Abstract
Objective: Mentalization-based treatment (MBT) is an evidence-based long-term treatment for borderline personality disorder (BPD). Alliance is central for effective psychotherapies. Few studies have addressed aspects of working alliance in BPD evidence-based treatments. This study aimed to investigate alliance development in MBT therapies with different clinical outcomes. Method: The sample included 155 patients in an MBT programme. Clinical outcomes were based on Global Assessment of Functioning (GAF). The sample was divided in two subgroups according to GAF levels at the end of treatment (cut-off = 60). Working alliance was assessed by patient report (Working Alliance Inventory, subscales, Goals, Bonds and Tasks) and assessed repeatedly over 36 months. The method for statistical analyses was linear mixed models. Results: Initial levels of Goals, Bonds, and Tasks did not differ by subgroup, but change over time differed significantly by subgroup. In the good outcome subgroup, ratings of Goals, Bonds, and especially Tasks increased significantly over time. In the poor outcome subgroup, paranoid PD was associated with poorer alliance development over time. Conclusions: Good outcome therapies were characterized by a process where the working alliance grew over time. Results encourage an explicit focus on tasks in therapy particularly for patients with high levels of mistrust.
Clinical or methodological significance of this article: This article points to the clinical importance of maintaining careful alliance work in the treatment of poorly functioning patients with BPD. Such work includes not only a longer-term process of attachment and bonding, but also keeping the goals of therapy understandable, current and updated, and making the therapeutic work, progress, and challenges relevant and explicit. As a specialized treatment for BPD, MBT includes interventions and structure aiming to support therapists and thereby facilitate therapy for poorly functioning patients with considerable emotional and relational problems.
The working alliance predicts approximately 7.5% of the variance in treatment outcomes and is considered a major mechanism of change in psychotherapy (Flückiger et al., Citation2018; Wampold & Imel, Citation2015). It has been operationalized in terms of (i) agreement on the Goals of treatment, (ii) the formation of personal Bonds between patient and therapist, and (iii) the therapeutic work process, conceptualized as Tasks (Bordin, Citation1979). Nevertheless, there are still few studies following the development of the working alliance in long-term therapies, especially the subparts of alliance—Goals, Bonds, and Tasks (Stiles & Goldsmith, Citation2010). The therapeutic alliance may be a crucial factor in treatment for borderline personality disorder (BPD; Dimaggio et al., Citation2019), but it is poorly investigated in evidence-based treatments for BPD.
The therapeutic alliance is not always easily established in psychotherapy (Colli et al., Citation2014), not least in the treatment of severe BPD patients. Epistemic trust––that is, the basic ability to trust significant social information from others—is a relevant concept possibly related to the working alliance. It is considered fundamental for the development of interpersonal and relational capacity, and impairment has been linked to BPD (Bo et al., Citation2017). In psychotherapy, work on difficulties in the alliance may in itself be essential (Safran & Muran, Citation2000; Wampold & Imel, Citation2015), and for BPD patients, alliance improvement can even be seen as a treatment outcome (Muran & Barber, Citation2011). In light of the profound attachment problems apparent among many BPD patients, we see a need for further investigation of alliance processes in structured BPD treatments.
Mentalizing is a core aspect of personality functioning and may be defined as an imaginative mental activity enabling perception and interpretation of mental states (e.g., needs, desires, feelings, beliefs, and goals) (Fonagy et al., Citation2015). Among patients with BPD, personality problems have been associated with attachment insecurity, tendencies of dysphoria, emotional dysregulation, and social misinterpretations—often in terms of hyper-mentalizing (Sharp, Citation2014; Vaskinn et al., Citation2015). Mentalization-based treatment (MBT) is a specialized BPD treatment developed from traditional psychoanalysis and research on attachment and social cognition (Bateman & Fonagy, Citation2016). Across different treatment theories and techniques, therapists primarily aim to engage the patient in work that feels meaningful, although the emphasis on each alliance component (Goals, Bonds, and Tasks) may be different (Falkenström & Larsson, Citation2017; Horvath & Greenberg, Citation1989; Muran & Barber, Citation2011). In this article we aim to investigate how the different alliance components develop in MBT.
MBT is a long-term, manualized, multicomponent treatment programme (Bateman & Fonagy, Citation2016; Karterud, Citation2015). It consists of five structural pillars (Bateman & Fonagy, Citation2016): (i) specific BPD psychoeducation about core personality problems and the focus of MBT treatment, (ii) an individually adjusted case formulation that is dynamic (changeable during the treatment process), (iii) the combination of individual and group formats of long-term psychotherapy, (iv) a team of therapists working together with regular MBT supervision, and (v) a frame and style of intervention aiming to facilitate a mentalizing process. Together these pillars can be seen as enforcements promoting the development of a therapeutic alliance. The first two explicitly address Goals and Tasks of treatment, the third adds the opportunity for interpersonal bonding (i.e., the bond part of the working alliance), and the fourth and fifth support therapists’ interventions, techniques, reflective practice, and handling of countertransference. The latter are considered essentially important as adherent therapist interventions in MBT have been associated with improved reflective functioning (Möller et al., Citation2017).
Positive effects of MBT are demonstrated in several studies, and outcomes mainly include symptomatic alleviation and the reduction of self-harming or suicidal behaviours and hospital admissions (Volkert et al., Citation2019). There are yet few investigations of working alliance for patients in MBT. Nonetheless, in a qualitative study of change processes in MBT, Morken et al. (Citation2019) emphasize the importance of repairing alliance ruptures. In other studies, patients’ positive experiences include the identification of personality problems, a feeling of symptom improvement, and the content of therapeutic work—learning to regulate oneself, gaining new perspectives, or attending groups (Dyson & Brown, Citation2016; Johnson et al., Citation2016; Lonargáin et al., Citation2017). A recent MBT study pointed to interventions focusing on mentalizing positive affects as possibly beneficial for alliance (Harpøth et al., Citation2019). Moreover, in a study of MBT group therapy, interpersonal personality features influenced the establishment of a working alliance in the group (Euler et al., Citation2018), and the authors recommended particular apprehension of BPD patients’ relational bias and hyper-mentalization in the early phase of therapy.
Specialized approaches involve specified therapeutic formats and techniques, and all have relational implications (Fonagy et al., Citation2002). Most structured treatments include explicit psychoeducation and the use of case formulations, which may be important factors in the early development of alliance—establishing mutual agreement on aims and tasks in therapy. In psychotherapy processes, therapist empathy is a recognized facilitating factor, contributing to the bond between patient and therapist. MBT manuals emphasize that the patient needs to be validated and understood before being challenged on maladaptive patterns (Karterud et al., Citation2020; Karterud & Bateman, Citation2010), and the recommended therapeutic stance is to be mentalizing and curious as well as genuine and non-judgmental. Correspondingly, in Schema-Focused Therapy (SFT), mutual trust and positive regard (Bonds) are emphasized as important alliance elements (Young et al., Citation2006), underlining the importance of an unthreatening, supportive therapist attitude. It is furthermore proposed that the SFT model itself promotes sympathy with the BPD patient (Young et al., Citation2006). A comparison study of SFT versus Transference-Focused Psychotherapy (TFP) indicated an increase in therapeutic alliance during both treatments (Spinhoven et al., Citation2007). In a study of Dialectical Behaviour Therapy (DBT), higher patient-rated therapy commitment and working capacity was associated with fewer suicide attempts (Bedics et al., Citation2015). As of yet, we have not found studies investigating relations between MBT alliance and outcomes.
