Abstract
The associations between circulating vitamin D concentrations and total and site-specific colorectal cancer (CRC) incidence have been examined in several epidemiological studies with overall inconclusive findings. The aim of this systematic review and meta-analysis of both case-control and prospective cohort studies was to evaluate the association between CRC and circulating levels of vitamin D. The main exposure and outcome were circulating total 25(OH)D and CRC, respectively, in the overall population (i.e., all subjects). Two reviewers, working independently, screened all the literature available to identify studies that met the inclusion criteria (e.g., case-control or prospective cohort studies, published in English, and excluding non-original papers). Data were pooled by the generic inverse variance method using a random or fixed effect model, as approriate. Heterogeneity was identified using the Cochran's Q-test and quantified by the I2 statistic. Results were stratified by study design, sex, and metabolite of vitamin D. Sensitivity and subgroup analyses were also performed. A total of 28 original studies were included for the quantitative meta-analysis. Meta-analyses comparing the highest vs lowest categories, showed a 39% lower risk between levels of total 25(OH)D and CRC risk (OR (95% CI): 0.61 (0.52; 0.71); 11 studies) in case-control studies; whereas a 20% reduced CRC risk in prospective cohort studies (HR (95% CI): 0.80 (0.66; 0.97); 6 studies). Results in women mirrored main results, whereas results in men were non-significant in both analyses. Our findings support an inverse association between circulating vitamin D levels and CRC risk.
Introduction
Colorectal cancer (CRC) is considered the third most common cancer diagnosis and second deadliest malignancy for both sexes combined (Siegel et al. Citation2020). Environmental and genetic risk factors for CRC include aging, family history of CRC, medical history of benign adenomatous polyps and inflammatory bowel diseases, obesity, diabetes, lack of physical exercise, as well as diet (Dekker et al. Citation2019). Since the first prospective study published by Garland et al. in 1989, showing a significant protective role of serum 25-hydroxyvitamin D [25(OH)D] on colon cancer, many studies have been conducted in human and animal models to explore this association (C. Garland, et al. Citation1989). Indeed, this first analysis was motivated by the circumstance that the areas of the world receiving the least amounts of light, were also the areas with the highest death rates by colon cancer (Garland and Garland Citation1980).
Vitamin D is a fat-soluble vitamin that can be synthesized in the skin through energy of sunlight or can be obtained from the diet or supplements. The 25(OH)D - the major circulating form of vitamin D - is a pre-hormone that is produced in the liver by hydroxylation of both isoforms, which in turn, comes from diet, supplements, or its production by the skin. In clinical practice, the measurement of 25(OH)D as a blood test is considered the best indicator of vitamin D status for different outcomes, including the risk of cancer. However, the active form for vitamin D is 1,25(OH)2D3 (calcitriol). Although there are some discrepancies on adequate serum levels of vitamin D for health outcomes, a recent study indicates that the recommended serum 25(OH)D for the prevention of CRC must exceed 30 ng/mL, and the best values were situated at levels between 36 and 40 ng/mL (Bischoff-Ferrari et al. Citation2006).
Overall, calcitriol – the biologically active form of vitamin D - exerts its biological effects by binding to the nuclear vitamin D receptor (VDR) and further regulating gene expression in many targets. However, the response of cancer cells to calcitriol not only depends on VDR expression, but also on the intracellular concentrations of calcitriol as well. Thus, mostly coming from in vitro studies, it has been shown that vitamin D may act on CRC by its action on proliferation, differentiation, apoptosis, angiogenesis, immune modulation, and/or epigenetic regulation (reviewed in (Dou et al. Citation2016)). These results suggest that vitamin D may play a chemopreventive role in colorectal malignant transformation and/or progression to CRC. However, results coming from different meta-analyses of epidemiological studies have reported either significant inverse associations or non-significant associations in populations worldwide (Huang et al. Citation2020; Lee et al. Citation2011; Ma et al. Citation2011). Even there have been considerable controversies about the association between vitamin D levels and CRC, the novelty of our meta-analysis suits best for an update of the literature, limited in CRC incidence - but not in adenoma incidence - and a robust systematic analysis. Likewise, these previous analyses have not simultaneously considered: i) the design of the studies; ii) sex differences; iii) CRC subsite (i.e., colon or rectal); iv) different metabolites of vitamin D (i.e., 25(OH)D, 1,25(OH)2D); among others.
Based on the previous inconclusive evidence reported by epidemiologic studies, our objective was to systematically review the literature and perform a meta-analysis of both case-control and prospective cohort studies evaluating the association between CRC and circulating levels of vitamin D. This article provides a complete and updated state of the art about vitamin D levels and CRC risk, while considers putative differences coming from sex, specific-site CRC, metabolites, and status of vitamin D (i.e., free, bioavailable or total 25(OH)D, and 1,25(OH)2D), and study designs.
Methods
Search strategy and study selection
For the present systematic review and meta-analysis, we followed the methodological guidelines of the Cochrane Handbook for Systematic Reviews of interventions (J. P. Higgins and Green Citation2019) and the results were reported according to Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al. Citation2000). The present study and the corresponding search protocol have been registered in the PROSPERO registry (http://www.crd.york.ac.uk/PROSPERO) as CRD42020207186.
We conducted a comprehensive electronic systematic search in two databases (Medline through PUBMED and Cochrane Library) until 24th August 2020, combining different MeSH terms and key words. PubMed search was conducted using R packages “pubmed.mineR” and “RISmed”. depicts detailed search strategy. Additionally, a manual review of the reference list from the retrieved articles was conducted to ensure that all relevant studies conducted in the field were identified.
Table 1. Characteristics of case-control studies included in the systematic review and meta-analysis.
In the first step, duplicate studies from the identified articles through the search strategy were discarded. In a second step, two independent reviewers (HB and SC) performed an initial screening of the titles and abstracts of the retrieved papers against the eligibility criteria. For that purpose, the Abstrackr (http://abstrackr.cebm.brown.edu/) online screening program was used. Their selection was supervised by PH-A and NB-T.
Eligible studies were those case-control or with prospective cohort design with at least 1-year of follow-up, conducted in adults (≥ 18 years old), and reporting the risk estimates as odd ratios (OR) or hazard ratios (HR) and their corresponding 95% confidence interval (CI) for the association between circulating vitamin D levels - including 25(OH)D and 1,25(OH)D - and the risk of CRC, colon cancer and/or rectal cancer. If more than one paper from the same study were found, both were included when different outcomes were reported (i.e., CRC in one and CC in the other one). However, if the same outcome was reported in different studies (Feskanich et al. Citation2004; Hiraki et al. Citation2014; Lee et al. Citation2011; M. Song et al. 2014, Citation2016; Wu et al. Citation2007, Citation2011), the one with the larger sample size and/or reporting non-merged cohort analyses was selected for the meta-analysis (Feskanich et al. Citation2004; Hiraki et al. Citation2014; Lee et al. Citation2011; M. Song et al. Citation2016; Wu et al. Citation2007). We did not consider for inclusion published abstracts or proceedings. Information available was sufficient to perform the analyses, therefore, we did not need to contact author for asking for extra information.
Data extraction
To verify that the articles that passed the previous process met the eligibility criteria, two independent researchers (HB and SC) reviewed the full text. In addition, they also extracted relevant information for the systematic review and meta-analysis of each of the studies using a standardized spreadsheet proforma. Collected data included authors, journal and year of publication, title of the article, study name, participant characteristics, sample size, follow-up (only for cohort studies), type of exposure, methodology for vitamin D assessment, type of outcome and assessment method, number of cases, statistical analyses, and multivariable-adjusted effect estimates (OR or HR, and 95% CI) for the association of interest. Disagreements between researchers were solved by consensus or consulting a third researcher (PH-A).
Quality assessment of the included studies
Two different tools were used to assess the quality of the included studies. For case-control studies, we used The Study Quality Assessment of Case-Control Studies from the National Heart, Lung, and Blood Institute (NHLBI Citation2014). It consists of 12 questions that help the researcher to rate the studies as good, fair or poor based on details that are reported. Poor quality is translated to high risk of bias, and good quality as low risk of bias.
