?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective:
Understanding psychological mechanisms of change is essential to advance treatments for patients suffering from medically unexplained physical symptoms (MUPS). This study aimed to test the role of selected change mechanisms (incl. interoceptive awareness, emotional regulation skills, symptom acceptance, relational needs satisfaction, clarification of meaning, working alliance, and group cohesion) in the modification of patients’ somatic symptom intensity and well-being.
Method:
N = 290 patients suffering from MUPS participated in a multi-component group-based treatment at seven clinical sites. Data were collected weekly. Multi-level modeling was used to test cross-lagged relationships between the hypothesized mechanisms and outcomes in terms of Granger causality (with lags of 1, 2, and 3 weeks).
Results:
None of the mechanisms predicted a time-lagged change in outcomes in the expected direction. In fact, there was a consistent pattern of negative time-lagged relationships (i.e., an increase in a mechanism predicted worsening of the outcome). Findings consistent with the hypothesized role of the mechanisms were found only in concurrent relationships between mechanisms and outcomes.
Conclusion:
This study did not support time-lagged relationships under the condition of weekly measurement and many methodological factors remain to be considered (e.g., a finer time resolution).
Clinical or methodological significance of this article: This study failed to find predicted cross-lagged relationships between hypothesized change mechanisms and outcomes. Meaningful relationships were found only within the same window of measurement (i.e., within the same week). A more nuanced time resolution may be necessary to understand the dynamics of the therapeutic changes in patients suffering from medically unexplained physical symptoms.
Medically unexplained physical symptoms (MUPS) can be defined as the presence of at least one somatic symptom not fully explained by a somatic or psychiatric disorder with a duration of at least six months (Kroenke, Citation2006). The term covers various functional somatic syndromes, such as chronic fatigue syndrome, irritable bowel syndrome, and fibromyalgia. In the classifications of mental disorders, unexplained symptom complaints are usually framed as somatoform disorders (American Psychiatric Association, Citation2000; World Health Organization, Citation2008). Recently, however, there has been a shift towards more descriptive terms, such as somatic symptom disorder (American Psychiatric Association, Citation2013) and bodily distress disorder (Gureje & Reed, Citation2016), that aim to overcome the body–mind dichotomy. While the presented somatic complaints may vary considerably, several authors have argued that these patients tend to share many characteristics and, therefore, they can be meaningfully treated as a single group (Lacourt et al., Citation2013; Nimnuan et al., Citation2001; Wessely et al., Citation1999). In this study, we have accepted this inclusive view. We use the term MUPS as an overarching category because of its wide use and aetiological neutrality.
Unexplained somatic suffering represents a challenge in treatment. Although several studies have suggested that psychotherapy is at least as effective as pharmacotherapy (Nüesch et al., Citation2013; Perrot & Russell, Citation2014) and other forms of treatment (Chambers et al., Citation2006) for patients with MUPS, meta-analyses of randomized trials revealed only small to medium effects of nonpharmacological treatments (Kleinstäuber et al., Citation2011; Lakhan & Schofield, Citation2013; van Dessel et al., Citation2014). This contrasts with considerably higher effects found in psychotherapy of other mental disorders (Lambert, Citation2013). Nevertheless, some studies in the context of MUPS have indicated that higher psychotherapeutic effects may be achieved with longer treatment duration and by more complex approaches (Glombiewski et al., Citation2010); thus, the full potential of psychotherapy for patients with MUPS remains unexplored.
This present study was focused on intensive, multi-component psychological treatment based on group psychotherapy provided on a daily basis. While several studies have demonstrated the effectiveness of multi-component treatments and group psychotherapy for patients with MUPS (e.g., Kashner et al., Citation1995; Lidbeck, Citation1997, Citation2003; Moreno et al., Citation2013; Selders et al., Citation2015; Yoshino et al., Citation2015), none of them investigated psychological change mechanisms behind the treatments.
To advance the development of an effective psychological treatment for patients with MUPS, we need to better understand the change mechanisms that operate within the treatment. Unfortunately, the empirical literature on change mechanisms in psychological treatments for MUPS is scarce and largely inconclusive. The most consistent support exists for increasing symptom acceptance and the development of coping strategies (Pourová, Klocek, et al., Citation2020). However, several hypothesized mechanisms that seem to be widely accepted across theoretical orientations have not yet been empirically tested as change mechanisms. These include mainly interoceptive awareness, emotional regulation skills, satisfaction of relational needs, clarification of symptom meaning, working alliance and group cohesion (Řiháček & Čevelíček, Citation2020).
Selected Mechanisms of Change
Somatization tends to be connected with difficulties in interoceptive awareness and the ability to interpret bodily signals (Schaefer et al., Citation2012). Interventions aimed at increasing the ability to attend to one’s body in an accepting and explorative manner are believed to lead to the reinvestment of the body with positive meanings (Luyten et al., Citation2012). Although the effect of relaxation training alone tends to be small or inconclusive (Meeus et al., Citation2015), body-awareness interventions have shown small to moderate effects for MUPS reduction (Courtois et al., Citation2015).
Patients suffering from MUPS often have difficulties in emotional processing and tend to misinterpret bodily manifestations of emotions as illness symptoms (De Gucht & Heiser, Citation2003). Therefore, various therapeutic interventions are focused on the development or restoration of emotional regulation skills (Payne & Brooks, Citation2017). Indeed, a link was found between emotional regulation and symptom reduction (Godfrey et al., Citation2007) and between emotional regulation and symptom adjustment (Agar-Wilson & Jackson, Citation2012).
Since MUPS themselves are difficult to control, many interventions aim to increase patients’ quality of life by helping them accept the existence of their symptoms and regain the ability to act despite the presence of symptoms (Surawy et al., Citation2015). In several studies, symptom acceptance mediated improvement in functioning, though not the symptom itself (Åkerblom et al., Citation2015; Hesser et al., Citation2014).
Social factors play an important role in the genesis and maintenance of MUPS, and somatic symptoms are sometimes regarded as an indicator of dysfunctions in patients’ interpersonal relationships (Luyten & van Houdenhove, Citation2013; Nezu et al., Citation2001). Hence, we may expect that the improvement in the satisfaction of patients’ relational needs contributes to symptom changes. Nonetheless, this aspect of MUPS has received only marginal attention in research. Some evidence has been found that perceived social support mediates symptom changes (Åkerblom et al., Citation2015). However, in another study, a decrease in interpersonal problems was found to be a consequence, rather than a mechanism, of symptom changes (Hyphantis et al., Citation2009).
Patients’ responses to their symptoms are based on the meaning that the patients attribute to them (Bullington, Citation2013; Salkovskis et al., Citation2016). The correction of dysfunctional beliefs about symptoms has been shown to be a mediator of change (Chow et al., Citation2018; Harvey et al., Citation2017). However, a broader process of clarifying symptom meaning has not been studied in patients with MUPS specifically but is predictive of outcomes in a more general sample (Mander et al., Citation2014).
Establishing an atmosphere of trust and collaboration, setting realistic goals, and providing a sense of validation are aspects of the working alliance that have been emphasized in the treatment of patients with MUPS (Řiháček & Čevelíček, Citation2020). Although the working alliance has long been recognized as a robust predictor of outcome in psychotherapy (Horvath et al., Citation2011), there is surprisingly little evidence in the context of MUPS. While the working alliance predicted outcomes in Heins, Knoop, and Bleijenberg (Citation2013), it did not predict outcomes in Trockel et al. (Citation2014) after controlling for adherence.
Group cohesion has been confirmed as an important predictor of outcomes in group psychotherapy (Burlingame et al., Citation2011). Although we found no evidence for this mechanism in the context of MUPS in the available literature, we assume group cohesion to be a common mechanism of change irrespective of the type of patient complaints.