The overriding aim of the current study was to investigate how aspects of therapeutic alliance (Goals, Bonds and Tasks) developed over time in MBT for patients with BPD. The study primarily aimed to investigate alliance processes in therapies with different clinical outcomes, and secondarily to explore variation associated with different patient characteristics.
Material and Methods
Design
The study is a quantitative, observational study with a longitudinal design.
Subjects
The studied sample included 155 BPD patients treated in an MBT unit during 2009–2016. Patients were referred on a regular basis to the outpatient clinic, which was on a specialist mental health service level, situated within a university hospital setting.
Mentalization-Based Treatment (MBT)
MBT was an outpatient treatment in accordance with MBT manuals (Karterud, Citation2011, Citation2012; Karterud & Bateman, Citation2010). The first year included weekly sessions of individual and group therapy and a psychoeducational group (12 sessions). Frequencies of individual therapy were gradually reduced in the second and third year, while group sessions continued throughout treatment. Treatment had an upper time limitation of 36 months.
Therapists
The team included three psychiatric nurses, three psychiatrists, an art therapist, a physiotherapist, a social worker, and two psychologists. Eight were qualified group analysts—one in psychoanalysis, one in individual psychodynamic psychotherapy—67% were females, and mean age (year 2009) was 53 (SD = 9) years. Other individual therapists within the research period were different resident doctors and psychologists in training. All had basic MBT training and attended weekly video-based supervision by qualified MBT supervisors.
Therapist MBT Fidelity
MBT adherence and competence was assessed by video-recorded therapy sessions using the MBT Adherence and Competence Scale (Karterud et al., Citation2013) and the Adherence and Competence Scale for Mentalization-based Group Therapy (Folmo et al., Citation2017). On a 1–7 scale, a score of four or higher indicates adequate MBT adherence/competence. In 2013–2015, five raters evaluated 19 individual sessions (eight therapists) and 9 group sessions in the programme. For individual therapists, the mean adherence level was 4.7 (SD = 1.2) and the mean MBT competence level was 4.4 (SD = 1.2) (Kvarstein et al., Citation2019). For group therapists, the mean adherence level was 5.1 (SD = 1.37) and competence level 4.9 (SD = 1.30) (Kvarstein et al., Citation2020). This is comparable to a recent RCT study of MBT in groups for adolescents with BPD (Beck et al., Citation2020).
Baseline Assessment of Diagnoses
The MBT unit was part of a collaborative cross-regional network for treatment and research on personality disorders where all units used standardized measures for diagnostic assessment. Diagnoses were decided in accordance with the DSM-IV using the Mini International Neuropsychiatric Interview (MINI; Lecrubier et al., Citation1998) for symptom disorders and for PDs and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II; First et al., Citation1994). Assessments were performed by clinical staff with systematic training provided by the network in diagnostic interviews and principles of the LEAD-procedure (Longitudinal, Expert, All-Data; Pedersen et al., Citation2013). Evaluations were concluded with a psychiatrist.
Baseline Assessment of Other Patient and Treatment Factors
Self-reports of personality functioning, life quality, and work/study functioning (patient factors) and information about treatment termination (treatment factors) included the following:
Severity Indices of Personality Functioning—Short Form (SIPP-SF; Rossi et al., Citation2017) is a 60-item version of the original SIPP-118 (Pedersen, Arnevik, et al., Citation2017). It includes five personality problem domains. In this study the three domains with greatest impairment were: Identity Integration (12 items, aspects of enjoyment, meaning, self-esteem, and self-perception), Relational Capacity (10 items, aspects of attachment, intimacy, enjoying relationships, feeling appreciated, and being affectionate), and Self-control (12 items, aspects of controlling emotional reactions and impulsive behaviours). The remaining SIPP-SF domains are Responsibility and Social Concordance (Normal range T-scores: 40–60).
EuroQol (EQ-5D) evaluates subjective life quality along five health dimensions and a global index (0–1). In the general population in Western societies, the global index score range is 0.80–0.89 (Saarni et al., Citation2007) and in PD populations 0.56 (Soeteman et al., Citation2008).
The number of months they worked or studied at least 50% during the previous year was recorded to indicate current work functioning status by the patients.
Reasons for treatment termination were recorded by the therapist.
Repeated Assessment of Working Alliance
The Working Alliance Inventory-Short (WAI-S; Tracey & Kokotovic, Citation1989), which is based on the Working Alliance Inventory (WAI; Horvath & Greenberg, Citation1989), was applied regularly after three months, then every sixth month during treatment, and once more at discharge. Due to the publication of the revised version (WAI-SR) by Hatcher and Gillaspy (Citation2006), the WAI-S was replaced by WAI-SR in 2012. Both WAI versions include three subscales—Goals, Bonds, and Tasks—with four items for each. Each item is rated on a 7-point scale, and scores above 4 signify satisfactory alliance. presents differences between WAI versions. In the following, we use the term WAI-S/SR. The possible impacts of differences in WAI versions were investigated using a categorical variable identifying subgroups with only the WAI-S version, only the WAI-SR version, and both versions (longitudinal data series with both WAI-S and WAI-SR). In the first part of the study, patients received the WAI-S (n = 34). From June 2012, admitted patients had only WAI-SR measures (n = 71). The remaining patients had longitudinal data-series including both versions.
Table I. Working alliance inventory—items according to WAI-S and WAI-SR.
Assessment of Clinical Outcomes
The observer-rated Global Assessment of Functioning (GAF) provides a composite score combining social and symptom-related impairment and was therefore chosen as a global outcome measure (0–100 scale, Axis V, DSM-IV) (Pedersen et al., Citation2018). GAF evaluations were performed by staff therapists (baseline, after three months, repeatedly every sixth month throughout treatment, and at treatment termination). All therapists working at the unit received a systematic GAF training course. The validity and generalizability of GAF scores was previously investigated within several treatment units representing the same clinical contexts and included therapists at the specific unit (Pedersen et al., Citation2007). The study demonstrated high consistency of GAF scores across different raters and also different treatment units (generalizability coefficients of absolute decision (the score) range .86 to .95).
High GAF scores indicate better psychosocial functioning; scores above 60 represent mild/no impairment (Pedersen et al., Citation2018). In this study, the sample (n = 155) was divided into two subgroups according to outcomes: (i) the poor outcome subgroup (GAF below 60 at the end of treatment; 43%) and (ii) the good outcome subgroup (GAF equal or above 60 at the end of treatment; 57%). All 155 patients had a baseline GAF assessment, and 7 patients lacked a final GAF assessment on treatment termination.
