?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Frequent attenders in primary care (FAs) consume a disproportionate amount of healthcare resources and often have depression, anxiety, chronic health issues, and interpersonal problems. Despite extensive medical care, they remain dissatisfied with the care and report no improvement in quality of life.
Objective
To pilot a Telephone-based Interpersonal Counseling intervention for Frequent Attenders (TIPC-FA) and assess its feasibility and efficacy in reducing symptoms and healthcare utilization.
Method
Top 10% of primary care visitors were randomly assigned to TIPC-FA, Telephone Supportive Contact (Support), or Treatment as Usual (TAU). TIPC-FA and Support groups received six telephone sessions over twelve weeks, while the TAU group was interviewed twice. Multilevel regression tested for changes over time, considering patient and counselor variance.
Results
TIPC-FA and Support groups demonstrated reduced depressive symptoms, and the TIPC-FA group showed decreased somatization and anxiety. The TIPC-FA group demonstrated a trend towards less healthcare utilization than the TAU group.
Conclusion
This pilot study suggests that IPC via telephone outreach is a feasible approach to treating FAs, achieving a reduction in symptoms not seen in other groups. Promising reduction in healthcare utilization in the TIPC-FA group warrants further exploration in larger-scale trials.
Clinical or methodological significance of this article: The results of this pilot study suggest that Telephone-based Interpersonal Counseling intervention for Frequent Attenders (TIPC-FA) may be a feasible and effective approach to reducing symptoms of depression, anxiety, and somatization in primary care patients. The trend towards less healthcare utilization in the TIPC-FA group also suggests a potential benefit in reducing healthcare costs. However, further research is necessary to confirm these findings and explore the long-term impact of TIPC-FA on patient outcomes and healthcare utilization.
Introduction
Frequent attenders (FAs) represent a significant portion of primary care visits, accounting for 20-30% of all visits (LaCalle & Rabin, Citation2010) and ranking among the top 10% of patients in terms of visit frequency (Shukla et al., Citation2020). Despite receiving medical treatment, FAs tend to suffer for prolonged periods (Kivelä et al., Citation2018; Matalon et al., Citation2009), which puts pressure on limited medical resources. Additionally, FAs consume 67% of medical expenses regardless of socio-economic class (Hammerman et al., Citation2021; Vedsted et al., Citation2002; Vedsted & Olesen, Citation2005; Wammes et al., Citation2018) and are more likely to receive a disability pension (Reho et al., Citation2021). These findings highlight the urgent need to address the underlying issues that lead to frequent attendance.
Notably, FAs also report higher levels of psychological distress, particularly in the form of depression and anxiety (Dowrick et al., Citation2000; Gili et al., Citation2011; Given et al., Citation2005; Kapur et al., Citation2004; Kersnik et al., Citation2001; Patel et al., Citation2015; Ronalds et al., Citation2002; Wyke et al., Citation2003). Although FAs tend to have more physical issues than other patients (LaCalle & Rabin, Citation2010), these differences are inconsistent and do not account for the excessive use of healthcare resources (Foster et al., Citation2006; Smits et al., Citation2013). As a result, a growing body of research has aimed to reduce medical visits by identifying and addressing the underlying psychological issues that drive frequent attendance. Some studies have screened FAs for psychological issues and provided medication or counseling, leading to improvements in mental health but no significant decrease in primary care visits (Barsky et al., Citation2013; Rasmussen et al., Citation2006; Simon et al., Citation2001).
However, this approach neglects the multifaceted factors that contribute to consistent attendance. For example, research suggests that FAs tend to place greater value on their physician visits than other patients (Huhtakangas et al., Citation2021; Sledge et al., Citation2011), and may prioritize discussing psychological and social issues over medical issues during these visits (Andersson et al., Citation1995). Furthermore, FAs may have more interpersonal issues than other patients, such as insecure or preoccupied attachment patterns styles (Taylor et al., Citation2000, Citation2012; Thompson & Ciechanowski, Citation2003), and may have poorer social functioning and support networks(Bellón et al., Citation1999; Patel et al., Citation2015; Scaife et al., Citation2000; Vedsted & Olesen, Citation2005). These findings suggest that addressing the relational and psychological issues contributing to frequent attendance may be more effective in reducing healthcare utilization among FAs (Stuart & Noyes, Citation2006).