Testing Change Mechanisms
Conceptually, change mechanisms can be defined as processes or events responsible for a psychotherapeutic change, i.e., the causal agents of change (Kazdin, Citation2007). As such, they must explain, at least partially, the relationship between the treatment and outcome. Since this study is based on data from an uncontrolled observational study, claims about causality could not be based on experimental manipulation with the hypothesized mechanisms in our case. Instead, we followed the logic of Granger causality testing (Granger, Citation1969; Tschacher & Ramseyer, Citation2009) and hypothesized that a change in a mechanism must precede a change in outcome (but not the other way around) to be regarded a plausible mechanism. The question whether both the outcome and the mechanism are causally related to the treatment, cannot be directly addressed in this study but can be approximated by examining the relationship between the outcome and the mechanism, on the one hand, and the treatment dose, on the other. On the operational level, a mechanism will receive empirical support in our study if (i) the dose of therapy predicts the amount of change in the outcome, (ii) the dose of therapy predicts the amount of change in the mechanism, and (iii) the change in the mechanism in week X-1 predicts the change in outcome in week X, but (iv) not the other way around.
This methodological approach also allows us to test an alternative connection between the hypothesized mechanisms and outcomes, which we refer to as reverse hypotheses in the following text. Traditionally, patients’ deficits in areas such as emotion regulation and body awareness have been considered the causes of somatic complaints. However, some authors (e.g., Luyten et al., Citation2012; Speckens et al., Citation1996) have argued that these deficits are consequences rather than antecedents of MUPS. From this point of view, MUPS represent an “attack” on patients’ psychological capacities, and these capacities are restored once somatic suffering subsides. Empirically, if the change in the outcome precedes the change in the mechanism (and not the other way around), this would be considered evidence for the reverse hypothesis.
Aim of the Study
The study aimed to test the seven change mechanisms outlined above using a sample of adult patients suffering from MUPS who underwent multi-component treatment provided on a daily basis with group psychotherapy as the main component. Multi-level modeling was used to test the four abovementioned Granger causality conditions for each hypothesized mechanism. Since the mechanisms may exhibit different relationships with different outcomes, we tested them with two outcome variables, namely, somatic symptom intensity (primary outcome) and well-being (as operationalized by the Outcome Rating Scale, Miller et al., Citation2003). The time lag of one week (i.e., lag-1) was used to test the hypotheses. This duration represents a period in which a meaningful change can be expected to occur, and it also corresponded to the frequency of data collection. However, it is possible that the real time lag between changes in a mechanism and an outcome is longer than one week because psychological changes may need to be consolidated and integrated in patients’ daily lives before they produce any discernible impact on an individual’s somatic symptoms or well-being (Falkenström et al., Citation2020). Therefore, for exploratory purposes, we conducted the same analysis with two- and three-week time lags. On the other hand, it is also possible that the real time lag is shorter than one week (Bloot et al., Citation2015; Kyron et al., Citation2018). In such cases, the weekly interval of measurement would represent a time resolution that is too coarse to capture the dynamics of therapeutic change. To explore this possibility, we tested the concurrent relationships between the change in the mechanism and outcome variables (i.e., variables measured in the same week). Although such an analysis does not allow us to draw definite conclusions about the direction of causality, it may still reveal the existence of relationships worth of further examination. This study complements another study in which we analysed the effectiveness of the treatment (Pourová et al., Citation2021).
Method
Patients
A total of N = 290 adult patients suffering from MUPS (75.3% women) participated in the study. Their age ranged from 19 to 74 years (M = 40.6 years, SD = 11.1 years; ). In terms of the ICD-10 diagnosis, most of the patients were classified under an F4-range diagnosis (75.9%). Almost 9% of the patients received multiple diagnoses. The most often reported somatic symptoms included feeling tired or having low energy (93.8%), trouble sleeping (86.6%), back pain (82.8%), headaches (79.0%), nausea, gas, or indigestion (77.2%), pain in arms, legs, or joints (71.7%), feeling one’s heart pound or race (70.7%), constipation, loose bowels or diarrhoea (67.6%), and stomach pain (60.7%).
Table I. Sample characteristics.
Treatment
The treatment was comparable across the seven sites with some degree of variation. The treatment length varied between four and twelve weeks, with the most common length being six weeks. At five sites, patients participated in five sessions of face-to-face group psychotherapy per week, while at two sites, they participated in either three or four sessions, depending on the site. Typically, a session lasted 90 min (except for one site, where sessions lasted 75 min). At three sites, the groups had rolling admission structure (i.e., new patients were incorporated as they were accepted into treatment programs), while they had fixed membership at another three sites (i.e., their composition did not change during treatment, except for dropouts). At the remaining site, both formats were used in different groups. Altogether, there were 79 groups (57% with fixed membership), with a median of 6 patients (range 1 to 12) participating in the study (the total number of patients per group was higher, since some patients chose not to participate in the study). Treatment was mostly psychodynamic, with the integration of humanistic and experiential approaches. Since not all patients participating in the therapeutic groups suffered from MUPS, treatment was not exclusively focused on somatic symptoms. The median proportion of participating patients suffering from MUPS was 50% (range 0% to 80%).
Group psychotherapy was supplemented with art therapy (6 sites), therapeutic community meetings (5 sites), relaxation training (5 sites), movement therapy (3 sites), music therapy (3 sites), thematic groups (3 sites), ergotherapy (2 sites), bibliotherapy (1 site), drama therapy (1 site), physiotherapy (1 site), cognitive training (1 site), and consultations with a social worker (1 site). The time allocation of these supplementary activities varied between 3 and 23.5 h per week (Mdn = 11.38; participation of the individual participants was not documented). At three sites, patients attended day-care-based outpatient programs (inpatient programs at the other four sites).
Therapists
Group therapy was performed by 16 female and 9 male therapists. The age of the therapists ranged from 25 to 59 years (M = 44.13, SD = 10.29), and their length of practice varied between 1 and 25 years (M = 12.21, SD = 7.30). Psychotherapists’ theoretical orientations included psychoanalysis and psychoanalytic psychotherapy (n = 9), psychodynamic psychotherapy (n = 6), gestalt therapy (n = 4), a person-centered approach (n = 3), daseinsanalysis (n = 1), and integrative psychotherapy (n = 2).
Measures
Outcome variables
Patient Health Questionnaire-15-modified (PHQ-15-M)
Somatic symptom intensity was measured by a self-report questionnaire derived from the Patient Health Questionnaire-15 (PHQ-15; Kroenke et al., Citation2002). The PHQ-15 is a 15-item self-report measure developed to assess somatization. Each item represents a somatic symptom or symptom cluster. Using a Likert-type scale, patients are to rate the degree to which they have been bothered by each of the symptoms over a specified period. The PHQ-15 has shown good concurrent validity with the Short-Form General Health Survey (Kroenke et al., Citation2002). In our study, the measure used had two modifications. First, patients were asked to rate the intensity of their symptoms over the last week (instead of over four weeks, as is the case in the original version) to allow for weekly measurements. Second, a five-level scale ranging from “not at all” to “very severe” (instead of the three-level scale used in the original version) was used to rate the items to offer a response scale that is potentially more sensitive to change. The symptom intensity score was computed as the average of all items. In this study, the Cronbach's α at baseline was α = .81.
Within the pre-therapy assessment, patients were also asked three questions about each item: (1) Was the symptom one of the main reasons why you sought therapy? (2) Has the symptom been present for more than six months? (3) Was your physician unable to find a cause of this symptom? Patients’ responses to these questions were used to classify patients into either the MUPS or non-MUPS group (see the Procedure section).
Outcome Rating Scale (ORS)
The ORS (Miller et al., Citation2003) is a brief evaluation of psychotherapy outcomes and is particularly suited for repeated assessment. On four items, patients rated their individual, relational, and social well-being. The total score is computed as the sum of the item ratings and falls within the range of 0 to 400; the higher the score is, the better a patient feels. The ORS has shown good concurrent validity with the Outcome Questionnaire-45.2 and high sensitivity to change (Miller et al., Citation2003). In this study, the Cronbach's α at baseline was α = .82.
Mechanism variables
Multidimensional Assessment of Interoceptive Awareness (MAIA)
The MAIA (Mehling et al., Citation2012) is a 32-item self-report measure of various aspects of interoceptive awareness, including awareness of body sensations, quality of attention towards these sensations, attitude towards the sensations, and mind–body integration. Patients rated each item on a six-point Likert-type scale ranging from “never” to “always”. Previous work supported the measure’s factor structure and convergent validity with established measures of related constructs (Mehling et al., Citation2012). The total score's Cronbach's α at baseline was α = .87.
