Abstract
Objective: Poverty is related to increased grief-related mental health problems, leading some to suggest bereavement counseling should be tailored to income. However, information about accessibility and effectiveness of such counseling programs serving low-income households is scarce. This longitudinal study therefore investigated the association between poverty and complicated grief (CG), and the effectiveness of a community-based bereavement counseling program in serving low-income households. Methods: Two hundred eighty-eight participants (75% female) were enrolled. Loss-related and demographic variables were assessed at baseline. Regression analyses were used to investigate household income as a predictor of CG, and examine bereavement counseling effectiveness by comparing CG symptom change across three household income categories across three time-points: baseline (T1), T1 + 12 months (T2), and T1 + 18 months (T3). Results: Of all participants, 35.8% reported below poverty-threshold income, twice the general population’s rate. Multiple regression analysis indicated poverty-threshold income was a predictor of CG symptoms over and above demographic and loss-related characteristics. Three-way interaction analysis detected a significant treatment effect for study condition across time, but no differences in treatment effects across income. Conclusion: Lower household income was associated with higher CG symptoms. Since income did not predict differential treatment response, community-based bereavement counseling appeared no less efficacious for members of low-income households.
Clinical or methodological significance of this article: While previous research has indicated low income may be a risk factor for mental health problems after bereavement, and it has therefore been suggested bereavement counseling should be tailored to income, no study to date has investigated the need for such tailoring. This controlled, longitudinal treatment study fills this gap in knowledge. Main findings are that low income is a key predictor of complicated grief symptoms. The study also shows that the effectiveness of one-to-one bereavement counseling does not appear to differ according to income level.
ABSTRACT
Obiettivo: La povertà è connessa a un incremento dei problemi di salute mentale associati al lutto, tanto da indurre qualcuno a suggerire che il counseling per il lutto dovrebbe essere adattato al reddito. Tuttavia, i dati sull'accessibilità e sull'efficacia di questo tipo di programmi di counseling rivolti alle famiglie a basso reddito sono scarse. Questo studio longitudinale ha dunque indagato la relazione tra povertà e lutto complicato (CG), e l'efficacia di un programma di counseling per il lutto basato sulla comunità rivolto a famiglie a basso reddito. Metodi: Sono state reclutati 288 partecipanti (75% di sesso femminile). Le variabili relative al lutto e alle informazioni demografiche sono state valutate all’inizio. Le analisi della regressione sono state usate per studiare il reddito familiare come un predittore del CG, e per esaminare l'efficacia del counseling per il lutto confrontando il cambiamento dei sintomi del CG attraverso le tre categorie di reddito familiare in tre fasi: baseline (T1), T1+12 mesi (T2), T1+18 mesi (T3). Risultati: Di tutti i partecipanti, il 35.8% ha riportato un reddito sotto la soglia della povertà, il doppio rispetto al tasso della popolazione generale. L'analisi della regressione multipla ha indicato che il reddito alla soglia di povertà era un predittore dei sintomi del CG oltre e aldilà delle caratteristiche demografiche e legate alla perdita. L'analisi dell'interazione a tre vie ha individuato un significativo effetto del trattamento per la condizione studiata trasversale alle varie fasi, ma nessuna differenza nell'effetto del trattamento trasversale al reddito. Conclusione: Un reddito familiare inferiore era associato a maggiori sintomi di CG. Dato che il reddito non è stato predittivo di risposte differenti al trattamento, il counseling per il lutto basato sulla comunità è parso non meno efficace per i membri di famiglie a basso reddito.
Significato metodologico e clinico dell'articolo: Anche se la ricerca precedente ha indicato che un basso reddito può essere un fattore di rischio per i problemi di salute mentale dopo un lutto, ed è stato quindi suggerito che il counseling per il lutto venisse adattato in base al reddito, a oggi nessuno studio ha indagato la necessità di tale tailoring. Questo studio longitudinale e controllato del trattamento colma questo gap nella ricerca. I principali risultati indicano che un basso reddito è un predittore chiave dei sintomi di CG. Lo studio mostra anche che l'efficacia del counseling sul lutto uno-a-uno non sembra differire in base al livello di reddito.
摘要
目的:貧窮和哀傷漸增的心理健康問題有關,因此有學者建議應該依據案主收入調整喪親哀傷治療 方式。然而,目前非常缺乏低收入戶家庭獲得此類諮商服務之普及率與有效性的相關研究。本縱貫 性研究探討貧窮與複雜性哀傷(CG)之間的關聯,以及社區機構提供低收入戶家庭喪親哀傷治療之有 效性。方法:本研究共計288 位研究參與者(75%為女性)。研究初有蒐集與失落以及人口變項相關之 變項。使用迴歸分析來探討以家庭收入作為複雜性哀傷的預測因子,並比較三個不同家庭收入類別 的複雜性哀傷症狀在三個時間段:基準點(T1)、基準點後12 個月(T2),以及基準點後18 個月(T3)之 改變來檢驗喪親哀傷治療的效果。結果:在全體研究參與者中有35.8%的參與者家庭收入低於貧窮 線,高於一般大眾兩倍。多元迴歸分析指出家庭收入貧窮線比人口變項或與失落有關的特性更能預 測複雜性哀傷症狀。三向交叉分析顯示本研究處遇效果在三個時間點間有顯著成效,但在不同收入 家庭間比較則無顯著差異。結論:較低家庭收入與較多複雜性哀傷症狀相關。既然收入差異對於治 療反應無預測效力,社區機構所提供之喪親哀傷治療對於來自低收入戶的家庭成員不會有較差的效 果。
Resumo
Objetivo: A pobreza está relacionada ao aumento dos problemas de saúde mental relacionados ao luto, levando alguns a sugerir que o aconselhamento ao luto deve ser adaptado à renda. No entanto, informações sobre acessibilidade e eficácia de tais programas de aconselhamento que atendem a famílias de baixa renda são escassas. Este estudo longitudinal, portanto, investigou a associação entre pobreza e luto complicado (CG), e a eficácia de um programa comunitário de aconselhamento ao luto no atendimento de famílias de baixa renda. Método: Duzentos e oitenta e oito participantes (75% mulheres) foram recrutados. Variáveis demográficas e relacionadas com perdas foram avaliadas no início do estudo. Análises de regressão foram usadas para investigar a renda familiar como um preditor de CG e para examinar a eficácia do aconselhamento de luto comparando a mudança de sintomas em três categorias de renda ao longo de três momentos: início (T1), T1 + 12 meses (T2) e T1 + 18 meses (T3). Resultados: De todos os participantes, 35.8% relataram renda abaixo do limiar da pobreza, o dobro da taxa da população geral. A análise de regressão múltipla indicou que a renda de limiar de pobreza era um preditor de sintomas de CG, além das características demográficas e relacionadas à perda. A análise de interação de três vias detectou um efeito de tratamento significativo para a condição do estudo ao longo do tempo, mas não houve diferenças nos efeitos do tratamento em relação à renda. Conclusão: A menor renda familiar associou-se a maiores sintomas de CG. Uma vez que a renda não previu resposta diferencial ao tratamento, o aconselhamento de luto comunitário não pareceu menos eficaz para os membros de famílias de baixa renda.