For this purpose, we explored Interpersonal Counseling (IPC), a brief and adaptive mental health treatment (Weissman et al., Citation2014). IPC is based on Interpersonal Psychotherapy (IPT), which was created to treat depression by Klerman, Weissman, and colleagues (Citation1984). Numerous research has looked into the efficacy of IPT, particularly for depression [see Van Hees et al. (Citation2013) for a review, and Cuijpers et al. (Citation2016) for a meta-analysis], but also for a variety of other illnesses (Allan et al., Citation2016; Bernecker et al., Citation2017; Ravitz et al., Citation2019).
For this patient population and setting, IPC appears to be a suitable fit: IPC was developed for non-professionals in primary care (Klerman et al., Citation1987) and is shorter than IPT [six sessions in early editions, three sessions in later versions (Weissman & Verdeli, Citation2012)]. Though not as extensively tested as IPT, many studies have successfully utilized IPC in various settings and conditions (Menchetti et al., Citation2010; Neugebauer et al., Citation2007; Rafaeli et al., Citation2021; Yamamoto et al., Citation2018).
Telephone Interpersonal Counseling for Frequent Attenders (TIPC-FA)
Several critical changes were needed to adapt IPC to the unique challenges of FAs, resulting in the modified protocol for Telephone-based Interpersonal Counseling for Frequent Attenders used in the current study (TIPC-FA). One of these modifications was to assign patients a flexible “sick role” not predefined (e.g., depression, frequent attendance) but instead generated by the patient's current life struggles. Another significant change was the substitution of a referral of patients to counselors [in which patients may feel “rejected” by the referee due to attachment insecurities that characterize them (Thompson & Ciechanowski, Citation2003; Waller et al., Citation2004)] with a two-step outreach process in which counselors first outreached to patients and only after establishing a primary relationship with them offer them the intervention, inside the relationship.
Furthermore, as noted previously, another significant difference between traditional IPC and TIPC-FA was that it was delivered over the phone, making FA treatment more accessible than seeing a therapist in person. Furthermore, because FAs seek medical treatment rather than mental health counseling, a counseling intervention may feel unusual, even intimidating, or as further invalidation of their concerns. Because telephone conversations do not always resemble the typical “counseling session” that a patient might expect, refusals to participate in counseling may be overlooked. Telephone-based psychological therapies have been widely and successfully used in various health and mental health settings in recent years, producing results that are often comparable to face-to-face interventions (Castro et al., Citation2020; Irvine et al., Citation2020).
The present study
TIPC-FA was compared to unstructured supportive contact (Support) and treatment as usual (TAU) in a randomized trial to assess IPC's feasibility and preliminary efficacy for FAs. We included a supportive contact group to assess the role of interpersonal intervention beyond simple personal contact with counselors on unstructured topics.
The study's hypotheses were as follows:
The TIPC-FA intervention would be acceptable to patients and feasible to implement in this population if delivered in the stepped-outreach manner proposed here.
The two intervention groups would exhibit symptom reduction and quality of life gains that the control group would not, with the TIPC-FA group outperforming the TAU group.
Participants in the TIPC-FA group will have lower primary care attendance following the intervention, whereas no such change will be seen in the TAU or support groups.
Method
Study Design, Therapists, and Setting
This study was a randomized multi-arm design, with participants randomly assigned to one of three parallel groups (1:1:1 ratio).
Participants and setting
All adults in Israel aged 21–70 registered with a large public health care provider and had a primary care visit frequency in the top 10% in 2010 were eligible. No exclusion criteria were used. Between February and July 2012, all patients were contacted by phone (no face-to-face contact was made).