In order to supplement GAF as an observer-rated instrument, outcomes additionally included two patient-reported measures also administered at baseline, after three months, repeatedly every sixth month throughout treatment, and at treatment termination. All self-report measures (outcomes and alliance) were administered by the secretary at the unit. The profiles from self-reports constituted a basis for clinical evaluation of treatment progress.
The Work and Social Adjustment Scale (WSAS) is a validated 5-item self-report measure of functional impairment (i.e., work, social and private leisure activities, domestic work, and close relations) (Pedersen, Kvarstein, et al., Citation2017). Total sum-scores below 15 represent mild/no impairment (Mundt et al., Citation2002); these scores were found among 58% of the patients who filled in self-reports at the end of treatment. Among these, 85% were also in the good outcome GAF subgroup. All 155 patients had the baseline assessment, but 42 patients lacked a final WSAS assessment on treatment termination.
The BSI-18 is a self-report measure derived from the 53-item Brief Symptom Inventory (BSI), a shortened form of the Symptom Checklist-90-Revised (SCL-90-R) (Derogatis, Citation2000). The BSI includes 18 items and assesses symptom distress (depression, somatization, anxiety) on a 0–4 scale. Non-clinical distress is indicated by a mean sum-score of 0.8 (Pedersen & Karterud, Citation2004), which was found among 48% of the patients who filled in self-reports at the end of treatment. Among these, 78% were also in the good outcome GAF subgroup. All 155 patients had the baseline assessment, but 42 patients lacked a final BSI assessment on treatment termination.
The process and outcome measures used in this study were a part of the standardized assessment and treatment evaluation used within the collaborative cross-regional network for treatment and research on personality disorders.
Ethics
All patients gave written, informed consent to participate in the research. The treatment unit collected clinical data, which was registered in an anonymous database administrated by Oslo University Hospital. Procedures for data collection ensured that participating individuals could not be identified. Data security systems were approved by the Data Protection Official at Oslo University Hospital. Based on anonymous data, ethical approval was not required from the Regional Committee for Medical Research and Ethics.
Statistical Procedures
Hierarchical models (mixed models) (Singer & Willett, Citation2003) were used for statistical analyses of longitudinal data (mixed models, IBM SPSS statistics version 25) in order to maximize utilization of available patient data and capture change over time. Time (months from baseline) was modelled as a continuous variable in all models. Linear trajectories captured significant longitudinal trends for all dependent variables, among which WAI-S/SR was the main dependent variable, and GAF, WSAS, and BSI represented preliminary analyses (p < 0.001). Log likelihood estimations of model fit indicated significant improvements from an unconditional model to a linear random coefficients (intercept and slope) model (critical values for chi-square statistic: p < 0.01) using an unstructured covariance type. The equation was: Yij = β0 + β1 timeij + b0 + b1 timeij + εij. Y is the dependent variable for all observations, individuals (i), and assessment times (j), β is the fixed effects regression coefficient, b the random effects regression coefficient, and ε indicates residual variation. The categorical variable for different WAI versions was investigated in the three WAI-S/SR subscale models; some reduction of longitudinal variation (3, 7, and 5%, respectively) was discovered, but estimate deviations were not statistically significant (p > 0.05) and did not improve AIC estimations of model fit.
Initial analyses investigated the longitudinal change of clinical outcome variables and variation associated with selected patient and treatment factors as predictors. The investigated patient and treatment factors were chosen on the basis of descriptive sample characteristics in the two outcome subgroups () and are given in . The main investigation included longitudinal change of WAI-S/SR subscales and variation associated with the dichotomous GAF variable as a predictor, as well as a moderator interaction combining the dichotomous GAF variable and patient factors. The equations for the predictor analyses were: Yij = β0 + β1 timeij + β2 PRED + β3 PRED timeij + b0 + b1 timeij + εij. The equations for the moderator analyses were: Yij = β0 + β1 timeij + β4 PREDMOD + β5 PREDMOD timeij + b0 + b1 timeij + εij. For interpretation of predictors/interactions; each model is judged by the predictor-associated deviation of the trajectory for the dependent variable (estimated deviation of intercept level and slope/change-rate), explained variation (% change from the estimated variation in the initial linear random coefficients model), and change in estimates of log likelihood statistics (indices of model fit, Akaikes Information Criterion, AIC).
Table II. Baseline characteristics for MBT patients in subgroups with good and poor outcomes.
Table III. Linear mixed model estimations: Clinical outcomes and variation for patients in MBT.
The sample had unbalanced data with different numbers of assessments per patient. The chosen method for longitudinal analyses incorporates unbalanced data and uses all available data for each individual trajectory. Therefore, in this study, we did not use imputation to compensate for missing data. All included patients had at least one assessment. The mean number of WAI-S/SR assessments was 3.2 (SD = 1.8, range 1–9), 48% lacked the final assessment, 22% had only one assessment, 58% had at least three, and 38% had four or more during the course of treatment. Among the 34 patients with only one assessment, 53% were early alliance assessments performed within the first year. A variable counting numbers of assessment points for each individual captured a relevant missing data pattern. To investigate the effect of this missing data pattern on the outcomes, the variable was added as a predictor in all three working alliance subscale models (Hedeker & Gibbons, Citation1997). Analyses indicated poorer initial alliance ratings for patients with fewer assessments (for all working alliance subscales p < 0.05), but no significant effect of the variable on alliance development over time (p > 0.05, all subscales). As longitudinal effects were of primary interest, we did no further overall estimation of missing-data effects.
All final longitudinal working alliance models included (a) investigations controlling for differences in WAI versions, (b) investigations controlling for different numbers of assessment, and (c) models investigating the supplementary dichotomous WSAS and BSI outcome variables.
Results
Descriptive Data in Subgroups with Different Outcomes
Patient factors
The vast majority had BPD with severe disorder, indicated by poor life-quality, considerable comorbidity, and personality problems across all domains, although most severe within the domains of identity and self-control (). Differences by GAF outcome subgroup were minor (p > 0.1, independent samples T-test) with the exception of younger age, fewer patients with no months of work/study at all previous year, and fewer with comorbid Paranoid PD and mood disorder in the good outcome subgroup (p < 0.05, independent samples T-test).
Treatment factors
Mean treatment duration was 27 months (SD 13), early drop out (<6-month duration) was minimal (2.5%), and neither differed by subgroup (p > 0.05, independent samples T-test/Pearson chi square test). Nearly all patients in the good outcome subgroup completed treatment according to plan (91%) versus 58% in the poor outcome subgroup (p < 0.05, Pearson chi square test). In the good outcome group, there were no later drop-outs, termination was advised for 2%, and no patients were referred to other institutions. In the poor outcome group, 9% were later drop-outs, termination was advised for 12%, and 13% were referred to other institutions when they terminated treatment.