For prospective cohort studies we used the Newcastle-Ottawa Scale (Wells et al. Citation2000). This is a rating scale ranging from 0 to 9 points that are given to the studies based on 3 domains. A maximum of 4, 3 and 2 points are given after evaluating the population selection, outcome assessment and comparability domains, respectively. Studies with a total punctuation of at least 7 points were considered as high quality. Any disagreement between researchers (HB and SC) was solved by consensus or consulting a third researcher (PH-A). A priori subgroup analysis for case-control and prospective cohort studies included: sex, obese status, assessment method of circulating vitamin D levels, and geographical data. In addition, a priori subgroup analysis for prospective studies included: follow-up duration (median) and individual domains of risk of bias (selection, outcome and comparability). Applicable subgroup analyses were reported in the Results’ section.
Circulating vitamin d and colorectal cancer outcomes
In this meta-analysis, we have considered as exposure circulating (i.e., plasma, serum, whole blood) levels of vitamin D, either total 25(OH)D or total 1,25(OH)2D metabolites. Moreover, in case of 25(OH)D, we have also collected data regarding free or bioavailable 25(OH)D.
Importantly, we considered the outcomes: CRC and its subsites (i.e., colon cancer and rectal cancer). However, the main exposure and outcome were circulating total 25(OH)D and CRC, respectively, in the overall population (i.e., all subjects). Results from the same study were included in the meta-analysis when data was reported by non-overlapping subjects (i.e., men and women to create all subjects). However, independent meta-analyses were performed for studies comprising only men, only women, or including both as it has been shown that CRC - and its subsites - risk is sex-dependent (Keum and Giovannucci Citation2019).
Statistical analyses
We conducted all the analyses using R version 3.6.3 software including packages “meta” (v. 4.11) and “dmetar” (v. 0.0.9). The natural log-transformed ORs, HRs, and 95% CI comparing highest versus lowest categories of circulating levels of vitamin D were pooled using the generic inverse variance method with fixed-effects model (when less than 5 study comparisons were available) or random-effects model (when at least 5 or more study comparisons were available). The results were reported back in the original scale. Studies using continuous risk per dose were excluded from the analyses, but we described their results within the text. Moreover, studies with other type of comparisons (e.g., bottom versus top; or middle versus top) were re-calculated (Acikgoz, Cimrin, and Ergor Citation2020; C. Garland, et al. Citation1989; Jenab et al. Citation2010; McCullough, et al. Citation2019; Neuhouser et al. Citation2012; José M. Ordóñez-Mena et al. Citation2016; Weinstein et al. Citation2011; Wong et al. Citation2014) in a highest versus lowest fashion using Jan Hamling et al. methodology (Hamling et al. Citation2008). We conducted separated meta-analyses for case-control and prospective cohort studies.
For all meta-analyses, the Cochran Q statistic was used to estimate inter-study heterogeneity and it was quantified by the I2 statistic. We considered substantial heterogeneity when I2 was ≥50% and Pheterogeneity < 0.10. We additionally reported the tau2 as the estimate of the between-study variance in random-effects meta-analyses.
Sensitivity analyses were conducted when more than 4 study comparisons (from independent studies) were available in the analyses by the removal of one study at a time (i.e., leave-one out approach) from the meta-analyses and recalculating the summary estimates and heterogeneity values. We considered an influential study that one that changed the evidence of heterogeneity or the magnitude by more than 20%, the significance and/or direction of the association. Moreover, the detection of outliers (i.e., study’s original confidence interval does not overlap with the confidence interval of the pooled effect) was also performed. Finally, a graphic display of heterogeneity (GOSH) plot was performed to test all the possible study combinations within a meta-analysis (2n − 1 individual analyses, where “n” is the number of studies) and then plot the pooled effect size on the x-axis and the between-study heterogeneity at the y-axis.
We performed a posteriori subgroup analyses by the method and sample used to determine vitamin D levels in each study, when at least two studies were available within each stratum.
Publication bias – by means of a funnel plot to visually assess small study effects – is only possible to be tested when 10 or more study comparisons are included in a meta-analysis (J. Higgins and Green Citation2015), thus we include it only for the meta-analysis of case-control studies assessing circulating vitamin D levels and CRC risk in all the subjects.
Results
Study characteristics
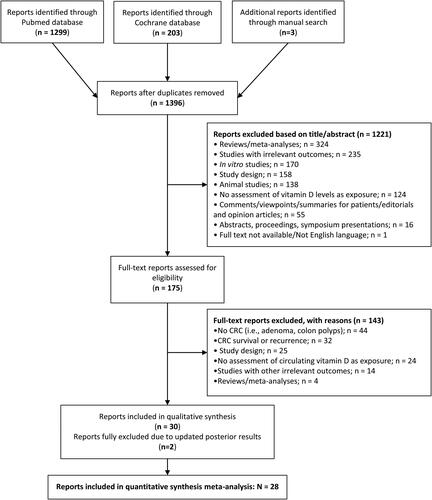
A primary search of MEDLINE-PubMed and Cochrane databases, together with manual search, retrieved a total of 1396 articles () after duplicates were removed. An 87.5% (n = 1221) were excluded based on its title and abstract information according to the eligibility criteria. Therefore, 175 articles were collected as full texts and were further assessed for inclusion. A total of 32 articles were included in the qualitative synthesis, whereas 28 were included in quantitative synthesis meta-analysis ().
Information regarding each study is included in and . This meta-analysis included 23 case-control studies and 10 prospective studies, representing a total of 140,112 subjects from different countries around the world: half of the included studies were from USA, one third from European countries (i.e., Finland, Denmark, or Germany), c.a. 7% from Australia, c.a. 7% from Japan, and one study from Jordan, Turkey and, China ( and ). The duration of the follow-up in the prospective cohort studies ranged from 4 to 20 years. Most of the studies assessed circulating vitamin D through chemiluminescent immunoassay (CLIA)/enzyme immunoassay (EIA) (28%), radioimmunoassay (RIA) (23%) or liquid chromatography (15%). Some studies stratified the analysis by sex. Therefore, we considered these results separately in each corresponding meta-analysis.
Table 2. Characteristics of prospective cohort studies included in the systematic review and meta-analysis.
In which regards the quality of the studies, most case-control studies were evaluated as “Good” (87%), whereas only 3 studies as “Fair” (13%). All the prospective studies except two (Ananthakrishnan et al. Citation2014; C. Garland, et al. Citation1989) which scored less than 7 (i.e., “low quality”) were qualified a mark at least “7/9” (i.e., “high quality”). Estimate risks from two prospective cohort studies (Ananthakrishnan et al. Citation2014; Vojdeman et al. Citation2019) were only reported on a continuous scale, instead of categories of circulating vitamin D (i.e., highest versus lowest) and were not included in the meta-analysis. Of note, participants in the included studies were overall classified in the highest category when 25(OH)D values were higher than 25-30 ng/ml (50-75 nM), whereas in the lowest category when values were below 15-20 ng/ml. These distribution of 25(OH)D levels were in accordance with the current 25(OH)D recommendations (Pludowski et al. Citation2018) and showed more variability restricted to the lowest category.
Meta-analyses of case-control and prospective studies
Colorectal cancer
We collected results from case-control studies (15.542 cases and 22.376 controls) assessing the risk of CRC by circulating levels of vitamin D (), which included data from total, bioavailable and free 25(OH)D (in all subjects and women only) and data considering 1,25(OH)2D (in men and women) in all subjects, men and women ().Regarding prospective cohort studies, a total of 1,402 incident cases of CRC were analyzed from 68,710 total population, as showed in . We only had data from 25(OH)D in all subjects, and for both men and women ().
Figure 2. Super plot of case-control and prospective cohort studies assessing the association between circulating vitamin D levels (highest versus lowest categories) and the risk of colorectal cancer (CRC). A. Case-control studies for CRC risk; B. Prospective studies for CRC risk. Meta-analyses were constructed using generic inverse-variance fixed-effects model (for meta-analysis with less than 5 studies) or random-effects model (for meta-analysis with 5 or more studies). Abbreviations: Bio, bioavailable; CI, confidence interval; HR, hazard ratio; NA, not applicable; OR, odds ratio.
