ABSTRACT
In recent years, research on issues such as health digitalization has been growing rapidly. This was partly caused by the COVID-19 pandemic and its growing burden on healthcare systems. In this study, we use a bibliometric approach to map the research dealing with digital innovations in the health sector, identify key research areas, and reveal knowledge gaps related to this emerging research topic. We conduct a bibliometric analysis of 151 papers from January 2010 to January 2023, indexed in the SCOPUS database using the R bibliometrix package and VOSviewer software. We find that, since 2010, there has been a huge increase in the number of publications, and the United States and the United Kingdom were the most influential knowledge centers for research collaboration on digital health. We identify four clusters of research themes: (1) IT and telemedicine, (2) digital technologies and mental health, (3) health digitalization resulting from the COVID-19 pandemic, (4) and digitalization, patients’ safety or resilience. Our contributions help to map the knowledge structure on digital innovation in health and to highlight unresolved issues, such as the social implications of digital health adoption. Social issues related to digital transformation of the health sector could provide future research directions.
Introduction
Scientific research on health-related issues has been growing rapidly in recent years, which to a large extent was caused by the COVID-19 pandemic and its growing burden on societies’ health and healthcare systems. Simultaneously, the COVID-19 outbreak has led to the rapid development of digital technologies and their adoption in all sectors, including health industries. A new term ‘digital health’ started to be used to describe the growing role of digitalization in the health-related sector. According to the World Health Organization, the digital health encompasses the use of information and communications technologies (ICT) to improve health. These technologies include the Internet of things, artificial intelligence, big data, blockchain and robotics. Digital health expands the concept of e-Health defined as the application of ICT in the cost-effective and secure way in health-related fields, including care services, health surveillance, health literature, and health research and education. Telemedicine means a remote delivery of healthcare services including diagnosis, treatment, prevention, education of healthcare workers, research and evaluation (WHO Citation2021, 39–46). Similar definition has a term ‘mobile health’ (mHealth) which means the use of wireless devices for the improvement of healthcare delivery, research and outcomes (Singh and Landman Citation2017). It also needs to be pointed out that e-Health is not only about technology but also about a state-of-mind focused on the improvements of health through the use of ICT (Eysenbach Citation2001).
To make the health system more flexible, increase its access to patients, and improve its efficiency, digital technologies have been implemented in the whole health sector, including treatment, prevention and clinical trials, as well as delivery of health services. E-health, mobile health, other digital health solutions and telemedicine have started to play a growing role for both health providers and patients, which caused intensification of research on the relationship between digitalization and health-related issues. The studies covered a variety of topics, such as digital health software development (e.g. Kokol, Kokol, and Zagoranski Citation2022; Msiska and Nielsen Citation2017), the impact of Internet and digitalization on health (e.g. Naslund et al. Citation2019; Rickard et al.), as well as research focused on selected countries (e.g. a study on Taiwan by Yuan et al. Citation2020 or the paper by Dutta, Gupta, and Sengupta Citation2019 on ICT adoption in the context of the health outcomes in selected Asian countries). Some papers analyzed various aspects of digital therapeutics (e.g. Sverdlov et al. Citation2018; Vedanthan et al. Citation2022); in particular, this theme became a hot topic during the COVID-19 pandemic (Capolongo et al. Citation2020; Egan Citation2020; Jovanovic et al. Citation2021). However, only a few studied covered a more complex issues encompassing a wide spectrum of aspects related to the process of digital transformation of health sector (e.g. Herrmann et al. Citation2018; Iyanna et al. Citation2022). Therefore, more cross-sectional research synthetizing findings from various disciplines are needed to explain this phenomenon. This paper offers an overview of the development of scientific literature published between January 2010 and January 2023 with regard to the relationship between digitalization and health. The main objective of this paper is to map the research field dealing with digital innovations in the health sector. We conducted a bibliometric analysis of publications in this area to identify streams of research, and the most influential papers that discuss digital innovative solutions in health.
This paper consists of six sections. These introductory remarks are followed by a literature review that sets the stage for our analysis. A methodological section comes next, explaining how the sample of relevant papers was selected for our analysis. Then results of our bibliometric analysis are presented in Section 4. Our analyses reveal the main trends in research on health digitalization measured by the publication output and geography of international collaboration as well as citations, and indicate the main research themes in this emerging field that may constitute the theoretical base for further studies on this topic. In Section 5, the thematic clusters distinguished through bibliometric analysis in the area of digitalization of health sector are discussed. Finally, the sixth section concludes and proposes future research avenues.
Literature review
The focus of this paper is the digitalization of health, in particular digital innovative solutions that have been introduced in the health system. This paper is of a multidisciplinary nature as it explores the intersection of the economics and management disciplines with health-related studies, in particular those studies that deal with management of health information, including needs in this respect. Therefore, this literature review offers an overview of the most important research results from various disciplines that cover digital innovation in health carried out from the perspective of economics and the management sciences. First, the notion of digital innovation in primary the health system needs to be explained, which refers to the general definition of innovation grounded in economic studies. It pinpoints novelty as a key element of this phenomenon, which may appear in a form of new products, production processes or markets, cutting-edge technologies as well as organization of activities in a novel way, and new business models (OECD/Eurostat Citation2018; Schumpeter Citation1934). All these elements are true when characterizing digital innovation in the health system; however, novelty refers here to digitalization, while the application of this novelty is narrowed down to the health sector. Digital innovation is seen in the literature as a result of acquiring, processing, and using information and knowledge through the adoption of automation, robotization, Internet of Things, cloud computing, big data analytics, or artificial intelligence (OECD Citation2019; Parida, Sjödin, and Reim Citation2019). These new digital technologies deployed in the health sector enable better access and more personalized health services (Planes-Satorra and Paunov Citation2019). Daher et al. (Citation2017) provide a wide definition of digital innovation in the health sector, pointing out that it is related to internet-enabled mobile health and other internet-based health interventions. A broader approach is presented by Egan (Citation2020), who underlines that digital innovative solutions in health sector mean the use of digital technologies in disease diagnosis, treatments and monitoring, as well as in health data analytics, accessing health care information, or health education. As Tromp et al. (Citation2022) point out, digital health innovations respond to the health system challenges faced by patients, healthcare providers and organizations collecting or processing health data.
However, the digital health innovations are not clearly conceptualized in the literature yet. There are a plethora of terms that are related to digitalization of health, i.e. digital health, e-health, mHealth, telemedicine, digital innovations in health, telemedicine, digital hospital and digital trial; however, they might not necessarily mean digital health innovations. The definitions of digital innovations in the health sector offered in the literature are either broad – trying to cover the whole spectrum of digital technologies as well as their applications in new products, processes and business models (Eysenbach Citation2001; Gleiss and Lewandowski Citation2022; WHO Citation2021) – or narrow. The latter ones focus only on a specific type of digital technology applied in the whole health sector or its one segment (e.g. study on big data by Giacalone et al. Citation2018) or various ICT components, such as web-based platforms, smartphone-based apps and so on mainly applied in health treatment (Anto-Ocrah et al. Citation2023). There are a growing number of studies related to specific types of treatment with the use of digital technologies. For example, digital health innovations, their advantages and barriers were discussed in cardiovascular disease (Tromp et al. Citation2022), cancer treatment (Anto-Ocrah et al. Citation2023; Di Giacomo et al. Citation2021; Patel et al. Citation2023) as well as COVID-19 and its further medical complications (Egan Citation2020).