Significância clínica ou metodológica deste artigo: Embora pesquisas anteriores tenham indicado que a baixa renda pode ser um fator de risco para problemas de saúde mental após o luto, e portanto tenha sido sugerido que o aconselhamento de luto deve ser adaptado à renda, nenhum estudo até o momento investigou a necessidade de tal adaptação. Este estudo longitudinal controlado preenche esta lacuna no conhecimento. Os principais achados são que a baixa renda é um preditor-chave de sintomas de luto complicado. O estudo também mostra que a efetividade do aconselhamento individual de luto não parece diferir de acordo com o nível de renda.
Parole chiave:
Palavras-chave:
The role of poverty as a risk factor for complicated grief (CG) has been the subject of debate. Some research into responses to bereavement has associated low income with higher levels of grief-related symptoms (Burke & Neimeyer, Citation2013). Generally, lower absolute incomes correspond with greater psychological distress (Garratt, Chandola, Purdam, & Wood, Citation2016), and an increased likelihood of experiencing mental and physical health problems (Robson & Gray, Citation2007; Santiago, Kaltman & Miranda, Citation2013). Notably, Cacciatore, Killian, and Harper (Citation2016) showed that low income had a stronger correlation with symptoms of depression, anxiety, and posttraumatic stress than recognized loss-related and demographic predictors of grief symptom complexity in parents bereaved of a child. This has led these authors to suggest that bereavement counseling programs should be tailored to income, by countering structural and attitudinal barriers to counseling uptake. To assess the need for such tailoring, the present study aims to investigate: (i) the relationship between income and grief symptom severity in a counseling-seeking sample; and, equally important; (ii) if the effectiveness of a community-based bereavement counseling intervention is influenced by participants’ income levels.
Given that low income has been identified as a risk factor for mental health problems, there are good reasons to seek to clarify the impact of poverty on adaptation to bereavement (Burke & Neimeyer, Citation2013). One major concern is whether low-income bereaved people are able to receive healthcare if and when they need it: do they, for example, have as easy access to professional services as people in higher income groups? This may not be the case. Living in poverty can limit an individual’s ability to access psychological support or practice psychological self-care (Thompson, Citation2002; Doornbos, Zandee, de Groot & Warpinski, Citation2013). One reason for this may be that people living in low-income households hold negative attitudes toward help-seeking. This reluctance to seek help may partly stem from a prevailing social norm that one should simply be “getting on with it” (Allen, Citation2007, p. 80). Additionally, structural barriers to receiving care may also play a part. First, service accessibility may be lower for the people from low-income households, that is, reflecting a lack of equitable distribution of services vis-à-vis the population they are intended to serve. Second, service acceptability may be inadequate for lower-income bereaved people, if for example the program and its providers are inappropriate to the population they serve (WHO, Citation2017).
An additional challenge to evaluating the accessibility and acceptability of care to low-income bereaved people is the lack of basic information concerning the proportion of this group wishing to receive support, and the extent to which interventions for bereavement-related grief are currently available (Stephen et al., Citation2009). The present research took place in the UK, where all residents have full medical coverage through a state-supplied healthcare system, the National Health Service (NHS). (A similar degree of nearly universal medical coverage, independent of financial status, exists in most developed countries.) Pathways to bereavement care through biomedical resources such as the NHS in the UK remain largely uncharted. To date, NHS recordkeeping generally does not collect data on bereavement-related patient health visits, leaving little opportunity to document any grief support services delivered (Stephen, Wilcock, & Wimpenny, Citation2013). It is currently estimated that between 70% and 90% of bereavement support in the UK is delivered through the non-profit sector, with similar estimates for care provision through non-profit hospices and palliative care organizations in Australia, Japan, and the US (Breen, Aoun, O’Connor & Rumbold, Citation2013). Whether such care is accessible, acceptable, and indeed efficacious for people living in relative poverty remains largely unexplored.
There are reasons to believe that an approach to bereavement intervention offering appropriate degrees of accessibility and accessibility for people from low-income households might be effective. For example, positive outcomes have been demonstrated for people from low-income households who received interventions tailored to increase acceptability and accessibility of therapy for other psychiatric disorders, including PTSD (Krupnick, Citation2002) and panic disorder (Roy-Byrne et al., Citation2006). In a review of successful, evidence-based psychotherapeutic interventions designed to support people from low-income households, Santiago et al. (Citation2013) list a number of practices that have been shown to increase uptake of services among low-income study participants. These include the provision of practical support, such as childcare and food, and additional outreach steps to encourage retention and participation. These recommendations, however, are at odds with another practice that has been shown to improve bereavement intervention outcomes, namely the provision of care on an in-reaching basis (i.e., bereaved people actively seek bereavement intervention themselves, instead of being contacted by the bereavement support organization (Schut et al., Citation2001). It would seem that while facilitating uptake of bereavement support—making it possible for people to attend sessions—might be beneficial, incentivizing uptake in such a way that encourages use of services where they may not actually need them could be unhelpful or even detrimental. (Incentivizing use of counseling services in this context might consist of offering users certain benefits, such as free childcare or snacks during visits.) Efforts to tailor bereavement support services to increase acceptability and accessibility among people from low-income households must, therefore, keep a delicate balance between facilitating but not incentivizing support.