Clinical Outcomes and Factors Associated with Longitudinal Outcome Variation
Baseline levels indicated severe problems of functioning and distress at the start of MBT, and significant variation was found within the longitudinal data for all three outcome variables. Overall, corresponding and significant longitudinal improvement over time was found for GAF, WSAS, and BSI (). Mean change was for GAFadmission 48.1 (SD 5.5) to GAFdischarge 61.7 (SD11.7) (n = 148), for WSASadmission 25.9 (SD 7.9) to WSASdischarge 13.7 (SD 10.7) (n = 107), and for BSIadmission 2.1 (SD 0.8) to BSIdischarge 1.2 (SD 0.9) (n = 107). Among significant treatment factors (), completing treatment according to plan was strongly associated with better GAF improvement, and this explains 25% of the GAF slope variation (). Age and paranoid PD were also noteworthy patient factors, explaining 2–5% of the GAF slope variation. Higher age was associated with significantly poorer GAF improvement (). Mood disorder was significantly associated with baseline GAF but did not explain further variation of GAF development over time (). These preliminary analyses suggested that intrinsic treatment factors were relevant for further investigation and also pointed to certain patient factors. We thus proceeded with investigations of the main dependent variable, WAI-S/SR, as a potential indicator of intrinsic treatment quality, with the dichotomous GAF subgroup variable as an indicator of outcome variation.
Main Analyses: Longitudinal Course of Working Alliance
Overall, patients rated high initial levels of working alliance. Goals, Bonds, and Tasks all had initial levels well within a satisfactory range, and the overall picture of change over time in the sample was a significant increase of all three working alliance subscales (). Analyses also revealed significant longitudinal between-subject variation. These change patterns also remained significant in models (a) controlling for variation associated with different WAI versions and (b) investigating possible bias of different assessment numbers.
Table IV. Working alliance in subgroups with high or poor end GAF in MBT individual therapy.
Variation associated with good and poor outcome subgroups
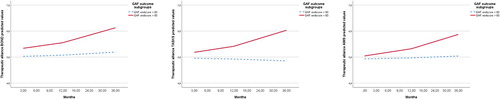
The good and poor outcome subgroup predictor was investigated in each of the three models. Initial levels of Goals, Bonds, and Tasks did not differ by subgroup, but change over time was significantly different by subgroup (; ). The subscale Goals accounted for 23% of the WAI-S/SR slope variation, Bonds for 25%, and Tasks for 35% (). Results remained significant (p < 0.05; all analyses used linear mixed models) for the three subscales—Goals, Bonds, and Tasks—in models (a) controlling for variation associated with different WAI versions, (b) investigating possible bias of different assessment numbers, and (c) corresponding differences were also found in models investigating the dichotomous WSAS and BSI outcome variables as predictors. Further investigation dividing the sample by outcome subgroup revealed the following. Including only patients in the good outcome subgroup, ratings of Goals, Bonds, and Tasks increased significantly over time (for all p < 0.05). Including only patients in the poor outcome subgroup, change over time was not significant for any of the WAI-S/SR subscales (for all p > 0.1).
Variation associated with patient factors
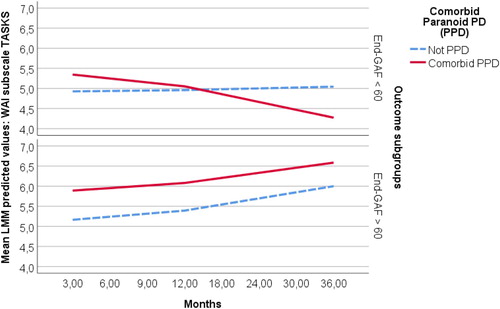
Relevant patient factors (age, comorbid mood disorder, and comorbid paranoid PD) were investigated as separate predictors added to the three WAI-S/SR subscale models. Age was not associated with significantly deviating initial alliance levels or deviating change over time (all subscales, p > 0.1), but explained some longitudinal variation. Paranoid PD was not significantly associated with initial alliance levels (all subscales, p > 0.1), but associated with significantly less improvement of two of the three subscales over time (Tasks and Bonds, p < 0.05). Although the slope deviation of Goals was not significant, paranoid PD explained 8% of the slope variation of this subscale (p = 0.11). Mood disorder was associated with significantly lower initial alliance levels, but not deviating change over time (all subscales, p > 0.1). demonstrates estimates for the subscale Tasks, also illustrated in .
Further investigation included the moderator interaction between outcome subgroups and (i) paranoid PD and (ii) age. Paranoid PD was not associated with baseline deviation of WAI-S/SR ratings in any of the two outcome subgroups (p > 0.1, all three subscales). The presence of paranoid PD was associated with significantly poorer development of WAI-S/SR subscales over time in the poor outcome subgroup (p < 0.05, all subscales), but not in the good outcome subgroup (p > 0.1, all subscales). The impact of age on alliance development was not further explained by differentiation according to outcome subgroup (p > 0.1, all subscales).
Significant results remained (p < 0.05) in models controlling for variation associated with different WAI versions. In models investigating possible bias of different assessment numbers, the trend of poorer development of WAI-S/SR subscales over time was less prominent (p < 0.1, all subscales). Corresponding results for paranoid PD were also found in models investigating the supplementary dichotomous WSAS and BSI outcome variables.
Discussion
There is little research on alliance and outcomes in specialized treatments for BPD. This study represents a large sample of patients attending a mentalization-based treatment (MBT) programme in an outpatient format in a regular, not an experimental, treatment setting. It is among the first longitudinal studies of alliance in MBT and captures patterns of early alliance in a large sample of patients with BPD.
Main Findings
Overall, patient-reported working alliance in MBT was initially within a satisfactory range (scores above 4). During therapy, all subscales—Goals, Bonds, and Tasks—increased over time. Differentiation in subgroups with good and poorer outcomes revealed the following:
Initial working alliance—Goals, Bonds, and Tasks—did not differ by outcome.
Positive temporal development of therapeutic alliance during therapy characterized good outcomes.
Outcome subgroups differed most in the development of the Tasks subscale.
Comorbid paranoid PD was more frequent in the subgroup with poor outcomes and associated with poorer alliance development in this subgroup.
In Bordin’s (Citation1979) operationalization of alliance, an important formative and collaborative aspect of the process takes place in the initial phase—the agreement upon Goals in therapy. In MBT, treatment Goals are defined in an early case formulation tailored for the individual patient. In line with other psychotherapy research, MBT also emphasizes the importance of patients’ own understanding in the negotiation of work in therapy (Muran & Barber, Citation2011). As poorly functioning patients may have difficulties formulating or understanding the concepts of therapy, MBT recommends clear, simple, and short formulations. Given the emphasis of relational problems among BPD patients, the early alliance ratings in this study were high—perhaps more so than could be expected. However, others have also demonstrated high alliance levels in psychotherapy despite severe interpersonal problems (Ollila et al., Citation2016). The authors discuss how patients with extensive interpersonal problems might feel a strong need for help and be motivated to engage in the process. In the present sample, initial alliance levels may likewise reflect positive expectations in the start of therapy.
Being referred to an extensive MBT programme is often preceded by several former treatment attempts. Illustrating this point, a recent qualitative study of MBT emphasized how patients experienced a positive shift of expectations when starting to engage in therapy (Gardner et al., Citation2020). Expectations were nevertheless ambiguous, ranging from seeing MBT as potentially life-saving to perceptions of MBT as “a last chance saloon.” The latter illustrates how the early alliance may also be extremely fragile. In the current poorly functioning BPD sample, self-reported relational problems, covering issues of attachment and intimacy, were notable. Characteristically, relational problems among BPD patients represent a strong need for close relationships together with high interpersonal sensitivity and overwhelming fear of rejection.
