Abstract
Objective: Meta-analyses show that Acceptance and Commitment Therapy (ACT) is an efficacious treatment for a wide range of mental health problems. However, few studies have examined the effectiveness of ACT in naturalistic inpatient settings and in direct comparison to Cognitive Behavior Therapy (CBT). The aim of this study was to investigate the effectiveness of ACT and CBT with regard to depression, general symptom strain and life satisfaction. Method: 177 inpatients in a psychiatric ward were included in the study and assigned to either ACT or CBT group intervention. All patients were assessed with the SCID-I interview and disorder-specific questionnaires as well as with a satisfaction with life scale. To control for confounding variables, amongst others, treatment integrity was evaluated. Results: Both the ACT and CBT intervention showed a large, statistically significant and stable symptom reduction over six months across all outcomes. Both approaches led to small improvement in life satisfaction. With regards to depressive symptoms, more than half of the patients reliably recovered due to therapy. Conclusion: ACT and CBT were similarly effective in treating patients with depressive and other mental disorders in a routine clinical setting. ACT is a viable alternative to CBT for treating inpatients.
Clinical or methodological significance of this article: This is the first study investigating the effectiveness of Acceptance and Commitment Therapy (ACT) compared to Cognitive Behavioral Therapy (CBT) for inpatients with different mental disorders. In addition to a structured diagnosis of all patients, psychometric data were collected at three measurement points. In addition to disorder-specific outcome measures, life satisfaction was assessed and clinical significance determined. Furthermore, treatment integrity of all therapists was monitored. The results of the study suggest that ACT and CBT are similarly effective in treating inpatients in routine clinical care. This offers flexibility in the delivery of psychological interventions to psychiatric inpatients.
Psychotherapy appears to be an effective treatment for adult depression, independent of the treatment approach chosen (e.g., Cuijpers et al., Citation2020). Although these results are promising, approximately one-fourth of patients do not benefit from established psychotherapies (Gloster et al., Citation2019). Therefore, it is worthwhile investigating other therapy approaches. One such therapy that has received considerable research and clinical attention in recent years is Acceptance and Commitment Therapy (ACT), a third wave Cognitive Behavior Therapy (CBT; Hayes, Citation2004). ACT is generally beneficial for a broad variety of clinical and non-clinical mental health issues (A-Tjak et al., Citation2015). However, results of previous studies differ as to whether outcome of ACT is comparable to established treatments like CBT (Dimidjian et al., Citation2016). Most of the studies concerning the efficacy of ACT and CBT have been randomized controlled trials (RCTs) and only a few studies have investigated psychiatric inpatient samples. Thus, an important question remains: How effective is ACT in inpatient clinical settings? The purpose of the present study is to investigate the effectiveness of ACT compared to CBT in an inpatient setting under naturalistic conditions.
In general, it can be deduced from the results of previous meta-analyses that both individual and group therapies are effective for depressive disorders (Cuijpers et al., Citation2008) and anxiety disorders (Barkowski et al., Citation2020). Concerning inpatient psychotherapeutic treatment, results of a recent meta-analysis by Schefft et al. (Citation2019), suggest significant effects of inpatient psychotherapy compared to treatment as usual for depressive disorders. Moreover, the pooled results of a meta-analysis investigating the effects of group psychotherapy for inpatients with a different symptomatology suggested superiority of group psychotherapy compared to waitlist and care as usual (Koesters et al., Citation2006).
In summary, regardless of the setting, psychotherapy is generally efficacious and more efficacious than treatment as usual. Yet, it has not been sufficiently demonstrated that this applies for newer psychotherapeutic approaches such as ACT. Instead of focusing on reducing symptoms of mental disorders, the main goal of ACT is the improvement of psychological flexibility (Hayes, Luoma, Bond, Masuda, & Lillis, Citation2006). This is achieved by focusing on acceptance of unwanted thoughts and feelings in the present while also taking action that is in the service of personal values (Fletcher & Hayes, Citation2005). The emphasis on mindful acceptance of inner experiencing instead of changing it, is a key factor that distinguishes ACT from traditional CBT (Hayes, Citation2008).
A considerable number of meta-analytic reviews analysed the results of studies concerning the efficacy of ACT for different disorders (e,g., A-Tjak et al., Citation2015; Hacker et al., Citation2016; Hayes et al., Citation2004; Öst, Citation2014; Ruiz, Citation2012). The results of all meta-analyses suggest that ACT is more efficacious for various mental disorders than waitlist, placebo and treatment as usual. With respect to active evidence-based control groups like CBT, results of the most recent meta-analysis lead to the conclusion that there are no significant differences between the effects of ACT and CBT (A-Tjak et al., Citation2015; Hacker et al., Citation2016; Öst, Citation2014).
With regards to inpatient settings, so far only a few studies with quite considerable methodological limitations have investigated the effectiveness of ACT on clinically relevant mental health-related outcomes. Petersen and Zettle (Citation2009) found significant effects of ACT for inpatients (n = 12) with comorbid depressive and substance abuse disorders, whereas ACT was not superior to a treatment as usual condition. A recent study by Benoy et al. (Citation2019) found moderate to large effects on general symptom reduction for 47 inpatients with various mental disorders. It should be noted that the authors used neither a manual nor a control or comparison group and did not collect follow-up data. Preliminary results of a study conducted by our research group with 67 patients indicate significant improvements in depression for inpatients in both the ACT and CBT conditions but no between group differences (Pleger et al., Citation2018).
In summary, most research on ACT has been performed with RCTs. Due to various methodological aspects (e.g. often less severely ill patients who suffer from one defined disorder), results from RCTs are not fully generalizable to clinical practice (Paterson et al., Citation2018). Effectiveness trials, which investigate treatments under routine clinical conditions, are rare and only a very small number of studies investigated ACT for inpatients (Schefft et al., Citation2019). Most study designs in this field are underpowered, lack evidence-based control groups and follow-up data, and have not examined clinical significance and often treatment integrity is not sufficiently evaluated.
The present study investigates whether ACT compared to CBT is an effective treatment for reducing depressive and overall symptom strain as well as for increasing life satisfaction for inpatients treated in routine clinical care. The main goal was to perform a trial under naturalistic conditions, with a rigorous methodology and high external validity. To enable high methodological rigor, we compared ACT to an active comparison group (CBT). Assessments were taken at pre, post and at 6-months follow-up. Additionally, we investigated the extent of therapeutic competence and treatment adherence.