With these considerations in mind, the present study sought to address the gaps in knowledge noted above by examining the uptake and effectiveness of bereavement support among bereaved people from households from below the poverty threshold. Specifically, we looked at a model of bereavement counseling offered nationwide through a community-based non-profit organization that operates to professional standards. Working with longitudinal data from a larger research project, “Coping with Bereavement in Scotland,” the study featured a naturalistic, controlled design, and compared outcomes for participants across income levels.
The investigation had three primary objectives. First, we aimed to establish a preliminary indication of the percentage of help-seeking bereaved people who were living in relative poverty. Specifically, we calculated which proportion of our naturalistic sample (comprised of people who had contacted a national community-based bereavement support organization in Scotland) represented people living at or below the poverty threshold. Although the non-profit organization offers services free of charge and with extended hours, no specific strategies had been implemented to make the service available to people from low-income households. We therefore expected the proportion of participants living at or below the poverty threshold to be underrepresented.
Second, following indications from Cacciatore et al. (Citation2016) that income is a strong predictor of loss-related depression, anxiety, and posttraumatic stress symptoms, we examined the association between income and grief levels among help-seeking bereaved adults. We expected to find a strong effect of poverty on CG symptoms even compared to other recognized predictors of CG, including cause of death and gender. In line with Cacciatore et al.’s (Citation2016) suggestion that the ability to provide effective self-care is lower among people with lower incomes, we expected to find an inverse relationship between income and CG levels. For the purposes of this study, CG was defined as “[a] deviation from the normal (in cultural and societal terms) grief experience in either time course or intensity of specific or general/reactions or symptoms of grief” (Stroebe, Schut & Boerner, Citation2017, p. 3).
Third, we examined the effectiveness of a community-based bereavement counseling program in supporting bereaved adults living at or below the poverty threshold. In a quasi-randomized controlled effectiveness investigation, we used three-way multilevel regression interaction analysis to examine the effect of household income (poverty threshold and below, low to below median, and median and above) and study condition (bereavement counseling vs. no intervention) on CG levels over an 18-month study period. While previous research has demonstrated the effectiveness of the same counseling intervention in reducing CG symptoms as compared to a no-invention control condition (Newsom et al., Citation2017), income had not yet been examined as a moderator of treatment effects. Though the intervention was community based, it was not tailored specifically toward supporting people with low-income levels. Following Cacciatore et al. (Citation2016), this could mean that it would be less effective for people from low-income households. We therefore expected to see a smaller magnitude of change in CG means between treatment conditions over time among the low-income group, compared to higher income groups.
Method
Two hundred eighty-eight residents of Scotland (age 18+) who had been bereaved for at least six months and requested support from Cruse Bereavement Care Scotland (CBCS) participated in the study. People requiring specialized support (language interpretation, support for cognitive impairment) were excluded from the study, as were people who were already receiving outside professional help for grief or other/additional psychiatric conditions or diagnoses at baseline (e.g., substance abuse, psychosis, schizophrenia). All participants had received an intake assessment result of 18 or higher on the Indicator of Bereavement Adaptation—Cruse Scotland (IBACS) (Newsom et al., Citation2016), indicating that intervention would be appropriate.
Sample Characteristics
presents details of participants’ baseline characteristics. The majority (78%) of participants were female, with a mean age of 49.2 years (SD = 13.35), and were bereaved of a parent (37%) or spouse (37%). Sixty-three percent of participants had been bereaved within the previous 12 months, and 92% within the last 3 years. Forty-three percent reported taking anti-anxiety or anti-depressant medication at baseline. Participants showed a range of income levels, with approximately a third (35.8%) from households at or below the poverty threshold; 27.8% from below-median income households, and 36.5% from households at median income and above. As residents of Scotland, all participants were entitled to full-service medical care from the NHS, including any prescription medication, at no cost to themselves.
Table I. Baseline personal characteristics by study condition and income group.
Sampling Procedure
Participants for the present study were drawn from a larger efficacy study “Coping with bereavement in Scotland” (cf., Newsom et al., Citation2017). Of the 344 participants enrolled in that study, the 84% who provided household income details (N = 288) comprised the sample for the present study. There were no differences between study accepters and decliners (i.e., participants who did and did not provide income information, respectively) on age, gender, risk of complications, and severity of grief symptoms (as indicated by IBACS intake assessment results—see next paragraph), use of medication or CG symptom levels as measured by the Inventory of Complicated Grief-Revised (ICG-R; Prigerson & Jacobs, Citation2001).
An institutional ethics review was conducted with approval granted by the NHS Tayside Research Ethics Committee 1 (IRAS project ID 56758) in November 2010. Recruitment for the larger study was conducted between January 2011 and September 2011. Prior to enrollment, participants received a written description of the research study and informed consent statements to sign and return. Participants also received informational materials from CBCS providing basic information about coping with grief, and spoke over the phone with a CBCS staff member or trained volunteer to provide details concerning the circumstances surrounding their bereavement, and contact and scheduling information. All participants also completed the IBACS, a semi-structured intake assessment for bereavement intervention, which was delivered either in person or over the telephone (Newsom et al., Citation2016).
Intervention Model
Organizational setting
CBCS is a non-profit organization that provides counseling and informational support services to bereaved people. CBCS provides 55,000 hours of support each year and responds to over 12,000 requests for help. Help-seeking people contact CBCS via a national phone line and are then directed to their nearest service location. The national telephone line operates throughout the week, days, and evenings. CBCS service locations are distributed throughout Scotland across rural and urban settings. Local services contact clients by telephone, or receive calls from them, to schedule sessions at mutually agreeable times. Sessions are available days and evenings during the week, and, in many locations, during the daytime on weekends. No fees are charged for CBCS services, but clients are informed of how donations can be made to CBCS if they wish.
Counselors are volunteers who have been professionally trained at a minimum to the standards of Scotland’s professional body for counseling and psychotherapy (COSCA), and have completed a bereavement-specific training module. CBCS recruits volunteer counselors on a semi-annual basis from within the communities that the organization serves. A local selection committee works with national training staff to select volunteers for training, which takes a year (for volunteers who are not counselors or psychologists by profession). Certification is transferrable and is paid for by CBCS. All counselors receive regular professional supervision, and fulfill a minimum continuing professional development commitment of a minimum of 11 hours per year.
