ABSTRACT
The COVID-19 pandemic’s effects on people’s lives and society induced a need for rapid individual and collective sensemaking, including communication forums enabling stakeholders in the health ecosystem to share information, solve problems, and learn. This study specifically focused on the needs of the patients and family caregivers living with cystic fibrosis (CF) or primary ciliary dyskinesia (PCD), conditions that lead to chronic infections and inflammation in the airways. We explored how CF and PCD patients, family caregivers, and clinicians collectively received, processed, and used information about COVID-19 to facilitate self-care and health care decisions at the beginning of the pandemic. We applied macrocognitive theory to analyze qualitatively the questions and answers exchanged in a series of six webinars facilitated by a CF learning network at the beginning of the pandemic (March – April 2020). We identified three macrocognitive functions: sensemaking, decision-making, and replanning. We further generated nine themes: (a) understanding the nature of COVID-19, (b) exploring self-care needs and possibilities, (c) understanding health care possibilities, (d) making decisions about prevention and testing, (e) managing COVID-19 within families, (f) adjusting planned care, (g) replanning chronic care management, (h) defining COVID-19 health care strategies, and (i) refining health care policies. The exchange of questions and answers played a central role in facilitating important cognitive processes, which enabled a rapid anticipation of needs and adaptation of services to support patients, family caregivers, and clinicians during the COVID-19 pandemic.
Introduction
The COVID-19 pandemic has been described as an extremely uncertain situation in which our minds have struggled to organize confusing information into coherent interpretations (Chater, Citation2020). This uncertainty has triggered a need for collective sensemaking and communication regarding COVID-19’s effects on people’s lives and society (Angeli & Montefusco, Citation2020). Studies have addressed a wide range of issues regarding the ways risks and preventive measures are communicated to the public and the way they affect behavior (Kowalski & Black, Citation2021; Nan & Thompson, Citation2021; Nazione et al., Citation2021). However, information dissemination that is intended for a wide audience may not meet the specific needs of vulnerable populations, such as risk groups (Guttman & Lev, Citation2021). This calls for forums that specifically address vulnerable populations’ needs and allow stakeholders in the health care industry to engage in bidirectional information sharing, sensemaking, and learning.
People living with chronic conditions have a particularly urgent need to make sense of the pandemic because of their increased risk of morbidity and mortality from COVID-19 infection (Shahid et al., Citation2020). Meanwhile, health care has shifted its resources toward managing the pandemic, which has affected the conditions for chronic care management, including access to health care and community support. This has required health care professionals and individuals living with chronic conditions to adapt (Danhieux et al., Citation2020). Health care visits have become digital, less frequent, and in some cases, disrupted entirely due to the heavy load on health care systems, social distancing, and quarantine policies (Bloem et al., Citation2020; Farooqi et al., Citation2021).
This study focused on the ways patients with cystic fibrosis (CF) or primary ciliary dyskinesia (PCD), and family caregivers engaged in collective sensemaking with clinicians regarding COVID-19’s effects on self-care and health care. CF and PCD are rare and life-limiting recessive genetic disorders that are usually diagnosed during childhood and lead to chronic infections and inflammation in the airways (Elborn, Citation2016; Lucas et al., Citation2014). The two disorders are similarly managed through complex drug therapies, daily self-care (e.g., airway clearance, nutrition monitoring, and physical exercise), logistical planning of everyday activities, and consistent health care contacts. Patients may spend almost two hours per day on self-care activities (Sawicki et al., Citation2009; Ziaian et al., Citation2006). As patients with these conditions are vulnerable to airway infections, they were potentially at higher risk during the pandemic.
Building shared meaning through communicating with others
For patients, understanding their condition and managing their self-care may involve a considerable challenge. When challenged by a disruptive event, sensemaking and communication become essential. Weick et al. (Citation2005) explained that people construct sense in an inherently communicative process to overcome the gap between the current and expected state of the world. Storytelling promotes social cohesion and enables collaborative development of skills and knowledge (Bietti et al., Citation2019). Thus, when facing challenges, coping and sensemaking can be supported by interventions that facilitate storytelling and reflection based on narratives (Koenig Kellas et al., Citation2020).
Storytelling may also be an effective method to combine patient and professional capital in communities of health and social care practice (le May, Citation2008a). Communities of practice are “groups of people who share a concern, a set of problems, or a passion about a topic, and who deepen their understanding and knowledge of this area by interacting on an ongoing basis” (Wenger et al., Citation2002, p. 4). Examples are collaborative chronic care networks that have been proposed as network-based learning systems to harness the collective intelligence of patients, families, clinicians, and researchers (Margolis et al., Citation2013; Seid et al., Citation2018).
Collective sensemaking and sensegiving
Communities of practice provide a forum for collective sensemaking in multiprofessional groups. In collective sensemaking, individuals interact to make collective sense of new information (Coburn, Citation2001). This effort does not necessarily require individuals to work toward a common goal, which has been shown in online health networks enabling patients with varying goals to learn from each other’s expertise and experiences (Mamykina et al., Citation2015). Maitlis and Sonenshein (Citation2010) highlighted the challenge of involving neither too few nor too many perspectives in collective sensemaking; some variety in perspectives may contribute to the critical appraisal of information, but too much variety may inhibit the process of constructing shared meaning and knowledge.
Sensegiving is a complementary process to sensemaking that is concerned with influencing others’ construction of meaning (Gioia & Chittipeddi, Citation1991). Communities of practice may contribute to sensegiving by creating documents, guidelines, or protocols that give form to shared meaning (le May, Citation2008b). The strategic use of sensegiving has often been studied in the context of organizational change, which focuses on managers’ or change leaders’ activities (Huzzard et al., Citation2014). Health care professionals may use sensegiving strategies (e.g., educating, personalizing information, promoting open communication) to help families make sense of their care experience (Gilstrap, Citation2021).