The digitalization processes in the health system lead to digitally-driven transformation. Digital transformation is a multidimensional concept as it combines both technological and managerial aspects seen from various perspectives and is applied at the macro and micro levels (Kraft, Lindeque, and Peter Citation2022). In the health sector, digital transformation may occur in diagnostics, equipment development and healthcare delivery, as well as the administration and management of healthcare (Iyanna et al. Citation2022). The digital transformation requires agility, which enables one to respond faster and better to patients’ needs. However, the agile approach should go beyond digital health software development and become an agile culture covering ‘soft’ elements such as agile collaboration, decision making, technology adoption or sharing knowledge (Kokol, Kokol, and Zagoranski Citation2022).
The studies on digitalization of health cover various fields from diagnostics, medical equipment and software development through healthcare delivery, to healthcare management. It has been widely recognized that digitalization of the health sector might bring better health outcomes (Dutta, Gupta, and Sengupta Citation2019; Francombe et al. Citation2023; Planes-Satorra and Paunov Citation2019). The benefits for patients and healthcare providers include improvements in treatment, and cost reduction, facilitating access to medical services and thus, reducing health inequalities (Patel et al. Citation2023; Qoseem et al. Citation2024).
However, digital innovations in healthcare may face various challenges and barriers. A wide-ranging literature review of digital innovations implemented in response to the COVID-19 pandemic indicated technological, infrastructural financial, legal, ethical, and social barriers that limit the introduction of innovative digital solutions in the health sector (Francombe et al. Citation2023). These barriers were also indicated in the interviews with healthcare providers from the UK. For example, security issues were pointed out, including patients’ privacy, the risk of a system crash, vulnerability to cyberattacks (Iyanna et al. Citation2022). A similar picture was revealed in a detailed study on digitalization of hospitals (Gleiss and Lewandowski Citation2022). The barriers for digital innovation in hospitals include not only technological, organizational or financial challenges, but also structural and behavioral ones. Some of these stem from psychological features and insufficient knowledge of individuals, i.e. medical staff or patients that causes lack of acceptance of digital solutions. Fears and doubts may arise from missing social contact replaced by digital communications or may be a result of low perceived usefulness of digital technology.
To dig deeper and recognize future trends in digital health innovation development, it is necessary to know where these innovations are created, and what are the specific topics they refer to. This paper aims to broaden the knowledge in this area to facilitate implementation and diffusion of digital innovations in the health sector. This need can be addressed through the knowledge mapping of this research field.
The paper addresses the following research questions:
What are the current trends in the research and publication ecosystem related to digital innovation in the health sector?
What aspects of digital innovation in health are undertaken in research in various science fields, and what are the contexts of this research?
How is collaboration in research on digitalization in health sector developing?
What are the existing gaps in knowledge and future research directions for exploring this interesting topic?
Methodology and data
The research process started with a sample selection. We searched titles, abstracts and keywords of articles indexed in the SCOPUS database of scientific publications. SCOPUS a high-quality digital database of peer-reviewed scientific publications (scientific journals, books, and conference proceedings) covers more than 25,100 titles from more than 5000 international publishers from different fields.
In our search strategy, we used a set of the following keywords: ‘digital innovation’ and ‘health’ or ‘e-health’ or ‘telemedicine’ or ‘medicine’ or ‘online’ or ‘Internet of Things’ or ‘digital trial’ or ‘digital hospital’ or ‘digital health’ or ‘blockchain’ or ‘big data’ or ‘artificial intelligence’ or digital technology’ or ‘patient’ or ‘clinical’ or ‘treatment’. These keywords have been selected after the preliminary screening of the literature on digital health innovation and supplemented with relevant keywords selected from the glossary of the WHO report on Global strategy on digital health 2020–2025 (WHO Citation2021).
The dataset contained 1150 documents, and when limited to the years 2010–2023 (January 1), 1145 documents published in English were selected. To have a homogenous set of data we decided to focus only on scientific articles, which sized down our search results to 574 papers. In the next step, we selected those documents that belong to 13 science fields relevant for the characteristics of digital innovation in health, namely (as classified by SCOPUS database): 13 scientific disciplines: (1) Social Sciences; (2) Business, Management & Accounting; (3) Computer Science; (4) Medicine; (5) Engineering; (6) Economics, Econometrics & Finance; (7) Psychology; (8) Nursing; (9) Health Professionals; (10) Pharmacology, Toxicology & Pharmaceuticals; (11) Immunology & Microbiology; (12) Dentistry and (13) Neuroscience. As a result, the sample consisted of 527 articles. Given the broad scope of our search a filtering procedure was carried out. It required the reading of all abstracts. After content analysis of the abstracts, the papers that appeared to be not relevant to the topic were deleted, and the final sample included 151 articles. summarizes our data source and sample selection.
Table 1. Sample selection.
The dataset was analyzed using a bibliometric methodology, defined as the application of mathematical and statistical methods to analyze written communication (Pritchard Citation1969) such as articles, books and scientific manuscripts, as well as bibliographic citations and co-citations (Broadus Citation1987; Pendelbury Citation2010; Yalcin and Daim Citation2021).
When it comes to the use of bibliometrics in medical sciences, a historical review by Thompson and Walker (Citation2015) should be pointed out as one of first attempts to explain why and how this method can be applied. Bibliometrics is an interesting and useful method for health researchers as well as practitioners providing new information about health sciences trends, and thus having an impact on medical research (Kokol, Blažun Vošner, and Završnik Citation2021). Building on the findings of these historical bibliometrics analyses, we employed a bibliometric approach to study digital innovation applied in the health sector. Science mapping allows us to explore the structure and evolution of a focal research area.
We started with a keyword analysis, which allowed to identify the thematic foci of the papers included in our sample and to group them into clusters. Bibliographic coupling analysis was used to identify the connections between the articles in the sample, showing how they are networked. Co-citation analysis focuses on the references cited in the articles, bringing some insights regarding the most influential ones in the studied topic.
The software VOSviewer and the R language were used as tools to perform the analysis and to provide the visualization. In particular, R’s bibliometrix package helped isolate all papers citied within each of the 151 studies analyzed here. One major issue that we uncovered was the variety of styles within citations – from initials and periods to inadvertently omitted authors – that made any counts of identical papers unreliable. R’s functionality, including the package stringr, helped standardize these entries to the greatest extent possible.
Even then, this variation might cause count data to miss repetitions of a single paper. As an example, the most-cited paper listed below, with 10 entries, has listings ranging from 81 characters to 106 characters – more than a 30 percent difference. One additional entry adds a DOI to the 81-character string, bringing the total length to 121 characters. A naïve matching method would consider this to be a separate paper. Appendix Table 1 shows five examples of a single paper. The original entries vary by 47% (100–147 characters). Even after adjustment, the citations may still vary too much for simple software applications to flag them.
