 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
The available literature points to the potential therapeutic benefits of alliance strengthening during treatment. Both supportive and expressive techniques have been suggested to be associated with strengthening of the alliance. The present study investigates whether patients may show different effects of supportive vs. expressive techniques in improving alliance as a function of their pretreatment insight levels.
Method
Fifty-five patients were randomly assigned to either supportive treatment (ST) or supportive-expressive treatment (SET), as part of a larger randomized controlled trial. Clinical interviews were administered at pretreatment to evaluate the patients’ level of insight. The working alliance was measured after each of the 16 sessions. A multilevel model, including a 3-way interaction of pretreatment insight by treatment condition (ST vs. SET) by time, was used to predict alliance strengthening.
Results
The findings suggest that, for individuals receiving ST, those with higher levels of insight show greater alliance strengthening. For individuals receiving SET, those with lower levels of insight show greater alliance strengthening.
Conclusion
The current study suggests that one size may not fit all and, whereas some individuals may benefit more from ST to achieve alliance strengthening, others may benefit more from SET.
Clinical or methodological significance of this article: The findings of the present study suggest that one size may not fit all in strengthening the alliance. Patients with different levels of insight at pretreatment may benefit from distinct techniques to show improvement in strengthening of the alliance. For patients with a higher initial level of pretreatment insight, it might be more beneficial to strengthen the SL alliance through supportive treatment. For patients with a lower initial level of pretreatment insight, however, it might be more beneficial to strengthen the SL alliance through supportive-expressive treatment. Thus, information about the patient’s level of insight at pretreatment can be useful as an empirically supported tool to decide how to strengthen the alliance.
The therapeutic alliance is commonly defined as the emotional bond established between the patient and the therapist, the agreement between them regarding the goals of treatment, and the degree of therapist-patient agreement regarding the tasks that are pertinent to accomplishing these goals (Bordin, Citation1979). A meta-analysis based on 295 independent samples indicated a positive, moderate-sized effect association between alliance and treatment outcome, which is consistent across different variables related to the measurement, population, setting and treatment types (Flückiger et al., Citation2018). Studies that examined the association between the therapeutic alliance and outcome suggest that stronger alliance is related to symptomatic improvement (Barber et al., Citation2013; Horvath et al., Citation2011) and that alliance improvements temporally precede symptomatic reduction throughout the course of treatment (Zilcha-Mano et al., Citation2014).
In recent years, some of the literature on the alliance has differentiated between two distinct components of alliance: trait-like (TL) and state-like (SL) alliance (Zilcha-Mano & Fisher, Citation2022). The TL component of alliance is conceptualized as referring to individual differences between people in their general tendency to form a strong alliance. A synthesis of the accumulating literature suggests that the TL alliance is a product of the patient’s and the therapist’s baseline TL characteristics, such as intra- and inter-personal characteristics (Zilcha-Mano & Fisher, Citation2022). In contrast, the SL component of the alliance is conceptualized as referring to changes in alliance occurring throughout the course of treatment, such as strengthening or weakening of the alliance from one session to the next, or within a session. The SL alliance can be conceptualized as the component of alliance responsible for its potential to serve as a mechanism of change in treatment (Zilcha-Mano, Citation2017, Citation2020), given that it reflects changes within the individual (Kazdin, Citation2007).
A synthesis of the literature, based on 41 studies that disentangled state-like and trait-like alliance, suggests that although different studies used a variety of approaches to estimate the SL alliance, the findings are relatively consistent across studies: the SL component is significantly associated with subsequent treatment outcome (Zilcha-Mano & Fisher, Citation2022). These findings, along with a conceptual understanding of SL alliance as the mechanism making alliance therapeutic in itself, raises the question of how alliance can be strengthened to improve treatment outcomes.
Currently, little is known about pretreatment characteristics of patients that may predict SL alliance. Most studies looking for such pretreatment characteristics failed to find a consistent association between patients’ demographics (e.g., age, years of education, gender, socioeconomic status) and SL alliance (Accurso et al., Citation2015; Folmo et al., Citation2021; Hersoug et al., Citation2009). A more consistent association was found between patients’ interpersonal characteristics and SL alliance. Specifically, findings suggest that patients who had more interpersonal problems showed greater SL alliance strengthening (Constantino & Smith-Hansen, Citation2008; Dinger et al., Citation2013; Hersoug et al., Citation2009; Ollila et al., Citation2016). Similarly, patients with higher attachment anxiety and lower avoidance (Tasca et al., Citation2007), higher level of distress (Busmann et al., Citation2021; Manne et al., Citation2012; Penzenstadler et al., Citation2018) and impairment in ego functioning (Stenius et al., Citation2021) were found to show greater SL alliance strengthening.