Exploring the cognitive work of sensemaking and sensegiving
Sensemaking and sensegiving are not only communicative processes; they can also be conceptualized as cognitive processes that happen in individuals’ minds (Crandall et al., Citation2006). The concept of macrocognition describes the mental activities that occur in natural settings when people perform complex tasks (Klein et al., Citation2003). Examples of mental activities that are described as primary macrocognitive functions include detecting problems, making sense of difficult situations, engaging in planning and replanning, making decisions, and coordinating team efforts (Crandall et al., Citation2006; Klein et al., Citation2003; Patterson & Hoffman, Citation2012). To accomplish these activities, we engage in macrocognitive processes such as developing mental models of situations as we gather new experiences, projecting mental models into the future through mental simulation and story-building, managing uncertainty and risk in situations where few things can be controlled, identifying leverage points and turning them into courses of action, and maintaining common ground to coordinate activities and engage in effective team work (Crandall et al., Citation2006). The primary functions can be understood as the goals of the work whereas the processes can be interpreted as the means to achieve those goals (Patterson & Hoffman, Citation2012). Any of the primary functions can be triggered by events in the world or by individuals’ reasoning and communication with others (Patterson & Hoffman, Citation2012). The information people share in collaborative chronic care networks during the pandemic could reveal the macrocognitive functions that collective COVID-19 sensemaking triggered.
Applying the macrocognitive framework
The macrocognitive framework has previously been applied in studies on non-routine events characterized by time pressure; competing situation assessments; high risk; and ill-defined, conflicting goals (Crandall et al., Citation2006; Klein et al., Citation2003; Klein, Citation2008). For example, it has been used in analyses of teamwork among clinicians in complex and critical situations (Patterson et al., Citation2020; Schubert et al., Citation2013). Methods used to study professionals’ cognitive work can also be employed to analyze the cognitive work involved in self-care for patients living with chronic illness (e.g., Dhukaram & Baber, Citation2015; Holden et al., Citation2020; Klein & Lippa, Citation2012; Lippa et al., Citation2008) and family caregivers (Abebe et al., Citation2020). However, very little research has been conducted that acknowledges patients as essential knowledge workers in collaboration with health care professionals (Papautsky & Patterson, Citation2021). To the best of our knowledge, no study has applied the macrocognitive framework to explore the ways patients, family caregivers, and health care professionals together engage in collective sensemaking and sensegiving when facing a public health crisis such as a pandemic. Understanding the macrocognitive functions and processes involved may allow us to create support tools and educational materials to strengthen individuals’ self-care and health care when faced with disruptive events. The aim of this study was to explore the ways CF and PCD patients, family caregivers, and clinicians collectively received, processed, and used information about COVID-19 to facilitate self-care and health care decisions at the beginning of the pandemic.
Methods
Study design
We conducted a theory-driven qualitative analysis of a series of webinars that the Swedish CF chronic care network hosted at the beginning of the COVID-19 pandemic to discuss CF and PCD patients’ and family caregivers’ questions. We explored the written summaries of the questions and answers to identify primary macrocognitive functions and processes, as Crandall et al. (Citation2006), and Patterson and Hoffman (Citation2012) defined them.
Context
The Swedish public health response during the initial phase of COVID-19 strongly emphasized personal responsibility rather than imposing restrictions on the population (Häyry, Citation2021; Rambaree & Nässén, Citation2020). It was recommended that the public stay home in case of symptoms, use social distance, and wash their hands (Public Health Agency of Sweden, Citation2020b). At the time of this study, wearing facemasks in public areas was not generally recommended, possibly to prevent people from taking risks because they felt protected (Guttman & Lev, Citation2021). Although working from home was recommended if possible, no complete lockdown was imposed. High schools and higher-education institutions were advised to introduce distance teaching (Public Health Agency of Sweden, Citation2020a), but preschools and elementary schools continued with traditional in-person teaching. People living with CF or PCD were not officially recognized as a risk group and were expected to follow the same recommendations as the general public; for example, children with CF or PCD were recommended to go to school unless distance teaching was implemented.
CF learning network
The CF learning network (a.k.a. Sweden Coalition CF) is a collaborative chronic care network that was established by professional and community leaders in the Swedish CF community to strengthen partnerships and trustful information sharing between persons living with CF, families, and healthcare professionals; we have previously reported how the network supported the orderly introduction of a new CF therapy (Hager et al., Citation2021). One of the coauthors (AH), who is a family caregiver and eHealth entrepreneur engaged in developing patient support systems, was a driver in the establishment of this network. The members are stakeholders from various professions and with various expertise who are involved in CF and PCD care in Sweden, including adult and pediatric clinicians from the four national CF centers, and representatives from the Swedish CF Association, a national patient association for CF and PCD patients and family caregivers. The CF learning network is a community of practice that is well suited for exploring the ways its members responded to and supported patients and family caregivers when the need for sensemaking emerged in the period of information uncertainty and crisis the pandemic posed.
COVID-19 webinars
The CF learning network hosted six webinars during March and April of 2020, which was the initial phase of the COVID-19 pandemic in Sweden (Public Health Agency of Sweden, Citation2021). The webinars were announced through the national CF Association’s website, e-mail campaigns, and Facebook groups; they were hosted live on Zoom and were open to the public. Patients and family caregivers were encouraged to submit their questions by e-mail to the secretary of the CF learning network before the webinars. The members of the network prioritized questions to discuss during the webinars, which AH facilitated. In the first five webinars, two CF clinicians (including one pediatrician) represented the CF learning network and answered the questions. The last webinar focused specifically on questions related to transplantations, which a clinician and nurse specializing in transplantations answered. Webinar participants could interact through a chat function. The number of webinar participants typically ranged from 60 to 120, with a peak of nearly 200 participants.
