition counselling increases fruit and vegetable intake in the edentulous. Journal of Dental Research 85 (5):463–8. doi: 10.1177/154405910608500513.
- British Nutrition Foundation. 2018. Older adults. https://www.nutrition.org.uk/nutritionscience/life/older-adults.html?start=1 (accessed 26 May 2019).
- Brodeur, J. M., D. Laurin, R. Vallee, and D. Lachapelle. 1993. Nutrient intake and gastrointestinal disorders related to masticatory performance in the edentulous elderly. Journal of Prosthetic Dentistry 70 (5):468–73.
- Brownie, S., H. Muggleston, and C. Oliver. 2015. The 2013 Australian dietary guidelines and recommendations for older Australians. Version 2 February 2019. www.nrv.gov.au (accessed 10 May 2019).
- Craig, P., P. Dieppe, S. Macintyre, S. Michie, I. Nazareth, and M. Petticrew. 2008. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 337:a1655.
- DerSimonian, R., and N. Laird. 1986. Meta-analysis in clinical trials. Controlled Clinical Trials 7 (3):177–88.
- Dombrowski, S. U., R. E. O’Carroll, and B. Williams. 2016. Form of delivery as a key ‘active ingredient’ in behavior change interventions. British Journal of Health Psychology 21 (4):733–40. doi: 10.1111/bjhp.12203.
- Fávaro-Moreira, N. C., S. Krausch-Hofmann, C. Matthys, C. Vereecken, E. Vanhauwaert, A. Declercq, G. E. Bekkering, and J. Duyck. 2016. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Advances in Nutrition 7 (3):507–22. doi: 10.3945/an.115.011254.
- French, D., E. Olander, A. Chisholm, and J. Mc Sharry. 2014. Which behavior change techniques are most effective at increasing older adults’ self-efficacy and physical activity behavior? A systematic review. Annals of Behavioral Medicine 48 (1):225–34.
- Greaves, C. J., K. E. Sheppard, C. Abraham, W. Hardeman, M. Roden, P. H. Evans, and P. Schwarz. 2011. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 11:119.
- Hamada, M. O., N. R. Garrett, E. D. Roumanas, K. K. Kapur, E. Freymiller, T. Han, R. M. Diener, T. Chen, and S. Levin. 2001. A randomized clinical trial comparing the efficacy of mandibular implant-supported overdentures and conventional dentures in diabetic patients. Part IV: Comparisons of dietary intake. The Journal of Prosthetic Dentistry 85 (1):53–60. doi: 10.1067/mpr.2001.112491.
- Hartmann-Boyce, J., D. J. Johns, S. A. Jebb, and P. Aveyard. 2014. Effect of behavioral techniques and delivery mode on effectiveness of weight management: Systematic review, meta-analysis and meta-regression. Obesity Reviews 15 (7):598–609. doi: 10.1111/obr.12165.
- Higgins, J. P., and S. G. Thompson. 2002. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 21 (11):1539–58. doi: 10.1002/sim.1186.
- Higgins, J. P. T., and S. Green. 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 current 5 March 2011. www.handbook.cochrane.org (accessed 1 May 2017).
- Hill, B., H. Skouteris, and M. Fuller-Tyszkiewicz. 2013. Interventions designed to limit gestational weight gain: A systematic review of theory and meta-analysis of intervention components. Obesity Reviews 14 (6):435–50. doi: 10.1111/obr.12022.
- Hollywood, L., D. Surgenor, M. Reicks, L. McGowan, F. Lavelle, M. Spence, M. Raats, A. McCloat, E. Mooney, and M. Caraher. 2017. Critical review of behavior change techniques applied in intervention studies to improve cooking skills and food skills among adults. Critical Reviews in Food Science and Nutrition 58 (17):2882–95.
- Kassebaum, N. J., E. Bernabé, M. Dahiya, B. Bhandari, C. J. Murray, and W. Marcenes. 2014. Global burden of severe tooth loss: A systematic review and meta-analysis. Journal of Dental Research 93 (7 Suppl):20S–8S. doi: 10.1177/0022034514537828.
- Kaushik, K., P. Dhawan, P. Tandan, and M. Jain. 2018. Oral health-related quality of life among patients after complete denture rehabilitation: A 12-month follow-up study. International Journal of Applied and Basic Medical Research 8 (3):169. doi: 10.4103/ijabmr.IJABMR_171_18.
- Kazemi, S., G. Savabi, S. Khazaei, O. Savabi, A. Esmaillzadeh, A. H. Keshteli, and P. Adibi. 2011. Association between food intake and oral health in elderly: SEPAHAN systematic review. Journal of Dental Research 8 (Suppl 1):S15–S20.