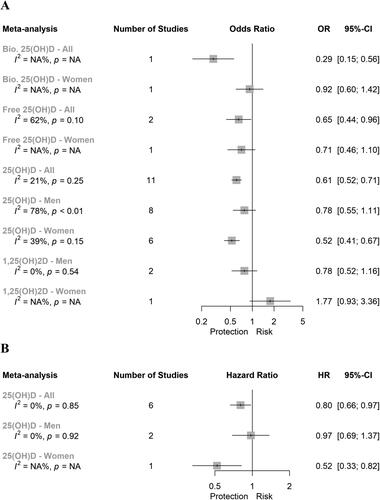
Bioavailable 25(OH)D and colorectal cancer
Only one case-control study has analyzed the association between bioavailable 25(OH)D in all subjects and CRC. Therefore, we could not perform a meta-analysis. The results of this study showed a 71% lower risk of CRC when comparing highest versus lowest categories of bioavailable 25(OH)D ((OR (95% CI): 0.29 (0.15; 0.56); ). Similarly, only one case-control study conducted in women was identified, which showed a non-significant association between bioavailable 25(OH)D and CRC ((OR (95% CI): 0.92 (0.60; 1.42); ). The search strategy did not identify any case-control study evaluating this association only in men.
Free 25(OH)D and colorectal cancer
The meta-analysis of two case-control studies evaluating the association between free 25(OH)D and CRC showed a 35% lower risk when considering all the subjects ((OR (95% CI): 0.65 (0.44; 0.96); and Supplementary Figure 1.A). We identified substantial heterogeneity for the meta-analysis of case-control studies evaluating the association between free 25(OH)D and CRC in all subjects (I2 = 62%; P = 0.10; ). In relation to women, only one case-control study has been published to date evaluating this association. The results showed a non-significant association between free 25(OH)D and CRC (). None-study has been published evaluating this association only in men.
Total 25(OH)D and colorectal cancer
Results from the meta-analysis of eleven case-control studies conducted in all subjects showed a significant 39% lower risk between levels of total 25(OH)D and CRC risk (OR (95% CI): 0.61 (0.52; 0.71)) when comparing extreme categories. shows the specific forest plot for that meta-analysis. When we analyzed the association between 25(OH)D and CRC risk stratified by sex, a significant 48% lower risk between levels of total 25(OH)D and CRC risk were observed in case of women (0.52 (0.41; 0.67); based on 6 studies; forest plot in Supplementary Figure 1.B), but not in men (0.78 (0.55; 1.11); based on 8 studies; forest plot in Supplementary Figure 1.C). We identified substantial heterogeneity for the meta-analysis of case-control studies evaluating the association between 25(OH)D and CRC considering only men (I2= 78%; P < 0.01; ).
Figure 3. Forest plot for the association between circulating vitamin D levels (25(OH)D; highest versus lowest categories) and risk of colorectal cancer including all subjects. Both meta-analyses were constructed using generic inverse-variance random-effects model for: A) case-control studies; B) prospective cohort studies. Abbreviations: CI, confidence interval; HR, hazard ratio; NA, not applicable; OR, odds ratio.
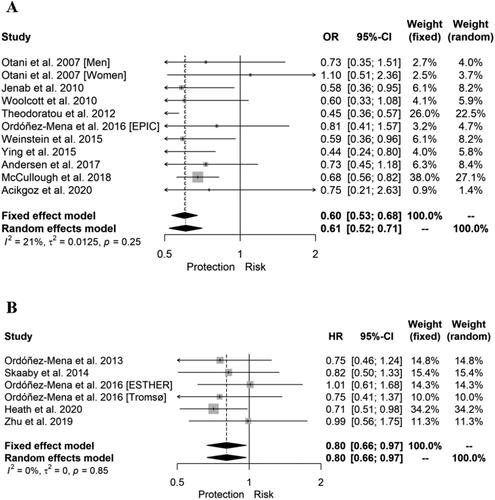
Results coming from prospective cohort studies are scarce. The levels of 25(OH)D were significantly associated with a 20% lower risk of CRC in the meta-analysis of six studies including all the subjects (HR (95% CI): 0.80 (0.66; 0.97); and ) and with a 48% lower risk in the unique study reported specifically in women (0.52 (0.33; 0.82); ), whereas non-significant association was reported in men based on two studies (0.97 (0.69; 1.37); and Supplementary Figure 1.D)
1,25(OH)2D and colorectal cancer
No study reported the association between 1,25(OH)2D and CRC in all subjects (i.e., irrespective of sex). A non-significant inverse association between 1,25(OH)2D and CRC was observed in the meta-analysis of two case-control studies considering only men ((OR (95% CI): 0.78 (0.52; 1.16); and Supplementary Figure 1.E). We could not perform a meta-analysis considering only women since a single study was identified, showing a non-significant association between 1,25(OH)2D and CRC ().
Colon cancer
In , we represent the results of case-control studies assessing the association between circulating vitamin D (25(OH)D and 1,25(OH)2D) and colon cancer. A total of 3,102 cases of colon cancer and c.a. 4,831 controls were analyzed as showed in . Regarding prospective studies, a total of 1.218 incident cases were analyzed out of the 222.056 total population, as showed in . No studies were identified analyzing the association between bioavailable neither free 25(OH)D and colon cancer comparing extreme categories. However, Andersen et al. 2017 reported in a case-control study a significant 37% lower risk of colon cancer per 1-SD increase in free 25(OH)D levels (OR (95%CI): 0.63 (0.44; 0.89) in all subjects (Andersen et al. 2017).
Figure 4. Super plot of case-control and prospective cohort studies assessing the association between circulating vitamin D levels (highest versus lowest categories) and the risk of colon cancer. A. Case-control studies for CC risk; B. Prospective studies for CC risk. Meta-analyses were constructed using generic inverse-variance fixed-effects model (for meta-analysis with less than 5 studies) or random-effects model (for meta-analysis with 5 or more studies). Abbreviations: CI, confidence interval; HR, hazard ratio; NA, not applicable; OR, odds ratio; vit, vitamin.
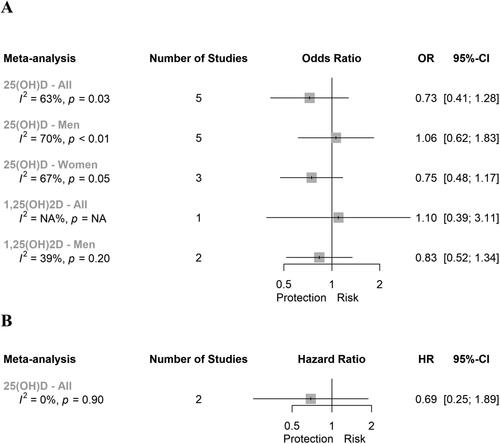
25(OH)D and Colon cancer
We reported a non-significant inverse association between levels of 25(OH)D and colon cancer in all subjects (based on 5 studies), and men (based on 5 studies) and women (based on 3 studies) separately (, and Supplementary Figures 2.A, 2.B and 2.C, respectively). This same result was observed in the meta-analysis of two prospective cohort studies conducted in all subjects ((HR (95% CI): 0.69 (0.25; 1.89); and Supplementary Figure 2.D). We reported substantial heterogeneity in the meta-analyses of all subjects (I2 = 63%; P = 0.03), men (I2 = 70%; P < 0.01) and women (I2 = 67%; P = 0.05). In a continuous scale, Vojdeman et al. Citation2019 reported the prospective associations between colon cancer and circulating 25(OH)D levels (per 1 nM increase) in all subjects, showing non-significant borderline inverse associations (HR (95% CI): 0.98 (0.96; 1.00)) (Vojdeman et al. Citation2019). Moreover, Ananthakrishnan et al. Citation2014, found in subjects with inflammatory bowel disease, a significant 6% lower risk of colon cancer by per 1ng/mL increase in 25(OH)D in all subjects (HR (95% CI): 0.94 (0.91; 0.97)) (Ananthakrishnan et al. Citation2014).
1,25(OH)2D and Colon cancer
A non-significant association was observed between 1,25(OH)2D and colon cancer in both the unique study assessing it in all subjects and in the meta-analysis of two studies conducted in men ( for both, and Supplementary Figure 2.E for men).