Other studies focused on in-treatment processes that are associated with SL alliance, such as feedback provided to the therapist about the progress of the treatment. These studies found that providing therapists with feedback was positively associated with greater SL alliance strengthening (Errázuriz & Zilcha-Mano, Citation2018; McClintock et al., Citation2017; She et al., Citation2018; Tzur Bitan et al., Citation2020). The theoretical literature suggests the potential role of supportive and expressive techniques in facilitating SL alliance strengthening. In supportive techniques, the therapists implement techniques aimed at actualizing the patient’s interpersonal wishes within the therapeutic relationship and focus on the patient’s strengths (Leibovich et al., Citation2018). Such supportive techniques prepare the ground for enhancing the SL alliance by providing a healing environment of safety and warmth (Solomonov et al., Citation2018). Empirical literature focusing on the association between supportive techniques and SL alliance strengthening suggest a positive association between the two. That is, greater use of supportive techniques was associated with greater SL alliance strengthening (Leibovich et al., Citation2020; Solomonov et al., Citation2018).
According to the theoretical literature focusing on expressive techniques, these techniques are aimed at helping the patient gain insight into maladaptive interpersonal patterns. Insight can be defined as understanding regarding the associations between components, such as past and present experiences, typical relationship patterns, and the relation between interpersonal challenges, emotional experience, and psychological symptoms (Jennissen et al., Citation2018). Insight is theorized to be strengthened by working through interpersonal patterns of the patient outside the therapy room and within the therapeutic relationship (Gibbons et al., Citation2007). To the best of our knowledge, no research to date focused on the association between expressive techniques and SL alliance. The available literature focused mainly on snapshots of the alliance on specific sessions and thus was not able to shed light on the association between expressive techniques and the development of the alliance from one session to the next, as captured by SL alliance. Yet, the available literature suggests a positive association between the use of expressive techniques and the alliance at specific sessions on treatment. That is, a greater use of expressive techniques was found to be associated with a stronger alliance at those specific sessions (for a review, see Ackerman & Hilsenroth, Citation2003).
The theoretical and several available findings regarding the techniques which are associated with SL alliance strengthening may indicate that both techniques are helpful for everyone, or that some individuals may benefit more from one than the other in enhancing SL alliance strengthening. That is, one size may not fit all, and whereas some individuals may benefit more from a supportive technique to achieve SL alliance strengthening, others may benefit more from expressive techniques. If one size does not fit all, indicating who may benefit from each type of technique for SL alliance strengthening is of critical importance.
One approach to determine who may benefit the most from each type of technique to facilitate SL alliance strengthening is by strength and weaknesses theories (Barber & Muenz, Citation1996; Cheavens et al., Citation2012). When focusing on pretreatment insight level, in supportive treatment, the therapists work with the patients capitalizing on their current level of insight into interpersonal patterns, rather than seeking to improve it. Thus, those individuals with a high level of pretreatment insight may bring such a strength to treatment focusing on supportive techniques. In contrast, in supportive-expressive treatment, the therapists seek to improve the patients’ level of insight into interpersonal patterns through the use of interpretations focusing on interpersonal patterns. Thus, those individuals with a low level of pretreatment insight may benefit from compensating for their weakness.
The present study aims to examine whether one size does not fit all when focusing on techniques to enhance SL alliance strengthening. We hypothesized that, for individuals with higher levels of pretreatment insight, supportive treatment focusing on their strength will be associated with greater SL alliance strengthening. In contrast, for individuals with low levels of pretreatment insight, supportive-expressive treatment focusing on the weakness will be associated with greater SL alliance strengthening.
Method
Study design and procedure
Fifty-five patients with major depressive disorder (MDD) were recruited through advertisements offering free treatment for depression at the psychotherapy research lab clinic. This study is part of a larger randomized controlled trial (RCT; Zilcha-Mano et al., Citation2018). The patients were from the main trial phases and the pilot of the RCT that were enrolled from the point in which the insight measure started to be collected. Individuals who met the inclusion criteria and did not meet the exclusion criteria (see below) received a time-limited psychodynamic treatment which consisted of sixteen therapy sessions of fifty minutes each. Participants were randomly assigned to either a “supportive” treatment condition or a “supportive-expressive” treatment condition (Luborsky, Citation1984; Luborsky et al., Citation1995). Written and oral informed consent was obtained from all participants, and protocols were approved by the Internal Review Board of the institution. Treatments were face-to-face until the start of the pandemic, which resulted in 13 patients being treated remotely ().
Table I. Patient demographic and clinical characteristics as a function of treatment condition.