We expected both treatments to lead to a significant reduction in depression and overall symptom reduction and that these treatment gains would remain stable at six months follow-up. However, since ACT is described as a transdiagnostic approach with the main goal of increasing psychological flexibility, we expected ACT to outperform CBT in overall symptom strain and life satisfaction.
Method
Trial Design
The study design was a clinical effectiveness trial comparing ACT and CBT in the treatment of various mental disorders under naturalistic conditions in a German inpatient psychiatric ward. The study was registered with the German Clinical Trial Register (DRKS00011700) and approved by the ethics commission of Humboldt University, Berlin.
Participants
Inclusion and exclusion criteria. Patients were included in the study if they were at least 18 years of age, had at least one DSM IV Axis I diagnosis and signed the consent form. Patients were excluded from the investigation if they entered the ward for a crisis intervention/were supposed to be shifted to another ward (1), were acutely psychotic (2), had an intellectual disability (3), were acutely intoxicated/primarily substance addicted/less than 3 months abstinent (4), had insufficient language skills to meet study requirements (5) or had previously participated in either intervention (6).
Interventions
Both treatments were offered in an open group setting twice a week. Group sessions were 50 minutes in duration. Patients were able to drop into their allocated treatment at any time during the course of the study. Thus, there was no start or end point regarding time and content. Additionally, patients had at least three one-on-one contacts with a therapist: One to define individual goals, one during treatment and one before discharge. If necessary (e.g., an acute crisis), patients received additional one-on-one contacts. Consistent with standard clinical practice in German psychiatric wards patients were also offered treatment as usual, which consisted of one daily session each of occupational therapy and physiotherapy. These additional services emphasized CBT or ACT processes consistent with the patient’s treatment condition allocation. For example, for CBT participants, physiotherapy focused on general bodily activation and occupational therapy emphasized behavioural activation. Whereas for the ACT group, physiotherapy focused on Yoga and Pilates and occupational therapy emphasized mindfulness training.
Therapists. Treatment groups were led by a single therapist. To minimize therapist effects different therapists facilitated groups in each treatment condition (ACT: n = 3; CBT: n = 2). To prevent blending between both approaches, the therapists were only assigned to one treatment condition. The therapists had to have had a minimum of three months experience facilitating therapy groups within the psychotherapy approach of the treatment condition they were assigned to. They also received weekly supervision. Two of the ACT therapists and one of the CBT therapists had more than a year of experience in delivering each treatment. The remaining therapists in each group had three months of experience. All therapists and clinic staff attended a one-day workshop on ACT and CBT specific techniques and were sensitized to the differences between both approaches.
CBT condition. The CBT treatment protocol was based on an evaluated German intervention manual for depression (Hautzinger & Kischkel, Citation1999), which included psychoeducation about emergence and maintenance of depression, behavioural activation using timetables and list of positive activities, cognitive restructuring using the ABC model and social competence training. The manual provided clear guidelines for the order and amount of time spent on each block of content. Due to the open group setting, we slightly adapted the manual such that treatment sessions could be expanded if necessary.
ACT condition. The ACT protocol (Dambacher & Samaan, Citation2020) was based on the transdiagnostic psychological flexibility framework and adaptations of the interventions developed by Eifert (Citation2011), Harris (Citation2011), Sonntag (Citation2011) and Wengenroth (Citation2012, Citation2013). Each ACT group session focused on one of the six ACT core processes (mindfulness, self as context, defusion, acceptance, values, and committed action) in accord with a treatment protocol which provided guidelines for session structure, content and experiential exercises. In contrast to the CBT manual, the ACT protocol did not determine the order of each block of content. In view of the overlap among these processes, references to multiple processes were included in a given session even though the primary focus was on a single process.
Treatment Integrity
To ensure therapists’ treatment integrity, ACT and CBT group sessions were audio recorded. In the absence of published German ACT/CBT competence and adherence scales, purpose-built measures were developed to assess therapists’ competence and adherence relevant to the intervention protocols for their assigned treatment condition. A total of 315 therapy sessions were conducted (ACT: n = 159, CBT: n = 156) during the study period. Thirty percent of the recorded sessions for each treatment condition were selected yielding a total of 71 sessions. One session for each treatment condition was excluded post-hoc due to poor audio quality, so that n = 38 ACT sessions and n = 31 CBT sessions formed the basis for evaluation. Two independent raters experienced in delivering ACT and CBT attended a two-day workshop to familiarize them with the scales and assessment procedure. Within six weeks both raters evaluated the middle third of each session in the same random order. Both raters were blinded to the treatment condition. Afterwards all scales were evaluated concerning psychometric properties (Müller, Citation2018; Samaan et al., Citationin press).
Competence Scale (CTS+). The CTS+ is a 15-item scale based on the German version of the Cognitive Therapy Scale (CTS; Weck et al., Citation2010) and the Drexel University ACT/tCBT adherence and competence rating scale (DUARCS; McGrath, Citation2012). It consists of three subscales: a CBT specific competence scale (4 items), an ACT specific competence scale (4 items) and an ACT/CBT cross-process competence scale (8 items). Items were rated on a seven-point Likert scale: 0 = “poor”, 1 = “just sufficient”, 2 = “moderate”, 3 = “satisfactory”, 4 = “good”, 5 = “very good” and 6 = “excellent”. An interrater reliability of ICC(2,2) = 0.95 (p < 0.01) was found for the ACT-specific competence mean scale value. The CBT-specific competence mean scale value yielded an interrater reliability of ICC(2,2) = 0.42 (p < 0.01). The interrater-reliability of the cross-process competence remained below an ICC of 0.4 both at item level and for the mean scale value. Cronbach’s alphas were 0.70 for the cross-process competence scale, 0.64 for the CBT-specific competence scale and 0.93 for the ACT-specific competence scale.
CBT Adherence Scale (CBT-Ad). The CBT-Ad consisted of 14 items. The psychoeducation, behavioural activation and cognitive restructuring modules were each represented by three items and five items gauged the social competence training module. Items were rated on a four-point Likert scale: 0 = “poor implementation”, 1 = “low implementation”, 2 = “moderate implementation” and 3 = “predominant implementation”. In order to determine the extent to which ACT and CBT could be differentiated, the CBT-Ad was used for ACT sessions as well. Raters were instructed to rate an item as not available (n/a) if a certain behaviour was not shown (Samaan et al., Citationin press). The interrater reliability calculated for the mean scale value was ICC = 0.98 (p < 0.001) and the Cronbach’s alphas for the subscales ranged from 0.94 to 0.99.