Rectal cancer
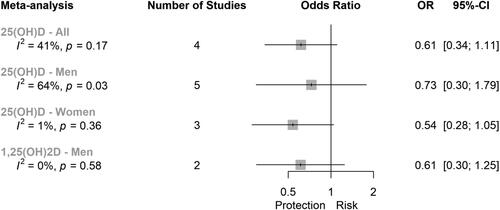
A total of 1.158 cases of rectal cancer and c.a. 2,130 controls were analyzed as showed in . depicts the forest plot for the meta-analyses of case-control studies evaluating the association between 25(OH)D and rectal cancer conducted in all subjects, men and women, as well as the meta-analysis evaluating the association between 1,25(OH)D and rectal cancer in men. Moreover, Andersen et al. 2017 reported in a case-control study a non-significant inverse association (per 1-SD increase) between free 25(OH)D levels and rectal cancer in all subjects (Andersen et al. 2017).
25(OH)D and rectal cancer
We did not report a significant association between 25(OH)D and rectal cancer when comparing extreme categories in the meta-analysis considering all subjects ( and Supplementary Figure 3.A, based on 4 studies), nor in the meta-analyses considering only men ( and Supplementary Figure 3.B, based on 5 studies) neither women ( and Supplementary Figure 3.C, based on 3 studies). Interestingly, we reported substantial heterogeneity for the meta-analysis of 25(OH)D considering only men (I2 = 64%; P = 0.03; ). In a continuous scale, Vojdeman et al. Citation2019 reported the prospective associations between circulating 25(OH)D levels and rectal cancer in 461 cases out of 217,244 total subjects, showing non-significant inverse associations (Vojdeman et al. Citation2019).
1,25(OH)2D and rectal cancer
Two case-control studies conducted only in men have been published so far evaluating the association between 1,25(OH)D and rectal cancer. Pooled analysis showed a non-significant inverse association between 1,25(OH)D and rectal cancer when comparing extreme categories ( and Supplementary Figure 3.D).
Meta-analyses heterogeneity and publication bias
Publication bias
The best way to visualize whether small studies with small effect sizes are missing is through funnel plots. Supplementary Figure 4 shows the funnel plot for the meta-analysis of case-control studies assessing the association between 25(OH)D and CRC in all the subjects. We did not detect evidence of publication bias by visual inspection of the funnel plot neither with the Egger’s test (P = 0.385). Because of the reduced number of studies (less than 10), we could not assess publication bias for the other meta-analyses.
Sensitivity analyses
We conducted a sensitivity analysis removing one study at a time in those meta-analyses with more than four independent studies included, in order to assess whether the results could have been substantially affected by a single study.
Importantly, in which regards the influence analyses, we reported influential studies – by means of different reasons as detailed in Methods section - in the meta-analyses of case-control studies between circulating 25(OH)D levels and CRC, CC and RC risk in men, together with in the case-control studies between circulating 25(OH)D levels and CRC risk in women. Interestingly, after removal of Anic et al. Citation2014 in the meta-analysis of case-control studies assessing the risk of CRC by 25(OH)D in men, the association became significant (OR (95% CI): 0.69 (0.51; 0.93)) unless the heterogeneity remained significant ().
Moreover, in the analyses of outliers, only in the meta-analysis of case-control studies assessing the risk of CRC by 25(OH)D in men, we found one outlier: Theodoratou et al. (Citation2012). Removal of Theodoratou et al. Citation2012 did not modify the non-significant association nor the high heterogeneity ().
In the meta-analysis of case-control studies assessing the risk of CRC by 25(OH)D in all subjects, we found that the removal of any of the studies did not significantly modify the OR nor the null heterogeneity reported. This pattern was also exhibited in the GOSH plot (Supplementary Figure 5.A), where all the iterations reported a pooled OR toward an inverse association and null heterogeneity among studies. However, GOSH plot in Supplementary Figure 5.B shows the dispersion of pooled OR with two clouds of results toward high heterogeneity and differential pooled ORs in case of the association between 25(OH)D in men and CRC. In fact, when we performed the GOSH plot (Supplementary Figure 6) excluding each of the influence studies, we observed that the pooled ORs were increased (blue versus red) when omitting Theodoratou et al. Citation2012 (Supplementary Figure 6.A), whereas are decreased (blue versus red) in case of omitting Anic et al. Citation2014 (Supplementary Figure 6.B), in both cases with a high heterogeneity.
Figure 5. Super plot of case-control studies assessing the association between circulating vitamin D levels (highest versus lowest categories) and the risk of rectal cancer. Meta-analyses were constructed using generic inverse-variance fixed-effects model (for meta-analysis with less than 5 studies) or random-effects model (for meta-analysis with 5 or more studies). Abbreviations: CI, confidence interval; HR, hazard ratio; NA, not applicable; OR, odds ratio; vit, vitamin.
In case of the meta-analysis with the same exposure and outcome but conducted in women, we found that the removal of any study did not modify the significant inverse association between 25(OH)D and CRC, but in some cases, it slightly modified the heterogeneity. This scenario was mirrored in the GOSH plot (Supplementary Figure 5.C).
In which regards the meta-analysis assessing the risk of colon cancer by 25(OH)D levels in men, the removal of Weinstein et al. (Citation2011) or Wu et al. (Citation2007) reduced the heterogeneity, but the association remained non-significant. A same trend happened in the meta-analysis assessing rectal cancer by levels of 25(OH)D in men, as the removal of any study did not modify the non-significant association neither the high heterogeneity. The GOSH plots for both meta-analyses showed this pattern (Supplementary Figure 5.D and E).
Finally, in the meta-analysis of prospective studies assessing the risk of CRC by 25(OH)D levels in all subjects, we found that the exclusion of Ordóñez-Mena et al. (Citation2013) or Heath et al. (Citation2020) made the inverse association non-significant, with a null impact on heterogeneity. In the GOSH plot we may observe that this null heterogeneity was reported with a gradient of pooled HRs toward inverse associations between 25(OH)D levels and CRC (Supplementary Figure 5.F).
Subgroup analyses by methodological procedure and sample source
Subgroup analyses by methodology and source of vitamin D were performed (Supplementary Table 3). We found no relevant change in ORs nor heterogeneity in the subgroup analysis by method nor sample source in case of case-control studies assessing CRC risk by circulating vitamin D in all subjects. In case of the same exposure and outcome in men, we reported a null heterogeneity and significant inverse association in case of RISA method (OR (95% CI): 0.67 (0.47; 0.95), I2=0%), but same non-significant association remained in CLIA method. The OR only considering plasma show a significant inverse association with reduced non-significant heterogeneity (OR (95% CI): 0.56 (0.41; 0.77), I2=42.2%), whereas no relevant change was found in serum. In case of women, subgroup analyses mirrored main results. Subgroup analyses in case-control studies assessing 25(OH)D and both colon and rectal cancer in men, showed the same non-significant associations reported in their main ORs. However, in case of colon cancer, RIA method showed a trend toward inverse association.
Finally, in case of prospective studies assessing the risk of CRC by 25(OH)D in all subjects, subgroup analysis by methods (immunoassays and LC-MS/MS) made the HRs non-significant, and the same happened with results focused on serum samples.
Discussion
The present systematic review and meta-analysis is the largest one assessing circulating vitamin D (including total, bioavailable and free 25(OH)D and 1,25(OH)D measurements) and site-specific CRC risk also considering differences by sex. Our results showed an inverse association between vitamin D levels (highest versus lowest categories) and risk of CRC including all subjects, where the differences between sexes were also considered.
In the present meta-analysis, regarding to case-control studies, we found that total, bioavailable and free 25(OH)D were significantly and inversely associated with CRC in all subjects, but not with CC and RC. However, when we separated the subjects by sex, we only observed a significant inverse association between total 25(OH)D and CRC in women. No significant associations were observed between 1,25(OH)2D and CRC in both men and women. With respect to the results from the meta-analysis of prospective cohort studies, a significant inverse association was found between 25(OH)D and CRC in all subjects, but not with CC. When we stratified the participants by sex, this association only remained significant in women. Importantly, subgroup analyses by sample source and methodological procedure for vitamin D determination were mostly consistent with our main analyses. In which regards the heterogeneity, we reported substantial and significant heterogeneity among studies in the meta-analyses of case-control studies: free 25(OH)D and CRC in all subjects, 25(OH)D and CRC in men, 25(OH)D and CC in all subjects, men and women, and 25(OH)D and RC in men. Based on sensitivity and subgroup analyses, we hypothesize that these increased heterogeneity values were explained either by specific studies - such as Wu et al. Citation2007 in case of case-control studies evaluating risk of CC by circulating 25(OH)D levels in men - and/or method and/or sample type of vitamin D measurement. However, it may also rely on the confounders by which each study adjusted their models for.