All participants that were included in the study met the following inclusion criteria: (a) MDD had to be diagnosed according to structured clinical interviews for Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-V), rating above 14 on the 17-item HRSD (Hamilton, Citation1967) at two different evaluation points, one week apart, and current MDD measured with the MINI assessment (MINI International Neuropsychiatric Interview; Sheehan et al., Citation1998); (b) patients on medication must have been on a stable dosage at least the three previous months before entering the study, and consent to maintaining a stable dosage as long as they receive the study’s treatment; (c) age between 18 and 60 years; (d) fluency in the Hebrew language; and (e) providing written informed consent. Exclusion criteria were: (a) current high risk of suicide or self-harm (HRSD suicide item > 2); (b) current substance abuse disorder; (c) current or past schizophrenia or psychosis, bipolar disorder, or severe eating disorders that require medical monitoring; (d) organic mental disease history; and (e) currently receiving psychotherapy.
Treatment conditions
The two treatment conditions of this study were: a supportive treatment condition (ST) or a supportive-expressive treatment condition (SET), which are a time-limited psychodynamic therapy adapted for depression and consisting of 16 fifty-min sessions. The ST included supportive techniques, such as affirmation and empathic validation and the SET included expressive techniques, such as interpretation, confrontation and clarification (Luborsky et al., Citation1995). The SET was based on the manual used by Luborsky et al. (Citation1995). The ST included all the supportive techniques detailed in the manual, but not the expressive techniques (Leibovich et al., Citation2018). Further details about the trial are provided in the trial protocol (Zilcha-Mano et al., Citation2018). All procedures were approved by the institutional review board.
Participants
Demographic and clinical characteristics of the sample are given in .
Therapists
Therapists had at least five years of expertise in psychodynamic psychotherapy. All Therapists received intensive training of 20 hours in supportive and supportive-expressive techniques and participated in both treatment conditions. During the study, therapists were supervised by two supervisors in group supervision and by one of the supervisors in individual supervision. Supervisors were licensed clinical psychologists and had extensive supervision experience. A total of six therapists participated in the study and the mean number of patients treated by each therapist was 16.1 (SD = 8.4), range 5–31.
Measures
Insight measure
An interview administered at baseline was used to assess insight based on the Self-Understanding of Interpersonal Patterns Scales-Interview version (SUIP-I; Gibbons & Crits-Christoph, Citation2017; Yaffe-Herbst et al., Citation2022), which is based on Luborsky’s Core Conflictual Relationship Theme framework (CCRT; Luborsky, Citation1977; Luborsky et al., Citation1990). SUIP-I was face-to-face until the start of the pandemic (COVID-19), which resulted in 13 patients being interviewed remotely using secured software. During the interview, patients are asked to share five interactions about relational exchanges with significant others, which they see as problematic. Structured questions are used to give the patient the opportunity to verbalize their understanding of each interaction without leading the patient. The interviewer evaluates the ability of the patients to recognize, understand and describe their conflictual pattern. Each story is coded along six levels. The first and lowest level evaluates whether there is a basic recognition of the pattern in the specific interaction, while the sixth and highest level evaluates whether the patient is able to think of an alternative way to understand the interaction while it is occurring and whether the patient is able to implement this understanding in a similar interaction. The SUIP-I code is based on a newly developed coding system which consists of Likert scales to evaluate each of the six levels (Yaffe-Herbst et al., Citation2022; the full description of the SUIP-I coding system appears in Table S1 in the Supplements). The total score was calculated as an average of all six levels across the different stories. Higher resulting scores indicate a higher level of insight. The SUIP-I interviewers were graduate students in clinical psychology, who received training and weekly supervision in the administration of the SUIP-I by a PhD student. All interviews were recorded to ensure reliability. The inter-rater reliability of each of the six levels, as evaluated by the agreement between two independent coders, was in the ‘excellent’ range (ICC(1,1) = .91–.97) for all the 6 levels (Portney & Watkins, Citation2009). Internal reliability of the SUIP-I was good (Cronbach’s α = .81, N = 55).
Alliance measure
Alliance was assessed with the Working Alliance Inventory (WAI; Horvath & Greenberg, Citation1989; Tracey & Kokotovic, Citation1989), a 12-item self-report measure, rated on a 7-point Likert scale, designed to evaluate therapeutic alliance. Items are rated from 1 (never) to 7 (always) and the overall score for the therapeutic alliance is obtained from three subscales: agreement on the goals of treatment, agreement on the tasks of treatment, and the affective bond between the patient and therapist. In this study, the patients’ therapeutic alliance was measured after each therapy meeting. The internal reliability range for the WAI throughout the treatment was .91–.96.
Data analysis
Baseline differences between treatment conditions in demographic and clinical characteristics were examined using independent-samples t-tests for continuous variables. Categorical variables were examined using tests of independence or Fisher exact tests by applying 10,000 Monte Carlo simulations.
To test the main hypothesis of the study, data were hierarchically nested, with sessions nested within patients and patients nested within therapists. To account for interdependence, and to prevent inflation of the nonindependence effects (Krull & MacKinnon, Citation2001; Laurenceau & Bolger, Citation2012), SAS PROC MIXED procedure was utilized (Littell et al., Citation2007). We used a model with Level 1 as the session level, Level 2 as the patient level, and Level 3 as the therapist level. Intra-class correlations (ICC) were used to measure the amount of unexplained variance in predicting working alliance (WAI) due to random effects of the therapist and patient.