ACT Adherence Scale (ACT-Ad). The ACT-Ad consisted of 12 items. Each of the six core ACT processes was represented by two items. Items were rated on the same four-point Likert scale used in the CBT-Ad and were also used for CBT sessions as part of the measurement of differentiation. An ICC of 0.96 (p < 0.001) was found for the mean scale value and the Cronbach’s alphas for the subscales ranged from 0.91 to 0.97.
Outcome
At baseline information on sociodemographic and clinical characteristics was obtained via a questionnaire and diagnostic information was obtained by the SCID I interview (Wittchen et al., Citation1997). We used the Wortschatztest (WST; Schmidt & Metzler, Citation1992), a German screening instrument, which estimates verbal intelligence. Primary and secondary outcome measures were administered at pre- and post-treatment and follow-up. All questionnaires were completed by the patients in electronic form using a tablet.
Primary Outcome. The ADS-k (Hautzinger & Bailer, Citation1993) was used to assess the presence of depressive symptoms and duration of impairment due to depressive symptoms within the past week. The ADS-k is a reliable 15-item short form of the German version of the Center for Epidemiological Studies Depression scale (CES-D; Radloff, Citation1977). The duration of depressive affect, somatic complaints, motor inhibition and negative thought patterns are rated on a 4-point scale. Internal consistency for this measure in our sample ranged from Cronbach’s α = 0.86 to α = 0.95 across assessments.
In addition, the German version of the Montgomery-Asperger Depression Rating Scale (MADRS; Neumann & Schulte, Citation1989) was used to determine depressive syndromes based on an expert rating. The rater estimates the severity of the respective symptom for 10 items with a severity of 0–6. Within an inpatient sample inter-rater reliability was 0.76 and considered acceptable (Davidson et al., Citation1986). In our sample internal consistency ranged from α = 0.83 to α = 0.87 across assessments.
ICD-10 Symptom Rating (ISR; Tritt et al., Citation2008) is a well evaluated self-rating screening instrument for a wide variety of psychological syndromes. The ISR consists of 29 items and yields a total score and six syndrome scale scores: Depression, Anxiety, Obsessive/Compulsive, Somatoform, Eating Disorders, and a Supplementary Scale which covers a variety of syndromes with one item each. Observed internal consistencies across the multiple assessments were: Depression: α = 0.80 to α = 0.90, Anxiety: α = 0.84 to α = 0.87, Obsessive/Compulsive: α = 0.75 to α = 0.77, Somatoform: α = 0.84 to α = 0.88, Eating Disorder: α = 0.83 to α = 0.86.
Secondary Outcome. The widely used German version of the Satisfaction with Life Scale (SWLS; Glaesmer et al., Citation2011) is a 5-item self-rating inventory. Each item is rated on a 7-point Likert scale. The Cronbach’s alphas ranged from 0.89 to 0.91 across assessments.
To measure treatment satisfaction after therapy, we adapted the ZUF-8 (Fragebogen zur Patientenzufriedenheit; Schmidt et al., Citation1989) to our treatment condition. The 8-item ZUF-8 is based on the Client Satisfaction Questionnaire (CSQ-8; Attkisson & Zwick, Citation1982). Our adapted version consisted of 7 items and included two items which assessed the extent to which the treatment was understandable and comprehensible. The highest possible score on this modified version is 28. Higher scores indicate higher treatment satisfaction (Cronbach’s α = 0.87).
Sample Size
G*Power was used to conduct a power analysis (Faul et al., Citation2007) for repeated measures MANOVA, within-between interaction. Referring to former efficacy and effectiveness trials investigating ACT and CBT, a moderate effect was expected (Hacker et al., Citation2016). To reach an effect of f = 0.25 and 80% Power, a two-tailed alpha of 0.05, two groups and three points of measurement where entered and resulted in a total sample size of 154. Since we expected dropouts, we targeted a sample size of 170 (n = 85 per group).
Allocation Procedure
To strengthen external validity, we did not change the usual admission for inpatient treatment and the therapy group allocation procedure. Patients were admitted as an emergency (e.g. after suicide attempt), based on relocation from another ward or from a waiting list. Patients were put on the waiting list, if no hospital bed was available and they did not report suicidal thoughts. Eligibility was first identified in a short screening by the head of the ward. Suitable patients were orally informed about the study. After deciding to participate and signing the consent form, patients were allocated to either ACT or CBT treatment condition. The allocation procedure was done by study nurses, who were not directly involved in the treatment procedure, and depended on group capacity. A maximum of 10 places were available in each intervention. Patients who were excluded from the study were placed in a third independent therapy group. If 8 patients had been allocated in the CBT condition and 7 in the ACT condition, a new patient was assigned to the ACT condition. If there were the same number of patients in both therapy groups, the study nurses rolled a dice for random group assignment. We deliberately decided against overall randomization due to the following reasons: First, allocation by capacity was the fastest way to provide patients with treatment. Second, this also ensured that there was no imbalance in the number of patients between the groups. Given that one therapist was responsible for one group at a time, randomization would have led to an imbalance in care. Third, in German clinical settings this is a common form of patient intervention allocation and therefore met this study’s naturalistic investigation design. Fourth, in a pilot study where the same group allocation procedure was applied, no between group differences due to the allocation process could be detected (Pleger et al., Citation2018).