Several systematic reviews and meta-analyses have been conducted to evaluate the association between circulating vitamin D and CRC risk (Ekmekcioglu, Haluza, and Kundi Citation2017; Gandini et al. Citation2011; C. F. Garland and Gorham Citation2017; Gorham et al. Citation2007; Grant Citation2010; Lee et al. Citation2011; Ma et al. Citation2011; Touvier et al. 2011; Yin et al. Citation2009), although these studies did not consider different factors that are crucial at the time of performing the meta-analysis. For instance, many of them included a combination of case-control and prospective cohort studies, but not separately, which could lead to a misinterpretation of results due to the nature of the study design. Likewise, these studies did not distinguish different circulating vitamin D subtypes, such as total, bioavailable, or free 25(OH)D, neither 1,25(OH)2D. Finally, many of these studies did not evaluate CRC, CC, or RC separately, neither accounted for differences between sexes.
Our results from the meta-analysis of case-control studies are in line with a previous one conducted by Gorham et al. (Citation2007). This study included five nested case-control studies and reported a 51% lower risk (OR: 0.49 (95% CI: 0.35; 0.68)) of CRC when comparing serum 25(OH)D level above 33 ng/mL to 12 ng/mL (Gorham et al. Citation2007). However, this study did not evaluate specific-site cancer and sex separately and neither different vitamin D metabolites (e.g. total, bioavailable or free).
Concerning meta-analyses of prospective cohort studies, four studies reported similar findings in regarding to our results, but with some dissimilarities. Grant (Citation2010) reported an inverse associated between 25(OH)D and CRC risk as well (Grant Citation2010), but did not evaluate specific-site cancer, sex and vitamin D metabolites separately. In addition, Ma et al. (Citation2011) also showed a negative association between CRC and CC and 25(OH)D levels (Ma et al. Citation2011). Although they find a significant decreased risk of rectal cancer, which disagree with our results, since they did not consider men and women separately. Lee et al. (Citation2011) observed a significant inverse association for CRC and RC but not for CC (Lee et al. Citation2011), which was partially in agreement with our results, since we found a significant association between vitamin D and CC. Finally, Touvier et al. (2011) reported an inverse association between CRC and CC risk and serum/plasma 25(OH)D, but not in case of RC (Touvier et al. 2011), which was partially in agreement with our results. With respect to meta-analyses including a combination of case-control and PC studies, four studies reported an inverse association between 25(OH)D levels and CRC (Ekmekcioglu, Haluza, and Kundi Citation2017; Gandini et al. Citation2011; C. F. Garland and Gorham Citation2017; Yin et al. Citation2009), which were according with our findings. However, most of the aforementioned studies did not consider some of potential cofounding variables, such as different metabolites of vitamin D or men and women separately.
The most common forms of pre-vitamin D are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol) which differ in the structure of their side chains but theoretically can be used by the body in an indistinguishable manner. In addition, to dietary and supplemental intakes, bioavailable vitamin D depends on a set of different variables that include sun exposure time, season, phototype, lifestyle data, and genetic polymorphisms. Calcitriol exerts its biological functions by binding to the VDR and modulating the gene expression of more than 1,600 target genes in numerous cell types (Nurminen et al. Citation2015). In fact, calcitriol - via VDR - is able to induce changes in nucleosome histones, thus enabling transcription (Carlberg and Muñoz Citation2020). In addition, vitamin D has been also associated with DNA methylation of genes related with CRC (Boughanem et al. Citation2020), which suggests a role in epigenetic pathways. Likewise, several studies have shown that vitamin D regulates the process of tumorigenesis, from initiation to stabilization, and the interaction with the cellular microenvironment (Feldman et al. Citation2014). Moreover, vitamin D has been shown to have anti-inflammatory, oxidative stress, and immune response, which may help to inhibit tumor cell initiation and progression (Wimalawansa Citation2019). In fact, an association between circulating levels of vitamin D and anti-inflammatory markers has been reported indicating that a modulation of inflammatory responses by vitamin D could probably result in improved cancer prognosis (Wesselink et al. 2020).
In our meta-analysis, we did not find an association between 1,25(OH)2D3 and CRC, maybe because this metabolite in blood is more associated with bone mineral density (Swanson et al. 2015). Interestingly, the action of calcitriol in cancer cells not only depends on VDR expression, but on the intracellular concentrations of calcitriol as well. The concentration of calcitriol in the intracellular cancer cells is determined by the circulating concentrations of 25(OH)D and calcitriol, but also by the activity of enzymes encoded by the genes CYP27B1 – which catalyzes the renal activation of vitamin D - and CYP24A1 (inactivation of vitamin D) and the VDR amount. The function of these genes is crucial to maintain the active form available into the cancer cells since these enzymes could be implicated in cellular vitamin D resistance. Overall, the concentration of circulating 25(OH)D seems to be important in the prevention of CRC, although there are some discrepancies on adequate circulating levels of vitamin D for different outcomes, such as bone mineral metabolism, heart disease, or overall mortality. In case of CRC, the optimal values are between 36 and 40 ng/mL (Bischoff-Ferrari et al. Citation2006). The US Endocrine Society defined vitamin D levels of 20 ng/mL or less as deficiency, 21–29 ng/mL as insufficiency, and 30 ng/mL or more as sufficiency (Bischoff-Ferrari et al. Citation2006).
The main strength of this meta-analysis, is that this is the first systematic review and meta-analysis that analyzed the association between circulating vitamin D levels, in both case-control and prospective cohort studies separately, taking into account sex, specific cancer sites, as well as different vitamin D metabolites. In addition, two different databases were used to identify available studies about the relationship between circulating vitamin D levels and on the CRC risk, in which a few of additional manually articles were identified and further added to the analyses. In fact, the research of literature and selected studies, data selection and extraction, was performed by two independent reviewers, which guarantee the lack of missing of related publishing data. Finally, we performed previously published methodological approaches for data transformation (e.g., changing reference of quintiles) to avoid excluding publications from the analyses. Several limitations also need to be addressed. First, results regarding the association between 1,25(OH)2D3 and CRC are limited by the few number of studies that evaluated this association3. Second, most of the studies only have one vitamin D measurement, which do not reflect the long-term vitamin D status. Third, the design of the included studies (case-control and prospective cohorts) does not allow us to exclude residual confounding and neither to stablish a causal association between circulating vitamin D and CRC. Finally, measurement of 25(OH)D was performed by several methods and from different sources (i.e., plasma, serum) in the included studies. Although these methods may be accurate and reproducible compared with many assays used in medicine, it could hinder the comparability between studies and introduce heterogeneity between them. Importantly, we performed different subgroup analyses to analyze the putative relevance of either sample source or methodological procedures to each overall meta-analysis OR or HR. However, it should be acknowledged that when less than 10 study comparisons are included in the meta-analysis, results from subgroup analysis might not be useful (Deeks, Higgins, and Altman Citation2021). Moreover, subgroup analysis based on sample source or methodological procedures was a post-hoc analysis not pre-specified in the protocol, which increases the likelihood of spurious findings.
Conclusions
In this large systematic review and meta-analysis of case-control and prospective studies, we observed that higher 25(OH)D concentration was associated with lower risk of CRC, especially in women. Our results support the hypothesis that circulating vitamin D levels could have a large beneficial impact for CRC prevention. However, further studies should elucidate underlying mechanisms involved in the progression of CRC and the role of vitamin D.
Author’s contribution to the manuscript
PH-A, MM-G, JS-S, SC, and NB-T designed research. HB and SC conducted research. PH-A performed statistical analysis. PH-A, HB, SC, NB-T, MF, NA, MM-G, and JS-S wrote paper. NB-T, SC, PH-A and JS-S had primary responsibility for final content. All authors have read and approved the final manuscript.
