ABSTRACT
Slow breathing guiding applications increasingly emerge, showing promise for helping knowledge workers to better cope with workaday stress. However, standard breathing guidance is non-interactive, with rigid paces. Despite their effects being proved, they could cause respiratory fatigue, or lack of training motivation, especially for novice users. To explore new design possibilities, we investigate using heart rate variability (HRV) data to mediate breathing guidance, which results in two HRV-enhanced guidance modes: (i) responsive breathing guidance and (ii) adaptive breathing guidance. These guidance modes are implemented on a soft haptic interface named “ViBreathe”. We conducted a user test (N = 24), and a one-week field deployment (N = 4) with knowledge workers, to understand the user experience of our design. The HRV-enhanced modes were generally experienced to reduce tiresome and improve engagement and comfort. And Vibreathe showed great potential for seamlessly weaving slow breathing practice into work routines. We thereby summarize related design insights and opportunities.
1. Introduction
Nowadays, work-related chronic stress has been a growing concern (American Psychological Association, Citation2015). Chronic stress may elevate cortisol (Chandola et al., Citation2006), disrupting various physiological processes. Moreover, if not adequately dealt with, chronic stress can result in emotional strain and health problems, including anxiety, depression, immune dysregulation (Padgett & Glaser, Citation2003) hypertension, and heart disease (Esler & Kaye, Citation2000). Therefore, stress management is meaningful and crucial for the health and well-being of office workers.
Slow breathing practice is a simple yet powerful self-regulation approach for reducing autonomic stress responses (Harris et al., Citation1976). In a short period of time, slow breathing can help people relieve symptoms of anxiety (Clark & Hirschman, Citation1990; Sisto et al., Citation1995), lower blood pressure (Schein et al., Citation2001), and focus the mind for optimal performance (Ley, Citation1999). In the long term, regular slow breathing practice can facilitate people to acquire a good breathing habit that sustains their autonomic balance and strengthens their resilience against stress (Gilbert, Citation2003). Given these validated health benefits, several end-user systems have been developed for facilitating slow breathing training. For instance, Just Breathe provides guided slow breathing intervention to help drivers manage stress (Paredes et al., Citation2018). Audio guidance for slow breathing is designed for the clinical population to relieve (Clark & Hirschman, Citation1990; Gavish, Citation2010). Many mobile applications have emerged as a portable tool to guide relaxed breathing, such as Sphere (Chittaro & Sioni, Citation2014), MyBreatheFootnote1, and PranayamaFootnote2.
Two types of signals are commonly used to aid novice users in slow breathing practice: feedforward guidance and biofeedback. With feedforward guidance, users are usually requested to follow the guidance to regulate their breathing pattern, for example, “to match their breathing rate to the alternation of the tones” (Clark & Hirschman, Citation1990). The pace of feedforward guidance is usually preset beforehand and not adjustable during the training. However, according to Gomez, et al. (Gomez et al., Citation2009), users may get respiratory muscle fatigue by repeating slow breathing at a fixed pace over time. As reported by Yu, Hu et al. (Citation2018), after a few minutes of deep breathing, some users apparently enter a fatigued state where their breath return to a habitual rate which is faster than the guidance. The biofeedback breathing training systems show users their respiration pattern or heart rate variability (HRV) information, which is often displayed as numbers or in charts on a screen. Instead of simply repeating a fixed pace, the users could learn to control the feedback and find an optimal breath pattern on their own. The continuous control process of feedback helps to keep users engaged with the training, but for novice users who do not have sufficient skills in regulating their breathing, it leads to increased threshold for learning. In this study, to explore new design possibilities and support low-threshold, easy-to-initiate breathing practice for novice users, we explore combining the strategies of feedforward guidance and biofeedback training.
In other words, we explore the design of interactive guidance that could respond or adapt itself to users’ real-time performance (based on HRV data), and address reduced engagement or increased fatigue caused by following the standard non-interactive guidance. Namely, we present two novel HRV-enhanced breathing guidance modes: responsive guidance and adaptive guidance. Responsive guidance uses its haptic display to also depict users’ HRV-based performance as real-time feedback, in addition to the fixed pace guidance. This real-time feedback is expected to enable users’ awareness about their current performance, potentially increasing their motivation and engagement within the training. Adaptive guidance employs a user’s HRV data to dynamically adjust its pace, which enables the guidance pace to adapt to the user’s physiological condition: when the user feels fatigue, the guidance pace will get closer to the users’ natural breathing pace, making it relatively less demanding to follow. Otherwise, it progressively directs the user to an ideal training pace.
To implement HRV-enhanced breathing guidance, we develop ViBreathe, a haptic respiration training interface which allows office workers to practice eye-free, low-threshold slow breathing exercise at short moments interleaved with their work routines (see ). ViBreathe integrates a photoplethysmogram (PPG) sensor and a vibration actuator into a soft woven object that can be held in users’ hand. The vibration actuator generates vibrotactile stimulus as the eye-free, haptic breathing guidance, and the PPG sensor senses a user’s HRV to manipulate vibration signal in real-time, making the guidance adaptive (with its pace dynamically adjusted) or responsive (with user performance conveyed in real-time) based on users’ HRV data.
This paper presents two studies with ViBreathe. In the first study, we conducted a user test to gather user experiences about the two HRV-enhanced breathing guidance modes, in comparison with the standard fixed guidance. ViBreathe was used as the tangible interface to present the responsive guidance, adaptive guidance, and standard fixed-pace breathing guidance in three slow breathing trials. We compare the HRV-enhanced guidance modes to the standard guidance to explore our first research question (RQ1): What differences, in terms of user experience, would the three modes of breathing guidance (two HRV-enhanced guidance modes and the standard guidance) have? Secondly, we conducted a field study in which ViBreathe was used by four office workers for one week, in their own naturalistic workaday settings. ViBreathe serves as a research product (Odom et al., Citation2016), through which we probe our second research question (RQ2): How could we facilitate short-term, informal slow breathing practice to be embedded into workaday routines of knowledge workers?
In the remainder of the paper, we discuss the related work about respiration training and breathing guidance, which informed our design exploration. We then address and discuss the findings of our first study which compared the three types of breathing guidance design in terms of user experiences for breathing training (to answer RQ1). Next, we address the field-based qualitative findings from the second study which probes opportunities of supporting informal respiration exercises in office routines (to answer RQ2). Finally, based on all these findings, we summarize a set of design implications about how to use HRV data to enrich technology-guided breathing practice, and how to unobtrusively weave breathing practice into knowledge workers’ workaday routines.
2. Related work & design considerations
2.1. Respiration training and breathing guidance
In recent years, HCI has witnessed an increasing interest in promoting calmness and emotion (stress) management in daily contexts (Azevedo et al., Citation2017; Costa et al., Citation2016; Papadopoulou et al., Citation2019). Regular respiration training, as a widely recognized beneficial activity, could help people develop healthy breathing habits and contribute to their stress management capability. Slow breathing training used to be guided by a tutor or a therapist. The trainees follow the tutor’s instruction to focus on and regulate their breathing pattern in some mind-body practice (Brown & Gerbarg, Citation2005; Pal & Velkumary, Citation2004), such as yoga, meditation, or mindfulness training. Recently, an increasing number of portable devices (Choi & Ishii, Citation2020; Reiner, Citation2008), mobile apps, and novel interactive systems (Ghandeharioun & Picard, Citation2017; Miri et al., Citation2020; Moraveji et al., Citation2011; Paredes & Chan, Citation2011; Paredes et al., Citation2018; Patibanda et al., Citation2017; Yu et al., Citation2015b; Yu et al., Citation2018) are developed for respiration training. Based on the guidance provided by these technology-mediated training systems, they can be mainly divided into two types: preset feedforward guidance systems and real-time biofeedback systems.
The idea of using feedforward guidance in breathing training is simple to understand: a system presents a targeted breathing pattern through visuals or audio tones for users to follow. The users are expected to match their breathing rate to a targeted rate, for example, at a slow frequency of 10 seconds per cycle (Vaschillo et al., Citation2006), or regulate breathing into a specific pattern, for instance, the ratio of 4:7:8 for inhale: hold: exhale (Fletcher, Citation2019). An extensive body of research (Clark & Hirschman, Citation1990; Gilbert, Citation2003; Harris et al., Citation1976; Ley, Citation1999; Schein et al., Citation2001; Sisto et al., Citation1995) has demonstrated the health benefits of slow breathing training guided by a feedforward signal. However, as mentioned before, repeating a fixed slow-paced breathing pattern over time may make users get respiratory muscle fatigue and lose motivation and engagement (Gomez et al., Citation2009; Yu, Hu et al., Citation2018). Moreover, a previous study by Yu et al. (Citation2015a) described some users failed in respiration training due to the difficulty of adapting to the pace of guidance from one’s habitual breathing. As a result, they suggest an adaptation in breathing guidance to address individual differences and the different stages in respiration training.
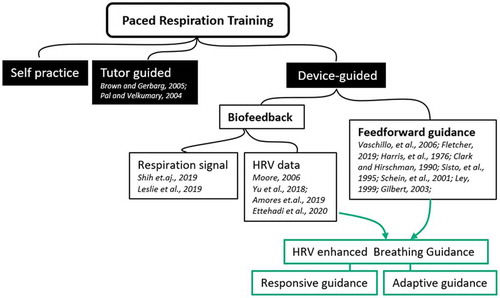
Besides feedforward guidance, a training system can also supply users with their heart rate variability (HRV) information for facilitating breathing regulation. Breathing modulates heart rate (Hirsch & Bishop, Citation1981). In each inhalation–exhalation cycle, the heart rate shows a natural rhythm. The heart rate increases on the inhale and decreases on the exhale (Lehrer et al., Citation2000). Research shows that slow breathing can enhance HRV and reach its maximum when breathing within the low-frequency range, at approximately six breaths/minute (Steffen et al., Citation2017). HRV can, therefore, describe the results of breathing regulation and used as real-time feedback, which is also referred to as HRV biofeedback. To be noted, we recognize that Electrodermal Activity (EDA) is also an important modality of biofeedback for relaxation and emotion regulation training (Miri et al., Citation2020). However, since the scope of this paper is respiration training, we mainly discuss two major types of biofeedback modalities: respiration rate and HRV (see ). Although breathing rate could be a very intuitive input to interact with an interface, HRV has been more widely used input data for biofeedback training. HRV has been widely accepted as a standard indicator of physiological stress. And using the breath to regulate one’s HRV is the immediate goal of biofeedback training for stress management.
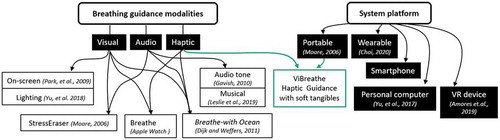
Figure 1. Based on current approaches of respiration training, we propose combining HRV biofeedback with feedforward guidance to create novel HRV-enhanced breathing guidance (in green boxes)
With HRV biofeedback, users learn to slow down their breathing rhythm to increase the HRV score and maintain it at a targeted level. In this learning process, the real-time feedback helps users to engage with self-regulation practice (Frank et al., Citation2010) and the users can be motivated when they have a higher score (which is based on their HRV). In an HRV biofeedback system, the feedback (HRV indices) is measured from each user and responds to his/her breathing regulation process. In other words, the HRV feedback changes across different individuals and changes over time within individuals as well. Therefore, HRV biofeedback systems often require a certain period of learning and practice to control the feedback and find the optimal breath pattern on their own. For instance, as suggested by Yu et al. (Citation2015a), Yu, Hu et al. (Citation2018), some users, with no prior exposure to breathing training, have difficulty in using biofeedback. It is therefore suggested that feedforward guidance and HRV biofeedback can be meaningfully combined to improve breathing training experiences for a broader range of users beyond the experienced ones.