Statistical Analysis
Any between-group differences on clinical and sociodemographic sample characteristics at baseline were determined with χ2 test for categorical variables and t-test for continuous variables. Study assessment completers and non-completers were compared on all baseline measures. Regarding missing data, SPSS expectation-maximization estimation was used to test whether data were missing completely at random (MCAR). We then performed the automatic multiple imputation technique in SPSS 20 to determine missing values for the intent to treat (ITT) sample. Therefore, missing post-treatment and follow-up data were estimated 10 times and generated 10 data sets with imputed data. Kolmogoroff-Smirnov test was used to determine whether the data was normally distributed. To compare the effects of ACT and CBT treatment at post-treatment and after 6-months follow-up, we used two-way repeated measures MANOVA for primary and ANOVA for secondary outcome measures (factor 1: intervention, factor 2: therapist). We determined effect sizes (Cohen’s d) between time points by the formula recommended by Dunlap et al. (Citation1996), whereby Cohen’s d is calculated by multiplying the t value with the root of [2 (1−r) / n]. Between-group effect sizes from before to after treatment were calculated by subtracting the means and dividing the result by the standard deviation, adjusting the calculation of the standard deviation with weights for the sample sizes (Morris, Citation2008). Clinically significant change was examined in accord with the two-step approach recommended by Jacobson et al. (Citation1984) and Jacobson and Truax (Citation1991). First, using the reliable change index (RCI), the extent to which a patient’s change from pre- to post-treatment is reliable (RCI ≥ 1.96) is determined. Second, the extent to which a patient’s score shifts out of the clinically dysfunctional range and into the functional range at post-treatment is determined by the cut-off scores for each outcome measure. For a further description of our sample, we sub-classified patient change as suggested by Jacobi et al. (Citation2011): reliable shift from a clinical to non-clinical population (remission), reliable improvement but no shift into a non-clinical band (response), reliable symptom increase (deterioration) and no change at post-treatment (nonresponse).
Results
Participant Flow
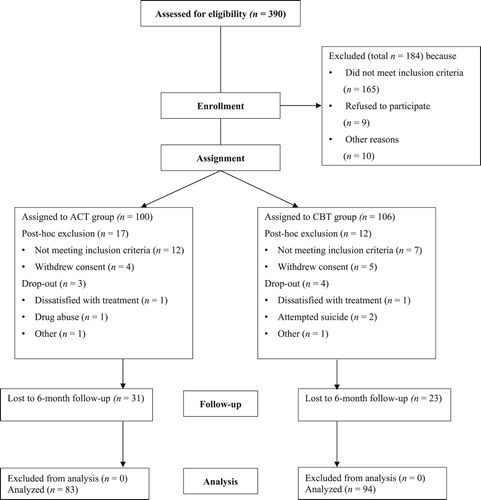
A flowchart of participant inclusion is depicted in . Of the 390 patients admitted to the ward during the study period, 206 were identified as potential participants and were allocated to one of the two treatment conditions for further eligibility assessment. Of the 83 patients allocated to the ACT condition and who met inclusion criteria, 80 completed the post-treatment assessment and of these, 49 completed the 6-month follow-up. In the CBT condition, of the 94 patients who met inclusion criteria, 90 completed the post-treatment assessment and 67 completed the 6-month follow-up. Differences in between-group dropout rates from post-treatment to follow-up did not reach significance [χ2 (1) = 2.92, p = 0.06].
Baseline Data
shows sociodemographic and clinical characteristics of the ACT and CBT ITT sample. The ACT and CBT groups did not differ on baseline sociodemographic or clinical characteristics. A total of 132 patients had a Major Depressive Disorder (MDD) only or an MDD and comorbid disorder and 45 fulfilled the criteria for another disorder other than an MDD. A table of all specific diagnoses is given in appendix A. In total 155 of the 177 patients (87.57%) were medically pretreated when they commenced therapy on the ward. For 88 patients, the treatment they underwent during the study was their first psychiatric intervention. A total of 49 patients were undergoing outpatient psychotherapy before their admission into the study and 89 patients had attended psychotherapy in the past. depicts the treatment characteristics of all patients. No differences between the ACT and CBT condition emerged. On average patients were treated for 41.9 days (SD = 13.17, Range = 10–108) and participated in 10.27 group therapy sessions (SD = 3.51, Range: 2–27). For approximately half of the 177 patients, medication was adjusted during their inpatient stay over the course of the study. A total of 128 of the 177 patients (72.3%) were discharged with medication.
Table I. Sociodemographic and clinical characteristics for the Acceptance and Commitment Therapy (ACT) group and Cognitive Behavioral Therapy (CBT) group at baseline.
Table II. Treatment characteristics of the ITT sample divided by group.
Dropouts and Study-Completers
Of the total sample, 7 patients dropped out during treatment (cf. ), which amounts to an overall dropout rate of 3.95% (ACT: 3.61%, CBT: 4.26%). Compared to other inpatient studies (median = 12%, Range = 0%–30%) this dropout rate can be considered low (Schefft et al., Citation2019). A total of 54 patients were lost to follow-up, resulting in a total rate of 31.76% (ACT: 38.75%, CBT: 25.56%) and corresponds to the average of other inpatient studies (30%, Schefft et al., Citation2019). We compared the baseline scores on primary and secondary outcomes of patients who dropped out at any time during the study (dropouts) with patients who completed all three assessments (study-completers). Results are depicted in . No significant between group differences emerged. Furthermore, we tested for between group differences due to treatment condition. Dropouts had significantly higher ADS scores than study-completers in the ACT condition, but study-completers and dropouts did not differ in the CBT condition [ACT: t(81) = 2.15, p < 0.05; CBT: t(92) = −1.85, p = 0.07].
Table III. Primary and secondary outcome scores of study-completers and dropouts at baseline.
Imputation of Missing Data
To estimate data for missing values at post-treatment and six months follow-up, Little’s Missing Completely at Random (MCAR) test (Little, Citation1988) was applied. Little’s MCAR test did not reach significance for any of the data sets: pre- and post-treatment data set, χ2(4) = 3.76, p = 0.44; post-treatment and follow-up data set, χ2(18) = 12.52, p = 0.82; pre-treatment and follow-up data set, χ2(18) = 12.62, p = 0.81. These results imply the data to be MCAR. This enables use of the multiple imputation technique for missing data estimation with the ITT sample (van Ginkel & Kroonenberg, Citation2014). All further analyses refer to the imputed data set, unless otherwise indicated.
Primary Outcome
Using Pillai’s trace, two-way MANOVA indicated a significant main effect of time on ADS, MADRS and ISR overall scores, V = 0.70, F(6, 131) = 50.37, p < 0.001. There were no significant interaction effects for either group x time or for therapist x time as well as no significant between group differences for any scale at any assessment point. presents pooled results of all measures by treatment condition. Both ACT and CBT patients reported large reductions on the primary outcomes at post-treatment, which remained stable over the follow up phase.
Table IV. ITT pre-treatment, post-treatment and 6-months follow-up scores on primary and secondary outcome measures and within- and between-group effect sizes (Cohen’s d).
Secondary Outcome
Two-way ANOVA indicated a significant main effect of time on SWLS F(2, 135) = 12.89, p < 0.001. No interaction effects and no between group differences could be detected. Both ACT and CBT patients reported a small increase in life satisfaction at post-treatment which remained stable over the follow-up period ().