Counseling model
The CBCS model for bereavement counseling is a hybrid approach, combining elements of the cognitive behavioral, person-centered and psychodynamic traditions (see Newsom et al., Citation2017; Simonsen & Cooper, Citation2015). Following standard CBCS practice, bereaved people who have contacted the organization seeking support—and who have been bereaved for at least six months, a point by which time the intensity of a typical bereavement response tends to subside (see Shear, Citation2015)—will participate in an intake process either in person or over the telephone. This intake process entails the use of the Indicator of Bereavement Adaptation Cruse Scotland (IBACS; see Newsom et al., Citation2016) to assess the risk and magnitude of the bereaved person’s difficulties coping with grief. IBACS scores indicating that the bereaved person is coping successfully result in a recommendation for watchful waiting, whereas indications that the bereaved person would benefit from intervention result in an allocation to a counselor. Allocation to counselors is based primarily on the level of symptoms and risks of developing complications at intake. Bereaved people with IBACS results >18 are assigned to counseling, and those with higher symptom levels (IBACS > 29) are assigned to more experienced counselors. Scheduling compatibility is a secondary factor in allocation to a counselor.
Procedure
A quasi-randomized approach was used to assign participants to study conditions. Following the naturalistic design of the larger study, participants who were allocated to a counselor and attended sessions were assigned to the intervention category. Participants were assigned to the control condition when they were unable to receive intervention due to personal scheduling conflicts, found their local service location was too distant or inconvenient to attend, or were on a waiting list at their local service location.
In the present investigation, intervention participants were assigned to counselors following standard CBCS procedure (as described above in the “Counseling model” section), with sessions were delivered on a one-to-one basis at CBCS service locations. Meeting rooms were simply and comfortably furnished and provide a quiet, private space for discussion. Sessions were held on a weekly basis, and participants met the same counselor at each session. Participants attended an average of 6 sessions (M = 5.80, SD = 2.95).
Measures
Data collection was completed using postal questionnaires distributed at three time-points: baseline (T1), 12 months later at post-measure (T2), and 18 months after baseline at follow up (T3). Participants who did not respond to a questionnaire were sent a reminder letter. If they did not respond to this second communication, they were considered to have dropped out of the study.
Complicated grief
The Inventory of Complicated Grief-Revised (ICG-R, Prigerson & Jacobs, Citation2001), a 30-item questionnaire, was used to assess symptoms of CG. The ICG-R is widely used and has demonstrated strong internal consistency (Cronbach’s α = .94) (Prigerson & Jacobs, Citation2001). Construct validity for the ICG-R has also been demonstrated through convergence with the Traumatic Grief Evaluation of Response to Loss (Prigerson & Jacobs, Citation2001). Excellent reliability, α = .95, was demonstrated at baseline, and increased slightly at post-measure and follow-up, α = .96.
Demographic and bereavement-related characteristics (including income)
A bespoke questionnaire was designed to assess demographic details (age in years, gender, medication use) including household income (“What is your yearly household income?”); and bereavement-related characteristics (cause of death, kinship of the deceased person, time since loss).
Gross household income was measured using a scale of six categories in addition to a seventh non-response option (“under £10,000; from £10,000–£19,999; from £20,000 to £29,999; £30,000 to £39,999; £40,000 to £49,999; £50,000 and above; prefer not to say”). The relative poverty metric, a widely used approach for assessing household poverty in the UK, was applied to identify participants living in deprived circumstances. Following this approach, people whose household incomes are at least 60% less than the national median are considered to live in relative poverty (see Mack, Citation2016). Guidelines from the Scottish Government (Citation2012), which were developed on this basis, indicated that the period of baseline data collection (2010–2011), one-person households reporting an income below £10,000 fell below the poverty threshold; those reporting £10,000–19,999 and £20,000–29,999 were below median; and those reporting £30,000 and above were at or above the median income level. In the present study, because in certain cases it was unclear how many people lived in participants’ households, all participants were treated as single-person households. Applying the highest cut-offs for income groups reduced the risk of false positives for poverty-level households; however, participants in the lowest and middle categories who had additional household members may, therefore, have experienced more deprivation than the income variable indicates. (Notably, Stephen et al. (Citation2013) demonstrated that equivalised income (i.e., household income that has been recalculated to take into account differences in household size and composition) remained the same before and after bereavement.)
After data collection was completed, self-reported household income data were used to assign participants to one of three income categories:
Lowest, whose income levels were at or below the poverty threshold;
Low-median, whose income levels were above the poverty threshold but below the median, and still including households at risk of real deprivation; and
Median-high, whose income levels were median and above median.
For the 2010–2011 period, which corresponds with data collection at baseline (including household income data) it was estimated that 14% of working-age adults and 16% of pensioners in Scotland lived in relative poverty (Scottish Government, Citation2012).
Research Design/Analyses
Analyses for the present study were divided into three sets. First, to establish an indication of the percentage of help-seeking bereaved people who are living in relative poverty, a cross-sectional analysis was conducted to calculate the proportion of participants in our sample who were living at or below the poverty threshold. To provide an initial indication of the degree of the intervention program’s accessibility and acceptability for people from low-income households, we compared the proportion of participants in the “poverty” group to this proportion of the Scottish general population.
Second, to test the predictive value of income on CG at baseline, a multiple regression model was developed. Seven independent variables were entered into the model as predictors. These included demographic characteristics: (i) participant’s age; (ii) gender; (iii) income group (three categories: lowest, low-median, median-high); (iv) use of anti-depressant/anxiolytic medication at baseline (yes, no) and bereavement-related characteristics; (v) cause of death (illness/health problem, accident, suicide, homicide, other/unknown); (vi) kinship of the deceased (partner, parent, child, sibling, other relative/friend); and (vii) time since bereavement (five categories: 6 months; between 6 and 12 months; between 1 and 2 years; between 2 and 5 years; 5 years or more). Following indications from Cacciatore et al. (Citation2016), we expected income to demonstrate the strongest effect on CG symptoms.