Emotional Regulation Skills Questionnaire (ERSQ)
The ERSQ (Berking & Znoj, Citation2008) is a 27-item self-report measure of patients’ emotional regulation skills. Patients rated each item on a five-point Likert-type scale ranging from “not at all” to “almost always”. This questionnaire is composed of nine subscales that measure aspects such as attention towards, regulation of and acceptance of, and understanding one’s emotions. Previously, the measure’s factor structure, convergent validity with other measures of emotion processing skills/deficits, and sensitivity to change has been supported (Berking & Znoj, Citation2008). The total score's Cronbach's α at baseline was α = .91.
Relational Needs Satisfaction Scale (RNSS)
The RNSS (Pourová, Řiháček, et al., Citation2020) is a 20-item self-report measure of the satisfaction of five relational needs (i.e., the need for authenticity, the need for protection, the need to have an impact, the need to have a shared experience, and the need to perceive initiative from others). Patients rated each item on a five-point Likert-type scale ranging from “never true” to “always true”. The measure’s factor structure and convergent validity with measures of related constructs has been supported (Pourová, Řiháček, et al., Citation2020). The total score's Cronbach's α at baseline was α = .87.
Chronic Pain Acceptance Questionnaire-modified (CPAQ-M)
To measure the level of patients’ acceptance of their problems that led them to psychotherapy, we used the Chronic Pain Acceptance Questionnaire (CPAQ, McCracken et al., Citation2004). It is a 20-item self-report measure of patients’ attitudes towards their chronic pain. The questionnaire consists of two subscales, namely, activity engagement and symptom willingness. Previously, the two-factor structure and convergent validity with other measures of human functioning has been established (McCracken et al., Citation2004). Since patients in our sample also suffered from symptoms other than chronic pain, we replaced the words “chronic pain” with “my symptoms”. Since the internal consistency of the total score was problematic (α = .58), we used the two subscales separately. The Cronbach's α coefficients for the two subscales at baseline were α = .80 and α = .66.
Scale for the Multi-perspective Assessment of General Change Mechanisms in Psychotherapy (SACiP)
The SACiP (Mander et al., Citation2013) is a 21-item self-report scale developed for the measurement of general psychotherapeutic mechanisms. The scale is composed of six subscales (problem actuation, resource activation, clarification of meaning, mastery, emotional bond, and agreement on collaboration) and could be administered after each session. Each item is rated on a five-point Likert-type scale ranging from “doesn’t fit at all” to “fits exactly”. The SACiP was found to be predictive of outcome, especially when rated by patients (Mander et al., Citation2013). In our study, a hypothesis was made about the clarification of meaning subscale only (three items). However, the problem actuation, resource activation, and mastery subscales were included for exploratory purposes as well (the results are reported in the Supplementary Materials). Two necessary modifications were made to the scale. First, the instructions were reframed to refer to all sessions over the past week, not just the last session. Second, items were reworded to explicitly refer to group psychotherapy sessions. The internal consistency was α = .76 for clarification of meaning, α = .64 for problem actuation, α = .71 for resource activation, and α = .79 for mastery.
Group Session Rating Scale (GSRS)
The GSRS (Quirk et al., Citation2013) is a brief measure of the working alliance in group psychotherapy. It is composed of four visual analogue scales that allow patients to rate their perception of emotional bond, goal consensus, and task consensus, as well as their overall perception of the working alliance. The total score is computed as the sum of the item ratings and falls within the range of 0 to 400. The GSRS has shown convergent validity with the Working Alliance Inventory and predicted psychotherapy outcome (Quirk et al., Citation2013). The score's Cronbach's α at baseline was α = .81.
Group Cohesiveness Scale (GCS)
The GCS (Wongpakaran et al., Citation2013) is a unidimensional 7-item measure of group cohesion. Items include statements about patients’ sense of acceptance, trust, and group participation and are rated on a five-point Likert-type scale ranging from “strongly disagree” to “strongly agree”. The measure’s factorial and convergent validity with other measures of group climate have been supported (Wongpakaran et al., Citation2013). The total mean's Cronbach's α at baseline was α = .88.
Demographic questionnaire
A questionnaire was administered to collect patients’ demographic data, including their gender, age, cohabitation status, marital status, employment, nationality, and education.
Procedure
Recruitment and data collection
The study was approved by the Research Ethics Committee of Masaryk University (ref. no. EKV-2017-029-R1). Patients were recruited at seven psychotherapeutic clinics by the local staff during 2018 and 2019. All patients who underwent treatment were invited to participate in the study. In case the patients agreed to participate in the study, the following battery of measures were administered to them at baseline: the PHQ-15-M, ORS, MAIA, ERSQ, CPAQ-M, and RNSS. The same battery, complemented with the SACiP, GSRS, and GCS, was then administered on a weekly basis. Patients were instructed to answer the process measures with respect to the past week of psychotherapy. The data were collected in paper-and-pencil form.
The MUPS vs. non-MUPS status of each patient was determined based on the following procedure. All patients who were diagnosed by their local clinical staff with a somatoform disorder (F45 according to World Health Organization, Citation2008) were considered to have MUPS (n = 82). In the remaining patients, the status was determined based on a triangulation of patients’ self-report data and data obtained from the local clinical staff. Patients who marked at least one somatic symptom in the PHQ-15-modified as “lasting for at least six months” and, at the same time, as “one of the main reasons for seeking psychotherapy” were provisionally classified as “self-identified MUPS”. Patients who were found to conform to Kroenke’s (Citation2006) definition of MUPS according to the local clinical staff were provisionally classified as having “site-identified MUPS”. When two classifications agreed with each other, patients were placed in the MUPS group (n = 47). In cases of a conflict between the two classifications, the patient’s records were reviewed by two physicians (a psychiatrist and a general practitioner) who were not familiar with any of the patients’ process and outcome data to determine the patient’s MUPS status (this resulted in n = 161 additional patients being placed into the MUPS group).
Statistical analysis
To minimize transcription errors, all data were transcribed into an Excel sheet by two independent coders, and automated checking was performed to find any mismatch and consolidate the transcription. Totals for each instrument were computed if a patient answered at least 80% of the instrument’s items; otherwise, the patient’s response was considered missing data. The analysis was conducted using R (4.1.0; R Core Team, Citation2021). For each hypothesized mechanism, the four conditions (see Introduction) were tested using multi-level modeling (lme4; Bates et al., Citation2015) with measurements nested within patients (Singer & Willett, Citation2003).
Before introducing the statistical models, we must distinguish between two types of mechanism variables we used in our study. Process-type mechanisms are variables that represent patients’ perception of the therapy within a particular week. They have no pre-treatment value and the week-by-week change in their scores represents a change in the perceived quality of treatment. These include the working alliance, group cohesion, and the clarification of meaning. Outcome-type mechanisms, on the other hand, represent patients’ evaluation of their own condition. They have a pre-treatment value, and, like outcome variables, they capture the patients’ actual state that is expected to change during treatment. These include the interoceptive awareness, emotional regulation skills, symptom acceptance, and relational needs satisfaction. To evaluate a week in therapy, we are primarily interested in the raw values of process-type mechanisms but in incremental (i.e., week-by-week) changes in outcome-type mechanisms.
Testing whether outcomes and mechanisms could be predicted by treatment dose
To test whether (i) a relationship between dose and a change in outcome status exists as well as whether (ii) there is a relationship between dose and a change in the mechanism level, we estimated a model for each outcome and mechanism variable in which the variable, centered to its baseline value, was predicted by time (i.e., treatment dose, defined as the number of weeks in therapy), controlling for gender, age, and baseline level of the variable (for process-type mechanisms, the first in-treatment measurement was treated as baseline).
Before we could proceed with testing the first two conditions, we had to decide how to best model the influence of time. There is a discussion in the literature about the shape of the change trajectory. While some studies suggest that there is a linear relationship between the dose of therapy and the amount of change (Nordmo et al., Citation2020), others have found a negatively accelerated pattern (Stulz et al., Citation2013). Since it was not clear which pattern to expect in our data, we tested both options and found that linear time (i.e., number of weeks) predicted outcomes better than a negatively accelerated pattern (i.e., log-transformed time). Therefore, we used the week number as the dose variable (DOSE) in the following model (Model 1) for each outcome and mechanism variable as follows. The dependent variable was centered to the individual pre-treatment value (or the first measurement in case of process-type mechanisms), therefore a random effect was only allowed for the slope of the dose variable:
where yit is the centered outcome or mechanism variable at week X; β0i is the model’s intercept with its fixed effect γ01; yi1 is the baseline value of the respective variable; eji the normally distributed occasion residual; γ10 the fixed effect for the coefficient of dose, and υ1i its normally distributed random effect. The relationship between the dose and the mechanism level was required only for outcome-type mechanisms but was tested with process-type mechanisms as well for exploratory purposes.