Treatment satisfaction levels were only determined for observed (n = 170), not imputed data. The mean post-treatment satisfaction score of the ACT condition x̅ = 23.4 (SD = 3.65, Range: 8.00–28.00) did not differ significantly from that of the CBT condition x̅ = 23.4 (SD = 3.19, Range: 16.00–28.00), t(167) = 0.10, p = 0.92.
Clinical Significance
Clinically significant pre- to post-treatment change data for the ACT and CBT conditions are reported in . Highest response rates were evident on depression focused outcomes. Regarding MADRS scores, a total of 85% reliably responded to either of the two interventions. More than half of the patients reliably shifted from a clinical to a non-clinical band (53%). Almost three quarters (74%) of all patients evidenced improvement on the ADS pre- to post-treatment. Across both conditions more than half of the patients reliably recovered (58%). In terms of general symptom strain measured with ISR, a total of 62 patients (35%) reliably responded to the therapy. A small portion of patients (12%) fell in the remission range. Approximately two-thirds of all patients remained unchanged. An average deterioration rate of 2% across all measures is relatively low. Rates of change on all measures did not significantly differ between the two conditions, χ2 (3) = 0.60, p = 0.11.
Table V. ITT percentage of patients who reliably remitted, reliably responded, reliably deteriorated and non-responded from pre- to post-treatment.
Treatment Integrity
Competence. The mean cross-process competence values for each condition did not differ (CBT x̅ = 4.74 (SD = 0.43, Range = 2.63–4.78; ACT x̅ = 4.66, SD = 0.43, Range = 4.21–4.95)). However, the mean CBT-specific competence score was significantly higher in the CBT condition (x̅ = 4.43, SD = 0.73, Range: 4.33–4.46) than the ACT condition – [t(67) = −6.58, p < .01]. The mean ACT-specific competencies score was significantly higher in the ACT condition (x̅ = 4.24, SD = 0.94, Range: 3.75–4.48) than in the CBT condition [t(67) = 17.52, p < .01].
Adherence. In all cases raters identified the correct treatment approach and rated all CBT sessions with the ACT adherence scale as n/a and vice versa. The mean CBT adherence score for CBT therapists was x̅ = 2.67 (SD = 0.40, Range: 1.75–3.00). The mean adherence score for each therapist was x̅ = 2.59 (SD = 0.64) and x̅ = 2.55 (SD = 0.40). The mean ACT adherence score for ACT therapists was x̅ = 2.50 (SD = 0.45, Range: 1.75–3.00). The mean adherence score for each therapist was x̅ = 2.51 (SD = 0.47), x̅ = 2.56 (SD = 0.45) and x̅ = 2.35 (SD = 0.42). The difference between the two overall means did not reach significance [t(3) = 1.17, p = 0.33].
Discussion
The main purpose of this study was to examine the effectiveness of ACT relative to the well-established CBT in a psychiatric inpatient sample with depression and mixed mental disorders, in the context of routine clinical care. We obtained confirmation of our hypothesis that both treatments lead to significant and stable symptom reductions as well as an increase in satisfaction with life. Our hypothesis that ACT would outperform CBT with respect to general symptom strain and life satisfaction was not supported. Most patients across both treatment conditions reliably improved with respect to depressive symptom strain.
Depressive Symptoms
The large and stable improvements in depressive symptoms across both therapy conditions are comparable to those of the effectiveness trial of ACT for inpatients by Benoy et al., Citation2019 and larger than those effect sizes reported in the most recently published meta-analysis of psychotherapy for inpatients (Paterson et al., Citation2018; Schefft et al., Citation2019). The present study shows that the effects of psychotherapy for inpatients found in RCTs can also be reproduced in naturalistic effectiveness trials, which supports the proposal that psychotherapy is effective in inpatient settings. Our study can add that ACT seems to be as effective as CBT and therefore, might be an alternative to CBT in the treatment of inpatients with depression. It should be noted that non-adherent patients in our sample had higher ADS scores than treatment completers within the ACT group. This suggests that patients with high symptom severity may have difficulties in engaging in this approach. Future studies should assess reasons for patient dropout and test this observation.
General Symptom Strain
In line with the effects on depressive symptoms, the treatment effects on general symptom strain were similar across the two treatment conditions. Again, the effect size is larger than the one for general symptom strain in a pre- to post-intervention study (d = 0.59) by Koesters et al. (Citation2006). Contrary to our expectation, ACT did not outperform CBT on general symptom strain. The reason why we did not find an effect may have been because ACT does not focus on symptom reduction, instead improvement in symptoms is considered a by-product of psychological flexibility. Future research should include measures of the ACT process variables in order to test whether they have an indirect effect on general symptom reduction (Stockton et al., Citation2019).
Satisfaction with Life
Similar to the pattern of treatment effects on symptoms, there was significant and stable improvement in life satisfaction in both therapy conditions. However, effects were small for both groups and stand in contrast to the results of studies investigating satisfaction and quality of life of outpatients. In these studies, large improvements in effectiveness trials of ACT and CBT could be found (A-Tjak et al., Citation2018; Forman et al., Citation2007; Oei & McAlinden, Citation2014). It may be unrealistic to expect life satisfaction to markedly improve after inpatient treatment, as the primary focus is on symptom reduction. More research on inpatient treatment effects on life satisfaction and quality of life is needed to test this proposal. However, the finding that compared to CBT, ACT was not associated with greater improvements in this domain is unexpected given that enhancing life satisfaction is a key goal of ACT (Hayes, et al., Citation2006). This may be explained by the fact that sustained personal growth in the longer term is also a focus of ACT (Hayes et al., Citation2013).
Clinical Relevance
Findings from the present study show that the statistically significant treatment effects at the group level are consistent with clinically significant improvements found at the individual level. Across both conditions most patients demonstrated clinically significant improvements, and more than half of all patients reliably improved with respects to depressive symptoms. The latter finding is similar to those of other inpatient studies (Voderholzer et al., Citation2012). With respect to general symptom strain, most patients remained unchanged across both treatment conditions. One possible explanation is, that the majority of patients were diagnosed with depression and, hence, treatment effects were more likely to emerge in this symptom domain.
Future research needs to take specific patient variables into account to investigate the potential differential effects of diagnosis, comorbidities, symptom severity and so forth.