- Krall, E., C. Hayes, and R. Garcia. 1998. How dentition status and masticatory function affect nutrient intake. Journal of the American Dental Association (1939) 129 (9):1261.
- Lara, J., E. H. Evans, N. O’Brien, P. J. Moynihan, T. D. Meyer, A. J. Adamson, L. Errington, F. F. Sniehotta, M. White, and J. C. Mathers. 2014. Association of behavior change techniques with effectiveness of dietary interventions among adults of retirement age: A systematic review and meta-analysis of randomized controlled trials. BMC Medicine 2:177.
- Lichtenstein, A. H., H. Rasmussen, W. W. Yu, S. R. Epstein, and R. M. Russell. 2008. Modified MyPyramid for older adults. The Journal of Nutrition 138 (1):5–11. doi: 10.1093/jn/138.1.5.
- Lopez, R., P. C. Smith, G. Göstemeyer, and F. Schwendicke. 2017. Ageing, dental caries and periodontal diseases. Journal of Clinical Periodontology 44:145–52.
- Luszczynska, A., K. Horodyska, K. Zarychta, N. Liszewska, N. Knoll, and U. Scholz. 2016. Planning and self-efficacy interventions encouraging replacing energy-dense foods intake with fruit and vegetable: A longitudinal experimental study. Psychology & Health 31 (1):40–64. doi: 10.1080/08870446.2015.1070156.
- Marcenes, W., J. G. Steele, A. Sheiham, and A. W. Walls. 2003. The relationship between dental status, food selection, nutrient intake, nutritional status, and body mass index in older people. Cadernos de Saúde Pública 19 (3):809–16. doi: 10.1590/S0102-311X2003000300013.
- Martin, J., A. Chater, and F. Lorencatto. 2013. Effective behaviour change techniques in the prevention and management of childhood obesity. International Journal of Obesity (2005) 37 (10):1287–94. doi: 10.1038/ijo.2013.107.
- Michie, S., M. Johnston, J. Francis, W. Hardeman, and M. Eccles. 2008. From theory to intervention: Mapping theoretically derived behavioral determinants to behavior change techniques. Applied Psychology 57 (4):660–80. doi: 10.1111/j.1464-0597.2008.00341.x.
- Michie, S., M. Richardson, M. Johnston, C. Abraham, J. Francis, W. Hardeman, M. P. Eccles, J. Cane, and C. E. Wood. 2013. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine 46 (1):81–95. doi: 10.1007/s12160-013-9486-6.
- Moher, D., A. Liberati, J. Tetzlaff, D. G. Altman, and PRISMA Group. 2009. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine 6 (7):e1000097. doi: 10.1371/journal.pmed.1000097.
- Morris, M. C., C. C. Tangney, Y. Wang, F. M. Sacks, D. A. Bennett, and N. T. Aggarwal. 2015. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s Dementia 11 (9):1007–14. doi: 10.1016/j.jalz.2014.11.009.
- Moynihan, P., T. J. Butler, J. M. Thomason, and N. J. A. Jepson. 2000. Nutrient intake in partially dentate patients: The effect of prosthetic rehabilitation. Journal of Dentistry 28 (8):557–63. doi: 10.1016/S0300-5712(00)00044-0.
- Moynihan, P. J., A. Elfeky, J. S. Ellis, C. J. Seal, R. M. Hyland, and J. M. Thomason. 2012. Do implant-supported dentures facilitate efficacy of eating more healthily? Journal of Dentistry 40 (10):843. doi: 10.1016/j.jdent.2012.07.001.
- Muller, K., J. Morais, and J. Feine. 2008. Nutritional and anthropometric analysis of edentulous patients wearing implant overdentures or conventional dentures. Brazilian Dental Journal 19 (2):145–50.
- Nabeshima, G., K. Fueki, Y. Inamochi, and N. Wakabayashi. 2018. Effect of dietary counselling with prosthetic restoration on fruit and vegetable intake in partially dentate patients: A prospective study. Journal of Oral Rehabilitation 45 (8):618–26. doi: 10.1111/joor.12647.
- National Institute of Dental and Craniofacial Research. 2018. Dental caries (tooth decay) in seniors (age 65 and over). Version July 2018. https://www.nidcr.nih.gov/research/data-statistics/dental-caries/seniors (accessed 10 May 2019).
- NHS Digital. 2011. Adult Dental Health Survey 2009 – Summary report and thematic series, 2011. Version 24 March 2011. https://digital.nhs.uk/data-and-information/publications/statistical/adult-dental-health-survey/adult-dental-health-survey-2009-summary-report-and-thematic-series (accessed 26 May 2019).