As a result, in this study, we explore combining HRV biofeedback with feedforward guidance, utilizing their respective advantages to offset the limitations of each. As shown in , we propose two types of HRV-enhanced breathing guidance. Both are still feedforward guidance that provides users with a targeted breathing pattern to follow; yet each of them utilizes users’ HRV data to either provide direct feedback or adapt its pace accordingly. We believe designing feedforward guidance mediated by HRV data can have benefits such as lower threshold to follow, better experiences in training, reduced respiratory fatigue, or enhanced training motivation, especially for novice users who could benefit from short and easy-to-initiate breathing exercise, but have limited skills in regulating their breathing.
2.2. Breathing guidance modality and platform
As shown in , breathing guidance can be presented in single or multiple sensory modalities. Most single-modal breathing guidance relies on visual displays, which could take a variety of forms, such as an accurate guiding wave (Park et al., Citation2009), an evocative metaphorical visualization (Yu et al., Citation2017), a playful animation or game (Shih et al., Citation2019; Sonne & Jensen, Citation2016), or an immersive light environment (Yu et al., Citation2018). Auditory breathing guidance usually employs a simple audio tone (Clark & Hirschman, Citation1990; Gavish, Citation2010) and nature sounds (Ettehadi et al., Citation2020) or uses musical elements (Leslie et al., Citation2019; Yu, Funk et al., Citation2018). Multi-modal interfaces are usually used for adding extra information to the guidance or enhancing immersive experiences in training. For instance, visual guidance is often augmented with an audio or haptic cue to emphasize the switch timing between inhale and exhale. A good example can be seen in some off-the-shelf applications, such as Breathe in Apple WatchFootnote3, StressEraser (Moore, Citation2006), and emWaveFootnote4 devices. Moreover, in new design explorations, the guidance is designed by combining visual, audio, and haptic stimuli to create an immersive experience for relaxation and stress mitigation, such as a tangible interface Breathe-with-the-Ocean (Dijk & Weffers, Citation2011), and VR-based biofeedback system Deep Reality (Amores et al., Citation2019).
While immersive experiences are valuable in ad-hoc breathing training sessions, our aim is to enable “micro” (lightweight, shortterm, and serendipitous) breathing training sessions that can be woven into workaday routines of users. Namely, instead of scheduling a place and a fixed period for training, users could grasp the tangible interface on their office desk whenever they feel like doing short relaxation from intensive tasks. As a result, in this study, we design the breathing guidance in haptic modality. The study by Gallace & Spence (Gallace & Spence, Citation2010) revealed that haptic feedback could reduce the perceived workload in learning task. Moreover, stimulating the tactile sense might also give people relaxing bodily experience (Windlin et al., Citation2019). Compared with visual and audio modality, breath guidance through solely haptic modality could allow users to perform breathing training with eyes closed and therefore better focus on their breathing with fewer distractions (Yu et al., Citation2015b). It could also enable users to regulate breath while visually engaging in other primary tasks, such as reading, browsing, or during a meeting. Also, haptic displays tend to be intimate and private (e.g., less noticeable to other people in the surrounding) and hence suitable for use in the workplace.
One possible or maybe the easiest way to implement haptic breathing guidance could be through a haptic engine embedded in smartphones or smart watches. However, according to the report by the American Psychological Association (Citation2017), these smart devices may stress out people by keeping them virtually connected and constantly sending them notifications from different media. Given the intrusive nature of these versatile devices, they may not be an ideal platform for everyday respiration training which means to help a user mitigate stress. Therefore, in light of the trend of Ubiquitous Computing (Abowd & Mynatt, Citation2000) and the Internet of Things, we argue that it is meaningful to explore the design space of breathing guidance mediated by unremarkable tangible objects rather than a centralized computing device (e.g., smartphone/watch).
Many people like to fiddle around with finger-fidgets or squeeze a stress ball, sponge, or other pliable objects when they are stressed at work. Those mindless actions could help people focus and reduce their feelings of stress and anxiety (Alonso et al., Citation2008). From another perspective, the moment when a user is squeezing the stress ball at hand might be a right timing for practicing slow breathing. Inspired by this direction, we design ViBreathe, a soft, tangible interface which can be held and squeezed in hands and functionally, can sense heartbeat data, and provide HRV-enhanced breathing guidance in haptic modality. We elaborate on the implementation of ViBreathe and the haptic design of responsive and adaptive guidance in the following section.
3. ViBreathe haptic guidance system
The design goal of ViBreathe is to provide eye-free breathing guidance through a tangible object within reach so that the users can use it at small moments at work to perform respiration training casually and comfortably. In , the photos from our filed implementation show the usage scenario of ViBreathe at workplace. When an office worker feels stressed at work, they can rest her hand on ViBreathe or pick it up and hold it by hand. After the PPG sensor detects his/her heartbeat data, ViBreathe starts to present the breathing guidance through its vibration rhythm. Accordingly, they can regulate breathing to match the guidance. After a few minutes of slow breathing, they put ViBreathe back to its wireless charging socket and goes back to work.
Figure 3. (a) The soft tangible interface of ViBreathe on its wireless charging dock placed on the desk within the user’s reach; (b) the user can follow its haptic breathing guidance while simultaneously focusing on the computer screen; (c, d) the user can also hold ViBreathe to have “micro” relaxation training during a short break from work

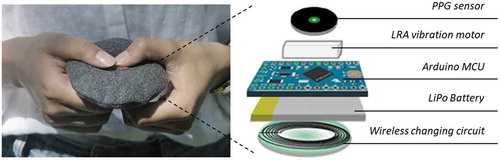
ViBreathe system consists of two parts: a handheld training device and a wireless charging dock. Regarding the handheld device, a round ring-shaped soft object filled with polyfill serves as the main body to support the shape, which is designed to be easy to hold in different ways users desire. The stuffing can also soften the vibration from the motor and reduce its noise. All electronics are nested at the center hollow part and encased by a cover crafted out of cashmere wool: a texture that we selected from several types of material for its most suitable tactile experience, which feels soft, warm, and inviting users to touch. shows the breakout of the components inside the handheld device. The electronics consists of a PPG sensor, an Arduino mini microcontroller, a vibration motor by an Adafruit DRV2605L, a haptic motor controller, a lithium battery, and a wireless charging circuit. Thereby, it does not require the user to explicitly charge the battery: when put aside on the plate, it automatically starts charging.
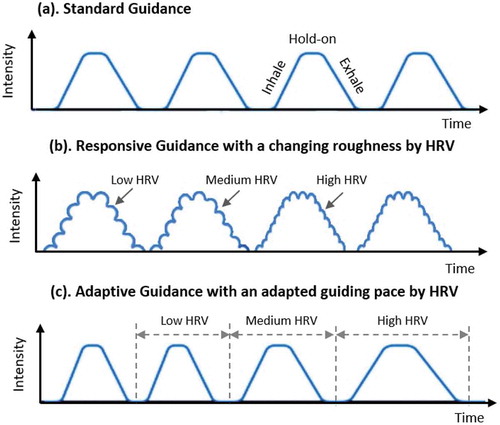
ViBreathe provides breathing guidance through a rhythmical change in vibration intensity. The vibration signal is generated by two sinusoidal signals (f1 and f2) that are superimposed with each other. We modify the amplitude of both sinusoidal signals to control vibration intensity. Thus, through amplitude-modulation, the rhythm of vibration represents a guiding breathing pattern that enables users to match with. In prior exploratory research, we have identified the maximum vibration intensity of comfort with touch and confirmed the users’ ability to interpret the guidance pattern through intensity changes. ViBreathe prompts users to inhale/exhale slowly in the following manner: an increasing vibration intensity indicates ‘breathe in’, a decreasing intensity indicates “breathe out”, and the maintained minimum and maximum intensity means “hold breath”, as shown in ). Such design rationales were inspired by the metaphor of inhalation/exhalation that is similarly used in yoga practice and Chinese traditional medicine. Inhalation could be seen as an absorption of substance (oxygen) and positive energy in the air, while exhalation could be seen as the release of substance (carbon dioxide) and negative energy. When inhaling, the vibrotactile intensity increases to “resonate” with the energy absorbed into the users’ body. As the user releases energy (exhaling), the intensity also decreases.
4. HRV-enhanced breathing guidance
Based on ViBreathe system, we developed three types of haptic breathing guidance: standard guidance and two types of HRV-enhanced breathing guidance: Responsive guidance and Adaptive guidance, as shown in . Used as a reference for evaluating our HRV-enhanced guidance designs, the standard guidance is based on traditional slow breathing practices (i.e., Gavish, Citation2010) that use fixed-pace cues for guiding participants to lower their breathing rate. The HRV-enhanced guidance is developed to study if and how HRV data can be used to mediate feedforward guidance so that users can be aware of their performance in real time or that the guidance can be adaptive to users’ current state. We hypothesize that by providing real-time performance feedback, or enabling user-adaptive feature, our novel guidance designs could lead to increased engagement or reduced respiratory fatigue, respectively. In an experiment to be addressed later in this paper, we have evaluated all these three types of breathing guidance to test their effectiveness and study their user experiences, in order to gather insights for informing future designs. We now present the design of the HRV-enhanced breathing guidance in detail to help the audience distinguish their differences from the standard guidance.
4.1. Heart rate variability calculation
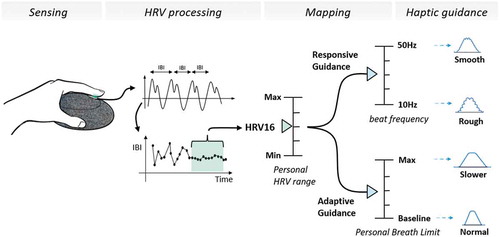
HRV sensing is based on a PPG sensor nested in the surface of ViBreathe. When a user places a finger on the PPG sensor, the sensor illuminates the skin and measures changes in light reflected from the LED during each pulse, resulting in a measurable voltage that is referred to as blood volume pulse (BVP) signal (Shelley et al., Citation2001). The BVP signal can well reflect the blood volume changes caused by the contraction of the heart. The heartbeats are then located in BVP signal through a peak detection algorithm (Pan & Tompkins, Citation1985) and the interval between two adjacent heartbeats is calculated into a series of inter-beat intervals (IBI) data. The standard deviation of inter-beat intervals (SDNN) is one of the most common HRV indexes (Stein et al., Citation1994). Thereby, in this study, a specially modified form of SDNN is calculated with a moving window of 16 heartbeats as a short-term HRV for mediating the breathing guidance. According to Yu et al. (Yu et al., Citation2017; Yu, Hu et al., Citation2018), the HRV16 is calculated with the following formula: HRV16 = (15× HRV16 + |IBI ̶ IBIavg|)/16, and IBIavg = (15 × IBIavg + IBI)/16. And HRV16 value is updated with each heartbeat.