To avoid this problem, three strategies were applied. First, only initial strings were considered (the first 10 and/or 20 characters for each cited paper). Second, entries were sorted alphabetically and tested for matches with the preceding value. Third, visual matches were considered to capture any ‘missed’ duplicates. Using these approaches, the most highly cited papers within our set of studies can be identified and analyzed.
Results
Publication outputs
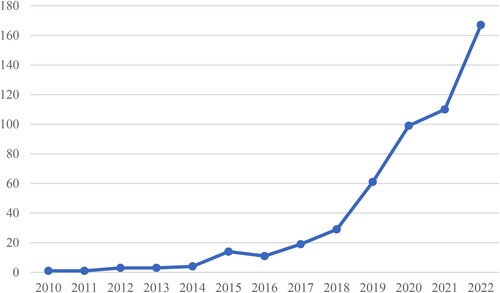
The analysis of the whole sample of 527 scientific articles published in 13 science fields relevant for digital innovation in health indicated that the number of scientific articles on digital innovation in health published in the years 2010–2022 has been growing, with a huge increase since 2018. The COVID-19 pandemic increased pressure to digitalize health industries (Weresa, Ciecierski, and Filus Citation2022). An increasing need for digital transformations in health is reflected in a fast growth of scientific publications in this area (), which during the years 2019–2022 reached on average 58% annually.
Figure 1. Papers published in the period of 1 January 2010-1 January 2023 (N = 527).
Source: Authors’ elaboration using the VOSviewer software.
Two countries are the world leaders in terms of the number of papers published on digital innovation in health sector, namely the United Kingdom (with the share of 13% in the total number of articles published in 2010–2022) and the United States (12%). Italy and Germany are next, having shares of around 7% each in the total set of publications in the analyzed period.
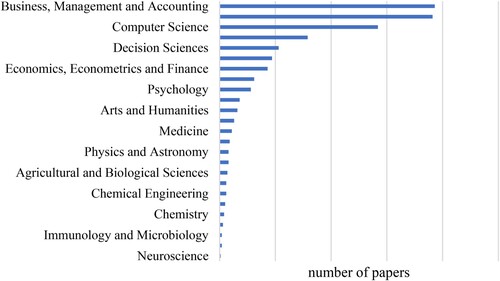
illustrates how the sample is divided by the field of science. The top three fields of science are Business, Management and Accounting, Computer Science, and Decision Science followed by Economics, Econometrics and Finance, and Psychology. The least frequent are papers that have been classified in Neuroscience and Immunology & Microbiology. These results need to be interpreted with caution at least for two reasons. First, the number of papers is higher than the sample as some papers are classified as multidisciplinary and belong to more than one field of science. Second, there are specific features of various fields of science. The results of the research on innovation (and digital innovation) in the field of Business and Management are published in scientific papers, while in Medicine, Neuroscience or Agriculture the research outcomes are either patented or published, which may limit the number of publications in these scientific areas in favor of patents.
Figure 2. Papers published in the period of 1 January 2010–1 January 2023 (N = 527) by research field.
Note: The research fields as defined by the SCOPUS database. The number of papers is higher than the sample as some papers are classified as multidisciplinary and belong to more than one field of science. Source: Authors’ elaboration.
Research collaboration
To measure collaboration in research in the area of digital innovation in health, we looked at the co-authorship of scientific articles on this topic. We employed the following research procedure, taking 5 as a minimum number of articles by country, which brought papers from 14 countries that met this threshold (out of the total 151 papers that were originated from 52 countries). For each of 14 countries, the strength of co-authorship with other countries was calculated. We took into account all countries with total link strength higher than 5, which resulted in the selection of 12 countries. Density of research collaboration among the 12 most important countries is presented on the left part of , while its right part shows networks strengths among these countries.
Figure 3. Density of research collaboration, 2010–2022 (n = 151). Source: Authors’ elaboration using VOSviewer software.
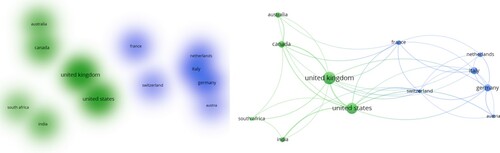
There are two broad clusters of countries that collaborate in the research on various topics related to digitalization in health. The first one is centered around the UK and the USA, and also includes Canada, Australia, South Africa and India. It can be named ‘the English-speaking block’ (in green in ). The second cluster consists of six Western European countries, with Germany and Switzerland playing the central role as they have the highest links strengths with authors from other countries. To this ‘European block’ led by Germany and Switzerland also belong the following countries: France Italy, Austria, and the Netherlands (all countries in blue on ). Both country blocks have some collaboration with each other, with the UK and the USA being the most important collaboration centers, followed by Germany (see right part of ).
Research topics and their clusters
This section aims to identify the most important research topics related to digital innovation in health. Employing the VOSviewer software tool for constructing bibliometric networks, we explored the co-occurrence of topics in the analyzed papers, taking into consideration three as the minimum number of occurrences of keywords. Of the 655 keywords, 37 met this threshold. Categorization of them into thematic blocks, using association strength as a criterion with 8 keywords as the minimum cluster size, allows identifying research fields that are associated with digital innovation in health (). The clusters of research hotspots were distinguished by distinct colors. There are three thematic areas where digital innovation/technology in health is studied.
Cluster I (blue), which combines research on digital innovation and information technologies in healthcare (telemedicine) and sustainability
Cluster II (red) consists of topics related to the COVID-19 pandemic that initiated the digital transformation of health care delivery
Cluster III (green), which is focused on digital health and contains papers that connect various types of digital technologies and innovation in health, such as big data, mobile health (mHealth) with mental health.
Figure 4. The most popular topics studied in the literature related to digital innovation and health.
Source: Authors’ elaboration using VOSviewer software.
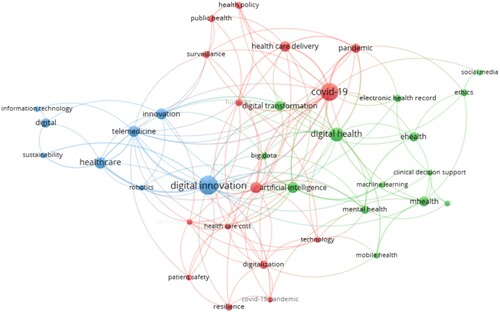
The first cluster looks at digital innovations in the heath sector through the lens of their application and impact. The types of digital innovations that have been often studied in the papers that belong this thematic cluster include digital platforms analyzed in various contexts, such as healthcare startups and entrepreneurship (Dong Citation2019), public–private partnership infrastructural investments (Moro Visconti and Morea Citation2020), or the collection and aggregation of health indicators (Msiska and Nielsen Citation2017). Other examples of digital innovation applied in the health sector are robots (Barrett et al. Citation2012; Jovanovic et al. Citation2021), digital telemedicine solutions (Downes, Horigan, and Teixeira Citation2019), or blockchain technology used for managing health records (Capece and Lorenzi Citation2020). The advantages of the implementation of these digital innovations found by scholars are improvements in patients’ satisfaction (Dong Citation2018; Moro Visconti and Morea Citation2020), cost reduction or revenue growth (Dong Citation2018; Downes, Horigan, and Teixeira Citation2019). However, there are also barriers, such as scarce resources for digital innovation (Msiska and Nielsen Citation2017) insufficient digital health literacy, or a lack of regulatory framework for using digital solutions.