Data and analysis
The data collection period was rather short (6 weeks), but given the specificity of the experiences and knowledge among the participants included in the sample, we determined that we reached satisfying information power to achieve internal validity (Malterud et al., Citation2016). Valuable contributions can be made with little data if the data are “new, unique, or rare” (LaDonna et al., Citation2018; Tracy, Citation2010), which was the case in this study. The first author (medical informatician) and the last author (pediatrician and patient safety researcher), who are trained in qualitative research, performed a thematic analysis (Braun & Clarke, Citation2006), combining a deductive and inductive approach. We observed the webinars to familiarize ourselves with the context and collected and compiled questions people had emailed to the CF learning network as well as a documentation of questions and answers that the network posted on the Swedish CF Association’s website after each webinar. After familiarizing ourselves with the data, we deductively coded macrocognitive functions and processes in the text and collated them into categories; we used a coding guide that specified definitions of the primary macrocognitive functions and what elements to look for in the data (). Thereafter, we inductively analyzed the data within each category whereby we created open codes, grouped them into themes, and reviewed and named the themes iteratively until we achieved an appropriate level of abstraction. We used the FreeMind mind-mapping software (Müller et al., Citation2013) to organize the data abstraction into a hierarchical structure, thus providing a full overview. We collaborated in the entire analysis process, which supported reflexivity, as we continuously discussed interpretations of the data (Braun & Clarke, Citation2019). To validate the analysis, we also discussed various stages of the analysis process with the other coauthors. In the final phase, we plotted the thematized data on a timeline to explore how the content and patterns of information sharing developed over time.
Table 1. Coding guide with definitions of the five primary macrocognitive functions and descriptions of what to look for in the data.
Ethical considerations
As the data were deidentified questions and answers from patients and family caregivers that we analyzed retrospectively, we obtained no informed consent from individual participants. The Swedish Ethical Review Authority approved the study (reg nr. 2019–03849 and 2020–01741).
Results
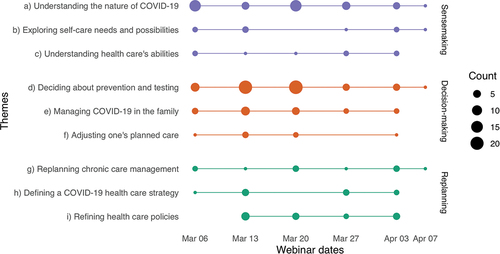
The data consisted of 167 questions (comprising 5,391 words) that patients and family caregivers posed to the CF learning network and 83 answers (comprising 5,730 words). We identified three primary macrocognitive functions in the data (sensemaking, decision-making, and replanning), which we further grouped into nine themes (). We illustrate the findings with translated quotes of questions (Q) and answers (A).
Figure 1. Timeline illustrating the frequency (dot size) and categorization of questions that patients and family caregivers posed to the CF learning network. The questions are categorized by macrocognitive functions (sensemaking = purple, decision-making = red, replanning = green) and inductively generated themes (a-i).
Sensemaking
Sensemaking was manifested in about one third of the questions (n = 58, 35%) and concerned the nature of COVID-19, self-care needs and possibilities, and health care’s abilities.
Understanding the nature of COVID-19
Questions that reflected how individuals tried to make sense of the nature of COVID-19 were discussed at each webinar. To expand their existing account of the pandemic, patients and family caregivers asked for general knowledge about the coronavirus as well as more specific knowledge about how it differs from other viruses and how it affects individuals with CF or PCD. They also asked questions about the routes of infection and course of illness, including incubation time, symptoms, and long-term effects, reflecting individuals’ need for sensemaking about possible future developments. Mental simulations were used to explore how symptoms of COVID-19 could differ from those of their chronic illness: “Patients with PCD/CF have a general problem with cough. Can we assume that with COVID-19, the cough is experienced differently?” (q148, w4). Rather than describing their personal situation, participants asked for information that applied to various groups of individuals: children, adolescents, and adults; individuals with mild versus severe CF or PCD symptoms; and individuals with lung transplants. This questioning indicates that they wanted to gain a general understanding of the situation in addition to making sense of their own experiences. At each webinar, clinicians provided updated information and knowledge about COVID-19 among people with CF or PCD that they had gained through collaboration with international networks, iteratively constructing and refining their shared understanding of the nature of COVID-19. The following example illustrates the pattern of information exchange from one of the webinars:
I wonder if you have received any more information about how persons with PCD/CF have been affected when infected with corona?
We received a report from Italy today. According to the CF doctor, they have three patients that have been diagnosed with COVID-19, one adult, one teenager, and one child. All had mild fever and cough as initial symptoms. According to the e-mail from the doctor, they are well. That is what we know. (q92 and a49, w3)
Exploring self-care needs and possibilities
The prospect of a longer period of isolation raised questions about how long the coronavirus outbreak may last and how to prepare practically (e.g., with food, hygiene, medications). When clinicians could not provide clear answers, they acknowledged their uncertainty about how matters would develop and referred to their current frame of reference to project possible developments: “We don’t know because this is a new virus, but from experiences of earlier viruses, it usually levels off during the warmer seasons. We don’t know for sure, but hopefully, also this virus will follow that pattern” (a30, w2). The possibility of taking routine tests at home was explored, which reflected how sensemaking was used to construct a novel account of what can be managed in self-care. Participants also explored COVID-19’s possible effects on daily self-care routines. The questions were sometimes complex and illustrated how individuals built on their preexisting understanding of viral infections to project possible future developments. For example, they expressed worry about using medications that lower their immune response and using inhalation therapy that could potentially spread infection to family members through droplets.
Understanding health care’s abilities
Patients and family caregivers sought to make sense about health care’s ability to prevent, diagnose, and treat COVID-19. Some posed open questions, such as, “Is there any medication that can mitigate the severity of a coronavirus-infection?” (q21, w1). Others sought clinicians’ responses to their suggestions and reasoning about possible means of prevention and treatment. The clinicians answered these questions by providing situation assessments based on their state of knowledge at the time:
The main [drug therapy] candidate is an already existing drug that was developed for Ebola but also proved to have good effect on SARS, which is another coronavirus (like COVID-19). The advantage with this is that it already exists and has been tested with humans in large scale. There are ongoing studies in China to test other antiviral drugs, where results are expected in the months to come. One of these is a malaria drug. Vaccine development has started, but it [may take] years before such a drug is on the market because it takes so much time to make new, safe drugs available. (a13, w1)
Decision-making
Half of the questions (n = 83, 50%) concerned individuals’ needs for support in making decisions about how to manage their everyday lives during the pandemic.