Practically, people are diverse in their inherent physiological features and their existing habits of breathing. When mediating the breathing guidance with HRV, to provide a correct performance feedback and an appropriate adjusted pace, ViBreathe needs to normalize the moderating effects of HRV on breathing guidance based on the personal HRV range and personal breath range of different individuals. Personal HRV range is determined by a user’s baseline HRV and maximum HRV; personal breath range is defined as the range between a user’s spontaneous breath length (representing the user’s baseline pace of breath) and the user’s longest breath (representing the user’s slowest possible pace of breath). Both a user’s personal HRV range and his/her personal breath range were measured before the trials. The measurement of personal HRV range and personal breath range consists of two steps: the user first keeps spontaneous breathing for one minute, during which the minimum HRV and breath length are calculated. Then, the user was asked to take deep breaths as slowly as possible for one minute, during which the maximum HRV and breath length are calculated.
This way, as shows, ViBreathe could assess the user’s HRV changes referring to his/her personal HRV range and be mapped to the proper controlling parameters (i.e., beat-frequency or guiding breath length) of haptic guidance. In addition, in the mode of adaptive breathing guidance, ViBreathe also refers to the user’s personal breath range, in order to adjust the guidance pace according to the user’s own bodily capability and respiratory skills.
4.2. Responsive breathing guidance
4.2.1. Design
The responsive breathing guidance aims to supply users with information about their performance in slow breathing in addition to the guiding breathing pattern. Thereby, ViBreathe needs to present two types of information through single-channel vibration. This is quite challenging due to the limited ability of using a single vibration motor to display multiple information simultaneously. In this design, we still use the intensity of vibration to present the guiding breathing pattern, which is the same as the standard guidance. Meanwhile, we modulate the tactile sensation of roughness as an extra channel to present HRV data. A high HRV leads to a smoother tactile feeling, which indicates a good performance in slow breathing. A “rougher” (i.e., more granular and coarse) tactile feeling represents lower HRV values (indicating less desirable training perforamnces). Therefore, from a user’s viewpoint, this breathing guidance could be responsive to their breathing regulation, informing about their performance in real time.
4.2.2. Implementation
The tactile sensation of roughness is implemented by modulating the envelope of the superposition signal of the sinusoidal signals, f1 and f2. The phase difference between the sinusoidal signals (f1-f2) will generate the “beats” in the envelope of their superposition signal, the amplitude oscillating up and down at a specific frequency – beat frequency (f-beat), as shown in ). As suggested by Park and Choi (Citation2011), the tactile roughness sensation is negatively correlated with the f-beat. An envelope signal with low f-beat can be perceived as a fluttering motion, and the one with high f-beat feels smooth. Therefore, we couple the HRV16 with beat frequency. Specifically, for each user, their personal HRV range is mapped to the beat frequency ranging from 10 to 50 Hz (see ). Thus, when their HRV16 is improved by slow breathing, the breathing guidance will become increasingly smooth.
4.3. Adaptive breathing guidance
4.3.1. Design
In standard guidance and responsive guidance, the guidance pace is set beforehand and fixed during the use. By contrast, in adaptive guidance, the pace is adjusted in real time based on a user’s short-term HRV. For instance, the guidance could start with a pace at 8 breaths per minute. The pace can become slower, e.g., 6 breaths/min, when a user performs well without too much effort. Or the pace can also become faster (which is easier to follow) when the user feels difficult or uncomfortable due to respiratory fatigue. This adaptiveness of guidance pace aims to prevent respiratory fatigue and improve physical comfort and mental satisfaction in respiration training.
4.3.2. Implementation
shows how ViBreathe adapts the length of the breathing guidance according to the value of HRV16 within a user’s personal HRV range. For each user, their personal HRV range is mapped to their own personal breath limit so that the newlycalculated HRV16 could determine the length of the next guiding breathing pattern within their spontaneous breath (baseline) and the longest breath length (maximum). When a user continuously performs well in respiration training, with the improvement of HRV, the breathing guidance will be adjusted to a slower pace close to his/her longest breath. Conversely, the guidance will be adjusted to a faster pace close to the user’s spontaneous breath rate when the HRV decreases due to respiratory fatigue or inability to follow as well as they might have previously.
5. Evaluation
5.1. Research questions
To investigate the feasibility and impact of the proposed HRV-enhanced breathing guidance, we pursued the following two open questions with exploratory nature: What differences would the three modes of breathing guidance (two HRV-enhanced guidance modes and the standard guidance) have, in terms of user experience (RQ1)? And how could we facilitate short-term, informal breathing training to be embedded into workaday routines of knowledge workers (RQ2)?
To answer RQ1, we conducted an in-lab user test, which was designed to compare the user experiences of the two HRV-enhanced guidance designs with the standard one. The user test follows a within-subject approach with counter-balancing to avoid carry-over effects. The participants were asked to perform three respiration training sessions with ViBreathe. In each session, they would receive one of the three types of breathing guidance, respectively.
To answer RQ2, we conducted a field evaluation of ViBreath with four knowledge workers. Each participant used the system for five workdays, in their naturalistic office environment. In-depth interviews have been conducted to comprehensively understand the opportunities and implications for weaving easy-to-initiate breathing training into knowledge workers’ professional routines, in order to inform future work aimed for enriching their repertoire for stress management in work routines.
5.2. Participants
Twenty-four office workers (13 males and 11 females) participated in the in-lab user test study (RQ1). And four office workers (two males and two females) participated in the field evaluation (RQ2). All participants age from 24 to 32 (M = 27.58; SD = 2.32). All participants were able to use the PPG sensor, and they were willing to perform slow breathing practice. They are considered as a novice group for slow breathing training: they had not performed slow breathing, paced respiration, yoga, or meditation regularly. Furthermore, the participants had no experience with HRV biofeedback technique. All participants gave the written informed consent. The whole study has followed the The Netherlands Code of Conduct for Research Integrity and the Eindhoven University of Technology (TU/e) Code of Scientific Conduct.
5.3. Measurements
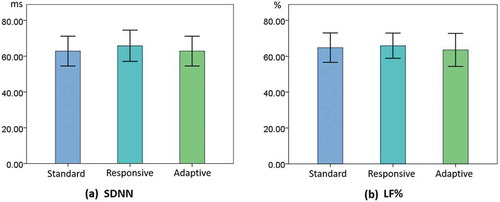
In the in-lab user test (RQ1), the independent variable was the type of breathing guidance, while the dependent variables include a posttest user experience survey. In addition, we gathered all participants’ HRV indices and respiration rate as objective references, to shed light on their physiological processes in the three breathing practice trials using the three different modes of breathing guidance. The HRV indices include SDNN (standard deviation of heartbeat intervals) and LF% (the low-frequency components in HRV power spectrum), which are widely applied to evaluate the respiration training and biofeedback relaxation systems, i.e., ExoBuilding by Schnädelbach et al. (Citation2012). According to Schipke et al. (Citation1999), in short-term recordings, HRV is highly related to the respiratory cycle of the participants and thereby could indicate the effectiveness of slow breathing training. When an individual performs well, the SDNN and LF% will both increase. During the respiration training, the user’s IBI data were measured by a PPG sensor attached to the index finger of the user’s hand which was not holding ViBreathe. The HRV indices were calculated from the IBI data by using HRVAS software.
Respiration data were measured with a belt stretch sensor which measures a trace for abdomen movement. Respiration rate (RSP-R) (cycles per minute) was derived from the respiration trace. We collected the user experience data through the core module of the game experience questionnaire developed by IJsselsteijn et al. (Citation2013). Based on our research purpose, we selected three relevant components from this module: Flow, Challenge, and Comfort. We did not use the inapplicable components of this module (such as Competence and Imaginative Immersion) due to the irrelevance of these components and the principle of parsimony.
A semi-structured interview was conducted both for the in-lab user test (RQ1) and the field evaluation (RQ2). For the in-lab user test, after each session and at the end of their participation, each participant was interviewed. We asked them to explicitly describe their feelings after experienced each breathing guidance mode. During the process, additional questions might be asked by the researcher, to ask a participant to expand or specify their responses that are related to the research questions. And in the end, we asked them to reflect on all three sessions and compare their experiences about all guidance modes. For the field evaluation (RQ2), each participant was interviewed after their participation. The interviews were loosely structured, starting from some pre-scripted questions such as: “How often did you use ViBreathe during the past week? How long did you use ViBreathe each time? At what moment(s) did you use ViBreathe? What did you like and dislike about the experience with ViBreathe? Any other comments?” There was enough space for the participants to share lived experiences about their using ViBreathe in a workaday context. All interviews were transcribed verbatim for later analyses.
5.4. In-lab user test procedure
The in-lab user test followed the procedure shown in . On arrival at the laboratory, the participants were attached with the PPG sensor and respiration sensor. First, the participants sat quietly, held ViBreathe at hand, and completed the measurement of personal HRV range and personal breath range for initialization of two HRV-enhanced breathing guidance. The specific steps can be found in . Second, the participants were asked to take one-minute slow and relaxing breath, the average length of which was calculated to set a personalized pace for feedforward breathing guidance. It is noteworthy that the breath length measured here is used to set the guiding pace for standard guidance and responsive guidance, and the initial guidance pace for adaptive guidance. It is a slow yet comfortable pace set by a user and, therefore, normally differs from the maximum value in personal breath range, which indicates the upper limit of a user’s physical capacity of slow breathing. Next, the participant undertook three respiration training sessions with different types of haptic guidance provided by ViBreathe. Each session lasted three minutes to ensure the effects of deep breathing on physiological relaxation (Russo et al., Citation2017; Sivakumar et al., Citation2011). After each session, the participants took three minutes break and then completed the experience questionnaire and a short interview to explain the reasons for their responses. At the conclusion of the experiment, a semi-structured interview was conducted to collect the qualitative data regarding the users’ opinions on each guidance and their relative strengths and weaknesses.
5.5. Data analysis
Quantitative data: In the in-lab user test (RQ1), the questionnaire responses, as well as the additional measures of HRV and respiration, were examined through the Shapiro–Wilk test. For those measures that fit the normal distribution, a repeated-measures ANOVA was conducted. Where the ANOVA was significant, a post-hoc analysis was conducted using paired samples t-tests to identify which conditions differed significantly. For those measures that fall into a non-normal distribution according to the Shapiro–Wilk test, a Friedman test was conducted. And when the result is significant, a nonparametric paired Wilcoxon test was conducted to identify which conditions differed significantly.
Qualitative data: The transcripts of the in-lab test and the field evaluation were analyzed separately to answer RQ1 and RQ2. Both analyses follow the procedure of the approach called Conventional Qualitative Content Analysis, detailed by Hsieh and Shannon (Citation2005). Each qualitative analysis began with the segmentation of the interview transcripts into quote statements with labels and annotations regarding a research question. Tow coders then categorized the labeled quotes using inductive coding to identify recurring patterns within predefined and emerging clusters. Additionally, in the analysis of the in-lab user test (RQ1), given that there were many predefined themes (characteristics of the three guidance modes), the frequency of statements attributed to the themes was counted to give further insight into the recurrent patterns among the quotes.