Treatment Integrity
Both ACT and CBT therapists were rated adherent to each treatment protocol and competent in their delivery of the treatment specific techniques. Raters were able to correctly and reliably distinguish ACT and CBT specific skills. These results suggest that ACT and CBT can be differentiated from each other in clinical settings; an issue which has been widely debated in the literature (Hofmann & Asmundson, Citation2008; Ruiz, Citation2012). In order to investigate the veracity of this finding, the ACT processes that foster psychological flexibility should also be assessed in future studies to determine whether they are change mechanisms unique to ACT or common to both ACT and CBT (Gaudiano, Citation2009).
Limitations
Due to the naturalistic setting, there are some study limitations which need critical consideration when interpreting our results. First, since we did not use randomization for treatment allocation, we are unable to completely rule out systematic bias. Nevertheless, our design can be considered quasi-random, thus, there should not be a bias because of treatment preferences of the participants. Moreover, our results showed no significant between condition differences for any baseline characteristics. Therefore, it can be assumed that systematic biases should be equally distributed between both conditions. Several confounding variables also need to be considered. Determining additional eligibility after treatment assignment might have introduced bias. Since patients receiving ACT or CBT were treated at the same time and on the same ward, an informal out-of-session blending of both approaches could have occurred. Patients might have exchanged their experiences of the treatment approach they received. We did not control the content of one-on-one contacts with therapists and patients. Most of the patients were on regular medication and for most patients it had to be adjusted during therapy. However, results showed that the two treatment groups did not differ with respect to previous medication and alteration of medication during the course of the study. In general, the effects of the usual care (e.g., occupational therapy, physiotherapy, medication, and contact with nurses) cannot be separated from therapy effects and might have increased the overall effect. Moreover, these additional treatments may lead to the underestimation of possible true differences between the treatment effects attributable to psychotherapeutic treatments.
Furthermore, the duration of stay and thus the number of group therapy sessions as well as the content of the group treatment varied among patients. However, it would have been unethical and uneconomical to treat patients on the ward for longer than was necessary. Findings suggest that for some patients, a relatively short treatment period can lead to clinically significant improvements in symptoms. Patient variables that predict earlier treatment success need to be investigated in future studies. There are also limitations concerning group delivery of the interventions. First, the ACT treatment protocol developed for this study had not been previously evaluated. Second, in contrast to the manualized CBT treatment, the ACT protocol had an open format. In line with the ACT psychological flexibility framework, this enabled therapists to apply the core ACT processes on a need’s basis. Third, not all patients received the same treatment in each condition due to the open group setting and the variations in treatment duration. Fourth, although treatment integrity was evaluated, the competence scale evidenced low interrater reliability. Therefore, results referring to therapists’ competence must be viewed critically and interpreted with caution.
Due to the above mentioned critical aspects, it is important to consider that our design and power – despite a quite large sample-size – might not has been suitable for a non-inferiority trial.
Conclusions
The present study investigated a sample of 177 inpatients of a psychiatric ward with depression and other mental disorders. We kept exclusion criteria to a minimum, did not use randomization for treatment allocation, determined the clinical significance of treatment effects and used a rigorous methodology to rule out major confounding variables by using adherence and competence scales. This is the first study that has investigated the effectiveness of ACT for inpatients by comparing it to the well-established evidence-based CBT. Results support previous research findings showing that both ACT and CBT lead to significant improvements in symptom distress and life satisfaction. Findings from this study extend those of prior studies, showing that the similar treatment effects across both interventions are also evident in a regular clinical inpatient setting. In addition, results from the present study showed that both treatments produced improvements that were clinically meaningful for most patients. Patients reported high levels of satisfaction with both ACT and CBT. Our results demonstrate that patients with severe mental illness, who require inpatient treatment, benefit from both ACT and CBT. For the clinician, this offers greater flexibility in the delivery of psychological interventions to psychiatric inpatients.
Acknowledgements
We would like to thank the entire clinical staff for their intensive collaboration on our project. In particular, we would like to thank the study therapists and the nurses of our ward P09, who have succeeded in integrating the study procedures into their daily work. In addition, we would like to thank our IT department and the research assistants: without their support, the data collection would not have been possible. We acknowledge support by the Open Access Publication Fund of Humboldt-Universität zu Berlin.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, MS, upon reasonable request.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- A-Tjak, J. G., Davis, M. L., Morina, N., Powers, M. B., Smits, J. A., & Emmelkamp, P. M. (2015). A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy Psychosomatics, 84(1), 30–36. https://doi.org/10.1159/000365764
- A-Tjak, J. G., Morina, N., Topper, M., & Emmelkamp, P. M. (2018). A randomized controlled trial in routine clinical practice comparing Acceptance and Commitment Therapy with Cognitive Behavioral Therapy for the treatment of Major depressive disorder. Psychotherapy and Psychosomatics, 87, 154–163. https://doi.org/10.1159/000486807
- Attkisson, C. C., & Zwick, R. (1982). The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5(3), 233–237. https://doi.org/10.1016/0149-7189(82)90074-X
- Barkowski, S., Schwartze, D., Strauss, B., Burlingame, G. M., & Rosendahl, J. (2020). Efficacy of group psychotherapy for anxiety disorders: A systematic review and meta-analysis. Psychotherapy Research, 1–18. https://doi.org/10.1080/10503307.2020.1729440
- Benoy, C., Meyer, A., Knitter, B., Pinhard, K., Walter, M., Bader, K., & Gloster, A. T. (2019). Akzeptanz-und Commiment-Therapie mit therapieresistenten Störungen im stationären Setting. [Acceptance and Commitment Therapy for therapy-resistent disorders in an inpatient setting]. Zeitschrift für Klinische Psychologie und Psychotherapie, 48(2), 90–100. doi: 10.1026/1616-3443/a000532
- Cuijpers, P., Karyotaki, E., de Wit, L., & Ebert, D. D. (2020). The effects of fifteen evidence-supported therapies for adult depression: A meta-analytic review. Psychotherapy Research, 30(3), 279–293. https://doi.org/10.1080/10503307.2019.1649732
- Cuijpers, P., van Straten, A., & Warmerdam, L. (2008). Are individual and group treatments equally effective in the treatment of depression in adults?: A meta-analysis. The European Journal of Psychiatry, 22(1), 38–51. https://doi.org/10.1177/0193392202027001008 doi: 10.4321/S0213-61632008000100005
- Dambacher, C., & Samaan, M. (2020). Akzeptanz- und Commitmentherapie in der Gruppe [Acceptance and Commitment Therapy in groups]. Beltz.