In the present study, poorer alliance levels were related to comorbid mood disorder, and overall, patients’ personality problems reflected low levels of self-esteem, enjoyment, and meaning. Comorbidity of BPD and mood disorder is generally common—the two conditions share vulnerabilities and may be hard to distinguish (Skodol et al., Citation2010). This study demonstrates that the collaborative starting point of therapy was negatively influenced by dysphoria. Interestingly, over time, its negative effect was not enduring. Although viewed as a potential setback at onset, comorbid mood disorder did not complicate a treatment process focusing on core personality problems.
Moreover, the subgroups with different clinical outcomes did not differ with respect to their initial ratings of alliance. Attachment processes in treatment are assumed to take time. The present study captures the development of alliance among BPD patients in a specialized treatment—MBT. The results confirm a positive development for the majority but also that the development of alliance over time is a vulnerable process. In treatments of BPD, the capacity to develop a working alliance suggests a process of gaining epistemic trust and relational competence. As a whole, a positive development of the working alliance was indeed a main trend in the present sample, as were favourable clinical improvements. Correspondingly, positive clinical outcomes were demonstrated in a former study of a smaller MBT sample within the same treatment context but reflecting a shorter study-period (Kvarstein et al., Citation2015). This study did not include measures of alliance, but low early drop-out rates may, nevertheless, be indicative of satisfactory initial bonding.
The MBT manual instructs the therapist to be an attachment figure (Karterud & Bateman, Citation2010), and as BPD patients display substantial attachment issues, these will be central in the further development of a working alliance. The MBT manual emphasizes that this process requires emotional involvement from the therapist (Karterud & Bateman, Citation2010). Self-perception and self-esteem are both aspects of mentalizing that may be developed in a validating and reflective attachment context. Irrespective of outcome, patients in our study reported severe personality problems of both self-aspects. In the present study, the majority of patients achieved a positive process with clinical improvement together with a growing working alliance. However, within this sample, less favourable processes were also evident.
The present results highlight how patients need to understand what psychotherapy is and see how it may work. Differences between outcome subgroups were particularly marked for the subscale Tasks. The specific items indicate confidence in the treatment method, clarity on the therapeutic work being done, and a sense of already noticing personal change. As Bordin (Citation1979) stated, alliance is the ingredient that “ … makes it possible for the patient to accept and follow treatment faithfully” (p. 2). In our study, initial experiences of tasks in MBT did not differ by subgroup, but emerged over time—for most patients, the process was fruitful.
A reasonable question is to what extent poorly mentalizing patients are able to understand how to work in therapy in the best way (Dimaggio et al., Citation2019). This is the main argument for the systematic use of both case formulations and psychoeducation in specialized BPD treatments. Both aim to increase patients’ knowledge about BPD, such as different problems of mentalizing, recognition and regulation of affects, or understanding patterns of relational attachment. The psychoeducation also introduces the treatment programme, what is expected of patients and therapists, and what kinds of things therapists may ask about (Karterud, Citation2011). In qualitative interviews of psychoeducation in MBT, patients reported the importance of feeling understood, often for the first time, and most essentially, experiencing hope for change (Ditlefsen et al., Citation2020). The study also points to negative experiences of feeling too different from other patients in the group. Positive experiences of validation and learning could indicate a strengthening of epistemic trust (Fonagy et al., Citation2015). Mutual agreement on problems and provision of the rationale behind a treatment method is considered crucial for the outcome (Wampold & Imel, Citation2015). In treatment of BPD, emotional dysregulation and high-risk impulsivity are often part of a challenging picture. In the present study, alliance developed despite substantial initial problems of self-control.
For patients with positive developments, it seems they became able to collaborate (Goals and Tasks), and cocreate a trusting relationship (Bonds). A qualitative study of therapist interventions in MBT described how therapists within a good working alliance context not only validated and supported the patient but could also challenge maladaptive patterns (Folmo et al., Citation2019). A positive alliance process could indicate that the patient gradually comes to understand the importance of working on the problems focused in therapy and becomes increasingly willing to be challenged directly on these matters. Therapy then becomes increasingly relevant—permitting work on central personality problems. In a study comparing alliance for BPD patients in SFT and TFP (Spinhoven et al., Citation2007), method-specific factors influenced the quality of the alliance. SFT, with its emphasis on the “necessary and sufficient conditions” in the client-centred approach, produced the better alliance, whereas the first stages of TFP, in which aggressive self- and object representations are activated and interpreted, demanded too much of the early alliance.
Results indicate that the long-term therapy process could also be cumbersome. The capacity for gaining mutual understanding is essential in therapy dyads, group treatments, and human interaction in general. Paranoid PD was characterized by a limited collaborative alliance process. Few have investigated the effect of MBT on other personality disorders (PD) besides BPD (Volkert et al., Citation2019). However, the clinical severity of PD in terms of comorbidity has been investigated. Studies of social cognition among patients with BPD have indicated that more impaired mentalizing is associated with more severe, comorbid PD (Normann-Eide et al., Citation2019), and MBT studies differentiating between patients with only BPD and patients with PD comorbidity recommend MBT for the more complex conditions (Kvarstein et al., Citation2019). BPD with comorbid paranoid PD represents a common form of severe personality pathology and can be conceptualized within the frame of epistemic trust. Counterintuitively, our study did not demonstrate differences in initial alliance or GAF levels related to comorbid paranoid PD. However, paranoid PD was overrepresented in the subgroup with poorer clinical improvement and associated with impeded alliance development over time; it is quite possible that many patient-therapist dyads were unable to handle alliance ruptures adequately. However, the present study also signals the possibility of a positive course. Paranoid PD was not associated with impeded alliance in the good outcome group.
In treatment of severe PD, the alliance process depends on the quality of the dyad between the patient—who, in the case of paranoid features, may be reserved, hostile, or dismissing—and the therapist—who, in such cases, has to keep up engagement and manage countertransference activated by rejection, criticism, or devaluation. It is plausible that adhering to a specific treatment model and strategy, such as MBT, could provide a helpful framework. As advanced in MBT, a genuine and frank style of communication may prevent paranoid phantasies about the therapist’s thoughts or intentions. An empathic, dyadic process of enquiry and reflection may also build confidence. A mentalizing process implies that therapists are reasonably transparent about their own mental states and that patients work on their understanding of self and others. Talented therapists may be more responsive and attentive to ways of facilitating alliance with their patients (Lemma et al., Citation2011; Wampold & Imel, Citation2015). Two studies of psychotherapy alliance recommended a combination of self-doubt as a therapist and self-affiliation as a person (Heinonen & Nissen-Lie, Citation2020; Nissen-Lie et al., Citation2017). In line with such findings, we may speculate that being willing to be transparent (e.g., display self-doubt) whilst having sufficient self-affiliation not to be overwhelmed by countertransferences (feeling devalued, mistrusted, rejected, etc.) is crucial for fostering alliance with patients presenting paranoid PD.