6. Findings I: What differences would the three modes of breathing guidance have in terms of user experience? (RQ1)
6.1. Quantitative results
6.1.1. User experience questionnaire
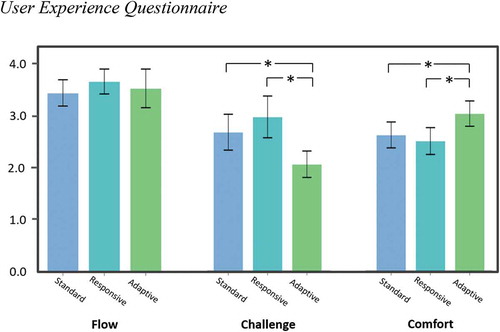
shows the results of the user experience survey. We used the core module of the game experience questionnaire and focused on three components: Flow, Challenge and Comfort. The questions in Flow component probe the users’ feelings of concentration and engagement (i.e., to what extent the user is engaged in the breathing training). The Challenge component assesses how demanding the users felt in following the guidance to regulate breathing. The Comfort component assesses how comfortable and enjoyable with the experienced trial. A Friedman test revealed that there were significant differences among the guidance types in components of Challenge (χ2(2) = 10.14, p = .006) and Comfort (χ2(2) = 16.12, p < .001). According to a Wilcoxon non-parametric test, the experience of challenge was significantly reduced with the adaptive guidance (M= 2.08, SD = 0.61) than with responsive guidance (M= 3.00, SD = 0.96), Z = ̶ 2.89, p = .004, and standard guidance (M= 2.71, SD = 0.83), Z= ̶ 3.33, p = .001. Regarding the experience of comfort, the participants reported a significant increase with adaptive guidance (M= 3.84, SD = 0.73) than responsive guidance (M= 3.17, SD = 0.78), Z= ̶ 3.55, p < .001, and standard guidance (M= 3.32, SD = 0.75), Z= ̶ 2.43, p = .015. These results have clearly revealed the advantages of adaptive breathing guidance in enhancing user experience with respiration training, by reducing its challenge and improving user comfort. These results will be further explained in light of our qualitative findings.
6.1.2. Heart rate variability (HRV)
In short-term recordings, an individual’s HRV closely correlates to his/her breath rate and thereby has been widely used as an indicator of the effects of respiration training on the autonomic nervous system (Schipke et al., Citation1999). When an individual performs well in slow breathing, the HRV indices: low-frequency components in the HRV power spectrum (LF%), as well as the standard deviation of heartbeat intervals (SDNN), will both increase. shows the results of HRV indices in three respiration training sessions. There are no significant differences in SDNN (χ2(2) = 1.083, p = .582) and LF% (F (1.88, 43.42) =0.153, p= .847) between three types of guidance, which indicate that the newlydesigned responsive and adaptive guidance has similar effectiveness with the standard, feedforward-only breathing guidance for respiration training. Besides, the responsive guidance led to a slightly higher HRV (both reflected by SDNN and LF%, as shows) in the training, which can suggest that the explicit feedback of HRV information may have motivated participants to perform slow breathing regulation more intensely. Participants’ reported experiences that are related to this will be further discussed in our qualitative findings.
6.1.3. Respiration rate
) shows the guidance pace set by the users before the training sessions and the average of their actual breath rate with different types of guidance. According to the Friedman test, there are no significant differences in the participant’s breath rate among the three sessions, χ2(2) = 2.051, p = .359. ) shows the deviation between the guidance pace and the participant’s actual breath rate. As the pace of adaptive guidance was adjusted during training, here it shows its initial pace which is the same with standard and responsive guidance. We can see the deviations were very small with standard guidance (M = ̶ 3%, SD = 37%) and responsive guidance (M = 3%, SD = 63%).
Figure 10. (a). Participants’ breathing rate for each session (the colors indicate different individuals). (b) boxplots of the deviation between the pre-set guiding and the participant’s actual breathing rate
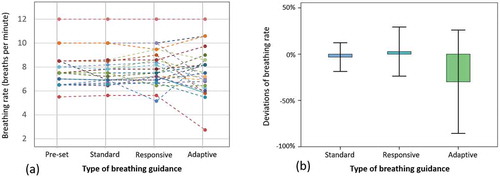
By contrast, as evident in ), with adaptive guidance, the participants’ breath rate showed a large deviation from the initially pre-set pace (M = ̶ 29.7%, SD = 132%). This is mainly because the guidance pace had been adjusted by the participants’ HRV data in real time, and in turn, by following the guidance, the participants’ breath is also dynamically adjusted during the training. Specifically, for nine participants, the guidance was stretched out compared with the initial pace; for eight participants, the guidance pace in average was shorter than the pre-set, which is easier for them to follow. These results suggest this adaptiveness of guidance led to more flexible and diversified breathing patterns, because of an ongoing interactive “negotiation” between the participants and the user-adaptive guidance. In this sense, the adaptive guidance offers an extra level of flexibility during training beyond the pre-setting of a personalized guiding breath rate. These results of respiration rate also explain why the adaptive guidance led to significantly lower challenge and higher user comfort from the user experience questionnaire. How this “flexibility” enabled by adaptive guidance had influenced the participants’ behaviors and experiences will be addressed in detail in our qualitative findings.
6.2. Qualitative results
shows the features of each type of breathing guidance as well as the corresponding implications from the interview data. Participants’ recurrent opinions on each type of guidance have been summarized in and sorted into positive aspects (benefits) and negative aspects (design challenge). This way, we present an overview of user experiences about the three evaluated types of breathing guidance, to inform future related works of the benefits, design challenges that are to be considered. Exemplar quotes selected from the responses from all 24 participants will be used to illustrate the user experiences.
Table 1. Summarizing the qualitative findings from the interviews
6.2.1. User experiences of standard guidance
6.2.1.1. Advantages
As shows, on the one hand, the standard guidance was experienced by the participants as easy to understand its guidance (four participants), and effortless to perform the training with it (two participants). For example, as S18 indicated, “[It’s] fixed and repetitive pattern takes the minimal mental effort of mine. It is easy to follow, takes not much effort. I felt I didn’t have to focus on breathing [training].”
6.2.1.2. Disadvantages
On the other hand, the participants experienced that its simple and non-reactive behavior during training could cause them to feel bored or sleepy or to be distracted by other things (seven participants). For instance: “It is easy to follow. But after following it for a while, I got tired, distracted” (S2). Similarly, S23 felt that “following this fixed frequency is kind of boring and three minutes felt quite long to me.”
Furthermore, its pre-set fixed guiding breath rate could cause some participants to feel uncomfortable or fatigued after a while following its guidance (four participants). For example, as S15 experienced, “The pre-set pace of the guidance didn’t match my own breath so well. I didn’t feel very comfortable near the end of the training.” Similarly, as S14 said, “Maybe because the pre-set rhythm of this breathing guidance didn’t match the pace of my deep breathing, I always felt hard to follow, uncomfortable.”
6.2.2. User experiences of responsive breathing guidance
6.2.2.1. Advantages
Five participants appreciated that the roughness change of responsive guidance had enriched the user experience, making the guidance more expressive (in comparison with the standard guidance). For example, as S15 said, “It has richer, multi-level feelings of touch. So, it’s less boring for touch.” And as S16 similarly put, “It’s interesting in terms of touch feeling. It has a stronger sense of vibration, so more explicit beats.” Such change of roughness is meant to present users’ current performance of breathing training reflected by their HRV. This HRV feedback was thereby experienced to have made the participants more motivated, engaged, and concentrated in their trainings, as mentioned by nine participants. For example, as S14 experienced, “the granular [roughness] feedback can make me more deliberate, concentrated on adjusting breathing pattern.” And S13 appreciated this guidance since “it’s relatively engaging: I adjusted to different breathing patterns to test the different levels of roughness. It’s fun.” S24 described that during training, “I was working hard to follow [the guidance] in order to achieve the smooth effect. This had been a big motivation.” Likewise, S12 experienced that with this feedback, “I am more concentrated [during the training]. So, the time had passed really quickly.”
6.2.2.2. Disadvantages
Contrarily, as also shows, six participants experienced that the roughness change made it more difficult for them to simultaneously perceive the intensity change of this guidance (the feedforward of the guidance). For example, as explained by S3, “the roughness [change] made it more difficult to feel the intensity changes. Sometimes, it’s hard to distinguish the peaks of the intensity, which made me miss the transition timing of breathing-in and breathing-out.” Also, adding the real-time HRV feedback could impose extra mental load onto users, as suggested by five participants. As S8 felt, “For me, the challenge is not about regulating my breath, but more about the mental effort: I need to not only follow the guidance, but also pay more attention to and care more about my results.” Moreover, seven participants indicated that the feedback HRV results indicating their training performance could sometimes cause pressure during training. Rather than perceiving the feeling of smooth as a reward (as S24 did), the seven participants tend to more perceive the feeling of roughness as a “negative alert (S5)”. As S14 experienced, “sometimes, the roughness didn’t decrease as I expected. That made me feel pressured.” And S12 indicated that “the increase of roughness brought anxiety.” Additionally, as similar to standard guidance, responsive guidance also uses a pre-set, fixed pace of breathing feedforward. Therefore, it could also lead to an uncomfortable feeling due to the mismatch between a user’s habitual breathing pattern and the guiding breathing pace, as addressed in the user experiences about standard guidance.
In summary, in comparison with standard guidance, responsive guidance could make the breathing training less tedious and more engaging through immediate feedback on user performance (based on HRV). However, during training, such immediate performance feedback could also impose more attentional load onto users, and cause pressure sometimes. As a result, S2 and S8 explicitly indicated that responsive breathing guidance was more suitable to be used in ad-hoc training settings, rather than in everyday contexts. As put by S2, “I think it [responsive guidance] is more suitable for clinical training as a training tool, because it requires users to focus on results and motivates the users to achieve good results. But in daily context, it requires too much attention, and hardly helps people relax.”
6.2.3. User experiences of adaptive breathing guidance
6.2.3.1. Advantages
As experienced by 17 participants, there was a prominent advantage of adaptive guidance: its adapted guidance pace made the breathing regulation easier and more comfortable and caused less respiratory fatigue during training. As mentioned earlier, some participants explicitly indicate that a breathing guidance with a pre-set, fixed pace could cause uncomfortable or fatigued feelings, due to the mismatch between the participants’ habitual breathing pace and the guiding pace. Regarding this problem, adaptive guidance was appreciated for its friendly adaptivity to users. As S4 experienced, “comparing with the fixed breathing frequency [of the other two guidance designs], this one [adaptive guidance] is much more effortless.” S1 further explained this with an example: “near the end [of the training], I did feel a bit tired, so I didn’t follow its rhythm. And then [each repetition of] the guidance turned shorter, allowing me to take a rest. I didn’t have to follow its intensity. [So, I] felt comfortable.” S10 also added to this: “you don’t have to maintain the same frequency, so it’s more comfortable.”