Testing whether a change in a mechanism precedes a change in outcome and/or vice versa
To test whether (iii) the change in mechanism precedes the change in outcome, we estimated Model 2 in which a weekly change (increment) in the outcome variable in week X was regressed on a weekly change (increment) in the mechanism variable in week X-1, controlling for the effects of gender, age, and site (as fixed effect). Centering and detrending are strategies recommended to prevent between-person differences on baseline and the overall time trend from confounding the mechanism-outcome relationships (Wang & Maxwell, Citation2015). By using increments of both the outcome and mechanism variables, rather than their raw values, we have effectively detrended these variables (i.e., by isolating “local”, session-by-session changes, we removed the cumulative effect of time) and also rendered centering irrelevant (since increments contain no information about the baseline value). Unlike the previous model, Model 2 contains a random effect only for the intercept. However, the intercept stands for the overall rate of change here and, therefore, must be interpreted as a within-person effect:
where ΔOUTCOMEit is an increment of the outcome variable between weeks X-1 and X; β0i is the model’s intercept; ΔMECHANISM(LAG1) is an increment of the mechanism variable between weeks X-2 and X-1; eji the normally distributed occasion residual; γ00 the fixed effect for the rate of change; and υ0i its normally distributed random effect.
The reverse hypothesis predicting that the change in outcome precedes the change in the hypothesized mechanism (iv) was tested in Model 3. Here, a weekly change (increment) in the mechanism variable in week X was regressed on a weekly change (increment) in the outcome variable in week X-1, again controlling for the effects of gender, age, and site (as fixed effect) as follows:
The interpretation of Model 3 is analogous to Models 2. In the case of process variables with no pre-treatment value, raw scores were used instead of increments. The analyses were conducted for each of the hypothesized mechanisms. Moreover, we explored the possibility that the two outcomes (i.e., somatic symptoms and well-being) might serve as mechanisms for each other.
Exploring different time lags
To explore the possibility that meaningful cross-lag relationships exist over a longer period of time, we repeated the abovementioned analysis with a two- and three-week lag. Furthermore, we explored the concurrent relationships between the change in the mechanism and outcome variables using the following model (Model 4):
where ΔOUTCOMEit is an increment of the outcome variable between weeks X-1 and X; β0i is the model’s intercept; ΔMECHANISM is an increment of the mechanism variable between weeks X-3 and X-2 (i.e., lag 2) or between weeks X-4 and X-3 (i.e., lag 3); eji the normally distributed occasion residual; γ00 the fixed effect for the rate of change; and υ0i its normally distributed random effect.
The entire set of analyses was conducted for the primary outcome (somatic symptom intensity) and for the secondary outcome (well-being). The hypotheses were tested at the p < .05 significance level. All coefficients reported in were standardized using the effectsize (Ben-Shachar et al., Citation2020) package. Models were estimated using the maximum likelihood method. The proportion of the variance of the outcome variable explained by the grouping variable (i.e., patient) was calculated as an intraclass correlation coefficient (ICC; Lorah, Citation2018). We encountered singularity issues caused by the fact that the random effects explained only a negligible amount of the total variation in some models. Since the aim of the analysis was not to estimate this portion of the variance but to control for it, we proceeded with the analysis as planned. The data and the script are available in the Open Science Framework (Řiháček, Citation2019).
Table II. Prediction of change in outcome and mechanism variables by treatment dose (N = 290; Model 1; all coefficients standardized).
Table III. The difference in symptom intensity as an outcome (all coefficients standardized).
Table IV. The difference in well-being as an outcome (all coefficients standardized).
Results
Sample Description
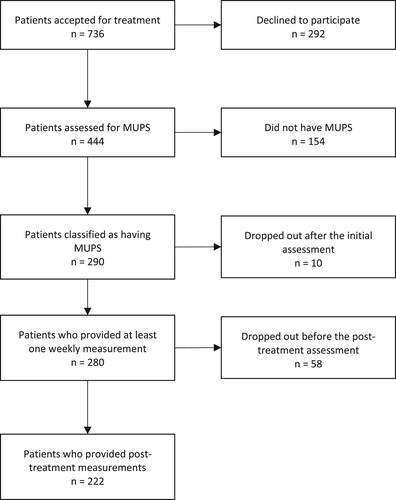
A total of 444 patients agreed to participate in the study, which was 60% of all patients accepted for treatment (see for the flow diagram). There was a high variability in the recruitment rate per site (35% to 91%, with a median value of 63%). Out of the total sample, N = 290 patients (65%) were classified as having MUPS. Only 280 of these patients commenced treatment after the initial assessment, and 222 provided the post-treatment measurements. The sample size decreased linearly until the sixth week (with a decrement of approximately 15 patients per week), followed by a more rapid decrease in the subsequent weeks. This corresponds with the length of the treatment programs. Most of the patients (84%) participated in outpatient programs. The dose of psychotherapy ranged from 1 to 60 sessions with a median of 32. See Supplement 1 for the descriptive statistics of the outcome and process variables.
Are Outcomes and Mechanisms Predicted by Treatment Dose?
The two outcomes and all outcome-type mechanisms were significantly related to time in therapy, with absolute β values ranging from .14 to .36. Although this condition was not required for process-type mechanisms, it was satisfied in cases of these mechanisms as well (see ). This indicates that a longer time in treatment was associated with greater intensity of the mechanisms and with better outcomes. Few statistically significant associations were found for demographic variables (see ): men reported higher increase of relational needs satisfaction (β = .10) and older people reported higher increase in symptom willingness (β = .05). The proportion of variance explained by between-person differences in slope parameters (i.e., rate of change) varied between 4 and 12%.
Does a Change in Mechanisms Precede a Change in Somatic Symptoms (and not Vice Versa)?
shows that when time-lagged relationships were considered, there were only a few statistically significant relationships between hypothesized mechanisms and somatic symptom intensity. More importantly, all relationships were in the opposite direction than hypothesized. Thus, improvement in emotional regulation skills (β = .06) and relational needs satisfaction (β = .06) preceded worsening of somatic symptoms in the following week, while worsening of somatic symptoms preceded an increase in activity engagement (β = .08). Well-being, when considered a change mechanism for somatic symptoms, exhibited a “bidirectional” pattern: an increase in well-being both preceded (β = .06) and was preceded by (β = .12) worsening of somatic symptoms, although the latter association was stronger.
With a lag of two weeks, an increase in well-being preceded a worsening of somatic symptoms (β = .08). With a lag of three weeks, an increase in symptom willingness preceded the worsening of somatic symptoms (β = .09) and, worsening somatic symptoms preceded an increase in interoceptive awareness.
When concurrent relationships were considered, all hypothesized mechanisms except for group cohesion were related to somatic symptom changes in the expected direction, meaning that the mechanisms tended to change concurrently (or within a time interval shorter than one week) with somatic symptoms. A change in well-being was the strongest concurrent predictor of somatic symptoms (β = -.28), followed by a change in emotional regulation skills (β = -.17), a change in activity engagement (β = -.15), and a change in relational needs satisfaction (β = -.11).
also shows the proportion of variance explained by individual differences in the rate of change. While patients’ individual rates of change did not vary in outcomes and outcome-type mechanisms (ICCs were zero), they varied markedly in process-type mechanisms (ICCs between .50 and .67). This pattern was consistent across all time lags, except for the concurrent analysis (Model 4).
Does a Change in Mechanisms Precede a Change in Well-Being (and not Vice Versa)?
shows that when a one-week lag is considered, only relationships opposite to those hypothesized were found. An increase in emotional regulation skills (β = -.07) preceded a worsening of well-being. In the reverse direction, an increase in well-being preceded a worsening of interoceptive awareness (β = -.06), emotional regulation skills (β = -.12), activity engagement (-.13), and relational needs satisfaction (β = -.11).