We examined whether the alliance development throughout treatment has a trend in time (session) (Curran & Bauer, Citation2011). The following trend models were evaluated: without time; with time not including slope as random; with time including slope as random; with linear in log of time not including slope as random; and with linear in log of time including slope as random. We used the log likelihood test and the Bayesian Information Criterion (BIC) to determine whether the inclusion of each term improved the model fit (a table with BICs and AICs of all appears in Table S2 in the Supplements). The model that was found to have the best fit, namely with the lowest BIC and AIC, for the alliance throughout treatment was the model with fixed and random linear in log of time. For each treatment type, the sample was divided according to their insight levels: higher than one standard deviation above average, average, and lower than one standard deviation below average. We introduced alliance development throughout treatment as the dependent variable. The three-way interaction between patient’s pretreatment level of insight, treatment condition (ST vs. SET), and log of time (an equation of the final model can be found in the supplements). The two-way interactions between pretreatment levels of insight with linear in log of time were also used as predictors. As sensitivity analyses, we tested whether findings were replicated when (a) the two dropout cases were removed, and (b) controlled for the mode of delivery (face to face vs. remote). In addition, as part of the sensitivity analysis, we assessed for each treatment type whether the different trajectories of the different insight groups on alliance were significantly different from each other.
We have calculated standardized effect sized for the effects of the main hypothesis analysis, as well as for the effects of the analysis assessing the alliance development throughout treatment. We followed Cohen’s guidelines, according to which the classification for a coefficient β is that effect sizes between 0.10 and 0.29 are small, effect sizes between 0.30 and 0.49 are moderate, and effect sizes of 0.50 or greater are large (Cohen, Citation2013).
Due to the relatively low number of missing observations (2% missing for SUIP-I, 4.6% for the WAI, and none missing for the treatment condition), and the use of multilevel models which can handle missing values under the missing at random assumption (e.g., Gallop & Tasca, Citation2009), we did not conduct any further imputation of missing data outside the multilevel modeling (MLM) models.
Results
Sample characteristics. The patient characteristics by treatment conditions appear in . For the sub-set of individuals included in the present study, no significant differences were found between treatment conditions for any baseline demographic or clinical characteristics.
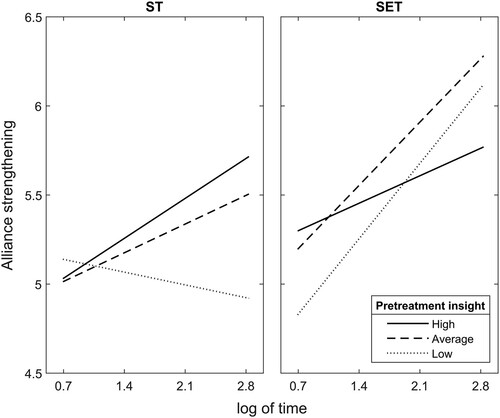
Main analyses. A significant three-way interaction was found between treatment conditions (ST vs. SET), patient’s level of pretreatment insight and time in predicting the alliance development throughout treatment ( = −.67, SE = 0.21, t(828) = −3.23, p = 0.001, CL 95% [−1.08, −0.26], β = −0.33, a moderate effect size; Cohen, Citation2013,
= 0.01). We found that, in each treatment, the two-way interaction was significant (ST:
= 0.45, SE = 0.18, t(828) = 2.48, p = 0.014, CL 95% [0.11, 0.8], β = 0.22, a small effect size,
= 0.01; SET:
= −0.22, SE = 0.11, t(828) = −2.07, p = 0.039, CL 95% [−0.43, −0.001], β = −0.10, a small effect size,
= 0.01).
When the two-way interaction was significant, simple mean analysis was used to reveal the source of significance. In the ST condition, average or higher levels of pretreatment insight significantly predicted the trajectory of alliance development (average level of insight: B = 0.16, SE = 0.07, t(406) = 2.5, p = .01, CL 95% [0.03, 0.29]; average+SD/higher level of insight: B = 0.37, SE = 0.1, t(406) = 3.6, p < .001, CL 95% [0.17, 0.5]), while lower pretreatment insight did not (average-SD/lower level of insight: B = −0.05, SE = 0.11, t(406) = −0.43, p = .67, CL 95% [−0.27, 0.17]). In other words, in ST, alliance improves over time only when patients’ pretreatment insight level is average or above. The higher the patient’s pretreatment insight levels, the more rapidly it strengthens.