Interventions
TIPC-FA
The intervention was based on the IPC protocol (Weissman & Klerman, Citation1993), with modifications to make it more suitable for FAs patients. The counseling process is divided into three stages, according to the framework of interpersonal psychotherapy: the initial phase, the intermediate phase, and the termination phase. In the current configuration, the initial and termination phases were each one session long, with the remainder constituting the intermediate phase. In the initial phase of IPC, counselors choose, together with patients, one of four interpersonal problem areas that serve as the primary focus for treatment (Klerman et al., Citation1984): Grief, role transition, role dispute, or interpersonal deficit. Focusing on a specific interpersonal problem area facilitates symptom reduction by activating four essential change mechanisms (Lipsitz & Markowitz, Citation2013): expressing emotions and learning better interpersonal skills to help resolve the problem in the chosen interpersonal domain; in turn, resolving an interpersonal problem increases the availability of social support and decreases interpersonal stress related to the problem; both factors are related to better mental and physical health.
A necessary modification to the protocol that made it more suitable for FAs was related to their problem definition. The “pathology,” or most noticeable “symptom,” of FAs is their maladaptive care-seeking behavior and difficulty recognizing this behavior as problematic. As a result, it is impossible to create a standard IPT formulation in which patients are educated about their disorder and assigned to the transitional “sick role,” designed to temporarily alleviate the responsibility and shame associated with current difficulties and malfunctioning (Stuart & Robertson, Citation2003). In addition, FAs have a wide range of medical and psychological symptoms. As a result, no single condition could be identified and presented as the “problem domain” for all patients. As an alternative to the diagnosis-focused problem, the TIPC-FA-defined problem was tailored based on the problem(s) most apparent in the initial evaluation (e.g., fatigue, malaise, pain complaints, irritation, inactivity, or low quality of life). After identifying the specific problem that is now the patient's “diagnosis,” the counselor will present a formulation explaining the relationship between interpersonal difficulties and problems in general, without explicitly discussing their specific condition, followed by explaining the patient's problem using the interpersonal model through a specific interpersonal problem area. After the problem is specified and an interpersonal domain is selected, the treatment plan can be identical to standard IPT/IPC.
Support
The support group was a “pseudo-placebo” group in which no specific therapy factors were included (Wampold & Imel, Citation2015). The sessions were unstructured, with no set topic or theme. Counselors were told to let the patients lead the dialogue during each session without supervision or interpretation. Just attentive listening and empathy were allowed.
Measures
Demographic factors
The age and gender of the patients were obtained from the healthcare provider's database. The initial interview also included questions about the birth country (to ascertain immigration status) and marital status.
Health and mental health
Data from the health care provider's database were retrieved in 2010 for three primary chronic health conditions (Diabetes, heart conditions, and chronic high blood pressure) and the purchase of psychiatrically labeled drugs (antidepressants, hypnotics/sedatives/anxiolytics, and antipsychotics).
Psychiatric symptoms
Symptoms were measured using the widely used Patient Health Questionnaire (PHQ-SADS; Kroenke et al., Citation2010), a combined brief measure of Depression, Somatization, and Anxiety. Internal reliability for the various scales was α = 0.88, α = 0.82, and α = 0.88, respectively.
Quality of life
The Quality of Life Scale (QoLS; Flanagan, Citation1978) assessed satisfaction levels in several life categories. Prior studies indicated that this measure had adequate reliability and validity (Burckhardt & Anderson, Citation2003). In the current sample, α = 0.895 for the total scale.
Healthcare utilization
During January 2013, data on healthcare utilization were obtained from medical records for all participants, regardless of participation status. The latter allowed for varying lengths of follow-up for participants, with some receiving up to 9 months. The data included monthly counts of primary care visits and monthly expenses for doctor visits, hospitalizations, and ambulatory expenses [in New Israeli Shekels (NIS)].