With a lag of two weeks, three relationships reached statistical significance – all of them were positive but in the reverse direction: an increase in well-being preceded an increase in interoceptive awareness (β = .07) and higher working alliance (β = .04). With a lag of three weeks, a decrease in well-being was preceded by an increase in relational needs satisfaction (β = -.07) and a decrease in well-being itself preceded increase in interoceptive awareness (β = -.06).
When concurrent relationships were considered, all hypothesized mechanisms were related to a well-being change in the expected direction, meaning that the mechanisms tended to change concurrently (or within a time interval shorter than one week) with well-being. Emotional regulation skills (β = .31), activity engagement (β = .26), and relational satisfaction needs (β = .24) were the strongest concurrent predictors of well-being, followed by interoceptive awareness (β = .20), clarification of meaning (β = .13), and working alliance (β = .13).
also shows the proportion of variance explained by individual differences in the rate of change. The pattern was similar to that found in and consistent across all time lags (except for the concurrent analysis, Model 4): while patients’ individual rates of change did not vary in outcomes and outcome-type mechanisms (ICCs were zero), they varied markedly in process-type mechanisms (ICCs between .50 and .68).
Sensitivity Analysis
The above-described analysis yielded unexpected, counter-intuitive findings. We explored the possibility that it was a consequence of the mechanisms working differently in patients with different baseline level of difficulties. We split the sample into three tiers based on the initial level of outcome variables (tertile split, i.e., low, medium, and high baseline levels) and re-run the main analyses. Overall, this analysis confirmed the above-described pattern of counter-intuitive relationships (i.e., improvement in mechanisms predicting deterioration in outcome and vice versa). There were three exceptions to this pattern: higher scores on the working alliance, group cohesion, and clarification of meaning preceded improvement in somatic symptoms in patients with low baseline scores on somatic symptoms (although with a marginal effect size). While a closer examination of the regression coefficients revealed some potentially meaningful differences among the three subsamples, the power of this analysis was limited and, therefore, we refrained from over-interpreting these findings. For details and the analysis and findings, see Supplements 4, 5, and 6.
Discussion
This study aimed to investigate the role of several mechanisms of therapeutic change in adult patients suffering from MUPS in the context of intensive group-based multi-component psychological treatment. We followed the logic of Granger causality testing in which the causal claims are based on temporal precedence (Tschacher & Ramseyer, Citation2009). While we regarded somatic symptoms as the primary outcome, we also investigated well-being as a secondary outcome. The relationships between mechanisms and outcomes were primarily tested for a one-week lag, but they were also explored for two- and three-week lags, as well as for concurrent changes (i.e., within the same week).
The most striking finding was a lack of support for any of the hypothesized mechanisms in the one-, two-, and three-week lags. Thus, none of the hypotheses were supported in our study. Generally, the lagged relationships found between the hypothesized mechanisms and outcomes were weak, and most of them were in the opposite direction than what was expected (i.e., an increase in a mechanism was related to a deterioration in an outcome and vice versa). This finding is counterintuitive and calls for further exploration. The fact that this pattern was present across mechanisms and outcomes suggests that this is a systematic phenomenon rather than a mere coincidence.
While it is possible that mild temporary deterioration is a part of the recovery process, this seems to be true only for a minority of patients (Owen et al., Citation2015). Instead, psychotherapy affects not only the level of symptoms/well-being but also the way patients perceive and evaluate their state (Sandell & Wilczek, Citation2016). For instance, an increase in emotional regulation skills (which includes more detailed monitoring of emotional and bodily reactions) may lead to a higher focus on symptoms, which, in turn, may appear as a deterioration displayed by an outcome measure later in the treatment (Salkovskis et al., Citation2016). At the same time, worsening of symptoms/well-being may cause patients to become more aware of their resources (such as activity engagement or, in the case of well-being, emotional regulation skills and relational support) and focus on utilizing these resources, which, in turn, may appear as an increase in these resources/mechanisms (Claassen-van Dessel et al., Citation2015). Worsening of symptoms—interpreted as in-treatment destabilization that makes patients sensitive to change—has been linked to better outcomes in patients with mood disorders (Olthof et al., Citation2020). Additionally, when patients begin to feel better in therapy, they may decrease their engagement in therapeutic activities in the following weeks, which may then result in a slowed pace of change or even in deterioration. Indeed, patients in our sample who were interviewed about the process of their treatment noted that abating the use of their resources and skills is one of the reasons why their symptoms returned during and/or after the treatment (Polakovská et al., Citation2021).
Relationships between the hypothesized mechanisms and outcomes that were consistent with our expectations were found almost exclusively within the same week (concurrent changes). From this perspective, all hypothesized mechanisms were related to changes in well-being, and all but group cohesion were related to changes in somatic symptoms. However, given that changes in both the mechanism and the outcome occurred in the same time window, we cannot make any claims about the direction of causality. We did not find any study that demonstrated a similar pattern of time-lagged relationships between change mechanisms and outcomes during treatment. There are studies that—similar to ours—showed theoretically meaningful concurrent changes in hypothesized mechanisms and symptoms but failed to demonstrate time-lagged relationships between changes in mechanisms and outcomes (Bloot et al., Citation2015; Heins, Knoop, Burk, et al., Citation2013). The results from our concurrent analyses are therefore in line with existing literature, and our results suggest that weekly measurements are too coarse to capture the dynamics of therapeutic change, at least in the context of intensive treatment consisting of several group therapy sessions per week. Future studies should adopt more frequent data collection schedules, for example, on a by-session or daily basis (Falkenström et al., Citation2020; Kyron et al., Citation2018), or utilize ecological momentary assessment strategies (Rief et al., Citation2017) to explore if meaningful time-lagged relationships can be found in shorter time frames. Furthermore, analysis focused on the identification of subgroups of patients with different change trajectories, as well as qualitative exploration of the change process, may also help explain these unexpected findings. To investigate the robustness of our findings, we also conducted the same analysis for patients without MUPS. The patterns of results were similar, suggesting that the findings are not specific for patients with MUPS. See Supplements 2 and 3 for the results based on the total sample with pooled MUPS and non-MUPS patient subsamples.
An alternative concept to explore is that changes in both the outcomes and the hypothesized mechanisms have a common cause, such as remoralization (Howard et al., Citation1993) or social connection (Wampold, Citation2012), which may cause the mechanisms to change simultaneously without being causally related to each other. From this point of view, the traditional distinction between mechanisms and outcomes would appear rather arbitrary, and researchers would have to focus on these “background” fundamental processes. This perspective would be consistent with the contextual model in psychotherapy (Wampold & Imel, Citation2015).
The hypothesized mechanisms were related more strongly to changes in well-being than to somatic symptom changes. Based on the strength of association, the best concurrent predictors of both outcomes included emotional regulation skills and activity engagement, which is in line with the available evidence (Agar-Wilson & Jackson, Citation2012; Heins, Knoop, Burk, et al., Citation2013; Hesser et al., Citation2014). The fact that relational needs satisfaction was also among the mechanisms with the strongest association with outcome appears to contradict studies that failed to find any strong association (Åkerblom et al., Citation2015; Pourová, Klocek, et al., Citation2020); this finding may be a consequence of the group psychotherapy setting.
Limitations
This was an uncontrolled, naturalistic study. The treatment was not standardized across sites, and the change mechanisms were not necessarily explicitly targeted to the same degree at all sites. Furthermore, the absence of experimental manipulation did not allow us to test the causal effects among the therapeutic intervention, the hypothesized mechanisms, and outcomes. Instead, this study capitalized on the variability naturally existing in a heterogeneous sample of patients and tested the temporal relationships between the outcome and mechanism variables using the Granger causality approach. While the four specified conditions represent a compelling case for a central role of the hypothesized mechanisms in the process of therapeutic change (Falkenström et al., Citation2020), our data suggest that meaningful temporal relationships between mechanisms and outcomes must be sought with a more fine-grained time resolution (cf. Zilcha-Mano, Citation2019).
Except for the CPAQ-M, we only used total scores of the measures in the analyses. However, important differences at the subscale level may exist. For instance, understanding one’s emotions may have a different effect on well-being than acceptance of emotions, although both are components of the total score of emotional regulation skill (Berking & Znoj, Citation2008; Kotsou et al., Citation2018). An exploration of these relationships was beyond the scope of this study, but it may provide more detailed insights into the dynamics of the therapeutic change.