- Davidson, J., Turnbull, C. D., Strickland, R., Miller, R., & Graves, K. (1986). The Montgomery-Åsberg Depression Scale: Reliability and validity. Acta Psychiatrica Scandinavica, 73(5), 544–548. https://doi.org/10.1111/j.1600-0447.1986.tb02723.x
- Dimidjian, S., Arch, J. J., Schneider, R. L., Desormeau, P., Felder, J. N., & Segal, Z. V. (2016). Considering meta-analysis, meaning, and metaphor: A systematic review and critical examination of “third wave” cognitive and behavioral therapies. Behavior Therapy, 47(6), 886–905. https://doi.org/10.1016/j.beth.2016.07.002
- Dunlap, W. P., Cortina, J. M., Vaslow, J. B., & Burke, M. J. (1996). Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods, 1(2), 170–177. https://doi.org/10.1037/1082-989X.1.2.170
- Eifert, G. H. (2011). Akzeptanz-und Commitment-Therapie (ACT) [Acceptance and Commitment Therapy (ACT)]. Hogrefe Verlag.
- Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Fischer, HF, Schirmer, N, Tritt, K, & Klapp, BF. (2011). Retest-Reliabilität und Änderungssensitivität des ICD-10-Symptom-Rating (ISR) in verschiedenen Stichproben. PPmP-Psychotherapie. Psychosomatik· Medizinische Psychologie, 61(03-04), 162–169.
- Fletcher, L., & Hayes, S. C. (2005). Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 23(4), 315–336. https://doi.org/10.1007/s10942-005-0017-7
- Forman, E. M., Herbert, J. D., Moitra, E., Yeomans, P. D., & Geller, P. A. (2007). A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification, 31(6), 772–799. https://doi.org/10.1177/0145445507302202
- Gaudiano, B. A. (2009). Öst's (2008) methodological comparison of clinical trials of acceptance and commitment therapy versus cognitive behavior therapy: Matching Apples with Oranges? Behaviour Research and Therapy, 47(12), 1066–1070. https://doi.org/10.1016/j.brat.2009.07.020
- Glaesmer, H., Grande, G., Braehler, E., & Roth, M. (2011). The German version of the satisfaction with life scale (SWLS). European Journal of Psychological Assessment, 27(2), 127–132. https://doi.org/10.1027/1015-5759/a000058
- Gloster, A. T., Rinner, M. T., Ioannou, M., Villanueva, J., Firsching, V. J., Ferrari, G., Benoy, C., Bader, K., & Karekla, M. (2019). Treating treatment non-responders: A meta-analysis of randomized controlled psychotherapy trials. Clinical Psychology Review, 101810), https://doi.org/10.1016/j.cpr.2019.101810
- Hacker, T., Stone, P., & MacBeth, A. (2016). Acceptance and commitment therapy–Do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. Journal of Affective Disorders, 190, 551–565. https://doi.org/10.1016/j.jad.2015.10.053
- Harris, R. (2011). ACT leicht gemacht [ACT made simple]. Arbor.
- Hautzinger, M., & Bailer, M. (1993). Allgemeine Depressions-Skala: ADS; Manual: Beltz-Test-GmbH.
- Hautzinger, M., & Kischkel, E. (1999). Kurzzeit-Psychotherapeutisches Behandlungskonzept für unterschwellige und leichte depressive Störungen. Ein Behandlungsmanual [Short term psychothera-peutic treatment concept for subliminal and minor depressivedisorders. A treatment manual] (Vol. 3.3.1). Klinik und Poliklinik für Psychiatrie und Psychotherapie der Rheinischen Friedrich Wilhelms Universität Bonn.
- Hayes, S. C. (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavior therapy. Behavior Therapy, 35, 639–665. https://doi.org/10.1016/S0005-7894(04)80013-3
- Hayes, S. C. (2008). Climbing our hills: A beginning conversation on the comparison of acceptance and commitment therapy and traditional cognitive behavioral therapy. Clinical Psychology: Science and Practice, 15(4), 286–295. https://doi.org/10.1111/j.1468-2850.2008.00139.x
- Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44(2), 180–198. https://doi.org/10.1016/j.beth.2009.08.002
- Hayes, S. C., Masuda, A., Bissett, R., Luoma, J., & Guerrero, L. F. (2004). DBT, FAP, and ACT: How empirically oriented are the new behavior therapy technologies? Behavior Therapy, 35(1), 35–54. https://doi.org/10.1016/S0005-7894(04)80003-0
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., Lillis, J. J. B. r., & therapy. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behavior Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006
- Hofmann, S. G., & Asmundson, G. (2008). Acceptance and mindfulness-based therapy: New wave or old hat? Clinical Psychology Review, 28(1), 1–16. https://doi.org/10.1016/j.cpr.2007.09.003
- Jacobi, F., Uhmann, S., & Hoyer, J. (2011). Wie häufig ist therapeutischer Misserfolg in der ambulanten Psychotherapie? Zeitschrift für Klinische Psychologie und Psychotherapie, 40, 246–256. https://doi.org/10.1026/1616-3443/a000122
- Jacobson, N. S., Follette, W. C., & Revenstorf, D. (1984). Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy, 15(4), 336–352. https://doi.org/10.1016/S0005-7894(84)80002-7
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006X.59.1.12
- Koesters, M., Burlingame, G. M., Nachtigall, C., & Strauss, B. (2006). A meta-analytic review of the effectiveness of inpatient group psychotherapy. Group Dynamics: Theory, Research, and Practice, 10(2), 146–163. https://doi.org/10.1037/1089-2699.10.2.146
- Little, R. J. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202. doi: 10.1080/01621459.1988.10478722
- McGrath, K. B. (2012). Validation of the Drexel University ACT/tCBT adherence and competence rating scale: Revised for use in a clinical population (Dissertation), Drexel University, Philadelphia. https://idea.library.drexel.edu/islandora/object/idea%3A3803
- Morris, S. B. (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. https://doi.org/10.1177/1094428106291059
- Müller, M. (2018). Entwicklung einer Skala zur Erfassung psychotherapeutischer Kompetenz in der Akzeptanz – Commitmenttherapie und der Kognitiven Verhaltenstherapie [Development of a scale to assess therapeutic competence in Acceptance and Commitment Therapy and Cognitive Behavior Therapy.] Unpublished manuscript. University of Potsdam.