Deciding about prevention and testing
Participants were concerned about how to prevent COVID-19 for patients and family members. When asking for support in deciding how to behave in various settings with increased risk of infection, including schools, workplaces, sports, and leisure, they sometimes shared personal narratives about their needs and life situations to contextualize their questions. For example, one person asked, “How should one reason about being a CF patient, 62 years old, and working as a teacher, where I meet hundreds of individuals every day? We don’t have any opportunity to work from home” (q57, w2). Some also related to their previous experiences and knowledge: “I have heard that a good guideline is to act as if one is newly transplanted. … Would you recommend that now, as well?” (q130, w3). Rather than telling the people which decisions to make, the clinicians responded with general guidance and explanations, phrasing their answers in a way that could support decision-making and be sufficiently generic to meet more than one individual’s needs. Questions and answers about school attendance developed in parallel with the changing COVID-19 situation in the country. One aspect of the conversation was concerned with which rules to follow, the national guidelines or guidelines from other countries regarding CF and PCD patients. The CF learning network recommended following national guidelines throughout, but the wording changed over time, increasingly emphasizing individual judgment.
It varies between different parts of the country now. Stockholm is more affected. One also needs to make individual assessments. Generally, we don’t recommend staying home if one has CF and feels healthy. The CF doctors’ general position is that it varies for different patients. The way it is now, one should be meticulous in following the general recommendations that have been issued. Everyone should limit their contacts. (a54, w3)
Managing COVID-19 in the family
Participants needed guidance in managing suspected or diagnosed COVID-19 cases in the family. The questions reflected how people engaged in mental simulations of possible situations (e.g., “If one develops symptoms … ”). A concern arose about how to diagnose and differentiate CF or PCD symptoms from possible COVID-19 symptoms. For example, patients and family caregivers asked how they could make best use of self-tracking and COVID-19 testing and when and where they should seek care if they should suspect COVID-19. They also asked for practical advice on how to arrange their lives at home to prevent spread if someone in the family contracted COVID-19. The clinicians’ answers affirmed the expressed concerns, confirming the importance of isolation in principle but also acknowledging the difficulties of sufficiently isolating family members in practice.
It is not easy to provide very clear answers. You generally want to separate people who have been infected, and particularly in times like these. But it is difficult to entirely avoid each other in a family. Not all people have the option to live in two separate locations. The natural thing would be to keep them separate until one is completely free of symptoms during two consecutive days. But the most important thing is to be very careful with hand hygiene and do the best you can. (a69, w4)
Adjusting one’s planned care
Patients and family caregivers sought support in deciding about planned care visits and what to do when they needed treatment: “Should we still go to follow-up appointments now that the risk of being infected is high in our region, or is it better to stay home given the risk?” (q70, w2). The clinicians approached these questions by giving examples of how to think about planned care visits and by identifying leverage points in terms of new opportunities, such as telehealth.
As far as planned visits are concerned, also known as elective care, most larger hospitals have minimized their provision of elective care. Many visits will be canceled. If they are not, you should make a judgment as always, and if it is a follow-up you do every third year, you may be able to postpone it, but if it is a critical situation that needs follow-up, you should assess this and if uncertain, contact the clinic. As far as CF is concerned, we will shift to telephone visits to a large extent. Patients who need to start [intravenous therapy] or who need care at their CF center will be able to come. Not everything will be canceled, but a selection will be made based on how easily situations can be managed via telephone or video meetings. (a45, w3)
Replanning
About one in five questions (n = 36, 22%) concerned COVID-19’s effects on the organization and management of health care and social services at the population level.
Replanning chronic care management
Participants wondered how the CF centers replanned their treatment and follow-up routines to continue providing CF and PCD care without exposing patients to risks. Several of the questions concerned how to deal with more limited resources (e.g., due to increased focus on COVID-19, reallocation of clinicians to other parts of health care, or supply chain interruptions). Observations of what happened in other countries may have prompted some of the issues people raised. For example, one person asked, “Will transplantation assessments be discontinued? … In Italy, no lung transplantations are performed” (q98, w3). A particular concern among patients was the assurance of CF medication supply whereas clinicians were more concerned about the pressure on the health care system.
Should we stock up on medications at home, or will medications be available for some time to come?
For the time being, we don’t recommend stockpiling [of medications]. There are no signs yet that this is needed. What we are more worried about is that there will be a high pressure on the entire health care system at a later stage with many severely ill people. It is maybe not COVID-19 itself that is the biggest challenge; it is pressure on health care. We have developed plans for how this should be managed, but it could still be a challenge. (q27 and a7, w1)
Defining a COVID-19 health care strategy
Patients and family caregivers wanted to know about health care providers’ strategies for managing COVID-19. They wondered if CF and PCD patients would receive specialized services and prevention measures that differed from the services the general public received in terms of testing and treatment. Also, having direct access to their specialized care team was identified as important in case they needed to seek care urgently. Participants engaged in mental simulations about possible future scenarios and how they would manage them. Patients were worried as they did not know how they would be treated: “What counts as multimorbidity, and will our risk group have lower priority in care if the choice stands between a normal healthy person and a CF patient?” (q159, w5).
Refining health care policies
Patients and family caregivers asked why no specific guidelines or recommendations for risk groups had been established and made comparisons to other countries that recommended CF patients stay isolated rather than going to school or work. Several of the participants described their personal situations, specifically how they rearranged their daily life to work from home or took vacation to stay home to protect family members. Based on their narratives, they raised questions about the possibility of preventive sick leave and reimbursement policies to compensate for missing income due to absence from work. They also wanted to know how the Swedish CF Association worked with these questions and whether there was a dialogue with the National Board of Health and Welfare regarding the refinement of health care policies. The clinicians’ answers show that they actively engaged in sensegiving by developing informational material to enhance employers’, schools’, and authorities’ understanding of how to create safe environments.
We have developed a generic certificate that is available from the CF Association’s homepage. Individualized certificates will be developed depending on needs (e.g., for patients that are very sick in their CF/PCD). An information leaflet that will remind schools and employers about their responsibility for creating a safe working environment is currently being developed. (a19, w2)
We discussed this among the clinicians, and the CF Association will continue to collaborate with the clinicians to write a petition that will be sent to the government agencies next week. (a38, w3)
Discussion
Our study illustrates how the CF learning network contributed to collective sensemaking and sensegiving about COVID-19’s effects on everyday lives by providing new ways of interaction and responding with information, explanations, and action to questions that mattered to patients and family caregivers. We identified three primary macrocognitive functions: sensemaking, whereby people tried to understand the nature of COVID-19 and anticipate its impacts on self-care and health care; decision-making, whereby individuals sought support in making decisions about their everyday lives and self-care during the pandemic; and replanning, which concerned information needs about impacts on the organization and management of health care and social services (e.g., policies for financial compensation).