While considered to reduce difficulty and fatigue in the training, the adaptivity of the guidance was also experienced by five participants to make them feel more in-control and less pressured during the training. For example, as S9 said, “the advantage [of adaptive guidance] was that I didn’t have the pressure to follow it. It’s a better experience – I can follow my own pace.” Similarly, as S6 experienced, “it made me feel relaxed. [Because] I can control its change […] it feels good, more like I’m in-control, rather than being taught.” S4 also had the similar feeling: “it feels like I was influencing it rather than it was guiding me […] I had little pressure. It doesn’t feel like a training.” Furthermore, six participants mentioned that because they could “control” the pace of adaptive guidance by adjusting their own breaths, the training experience became playful and enjoyable. As S3 commented, “the duration of the guidance changes according to my performance. It’s more fun, enjoyable, and interactive. I could play with it: I tried to breathe slower, and it slowed down as well; Then I breathed faster, and I could clearly feel the vibration [reacting to me].” S5 also thought “it feels fun, like interaction [with the guidance].” And to S6, “it’s [adaptive guidance] like a companion. And we are practicing breathing together.” For the same reason, three participants thought adaptive guidance is relatively more engaging, and less boring in comparison to the Standard Guidance. As S12 experienced, “it’s easy to get immersed in it [interacting with adaptive guidance]. So, it’s not boring.”
6.2.3.2. Disadvantages
As experienced by four participants, one of the disadvantages of adaptive guidance was that its user-adaptive mechanism required certain learning in order to be understood. Unlike standard guidance which is non-reactive, or responsive guidance, which reacts to users immediately, adaptive guidance reacts to users’ breathing performance by adjusting its pace of upcoming breathing guidance. Therefore, its mechanism is less apparent than the other two guidance designs, which could require more learning. As S7 experienced, “because it [adaptive guidance] adjusts with certain delay, it could feel a bit confusing sometimes.” Four participants reported another disadvantage of this user-adaptive breathing guidance: it required certain practice for users to control its pace at will. As appreciated by some participants, adaptive guidance enabled users to both follow and proactively “control” its pace. However, such control may require certain practice. For example, as S10 experienced, “because it [adaptive guidance] varies its pace, I had to make efforts to adjust my own breath and meanwhile follow its new pace.” And in S11’s words, this process requires certain “rapport” through practicing. Despite relatively more learning and practicing were needed for using adaptive guidance, the interviews suggest that all the participants were able to understand its mechanism and complete their trainings with adaptive guidance. As S4 experienced, “the process of adapting [to adaptive guidance] is a bit strange, but once you adapted, it’s quite comfortable.”
In summary, the adaptive guidance was more effortless and comfortable to follow than the pre-set, fixed pace of standard guidance and responsive guidance. In comparison with responsive guidance which shows users’ real-time performance, adaptive guidance made the participants feel less pressured and more in-control during training. Moreover, its adaptive mechanism was also experienced to be playful and enjoyable during use, although extra learning and practicing could be needed before users adapt to it. Unlike responsive guidance which made users engaged in and concentrated on improving their training performance, adaptive guidance was considered to be more friendly and less demanding. For this reason, S2 and S4 explicitly indicated that adaptive guidance was more suitable to be used in everyday contexts, in which it could provide casual and relaxing trainings depending on users’ current physiological states. As S2 said, “I think this training [with adaptive guidance] is better for everyday use, in daily environments […] It can adjust itself based on my [current] data, and adapt to a pace which is comfortable to me.”
7. Findings II: How could we facilitate short-term, informal breathing training to be embedded into workaday routines of knowledge workers? (RQ2)
The above study has been intended to evaluate the user experiences of two novel designs of HRV-enhanced breathing guidance, in comparison with a standard (feedforward-only) breathing guidance design. As we have found, the responsive breathing guidance was experienced to afford better user engagement in breathing training; and the adaptive breathing guidance was reported to impose less breathing fatigue onto the users during training. Besides these two advantages regarding user experiences, the users’ physiological measures (including heart rate data and respiration rata data) have suggested that the two novel guidance modes and the standard guidance mode did not show significant differences in terms of effects on users’ HRV data. We therefore demonstrate the feasibility of utilizing user’s real-time HRV data to mediate breathing guidance in improving user engagement and reducing respiratory fatigue for our targeted users (knowledge workers who are not experienced with breathing training and have limited skills in regulating their breathing behaviors).
Building further upon this, in the current section, we discuss our findings from the second study, a field evaluation aimed at probing insights into how we could embed such easy-to-initiate, short-term breathing trainings into the real-life office routines of the knowledge workers (RQ2). To gather contextualized and concrete empirical knowledge, we offered ViBreath (with adaptive guidance) to four office workers, who used the system over the course of five workdays. We provided adaptive guidance design to the participants due to its flexibility in supporting users with different levels of respiration skills. Moreover, the adaptive guidance seemed to be the most comfortable design in the in-lab user test. Before the study, we measured each participant’s personal HRV range and personal breath range to initialize the adaptive guidance. After the evaluation, in-depth interviews were conducted to probe opportunities and implications for design. The empirical findings are reported in the following clusters. These empirical understandings are reported in the following clusters.
7.1. Weaving “micro” breathing training into daily routines
What we mean by “micro” in this paper is three-fold: i.e., the breathing training being lightweight (effortless to perform), short term, and serendipitous (possible to be triggered at any moment without deliberate planning). These intended properties have been partially verified in the data. shows the common usage scenarios of ViBreathe in the field study. Most participants used ViBreathe two to three times per day for an average of three minutes per session. All participants responded that they normally used it when taking a break between their daily tasks (see )). For instance, S1 mentioned that “during work, I usually take a 5-minute break every 25 minutes. This device [ViBreathe] was very handy for that.” S2 and S4 reported that the physical presence of ViBreathe on their worktable (see )) seemed to make them more likely to use it. As S2 said, “[I used ViBreathe] at moments between tasks when I saw it”. And for S4, “I used it [ViBreathe] kind of randomly when I saw it. And sometimes, I even used it during the work, just put my hand on it, like a palm rest.” S3 reported more regular use of ViBreathe “at the start of the day, mid-day and sometimes at the end of the day”. Also, S2 and S3 reported that they took ViBreathe with them so that they could use it for slow breathing practice “at home”, “walk around campus” and “on the way home.”
7.2. Promoting relaxation and calmness during work hours
All four participants responded that ViBreathe helped them to practice slow breathing and relax mind at work. For example, S1 indicated that “it [ViBreathe] was kind of much slower than my normal breath, so I tried hard to regulate my breath to follow it, so I think it is helpful to me to practice slow breathing (S1).” Also, S2 stated that “when I matched my breathing to it [ViBreathe], and my breathing just became slowly and calmly, so I just keep do it [slow breathing].” S3 and S4 explicitly indicated that ViBreathe helped them relieve their stress at work. As put by S3, “It [ViBreathe] helps me to consciously step out of my work, focus on my breathing, and relax my mind.” Likewise, S4 stated that “when I hold it at hands and breathed slowly with it, I felt very relaxing and it made me to take a break from work”
7.3. The nuanced feelings enabled by Vibrotactile stimuli
Three participants reported the vibrotactile guidance of ViBreathe was comforting and pleasant. For instance, S4 stated that “this [vibration] gives me a relaxed feeling.” S2 thought the vibrotactile guidance had relaxing benefits “this smooth vibration helps me well to get into my body and let go of all kinds of thoughts for a while.” Similarly, S1 mentioned that “the subtle vibration guidance calmed me down and helped me to concentrate and relax”. However, the clarity of the information conveyed through the vibration can be improved. S2 and S3 indicated they could not always follow the tactile guidance. “Sometimes it is hard to feel the rhythm (S2).” “The transitions between breathing-in and breathing-out were not clearly distinguished, so sometimes I didn’t know when to breathe in, and when to breathe out (S3).” And S1 also stated that “the vibration is sometimes too subtle, only when I was very focused, I can clearly feel the rhythm of guidance.”
7.4. Users’ appreciation of holding soft tangible artifact for breathing training
Three participants mentioned the tangibility of ViBreathe is what they like best. For example, as S3 said, “It is more fun to grab a physical gimmick, I hold it to feel the guidance during slow breathing, and I can also play with it at hands, squeeze it like a hand toy, a stress ball.” S1 stated that “it is a physically fun and handy device, very simple to handle; the soft cover material is very user-friendly.” The participants also indicated their preference for ViBreathe compared to an APP on a smartphone. As S2 said, “I think it [ViBreathe] is better than many smartphone apps for meditation and relaxation, because I felt more concentrated when I closed my eyes and breathe deeply holding it.” And S4 also added to this, “It [ViBreathe] is a standalone device, the benefit of this is when you see it laying around you immediately think of its function.” Also, two participants responded they would prefer this technology to be integrated into an everyday object in the workplace. According to them, potential objects could be a pen, a mug, or a computer mouse.
In summary, these results suggest that the eye-free breathing guidance provided by the ViBreathe tangible interface has great potential as a handy tool for respiration training and stress mitigation at a workplace. The tangible interface may remind users to use it in their work breaks, increasing the frequency of casual respiration training at work. The breathing guidance from a solely vibrotactile display is comforting and pleasant and could help users to regulate breathing with eyes closed, which makes them more mindful and relaxed. But the clarity of haptic display could be improved in future development.
8. Discussion and design implications
In the past two decades, feedforward guidance and HRV biofeedback have been widely studied and recognized as two different methods for respiration training. Feedforward guidance enables users to practice slow breathing by matching their breath to a guiding pattern (Chittaro & Sioni, Citation2014; Gavish, Citation2010; Paredes et al., Citation2018). HRV biofeedback communicates real-time HRV data as performance feedback, so that users can accordingly adjust their performance, and gradually develop their breathing skills: e.g., resonant breathing (Lehrer et al., Citation2000). In this study, we have explored combining these two methods by integrating HRV data into a feedforward breathing guidance. By doing so, we intend to improve user experiences of existing breathing guidance, namely to reduce respiratory fatigue or enhance user engagement during the training. Two types of HRV-enhanced breathing guidance, responsive guidance and adaptive guidance, have been developed and evaluated. Our results suggested that the adaptive guidance could significantly reduce the difficulty and improve user comfort in the training, and the responsive guidance might make users more motivated and engaged in breathing regulation. In addition to these advantages on user experience, the results of HRV indices suggested that the two HRV-enhanced breathing guidance modes and the standard mode did not show significant differences in terms of effects on users’ HRV data.
The qualitative results provided consistent yet more detailed information about user experiences of each type of breathing guidance. The fixed-paced standard guidance requires low mental effort to learn, but over time and with repeated exposure, the users are easy to get fatigued, bored, distracted, or sleepy. These findings are in line with previous research by Gomez et al. (Citation2009) and Yu, Hu et al. (Citation2018) that shows users tend to enter a fatigued state and return to their habitual breathing pattern after a few minutes of deep breathing. The responsive guidance informs users about the training results and enriches tactile feelings. This added HRV feedback makes users more motivated, concentrated, engaged in breathing regulation but may also cause extra information load for users to perceive the guiding information, by requiring their extra attention and mindfulness in training. The adaptive guidance could change the guiding pace, which reduces the difficulty in the training and improves comfort and satisfaction, especially when users felt fatigue in practice. Adaptiveness of the guidance makes the training process more interactive and enjoyable so that the users reported a higher engagement and less boredom. However, the continuous changes of the guidance also require efforts from users to learn the updated pattern.
Moreover, the ViBreathe system has also been evaluated in our field study in which four office workers used ViBreathe at their workplace for five workdays. The aim was to contextually probe the design opportunities and implications for embedding short-term, easy-to-initiate breathing trainings into the everyday work routines of knowledge workers. The rich results show that it is a promising design direction for future development. Namely, the participants reported that the eye-free guidance and the textile-based tangible interface give ViBreathe great potential as a soft and inviting object for users to hold in respiration training and stress mitigation at the workplace. Based on the above quantitative results and qualitative findings, a set of implications for the design of HRV-enhanced breathing guidance for everyday contexts are summarized as follows.