In SET, the prediction of the trajectory of alliance development was significant in all levels of pretreatment insight (average-SD/lower level of insight: B = 0.57, SE = 0.07, t(420) = 7.77, p < .001, CL 95% [0.43, 0.72]; average level of insight: B = 0.48, SE = 0.06, t(420) = 8.11, p < .001 CL 95% [0.36, 0.59]; average+SD/higher level of insight: B = 0.38, SE = 0.08, t(420) = 4.79, p < .001, CL 95% [0.22, 0.53]). This indicates that the lower the patient’s pretreatment insight, the more rapidly it strengthens ().
Figure 1. The 3-way interaction between pretreatment insight, treatment condition and time in predicting alliance strengthening. Note. The X axis refers to time operationalized as log of time according to the model. The Y axis refers to strengthening of the alliance (WAI) from one session to the next throughout treatment. The Solid line refers to patients with a high level (average+SD) of pretreatment insight (SUIP-I); the Dashed line refers to patients with an average level of pretreatment insight; and the Dotted line refers to patients with a low level (average–SD) of pretreatment insight. ST = supportive-treatment, SET = supportive-expressive treatment.
Sensitivity analyses. The sensitivity analysis revealed that findings were replicated when the two dropout cases were removed and when controlled for the mode of delivery (see the Supplements for more details). In addition, for each treatment type, all three trajectories were significantly different from each other. Meaning, that different levels of pretreatment insight were associated with different trajectories of alliance development, within each of the two treatments: ST (F(1, 406) = 6.13, p = 0.014) and SET (F(1, 420) = 4.27, p = 0.039).
Discussion
Given the established importance of strengthening the SL alliance, it is important to identify how such strengthening can be accomplished. The current study aimed to investigate whether differences in pretreatment insight level affect SL alliance strengthening differences between ST vs. SET. We tested whether patients with higher pretreatment insight benefit from supportive treatment in strengthening the alliance, with the therapists working to capitalize on the patients’ current level of insight into interpersonal patterns, rather than seeking to improve it (Zilcha-Mano, Citation2020). For patients with lower levels of pretreatment insight, we tested whether they would benefit from supportive-expressive treatment in strengthening the alliance, where therapists seek to improve the patients’ level of insight into interpersonal patterns using interpretations that focus on interpersonal patterns.
The findings suggest that, for individuals receiving ST, those with higher levels of insight show greater SL alliance strengthening, compared to those with lower level of insight, who show less SL alliance strengthening. In ST, the therapist works with the patient from their pretreatment level of insight with which they started treatment. When patients start treatment with higher levels of pretreatment insight, as manifested in better understanding of their interpersonal patterns, they are able to build on these strengths to achieve SL alliance strengthening. Therefore, during treatment, the patient might be better able to develop an effective bond with the therapist and an agreement about the goals and tasks of treatment (Bordin, Citation1979). When patients start treatment with a lower level of pretreatment insight, as manifested in poor understanding of their interpersonal patterns, the result is less SL alliance strengthening. These findings are consistent with previous studies showing an association between supportive techniques and SL alliance strengthening (Leibovich et al., Citation2020; Solomonov et al., Citation2018), but further specify them to identify the subpopulation most likely to benefit from it.
In relation to the SET condition, the findings suggest that those with lower levels of pretreatment insight show greater SL alliance strengthening, while those with higher levels of pretreatment insight show less SL alliance strengthening. In SET, the therapist and patient work on gaining insight into maladaptive interpersonal patterns and expanding the repertoire of responses (RS), such as adding interpersonal responses that are more adaptive and might also be beneficial in the current relationship with the therapist. When the patient starts SET with a lower level of pretreatment insight, as manifested in lower understanding of their interpersonal patterns, they have a potential for additional gaining of insight through the expansion of their repertoire, which results in strengthening the SL alliance. Such gaining of insight allows the patient to facilitate better relationships with the therapist throughout treatment. In contrast, when the patient starts treatment with a higher level of pretreatment insight, as manifested in better understanding of their interpersonal patterns, less SL alliance strengthening occurs. These findings are also consistent with the theoretical literature, according to which the use of expressive techniques is expected to be associated with alliance strengthening. However, they further specify them as attributed to SL alliance strengthening and indicate the subpopulation most likely to benefit from it.
The current study suggests that one size may not fit all and, whereas some individuals may benefit more from a ST to achieve SL alliance strengthening, others may benefit more from SET. Thus, information about the patient’s level of pretreatment insight can be useful in assigning them to the suitable treatment type to strengthen the alliance. For patients with a higher initial level of pretreatment insight, based on the finding, it could be suggested that it might be more beneficial to strengthen the SL alliance through their strength of high pretreatment insight level, such as through ST. As one patient remarked when interviewed at the end of the treatment:
The therapist made me feel like he was seeing me, listening to me and believing in me. During the treatment I was able to realize my abilities and through that I understood that I could get out of the situation.