A macrocognitive perspective on collective sensemaking
Previous research highlights the importance of verbal and nonverbal communication for shared meaning construction (Keyton & Beck, Citation2010). Behaviors such as showing agreement, attentiveness, affective tone, and validating another’s identity have been identified as important when people share difficulties (e.g., in marriages and friendships; Koenig Kellas et al., Citation2013, Citation2021). Our study setting, in which participants were dislocated from each other and communicated through written messages and online webinars, was less suitable for studying how communicative behaviors shaped sensemaking. Nevertheless, online chronic care networks have also been identified as valuable resources for leveraging collective sensemaking through sharing of information and knowledge with others in similar health situations (Mamykina et al., Citation2015; Swan, Citation2009). Such networks gained particular importance during the pandemic, when opportunities for physical interaction were limited (Ihm & Lee, Citation2021). Our findings show that despite communicating in writing through short messages, patients and family caregivers shared personal narratives, and clinicians responded to these narratives by tailoring their answers to the situations that had been described. This communication shows how storytelling supported the construction of a shared understanding about difficulties related to COVID-19, in line with communicated narrative sensemaking theory (Koenig Kellas & Horstman, Citation2015). By analyzing the narratives from a macrocognitive perspective, we found that clinicians’ responses varied depending on the goals and concerns that patients and family caregivers raised. Clinicians responded by providing facts when the goal was to make sense; they provided tailored guidance and explanations when decision-making support was sought; and they developed information materials and action plans to support replanning. These results suggest that different communication strategies may be suitable for facilitating collective sensemaking and sensegiving that is driven by different goals and concerns.
Making sense of the nature of COVID-19
The study’s time span covered an inflection point in a disruptive change process in people’s lives. At the time of the first webinar, very few cases of COVID-19 had been diagnosed in Sweden; thereafter, the number of cases steadily increased (Public Health Agency of Sweden, Citation2021). The webinars provided a space in which uncertainties and risks related to the rapidly changing situation could be addressed on several occasions, allowing participants to update and expand their understanding collectively of the nature of COVID-19 and its impact on their chronic condition, self-care, and health care. Readdressing questions repeatedly shows that the CF learning network enabled adaptive sensemaking (Maitlis & Sonenshein, Citation2010), whereby they continuously updated and critically assessed their interpretations based on new information. Weick et al. (Citation2005) highlighted that apart from making sense of what is going on in a given situation (i.e., asking “What’s the story?”), another central aspect of sensemaking involves presumptions about the future (i.e., asking “Now what?”). Participants made presumptions about the future by embedding mental simulations and story-building in their questions and answers, which are macrocognitive processes commonly involved in sensemaking (Crandall et al., Citation2006).
Transforming general recommendations to individualized decisions
Decision-making was the most salient macrocognitive function that we identified in our data. Rasmussen (Citation1983) distinguished rule-based from knowledge-based decision-making: rule-based decision-making strategies are based on previous experiences, others’ knowledge, or problem solving on occasion. This type of strategy is commonly chosen for familiar situations. We found many examples of patients and family caregivers engaging in rule-based decision-making based on previous experiences of living with CF or PCD. The way patients and family caregivers framed questions and answers showed that they had experience preventing infections by avoiding situations of exposure. These experiences could be applied to navigate everyday situations during the pandemic. During unfamiliar situations, faced with an environment for which no knowledge or rules for control are available from previous encounters, decision-making must move to a higher conceptual level, in which decisions are goal-controlled and knowledge-based (Rasmussen, Citation1983). Examples of knowledge-based decision-making can be found in questions about testing and diagnostics for COVID-19 and when to seek care when previous rules did not apply. For example, it was difficult to distinguish COVID-19 from complications relating to respiratory symptoms caused by CF or PCD, which implies that prior intuitive conclusions about the possible cause of symptoms had to be reassessed.
Given that the Swedish public health response imposed few legal restrictions at the population level, individuals were trusted to determine how to act on a daily basis, which caused uncertainty and raised much concern and debate among scholars (Claeson & Hanson, Citation2021; Lindström, Citation2020). The CF learning network played an important role in reconciling conflicting rules when supporting decision-making about self-care. The clinicians helped interpret and tailor recommendations to specific contexts and conditions, thereby contributing to sensegiving. However, they were also transparent about their uncertainties and that recommendations needed to be interpreted with some flexibility (e.g., considering the severity of community spread in a local context). Our study does not provide any data on reasoning in the CF learning network regarding how to phrase their answers or how patients and family caregivers received the answers. Yet, research has shown that being open, frank, and honest is of central importance when one communicates with the public in crisis situations in which uncertainty is inevitable (Hyland-Wood et al., Citation2021).
Replanning of health care services and social support policies
The need for replanning was manifested in questions and concerns about COVID-19’s effects at the health care-system level. The management of risk groups in health care and the development of social support policies for reimbursing individuals financially if members had to stay at home were recurrent topics. The patients and family caregivers provided the clinicians insights about problems with existing policies and raised concerns about conflicts between the goals of chronic care management and the acute management of COVID-19. Although the presence of ill-defined and conflicting goals could pose challenges to replanning (Klein, Citation2007), the CF learning network identified leverage points for sensegiving. They engaged in dialogue with authorities to influence policy making. Additionally, they developed information and certificates that CF and PCD patients could use to inform their schools and employers about their specific needs. The CF learning network thus played a central role in responding to risk groups’ needs for tailored information and action, which could contribute to a more inclusive public health communication ecosystem that caters to the needs of vulnerable groups (Tagliacozzo et al., Citation2021).