Third, to determine whether study condition and income interacted to predict mean scores in participants’ CG symptom levels across time, a three-way multilevel multiple regression model using Maximum Likelihood estimation was developed in SPSS (version 23). To account for high inter-subject correlation (through repeated measures), a hierarchical linear mixed-effects approach was used, with a random effect for participant ID, and fixed effects for the three predictor variables: income group (three categories), study condition (two categories) and time (three categories). Preliminary analyses were conducted to ensure there was no violation of the assumptions of linearity, an absence of multicollinearity, homoscedasticity, and normality of residuals. Personal and loss-related characteristics that were unevenly distributed across income groups were added to the statistical model as covariates to control for differences and to partly account for between-subject variability.
A significance level was established at α = 0.05 (two-sided) and would pertain to all tests conducted in this study. To examine effect sizes within a mixed model, R2 is reported. Because of the presence of random effects in the model, R2 was computed from the residual variance by subtracting the variance of the model with predictors from the variance of the null model, then dividing by the null model (Peugh, Citation2010; Selya, Rose, Dierker, Hedeker & Mermelstein, Citation2012).
Results
Participant Flow
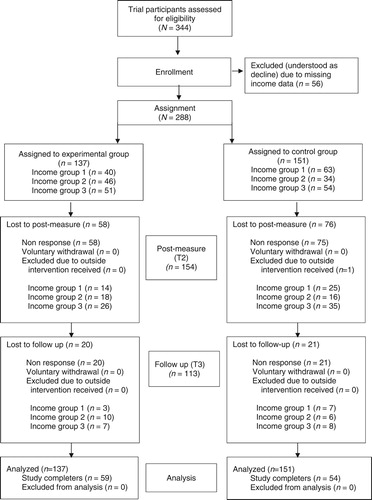
describes participation across the two study categories, including income category information. At baseline, a total of 288 participants were enrolled. One hundred thirty-seven participants were assigned to the intervention condition, and 151 to the control condition. A cumulative response rate was calculated for the three time-points as 46%, following patterns common to bereavement research and longitudinal investigations using postal questionnaires (Aoun et al., Citation2015).
Attrition
Comparisons between study completers and dropouts by T3 (cumulative) showed no significant differences with respect to gender, income level, study condition, use of anti-depressants or anxiolytics, or CG symptoms at baseline.
Baseline Characteristics
Baseline measures of demographic and bereavement-related characteristics by income group are presented in . A small but significant intervention group difference, χ2(2, N = 288) =6.36; p = .042, was shown for income. A higher proportion of the lowest income group participants were assigned to the control condition (61.2%) than to the intervention condition (38.8%). No group differences were found with respect to other personal characteristics (age, gender, medication use or work status) or loss-related characteristics (cause of death, kinship to the deceased, time since loss).
Analyses also identified several differences between the income categories. Differences in kinship to the deceased, χ2(6, n = 286) =13.05; p = .042, indicated that a higher proportion of low-median income group participants (49.4%) were bereaved of a partner, whereas the majority of the lowest income group (35.9%) and median-high income group participants (36.7%) were bereaved of a parent. A difference in mean ages was detected, F(2, 285) = 3.44, p = .033, with median-high income participants reporting the lowest average age of M = 46.6 years, SD = 12.86. The low-median income group reported the highest mean age, M = 51.4 years, SD = 12.86, while the lowest income group reported a mean age of M = 50.30 years, SD = 13.88). Work status also varied across groups, χ2(2, n = 286) = 80.11; p < .001, with 19.6% of the low-income group reporting employment, compared to 61.3% of low-median and 80.8% of the median-high income categories. Lastly, differences between income groups were also found in their use of medication at baseline χ2(2, n = 288) = 10.22; p = .006), with 55.4% of the lowest income group participants reporting medication use at baseline, compared to 35.4% and 36.2% of low-median and median-high income groups, respectively. No differences were found between income categories with respect to cause of death, or time since loss.
Statistical Tests
Analysis 1: Proportion of participants living at or below poverty threshold
Cross-sectional analysis of baseline data showed that 103 participants (35.8%) reported a household income in the lowest income category. Crosstabs revealed that this was more than twice the rate of general population living at or below the poverty threshold, χ2 (1, N = 5,310,288) = 105.01, p < .001, which was estimated at 14% for working-age adults and 16% for the elderly during the study period (Scottish Government, Citation2012). Eighty participants (27.8%) reported a household income in the low-median category, compared to 35% in the general population, and 105 (36.5%) reported a median-high category income, compared to 50% in the general population.
Analysis 2: The association of income with CG at baseline
A multiple linear regression was conducted to examine the associations at baseline between income and covariates (i.e., gender, age, medication, time since bereavement, cause of death, and relationship to deceased) on the one hand, and CG levels on the other. Two hundred seventy-five cases were included in the model. Preliminary tests indicated no violation of assumptions of linearity, homoscedasticity, lack of multicollinearity, or normal distribution of CG residuals at baseline. Six of the variables in the model demonstrated an association with CG.
shows the unstandardized and standardized regression coefficients. Results show that participants in the lowest income group had significantly higher CG levels compared to participants in the median-high income group, β = .32, SE = 3.34, p < .001, while participants in the low-median income presented CG levels that did not differ significantly from those of participants in the median-high group, β = .10, SE = 3.51, p = .129. Several other covariates were significantly associated with CG at baseline, although none of the relationships were as strong as for income. Participants who lost a partner, β = .23, SE = 3.65, p = .002, or a child, β = .18, SE = 5.39, p = .010, had significantly higher CG than those who lost a parent. Those who reported use of prescription medication had significantly higher CG than those who did not report prescription medication use, β = .19, SE = 2.86, p = .001, females had significantly higher grief than males, β = .15, SE = 3.45, p = .008. In addition, age was negatively associated with CG, β = −.14, SE =.13, p = .042, indicating that lower age was associated with higher CG. The model explained 19.7% of the total variance in CG mean scores at baseline, F(13, 261) = 4.93, p < .001, R2 = .20.
Table II. Variables associated with CG at baseline.