The sensitivity of the analysis was limited by factors such as the reliability of the measures and a limited number of observations per patient. The results could be also confounded by a group effect. Although there are techniques that allow controlling for the group effect in rolling groups (e.g., Tasca et al., Citation2010), they did not provide a straightforward solution for our statistical models.
The generalizability of our findings is limited by a relatively low recruitment rate and subsequent attrition. Patients who did not consent to be included in the study might share some characteristics related to the phenomena under study, including diagnosis; symptom severity; and nondiagnostic characteristics such as readiness for change, psychological mindedness, social support, and others. Furthermore, only patients who provided at least two weekly measurements (for concurrent analysis), three weekly measurements (for one-week lag analysis), four weekly measurements (for two-week lag analysis), and five weekly measurements (for three-week lag analysis) were included. The exclusion of patients who dropped out early from the treatment could have introduced another systematic bias.
Conclusions
This study failed to find cross-lagged relationships between hypothesized change mechanisms and outcomes that are consistent with theory. In other words, speaking from the framework of Granger causality testing, we did not find evidence that the hypothesized variables acted as change mechanisms in the alteration of somatic symptom intensity and well-being of patients suffering from MUPS. However, we found meaningful concurrent relationships that suggest that time-lagged relationships are likely to be found using a more fine-grained time resolution (e.g., with daily measurement). Furthermore, we found a counterintuitive yet consistent pattern of time-lagged relationships between the hypothesized change mechanisms and outcomes that call for exploration in future studies. The study has shown that determining the optimal duration of the lag between the changes in mechanisms and outcomes is crucial for successfully modeling the process of change. Researchers are advised to adopt more frequent data collection schedules and obtain a larger number of observations per patient to model these time-related relationships in future studies. Furthermore, given the counterintuitive nature of our results, multiple methods of analysis, such as time-lagged panel data analysis (Falkenström et al., Citation2020), should be employed to investigate these phenomena and results from multiple studies should be aggregated to see how robust these findings are.
Supplemental Material
Download MS Word (69 KB)Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplemental Data
Supplemental data for this article can be accessed https://doi.org/10.1080/10503307.2022.2061874.
Additional information
Funding
References
- Agar-Wilson, M., & Jackson, T. (2012). Are emotion regulation skills related to adjustment among people with chronic pain, independent of pain coping? European Journal of Pain, 16(1), 105–114. https://doi.org/10.1016/j.ejpain.2011.05.011
- Åkerblom, S., Perrin, S., Rivano Fischer, M., & McCracken, L. M. (2015). The mediating role of acceptance in multidisciplinary cognitive-behavioral therapy for chronic pain. Journal of Pain, 16(7), 606–615. https://doi.org/10.1016/j.jpain.2015.03.007
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (DSM-IV-TR).
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5).
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. https://doi.org/10.18637/jss.v067.i01
- Ben-Shachar, M. S., Makowski, D., & Lüdecke, D. (2020). Compute and interpret indices of effect size. CRAN. https://github.com/easystats/effectsize.
- Berking, M., & Znoj, H. (2008). Entwicklung und validierung eines fragebogens zur standardisierten selbsteinschätzung emotionaler kompetenzen (SEK-27). Zeitschrift Fur Psychiatrie, Psychologie Und Psychotherapie, 56(2), 141–153. https://doi.org/10.1024/1661-4747.56.2.141
- Bloot, L., Heins, M. J., Donders, R., Bleijenberg, G., & Knoop, H. (2015). The process of change in pain during cognitive behavior therapy for chronic fatigue syndrome. Clinical Journal of Pain, 31(10), 914–921. https://doi.org/10.1097/AJP.0000000000000191
- Bullington, J. (2013). The expression of the psychosomatic body from a phenomenological perspective. Springer.
- Burlingame, G. M., McClendon, D. T., & Alonso, J. (2011). Cohesion in group therapy. Psychotherapy, 48(1), 34–42. https://doi.org/10.1037/a0022063
- Chambers, D., Bagnall, A., Hempel, S., & Forbes, C. (2006). Interventions for the treatment, management and rehabilitation of patients with chronic fatigue syndrome/ myalgic encephalomyelitis: An updated systematic reviewmyalgic encephalomyelitis : an updated systematic review. Journal of the Royal Society of Medicine, 99(10), 506–520. https://doi.org/10.1258/jrsm.99.10.506
- Chow, P. I., Ingersoll, K. S., Thorndike, F. P., Lord, H. R., Gonder-Frederick, L., Morin, C. M., & Ritterband, L. M. (2018). Cognitive mechanisms of sleep outcomes in a randomized clinical trial of internet-based cognitive behavioral therapy for insomnia. Sleep Medicine, 47, 77–85. https://doi.org/10.1016/j.sleep.2017.11.1140
- Claassen-van Dessel, N., Velzeboer, F. R., van der Wouden, J. C., den Boer, C., Dekker, J., & van der Horst, H. E. (2015). Patients’ perspectives on improvement of medically unexplained physical sqymptoms: A qualitative analysis. Mental Health in Family Medicine, 11(02), https://doi.org/10.25149/1756-8358.1102007
- Courtois, I., Cools, F., & Calsius, J. (2015). Effectiveness of body awareness interventions in fibromyalgia and chronic fatigue syndrome: A systematic review and meta-analysis. Journal of Bodywork and Movement Therapies, 19(1), 35–56. https://doi.org/10.1016/j.jbmt.2014.04.003
- De Gucht, V., & Heiser, W. (2003). Alexithymia and somatisation: A quantitative review of the literature. Journal of Psychosomatic Research, 54(5), 425–434. https://doi.org/10.1016/S0022-3999(02)00467-1
- Falkenström, F., Solomonov, N., & Rubel, J. (2020). Using time-lagged panel data analysis to study mechanisms of change in psychotherapy research: Methodological recommendations. Counselling and Psychotherapy Research, 20(3), 435–441. https://doi.org/10.1002/capr.12293
- Glombiewski, J. A., Sawyer, A. T., Gutermann, J., Koenig, K., Rief, W., & Hofmann, S. G. (2010). Psychological treatments for fibromyalgia: A meta-analysis. Pain, 151(2), 280–295. https://doi.org/10.1016/j.pain.2010.06.011
- Godfrey, E., Chalder, T., Ridsdale, L., Seed, P., & Ogden, J. (2007). Investigating the “active ingredients” of cognitive behaviour therapy and counselling for patients with chronic fatigue in primary care: Developing a new process measure to assess treatment fidelity and predict outcome. British Journal of Clinical Psychology, 46(3), 253–272. https://doi.org/10.1348/014466506X147420
- Granger, C. W. J. (1969). Investigating causal relations by econometric models and cross-spectral methods. Econometrica, 37(3), 424–438. https://doi.org/10.2307/1912791
- Gureje, O., & Reed, G. M. (2016). Bodily distress disorder in ICD-11: Problems and prospects. World Psychiatry, 15(3), 291–292. https://doi.org/10.1002/wps.20353
- Harvey, A. G., Dong, L., Bélanger, L., & Morin, C. M. (2017). Mechanisms of change and treatment matching in behavior therapy, cognitive therapy and cognitive behavior therapy for chronic insomnia. Journal of Consulting and Clinical Psychology, 85(10), 975–987. https://doi.org/10.1037/ccp0000244
- Heins, M. J., Knoop, H., & Bleijenberg, G. (2013). The role of the therapeutic relationship in cognitive behaviour therapy for chronic fatigue syndrome. Behaviour Research and Therapy, 51(7), 368–376. https://doi.org/10.1016/j.brat.2013.02.001
- Heins, M. J., Knoop, H., Burk, W. J., & Bleijenberg, G. (2013). The process of cognitive behaviour therapy for chronic fatigue syndrome: Which changes in perpetuating cognitions and behaviour are related to a reduction in fatigue? Journal of Psychosomatic Research, 75(3), 235–241. https://doi.org/10.1016/j.jpsychores.2013.06.034
- Hesser, H., Westin, V. Z., & Andersson, G. (2014). Acceptance as a mediator in internet-delivered acceptance and commitment therapy and cognitive behavior therapy for tinnitus. Journal of Behavioral Medicine, 37(4), 756–767. https://doi.org/10.1007/s10865-013-9525-6