Limitations and areas for future research
It has been argued that learning from real-world experience in challenging contexts, such as health care, is needed to explore sensemaking during the pandemic (Christianson & Barton, Citation2021). At the same time, performing a real-world study in a natural setting, we had to accept tradeoffs in the study design. We had no access to demographic information about the patients and family caregivers who participated in the online webinars. Not being able to describe the study population in detail makes determining the transferability to other settings challenging for readers. Further, our data may not have been expressive enough to capture fully how shared meaning was created (Keyton & Beck, Citation2010). In future research, we envision that a triangulation of data collection methods (e.g., adding observations and interviews) could help to identify more nuances in the macrocognitive functions and communication processes at play, thereby contributing to reach a deeper understanding of shared meaning construction. Nevertheless, we believe that the insights gained from this study may be of value for other chronic care settings where communities of practice (e.g., collaborative chronic care networks) have been established to support collective sensemaking and sensegiving in questions that concern self-care management, particularly when challenged by disruptive events.
Conclusions
Our findings suggest that the CF learning network played a central role in facilitating collective sensemaking by responding to various needs. The need to make sense was primarily addressed by communicating facts and providing updated information, the need for decision-making support regarding self-care behaviors was addressed by providing tailored guidance and explanations, and the need for replanned health care services and policies was addressed by developing tailored information materials and by providing schools, workplaces, and authorities suggestions, thus actively engaging in sensegiving. The CF learning network was an asset in supporting the public health response by acting as an information and knowledge broker in dialogue with various stakeholders. Future studies may further explore how different communication strategies can cater to various needs that are addressed in collective sensemaking.
Author contributions
Conceptualization, all authors; data curation, C.W.; methodology, C.W. and K.P.H.; investigation, C.W., K.P.H., and A.H.; formal analysis, C.W. and K.P.H.; visualization, C.W.; writing – original draft preparation, C.W., K.P.H., and H.H.; writing – review and editing, all authors; project administration, C.W.; funding acquisition, C.W., K.P.H, and H.H. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
The authors extend their gratitude to the Sweden Coalition CF, the CF community, and the Swedish CF Association for their valuable contribution to this research. Specifically, we thank Madeleine Grimhusen for assisting with the data collection and Åsa Silfverplatz for preparing and hosting the webinars together with A.H.
Disclosure statement
A.H. is a member of the CF learning network; he is a parent of children with CF and an eHealth entrepreneur engaged in developing the Genia patient support system and health information exchanges.
Additional information
Funding
References
- Abebe, E., Scanlon, M. C., Lee, K. J., & Chui, M. A. (2020). What do family caregivers do when managing medications for their children with medical complexity? Applied Ergonomics, 87, 103108. https://doi.org/10.1016/j.apergo.2020.103108
- Angeli, F., & Montefusco, A. (2020). Sensemaking and learning during the Covid-19 pandemic: A complex adaptive systems perspective on policy decision-making. World Development, 136, 105106. https://doi.org/10.1016/j.worlddev.2020.105106
- Bietti, L. M., Tilston, O., & Bangerter, A. (2019). Storytelling as adaptive collective sensemaking. Topics in Cognitive Science, 11(4), 710–732. https://doi.org/10.1111/TOPS.12358
- Bloem, B. R., Dorsey, E. R., & Okun, M. S. (2020). The coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurology, 77(8), 927–928. https://doi.org/10.1001/jamaneurol.2020.1452
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11(4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
- Chater, N. (2020). Facing up to the uncertainties of COVID-19. Nature Human Behaviour, 4(5), 439. https://doi.org/10.1038/s41562-020-0865-2
- Christianson, M. K., & Barton, M. A. (2021). Sensemaking in the time of COVID‐19. Journal of Management Studies, 58(2), 572–576. https://doi.org/10.1111/joms.12658
- Claeson, M., & Hanson, S. (2021). COVID-19 and the Swedish enigma. The Lancet, 397(10271), 259–261. https://doi.org/10.1016/S0140-6736(20)32750-1
- Coburn, C. E. (2001). Collective sensemaking about reading: How teachers mediate reading policy in their professional communities. Educational Evaluation and Policy Analysis, 23(2), 145–170. https://doi.org/10.3102/01623737023002145
- Crandall, B., Klein, G., & Hoffman, R. (2006). Working minds: A practitioner’s guide to cognitive task analysis. MIT Press.
- Danhieux, K., Buffel, V., Pairon, A., Benkheil, A., Remmen, R., Wouters, E., & van Olmen, J. (2020). The impact of COVID-19 on chronic care according to providers: A qualitative study among primary care practices in Belgium. BMC Family Practice, 21(1), 255. https://doi.org/10.1186/s12875-020-01326-3
- Dhukaram, A. V., & Baber, C. (2015). Modelling elderly cardiac patients decision making using cognitive work analysis: Identifying requirements for patient decision aids. International Journal of Medical Informatics, 84(6), 430–443. https://doi.org/10.1016/j.ijmedinf.2015.01.001
- Elborn, J. S. (2016). Cystic fibrosis. The Lancet, 388(10059), 2519–2531. https://doi.org/10.1016/S0140-6736(16)00576-6
- Farooqi, A. T., Snoek, F. J., & Khunti, K. (2021). Management of chronic cardiometabolic conditions and mental health during COVID-19. Primary Care Diabetes, 15(1), 21–23. https://doi.org/10.1016/j.pcd.2020.08.016