Because the proportion of those below the poverty level was different between the control and intervention group, a multiple linear regression with the same covariates was conducted, which included an interaction term for study condition and income. No significant interaction was found, F(2, 259) = 1.58, p = .207, partial eta squared = .012, indicating that poverty was associated with CG in similar ways for the control and experimental group at baseline.
Analysis 3: Change in CG means across income groups and study categories over time
Two hundred seventy-six participants were included in the model with 529 observations. Based on degrees of freedom, an upper limit of parameters that could be included in the model while retaining adequate power was set at 35.27. Due to an uneven distribution of some variables across income groups at baseline, the following variables were added to the model as covariates: use of medication at baseline (yes/no), gender, relationship to the deceased (partner, parent, child, sibling/friend/other), cause of death (illness, accident, suicide, unknown/other). Including covariates, the model contained a total of 18 parameters, which was within the acceptable range. As expected with a repeated measures design, inter-subject variance was high, 401.29, p < .001, with an interclass correlation for participant ID of ICC = .73, warranting the use of a hierarchical approach.
The hierarchical model with participant ID included as a random effect was evaluated using a two-step process. The model was first run without the three-way interaction in order to reveal the main effects of the primary independent variables of time, group, and income category, before introducing the three-way interaction to the model and evaluating the interaction effects. As shown in , the fixed effects model demonstrated significance for five lower order (main) effects on CG levels: income category, F(2, 275.53) = 12.36, p < .001; time, F(2, 280.58) = 48.69, p < .001; use of medication at baseline, F(1, 276.95) = 11.47, p = .001, d = 1.20; age, F(1, 277.90) = 5.70, p = .018, d = .76; and relationship to the deceased, F(3, 275.50) = 3.86, p = .010. These significant main effects for income, medication, and relationship to the deceased extend the earlier, baseline-only regression results by showing that the differences between demographic groups persist when CG scores are evaluated at all three time-points. Pairwise comparisons showed large-magnitude differences between the poverty income category and the other two income categories, with CG scores that were on average 16.58 points higher than the mid-plus income group (p < .001, d = 1.79) and 9.47 points higher than the low-mid income group (p = .008, d = .98) across all three time-points. The low-median income group also had higher mean CG scores than the median-high income group, with a mean difference of 7.11 points (p = .043, d = .72) and a medium effect size. Participants who did not take anti-depressants or anxiolytics at baseline had a mean CG score 9.67 points lower across all three time-points than those who reported taking these medications (p = .001, d = 1.20), a large magnitude difference. Comparisons for time showed a large magnitude effect at two measurement points, with a reduction of 10.82 points in CG levels between T1 and T2 (p < .001, d = 1.78), and a cumulative reduction in CG means (13.75 points, p < .001, d = 2.17) occurring between T1 and T3.
Table III. Hypothesis tests for the significance of each fixed effect.
illustrates the change in CG symptom levels within income groups and across study conditions over time. As a next step, the three-way interaction term time × study condition × income category, along with each of the associated two-way interactions, time × study condition, time × income category, and study condition × income category, were added to the hierarchical model. (All three-interaction variables—income, group, and time—were categorical and dummy-coded for inclusion in the model.) The omnibus test for three-way interaction of time × study condition × income category was not significant, F(4, 280) = 1.69, p = .150, therefore the individual beta coefficients are presented but not interpreted further. Compared to the interaction term Median-high income × experimental condition × T3, the estimate for Lowest income × control condition × T1 was not significant (β = 1.99, SE = 7.13, p = .781); the estimate for Lowest income × control condition × T2 was not significant (β = 1.61, SE = 7.33, p = .826); the estimate for Low-median income × control condition × T1 was significant (β = −16.48, SE = 7.78, p = .035); and the estimate for Low-median income × control condition × T2 was not significant (β = −10.55, SE = 8.03, p = .190). (Due to the dummy coding, the other parameters were set to zero, as they were redundant to the given estimates.). The additional explained variance of the model with the interaction included was negligible in size (R2 change <.01), suggesting that income did not affect the effectiveness of the intervention over time.
Figure 2 Change in mean complicated grief (ICG) symptom levels by income groups and study category over time.
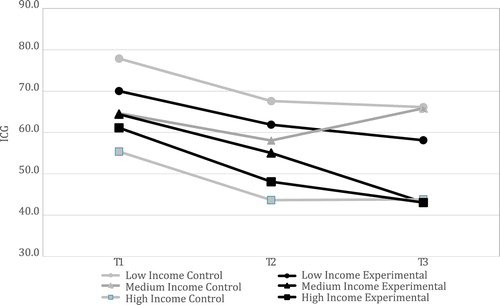
For informational purposes, the two-way interactions were also examined. The two-way interaction of study condition × time, was significant, F(2, 279.40) = 4.90, p = .008, R2 = .17, indicating that there was a difference in symptom levels between those who received intervention compared to those who did not over time. This conforms with the demonstration of intervention efficacy previously reported in Newsom et al., (Citation2017). The two-way interaction income category × study condition, however, was not significant, F(2, 306.13) = 2.45, p = .088, R2 = .18, suggesting that overall, participants’ study condition assignments were related to CG levels in a similar manner across income categories. Lastly, the two-way interaction of income category × time was not significant, F(4, 279.75) = .97, p = .424, R2 = .18, indicating that the degree to which CG scores changed over time was not detectably different between income groups.
Discussion
The goals of this investigation were to examine the relationship between income levels and CG among help-seeking bereaved adults, and to explore whether income levels influence the effectiveness of a community-based bereavement counseling intervention. Results indicated that a substantial number of bereaved people who were struggling to cope with grief and were seeking help were living in relative poverty. Over a third (36%) of this study’s sample reported living in below poverty-threshold households——more than twice the proportion of Scottish people in this income category (estimated at 14% for working-age adults and 16% for the elderly) during the study period (Scottish Government, Citation2012). Results of the present study also indicated an association between (low) household income and CG. At baseline, income quite remarkably showed the strongest effect on CG levels compared to other demographic and loss-related variables. Lastly, concerning the effectiveness of counseling for bereaved participants from different income levels, the analyses detected no effect of income level on CG levels in the intervention and control conditions over time. In other words, it appears that income did not influence counseling effects.