Procedure
The study was approved by the Soroka Hospital Helsinki Committee. In all processes, the CONSORT statement was used (Montgomery et al., Citation2018). As we did not have direct access to the data source, a list of FA patients who met the inclusion criteria was drawn randomly from the healthcare provider's database by their data analyst. The patients’ first names and phone numbers are the only information on the list. The first author used an Excell application to generate random numbers (1,2, 3, in balance) and assigned them to each patient on the list of patients provided. Because the interviewers conducting the initial interviews with patients were to become their counselors later, the patients had to be assigned to a group before any contact was made with them. As a result, the group assignment was not hidden from any of the counselors or interviewers. Because not all of the patients on our list had adequate contact information or could not be reached for other reasons, they were excluded from the study (n = 72).
This study used a phased “outreach approach,” recognizing the necessity of avoiding the intervention referral process. Consequently, rather than having FAs initiate contact with therapists after being referred, therapists initiate communication with them.
Initial interview
All patients with whom telephone contact was established were invited to participate in a telephone-based survey of mental health and quality of life, for which consent was given orally. A telephone interview was conducted for consenting patients, with the interviewers instructed to conduct it “in an empathetic manner” to establish a primary relationship with their interviewees during the interview and leverage this fundamental relationship to continue telephone sessions.
Invitation to take part in the intervention
Following the initial interview (on the same phone call), interviewers in the TIPC-FA and Support groups mentioned the treatment program, offering their interviewees the opportunity to continue telephone communication with their interviewers for six more sessions over the next 12 weeks and the next telephone session was then scheduled with consenting patients as the intervention's first session. Patients in the Control group were asked to consent to be interviewed again twelve weeks later.
Intervention
The TIPC-FA and support groups included six 30-minute phone calls spaced out over twelve weeks (four weekly sessions, then two bi-weekly sessions).
Counselors
The counselors were ten Ben-Gurion University third-year bachelor of psychology students who had completed psychopathology and theories of personality courses. Participants received a series of lectures from the last author about the treatment to be administered. Weekly group supervision meetings were held (by the first and last authors) separately for TIPC-FA counselors and Support counselors. Furthermore, the first author provided personalized supervision in biweekly meetings lasting 30 min to one hour.
Final interview
Patients in all groups were called again 12 weeks after the initial contact to be re-interviewed by an interviewer (other than the one who counseled them).
Statistical analysis
Scale scores
The study measured quantitative scale scores for depression, anxiety, somatization, and quality of life at two different time points: once during the initial interview before the intervention and again during a follow-up interview one week after the last intervention session (12 weeks later). The initial and final interviews for the control group where these scale scores were collected were also 12 weeks apart.
We utilized multilevel linear regression (ML) to examine the outcome measures, accounting for the nested structure of the data. The time points (x2) were positioned on Level 1, nested within subjects on Level 2, and counselors/interviewers on Level 3. Due to the limited number of observations, we only used random intercepts and did not apply a random slope and intercept model for all measures. We tested the Time x group interaction to identify any variations between groups in the change from the pre- to post-intervention period. The Group was treated as a Level 2 variable, given that counselors worked across groups. We used dummy coding to treat “Groups” as a categorical variable, with the TAU group as the reference category and being compared separately to the TIPC-FA and the Support group. The dummy coding was reversed so that the interaction term could also be tested for the difference between the Support and TIPC-FA groups. Any significant interactions that arose were further investigated through a simple slope analysis. Equations for these 3-level models are provided in Appendix A.
Health care utilization
Analysis of utilization scores was performed using Multilevel Linear Regression (ML), with monthly time points beginning a month before the intervention and follow-up until eight months after the intervention in Level 1, nested within subjects on Level 2, and interviewers/therapists at Level 3. Since healthcare utilization variables were all positively skewed, these variables were log-transformed before entering regression equations, and results were interpreted accordingly [as exponentiated Relative Risk (RR)].