There are many possible pitfalls in such processes. Studies of psychotherapy with relationally disturbed patients have indicated high sensitivity towards therapists’ countertransference reactions or behaviours. Negative therapist feelings of disengagement or inadequacy are associated with poorer outcomes, and therapists’ anxiety or negative reactions may contribute to a poorer working alliance (Dahl et al., Citation2016, Citation2017; Nissen-Lie et al., Citation2015). Moreover, too great a degree of self-confidence or self-concern may not facilitate alliance (Heinonen & Nissen-Lie, Citation2020; Nissen-Lie et al., Citation2010). In order to support therapist competence, MBT recommends transparency, not only within sessions, but including active collaboration with a team of therapists and regular supervision—all to ensure a mentalizing culture on all levels. It is noteworthy that studies have demonstrated that outcomes in MBT for poorly functioning patients depend on overall quality of both therapist competence and treatment organization (Bales, Timman, et al., Citation2017; Bales, Verheul, et al., Citation2017).
Strengths and Limitations
The sample represented a large, clinically representative, and severe BPD population of 155 patients treated in an MBT programme, and the study has a longitudinal design. Few MBT studies include fidelity measures and as such are often neglected in psychotherapy research (Perepletchikova et al., Citation2007). As is often the case in clinical studies, longitudinal data were unbalanced with different numbers of assessments. Assessments were performed during treatment, and one reason for different assessment numbers is different treatment durations. To compensate, assessments at termination were placed at the last 36-month time-point. We chose a maximum likelihood-based statistical method for longitudinal analyses, generating individual curves based on all available data for each patient. Different assessment numbers were not associated with longitudinal deviation, and all reported results remained evident when we investigated possible bias of different assessment numbers. The study included two different versions of WAI, and differently formulated items may have affected the alliance ratings. We present both versions and include investigations controlling for possible impacts of WAI. The limitation is considered minor, as we found little conceptual difference between the two WAI versions. Different WAI versions were not associated with significant longitudinal deviation, and all reported results remained evident when we controlled for different WAI versions. As a study of alliance, it is limited in that it only includes patient ratings. Even though patient- and therapist-rated alliance are equally good predictors of outcome (Flückiger et al., Citation2018), our findings are restricted by the fact that we only study patient-rated alliance. There could be a tendency to both over- and underestimate the alliance based on self-report only (Tryon et al., Citation2008), thus potentially making our results less reliable. Moreover, more frequent measures of alliance would have been a better basis for longitudinal trends and would have compensated for the possible bias of session to session fluctuations. However, the study design was pragmatic, as it investigated an ongoing treatment, and research was based on assessments, which were part of the unit’s regular clinical evaluation routines.
Conclusion
The study demonstrates satisfactory levels of initial working alliance among BPD patients in MBT irrespective of clinical outcomes and an overall increase of all alliance aspects over time. Further investigation revealed that comorbid paranoid PD was more frequent in the subgroup with poor outcomes and associated with poorer alliance development in this subgroup. Differences in alliance development according to outcome were most pronounced for the subscale tasks.
References
- Bales, D. L., Timman, R., Luyten, P., Busschbach, J., Verheul, R., & Hutsebaut, J. (2017). Implementation of evidence-based treatments for borderline personality disorder: The impact of organizational changes on treatment outcome of mentalization-based treatment. Personality and Mental Health, 11(4), 266–277. https://doi.org/10.1002/pmh.1381
- Bales, D. L., Verheul, R., & Hutsebaut, J. (2017). Barriers and facilitators to the implementation of mentalization-based treatment (MBT) for borderline personality disorder. Personality and Mental Health, 11(2), 118–131. https://doi.org/10.1002/pmh.1368
- Bateman, A., & Fonagy, P. (2016). Mentalization-based treatment for personality disorders: A practical guide. Oxford University Press.
- Beck, E., Bo, S., Jørgensen, M. S., Gondan, M., Poulsen, S., Storebø, O. J., Andersen, C. F., Folmo, E., Sharp, C., Pedersen, J., & Simonsen, E. (2020). Mentalization-based treatment in groups for adolescents with borderline personality disorder: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 61(5), 594–604. https://doi.org/10.1111/jcpp.13152
- Bedics, J. D., Atkins, D. C., Harned, M. S., & Linehan, M. M. (2015). The therapeutic alliance as a predictor of outcome in dialectical behavior therapy versus nonbehavioral psychotherapy by experts for borderline personality disorder. Psychotherapy, 52(1), 67–77. https://doi.org/10.1037/a0038457
- Bo, S., Sharp, C., Fonagy, P., & Kongerslev, M. (2017). Hypermentalizing, attachment, and epistemic trust in adolescent BPD: Clinical illustrations. Personality Disorders: Theory, Research, and Treatment, 8(2), 172. https://doi.org/10.1037/per0000161
- Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16(3), 252. https://doi.org/10.1037/h0085885
- Colli, A., Tanzilli, A., Dimaggio, G., & Lingiardi, V. (2014). Patient personality and therapist response: An empirical investigation. American Journal of Psychiatry, 171(1), 102–108. https://doi.org/10.1176/appi.ajp.2013.13020224
- Dahl, H. S. J., Høglend, P., Ulberg, R., Amlo, S., Gabbard, G. O., Perry, J. C., & Christoph, P. C. (2017). Does therapists’ disengaged feelings influence the effect of transference work? A study on countertransference. Clinical Psychology & Psychotherapy, 24(2), 462–474. https://doi.org/10.1002/cpp.2015
- Dahl, H.-S. J., Ulberg, R., Friis, S., Perry, J. C., & Høglend, P. A. (2016). Therapists’ inadequate feelings and long-term effect of transference work. Psychotherapy and Psychosomatics, 85(5), 309–310. https://doi.org/10.1159/000444647
- Derogatis, L. (2000). The brief symptom inventory-18 (BSI-18): Administration. Scoring, and procedures manual (3rd ed.). National Computer Systems.
- Dimaggio, G., Maillard, P., MacBeth, A., & Kramer, U. (2019). Effects of therapeutic alliance and metacognition on outcome in a brief psychological treatment for borderline personality disorder. Psychiatry, 82(2), 143–157. https://doi.org/10.1080/00332747.2019.1610295
- Ditlefsen, I. T., Nissen-Lie, H., Andenæs, A., Normann-Eide, E., Johansen, M. S., & Kvarstein, E. H. (2020). “Yes, there is actually hope!”– A qualitative investigation of how patients experience mentalization-based psychoeducation tailored for borderline personality disorder. Manuscript submitted for publication.