- Gilstrap, C. M. (2021). Organizational sensegiving in family-centered care: How NICU nurses help families make sense of the NICU experience. Health Communication, 36(13), 1623–1633. https://doi.org/10.1080/10410236.2020.1785373
- Gioia, D. A., & Chittipeddi, K. (1991). Sensemaking and sensegiving in strategic change initiation. Strategic Management Journal, 12(6), 433–448. https://doi.org/10.1002/smj.4250120604
- Guttman, N., & Lev, E. (2021). Ethical issues in COVID-19 communication to mitigate the pandemic: Dilemmas and practical implications. Health Communication, 36(1), 116–123. https://doi.org/10.1080/10410236.2020.1847439
- Hager, A., Lindblad, S., Brommels, M., Salomonsson, S., & Wannheden, C. (2021). Sharing patient-controlled real-world data through the application of the theory of commons: Action research case study. Journal of Medical Internet Research, 23(1), e16842. https://doi.org/10.2196/16842
- Häyry, M. (2021). The COVID-19 pandemic: Healthcare crisis leadership as ethics communication. Cambridge Quarterly of Healthcare Ethics, 30(1), 42–50. https://doi.org/10.1017/S0963180120000444
- Holden, R. J., Daley, C. N., Mickelson, R. S., Bolchini, D., Toscos, T., Cornet, V. P., Miller, A., & Mirro, M. J. (2020). Patient decision-making personas: An application of a patient-centered cognitive task analysis (P-CTA). Applied Ergonomics, 87, 103107. https://doi.org/10.1016/j.apergo.2020.103107
- Huzzard, T., Hellström, A., & Lifvergren, S. (2014). System-wide change in cancer care: Exploring sensemaking, sensegiving, and consent. In A. B. Shani & D. A. Noumair (Eds.), Research in organizational change and development (Vol. 22, pp. 191–218). Emerald Group Publishing Limited. https://doi.org/10.1108/S0897-301620140000022005
- Hyland-Wood, B., Gardner, J., Leask, J., & Ecker, U. K. H. (2021). Toward effective government communication strategies in the era of COVID-19. Humanities and Social Sciences Communications, 8(1), 30. https://doi.org/10.1057/s41599-020-00701-w
- Ihm, J., & Lee, C.-J. (2021). Toward more effective public health interventions during the COVID-19 pandemic: Suggesting audience segmentation based on social and media resources. Health Communication, 36(1), 98–108. https://doi.org/10.1080/10410236.2020.1847450
- Keyton, J., & Beck, S. J. (2010). Perspectives: Examining communication as macrocognition in STS. Human Factors: The Journal of the Human Factors and Ergonomics Society, 52(2), 335–339. https://doi.org/10.1177/0018720810371338
- Klein, G. (2007). Flexecution as a paradigm for replanning, part 1. IEEE Intelligent Systems, 22(5), 79–83. https://doi.org/10.1109/MIS.2007.4338498
- Klein, G. (2008). Naturalistic decision making. Human Factors: The Journal of the Human Factors and Ergonomics Society, 50(3), 456–460. https://doi.org/10.1518/001872008X288385
- Klein, H. A., & Lippa, K. D. (2012). Assuming control after system failure: Type II diabetes self-management. Cognition, Technology & Work, 14(3), 243–251. https://doi.org/10.1007/s10111-011-0206-3
- Klein, G., Ross, K. G., Moon, B. M., Klein, D. E., Hoffman, R. R., & Hollnagel, E. (2003). Macrocognition. IEEE Intelligent Systems, 18(3), 81–85. https://doi.org/10.1109/MIS.2003.1200735
- Koenig Kellas, J., Baker, J., Cardwell, M., Minniear, M., & Horstman, H. K. (2021). Communicated perspective-taking (CPT) and storylistening: Testing the impact of CPT in the context of friends telling stories of difficulty. Journal of Social and Personal Relationships, 38(1), 19–41. https://doi.org/10.1177/0265407520955239
- KoenigKellas, J., & Horstman, H. (2015). Communicated narrative sense-making: Understanding family narratives, storytelling, and the construction of meaning through a communicative lens. In L. H. Turner & R. West (Eds.), The SAGE handbook of family communication (pp. 76–90). SAGE Publications, Inc. https://doi.org/10.4135/9781483375366.n5
- Koenig Kellas, J., Morgan, T., Taladay, C., Minton, M., Forte, J., & Husmann, E. (2020). Narrative connection: Applying CNSM theory’s translational storytelling heuristic. Journal of Family Communication, 20(4), 360–376. https://doi.org/10.1080/15267431.2020.1826485
- Koenig Kellas, J., Willer, E. K., & Trees, A. R. (2013). Communicated perspective-taking during stories of marital stress: Spouses’ perceptions of one another’s perspective-taking behaviors. Southern Communication Journal, 78(4), 326–351. https://doi.org/10.1080/1041794X.2013.815264
- Kowalski, R. M., & Black, K. J. (2021). Protection motivation and the COVID-19 virus. Health Communication, 36(1), 15–22. https://doi.org/10.1080/10410236.2020.1847448
- LaDonna, K. A., Taylor, T., & Lingard, L. (2018). Why open-ended survey questions are unlikely to support rigorous qualitative insights. Academic Medicine, 93(3), 347–349. https://doi.org/10.1097/ACM.0000000000002088
- le May, A. (2008a). Generating patient capital: The contribution of storytelling in communities of practice designed to develop older people’s services. In A. le May (Ed.), Communities of practice in health and social care (pp. 95–106). John Wiley & Sons. http://ebookcentral.proquest.com/lib/bcu-trial/detail.action?docID=428209
- le May, A. (2008b). Introducing communities of practice. In A. le May (Ed.), Communities of practice in health and social care (pp. 1–16). John Wiley & Sons. http://ebookcentral.proquest.com/lib/ki/detail.action?docID=428209
- Lindström, M. (2020). The COVID-19 pandemic and the Swedish strategy: Epidemiology and postmodernism. SSM - Population Health, 11, 100643. https://doi.org/10.1016/j.ssmph.2020.100643
- Lippa, K. D., Klein, H. A., & Shalin, V. L. (2008). Everyday expertise: Cognitive demands in diabetes self-management. Human Factors: The Journal of the Human Factors and Ergonomics Society, 50(1), 112–120. https://doi.org/10.1518/001872008X250601
- Lucas, J. S., Burgess, A., Mitchison, H. M., Moya, E., Williamson, M., & Hogg, C. (2014). Diagnosis and management of primary ciliary dyskinesia. Archives of Disease in Childhood, 99(9), 850–856. https://doi.org/10.1136/archdischild-2013-304831