However, for patients with a lower initial level of pretreatment insight, it could be suggested that it might be more beneficial to strengthen the SL alliance through treatment that focuses on the weakness of their low pretreatment insight level and to choose a treatment, such as SET, that focuses on gaining insight into maladaptive interpersonal patterns. As one patient remarked when interviewed at the end of the treatment:
The therapist helped me understand how I avoid and please others, so they misunderstand my needs. This understanding allowed me to make a positive change in my relationships with others so that they would be more meaningful and supporting, as it was in my relationship with the therapist.
There are some limitations in the current study that should be considered in future research. First, our findings are based on a small sample size and are specific to MDD patients. The validity of our findings, therefore, should be explored in future studies with a larger sample size and other clinical populations. Second, our study does not determine how other individual differences, besides insight, may affect each treatment condition in SL alliance strengthening. Furthermore, only two different treatment conditions were included in the study, and it would be beneficial to investigate how other types of treatment interact with patients’ individual differences. Third, although it is a common practice to use pretreatment characteristics that are assumed to be relatively stable without treatment, such as insight, as capturing TL characteristics of the individual, this trait may also have some inherent dynamics that can be explored in future studies. Finally, an important direction for future studies with larger samples would be to investigate moderated mediation models testing whether the mechanism underlying symptom reduction is greater improvement in insight for individuals with lower levels of insight assigned to SET.
The current study investigates whether pretreatment insight level predicts differences in effects for ST vs. SET on SL alliance strengthening. In ST, for patients with high levels of pretreatment insight, SL alliance can be strengthened through capitalizing on their high insight. Conversely, in SET, for patients with low levels of pretreatment insight, SL alliance can be strengthened by gaining insight into maladaptive interpersonal patterns. Future studies should shed light on the in-session processes contributing to these findings, as well as their immediate and long-term effects on patients’ well-being. If replicated in future research, the present findings may serve as an evidence-based personalized tool for strengthening the alliance.
Supplemental Material
Download MS Word (28.1 KB)Disclosure Statement
No potential conflict of interest was reported by the authors.
Supplemental data
Supplemental data for this article can be accessed here https://doi.org/10.1080/10503307.2023.2189028.
Additional information
Funding
References
- Accurso, E. C., Fitzsimmons-Craft, E. E., Ciao, A., Cao, L., Crosby, R. D., Smith, T. L., Klein, M. H., Mitchell, J. E., Crow, S. J., & Wonderlich, S. A. (2015). Therapeutic alliance in a randomized clinical trial for bulimia nervosa. Journal of Consulting and Clinical Psychology, 83(3), 637. https://doi.org/10.1037/ccp0000021
- Ackerman, S. J., & Hilsenroth, M. J. (2003). A review of therapist characteristics and techniques positively impacting the therapeutic alliance. Clinical Psychology Review, 23(1), 1–33. https://doi.org/10.1016/S0272-7358(02)00146-0
- Barber, P., & Muenz, L. R. (1996). The role of avoidance and obsessiveness in matching patients to cognitive and interpersonal psychotherapy: Empirical findings from the Treatment for Depression Collaborative Research Program. Journal of Consulting and Clinical Psychology, 64(5), 951. https://doi.org/10.1037/0022-006X.64.5.951
- Barber, P., Muran, J. C., McCarthy, K. S., & Keefe, J. R. (2013). Research on dynamic therapies. Bergin and Garfield’s handbook of psychotherapy and behavior change (pp. 443–494).
- Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice, 16(3), 252. https://doi.org/10.1037/h0085885
- Busmann, M., Meyer, A. H., Wrege, J., Lang, U. E., Gaab, J., Walter, M., & Euler, S. (2021). Vulnerable narcissism as beneficial factor for the therapeutic alliance in borderline personality disorder. Clinical Psychology & Psychotherapy, 28(5), 1222–1229. https://doi.org/10.1002/cpp.2570
- Cheavens, J. S., Strunk, D. R., Lazarus, S. A., & Goldstein, L. A. (2012). The compensation and capitalization models: A test of two approaches to individualizing the treatment of depression. Behaviour Research and Therapy, 50(11), 699–706. https://doi.org/10.1016/j.brat.2012.08.002
- Cohen, J. (2013). Statistical power analysis for the behavioral sciences. Routledge.