The results of this study have a number of important implications. First, the association between low household income and CG symptoms demonstrates the importance of low income as a potential risk factor in the development and persistence of CG. This association complements the study of Cacciatore et al. (Citation2016), which demonstrated a correlation between poverty and grief-related symptoms of depression and PTSD in bereaved parents. In the present analysis, these findings are extended to a bereavement-specific outcome variable (CG), among a more heterogeneous sample of help-seeking bereaved adults. The association between low income and CG also appears congruent with Lazarus and Folkman’s broader transactional model of stress (Lazarus & Folkman, Citation1987). Following this model, financial instability could be expected to (negatively) affect patterns of appraisal and coping, and in particular hinder the use of effective strategies for coping with bereavement (see Stroebe & Schut, Citation1999). Low household income may, therefore, be an important factor to include when assessing an individual’s risk of developing grief complications.
Next, the substantial percentage of participants living at or below the poverty threshold in our sample demonstrates their wish to receive support—and contrasts with the assumption of a “getting-on-with-it” social norm preventing people from low-income households from accessing support services (cf., Allen, Citation2007). Furthermore, this shows that the CBCS counseling program is initially considered acceptable as a source of support to low-income participants. Though the organization has not specifically tailored the intervention to income, certain provisions may have contributed towards service acceptability (e.g., providing professional training and certification of locally based volunteers to serve as counselors) and accessibility (e.g., not charging fees for services, operating a national phone line, and running local services with extended weekday and weekend hours).
The present study also showed that despite a quasi-randomized process of study condition assignment (which was shown to be equally effective in controlling for group differences in bereavement counseling research; Currier et al., Citation2008), a relatively higher percentage of low-income participants enrolled in the control condition. In other words, more bereaved people from below poverty-threshold households sought help from CBCS and went through the initial steps to receive it, but did not end up receiving counseling services. Reasons for not attending (when offered) often concerned logistical difficulties with scheduling or transport to the service location. Further investigation is recommended to identify any organization- or location-specific barriers to service access. Taken together, these results suggest the need for all bereavement support organizations to carefully consider their strategies for making accessible and acceptable support available to members of low-income households.
Although not the primary aim of our study, another notable finding was that a baseline difference was found between income categories concerning the use of anti-depressants and anxiolytics, which was relatively higher among the participants from low-income households. Considering recent evidence that anti-depressant medication did not affect CG symptoms in a randomized controlled trial of CG treatment (Shear et al., Citation2016), no impact from the use of these medications on CG was expected in the present study. It is nevertheless a puzzling indication that corresponds with recent observations of higher anti-depressant use in areas of deprivation (Gayle, Citation2017), and suggests the need for further investigation.
Limitations
Several limitations in this research should be noted. First, as is frequently the case in bereavement research, the present study sample predominantly consisted of women (74.8%) bereaved of a spouse (or a parent). Future research needs to determine if results generalize across samples with more men, and different kinship ties to the deceased person. Participant attrition could be considered another concern for the present study, though it conformed with dropout patterns in bereavement research in general and postal questionnaire research in particular (Aoun et al., Citation2015). Dropout analyses indicated no detectable differences between participants who remained in the study for all three time-points and those who dropped out.
Another limitation is that due to a lack of detailed information about the number of household members, we applied poverty-threshold guidelines for a single-person household. The incidence of poverty and deprivation in our sample, therefore, may be underestimated. Next, given the higher incidence of psychological health problems among people living in poverty, excluding people with pre-existing or co-existing psychiatric diagnoses may have limited participation among the lowest income group. Prevalence of CG in our lowest income category sample could therefore similarly underestimate the prevalence of CG in this income category in the general (bereaved) population. Lastly, while people were quasi-randomized to study conditions, inclusion in the current investigation of household income was conducted on an opt-in basis, since people chose whether to provide household income information. It may be the case that people from a particular income group were more or less likely to provide income information and were, therefore, less likely to participate. While we cannot refute this argument entirely, our analyses detected no differences on demographic and loss-related variables (including variables that were distributed unevenly between income categories) between people who did and did not provide this income information. This suggests that income differences between study accepters and decliners are unlikely.
Conclusion
Despite indications that people from below-poverty threshold income households generally struggle to access services and practice self-care, approximately a third of the participants in this naturalistic study who had sought help from a volunteer-based counseling service came from this income category. Though the counseling program in this study was not tailored to income, it was community based, and several service characteristics may have improved its accessibility (i.e., local service locations, no services fees, extended hours service)—and acceptability (i.e., providing professionally trained, local volunteer counselors) to people from low-income households. On average, bereaved people from the lowest income households experienced relatively higher levels of grief symptoms, yet the effectiveness of the intervention in reducing grief levels did not appear to differ across income groups. Taken together, these results suggest community-based services are accessible, acceptable and beneficial to people with low incomes.
Geolocation Information
Data collection for this research was conducted across Scotland.
ORCID
HENK SCHUT http://orcid.org/0000-0001-8744-4322
MAARTEN C. EISMA http://orcid.org/0000-0002-6109-2274
Additional information
Funding
References
- Allen, C. (2007). The poverty of death: Social class, urban deprivation, and the criminological consequences of sequestration of death. Mortality, 12(1), 79–93. doi: 10.1080/13576270601088392
- Aoun, S. M., Breen, L. J., Howting, D. A., Rumbold, B., McNamara, B., & Hegney, D. (2015). Who needs bereavement support? A population based survey of bereavement risk and support need. PloS One, 10(3), e0121101. doi: 10.1371/journal.pone.0121101
- Breen, L. J., Aoun, S. M., O’Connor, M., & Rumbold, B. (2013). Bridging the gaps in palliative care bereavement support: An international perspective. Death Studies, 38(1), 54–61. doi: 10.1080/07481187.2012.725451
- Burke, L. A., & Neimeyer, R. A. (2013). 11 prospective risk factors for complicated grief. In M. Stroebe, H. Schut, & J. van den Bout (Eds.), Complicated grief: Scientific foundations for health care professionals (pp. 145–161). London: Routledge.