The second thematic cluster is centered around the COVID-19 pandemic and its impact on health digitalization. The pandemic disrupted the health system and initiated its digital transformation (Capolongo et al. Citation2020). Digital technologies facilitate personalized therapy and treatment (Javaid et al. Citation2020) and enable constant real-time monitoring of availability of protective materials and pharmaceuticals (Yuan et al. Citation2020), which brings improvements in healthcare delivery. The COVID-19 crisis revealed that resilience remains the main challenge to healthcare systems, therefore appropriate strategies for healthcare design and its digitalization need to be developed and implemented (Capolongo et al. Citation2020).
The third thematic cluster can be characterized by the keyword ‘digital health’. The papers classified to this cluster focus on new treatments based on digital technologies. The examples are digital therapeutics (Sverdlov et al. Citation2018) or monitoring emotional changes with mobile apps (Rickard et al. Citation2016). Challenges in digital health implementation identified by scholars are related to inequities in access to e-health, insufficient involvement of patients in digital interventions and the risk of misuse of big data in health analyses (Naslund et al. Citation2019).
There are also interesting findings about the organizational aspects of digital health. Herrmann et al. (Citation2018) studied technological enablers, business models and value creation networks in digital transformation of health companies. It appeared that the company maturity has some important implications for the type of digital health innovations that the company introduces. Startups are more keen to create and implement disruptive digital health solutions and new digital business models than established corporations which rely more on incremental innovation supporting existing business models.
An in-depth discussion synthetizing our findings concerning these three thematic clusters is offered in the next section of this paper.
Most-cited papers
There are two possible ways to analyze citations. The first one to look how many times our sample papers have been cited. The second one is to look at references cited in our sample papers to find out what are the sources of knowledge that constitute a base for studying digital innovation in health.
The first approach allows to identify the most influential papers from our sample. By the end of 2022, 121 out of all 151 studies included in our sample had no citations, while the remaining 30 papers were cited 1284 times. The top 10 highly cited papers from our sample got 666 citations, of which 6 papers, cited more than 50 times each, had 583 citations. shows the top 10 most highly cited papers from our sample. One could expect that the themes related to digital innovation during the COVID-19 pandemic predominate among these highly cited papers, but unexpectedly, they relatively proportionally represent the thematic clusters identified and characterized in the previous sections of the paper. Two papers with the highest citation count were published nearly a decade ago, which to some extent may explain their impact, first because of the long period from the moment of their publishing, second because of the novelty of this topic at the time of publishing, which made them unique reference points at that time. The most cited paper is the study by Barrett at al., published in 2012, on the influence of robotics on 3 different occupational employed in hospital pharmacies (215 citations). The second in the ranking is the paper by Rich and Miah (Citation2014) with 89 citations, which explains expectations of digital health and shows how a public pedagogy approach can be used to mediate tensions that digital disruptive innovation may create in the health sector ().
Table 2. The top 10 highly cited papers on digital innovations in health sector.
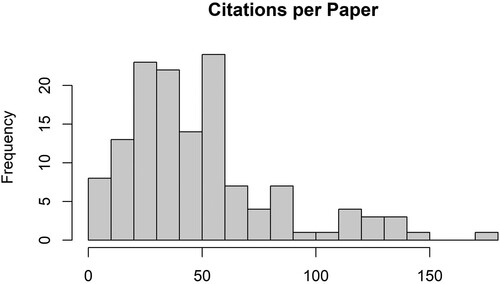
The second approach to the citation analysis focuses on the references used by the authors of papers in our sample, which could show the most influential studies. The 151 papers analyzed here have 7369 total citations. As might be expected, some papers have more citations than others. Counts range from a minimum of 1 to a maximum of 137; provides their distribution. The median citation count is 34 (mean 44.67), with a standard deviation of 31.23. Within this set of studies, many cited papers appear only once. Based on an examination of these total citations, we chose a threshold of four appearances of a single paper in our selection of the most-highly cited papers.
Figure 5. Distribution of citation counts across 151 papers. Mean = 44.67, median = 36, sd = 31.23, min = 1 max = 137.
Source: Authors’ elaboration.
shows the 15 papers that fall into this category. Over these, 1 appeared 10 times, while 11 appeared 4 times. It is interesting to note that the top two cited publications are books, which can applied to a wide range of analyses. One of the third-most-cited papers (with five occurrences) also serves a general audience. The other, by Greenhalgh et al., is a journal article. Studies with four appearances include three books and eight articles, with a mix of general topics and terms related to e-health. We are surprised, however, that there are no ‘essential references’ that were able to make their way into a larger proportion of the 151 studies analyzed here.
Table 3. Top-cited publications within 151 papers.
Discussion
Our bibliometric study of scientific literature on digital innovation in health published in English in the years 2010–2022 shows that since 2018 the number of papers has been rapidly growing. It can be explained by the progress in the fourth industrial revolution, which was initiated in the second decade of the twenty-first century (Santos et al. Citation2017; Schwab Citation2016). Digital technologies started to shape the innovation landscape in various sectors as they become general purpose technologies (Planes-Satorra and Paunov Citation2019). Digitalization of health industries was speeded up by the COVID-19 pandemic (Weresa, Ciecierski, and Filus Citation2022) as the impediments to accessing healthcare services became a huge problem around the globe. To address healthcare delivery challenges, digital health innovations, such as e-health, mobile health, telemedicine, digital health platforms, remote monitoring, etc. were scaled up and integrated with existing health systems. This rapid development was possible as the nature of innovation started to evolve already before the pandemic, in the beginning of the second decade of the twenty-first century, with information and communication technologies (ICT) and data playing important roles in discovering new solutions. Innovation processes shifted towards experimentation and personalization, innovation cycles become faster than in the past, with increasing importance of collaboration, partnerships, and data sharing (OECD Citation2019, 26–35).
This trend is also visible in the growing number of scientific papers on digitalization of healthcare systems and health-related industries published as collaborative works. The analysis of co-authorship revealed that the density of collaboration in research on health digitalization varies by country. Two groups of countries with relatively more intensive collaboration among group members in research on various topics related to digitalization in health were distinguished. These are ‘English-speaking block’ centered around the USA and the UK, and the ‘Continental Europe block’ with Germany and Switzerland as core members. Authors from both groups of countries have also some collaboration with the other group members, and the UK, the USA and Germany serve as the key collaboration centers.
These findings inspire us to figure out which factors can explain this geographical pattern of the collaboration. It is also interesting to explain the minor role in research collaborative works on digital innovation played by innovation leaders from Asia, namely Japan, South Korea and China. The latter of these is an emerging innovator catching up fast with the leaders (Hollanders, Es-Sadki, and Khalilova Citation2022). It appeared that these Asian countries, although relatively strong in terms of innovation, have total link strength of research collaboration in the field of digital health lower than 5. This result means that the joint research on health digitalization conducted by researchers from these countries with researchers from other countries appears relatively less frequently than co-authorship of researchers from the 12 countries indicated above in , which are the most collaborative in this field (i.e. the USA, the UK, Germany, Switzerland, India, South Africa, Australia, Canada, France, Italy, the Netherlands and Austria).