- Dyson, H., & Brown, D. (2016). The experience of mentalization-based treatment: An interpretative phenomenological study. Issues in Mental Health Nursing, 37(8), 586–595. https://doi.org/10.3109/01612840.2016.1155246
- Euler, S., Wrege, J., Busmann, M., Lindenmeyer, H. J., Sollberger, D., Lang, U. E., Gaab, J., & Walter, M. (2018). Exclusion-proneness in borderline personality disorder inpatients impairs alliance in mentalization-based group therapy. Frontiers in Psychology, 9, 824. https://doi.org/10.3389/fpsyg.2018.00824
- Falkenström, F., & Larsson, M. H. (2017). The working alliance: From global outcome prediction to micro-analyses of within-session fluctuations. Psychoanalytic Inquiry, 37(3), 167–178. https://doi.org/10.1080/07351690.2017.1285186
- First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. (1994). Structured clinical interview for Axis I DSM-IV disorders. Biometrics Research.
- Flückiger, C., Del Re, A., Wampold, B. E., & Horvath, A. O. (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy, 55(4), 316. https://doi.org/10.1037/pst0000172
- Folmo, E. J., Karterud, S. W., Bremer, K., Walther, K. L., Kvarstein, E. H., & Pedersen, G. A. (2017). The design of the MBT-G adherence and quality scale. Scandinavian Journal of Psychology, 58(4), 341–349. https://doi.org/10.1111/sjop.12375
- Folmo, E., Karterud, S., Kongerslev, M., Kvarstein, E., & Stänicke, E. (2019). Battles of the comfort zone: Modelling therapeutic strategy, alliance, and epistemic trust—a qualitative study of mentalization-based therapy for borderline personality disorder. Journal of Contemporary Psychotherapy, 49(3), 141–151. https://doi.org/10.1007/s10879-018-09414-3
- Fonagy, P., Gergely, G., Target, M., & Jurist, E. L. (2002). Affect regulation, mentalization, and the development of the self. Other Press, LLC.
- Fonagy, P., Luyten, P., & Bateman, A. (2015). Translation: Mentalizing as treatment target in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 6(4), 380–392. https://doi.org/10.1037/per0000113
- Gardner, K. J., Wright, K. M., Elliott, A., Graham, S., & Fonagy, P. (2020). The weirdness of having a bunch of other minds like yours in the room: The lived experiences of mentalization-based therapy for borderline personality disorder. Psychology and Psychotherapy: Theory, Research and Practice, 93(3), 572–586. https://doi.org/10.1111/papt.12243
- Harpøth, T. S., Kongerslev, M. T., Moeyaert, M., Bo, S., Bateman, A. W., & Simonsen, E. (2019). Evaluating “mentalizing positive affect” as an intervention for enhancing positive affectivity in borderline personality disorder using a single-case multiple-baseline design. Psychotherapy. https://doi.org/10.1037/pst0000251
- Hatcher, R. L., & Gillaspy, J. A. (2006). Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research, 16(1), 12–25. https://doi.org/10.1080/10503300500352500
- Hedeker, D., & Gibbons, R. D. (1997). Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods, 2(1), 64–78. https://doi.org/10.1037/1082-989X.2.1.64
- Heinonen, E., & Nissen-Lie, H. A. (2020). The professional and personal characteristics of effective psychotherapists: A systematic review. Psychotherapy Research, 30(4), 417–432. https://doi.org/10.1080/10503307.2019.1620366
- Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the working alliance inventory. Journal of Counseling Psychology, 36(2), 223. https://doi.org/10.1037/0022-0167.36.2.223
- Johnson, E. L., Mutti, M.-F., Springham, N., & Xenophontes, I. (2016). Mentalizing after mentalization based treatment. Mental Health and Social Inclusion, 20(1), 44–51. https://doi.org/10.1108/MHSI-11-2015-0042
- Karterud, S. (2011). Manual for mentaliseringsbasert psykoedukativ gruppeterapi (MBT-I). Gyldendal akademisk.
- Karterud, S. (2012). Manual for mentaliseringsbasert gruppeterapi (MBT-G). Gyldendal akademisk.
- Karterud, S. (2015). Mentalization-based group therapy (MBT-G): A theoretical, clinical, and research manual. OUP.
- Karterud, S., & Bateman, A. (2010). Manual for mentaliseringsbasert terapi (MBT) og MBT vurderingsskala. Versjon individualterapi. Gyldendal akademisk.
- Karterud, S., Folmo, E., & Kongerslev, M. (2020). Mentaliseringsbasert terapi MBT. Gyldendal Akademisk.
- Karterud, S., Pedersen, G., Engen, M., Johansen, M. S., Johansson, P. N., Schlüter, C., Urnes, O., Wilberg, T., & Bateman, A. W. (2013). The MBT adherence and competence scale (MBT-ACS): Development, structure and reliability. Psychotherapy Research, 23(6), 705–717. https://doi.org/10.1080/10503307.2012.708795
- Kvarstein, E. H., Folmo, E., Antonsen, B. T., Normann-Eide, E., Pedersen, G., & Wilberg, T. (2020). Social cognition capacities as predictors of outcome in mentalization-based treatment (MBT). Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00691
- Kvarstein, E. H., Pedersen, G., Folmo, E., Urnes, Ø, Johansen, M. S., Hummelen, B., Wilberg, T., & Karterud, S. (2019). Mentalization-based treatment or psychodynamic treatment programmes for patients with borderline personality disorder–the impact of clinical severity. Psychology and Psychotherapy: Theory, Research and Practice, 92(1), 91–111. https://doi.org/10.1111/papt.12179
- Kvarstein, E. H., Pedersen, G., Urnes, Ø, Hummelen, B., Wilberg, T., & Karterud, S. (2015). Changing from a traditional psychodynamic treatment programme to mentalization-based treatment for patients with borderline personality disorder–does it make a difference? Psychology and Psychotherapy: Theory, Research and Practice, 88(1), 71–86. https://doi.org/10.1111/papt.12036
- Lemma, A., Target, M., & Fonagy, P. (2011). Brief dynamic interpersonal therapy: A clinician’s guide. Oxford University Press.
- Lonargáin, DÓ, Hodge, S., & Line, R. (2017). Service user experiences of mentalisation-based treatment for borderline personality disorder. The Mental Health Review, 22(1), 16–27. https://doi.org/10.1108/MHRJ-04-2016-0008
- Möller, C., Karlgren, L., Sandell, A., Falkenström, F., & Philips, B. (2017). Mentalization-based therapy adherence and competence stimulates in-session mentalization in psychotherapy for borderline personality disorder with co-morbid substance dependence. Psychotherapy Research, 27(6), 749–765. https://doi.org/10.1080/10503307.2016.1158433
- Morken, K. T. E., Binder, P.-E., Arefjord, N. M., & Karterud, S. W. (2019). Mentalization-based treatment from the patients’ perspective–what ingredients do they emphasize? Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.01327
- Mundt, J. C., Marks, I. M., Shear, M. K., & Greist, J. M. (2002). The work and social adjustment scale: A simple measure of impairment in functioning. The British Journal of Psychiatry, 180(5), 461–464. https://doi.org/10.1192/bjp.180.5.461
- Muran, J. C., & Barber, J. P. (2011). In J. C. Muran & J. P. Barber (Eds.), The therapeutic alliance: An evidence-based approach to practice and training (pp. 44–62). New York, NY: Guilford Press.