- Cacciatore, J., Killian, M., & Harper, M. (2016). Adverse outcomes in bereaved mothers: The importance of household income and education. SSM-Population Health, 2, 117–122. doi: 10.1016/j.ssmph.2016.02.009
- Currier, J. M., Neimeyer, R. A., & Berman, J. S. (2008). The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychological Bulletin, 134(5), 648–661. doi: 10.1037/0033-2909.134.5.648
- Doornbos, M., Zandee, G., DeGroot, J. & Warpinski, M. (2013). Desired mental health resources for urban, ethnically diverse, impoverished women struggling with anxiety and depression. Qualitative Health Research, 23(1), 78–92. doi: 10.1177/1049732312465018
- Garratt, E. A., Chandola, T., Purdam, K., & Wood, A. M. (2016). The interactive role of income (material position) and income rank (psychosocial position) in psychological distress: A 9-year longitudinal study of 30,000 UK parents. Social Psychiatry and Psychiatric Epidemiology, 51(10), 1361–1372. doi: 10.1007/s00127-016-1255-y
- Gayle, D. (2017, April 14). Anti-depressants prescribed far more in deprived English coastal towns. The Guardian. Retrieved from https://www.theguardian.com/society/2017/apr/14/antidepressants-prescribed-deprived-seaside-towns-of-north-and-east-blackpool-sunderland-and-east-lindsey-nhs
- Krupnick, J. L. (2002). Brief psychodynamic treatment of PTSD. Journal of Clinical Psychology, 58(8), 919–932. doi: 10.1002/jclp.10067
- Lazarus, R. S., & Folkman, S. (1987). Transactional theory and research on emotions and coping. European Journal of Personality, 1(3), 141–169. doi: 10.1002/per.2410010304
- Mack. (2016). http://www.poverty.ac.uk/definitions-poverty/income-threshold-approach
- Newsom, C., Schut, H., Stroebe, M. S., Wilson, S., & Birrell, J. (2016). Initial validation of a comprehensive assessment instrument for bereavement-related grief symptoms and risk of complications: The Indicator of Bereavement Adaptation—Cruse Scotland (IBACS). PloS One, 11(10), e0164005. doi: 10.1371/journal.pone.0164005
- Newsom, C., Schut, H., Stroebe, M.S., Wilson, S., Birrell, J., Moerbeck, M., & Eisma, M.C. (2017). The effectiveness of bereavement counseling through a community-based organization: A naturalistic, controlled trial. Clinical Psychology and Psychotherapy. doi:10.1002/cpp.2113
- Peugh, J. L. (2010). A practical guide to multilevel modeling. Journal of School Psychology, 48(1), 85–112. doi: 10.1016/j.jsp.2009.09.002
- Prigerson, H. G., & Jacobs, S. C. (2001). Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schut (Eds.), Handbook of bereavement research: Consequences, coping and care (pp. 705–737). Washington, DC: American Psychological Association.
- Robson, D., & Gray, R. (2007). Serious mental illness and physical health problems: A discussion paper. International Journal of Nursing Studies, 44(3), 457–466. doi: 10.1016/j.ijnurstu.2006.07.013
- Roy-Byrne, P., Sherbourne, C., Miranda, J., Stein, M., Craske, M., Golinelli, D., & Sullivan, G. (2006). Poverty and response to treatment among panic disorder patients in primary care. American Journal of Psychiatry, 163(8), 1419. doi: 10.1176/ajp.2006.163.8.1419
- Santiago, C. D., Kaltman, S., & Miranda, J. (2013). Poverty and mental health: How do low income adults and children fare in psychotherapy? Journal of Clinical Psychology, 69(2), 115–126. doi: 10.1002/jclp.21951
- Schut, H., Stroebe, M. S., Van den Bout, J., & Terheggen, M. (2001). The efficacy of bereavement interventions: Determining who benefits. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schut (Eds.), Handbook of bereavement research: Consequences, coping and care (3rd ed., pp. 705–737). Washington, DC: American Psychological Association.
- Scottish Government (2012). Poverty and income inequality in Scotland: 2010–11. Retrieved from http://www.gov.scot/Publications/2012/06/7976
- Selya, A. S., Rose, J. S., Dierker, L. C., Hedeker, D., & Mermelstein, R. J. (2012). A practical guide to calculating Cohen’s f2, a measure of local effect size, from PROC MIXED. Frontiers in Psychology, 3, 111. doi: 10.3389/fpsyg.2012.00111
- Shear, K. (2015). Complicated grief. New England Journal of Medicine, 372, 153–160. doi: 10.1056/NEJMcp1315618
- Shear, M. K., Reynolds, C. F., Simon, N. M., Zisook, S., Wang, Y., Mauro, C., … Skritskaya, N. (2016). Optimizing treatment of complicated grief: A randomized clinical trial. JAMA Psychiatry, 73(7), 685–694. doi: 10.1001/jamapsychiatry.2016.0892
- Simonsen, G., & Cooper, M. (2015). Helpful aspects of bereavement counseling: An interpretative phenomenological analysis. Counselling and Psychotherapy Research, 15(2), 119–127.
- Stephen, A. I., Wilcock, S. E., & Wimpenny, P. (2013). Bereavement care for older people in healthcare settings: Qualitative study of experiences. International Journal of Older People Nursing, 8(4), 279–289. doi: 10.1111/j.1748-3743.2012.00319.x
- Stephen, A. I., Wimpenny, P., Unwin, R., Work, F., Dempster, P., MacDuff, C., … Brown, A. (2009). Bereavement and bereavement care in health and social care: Provision and practice in Scotland. Death Studies, 33(3), 239–261. doi: 10.1080/07481180802671944
- Stroebe, M., Schut, H., & Boerner, K. (2017). Modelos de afrontamiento en duelo: un resumen actualizado [Models of coping with bereavement: An updated overview]. Estudios de Psicología, 1–26. doi:10.1080/02109395.2017.1340055
- Stroebe, M. S., & Schut, H. (1999). The dual process model of coping with bereavement: Rationale and description. Death Studies, 23(3), 197–224. doi: 10.1080/074811899201046
- Thompson, N. (2002). Loss and grief: A guide for human services practitioners. Basingstoke: Palgrave Macmillan.
- The World Health Organization. (2017). Retrieved from http://www.who.int/workforcealliance/media/qa/04/en/