These trends in the geography of research collaboration can be explained by the proximity factors that are regarded as key determinants of R&D collaboration. Various proximity dimensions are widely explained in the literature (e.g.: Balland, Boschma, and Frenken Citation2015; Boschma Citation2005; Boschma and Frenken Citation2010; Cao, Derudder, and Peng Citation2019). In particular, these are institutional, social and cultural proximities (including language and psychological distance), which, to some extent, are a result of a common historical heritage of the collaborating countries. Since we studied in this paper digital innovations, it is also necessary to have a closer look at technological proximity and its role in enhancing research collaboration. Technological proximity refers to technological experiences and knowledge shared by collaborating partners (Knoben and Oerlemans Citation2006) and is based on the concept of absorptive capacity. This facilitates knowledge acquisition, transformation and integration (Vasconcelos et al. Citation2019) leading to improvements in innovation performance (Sancho-Zamora et al. Citation2022). However, when looking at the geographical pattern of collaboration in research on digital innovation in health, it can be noted that countries that belong to each of the two collaborating centers differ in terms of the dynamics of digital technologies’ development.
The data collected by the OECD (Citation2020) on the volumes of patents granted in ICT-related technologies embodied in products or processes that bring novel technical solutions can offer an indication of the innovation activity in this area. This data can also explain the differences in involvement of Asian innovation leaders and emerging innovators in collaborative research on health digitalization. Over the period from 2014 to 2017, China and South Korea were the world’s leaders in patenting in ICT-related technologies. In China, the volume of these patents increased significantly (by one-fifth), making this country’s IP5 patent portfolio the most specialized in ICT. During the same period, the share of ICT-related patents in India more than doubled and the country occupied the seventh position in terms of patenting in ICT (OECD Citation2020). While the latter (i.e. India) has been involved in research collaboration on digital innovation in health, the two other Asian countries (i.e. China and South Korea) are not that strongly involved in sharing knowledge in this area through collaboration. This may reflect to some extent a different approach to science openness in these countries, however, further research is required to confirm this tentative conclusion. Another explanation for this trend might be related to the level of novelty of ideas related to digital solutions and their importance for this research field measured by the citations of relevant papers. A comparison of countries in terms of the percentage of domestic documents (fractional counts) in the top 10% citation-ranked documents in computer science based on the data by the OECD (Citation2020) indicates that all Asian countries analyzed above have lower percentages in comparison with both:
the same indicators calculated for the remaining countries that collaborate intensively in research on health digitalization, regardless the group they belong (either ‘English-speaking’ or ‘European’)
the citation rate of all publications (excluding computer science) in top 10% cited documents.
This may indicate that the ideas presented in these papers are not that impactful for the whole research field, which might be reflected a relative lower involvement in research collaboration with other countries.
When it comes to the thematic content of the publications related to digital innovation in health, based on the combination of quantitative methods and qualitative content analysis we found three thematic clusters. A more detailed discussion helps to explain the state of art of the literature in these fields. Cluster I focuses on the characteristics of information technologies and telemedicine reflecting various types of digital innovation. This theme mainly reflects the ‘pure’ creation and application of digital innovations or technologies. The growing number of papers related to this theme shows that digital innovations in the health sector (such as delivery systems or the development and widespread application of new technologies) will be an emerging topic for research. Papers that belong to Cluster II center around the COVID-19 pandemic, which was an ‘exogenous shock’ that hastened the adoption of digital technologies. As a result, digital innovations were more quickly scaled up and implemented. We also realize that ‘COVID papers’ have been popular in academia, and the appearance of such thematic cluster reflects this trend. Cluster III captures the societal implications of digital transformation in health. In particular, Cluster III details the types and scope of these various technologies, such as Big Data or mHealth and covers the issues related to mental health changes caused by digitalization. It also includes cost and safety considerations related to digitalization of health. These themes can be considered as a third step in the logic of innovation – adoption – implication process. In short, the clusters identified in this analysis accurately capture three separate themes studied so far in the literature. They are related to (1) digital technology, its creation and development (Cluster I); (2) the adoption of digital innovations leading to digital transformation of the health sector which was speeded up by the COVID-19 pandemic (Cluster II); (3) the societal implications of health digitalization (Cluster III). Additional research might be able to identify each in detail.
As we also found that there were no ‘essential references’ that were cited in a larger proportion of the 151 studies analyzed here. It should be pointed out however, that among the top 15 publications cited in the articles we studied, 5 are books, of which the book by Rogers (Citation2003) on diffusion of innovations got the highest number of citations. The second is the book by Christensen, Grossman, and Hwang (Citation2009), which reviews the concept of disruptive innovation and applies it to healthcare. The two remaining highly cited books (Osterwalder and Pigneur Citation2010; Patton Citation1990) are of a methodological nature dealing with qualitative research. There are also some other methodologically-oriented articles in the set of highly refereed publications. Another group of references include general papers dealing with digital transformation or innovation (e.g. ; Kohli and Melville Citation2019; Nambisan Citation2017; Vial Citation2019) and do not focus on digital health. There are only two articles among the top 15 highly cited studies, both published in the Journal of Medical Internet Research, that made attempts to explain digital innovation in health, but they do not have many citations yet. These are: a paper by Greenhalgh et al. Citation2017 (5 cites) and an editorial by Eysenbach Citation2001 (4 cites).
Therefore, bearing in mind that majority of publications cited in the 151 studies analyzed here are either general innovation studies or methodological ones, we can hypothesize that the concept of digital innovation in health being a recently emerging field of research has been under development. It seems that here is no sound theoretical basis yet that could fully explain the concept of digital innovation in health, as it is a complex phenomenon appearing in various parts of the health sector ranging from healthcare services to pharmaceutical goods. We suggest an interdisciplinary approach to explore this field that integrates economics and business studies with medical and pharma science.
Conclusion and future research directions
This paper is a knowledge mapping study, which focuses on the body of research dealing with digital innovations in the health sector. Given a growing number of studies showing how digital innovations are applied in the health sector, as well as wide spectrum of potential areas of digital technologies applications (healthcare services, i.e. diagnosis, treatment, prevention, communication with patients; health administration; health education; research on health-related issues; healthcare management; evaluation of the health system; collection and analysis of health data; digitally-driven transformations of medical equipment; digital business models of healthcare companies etc.), there is a need to deliver a framework for organizing observations and studies on this topic to combine different characteristics or particulars of digital health innovations. A mapping of relevant literature from various disciplines offered in our paper is a first step in this process. To identify key research areas and reveal knowledge gaps in this recently emerging research topic, we analyzed the most relevant papers selected from the SCOPUS database using a set of keywords that reflect digitalization of the health sector.
We conducted a bibliometric analysis of the selected 151 papers using the R bibliometrix package and the VOSviewer software. We identified two geographical knowledge centers of research collaboration on digital innovation in health with the USA and the UK being two core countries leading in collaborative research on this topic.