- Maitlis, S., & Sonenshein, S. (2010). Sensemaking in crisis and change: Inspiration and insights from Weick (1988). Journal of Management Studies, 47(3), 551–580. https://doi.org/10.1111/j.1467-6486.2010.00908.x
- Malterud, K., Siersma, V. D., & Guassora, A. D. (2016). Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research, 26(13), 1753–1760. https://doi.org/10.1177/1049732315617444
- Mamykina, L., Nakikj, D., & Elhadad, N. (2015). Collective sensemaking in online health forums. Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, 2015-April, 3217–3226. https://doi.org/10.1145/2702123.2702566
- Margolis, P. A., Peterson, L. E., & Seid, M. (2013). Collaborative chronic care networks (C3Ns) to transform chronic illness care. Pediatrics, 131(Suppl 4), S219–223. https://doi.org/10.1542/peds.2012-3786J
- Müller, J., Polansky, D., Novak, P., Foltin, C., & Polivaev, D. (2013). FreeMind (Version 1.0.1) [Computer Software]. GNU General Public License. http://freemind.sourceforge.net
- Nan, X., & Thompson, T. (2021). Introduction to the special issue on “Public health communication in an age of COVID-19”. Health Communication, 36(1), 1–5. https://doi.org/10.1080/10410236.2020.1853330
- Nazione, S., Perrault, E., & Pace, K. (2021). Impact of information exposure on perceived risk, efficacy, and preventative behaviors at the beginning of the COVID-19 pandemic in the United States. Health Communication, 36(1), 23–31. https://doi.org/10.1080/10410236.2020.1847446
- Papautsky, E. L., & Patterson, E. S. (2021). Patients are knowledge workers in the clinical information space. Applied Clinical Informatics, 12(01), 133–140. https://doi.org/10.1055/s-0041-1723022
- Patterson, E. S., & Hoffman, R. R. (2012). Visualization framework of macrocognition functions. Cognition, Technology & Work, 14(3), 221–227. https://doi.org/10.1007/s10111-011-0208-1
- Patterson, E. S., Su, G., & Sarkar, U. (2020). Reducing delays to diagnosis in ambulatory care settings: A macrocognition perspective. Applied Ergonomics, 82, 102965. https://doi.org/10.1016/j.apergo.2019.102965
- Public Health Agency of Sweden. (2020a, March 17). Lärosäten och gymnasieskolor uppmanas nu att bedriva distansundervisning [Higher education institutions and high schools are requested to perform distance education]. https://www.folkhalsomyndigheten.se/nyheter-och-press/nyhetsarkiv/2020/mars/larosaten-och-gymnasieskolor-uppmanas-nu-att-bedriva-distansundervisning/
- Public Health Agency of Sweden. (2020b, March 13). Ny fas kräver nya insatser mot covid-19 [New phase requires new measures against COVID-19]. https://www.folkhalsomyndigheten.se/nyheter-och-press/nyhetsarkiv/2020/mars/ny-fas-kraver-nya-insatser-mot-covid-19/
- Public Health Agency of Sweden. (2021, March 10). Bekräftade fall i Sverige – daglig uppdatering [Confirmed cases in Sweden - daily updates]. Retrieved March 29, 2021, from https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/bekraftade-fall-i-sverige/
- Rambaree, K., & Nässén, N. (2020). ‘The Swedish strategy’ to COVID-19 pandemic: Impact on vulnerable and marginalised communities. The International Journal of Community and Social Development, 2(2), 234–250. https://doi.org/10.1177/2516602620936048
- Rasmussen, J. (1983). Skills, rules, and knowledge; signals, signs, and symbols, and other distinctions in human performance models. IEEE Transactions on Systems, Man, and Cybernetics, SMC-13(3), 257–266. https://doi.org/10.1109/TSMC.1983.6313160
- Sawicki, G. S., Sellers, D. E., & Robinson, W. M. (2009). High treatment burden in adults with cystic fibrosis: Challenges to disease self-management. Journal of Cystic Fibrosis, 8(2), 91–96. https://doi.org/10.1016/j.jcf.2008.09.007
- Schubert, C. C., Denmark, T. K., Crandall, B., Grome, A., & Pappas, J. (2013). Characterizing novice-expert differences in macrocognition: An exploratory study of cognitive work in the emergency department. Annals of Emergency Medicine, 61(1), 96–109. https://doi.org/10.1016/j.annemergmed.2012.08.034
- Seid, M., Dellal, G., Peterson, L. E., Provost, L., Gloor, P. A., Fore, D. L., & Margolis, P. A. (2018). Co-designing a collaborative chronic care network (C3N) for inflammatory bowel disease: Development of methods. JMIR Human Factors, 5(1), 1–10. https://doi.org/10.2196/humanfactors.8083
- Shahid, Z., Kalayanamitra, R., McClafferty, B., Kepko, D., Ramgobin, D., Patel, R., Aggarwal, C. S., Vunnam, R., Sahu, N., Bhatt, D., Jones, K., Golamari, R., & Jain, R. (2020). COVID‐19 and older adults: What we know. Journal of the American Geriatrics Society, 68(5), 926–929. https://doi.org/10.1111/jgs.16472
- Swan, M. (2009). Emerging patient-driven health care models: An examination of health social networks, consumer personalized medicine and quantified self-tracking. International Journal of Environmental Research and Public Health, 6(2), 492–525. https://doi.org/10.3390/ijerph6020492
- Tagliacozzo, S., Albrecht, F., & Ganapati, N. E. (2021). International perspectives on COVID-19 communication ecologies: Public health agencies’ online communication in Italy, Sweden, and the United States. The American Behavioral Scientist, 65(7), 934–955. https://doi.org/10.1177/0002764221992832
- Tracy, S. J. (2010). Qualitative quality: Eight “Big-Tent” criteria for excellent qualitative research. Qualitative Inquiry, 16(10), 837–851. https://doi.org/10.1177/1077800410383121
- Weick, K. E., Sutcliffe, K. M., & Obstfeld, D. (2005). Organizing and the process of sensemaking. Organization Science, 16(4), 409–421. https://doi.org/10.1287/orsc.1050.0133
- Wenger, E., McDermott, R., & Snyder, W. M. (2002). Cultivating communities of practice: A guide to managing knowledge. Harvard Business School Press.
- Ziaian, T., Sawyer, M. G., Reynolds, K. E., Carbone, J. A., Clark, J. J., Baghurst, P. A., Couper, J. J., Kennedy, D., Martin, A. J., Staugas, R. E., & French, D. J. (2006). Treatment burden and health-related quality of life of children with diabetes, cystic fibrosis and asthma. Journal of Paediatrics and Child Health, 42(10), 596–600. https://doi.org/10.1111/j.1440-1754.2006.00943.x