- Olander, E., H. Fletcher, S. Williams, L. Atkinson, A. Turner, and D. French. 2013. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behavior: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity 10 (1):29. doi: 10.1186/1479-5868-10-29.
- Olivier, M., D. Laurin, J. M. Brodeur, M. Boivin, N. Leduc, M. Lévy, and R. H. Taché. 1995. Prosthetic relining and dietary counselling in elderly women. Journal of the Canadian Dental Association 6:882–6.
- Prakash, N., N. Kalavathy, J. Sridevi, and K. Premnath. 2012. Nutritional status assessment in complete denture wearers. Gerodontology 29 (3):224–30. doi: 10.1111/j.1741-2358.2011.00620.x.
- Prochaska, J. O., C. C. DiClemente, and J. C. Norcross. 1992. In search of how people change. Applications to addictive behaviors. American Psychologist 47 (9):1102–14.
- Reynolds, A., J. Mann, J. Cummings, N. Winter, E. Mete, and L. Te Morenga. 2019. Carbohydrate quality and human health: A series of systematic reviews and meta-analyses. Lancet (London, England) 393 (10170):434–45. doi: 10.1016/S0140-6736(18)31809-9.
- Scientific Advisory Committee on Nutrition. 2011. Dietary Reference Values for Energy Scientific Advisory Committee on Nutrition 2011. Version current 1 November 2011. https://www.gov.uk/government/publications/sacn-dietary-reference-values-for-energy (accessed 9 March 2019).
- Slade, G. D., A. A. Akinkugbe, and A. E. Sanders. 2014. Projections of U.S. Edentulism prevalence following 5 decades of decline. Journal of Dental Research 93 (10):959–65. doi: 10.1177/0022034514546165.
- Sterne, J. A., M. A. Hernán, B. C. Reeves, J. Savović, N. D. Berkman, M. Viswanathan, D. Henry, D. G. Altman, M. T. Ansari, I. Boutron, et al. 2016. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical Research ed.) 355:i4919. doi: 10.1136/bmj.i4919.
- Suzuki, H., M. Kanazawa, Y. Komagamine, M. Iwaki, A. Jo, N. Amagai, and S. Minakuchi. 2017. The effect of new complete denture fabrication and simplified dietary advice on nutrient intake and masticatory function of edentulous elderly: A randomized-controlled trial. Clinical Nutrition 37 (5):1441–1447.
- Toniazzo, M. P., P. de Sant'Ana Amorim, F. W. M. G. Muniz, and P. Weidlich. 2018. Relationship of nutritional status and oral health in elderly: Systematic review with meta-analysis. Clinical Nutrition 37 (3):824–30. doi: 10.1016/j.clnu.2017.03.014.
- Tyrovolas, S., A. Koyanagi, D. B. Panagiotakos, J. M. Haro, N. J. Kassebaum, V. Chrepa, and G. A. Kotsakis. 2016. Population prevalence of edentulism and its association with depression and self-rated health. Scientific Reports 6:37083.
- United States Department of Agriculture. 2018. Older adults choose MyPlate. Version 17 July 2018. https://www.choosemyplate.gov/older-adults (accessed 26 May 2019).
- Wang, X., Y. Ouyang, J. Liu, M. Zhu, G. Zhao, W. Bao, and F. B. Hu. 2014. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 349:g4490. doi: 10.1136/bmj.g4490.
- Watson, S., C. Cardwell, L. McGowan, L. McCrum, B. McGuiness, C. Moore, J. V. Woodside, and G. McKenna. 2019. The impact of dental status on perceived ability to eat certain foods, nutrient intake and nutritional status in older adults: UK National Diet and Nutrition Survey 2008–2014. International Journal of Behavioral Nutrition and Physical Activity 16 (1):43.
- Weinstein, N. O. 1980. Unrealistic optimism about future life events. Journal of Personality and Social Psychology 39 (5):806–20. doi: 10.1037/0022-3514.39.5.806.
- World Health Organization (WHO). 2018. Ageing and health. Version current 5 February 2018. http://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed 5 July 2018).
- Wöstmann, B., T. Simon, M. Neuhäuser-Berthold, and P. Rehmann. 2016. Pilot study on the influence of nutritional counselling and implant therapy on the nutritional status in dentally compromised patients. PLoS One 11 (1):e0147193. doi: 10.1371/journal.pone.0147193.
- Zani, S. R., E. G. Rivaldo, L. C. Frasca, and L. F. Caye. 2009. Oral health impact profile and prosthetic condition in edentulous patients rehabilitated with implant-supported overdentures and fixed prostheses. Journal of Oral Science 51 (4):535–43.