8.1. Designing adaptive guidance to prevent fatigue and enhance comfort
The adaptive user interface has been recognized as a promising direction in HCI design (Rothrock et al., Citation2002). Based on physiological indices, the system feedback and user interface could be adapted to users’ physiological and affective states to facilitate natural human-computer communication (Nasoz & Lisetti, Citation2007; Saiwaki et al., Citation1996). As suggested by Bell and Kozlowski (Citation2008), in a learning or training process, adaptive guidance also shows advantages in the involvement of the learner in a learning process, resulting in improved satisfaction and outcomes. According to Jackson et al. (Citation2001), the task’s challenge and user’s ability should be adapted continuously in a dynamic balance to maintain users in a flow state, in which the training is more likely to result in both desirable results and pleasant user experiences. However, as documented in Yu, Hu et al. (Citation2018), the traditional respiration training is insufficient to keep users in a ‘flow’ state, because of the feelings of fatigue or boredom of following the repetitive, invariable pace of the breathing guidance. Although such fixed guidance is usually set as an ideal pace for users to follow, it lacks adaptiveness to users who differ in their inherent physiological features, existing breathing skills, as well as current states (e.g., whether they feel tired and need to take it easy for a few seconds) in a moment of training.
The results of this study have shown some promises of adaptive breathing guidance. A recently similar study (Leslie et al., Citation2019) exploring personalized musical breathing guidance has also shown that adaptive guidance could be more effective in slowing down breathing rates and leading to a more calm state. The adaptive guidance enables the flexibility for the system to fit different individuals. For those participants who performed well, their increase of HRV influenced the guidance to gradually turn slower, stretching their breathing pace toward their maximum breathing pace. And when the participants felt fatigue in continuing following it, they took a few breaths at their habitual pace, and then their HRV measures decreased. In response, the guidance became easier to follow. Such a dynamic process can be described as an interactive “negotiation” between the user and the adaptive guidance; it could therefore gradually persuade the user to increase performance. In this way, as suggested in the qualitative data, the adaptive guidance avoided users from feeling obliged to follow the fixed optimal pace of breathing guidance. Therefore, they experienced more comfort, less fatigue, or challenge in training with adaptive guidance.
Besides proving the benefits of user-adaptive guidance in improving user experiences, our empirical study also revealed some design implications on how to better leverage the user-adaptive mechanism in breathing guidance. During the experiments, we also observed how the participants “negotiated” with the adaptive guidance. In our observation, a few participants tended to stay in their “comfort zone” of breathing (rather than actively increasing their performance), and thus their training results may be somewhat weakened. This implies that the adaptive guidance design could involve an incentive mechanism to further motivate users to maximize their breathing performance and avoid them staying inside their “comfort zone” throughout the training. In other words, HRV-adaptive guidance offers an effective way of reducing the challenge to match a user’s capability, but still needs an approach of increasing challenges to keep the user in a flow state, gaining high training effects. For example, a possible design solution would be: when the system detects the user’s HRV stays lower than a pre-set threshold for a certain period, the pace of guidance is going to be extended programmatically to nudge the users to breathe a bit slower.
8.2. Designing performance feedback to engage users with respiration training
The role of feedback in learning and motivation has been well researched, i.e., by Nicol and Macfarlane‐Dick (Citation2006) and Kiili (Citation2005). Like other self-learning processes, respiration training also requires users’ motivation and engagement in breathing regulation for habituating to a targeted breathing pattern. Our gathered user experiences suggested that the HRV feedback integrated with the responsive guidance helped to maintain a user’s attention and concentration in training. Beyond merely following the guidance, the real-time HRV information of the responsive guidance could facilitate users in reflecting on and simultaneously adjusting their respiration for improving the results. However, we also found that simultaneously presenting feedback and feedforward guidance to users might increase their perceptual workload for interpreting their current performance based on the vibro-tactile pattern. Also, when users do not perform to expectations, the feedback on their performance may precipitate tension and negative attitude or emotions. These negative effects caused by performance feedback are reported in biofeedback breathing training (Yu, Hu et al., Citation2018) and common in motor skills training (Young et al., Citation2008) or e-learning program (Feidakis et al., Citation2012; Li et al., Citation2008).
Based on our empirical findings, we propose two suggestions for presenting HRV feedback with feedforward breathing guidance. First, we suggest condensing HRV data into a low-resolution indicating scale and reducing the feedback fidelity to prevent information overload. This helps a designed HRV feedback to be more effortless for users to perceive, and thus they can be more focused on practicing breathing relying on the feedback rather than interpreting the feedback per se. As indicated by Willems et al. (Citation2015), it takes less mental effort for users to process low-resolution information, i.e., information that is provided with low-fidelity and in smaller bits. Therefore, taking ViBreathe as an example, for future design, we suggest compressing HRV data (typically ranging from 10 to 180 ms) into a low-resolution scale (i.e., from 1 to 10 score) to map with roughness level and presenting the HRV feedback only at the intervals between the guiding breath cycles (5–10 Hz) instead of being updated with each heartbeat (generally at 75 to 120 Hz). Thus, during each breath cycle, the users can focus on matching to feedforward guidance, and after finishing each breath cycle, they can also be engaged with their HRV results.
Second, we suggest designing a feedback mechanism that “rewards” users’ good performance rather than “indicating” their poor performance. For instance, seven participants in our experiment expressed that the increasing roughness seemed as a “negative alert (S5)”, “felt pressured (S14)” and “brought anxiety (S12).” Thus, we suggest presenting HRV feedback only when the results are good and in a clear positive form-giving, which could be perceived as a reward or pleasure. For instance, some participants suggested just using a brisk haptic cue as a reward when they perform well.
8.3. Leveraging handy tangibles to embed breathing training into daily routines
Being a soft tangible interface that can be touched, held, and squeezed, ViBreathe enriched the user–device interaction beyond digital graphics. In this way, ViBreathe was reported to have afforded users’ enjoyable experiences from fiddling with its Cashmere wool cover, and their mindfulness in receiving breathing guidance from subtle vibration. Our field study thereby has revealed the strengths of a soft tangible artifact in supporting users’ “micro” breathing training during their daily office routines. Moreover, as reported, its physical presence served as a contextual cue, or inherent feedforward (Wensveen et al., Citation2004), which reminded users to improvise a short respiration training without having to consciously plan the timing. Also, its haptic information is experienced as unobtrusive and intimate at open workplaces, since only the user him/her-self could receive it. Besides, without intrusively requesting attention from users, ViBreathe can be easily shifted to the “background” of the surrounding when users are engaged in busy tasks. In this sense, Vibreathe seems to suggest a different design possibility than the current commercial respiration training applications on the mobile devices. Namely, those mobile commercial applications often push notifications or send reminders to users, in order to make them regularly check the mobile device, enter the training application, and continue their training exercise, which can be intrusive to their daily life. Differently, as depicts, Vibreathe is designed to fit into the physical surrounding of an office setting, stay within reach of the user, and afford the user’s spontaneous fiddling with its soft textile without requiring the user’s focal (visual) attention. Such lightweight, short-term and serendipitous way of performing breathing training could greatly benefit the daily stress management capability of office workers and suggest promising design space that needs further exploration.
As a result, our case of Vibreathe has demonstrated that it is meaningful to explore the design space of using everyday objects as a tangible medium for haptic breathing guidance. We hence suggest more future works exploring embedding breathing guidance into everyday tangibles that are frequently used, fiddled with, or grasped in our daily context (e.g., a mouse, a pen, or a mug). For instance, when the ambient system detects that an office worker picks up his/her coffee mug, the mug can start to provide him/her nuanced haptic cues about slow breathing. In this way, an everyday handy tangible can find some short and nonsignificant moments to afford (rather than explicitly instruct) the user to take a few deep and slow breaths. In other words, besides pushing users into respiration training through intrusive notifications on mobile devices, we could also carefully design their physical surroundings of users, in order to afford their spontaneous, self-initiated, inattentive breathing practice that takes place in the midst of their work, without disrupting their existing workflows. This could serve as an unobtrusive complementary approach in addition to existing approaches, such as notifications, to more effectively promote the healthy behaviors of users. It is in this sense we argue that slow breathing training can be weaved into the unremarkable routines of users without requiring their focal attention or paralyzing their unfolding workflow.
9. Concluding remarks
This paper presents the design of ViBreathe, a tangible respiration training system that aims at facilitating users to unobtrusively practice slow breathing at small moments of time during work. We have also evaluated two novel designs of HRV-enhanced haptic breathing guidance, which are meant for enhancing user experiences with respiration training. Responsive guidance presents HRV as an extra performance feedback in addition to the feedforward guidance. Adaptive guidance adjusts the pace of the feedforward guidance based on the user’s real-time HRV level. Such responsive and user-adaptive types of breathing guidance have meaningfully increased the interactivity of traditional feedforward-only breathing guidance. As demonstrated in the findings, the performance feedback of responsive guidance was experienced to have made the users mindfully deliberate on their current performance. This increased their engagement and concentration during breathing training and avoided them feeling bored as they did when training with the standard guidance. As also demonstrated in the findings, the user-adaptiveness of adaptive guidance has significantly improved the comfort of training and lowered the challenge for the users. As appreciated by the users, adaptive guidance adjusted the difficulty of training according to the users’ current state and avoided the users feeling breathing fatigue. Moreover, as the users’ physiological data show, both responsive and adaptive guidance designs did not sacrifice the effectiveness of breathing training: besides their reported advantages regarding user experience, they were as effective as the standard guidance in improving the HRV and breathing rate of the users.
On top of that, based on interview data, we thoroughly examined both the positive aspects and negative aspects of all three types of breathing guidance that we evaluated. By doing so, we intend to practically inform future designers of when to use which type of breathing guidance design according to their design aims. Having examined the three different types of haptic breathing guidance in our first study, we then implemented adaptive guidance via the tangible interface of ViBreathe and conducted a field deployment with four participants in their own workaday contexts. The contextual data have revealed several benefits of using soft tangible artifacts for unobtrusively promoting micro breathing training in the midst of users’ work routines. Namely, the haptic tangible interface within reach of the users enabled them to receive the haptic guidance while simultaneously focusing on their tasks on the computer screen. Or, the users could choose to close their eyes for a few minutes when practicing breathing with the haptic guidance of ViBreathe. The soft Cashmere wool cover of ViBreathe encouraged the users’ to spontaneously touch, grab, or squeeze it. Since the users indeed enjoyed fiddling with it inattentively, ViBreathe could tacitly increase the chance for users to perform relaxation practice in their short work breaks. Additionally, the physical presence of this tangible artifact served as a contextual cue to subtly nudge the users to initiate breathing practice without explicitly requesting their focus (e.g., a notification from a mobile application); and the users could easily ignore this artifact as part of their physical background when they are engaged in busy tasks.