In the 151 papers analyzed, over 7000 publications have been cited, but only 4 publications had 5 cites or more, with 10 being a maximum number of citations. Studies with four appearances include four books and seven articles, with a mix of general topics and terms related to innovation, digital transformation and research methodology. It is surprising that there are no highly cited key references on health digitalization that were able to make their way into a larger proportion of the 151 studies analyzed here. It may indicate that health digitalization has become an emerging topic quite recently and the theoretical base to study this topic is still under development. Studies on health digitalization started to be published more intensively during the COVID-19 pandemic. In 2017, there were only 19 papers listed in the SCOPUS database on digital health, while in 2022 there were already 167 papers; therefore it is too early to expect huge number of citations in such a short period as the topic is new. Furthermore, is should be noted that our sample covered papers from 13 scientific disciplines, so one cannot expect such intensive references across the disciplines.
We identified three clusters of research themes explored so far in the analyzed bunch of papers. The first cluster is related to IT and telemedicine and identifies the types of digital technologies. Another cluster captures the COVID-19 pandemic as an ‘exogenous shock’ that hastened health digitalization. The remaining cluster tackles other issues of health digitalization, including patients’ safety or resilience.
There are implications of our findings for both theory and practice. First, our findings bring the attention of scholars, research funding organizations and practitioners to the digitalization of health sector being an emerging field of research as the number of publications on this topic have been growing rapidly in recent years. Furthermore, our study indicates that some important issues need more attention in medical practice. In particular, our findings, which pinpoint three clusters of research themes on digital innovation in the health sector, might be interesting for scholars and research funding organizations when designing, financing, and conducting further research. It seems that further research on digital transformation of the health sector regardless the scientific discipline should include sustainability issues, ethics and patients’ safety. Our study also indicates that mental health is another new area that gained high importance in the context of digital health development. This finding has some implications for organizations and medical practitioners in the process of healthcare delivery as well as for policy makers as these groups should address mental health issues related to digital healthcare and mitigate it.
Second, the concentration of collaboration networks of scholars involved in publishing jointly on this topic in a few locations implies that theoretical considerations of scientific centers of excellence might also be considered and further studied in this context. Information what geographical locations produce knowledge and intensively collaborate in research on digital health may be useful for organizations that finance research in this field, as well as for scholars who explore this topic and seek for research partners.
Third, various facets of digital innovations discussed here seem to be related to the type of digital technology adopted in healthcare and maturity of health organizations. This finding has some policy implications. Digital transformation of the heath sector may be speeded with innovation policy, which incentivizes companies from the health sector to match available digital technologies with patients’ needs and digital health literacy. The focus should be not only on the development of specific digital health interventions, but also on increasing awareness of patients and citizens and initiating the dialogue for shaping the future of digital healthcare as well as on increasing digital skills that are necessary to reap the benefits of digital innovations in the health sector.
Our contributions pertain to map the knowledge structure of this emerging field of research and to highlight unresolved issues, such as social, ethical and psychological implications of digital health adoption. In particular, mental health is one of such hot themes related to digital innovation in the health sector that we identified. These issues could be future research directions on digital innovation in the area of health.
There is a diverse set of approaches to this theme ranging from medical sciences to economics and management. Our mapping of the literature is the first attempt to conduct research on digital health innovation that combines findings from different disciplines. It could help to create a framework to further explain this phenomenon, develop it into a concept and prepare a typology by various areas of application across different digital technologies.
The future research also could focus more on the differences in involvement of various countries in collaborative research on health digitalization comparing the pattern we revealed with the science systems of these countries. Further explorative studies may be conducted to explain the collaboration pattern at institutional and authors levels. Another study could focus on exploring in more detail the thematic areas we identified in the research conducted so far.
This study is of exploratory nature, therefore it is not free from some potential limitations. Despite the adoption of a rigorous bibliometric methodology, one limitation may lie in the focus on peer-reviewed papers. To guarantee homogeneity and allow for comparisons, the analysis has not considered books and conference proceedings. Another issue is the use of one database of scientific publications, i.e. SCOPUS. This type of research can be repeated using data from other databases, such as Web of Science, ProQuest, etc. Last but not least, bibliometric analysis offers a science map that allows for the identification of key thematic threads. It does not cover other issues such as the impact of the selected publications on the studied area or research methodology analysis. These are undoubtedly potential research themes that could be undertaken in the future.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anto-Ocrah, M., M. Asiedu, S. Rao, L. DeSplinter, and S. Hollenbach. 2023. “If You Build It, They Will Come … or Not. Considerations for Women’s Health in the Post-Pandemic Era of Digital Innovation.” Frontiers in Public Health 11:1–7. https://doi.org/10.3389/fpubh.2023.1228212.
- Balland, P.-A., R. Boschma, and K. Frenken. 2015. “Proximity and Innovation: From Statics to Dynamics.” Regional Studies 49 (6): 907–920. https://doi.org/10.1080/00343404.2014.883598.
- Barrett, M., E. Oborn, W. J. Orlikowski, and J. Yates. 2012. “Reconfiguring Boundary Relations: Robotic Innovations in Pharmacy Work.” Organization Science 23 (5): 1448–1466. https://doi.org/10.1287/orsc.1100.0639.
- Boschma, R. A. 2005. “Proximity and Innovation: A Critical Assessment.” Regional Studies 39 (1): 61–74. https://doi.org/10.1080/0034340052000320887
- Boschma, R., and K. Frenken. 2010. “The Spatial Evolution of Innovation Networks: A Proximity Perspective.” In The Handbook of Evolutionary Economic Geography, edited by R. Boschma and R. Martin, 20–137. Northampton, MA: Edward Elgar Publishing.
- Broadus, R. N. 1987. “Toward a Definition of “Bibliometrics”.” Scientometrics 12 (5–6): 373–379. https://doi.org/10.1007/BF02016680.
- Cao, Z., B. Derudder, and Z. Peng. 2019. “Interaction Between Different Forms of Proximity in Inter-Organizational Scientific Collaboration: The Case of Medical Sciences Research Network in the Yangtze River Delta Region.” Papers in Regional Science 98 (5): 1903–1925. https://doi.org/10.1111/pirs.12438.
- Capece, G., and F. Lorenzi. 2020. “Blockchain and Healthcare: Opportunities and Prospects for the EHR.” Sustainability 12 (22): 9693. https://doi.org/10.3390/su12229693.
- Capolongo, S., M. Gola, A. Brambilla, A. Morganti, E. I. Mosca, and P. Barach. 2020. “COVID-19 and Healthcare Facilities: A Decalogue of Design Strategies for Resilient Hospitals.” Acta Bio-Medica 91 (9-S): 50–60. https://doi.org/10.23750/abm.v91i9-S.10117.
- Christensen, C., J. Grossman, and J. Hwang. 2009. The Innovator’s Prescription. New York: McGraw-Hill.
- Daher, J., R. Vijh, B. Linthwaite, S. Dave, J. Kim, K. Dheda, T. Peter, and N. P. Pai. 2017. “Do Digital Innovations for HIV and Sexually Transmitted Infections Work? Results From a Systematic Review (1996-2017).” BMJ Open 7 (11): e017604. http://doi.org/10.1136/bmjopen-2017-017604.