- Horvath, A. O., Del Re, a. C., Flückiger, C., & Symonds, D. (2011). Alliance in individual psychotherapy. Psychotherapy, 48(1), 9–16. https://doi.org/10.1037/a0022186
- Howard, K. I., Lueger, R. J., Maling, M. S., & Martinovich, Z. (1993). A phase model of psychotherapy outcome: Causal mediation of change. Journal of Consulting and Clinical Psychology, 61(4), 678–685. https://doi.org/10.1037/0022-006X.61.4.678
- Hyphantis, T., Guthrie, E., Tomenson, B., & Creed, F. (2009). Psychodynamic interpersonal therapy and improvement in interpersonal difficulties in people with severe irritable bowel syndrome. Pain, 145(1–2), 196–203. https://doi.org/10.1016/j.pain.2009.07.005
- Kashner, T. M., Rost, K., Cohen, B., Anderson, M., & Smith, G. R. (1995). Enhancing the health of somatization disorder patients: Effectiveness of short-term group therapy. Psychosomatics, 36(5), 462–470. https://doi.org/10.1016/S0033-3182(95)71627-9
- Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3(1), 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432
- Kleinstäuber, M., Witthöft, M., & Hiller, W. (2011). Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: A meta-analysis. Clinical Psychology Review, 31(1), 146–160. https://doi.org/10.1016/j.cpr.2010.09.001
- Kotsou, I., Leys, C., & Fossion, P. (2018). Acceptance alone is a better predictor of psychopathology and well-being than emotional competence, emotion regulation and mindfulness. Journal of Affective Disorders, 226, 142–145. https://doi.org/10.1016/j.jad.2017.09.047
- Kroenke, K. (2006). Physical symptom disorder: A simpler diagnostic category for somatization-spectrum conditions. Journal of Psychosomatic Research, 60(4), 335–339. https://doi.org/10.1016/j.jpsychores.2006.01.022
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2002). The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine, 64(2), 258–266. https://doi.org/10.1097/00006842-200203000-00008
- Kyron, M. J., Hooke, G. R., & Page, A. C. (2018). Daily assessment of interpersonal factors to predict suicidal ideation and non-suicidal self-injury in psychiatric inpatients. Journal of Consulting and Clinical Psychology, 86(6), 556–567. https://doi.org/10.1037/ccp0000305
- Lacourt, T., Houtveen, J., & van Doornen, L. (2013). Functional somatic syndromes, one or many?”: An answer by cluster analysis. Journal of Psychosomatic Research, 74(1), 6–11. https://doi.org/10.1016/j.jpsychores.2012.09.013
- Lakhan, S. E., & Schofield, K. L. (2013). Mindfulness-based therapies in the treatment of somatization disorders: A systematic review and meta-analysis. PloS One, 8(8), e71834. https://doi.org/10.1371/journal.pone.0071834
- Lambert, M. J. (2013). The efficacy and effectiveness of psychotherapy. In M. J. Lambert (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change (6th ed) (pp. 169–218). John Wiley.
- Lidbeck, J. (1997). Group therapy for somatization disorders in general practice: Effectiveness of a short cognitive-behavioural treatment model. Acta Psychiatrica Scandinavica, 96(1), 14–24. https://doi.org/10.1111/j.1600-0447.1997.tb09899.x
- Lidbeck, J. (2003). Group therapy for somatization disorders in primary care: Maintenance of treatment goals of short cognitive-behavioural treatment one-and-a-half-year follow-up. Acta Psychiatrica Scandinavica, 107(6), 449–456. https://doi.org/10.1034/j.1600-0447.2003.00048.x
- Lorah, J. (2018). Effect size measures for multilevel models: Definition, interpretation, and TIMSS example. Large-scale Assess Educ, 6(8), 1–11. https://doi.org/10.1186/s40536-018-0061-2
- Luyten, P., & van Houdenhove, B. (2013). Common and specific factors in the psychotherapeutic treatment of patients suffering from chronic fatigue and pain. Journal of Psychotherapy Integration, 23(1), 14–27. https://doi.org/10.1037/a0030269
- Luyten, P., van Houdenhove, B., Lemma, A., Target, M., & Fonagy, P. (2012). A mentalization-based approach to the understanding and treatment of functional somatic disorders. Psychoanalytic Psychotherapy, 26(2), 121–140. https://doi.org/10.1080/02668734.2012.678061
- Mander, J., Wittorf, A., Klingberg, S., Teufel, M., Zipfel, S., & Sammet, I. (2014). The patient perspective on therapeutic change: The investigation of associations between stages of change and general mechanisms of change in psychotherapy research. Journal of Psychotherapy Integration, 24(2), 122–137. https://doi.org/10.1037/a0036976
- Mander, J., Wittorf, A., Schlarb, A., Hautzinger, M., Zipfel, S., & Sammet, I. (2013). Change mechanisms in psychotherapy: Multiperspective assessment and relation to outcome. Psychotherapy Research, 23(1), 105–116. https://doi.org/10.1080/10503307.2012.744111
- McCracken, L. M., Vowles, K. E., & Eccleston, C. (2004). Acceptance of chronic pain: Component analysis and a revised assessment method. Pain, 107(1–2), 159–166. https://doi.org/10.1016/j.pain.2003.10.012
- Meeus, M., Nijs, J., Vanderheiden, T., Baert, I., Descheemaeker, F., & Struyf, F. (2015). The effect of relaxation therapy on autonomic functioning, symptoms and daily functioning, in patients with chronic fatigue syndrome or fibromyalgia: A systematic review. Clinical Rehabilitation, 29(3), 221–233. https://doi.org/10.1177/0269215514542635
- Mehling, W. E., Price, C., Daubenmier, J. J., Acree, M., Bartmess, E., & Stewart, A. (2012). The Multidimensional Assessment of Interoceptive awareness (MAIA). PLoS ONE, 7(11), 1–22. https://doi.org/10.1371/journal.pone.0048230
- Miller, S. D., Duncan, B. L., Brown, J., Sparks, J. A., & Claud, D. A. (2003). The outcome Rating Scale: A preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. Journal of Brief Therapy, 2(2), 91–100.
- Moreno, S., Gili, M., Magallón, R., Bauzá, N., Roca, M., Del Hoyo, Y. L., & Garcia-Campayo, J. (2013). Effectiveness of group versus individual cognitive-behavioral therapy in patients with abridged somatization disorder: A randomized controlled trial. Psychosomatic Medicine, 75(6), 600–608. https://doi.org/10.1097/PSY.0b013e31829a8904
- Nezu, A. M., Nezu, C. M., & Lombardo, E. R. (2001). Cognitive-behavior therapy for medically unexplained symptoms: A critical review of the treatment literature. Behavior Therapy, 32(3), 537–583. doi:http://doi.org/10.1016/S0005-7894(01)80035-6
- Nimnuan, C., Rabe-Hesketh, S., Wessely, S., & Hotopf, M. (2001). How many functional somatic syndromes? Journal of Psychosomatic Research, 51(4), 549–557. https://doi.org/10.1016/S0022-3999(01)00224-0
- Nordmo, M., Monsen, J. T., Høglend, P. A., & Solbakken, O. A. (2020). Investigating the dose-response effect in open-ended psychotherapy. Psychotherapy Research. Advance online publication. https://doi.org/10.1080/10503307.2020.1861359
- Nüesch, E., Häuser, W., Bernardy, K., Barth, J., & Jüni, P. (2013). Comparative efficacy of pharmacological and non-pharmacological interventions in fibromyalgia syndrome: Network meta-analysis. Annals of the Rheumatic Diseases, 72(6), 955–962. https://doi.org/10.1136/annrheumdis-2011-201249
- Olthof, M., Hasselman, F., Strunk, G., Aas, B., Schiepek, G., & Lichtwarck-Aschoff, A. (2020). Destabilization in self-ratings of the psychotherapeutic process is associated with better treatment outcome in patients with mood disorders. Psychotherapy Research, 30(4), 520–531. https://doi.org/10.1080/10503307.2019.1633484
- Owen, J., Adelson, J., Budge, S., Wampold, B., Kopta, M., Minami, T., & Miller, S. (2015). Trajectories of change in psychotherapy. Journal of Clinical Psychology, 71(9), 817–827. https://doi.org/10.1002/jclp.22191
- Payne, H., & Brooks, S. D. M. (2017). Moving on: The BodyMind ApproachTM for medically unexplained symptoms. Journal of Public Mental Health, 16(2), 63–71. https://doi.org/10.1108/JPMH-10-2016-0052
- Perrot, S., & Russell, I. J. (2014). More ubiquitous effects from non-pharmacologic than from pharmacologic treatments for fibromyalgia syndrome: A meta-analysis examining six core symptoms. European Journal of Pain, 18(8), 1067–1080. https://doi.org/10.1002/ejp.564
- Polakovská, L., Čevelíček, M., Roubal, J., & Řiháček, T. (2021). Changes after multicomponent psychological treatment in patients with medically unexplained physical symptoms: A qualitative study. Manuscript Submitted for publication.