Supplemental Material
Download MS Word (1.1 MB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Acikgoz, A., D. Cimrin, and G. Ergor, 2020. Effect of serum 25-hydroxyvitamin D level on lung, breast, colorectal and prostate cancers: A nested case–control study. Eastern Mediterranean Health Journal = La Revue de Sante de la Mediterranee Orientale = al-Majallah al-Sihhiyah li-Sharq al-Mutawassit 26 (7):794–802. https://applications.emro.who.int/emhj/v26/07/1020-3397-2020-2607-794-802-eng.pdf. doi: 10.26719/emhj.20.035.
- Ananthakrishnan, A. N., S.-C. Cheng, T. Cai, A. Cagan, V. S. Gainer, P. Szolovits, S. Y. Shaw, S. Churchill, E. W. Karlson, S. N. Murphy, et al. 2014. Association between reduced plasma 25-hydroxy Vitamin D and increased risk of cancer in patients with inflammatory bowel diseases. Clinical Gastroenterology and Hepatology 12 (5):821–7. https://linkinghub.elsevier.com/retrieve/pii/S1542356513016443. doi: 10.1016/j.cgh.2013.10.011.
- Andersen, S. W., X.-O. Shu, Q. Cai, N. K. Khankari, M. D. Steinwandel, P. W. Jurutka, W. J. Blot, and W. Zheng, 2017. Total and free circulating Vitamin D and Vitamin D-binding protein in relation to colorectal cancer risk in a prospective study of African Americans. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 26 (8):1242–7. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-17-0133. doi: 10.1158/1055-9965.EPI-17-0133.
- Anic, G. M., S. J. Weinstein, A. M. Mondul, S. Männistö, and D. Albanes, 2014. Serum Vitamin D, Vitamin D binding protein, and risk of colorectal cancer. PLoS ONE 9 (7):e102966. doi: 10.1371/journal.pone.0102966.
- Bischoff-Ferrari, H. A., E. Giovannucci, W. C. Willett, T. Dietrich, and B. Dawson-Hughes. 2006. Estimation of optimal serum concentrations of 25-Hydroxyvitamin D for multiple health outcomes. The American Journal of Clinical Nutrition 84 (1):18–28. https://academic.oup.com/ajcn/article/84/1/18/4633029. doi: 10.1093/ajcn/84.1.18.
- Boughanem, H., A. Cabrera-Mulero, P. Hernández-Alonso, M. Clemente-Postigo, F. F. Casanueva, F. J. Tinahones, S. Morcillo, A. B. Crujeiras, and M. Macias-Gonzalez, 2020. Association between variation of circulating 25-OH Vitamin D and methylation of secreted frizzled-related protein 2 in colorectal cancer. Clinical Epigenetics 12 (1):83. https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-020-00875-9. doi: 10.1186/s13148-020-00875-9.
- Braun, M. M., K. J. Helzlsouer, B. W. Hollis, and G. W. Comstock, 1995. Colon Cancer and Serum Vitamin D metabolite levels 10-17 years prior to diagnosis. American Journal of Epidemiology 142 (6):608–11. https://academic.oup.com/aje/article/53799/Colon. doi: 10.1093/oxfordjournals.aje.a117682.
- Carlberg, C., and A. Muñoz. 2020. An update on Vitamin D signaling and cancer. Seminars in Cancer Biology. doi: 10.1016/j.semcancer.2020.05.018
- Chandler, P. D., J. E. Buring, J. E. Manson, E. L. Giovannucci, M. V. Moorthy, S. Zhang, I.-M. Lee, and J. H. Lin, 2015. Circulating Vitamin D levels and risk of colorectal cancer in women. Cancer Prevention Research (Philadelphia, PA) 8 (8):675–82. http://cancerpreventionresearch.aacrjournals.org/lookup/doi/10.1158/1940-6207.CAPR-14-0470. doi: 10.1158/1940-6207.CAPR-14-0470.
- Cheney, C. P., B. Thorand, C. Huth, K. Berger, A. Peters, V. Seifert-Klauss, M. Kiechle, K. Strauch, and A. S. Quante, 2018. The Association between Serum 25-Hydroxyvitamin D and cancer risk: results from the prospective KORA F4 Study. Oncology Research and Treatment 41 (3):117–21. https://www.karger.com/Article/FullText/485512. doi: 10.1159/000485512.
- Deeks, J. J., J. P. T. Higgins, and D. G. Altman. 2021. “Chapter 10: Analysing Data and Undertaking Meta-Analyses.” In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021). https://training.cochrane.org/handbook/current/chapter-10 (May 25, 2021).
- Dekker, E., P. J. Tanis, J. L. A. Vleugels, P. M. Kasi, and M. B. Wallace, 2019. Colorectal cancer. The Lancet 394 (10207):1467–80. https://linkinghub.elsevier.com/retrieve/pii/S0140673619323190. doi: 10.1016/S0140-6736(19)32319-0.
- Dou, R., K. Ng, E. L. Giovannucci, J. E. Manson, Z. R. Qian, and S. Ogino, 2016. Vitamin D and colorectal cancer: molecular, epidemiological and clinical evidence. The British Journal of Nutrition 115 (9):1643–60. https://www.cambridge.org/core/product/identifier/S0007114516000696/type/journal_article. doi: 10.1017/S0007114516000696.
- Ekmekcioglu, C., D. Haluza, and M. Kundi, 2017. 25-Hydroxyvitamin D status and risk for colorectal cancer and Type 2 diabetes mellitus: A systematic review and meta-analysis of epidemiological studies. International Journal of Environmental Research and Public Health 14 (2):127. http://www.mdpi.com/1660-4601/14/2/127. doi: 10.3390/ijerph14020127.
- Feldman, D., A. V. Krishnan, S. Swami, E. Giovannucci, and B. J. Feldman, 2014. The Role of Vitamin D in reducing cancer risk and progression. Nature Reviews. Cancer 14 (5):342–57. http://www.nature.com/articles/nrc3691. doi: 10.1038/nrc3691.
- Feskanich, D., J. Ma, C. S. Fuchs, G. J. Kirkner, S. E. Hankinson, B. W. Hollis, and E. L. Giovannucci, 2004. Plasma Vitamin D metabolites and risk of colorectal cancer in women. Cancer Epidemiology, Biomarkers & Prevention : a Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 13 (9):1502–8.
- Gandini, S., M. Boniol, J. Haukka, G. Byrnes, B. Cox, M. J. Sneyd, P. Mullie, and P. Autier, 2011. Meta-analysis of observational studies of Serum 25-Hydroxyvitamin D levels and colorectal, breast and prostate cancer and colorectal adenoma. International Journal of Cancer 128 (6):1414–24. http://doi.wiley.com/10.1002/ijc.25439. doi: 10.1002/ijc.25439.
- Garland, C. F., et al. 1989. Serum 25-Hydroxy Vitamin D and colon cancer: eight-year prospective study. The Lancet 334 (8673):1176–8. https://linkinghub.elsevier.com/retrieve/pii/S0140673689917893.
- Garland, C. F., and F. C. Garland, 1980. Do Sunlight and Vitamin D reduce the likelihood of colon cancer? International Journal of Epidemiology 9 (3):227–31. https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/9.3.227. doi: 10.1093/ije/9.3.227.
- Garland, C. F., and E. D. Gorham, 2017. Dose-Response of Serum 25-Hydroxyvitamin D in association with risk of colorectal cancer: a meta-analysis. The Journal of Steroid Biochemistry and Molecular Biology 168:1–8. https://linkinghub.elsevier.com/retrieve/pii/S0960076016303429. doi: 10.1016/j.jsbmb.2016.12.003.
- Gorham, E. D., C. F. Garland, F. C. Garland, W. B. Grant, S. B. Mohr, M. Lipkin, H. L. Newmark, E. Giovannucci, M. Wei, M. F. Holick, et al. 2007. Optimal Vitamin D status for colorectal cancer prevention. American Journal of Preventive Medicine 32 (3):210–6. https://linkinghub.elsevier.com/retrieve/pii/S0749379706004983. doi: 10.1016/j.amepre.2006.11.004.
- Grant, W. B. 2010. Relation between prediagnostic serum 25-Hydroxyvitamin D level and incidence of breast, colorectal, and other cancers. Journal of Photochemistry and Photobiology. B, Biology 101 (2):130–6. https://linkinghub.elsevier.com/retrieve/pii/S1011134410001065. doi: 10.1016/j.jphotobiol.2010.04.008.