Consequently, this paper contributes a design exploration as well as a set of implications regarding tangible interface for biofeedback respiratory training. More specifically, we have proposed using soft everyday tangibles as media of breathing guidance and demonstrated how such a tangible artifact could unobtrusively help office workers to weave lightweight, short-term relaxation training into their busy workaday routines. This work hopes to provide a room for future discussion among HCI researchers who design the biofeedback devices and interactions.
Authors’ contributions
The third author and fourth author took the lead in conducting the in-lab user test and the field evaluation. The third author and first author led the technical development of Vibreath. The first author took the lead in data analyses. The first author and corresponding author led the writing of the paper. All authors have made contributions to this work, encompassing the technical development, research, analysis, or writing processes.
Acknowledgments
We would like to thank all our participants for their participation and our colleagues from Systemic Change Group of industrial design department in Eindhoven Technology University for their supports in our study and suggestions and comments for our manuscript.
Additional information
Funding
Notes on contributors
Bin Yu
Bin Yu is a data designer in Philips, and a guest researcher at the Department of Industrial Design (ID), Eindhoven University of Technology (TU/e). He received his Ph.D. from ID, TU/e (2018) and M.Sc. in Biomedical Engineering (2012) from Northeastern University (China). His research interests include biofeedback, healthcare, and data visualization.
Pengcheng An
Pengcheng An is a postdoctoral researcher in HCI. He received his Ph.D. (2019) from Eindhoven University of Technology on Peripheral Interaction and Ambient Intelligence, and M.Sc. (2014) in Industrial Design. His research encompasses design research in Calm Technology, Seamless Interaction, and emerging intelligent systems for augmenting the future of work.
Sjoerd Hendriks
Sjoerd Hendriks is an adjunct teacher and design researcher at Chalmers University of Technology, Sweden. He holds a MSc in Interaction Design from Chalmers (2020) and a BSc in Industrial Design from Eindhoven University of Technology, Netherlands (2018). His research interests include soma design, slow technology and biofeedback.
Ning Zhang
Ning Zhang is a lecturer at Shandong University of Science and Technology, and visiting researcher at Eindhoven University of Technology from 2017 to 2018. She received her Ph.D. (2018) from Nanjing University of Science and Technology. Her research interests include HCI and product designing for the elderly.
Loe Feijs
Loe Feijs is Emeritus Professor of Industrial Design at TU/e. He studied Electrical Engineering and holds a PhD in Computer Science. Feijs has coauthored three books on formal methods and over 200 publications. In 2020 Feijs has launched his personal brand LAURENTIUS LAB., connecting art, fashion, mathematics and creative programming.
Min Li
Min Li received B.E. degree from Zhejiang University, China and PhD degree from KU Leuven, Belgium. He has been with Lucent Bell Labs Research, Microsoft Research, UIUC, and IMEC. He is currently a Senior Principal Architect with NXP semiconductors. He is also an adjunct Associate Professor with Eindhoven University of Technology.
Jun Hu
Jun Hu is an Associate Professor in Design Research on Social Computing, at the Department of Industrial Design, Eindhoven university of Technology. He is a Distinguished Adjunct Professor at Jiangnan University and a Guest Professor at Zhejiang University. His research interests include social computing, cyber-physical systems, IoT, HCI, and design education.
Notes
1. MyBreathe iPhone app. http://BreathResearch.com, (accessed July 20, 2020)
2. Pranayama iPhone application. http://Saagara.com, (accessed July 20, 2020).
3. Breathe App in Apple Watch, https://www.stuff.tv/features/apple-watchs-breathe-app-simply-breathtaking, (accessed April 20, 2019).
4. HeartMath, emwave2: https://store.heartmath.com/emwave2, (accessed April 20, 2019).
References
- Abowd, G. D., & Mynatt, E. D. (2000). Charting past, present, and future research in ubiquitous computing. ACM Transactions on Computer-Human Interaction, 7(1), 29–58. https://doi.org/10.1145/344949.344988
- Alonso, M. B., Keyson, D. V., & Hummels, C. C. M. (2008). Squeeze, rock, and roll; can tangible interaction with affective products support stress reduction? Proceedings of the 2nd international conference on tangible and embedded interaction (pp. 105–108). https://doi.org/10.1145/1347390.1347413
- American Psychological Association. (2015). Stress in America: Paying with our health (pp. 9–14). Stress in America Survey.
- American Psychological Association. (2017). Stress in America: Coping with Change (pp. 2–6). Stress in America Survey.
- Amores, J., Fuste, A., & Richer, R. (2019). Deep reality: Towards increasing relaxation in VR by Subtly changing light, sound and movement based on HR, EDA, and EEG. Extended abstracts of the 2019 CHI conference on human factors in computing systems (pp. 1–2). https://doi.org/10.1145/3290607.3311770
- Azevedo, R. T., Bennett, N., Bilicki, A., Hooper, J., Markopoulou, F., & Tsakiris, M. (2017). The calming effect of a new wearable device during the anticipation of public speech. Scientific Reports, 7(1), 2285. https://doi.org/10.1038/s41598-017-02274-2
- Bell, B. S., & Kozlowski, S. W. J. (2008). Active learning: Effects of core training design elements on self-regulatory processes, learning, and adaptability. Journal of Applied Psychology, 93(2), 296. https://doi.org/10.1037/0021-9010.93.2.296
- Brown, R. P., & Gerbarg, P. L. (2005). Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression: Part II – Clinical applications and guidelines. Journal of Alternative and Complementary Medicine, 11(4), 711–717. Mary Ann Liebert, Inc. 2 Madison Avenue Larchmont, NY 10538 USA. https://doi.org/10.1089/acm.2005.11.711
- Chandola, T., Brunner, E., & Marmot, M. (2006). Chronic stress at work and the metabolic syndrome: Prospective study. BMJ, 332(7540), 521–525. https://doi.org/10.1136/bmj.38693.435301.80
- Chittaro, L., & Sioni, R. (2014). Evaluating mobile apps for breathing training: The effectiveness of visualization. Computers in Human Behavior, 40, 56–63. https://doi.org/10.1016/j.chb.2014.07.049
- Choi, K. Y., & Ishii, H. (2020). AmbienBeat: Wrist-worn mobile tactile biofeedback for heart rate rhythmic regulation. Proceedings of the fourteenth international conference on tangible, embedded, and embodied interaction (pp. 17–30). https://doi.org/10.1145/3374920.3374938
- Clark, M. E., & Hirschman, R. (1990). Effects of paced respiration on anxiety reduction in a clinical population. Biofeedback and Self-Regulation, 15(3), 273–284. https://doi.org/10.1007/BF01011109
- Costa, J., Adams, A. T., Jung, M. F., Guimbretière, F., & Choudhury, T. (2016). EmotionCheck: Leveraging bodily signals and false feedback to regulate our emotions. Proceedings of the 2016 ACM international joint conference on pervasive and ubiquitous computing (pp. 758–769). https://doi.org/10.1145/2971648.2971752
- Dijk, E. O., & Weffers, A. (2011). Breathe with the ocean: A system for relaxation using audio, haptic and visual stimuli. Special symposium at eurohaptics 2010: Haptic and audio-visual stimuli: Enhancing experiences and interaction, Amsterdam, The Netherlands.
- Esler, M., & Kaye, D. (2000). Sympathetic nervous system activation in essential hypertension, cardiac failure and psychosomatic heart disease. Journal of Cardiovascular Pharmacology, 35(7), S1–S7. https://doi.org/10.1097/00005344-200000004-00001
- Ettehadi, O., Jones, L., & Hartman, K. (2020). Heart waves: A heart rate feedback system using water sounds. Proceedings of the fourteenth international conference on tangible, embedded, and embodied interaction (pp. 527–532). https://doi.org/10.1145/3374920.3374982
- Feidakis, M., Daradoumis, T., Caballé, S., & Conesa, J. (2012). Design of an emotion aware e-learning system. International Journal of Knowledge and Learning, 38(3–4), 219–238. https://doi.org/10.1504/IJKL.2012.051676
- Fletcher, J. (2019). How to use 4-7-8 breathing for anxiety. Medical News Today. https://www.medicalnewstoday.com/articles/324417
- Frank, D. L., Khorshid, L., Kiffer, J. F., Moravec, C. S., & McKee, M. G. (2010). Biofeedback in medicine: Who, when, why and how? Mental Health in Family Medicine, 7(2), 85–91. https://pubmed.ncbi.nlm.nih.gov/22477926
- Gallace, A., & Spence, C. (2010). The science of interpersonal touch: An overview. Neuroscience and Biobehavioral Reviews, 34(2), 246–259. https://doi.org/10.1016/j.neubiorev.2008.10.004
- Gavish, B. (2010). Device-guided breathing in the home setting: Technology, performance and clinical outcomes. Biological Psychology, 84(1), 150–156. https://doi.org/10.1016/j.biopsycho.2010.02.013
- Ghandeharioun, A., & Picard, R. (2017). BrightBeat: Effortlessly influencing breathing for cultivating calmness and focus. In Proceedings of the 2017 CHI conference extended abstracts on human factors in computing systems (pp. 1624–1631). Association for Computing Machinery. https://doi.org/10.1145/3027063.3053164
- Gilbert, C. (2003). Clinical applications of breathing regulation: Beyond anxiety management. Behavior Modification, 27(5), 692–709. https://doi.org/10.1177/0145445503256322
- Gomez, C. L., Strongoli, L. M., & Coast, J. R. (2009). Repeated abdominal exercise induces respiratory muscle fatigue. Journal of Sports Science & Medicine, 8(4), 543. https://pubmed.ncbi.nlm.nih.gov/24149595/
- Harris, V. A., Katkin, E. S., Lick, J. R., & Habberfield, T. (1976). Paced respiration as a technique for the modification of autonomic response to stress. Psychophysiology, 13(5), 386–391. https://doi.org/10.1111/j.1469-8986.1976.tb00850.x
- Hirsch, J. A., & Bishop, B. (1981). Respiratory sinus arrhythmia in humans: How breathing pattern modulates heart rate. American Journal of Physiology-Heart and Circulatory Physiology, 241(4), H620–H629. https://doi.org/10.1152/ajpheart.1981.241.4.H620
- Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
- IJsselsteijn, W. A., De Kort, Y. A. W., & Poels, K. (2013). The game experience questionnaire. Technische Universiteit Eindhoven.