- Di Giacomo, D., F. Guerra, K. Cannita, A. Di Profio, and J. Ranieri. 2021. “Digital Innovation in Oncological Primary Treatment for Well-Being of Patients: Psychological Caring as Prompt for Enhancing Quality of Life.” Current Oncology 28 (4): 2452–2465. https://doi.org/10.3390/curroncol28040224.
- Dong, J. Q. 2019. “Moving a Mountain With a Teaspoon: Toward a Theory of Digital Entrepreneurship in the Regulatory Environment.” Technological Forecasting and Social Change 146:923–930. https://doi.org/10.1016/j.techfore.2018.07.050.
- Downes, E., A. Horigan, and P. Teixeira. 2019. “The Transformation of Health Care for Patients.” Journal of the American Association of Nurse Practitioners 31 (3): 156–161. https://doi.org/10.1097/jxx.0000000000000109.
- Dutta, U. P., H. Gupta, and P. P. Sengupta. 2019. “ICT and Health Outcome Nexus in 30 Selected Asian Countries: Fresh Evidence From Panel Data Analysis.” Technology in Society 59:101184. https://doi.org/10.1016/j.techsoc.2019.101184.
- Egan, K. 2020. “Digital Technology, Health and Well-Being and the Covid-19 Pandemic: It’s Time to Call Forward Informal Carers From the Back of the Queue.” Seminars in. Oncology Nursing 36 (6): 151088. https://doi.org/10.1016/j.soncn.2020.151088.
- Eisenhardt, K. M. 1989. “Building Theories from Case Study Research.” The Academy of Management Review 14 (4): 532–550. https://doi.org/10.2307/258557.
- Eysenbach, G. 2001. “What Is e-Health?” Journal of Medical Internet Research 3 (2): e20. https://doi.org/10.2196/jmir.3.2.e20.
- Francombe, J., G. C. Ali, E. R. Gloinson, C. Feijao, K. I. Morley, S. Gunashekar, and H. de Carvalho Gomes. 2023. “Assessing the Implementation of Digital Innovations in Response to the COVID-19 Pandemic to Address Key Public Health Functions: Scoping Review of Academic and Nonacademic Literature.” JMIR Public Health and Surveillance 8 (7): e34605. https://doi.org/10.2196/34605.
- Giacalone, M., C. Cusatelli, A. Romano, A. Buondonno, and V. Santarcangelo. 2018. “Big Data and Forensics: An Innovative Approach for a Predictable Jurisprudence.” Information Sciences 426: 160–170.
- Gleiss, A., & Lewandowski, S. (2022). Removing Barriers for Digital Health Through Organizing Ambidexterity in Hospitals. Journal of Public Health: From Theory to Practice, 30, 21–35. https://doi.org/10.1007/s10389-021-01532-y.
- Greenhalgh, T., J. Wherton, C. Papoutsi, J. Lynch, G. Hughes, C. A’Court, S. Hinder, N. Fahy, R. Procter, and S. Shaw. 2017. “Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies.” Journal of Medical Internet Research 19 (11): e367. https://doi.org/10.2196/jmir.8775.
- Herrmann, M., P. Boehme, T. Mondritzki, J. P. Ehlers, S. Kavadias, and H. Truebel. 2018. “Digital Transformation and Disruption of the Health Care Sector: Internet-Based Observational Study.” Journal of Medical Internet Research 20 (3): e104. https://doi.org/10.2196/jmir.9498.
- European Commission, Directorate-General for Research and Innovation, Hollanders, H., N. Es-Sadki, and A. Khalilova. 2022. European Innovation Scoreboard 2022. Luxembourg: Publications Office of the European Union. https://data.europa.eu/doi/10.2777309907.
- Iyanna, S., P. Kaur, P. Ractham, S. Talwar, and N. A. K. M. Islam. 2022. “Digital Transformation of Healthcare Sector. What is Impeding Adoption and Continued Usage of Technology-Driven Innovations by End-Users?” Journal of Business Research 153:150–161. https://doi.org/10.1016/j.jbusres.2022.08.007.
- Javaid, M., A. Haleem, R. P. Singh, M. I. U. Haq, A. Raina, and R. Suman. 2020. “Industry 5.0: Potential Applications in COVID-19.” Journal of Industrial Integration and Management 5 (4): 507–530. https://doi.org/10.1142/s2424862220500220.
- Jovanovic, K., A. Schwier, E. Matheson, M. Xiloyannis, E. Rozeboom, N. Hochhausen, B. Vermeulen, et al. 2021. “Digital Innovation Hubs in Health-Care Robotics Fighting COVID-19: Novel Support for Patients and Health-Care Workers Across Europe.” IEEE Robotics & Automation Magazine 28 (1): 40–47. https://doi.org/10.1109/mra.2020.3044965.
- Knoben, J., and L. A. G. Oerlemans. 2006. “Proximity and Inter-Organizational Collaboration: A Literature Review.” International Journal of Management Reviews 8 (2): 71–89. https://doi.org/10.1111/j.1468-2370.2006.00121.x.
- Kohli, R., and N. P. Melville. 2019. “Digital Innovation: A Review and Synthesis.” Information Systems Journal 29 (1): 200–223. https://doi.org/10.1111/isj.12193.
- Kokol, P., H. Blažun Vošner, and J. Završnik. 2021. “Application of Bibliometrics in Medicine: A Historical Bibliometrics Analysis.” Health Information & Libraries Journal 38 (2): 125–138. http://doi.org/10.1111/hir.v38.2.
- Kokol, P., M. Kokol, and S. Zagoranski. 2022. “Machine Learning on Small Size Samples: A Synthetic Knowledge Synthesis.” Science Progress 105 (1): 1–16. https://doi.org/10.1177/00368504211029777.
- Kraft, C., J. P. Lindeque, and M. K. Peter. 2022. “The Digital Transformation of Swiss Small and Medium-Sized Enterprises: Insights From Digital Tool Adoption.” Journal of Strategy and Management 15 (3): 468–494. https://doi.org/10.1108/JSMA-02-2021-0063.
- Moro Visconti, R., and D. Morea. 2020. “Healthcare Digitalization and Pay-for-Performance Incentives in Smart Hospital Project Financing.” International Journal of Environmental Research and Public Health 17 (7): 2318. https://doi.org/10.3390/ijerph17072318.
- Msiska, B., and P. Nielsen. 2017. “Innovation in the Fringes of Software Ecosystems: The Role of Socio-Technical Generativity.” Information Technology for Development 24 (2): 398–421. https://doi.org/10.1080/02681102.2017.140093.
- Nambisan, S. 2017. “Digital Entrepreneurship: Toward a Digital Technology Perspective of Entrepreneurship.” Entrepreneurship Theory and Practice 41 (6): 1029–1055. https://doi.org/10.1111/etap.12254.
- Naslund, J. A., P. P. Gonsalves, O. Gruebner, S. R. Pendse, S. L. Smith, A. Sharma, and G. Raviola. 2019. “Digital Innovations for Global Mental Health: Opportunities for Data Science, Task Sharing, and Early Intervention.” Current Treatment Options in Psychiatry 6 (4):337–351. https://doi.org/10.1007/s40501-019-00186-8.