- Hamling, J., P. Lee, R. Weitkunat, and M. Ambühl, 2008. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Statistics in Medicine 27 (7):954–70. http://doi.wiley.com/10.1002/sim.3013. doi: 10.1002/sim.3013.
- Heath, A. K., A. M. Hodge, P. R. Ebeling, D. Kvaskoff, D. W. Eyles, G. G. Giles, D. R. English, and E. J. Williamson, 2020. Circulating 25-Hydroxyvitamin D concentration and cause-specific mortality in the melbourne collaborative cohort study. The Journal of Steroid Biochemistry and Molecular Biology 198:105612. https://linkinghub.elsevier.com/retrieve/pii/S0960076019304844. doi: 10.1016/j.jsbmb.2020.105612.
- Higgins, J. P. T., and S. Green, eds. 2019. Cochrane handbook for systematic reviews of interventions. United Kingdom: The Cochrane Collaboration.
- Higgins, J., and S. Green, 2015. Cochrane handbook for systematic reviews of interventions Version 5.3.0. Chichester. The Cochrane Collaboration 2 (2):126–30. www.cochrane-handbook.org.
- Hiraki, L. T., A. D. Joshi, K. Ng, C. S. Fuchs, J. Ma, A. Hazra, U. Peters, E. W. Karlson, E. Giovannucci, P. Kraft, et al. 2014. Joint effects of colorectal cancer susceptibility loci, circulating 25-Hydroxyvitamin D and risk of colorectal cancer”. PLoS ONE 9 (3):e92212. https://dx.plos.org/10.1371/journal.pone.0092212. doi: 10.1371/journal.pone.0092212.
- Huang, D., S. Lei, Y. Wu, M. Weng, Y. Zhou, J. Xu, D. Xia, E. Xu, M. Lai, H. Zhang, et al. 2020. Additively protective effects of Vitamin D and calcium against colorectal adenoma incidence, malignant transformation and progression: A systematic review and meta-analysis. Clinical Nutrition (Edinburgh, Scotland) 39 (8):2525–38. https://linkinghub.elsevier.com/retrieve/pii/S0261561419331395. doi: 10.1016/j.clnu.2019.11.012.
- Jenab, M., H. B. Bueno-de-Mesquita, P. Ferrari, F. J. B. van Duijnhoven, T. Norat, T. Pischon, E. H. J. M. Jansen, N. Slimani, G. Byrnes, S. Rinaldi, et al. 2010. Association between pre-diagnostic circulating Vitamin D concentration and risk of colorectal cancer in European Populations: A nested case-control study. BMJ (Clinical Research ed.) 340 (jan21 3):b5500–b5500. https://www.bmj.com/lookup/doi/10.1136/bmj.b5500. doi: 10.1136/bmj.b5500.
- Keum, N. N. a., and E. Giovannucci, 2019. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nature Reviews Gastroenterology & Hepatology 16 (12):713–32. http://www.nature.com/articles/s41575-019-0189-8. doi: 10.1038/s41575-019-0189-8.
- Lee, J. E., H. Li, A. T. Chan, B. W. Hollis, I.-M. Lee, M. J. Stampfer, K. Wu, E. Giovannucci, and J. Ma, 2011. Circulating levels of Vitamin D and colon and rectal cancer: The physicians' health study and a meta-analysis of prospective studies . Cancer Prevention Research (Philadelphia, PA) 4 (5):735–43. http://cancerpreventionresearch.aacrjournals.org/lookup/doi/10.1158/1940-6207.CAPR-10-0289. doi: 10.1158/1940-6207.CAPR-10-0289.
- Ma, Y., P. Zhang, F. Wang, J. Yang, Z. Liu, and H. Qin, 2011. Association between Vitamin D and risk of colorectal cancer: A systematic review of prospective studies. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 29 (28):3775–82. http://ascopubs.org/doi/10.1200/JCO.2011.35.7566. doi: 10.1200/JCO.2011.35.7566.
- McCullough, M. L., et al. 2019. Circulating Vitamin D and colorectal cancer risk: An international pooling project of 17 Cohorts. JNCI: Journal of the National Cancer Institute 111 (2):158–69. https://academic.oup.com/jnci/article/111/2/158/5035027.
- Neuhouser, M. L., J. E. Manson, A. Millen, M. Pettinger, K. Margolis, E. T. Jacobs, J. M. Shikany, M. Vitolins, L. Adams-Campbell, S. Liu, et al. 2012. The influence of health and lifestyle characteristics on the relation of serum 25-hydroxyvitamin D with risk of colorectal and breast cancer in postmenopausal women. American Journal of Epidemiology 175 (7):673–84. https://academic.oup.com/aje/article-lookup/doi/10.1093/aje/kwr350. doi: 10.1093/aje/kwr350.
- NHLBI. 2014. Quality assessment tool for observational cohort and cross-sectional studies, 1–4. Bethesda, MD: National Institutes of Health, Department of Health and Human Services. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort.
- Nurminen, V., A. Neme, J. Ryynänen, S. Heikkinen, S. Seuter, and C. Carlberg, 2015. The transcriptional regulator BCL6 participates in the secondary gene regulatory response to Vitamin D. Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms 1849 (3):300–8. https://linkinghub.elsevier.com/retrieve/pii/S1874939914002958. doi: 10.1016/j.bbagrm.2014.12.001.
- Ordóñez-Mena, J. M., B. Schöttker, V. Fedirko, M. Jenab, A. Olsen, J. Halkjaer, E. Kampman, L. de Groot, E. Jansen, H. B. Bueno-de-Mesquita, et al. 2016. Pre-Diagnostic Vitamin D concentrations and cancer risks in older individuals: an analysis of cohorts participating in the CHANCES Consortium. European Journal of Epidemiology 31 (3):311–23. http://link.springer.com/10.1007/s10654-015-0040-7. doi: 10.1007/s10654-015-0040-7.
- Ordóñez-Mena, J. M., B. Schöttker, U. Haug, H. Müller, J. Köhrle, L. Schomburg, B. Holleczek, and H. Brenner, 2013. Serum 25-Hydroxyvitamin D and cancer risk in older adults: Results from a large German prospective cohort study. Cancer Epidemiology Biomarkers & Prevention 22 (5):905–16. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-12-1332. doi: 10.1158/1055-9965.EPI-12-1332.
- Otani, T., for the Japan Public Health Center-Based Prospective Study Group, M. Iwasaki, S. Sasazuki, M. Inoue, and S. Tsugane, 2007. Plasma Vitamin D and risk of colorectal cancer: The Japan public health center-based prospective study. British Journal of Cancer 97 (3):446–51. http://www.nature.com/articles/6603892. doi: 10.1038/sj.bjc.6603892.
- Pludowski, P., M. F. Holick, W. B. Grant, J. Konstantynowicz, M. R. Mascarenhas, A. Haq, V. Povoroznyuk, N. Balatska, A. P. Barbosa, T. Karonova, et al. 2018. Vitamin D supplementation guidelines. The Journal of Steroid Biochemistry and Molecular Biology 175:125–35. https://pubmed.ncbi.nlm.nih.gov/28216084/ (May 26, 2021). doi: 10.1016/j.jsbmb.2017.01.021.
- Siegel, Rebecca, L., et al. 2020. Colorectal cancer statistics, 2020. CA: A Cancer Journal for Clinicians 70 (3):145–64. https://onlinelibrary.wiley.com/doi/abs/10.3322/caac.21601.
- Skaaby, T., L. L. N. Husemoen, B. H. Thuesen, C. Pisinger, T. Jørgensen, N. Roswall, S. C. Larsen, and A. Linneberg, 2014. Prospective population-based study of the association between serum 25-Hydroxyvitamin-D Levels and the incidence of specific types of cancer. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 23 (7):1220–9. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-14-0007. doi: 10.1158/1055-9965.EPI-14-0007.
- Song, M., G. G. Konijeti, C. Yuan, A. N. Ananthakrishnan, S. Ogino, C. S. Fuchs, E. L. Giovannucci, K. Ng, and A. T. Chan, 2016. Plasma 25-Hydroxyvitamin D, Vitamin D binding protein, and risk of colorectal cancer in the nurses' health study. Cancer Prevention Research (Philadelphia, PA) 9 (8):664–72. http://cancerpreventionresearch.aacrjournals.org/lookup/doi/10.1158/1940-6207.CAPR-16-0053. doi: 10.1158/1940-6207.CAPR-16-0053.