An unconditional model examining variance partition among the three levels of analyses showed that none of the variance in primary care visits was attributed to differences among therapists. Therefore, nesting within therapists was not included in the final ML equation. In the final model, the Group was a Level 2 variable. We tested the Time x Group interaction to detect differences in monthly rates of change in the number of visits from the fourth month after the intervention. Equations for these 2-level models are provided in Appendix B.
We performed a separate extra analysis for the log visits to primary care variable, just for the period of 3 months before intervention up to 8 months after intervention initiation, to try and detect other differences in the specific outcome that was of interest in this study, using the same ML model.
Results
Sample Characteristics
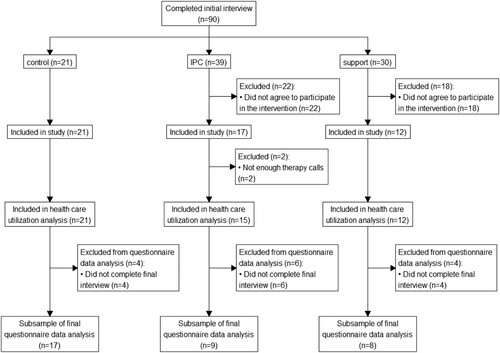
We received from the healthcare provider a random sample of n = 369 FAs. n = 207 refused to take part in the initial interview. Therefore, the final sample included n = 90 patients who completed the interview (n = 21 in the TAU group, n = 39 in the TIPC-FA group, and n = 30 in the support group). N = 2 patients in the TIPC-FA did not complete at least two counseling calls and were therefore removed from the analysis. The remaining patients were all included in the analysis of healthcare utilization. Some patients were lost to the follow-up interview, so a second measurement of the scale scores was missing. The sample for analysis of scale measurements included n = 17, n = 9, and n = 8 patients in the TAU, TIPC-FA, and support group, respectively. See for complete details.
Characteristics of the sample analyzed for healthcare utilization are presented in . The total sample consisted mainly of men (56.2%), with a mean age of 56.3 years (SD = 10.5). There were no significant differences between groups on any pre-intervention demographic or other variables, except for the rates of Diabetes, which were slightly lower in the TIPC-FA group (p = .036).
Table I. Baseline characteristics of the sample.
Treatment Effectiveness
Psychiatric symptoms and quality of life
Means and standard errors of the different scores in different groups are presented in . Unconditional models examining variance partitioning across the three levels of analyses revealed that differences in depression, anxiety, somatization, and QoL scores were attributed to differences between counselors (ICC = 0.16, ICC = 0.19, ICC = 0.22, and ICC = 0.2, respectively) as well as differences between participants (ICC = 0.66, ICC = 0.44, ICC = 0.61, and ICC = 0.65). As a result, nesting within therapists was incorporated into the ML equation. The results of the MLM analysis, including all levels, are presented in .
Table II. Comparison of scale scores before and after the intervention in the different groups.
Table III. Results of the multilevel model predicting scale scores from group and time.
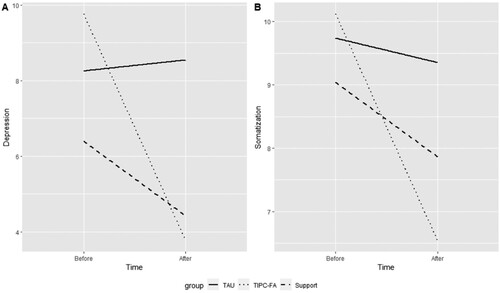
There were no main effects for Group in any scale scores, nor were there any group differences in the pre-intervention or post-intervention scores. There was a significant main effect for Time for depression (b = −2.31, t(29) = −2.95, p = .006), anxiety (b = −1.96, t(30) = −2.08, p = .046), and somatization (b = −1.66, t(30) = −2.56, p = .016), indicating a reduction in symptoms above and beyond group membership.