- Neumann, N., & Schulte, R. (1989). MADR-Skala zur psychometrischen Beurteilung depressiver Symptome (MADRS) [MADR-Scale for psychometric assessment of depressive symptoms]. Perimed.
- Oei, T. P., & McAlinden, N. M. (2014). Changes in quality of life following group CBT for anxiety and depression in a psychiatric outpatient clinic. Psychiatry Research, 220(3), 1012–1018. https://doi.org/10.1016/j.psychres.2014.08.036
- Öst, L.-G. (2014). The efficacy of Acceptance and Commitment Therapy: An updated systematic review and meta-analysis. Behaviour Research Therapy, 61, 105–121. https://doi.org/10.1016/j.brat.2014.07.018
- Paterson, C., Karatzias, T., Dickson, A., Harper, S., Dougall, N., & Hutton, P. (2018). Psychological therapy for inpatients receiving acute mental health care: A systematic review and meta-analysis of controlled trials. British Journal of Clinical Psychology, 57(4), 453–472. https://doi.org/10.1111/bjc.12182
- Petersen, C. L., & Zettle, R. D. (2009). Treating inpatients with comorbid depression and alcohol use disorders: A comparison of acceptance and commitment therapy versus treatment as usual. The Psychological Record, 59(4), 521–536. https://doi.org/10.1007/BF03395679
- Pleger, M., Treppner, K., Diefenbacher, A., Schade, C., Dambacher, C., & Fydrich, T. (2018). Effectiveness of Acceptance and Commitment Therapy compared to CBT+: Preliminary results. The European Journal of Psychiatry, 32(4), 166–173. https://doi.org/10.1016/j.ejpsy.2018.03.003
- Radloff, L. S. (1977). The CES-D Scale: A Self-Report Depression Scale for research in the general population. Applied Psychological Measurement, 1, 385–401. https://doi.org/10.1177/014662167700100306
- Ruiz, F. J. (2012). Acceptance and commitment therapy versus traditional cognitive behavioral therapy: A systematic review and meta-analysis of current empirical evidence. International Journal of Psychology Psychological Therapy, 12(3), 333–358.
- Samaan, M., Sauer, E., Müller, M., Fydrich, T., Diefenbacher, A., Burian, R., Schade, C., & Weck, F. (in press). Entwicklung und Validierung von Skalen zur Erfassung der Adhärenz von ACT und KVT Therapeuten im transdiagnostischen Gruppensetting [Development and validation of scales to assess adherence of ACT and CBT therapists for transdiagnostic groupsettings]. Zeitschrift für Klinische Psychologie und Psychotherapie.
- Schefft, C., Guhn, A., Brakemeier, E. L., Sterzer, P., & Köhler, S. (2019). Efficacy of inpatient psychotherapy for major depressive disorder: A meta-analysis of controlled trials. Acta Psychiatrica Scandinavica, 139(4), 322–335. https://doi.org/10.1111/acps.12995
- Schmidt, J., Lamprecht, F., & Wittmann, W. W. (1989). Zufriedenheit mit der stationären Versorgung. Entwicklung eines Fragebogens und erste Validitätsuntersuchungen [Satisfaction with inpatient care: Development of a questionnaire and first validity assessments]. PPmP: Psychotherapie Psychosomatik Medizinische Psychologie, 39(7), 248–255.
- Schmidt, K.-H., & Metzler, P. (1992). Wortschatztest: WST [Vocabulary test: WST]: Beltz.
- Sonntag, R. F. (2011). Akzeptanz-und Commitment-Therapie [Acceptance and Commitment therapy]. In M. Linden, & M. Hautzinger (Eds.), Verhaltenstherapiemanual (pp. 363–370). Springer.
- Stockton, D., Kellett, S., Berrios, R., Sirois, F., Wilkinson, N., & Miles, G. (2019). Identifying the underlying mechanisms of change during acceptance and commitment therapy (ACT): A systematic review of contemporary mediation studies. Behavioural Cognitive Psychotherapy, 47(3), 332–362. https://doi.org/10.1017/S1352465818000553
- Tritt, K, Von Heymann, F, Zaudig, M, Probst, T, Loew, T, Klapp, B, Söllner, W, Fydrich, T, & Bühner, M. (2015). ICD-10-Symptom-Rating (ISR) - Das Handbuch zum Fragebogen. Graz: neobooks.
- Tritt, K., von Heymann, F., Zaudig, M., Zacharias, I., Söllner, W., & Loew, T. (2008). Entwicklung des Fragebogens» ICD-10-Symptom-Rating «(ISR). Zeitschrift für Psychosomatische Medizin und Psychotherapie, 54(4), 409–418. https://doi.org/10.13109/zptm.2008.54.4.409
- van Ginkel, J. R., & Kroonenberg, P. M. (2014). Analysis of variance of multiply imputed data. Multivariate Behavioral Research, 49(1), 78–91. https://doi.org/10.1080/00273171.2013.855890
- Voderholzer, U., Koch, S., Hillert, A., & Schlegl, S. (2012). Response und non-response in der stationären Psychotherapie depressiver Patienten [Response and non-response in inpatient psychotherapy of depressive patients]. Psychotherapeut, 57(5), 410–416. https://doi.org/10.1007/s00278-012-0931-y
- Weck, F., Hautzinger, M., Heidenreich, T., & Stangier, U. (2010). Erfassung psychotherapeutischer Kompetenzen: Validierung einer deutschsprachigen Version der Cognitive Therapy Scale [Assessing psychotherapeutic competencies: Validation of a German version of the Cognitive Therapy Scale]. Zeitschrift für Klinische Psychologie und Psychotherapie: Forschung und Praxis, 39(4), 244–250. https://doi.org/10.1026/1616-3443/a000055
- Wengenroth, M. (2012). Therapie-Tools Akzeptanz-und Commitmenttherapie: Mit Online-Materialien [Acceptance and Commitment Therapy: With online material]. Beltz.
- Wengenroth, M. (2013). Das Leben annehmen: so hilft die Akzeptanz-und Commitmenttherapie (ACT) [Accepting life: that is how Acceptance and Commitment Therapy (ACT) works]. Huber.
- Wittchen, H.-U., Wunderlich, G., & Zaudig, M. (1997). Strukturiertes Klinisches Interview für DSM-IV [Structured Clinical Interview for DSM-IV]. Hogrefe.