- Song, M., K. Wu, A. T. Chan, C. S. Fuchs, and E. L. Giovannucci, 2014. Plasma 25-Hydroxyvitamin D and risk of colorectal cancer after adjusting for inflammatory markers. Cancer Epidemiology, Biomarkers & Prevention : a Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 23 (10):2175–80. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-14-0712. doi: 10.1158/1055-9965.EPI-14-0712.
- Stroup, D. F., J. A. Berlin, S. C. Morton, I. Olkin, G. D. Williamson, D. Rennie, D. Moher, B. J. Becker, T. A. Sipe, and S. B. Thacker, 2000. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283 (15):2008–12. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.283.15.2008. doi: 10.1001/jama.283.15.2008.
- Swanson, C. M., Osteoporotic Fractures in Men MrOS Study Research Group, P. Srikanth, C. G. Lee, S. R. Cummings, I. Jans, J. A. Cauley, R. Bouillon, D. Vanderschueren, E. S. Orwoll, and C. M. Nielson, 2015. Associations of 25-Hydroxyvitamin D and 1,25-Dihydroxyvitamin D with bone mineral density, bone mineral density change, and incident nonvertebral fracture. Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research 30 (8):1403–13. http://doi.wiley.com/10.1002/jbmr.2487. doi: 10.1002/jbmr.2487.
- Tangrea, J., K. Helzlsouer, P. Pietinen, P. Taylor, B. Hollis, J. Virtamo, and D. Albanes, 1997. Serum Levels of Vitamin D metabolites and the subsequent risk of colon and rectal cancer in Finnish men. Cancer Causes and Control 8 (4):615–25. doi: 10.1023/A:1018450531136.
- Theodoratou, E., T. Palmer, L. Zgaga, S. M. Farrington, P. McKeigue, F. V. N. Din, A. Tenesa, G. Davey-Smith, M. G. Dunlop, and H. Campbell, 2012. Instrumental variable estimation of the causal effect of plasma 25-Hydroxy-Vitamin D on colorectal cancer risk: A Mendelian randomization analysis. PLoS One 7 (6):e37662. doi: 10.1371/journal.pone.0037662.
- Touvier, M., D. S. M. Chan, R. Lau, D. Aune, R. Vieira, D. C. Greenwood, E. Kampman, E. Riboli, S. Hercberg, and T. Norat, 2011. Meta-analyses of Vitamin D intake, 25-Hydroxyvitamin D Status, Vitamin D receptor polymorphisms, and colorectal cancer risk. Cancer Epidemiology, Biomarkers & Prevention : a Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology 20 (5):1003–16. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-10-1141. doi: 10.1158/1055-9965.EPI-10-1141.
- Vojdeman, F. J., C. M. Madsen, K. Frederiksen, D. Durup, A. Olsen, L. Hansen, A.-M. Heegaard, B. Lind, A. Tjønneland, H. L. Jørgensen, et al. 2019. Vitamin D Levels and cancer incidence in 217,244 individuals from primary health care in Denmark. International Journal of Cancer 145 (2):338–46. https://onlinelibrary.wiley.com/doi/abs/10.1002/ijc.32105. doi: 10.1002/ijc.32105.
- Weinstein, S. J., et al. 2015. Serum 25-Hydroxyvitamin D, Vitamin D binding protein and risk of colorectal cancer in the prostate, lung, colorectal and ovarian cancer screening trial. International Journal of Cancer 136 (6):E654–64. http://doi.wiley.com/10.1002/ijc.29157.
- Weinstein, S. J., K. Yu, R. L. Horst, J. Ashby, J. Virtamo, and D. Albanes, 2011. Serum 25-Hydroxyvitamin D and risks of colon and rectal cancer in Finnish Men. American Journal of Epidemiology 173 (5):499–508. https://academic.oup.com/aje/article-lookup/doi/10.1093/aje/kwq398. doi: 10.1093/aje/kwq398.
- Wells, G. A., B. Shea, D. O’Connell, and J. Peterson. 2000. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Wesselink, E., M. Balvers, M. J. L. Bours, J. H. W. de Wilt, R. F. Witkamp, H. van Baar, A. J. M. R. Geijsen, H. van Halteren, E. T. P. Keulen, D. E. Kok, et al. 2020. The association between circulating levels of Vitamin D and inflammatory markers in the first 2 years after colorectal cancer diagnosis. Therapeutic Advances in Gastroenterology 13:1756284820923922. http://journals.sagepub.com/doi/10.1177/1756284820923922. doi: 10.1177/1756284820923922.
- Wimalawansa, S. J. 2019. Vitamin D deficiency: effects on oxidative stress, epigenetics. Gene Regulation, and Aging. Biology 8 (2):30. https://www.mdpi.com/2079-7737/8/2/30. doi: 10.3390/biology8020030.
- Wong, Y. Y. E., Z. Hyde, K. A. McCaul, B. B. Yeap, J. Golledge, G. J. Hankey, and L. Flicker, 2014. In older men, lower plasma 25-Hydroxyvitamin D is associated with reduced incidence of prostate, but not colorectal or lung cancer” ed. Suminori Akiba. PLoS One 9 (6):e99954. https://dx.plos.org/10.1371/journal.pone.0099954. doi: 10.1371/journal.pone.0099954.
- Woolcott, C. G., L. R. Wilkens, A. M. Y. Nomura, R. L. Horst, M. T. Goodman, S. P. Murphy, B. E. Henderson, L. N. Kolonel, and L. Le Marchand, 2010. Plasma 25-Hydroxyvitamin D levels and the risk of colorectal cancer: The multiethnic cohort study. Cancer Epidemiology Biomarkers & Prevention 19 (1):130–4. http://cebp.aacrjournals.org/lookup/doi/10.1158/1055-9965.EPI-09-0475. doi: 10.1158/1055-9965.EPI-09-0475.
- Wu, K., D. Feskanich, C. S. Fuchs, A. T. Chan, W. C. Willett, B. W. Hollis, M. N. Pollak, and E. Giovannucci, 2011. Interactions between plasma levels of 25-Hydroxyvitamin D, Insulin-like Growth Factor (IGF)-1 and C-peptide with risk of colorectal cancer.” ed. Libing Song. PloS One 6 (12):e28520. https://dx.plos.org/10.1371/journal.pone.0028520. doi: 10.1371/journal.pone.0028520.
- Wu, K., D. Feskanich, C. S. Fuchs, W. C. Willett, B. W. Hollis, and E. L. Giovannucci, 2007. A Nested case control study of plasma 25-hydroxyvitamin D concentrations and risk of colorectal cancer. Journal of the National Cancer Institute 99 (14):1120–9. https://academic.oup.com/jnci/article-lookup/doi/10.1093/jnci/djm038. doi: 10.1093/jnci/djm038.
- Yin, L., N. Grandi, E. Raum, U. Haug, V. Arndt, and H. Brenner, 2009. Meta-analysis: Longitudinal studies of serum Vitamin D and colorectal cancer risk. Alimentary Pharmacology & Therapeutics 30 (2):113–25. http://doi.wiley.com/10.1111/j.1365-2036.2009.04022.x. doi: 10.1111/j.1365-2036.2009.04022.x.
- Ying, H.-Q., H.-L. Sun, B.-S. He, Y.-Q. Pan, F. Wang, Q.-W. Deng, J. Chen, X. Liu, and S.-K. Wang, 2015. Circulating Vitamin D binding protein, total, free and bioavailable 25-Hydroxyvitamin D and risk of colorectal cancer. Scientific Reports 5 (1):7956. http://www.nature.com/articles/srep07956. doi: 10.1038/srep07956.
- Zhu, K. M., Knuiman, M. Divitini, J. Hung, E. M. Lim, B. R. Cooke, and J. P. Walsh, 2019. Lower Serum 25-Hydroxyvitamin D is associated with colorectal and breast cancer, but not overall cancer risk: a 20-year cohort study. Nutrition Research 67:100–7. https://linkinghub.elsevier.com/retrieve/pii/S0271531718309291. doi: 10.1016/j.nutres.2019.03.010.