The interaction between Time and Group (TIPC-FA vs. TAU) was significant only for depression (b = −4.38, t(29) = −2.37, p = .024) and somatization (b = −3.42, t(30) = −2.28, p = .03), but not for anxiety or QoL. The interactions between Time and Group (Support vs. TAU) and Time and Group (TIPC-FA vs. Support) were insignificant for any scale scores.
Probing the significant interaction for depression revealed a significant simple slope for Time in the TIPC-FA group (b = −4.10, t(29) = 2.66, p = .013) that was not present in the TAU group (b = −0.28, t(29) = −0.27, p = .787).
For the significant interaction found for somatization, simple effects analysis showed a significant reduction in the TIPC-FA group (b = 3.35, t(30) = 2.73, p = .011) that was not present in the TAU group (b = −0.1, t(30) = −0.08, p = .937 for somatization).
Further exploratory analysis
Although most interaction effects were insignificant and did not reveal a difference in slopes between groups, exploratory simple slopes analyses were performed for the effect of time in all groups and for all measures separately to detect trends. These are also presented in .
An exploratory simple slopes analysis revealed a significant decrease in depression over time in the Support group (b = −3.11, t(29) = −2.14, p = .041), as well as a significant decrease in anxiety in the TIPC-FA group (b = 4.62, t(30) = 2.6, p = .014), which was not found in the TAU or Support groups. However, as previously stated, the difference between slopes across groups were minor due to insignificant interactions.
illustrates the significant interactions.
Health Care Utilization
One month prior to the intervention, into the eight months follow-up
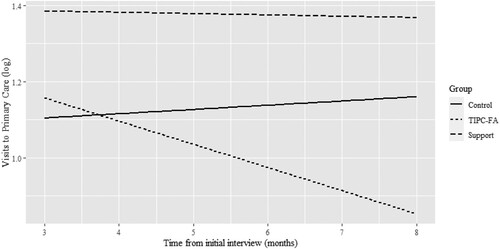
The Group x time interaction was significant only when comparing the TIPC-FA and TAU groups for the Log of Total Expenses (b = −0.1, p = .013) and Log of Visit Expenses (b = −0.1, p = .047). Simple slopes analysis for log total expenses revealed a significant increase in the control group (RR = 1.07, 95%CI[1.01,1.13], p = .025) but no change in the IPC or support groups, indicating a monthly increase in the control group but not in the treatment groups. A simple slopes analysis of log visits expenses revealed a similar pattern, with a marginally significant increase in the control group (RR = 1.08, 95%CI[1.1,1.16], p = .054) and no significant change in the other groups. An exploratory simple slopes analysis for non-significant interaction revealed a significant decrease in the IPC group only for the log of expenses related to hospitalizations (RR = 0.84, 95%CI[0.71,1], p = .049). shows the specific changes in each Group.
Table 4. Mixed model results predicting change in health care utilization by time and group.
Follow-up (3–8 months from the beginning of the intervention)
The Time x Group interaction was significant when comparing the TIPC-FA group to the Control (b = −0.35, p = .041) but not when comparing Support to the Control (b = −0.13, p = .415). The Control group had a significant increase in visit rates (RR = 1.22, 95% CI [1.01, 1.48], p = .045), while the TIPC-FA group had a non-significant decrease (RR = 0.86, 95% CI [0.66, 1.12], p = .272) and the Support group had no change (RR = 1.07, 95% CI [0.83, 1.38], p = .608). The outcomes are depicted in .
Acceptability and Feasibility
The study enrolled n = 21, n = 39, and n = 30 participants from the TAU, TIPC-FA, and Support groups who completed the initial interview and were offered the intervention in the active groups. Among the patients offered treatment in the TIPC-FA group, 38% (n = 15) agreed to participate and completed at least two sessions, and 23% (n = 9) completed all sessions and the follow-up interview. In the Support group, 40% (n = 12) of patients agreed to participate and completed at least two sessions, while 27% (n = 8) completed all sessions and the follow-up interview.