- Constantino, M., & Smith-Hansen, L. (2008). Patient interpersonal factors and the therapeutic alliance in two treatments for bulimia nervosa. Psychotherapy Research, 18(6), 683–698. https://doi.org/10.1080/10503300802183702
- Curran, P. J., & Bauer, D. J. (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62(1), 583–619. https://doi.org/10.1146/annurev.psych.093008.100356
- Dinger, U., Zilcha-Mano, S., McCarthy, K. S., Barrett, M. S., & Barber, J. P. (2013). Interpersonal problems as predictors of alliance, symptomatic improvement and premature termination in treatment of depression. Journal of Affective Disorders, 151(2), 800–803. https://doi.org/10.1016/j.jad.2013.07.003
- Errázuriz, P., & Zilcha-Mano, S. (2018). In psychotherapy with severe patients discouraging news may be worse than no news: The impact of providing feedback to therapists on psychotherapy outcome, session attendance, and the alliance. Journal of Consulting and Clinical Psychology, 86(2), 125–139. https://doi.org/10.1037/ccp0000277
- Flückiger, C., Del Re, A. C., Wampold, B. E., & Horvath, A. O. (2018). The alliance in adult psychotherapy: A meta-analytic synthesis. Psychotherapy, 55(4), 316–340. https://doi.org/10.1037/pst0000172
- Folmo, E. J., Stänicke, E., Johansen, M. S., Pedersen, G., & Kvarstein, E. H. (2021). Development of therapeutic alliance in mentalization-based treatment – Goals, bonds, and tasks in a specialized treatment for borderline personality disorder. Psychotherapy Research, 31(5), 604–618. https://doi.org/10.1080/10503307.2020.1831097
- Gallop, R., & Tasca, G. A. (2009). Multilevel modeling of longitudinal data for psychotherapy researchers: II. The complexities. Psychotherapy Research, 19(4–5), 438–452. https://doi.org/10.1080/10503300902849475
- Gibbons, M. B. C., Crits-Christoph, P., Barber, J. P., & Schamberger, M. (2007). Insight in Psychotherapy: A Review of Empirical Literature. In L. G. Castonguay & C. Hill (Eds.), Insight in psychotherapy (pp. 143–165). American Psychological Association. https://doi.org/10.1037/11532-007
- Gibbons, M. B. C., & Crits-Christoph, P. (2017). The self-understanding of interpersonal patterns scales-interview version [Unpublished manuscript], University of Pennsylvania, Philadelphia.
- Hamilton. (1967). Development of a rating scale for primary depressive illness. British Journal of Clinical Psychology, 6(4), 278–296. https://doi.org/10.1111/j.2044-8260.1967.tb00530.x
- Hersoug, A. G., Hoglend, P., Havik, O. E., von der Lippe, A., & Monsen, J. T. (2009). Pretreatment patient characteristics related to the level and development of working alliance in long-term psychotherapy. Psychotherapy Research, 19(2), 172–180. https://doi.org/10.1080/10503300802657374
- Horvath, A. O., Del Re, A. C., Flückiger, C., & Symonds, D. (2011). Alliance in individual psychotherapy. Psychotherapy, 48(1), 9. https://doi.org/10.1037/a0022186
- Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36(2), 223. https://doi.org/10.1037/0022-0167.36.2.223
- Jennissen, S., Huber, J., Ehrenthal, J. C., Schauenburg, H., & Dinger, U. (2018). Association between insight and outcome of psychotherapy: Systematic review and meta-analysis. The American Journal of Psychiatry, 175(10), 961–969. https://doi.org/10.1176/appi.ajp.2018.17080847
- Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3(1), 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432
- Krull, J. L., & MacKinnon, D. P. (2001). Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research, 36(2), 249–277. https://doi.org/10.1207/S15327906MBR3602_06
- Laurenceau, J.-P., & Bolger, N. (2012). Analyzing diary and intensive longitudinal data from dyads. In M. Csikszentmihalyi (Ed.), Handbook of research methods for studying daily life (pp. 407–422). Guilford Press.
- Leibovich, L., McCarthy, K. S., & Zilcha-Mano, S. (2020). How do supportive techniques bring about therapeutic change: The role of therapeutic alliance as a potential mediator. Psychotherapy, 57(2), 151. https://doi.org/10.1037/pst0000253
- Leibovich, L., Nof, A., Auerbach-Barber, S., & Zilcha-Mano, S. (2018). A practical clinical suggestion for strengthening the alliance based on a supportive–expressive framework. Psychotherapy, 55(3), 231. https://doi.org/10.1037/pst0000195
- Littell, R. C., Milliken, G. A., Stroup, W. W., Wolfinger, R. D., & Schabenberger, O. (2007). Textbook. SAS for mixed models. SAS Institute.
- Luborsky, L. (1977). Measuring a pervasive psychic structure in psychotherapy: The core conflictual relationship theme. In Norbert Freedman & Stanley Grand (Eds.), Communicative structures and psychic structures (pp. 367–395). Springer.
- Luborsky, L. (1984). Principles of psychoanalytic psychotherapy: A manual for supportive-expressive treatment (Issue 616.8917 L8). Basic Books.
- Luborsky, L., Barber, J. P., & Crits-Christoph, P. (1990). Theory-based research for understanding the process of dynamic psychotherapy. Journal of Consulting and Clinical Psychology, 58(3), 281–287. https://doi.org/10.1037/0022-006X.58.3.281
- Luborsky, L., Mark, D., Hole, A. V., Popp, C., Goldsmith, B., & Cacciola, J. (1995). Supportive-expressive dynamic psychotherapy of depression: A time-limited version.