- OECD. 2019. Digital Innovation: Seizing Policy Opportunities. Paris: OECD Publishing. https://doi.org/10.1787/a298dc87-en
- OECD. 2019. Measuring the Digital Transformation: A Roadmap for the Future. Paris: OECD Publishing. https://doi.org/10.1787/9789264311992-en.
- OECD. 2020. OECD Digital Economy Outlook 2020. Paris: OECD Publishing. https://doi.org/10.1787/bb167041-en.
- OECD/Eurostat. 2018. Oslo Manual 2018: Guidelines for Collecting, Reporting and Using Data on Innovation, 4th Edition, The Measurement of Scientific, Technological and Innovation Activities. Paris/Eurostat, Luxembourg: OECD Publishing. https://doi.org/10.1787/9789264304604-en.
- Osterwalder, A., and Y. Pigneur. 2010. Business Model Generation: A Handbook for Visionaries, Game Changers, and Challengers. Hoboken, NJ: John Wiley & Sons.
- Parida, V., D. Sjödin, and W. Reim. 2019. “Reviewing Literature on Digitalization, Business Model Innovation, and Sustainable Industry: Past Achievements and Future Promises.” Sustainability 11 (2): 391. https://doi.org/10.3390/su11020391.
- Patel, S., J. C. Goldsack, G. Cordovano, A. Downing, K. K. Fields, C. Geoghegan, U. Grewal, et al. 2023. “Advancing Digital Health Innovation in Oncology: Priorities for High-Value Digital Transformation in Cancer Care.” Journal of Medical Internet Research 25: e43404. https://doi.org/10.2196/43404.
- Patton, M. Q. 1990. Qualitative Evaluation and Research Methods. Washington, DC: Sage Publications, Inc.
- Pendelbury, D. A. 2010. White Paper. Using Bibliometrics in Evaluating Research. Toronto: Thomson Reuters.
- Planes-Satorra, S., and C. Paunov. 2019. “The Digital Innovation Policy Landscape in 2019.” OECD Science and Innovation Policy Papers 71: 1–55.
- Pritchard, A. 1969. “Statistical Bibliography or Bibliometrics.” Journal of Documentation 25:348–349.
- Qoseem, I. O., O. J. Okesanya, N. O. Olaleke, B. M. Ukoaka, B. O. Amisu, J. B. Ogaya, and D. E. Lucero-Prisno III. 2024. “Digital Health and Health Equity: How Digital Health Can Address Healthcare Disparities and Improve Access to Quality Care in Africa.” Health Promotion Perspectives 14 (1): 3–8. https://doi.org/10.34172/hpp.42822.
- Rich, E., and A. Miah. 2014. “Understanding Digital Health as Public Pedagogy: A Critical Framework.” Societies 4 (2): 296–315. https://doi.org/10.3390/soc4020296.
- Rickard, N., H. Arjmand, D. Bakker, and E. Seabrook. 2016. “Development of a Mobile Phone app to Support Self-Monitoring of Emotional Well-Being: A Mental Health Digital Innovation.” JMIR Mental Health 3 (4): e49. https://doi.org/10.2196/mental.6202.
- Rogers, E. 2003. Diffusion of Innovations. 5th ed. New York: Free Press.
- Sancho-Zamora, R., F. Hernández-Perlines, I. Peña-García, and S. Gutiérrez-Broncano. 2022. “The Impact of Absorptive Capacity on Innovation: The Mediating Role of Organizational Learning.” International Journal of Environmental Research and Public Health 19 (2): 842. https://doi.org/10.3390/ijerph19020842.
- Santos, C., A. Mehrsai, A. C. Barros, M. Araújo, and E. Ares. 2017. “Towards Industry 4.0.: An Overview of European Strategic Roadmaps.” Procedia Manufacturing 13:972–979. https://doi.org/10.1016/j.promfg.2017.09.093
- Schumpeter, J. 1934. The Theory of Economic Development: An Inquiry into Profits, Capital, Credit, Interest, and the Business Cycle. Cambridge, MA: Harvard University Press.
- Schwab, K. 2016. The Fourth Industrial Revolution. Cologny: World Economic Forum.
- Singh, K., and A. B. Landman. 2017. “Mobile Health.” Key Advances in Clinical Informatics, 183–196. https://doi.org/10.1016/b978-0-12-809523-2.00013-3.
- Sverdlov, O., J. van Dam, K. Hannesdottir, and T. Thornton-Wells. 2018. “Digital Therapeutics: An Integral Component of Digital Innovation in Drug Development.” Clinical Pharmacology & Therapeutics 104 (1): 72–80. https://doi.org/10.1002/cpt.1036.
- Thompson, D. F., and C. K. Walker. 2015. “A Descriptive and Historical Review of Bibliometrics With Applications to Medical Sciences.” Pharmacotherapy. The Journal of Human Pharmacology and Drug Therapy 35 (6): 551–559. https://doi.org/10.1002/phar.1586.
- Tromp, J., D. Jindal, J. Redfern, A. Bhatt, T. Séverin, A. Banerjee, J. Ge, et al. 2022. “World Heart Federation Roadmap for Digital Health in Cardiology.” Global Heart 17 (1): 1–22. https://doi.org/10.5334/gh.1141.
- Vasconcelos, J. C., J. T. Martins, D. Ellis, and E. Fontainha. 2019. “Absorptive Capacity: A Process and Structure Approach.” Journal of Information Science 45 (1): 68–83. https://doi.org/10.1177/0165551518775306.
- Vedanthan, R., A. Verstrael, K. K. Yeo, K. Zulfiya, D. Prabhakaran, C. S. P. Lam, and M. R. Cowie. 2022. “World Heart Federation Roadmap for Digital Health in Cardiology.” Global Heart 17 (1): 61. https://doi.org/10.5334/gh.1141.
- Vial, G. 2019. “Understanding Digital Transformation: A Review and a Research Agenda.” The Journal of Strategic Information Systems 28 (2): 118–144. https://doi.org/10.1016/j.jsis.2019.01.003.
- Weresa, M. A., C. Ciecierski, and L. Filus. eds. 2022. Economics and Mathematical Modeling in Health-Related Research. Leiden: BRILL. https://brill.com/display/title/62026.
- WHO. 2021. Global Strategy on Digital Health 2020–2025. Geneva: World Health Organization.
- Yalcin, H., and T. Daim. 2021. “A Scientometric Review of Technology Capability Research.” Journal of Engineering and Technology Management 62:101658. https://doi.org/10.1016/j.jengtecman.2021.101658
- Yuan, E. J., C.-A. Hsu, W.-C. Lee, T.-J. Chen, L.-F. Chou, and S.-J. Hwang. 2020. “Where to buy Face Masks? Survey of Applications Using Taiwan’s Open Data in the Time of Coronavirus Disease 2019.” Journal of the Chinese Medical Association 83 (6): 557–560. https://doi.org/10.1097/jcma.0000000000000325.
Appendix
Table A1. Variations in citations.