- Pourová, M., Klocek, A., Řiháček, T., & Čevelíček, M. (2020). Therapeutic change mechanisms in adults with medically unexplained physical symptoms: A systematic review. Journal of Psychosomatic Research, 134, Article 110124. https://doi.org/10.1016/j.jpsychores.2020.110124
- Pourová, M., Řiháček, T., Boehnke, J. R., Šimek, J., Saic, M., Kabát, J., & Šilhán, P. (2021). Effectiveness of a multicomponent group-based psychological treatment in patients with medically unexplained physical symptoms: A multisite naturalistic study. Manuscript Submitted for publication.
- Pourová, M., Řiháček, T., & Žvelc, G. (2020). Validation of the Czech version of the relational needs satisfaction scale. Frontiers in Psychology, 11(March), 1–11. https://doi.org/10.3389/fpsyg.2020.00359
- Quirk, K., Miller, S., Duncan, B., & Owen, J. (2013). Group Session Rating Scale: preliminary psychometrics in substance abuse group interventions. Counselling and Psychotherapy Research, 13(3), 194–200. https://doi.org/10.1080/14733145.2012.744425
- R Core Team. (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing. URL https://www.R-project.org/.
- Rief, W., Burton, C., Frostholm, L., Henningsen, P., Kleinstäuber, M., Kop, W. J., Löwe, B., Martin, A., Malt, U., Rosmalen, J., Schröder, A., Shedden-Mora, M., Toussaint, A., & Van Der Feltz-Cornelis, C. (2017). Core outcome domains for clinical trials on somatic symptom disorder, bodily distress disorder, and functional somatic syndromes: European network on somatic symptom disorders recommendations. Psychosomatic Medicine, 79(9), 1008–1015. https://doi.org/10.1097/PSY.0000000000000502
- Řiháček, T. (2019). Effectiveness of psychotherapy in patients with medically unexplained physical symptoms: A multi-site naturalistic study. https://osf.io/dfrma.
- Řiháček, T., & Čevelíček, M. (2020). Common therapeutic strategies in psychological treatments for medically unexplained somatic symptoms. Psychotherapy Research, 30(4), 532–545. https://doi.org/10.1080/10503307.2019.1645370
- Salkovskis, P. M., Gregory, J. D., Sedgwick-Taylor, A., White, J., Opher, S., & Ólafsdóttir, S. (2016). Extending cognitive-behavioural theory and therapy to medically unexplained symptoms and long-term physical conditions: A hybrid transdiagnostic/problem specific approach. Behaviour Change, 33(4), 172–192. https://doi.org/10.1017/bec.2016.8
- Sandell, R., & Wilczek, A. (2016). Another way to think about psychological change: Experiential vs. Incremental. European Journal of Psychotherapy & Counselling, 18(3), 228–251. https://doi.org/10.1080/13642537.2016.1214163
- Schaefer, M., Egloff, B., & Witthöft, M. (2012). Is interoceptive awareness really altered in somatoform disorders? Testing competing theories with two paradigms of heartbeat perception. Journal of Abnormal Psychology, 121(3), 719–724. https://doi.org/10.1037/a0028509
- Selders, M., Visser, R., van Rooij, W., Delfstra, G., & Koelen, J. A. (2015). The development of a brief group intervention (Dynamic interpersonal therapy) for patients with medically unexplained somatic symptoms: A pilot study. Psychoanalytic Psychotherapy, 29(2), 182–198. https://doi.org/10.1080/02668734.2015.1036106
- Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press.
- Speckens, A. E. M., Spinhoven, P., Hawton, K. E., Bolk, J. H., & Van Hemert, A. M. (1996). Cognitive behavioural therapy for medically unexplained physical symptoms: A pilot study. Behavioural and Cognitive Psychotherapy, 24(1), 1–16. https://doi.org/10.1017/S1352465800016799
- Stulz, N., Lutz, W., Kopta, S. M., Minami, T., & Saunders, S. M. (2013). Dose-effect relationship in routine outpatient psychotherapy: Does treatment duration matter? Journal of Counseling Psychology, 60(4), 593–600. https://doi.org/10.1037/a0033589
- Surawy, C., McManus, F., Muse, K., & Williams, J. M. G. (2015). Mindfulness-Based Cognitive Therapy (MBCT) for Health anxiety (Hypochondriasis): Rationale, implementation and case illustration. Mindfulness, 6(2), 382–392. https://doi.org/10.1007/s12671-013-0271-1
- Tasca, G. A., Ramsay, T., Corace, K., Illing, V., Bone, M., Bissada, H., & Balfour, L. (2010). Modeling longitudinal data from a rolling therapy group program with membership turnover: Does group culture affect individual alliance? Group Dynamics, 14(2), 151–162. https://doi.org/10.1037/a0018778
- Trockel, M., Karlin, B. E., Taylor, C. B., & Manber, R. (2014). Cognitive behavioral therapy for insomnia with veterans: Evaluation of effectiveness and correlates of treatment outcomes. Behaviour Research and Therapy, 53(1), 41–46. https://doi.org/10.1016/j.brat.2013.11.006
- Tschacher, W., & Ramseyer, F. (2009). Modeling psychotherapy process by time-series panel analysis (TSPA). Psychotherapy Research, 19(4–5), 469–481. https://doi.org/10.1080/10503300802654496
- van Dessel, N., den Boeft, M., van der Wouden, J. C., Kleinstäuber, M., Leone, S., Terluin, B., Numans, M., van der Horst, H., & van Marwijk, H. (2014). Non-pharmacological interventions for somatoform disorders and medically-unexplained physical symptoms (MUPS) in adults (Protocol). Cochrane Database of Systematic Reviews, 11(6), CD011142. https://doi.org/10.1002/14651858.CD011142.pub2
- Wampold, B. E. (2012). Humanism as a common factor in psychotherapy. Psychotherapy, 49(4), 445–449. https://doi.org/10.1037/a0027113
- Wampold, B. E., & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge.
- Wang, L. P., & Maxwell, S. E. (2015). On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychological Methods, 20(1), 63–83. https://doi.org/10.1037/met0000030
- Wessely, S., Nimnuan, C., & Sharpe, M. (1999). Functional somatic syndromes: One or many? The Lancet, 354(9182), 936–939. https://doi.org/10.1016/S0140-6736(98)08320-2
- Wongpakaran, T., Wongpakaran, N., Intachote-Sakamoto, R., & Boripuntakul, T. (2013). The Group Cohesiveness Scale (GCS) for psychiatric inpatients. Perspectives in Psychiatric Care, 49(1), 58–64. https://doi.org/10.1111/j.1744-6163.2012.00342.x
- World Health Organization. (2008). The international statistical classification of diseases and health related problems (ICD-10) (10th ed.).
- Yoshino, A., Okamoto, Y., Doi, M., Horikoshi, M., Oshita, K., Nakamura, R., Otsuru, N., Yoshimura, S., Tanaka, K., Takagaki, K., Jinnin, R., Yamashita, H., Kawamoto, M., & Yamawaki, S. (2015). Effectiveness of group cognitive behavioral therapy for somatoform pain disorder patients in Japan: A preliminary non-case-control study. Psychiatry and Clinical Neurosciences, 69(12), 763–772. https://doi.org/10.1111/pcn.12330
- Zilcha-Mano, S. (2019). Major developments in methods addressing for whom psychotherapy may work and why. Psychotherapy Research, 29(6), 693–708. https://doi.org/10.1080/10503307.2018.1429691