- Nissen-Lie, H. A., Havik, O. E., Høglend, P. A., Rønnestad, M. H., & Monsen, J. T. (2015). Patient and therapist perspectives on alliance development: Therapists’ practice experiences as predictors. Clinical Psychology & Psychotherapy, 22(4), 317–327. https://doi.org/10.1002/cpp.1891
- Nissen-Lie, H. A., Monsen, J. T., & Rønnestad, M. H. (2010). Therapist predictors of early patient-rated working alliance: A multilevel approach. Psychotherapy Research, 20(6), 627–646. https://doi.org/10.1080/10503307.2010.497633
- Nissen-Lie, H. A., Rønnestad, M. H., Høglend, P. A., Havik, O. E., Solbakken, O. A., Stiles, T. C., & Monsen, J. T. (2017). Love yourself as a person, doubt yourself as a therapist? Clinical Psychology & Psychotherapy, 24(1), 48–60. https://doi.org/10.1002/cpp.1977
- Normann-Eide, E., Antonsen, B. R. T., Kvarstein, E. H., Pedersen, G., Vaskinn, A., & Wilberg, T. (2019). Are impairments in theory of mind specific to borderline personality disorder? Journal of Personality Disorders, 1–15. https://doi.org/10.1521/pedi_2019_33_417
- Ollila, P., Knekt, P., Heinonen, E., & Lindfors, O. (2016). Patients’ pre-treatment interpersonal problems as predictors of therapeutic alliance in long-term psychodynamic psychotherapy. Psychiatry Research, 241, 110–117. https://doi.org/10.1016/j.psychres.2016.04.093
- Pedersen, G., Arnevik, E. A., Hummelen, B., Walderhaug, E., & Wilberg, T. (2017). Psychometric properties of the severity indices of personality problems (SIPP) in two samples. European Journal of Psychological Assessment, 35. https://doi.org/10.1027/1015-5759/a000436
- Pedersen, G., Hagtvet, K. A., & Karterud, S. (2007). Generalizability studies of the global assessment of functioning–split version. Comprehensive Psychiatry, 48(1), 88–94. https://doi.org/10.1016/j.comppsych.2006.03.008
- Pedersen, G., & Karterud, S. (2004). Is SCL-90R helpful for the clinician in assessing DSM-IV symptom disorders? Acta Psychiatrica Scandinavica, 110(3), 215–224. https://doi.org/10.1111/j.1600-0447.2004.00321.x
- Pedersen, G., Karterud, S., Hummelen, B., & Wilberg, T. (2013). The impact of extended longitudinal observation on the assessment of personality disorders. Personality and Mental Health, 7(4), 277–287. https://doi.org/10.1002/pmh.1234
- Pedersen, G., Kvarstein, E., & Wilberg, T. (2017). The work and social adjustment scale: Psychometric properties and validity among males and females, and outpatients with and without personality disorders. Personality and Mental Health, 11(4), 215–228. https://doi.org/10.1002/pmh.1382
- Pedersen, G., Urnes, Ø, Hummelen, B., Wilberg, T., & Kvarstein, E. (2018). Revised manual for the global assessment of functioning scale. European Psychiatry, 51, 16–19. https://doi.org/10.1016/j.eurpsy.2017.12.028
- Perepletchikova, F., Treat, T. A., & Kazdin, A. E. (2007). Treatment integrity in psychotherapy research: Analysis of the studies and examination of the associated factors. Journal of Consulting and Clinical Psychology, 75(6), 829–841. https://doi.org/10.1037/0022-006X.75.6.829
- Rossi, G., Debast, I., & Van Alphen, S. (2017). Measuring personality functioning in older adults: Construct validity of the severity indices of personality functioning–short form (SIPP-SF). Aging & Mental Health, 21(7), 703–711. https://doi.org/10.1080/13607863.2016.1154012
- Saarni, S. I., Suvisaari, J., Sintonen, H., Koskinen, S., Härkänen, T., & Lönnqvist, J. (2007). The health-related quality-of-life impact of chronic conditions varied with age in general population. Journal of Clinical Epidemiology, 60(12), 1288. e1281–e1288. e1211. https://doi.org/10.1016/j.jclinepi.2007.03.004
- Safran, J. D., & Muran, J. C. (2000). Resolving therapeutic alliance ruptures: Diversity and integration. Journal of Clinical Psychology, 56(2), 233–243. https://doi.org/10.1002/(SICI)1097-4679(200002)56:2<233::AID-JCLP9>3.0.CO;2-3
- Sharp, C. (2014). The social–cognitive basis of BPD: A theory of hypermentalizing. In C. Sharp & J. L. Tackett (Eds.), Handbook of borderline personality disorder in children and adolescents (Vol. 1, pp. 211–225). New York: Springer. https://doi-org.ezproxy.uio.no/10.1007/978-1-4939-0591-1_15
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., & Dunbar, G. C. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20 (22–33)).
- Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford university press.
- Skodol, A. E., Shea, M. T., Yen, S., White, C. N., & Gunderson, J. G. (2010). Personality disorders and mood disorders: Perspectives on diagnosis and classification from studies of longitudinal course and familial associations. Journal of Personality Disorders, 24(1), 83–108. https://doi.org/10.1521/pedi.2010.24.1.83
- Soeteman, D. I., Verheul, R., & Busschbach, J. J. (2008). The burden of disease in personality disorders: Diagnosis-specific quality of life. Journal of Personality Disorders, 22(3), 259–268. https://doi.org/10.1521/pedi.2008.22.3.259
- Spinhoven, P., Giesen-Bloo, J., van Dyck, R., Kooiman, K., & Arntz, A. (2007). The therapeutic alliance in schema-focused therapy and transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 75(1), 104. https://doi.org/10.1037/0022-006X.75.1.104
- Stiles, W. B., & Goldsmith, J. Z. (2010). The alliance over time. The Therapeutic Alliance: An Evidence-Based Guide to Practice, 44–62.
- Tracey, T. J., & Kokotovic, A. M. (1989). Factor structure of the working alliance inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1(3), 207–210. https://doi.org/10.1037/1040-3590.1.3.207
- Tryon, G. S., Blackwell, S. C., & Hammel, E. F. (2008). The magnitude of client and therapist working alliance ratings. Psychotherapy: Theory, Research, Practice, Training, 45(4), 546. https://doi.org/10.1037/a0014338
- Vaskinn, A., Antonsen, B. T., Fretland, R. A., Dziobek, I., Sundet, K., & Wilberg, T. (2015). Theory of mind in women with borderline personality disorder or schizophrenia: Differences in overall ability and error patterns. Frontiers in Psychology, 6, 1239. https://doi.org/10.3389/fpsyg.2015.01239
- Volkert, J., Hauschild, S., & Taubner, S. (2019). Mentalization-based treatment for personality disorders: Efficacy, effectiveness, and new developments. Current Psychiatry Reports, 21(4), 25. https://doi.org/10.1007/s11920-019-1012-5
- Wampold, B. E., & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work. Routledge.
- Young, J. E., Klosko, J. S., & Weishaar, M. E. (2006). Schema therapy: A practitioner’s guide. Guilford Press.