- Manne, S. L., Kashy, D. A., Rubin, S., Hernandez, E., & Bergman, C. (2012). Therapist and patient perceptions of alliance and progress in psychological therapy for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology, 80(5), 800. https://doi.org/10.1037/a0029158
- McClintock, A. S., Perlman, M. R., McCarrick, S. M., Anderson, T., & Himawan, L. (2017). Enhancing psychotherapy process with common factors feedback: A randomized, clinical trial. Journal of Counseling Psychology, 64(3), 247. https://doi.org/10.1037/cou0000188
- Ollila, P., Knekt, P., Heinonen, E., & Lindfors, O. (2016). Patients’ pre-treatment interpersonal problems as predictors of therapeutic alliance in long-term psychodynamic psychotherapy. Psychiatry Research, 241, 110–117. https://doi.org/10.1016/j.psychres.2016.04.093
- Penzenstadler, L., Kolly, S., Rothen, S., Khazaal, Y., & Kramer, U. (2018). Effects of substance use disorder on treatment process and outcome in a ten-session psychiatric treatment for borderline personality disorder. Substance Abuse Treatment, Prevention, and Policy, 13(1), 1–11. https://doi.org/10.1186/s13011-018-0145-6
- Portney, L. G., & Watkins, M. P. (2009). Foundations of clinical research: applications to practice (Vol. 892). Pearson.
- She, Z., Duncan, B. L., Reese, R. J., Sun, Q., Shi, Y., Jiang, G., Wu, C., & Clements, A. L. (2018). Client feedback in China: A randomized clinical trial in a college counseling center. Journal of Counseling Psychology, 65(6), 727. https://doi.org/10.1037/cou0000300
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(20), 22–33.
- Solomonov, N., McCarthy, K. S., Keefe, J. R., Gorman, B. S., Blanchard, M., & Barber, J. P. (2018). Fluctuations in alliance and use of techniques over time: A bidirectional relation between use of “common factors” techniques and the development of the working alliance. Clinical Psychology & Psychotherapy, 25(1), 102–111. https://doi.org/10.1002/cpp.2143
- Stenius, J., Knekt, P., Heinonen, E., Holma, J., Antikainen, R., & Lindfors, O. (2021). Predicting the working alliance over the course of long-term psychodynamic psychotherapy with the Rorschach Ego Impairment Index, self-reported defense style, and performance-based intelligence: An evaluation of three methodological approaches. Psychoanalytic Psychology, 38(1), 58. https://doi.org/10.1037/pap0000318
- Tasca, G. A., Balfour, L., Ritchie, K., & Bissada, H. (2007). The relationship between attachment scales and group therapy alliance growth differs by treatment type for women with binge-eating disorder. Group Dynamics: Theory, Research, and Practice, 11(1), 1. https://doi.org/10.1037/1089-2699.11.1.1
- Tracey, T. J., & Kokotovic, A. M. (1989). Factor structure of the working alliance inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1(3), 207. https://doi.org/10.1037/1040-3590.1.3.207
- Tzur Bitan, D., Kivity, Y., Ganor, O., Biran, L., Grossman-Giron, A., & Bloch, Y. (2020). The effect of process and outcome feedback in highly distressed outpatients: A randomized controlled trial. Psychotherapy Research, 30(3), 325–336. https://doi.org/10.1080/10503307.2019.1627014
- Yaffe-Herbst, L., Joffe, M., Peysachov, G., Nof, A., Gibbons, M. B. C., Crits-Christoph, P., & Zilcha-Mano, S. (2022). The development of a comprehensive coding system for evaluating insight based on a clinical interview: The SUIP-I coding system [revise and resubmit].
- Zilcha-Mano, S. (2017). Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. American Psychologist, 72(4), 311. https://doi.org/10.1037/a0040435
- Zilcha-Mano, S. (2020). Toward personalized psychotherapy: The importance of the trait-like/state-like distinction for facilitating therapeutic change.
- Zilcha-Mano, S., Dinger, U., McCarthy, K. S., & Barber, J. P. (2014). Does alliance predict symptoms throughout treatment, or is it the other way around? Journal of Consulting and Clinical Psychology, 82(6), 931. https://doi.org/10.1037/a0035141
- Zilcha-Mano, S., Dolev, T., Leibovich, L., & Barber, J. P. (2018). Identifying the most suitable treatment for depression based on patients’ attachment: Study protocol for a randomized controlled trial of supportive-expressive vs. supportive treatments. BMC Psychiatry, 18(1), 1–9. https://doi.org/10.1186/s12888-018-1934-1
- Zilcha-Mano, S., & Fisher, H. (2022). Distinct roles of state-like and trait-like patient–therapist alliance in psychotherapy. Nature Reviews Psychology, 1(4), 194–210. https://doi.org/10.1038/s44159-022-00029-z