- Jackson, S. A., Thomas, P. R., Marsh, H. W., & Smethurst, C. J. (2001). Relationships between flow, self-concept, psychological skills, and performance. Journal of Applied Sport Psychology, 13(2), 129–153. https://doi.org/10.1080/104132001753149865
- Kiili, K. (2005). Digital game-based learning: Towards an experiential gaming model. The Internet and Higher Education, 8(1), 13–24. https://doi.org/10.1016/j.iheduc.2004.12.001
- Lehrer, P. M., Vaschillo, E., & Vaschillo, B. (2000). Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Applied Psychophysiology and Biofeedback, 25(3), 177–191. https://doi.org/10.1023/A:1009554825745
- Leslie, G., Ghandeharioun, A., Zhou, D., & Picard, R. W. (2019). Engineering music to slow breathing and invite relaxed physiology. 2019 8th international conference on Affective Computing and Intelligent Interaction (ACII) (pp. 1–7). https://doi.org/10.1109/ACII.2019.8925531
- Ley, R. (1999). The modification of breathing behavior: Pavlovian and operant control in emotion and cognition. Behavior Modification, 23(3), 441–479. https://doi.org/10.1177/0145445599233006
- Li, L., Cheng, L., & Qian, K. (2008). An e-learning system model based on affective computing. 2008 international conference on cyberworlds (pp. 45–50). https://doi.org/10.1109/CW.2008.41
- Miri, P., Flory, R., Uusberg, A., Culbertson, H., Harvey, R. H., Kelman, A., Peper, D. E., Gross, J. J., Isbister, K., & Marzullo, K. (2020). PIV: Placement, pattern, and personalization of an inconspicuous vibrotactile breathing pacer. ACM Transactions on Computer-Human Interaction, 27(1), 1–44. https://doi.org/10.1145/3365107
- Moore, S. K. (2006). Calm in your palm: Biofeedback device promises to reduce stress. IEEE Spectrum, 43(3), 60. https://doi.org/10.1109/MSPEC.2006.1604843
- Moraveji, N., Olson, B., Nguyen, T., Saadat, M., Khalighi, Y., Pea, R., & Heer, J. (2011). Peripheral paced respiration: Influencing user physiology during information work. Proceedings of the 24th annual ACM symposium on user interface software and technology (pp. 423–428). https://doi.org/10.1145/2047196.2047250
- Nasoz, F., & Lisetti, C. L. (2007). Affective user modeling for adaptive intelligent user interfaces BT - Human-computer interaction. HCI intelligent multimodal interaction environments. (J. A. Jacko (ed.). Springer Berlin Heidelberg.
- Nicol, D. J., & Macfarlane‐Dick, D. (2006). Formative assessment and self‐regulated learning: A model and seven principles of good feedback practice. Studies in Higher Education, 31(2), 199–218. https://doi.org/10.1080/03075070600572090
- Odom, W., Wakkary, R., Lim, Y., Desjardins, A., Hengeveld, B., & Banks, R. (2016). From research prototype to research product. Proceedings of the 2016 CHI conference on human factors in computing systems (pp. 2549–2561). https://doi.org/10.1145/2858036.2858447
- Padgett, D. A., & Glaser, R. (2003). How stress influences the immune response. Trends in Immunology, 24(8), 444–448. https://doi.org/10.1016/S1471-4906(03)00173-X
- Pal, G. K., & Velkumary, S. (2004). Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian Journal of Medical Research, 120(2), 115. https://pubmed.ncbi.nlm.nih.gov/15347862/
- Pan, J., & Tompkins, W. J. (1985). A real-time QRS detection algorithm. IEEE Transactions on Biomedical Engineering, BME-32(3), 230–236. https://doi.org/10.1109/TBME.1985.325532
- Papadopoulou, A., Berry, J., Knight, T., & Picard, R. (2019). Affective sleeve: Wearable materials with haptic action for promoting calmness. In N. Streitz & S. Konomi (Eds.), Distributed, ambient and pervasive interactions (pp. 304–319). Springer International Publishing.
- Paredes, P., & Chan, M. (2011). CalmMeNow: Exploratory research and design of stress mitigating mobile interventions. CHI ’11 extended abstracts on human factors in computing systems (pp. 1699–1704). https://doi.org/10.1145/1979742.1979831
- Paredes, P. E., Zhou, Y., Hamdan, N. A.-H., Balters, S., Murnane, E., Ju, W., & Landay, J. A. (2018). Just Breathe: In-car interventions for guided slow breathing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol, 2(1), 1–23. https://doi.org/10.1145/3191760
- Park, G., & Choi, S. (2011). Perceptual space of amplitude-modulated vibrotactile stimuli. 2011 IEEE world haptics conference (pp. 59–64). https://doi.org/10.1109/WHC.2011.5945462
- Park, S.-H., Jang, D.-G., Son, D.-H., Zhu, W., & Hahn, M.-S. (2009). A biofeedback-based breathing induction system. 2009 3rd international conference on bioinformatics and biomedical engineering (pp. 1–4).
- Patibanda, R., Mueller, F., Floyd, Leskovsek, M., & Duckworth, J. (2017). Life Tree: Understanding the design of breathing exercise games. Proceedings of the annual symposium on computer-human interaction in play (pp. 19–31). https://doi.org/10.1145/3116595.3116621
- Reiner, R. (2008). Integrating a portable biofeedback device into clinical practice for patients with anxiety disorders: Results of a pilot study. Applied Psychophysiology and Biofeedback, 33(1), 55–61. https://doi.org/10.1007/s10484-007-9046-6
- Rothrock, L., Koubek, R., Fuchs, F., Haas, M., & Salvendy, G. (2002). Review and reappraisal of adaptive interfaces: Toward biologically inspired paradigms. Theoretical Issues in Ergonomics Science, 3(1), 47–84. https://doi.org/10.1080/14639220110110342
- Russo, M. A., Santarelli, D. M., & O’Rourke, D. (2017). The physiological effects of slow breathing in the healthy human. Breathe, 13(4), 298–309. https://doi.org/10.1183/20734735.009817
- Saiwaki, N., Togashi, H., Tsujimoto, H., & Nishida, S. (1996). An adaptive interface based on physiological indices. 1996 IEEE international conference on systems, man and cybernetics. Information intelligence and systems (Cat. No.96CH35929), 4 (Vol. 4, pp. 2793–2798). https://doi.org/10.1109/ICSMC.1996.561383
- Schein, M. H., Gavish, B., Herz, M., Rosner-Kahana, D., Naveh, P., Knishkowy, B., Zlotnikov, E., Ben-Zvi, N., & Melmed, R. N. (2001). Treating hypertension with a device that slows and regularises breathing: A randomised, double-blind controlled study. Journal of Human Hypertension, 15(4), 271–278. https://doi.org/10.1038/sj.jhh.1001148
- Schipke, J. D., Arnold, G., & Pelzer, M. (1999). Effect of respiration rate on short-term heart rate variability. Journal of Clinical and Basic Cardiology, 2(1), 92–95. https://www.kup.at/kup/pdf/39.pdf
- Schnädelbach, H., Irune, A., Kirk, D., Glover, K., & Brundell, P. (2012). ExoBuilding: Physiologically driven adaptive architecture. ACM Transactions on Computer-Human Interaction, 19(4), 1–22. https://doi.org/10.1145/2395131.2395132
- Shelley, K., Shelley, S., & Lake, C. (2001). Pulse oximeter waveform: Photoelectric plethysmography. Clinical Monitoring, 420–428. https://www.kup.at/kup/pdf/39.pdf
- Shih, C.-H. (Iris), Tomita, N., Lukic, Y. X., Reguera, Á. H., Fleisch, E., & Kowatsch, T. (2019). Breeze: Smartphone-based acoustic real-time detection of breathing phases for a gamified biofeedback breathing training. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies, 3(4), 1–30. https://doi.org/10.1145/3369835
- Sisto, S. A., Tapp, W., Drastal, S., Bergen, M., DeMasi, I., Cordero, D., & Natelson, B. (1995). Vagal tone is reduced during paced breathing in patients with the chronic fatigue syndrome. Clinical Autonomic Research, 5(3), 139–143. https://doi.org/10.1007/BF01826195
- Sivakumar, G., Prabhu, K., Baliga, R., Pai, M. K., & Manjunatha, S. (2011). Acute effects of deep breathing for a short duration (2-10 minutes) on pulmonary functions in healthy young volunteers. Indian Journal of Physiology and Pharmacology, 55(2), 154–159. https://pubmed.ncbi.nlm.nih.gov/22319896/
- Sonne, T., & Jensen, M. M. (2016). ChillFish: A respiration game for children with ADHD. Proceedings of the TEI ’16: tenth international conference on tangible, embedded, and embodied interaction (pp. 271–278). https://doi.org/10.1145/2839462.2839480
- Steffen, P. R., Austin, T., DeBarros, A., & Brown, T. (2017). The impact of resonance frequency breathing on measures of heart rate variability, blood pressure, and mood. Frontiers in Public Health, 5, 222. https://doi.org/10.3389/fpubh.2017.00222
- Stein, P. K., Bosner, M. S., Kleiger, R. E., & Conger, B. M. (1994). Heart rate variability: A measure of cardiac autonomic tone. American Heart Journal, 127(5), 1376–1381. https://doi.org/10.1016/0002-8703(94)90059-0
- Vaschillo, E. G., Vaschillo, B., & Lehrer, P. M. (2006). Characteristics of resonance in heart rate variability stimulated by biofeedback. Applied Psychophysiology and Biofeedback, 31(2), 129–142. https://doi.org/10.1007/s10484-006-9009-3
- Wensveen, S. A. G., Djajadiningrat, J. P., & Overbeeke, C. J. (2004). Interaction frogger: A design framework to couple action and function through feedback and feedforward. DIS ’04 proceedings of the 5th conference on designing interactive systems: Processes, practices, methods, and techniques (pp. 177–184). https://doi.org/10.1145/1013115.1013140
- Willems, L., Tetteroo, D., & Markopoulos, P. (2015). Towards guidelines for the design of patient feedback in stroke rehabilitation technology. In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), (pp. 60–68).
- Windlin, C., Ståhl, A., Sanches, P., Tsaknaki, V., Karpashevich, P., Balaam, M., & Höök, K. (2019). Soma Bits-mediating technology to orchestrate bodily experiences. RTD 2019-Research through design conference 2019, the science centre, Delft, on 19th to 22nd March 2019.
- Young, C. A., Manmathan, G. P., & Ward, J. C. R. (2008). Perceptions of goal setting in a neurological rehabilitation unit: A qualitative study of patients, carers and staff. Journal of Rehabilitation Medicine, 40(3), 190–194. https://doi.org/10.2340/16501977-0147
- Yu, B., Feijs, L., Funk, M., & Hu, J. (2015a). Designing auditory display of heart rate variability in biofeedback context. In Proceedings of International Conference on Auditory Display (ICAD 2015) (pp. 294–298). https://smartech.gatech.edu/handle/1853/54153
- Yu, B., Feijs, L., Funk, M., & Hu, J. (2015b). Breathe with touch: A tactile interface for breathing assistance system BT – Human-computer interaction – INTERACT 2015. (J. Abascal, S. Barbosa, M. Fetter, T. Gross, P. Palanque, & M. Winckler (eds.)). Springer International Publishing.
- Yu, B., Funk, M., Hu, J., & Feijs, L. (2017). StressTree: A metaphorical visualization for biofeedback-assisted stress management. Proceedings of the 2017 conference on designing interactive systems (pp. 333–337). https://doi.org/10.1145/3064663.3064729
- Yu, B., Funk, M., Hu, J., & Feijs, L. (2018). Unwind: A musical biofeedback for relaxation assistance. Behaviour & Information Technology, 37(8), 800–814. https://doi.org/10.1080/0144929X.2018.1484515
- Yu, B., Hu, J., Funk, M., & Feijs, L. (2018). DeLight: Biofeedback through ambient light for stress intervention and relaxation assistance. Personal and Ubiquitous Computing, 22(4), 787–805. https://doi.org/10.1007/s00779-018-1141-6
- Yu, B., Hu, J., Funk, M., Liang, R., Xue, M., & Feijs, L. (2018). RESonance: Lightweight, room-scale audio-visual biofeedback for immersive relaxation training. IEEE Access, 6, 38336–38347. https://doi.org/10.1109/ACCESS.2018.2853406