Discussion
We developed TIPC-FA, a version of IPC adapted to suit the unique needs of individuals with FAs, given the significant interpersonal characteristics of this population and the potential for interpersonal aspects in their medical care. Our study compared the feasibility and preliminary effectiveness of TIPC-FA to an unstructured, non-therapeutic supportive contact (Support) and treatment as usual (TAU) in a small randomized controlled trial. The study had several objectives, including evaluating the applicability of TIPC-FA among individuals with FAs, comparing its effectiveness and tolerability to the two control groups, and investigating whether it could serve as a valuable alternative to the standard treatment as usual for this population.
The results of our study indicate that it is possible to engage individuals with FAs in a rigorously controlled study, although it can be challenging. Despite being initially guarded, many FAs established a meaningful rapport with their interviewers over the phone. Approximately 40% agreed to participate in brief counseling, with a reasonable portion completing the recommended six telephone sessions. Notably, individuals with FAs are known to reject psychological explanations for their physical complaints and decline referrals to mental health professionals (Karlsson et al., Citation1995). Therefore, the consent rate achieved in our study is considered acceptable and not low.
In terms of efficacy, our preliminary study yielded promising results. We observed a significant reduction in depression and somatization in the TIPC-FA group, which was not evident in the TAU group. Moreover, the exploratory analysis found a trend for reducing anxiety symptoms in the TIPC-FA group and reducing depressive symptoms in the Support group. None of those were found in the TAU group.
Furthermore, we discovered several significant differences between groups regarding visits to primary care physicians and related expenses. In general, we discovered a slight increase in visits and visit-related expenses in the TAU group that was not seen in the TIPC-FA or Support groups, as well as a non-significant trend for a decrease in those expenses and visits in the TIPC-FA group. During the follow-up period, a distinct difference between groups was discovered, with increased visits observed in the control group but not in the TIPC-FA or Support groups.
These findings add to the growing body of evidence supporting the efficacy of IPT/IPC in reducing levels of psychopathology (Bernecker et al., Citation2017; Rafaeli et al., Citation2021; Stuart & Robertson, Citation2003; Yamamoto et al., Citation2018) and extend it to the unique context of frequent attendance at primary care.
Our study's results provide evidence that the TIPC-FA group showed greater improvements compared to both the Support and TAU groups. While there were some improvements in the Support group, they were more limited, suggesting that while basic human contact may be important, the specific techniques and formulation incorporated in TIPC-FA played a crucial role in the observed improvements. The IPT framework's focus on current interpersonal problems in the patient's life and either resolving them or changing one's perspective towards them is a suggested factor associated with this change (Lipsitz & Markowitz, Citation2013). By addressing interpersonal stress and enhancing social support, the TIPC-FA group experienced significant reductions in depression, somatization, and potentially anxiety symptoms, as well as a potential change in visits and related expenses to primary care physicians.
Given the well-established finding of lower interpersonal functioning and social support among FAs (e.g., Vedsted & Olesen, Citation2005) and their unmet attachment needs (Hunter & Maunder, Citation2001), the TIPC-FA's unique approach of focusing on interpersonal problems and helping patients to gain a new perspective may be particularly beneficial.
In that regard, it is worth noting that throughout the study, counselors consistently expressed clinical impressions that patients were largely unaware of the link between interpersonal problems and distress. Patients were initially skeptical when therapists suggested solutions such as contacting family members, resolving disputes, and challenging assumptions and expectations from their surroundings. On the other hand, patients in the TIPC-FA group had the opportunity to explore and experiment with these ideas throughout the intervention. Some were surprised to discover they could openly discuss and resolve painful interpersonal conflicts.
Furthermore, the differences between contact alone (i.e., Support group) and implementation of a specific formulation and technique (i.e., TIPC-FA) are even more intriguing when FAs are already de facto seeing their physicians on average once a week; in other words, FAs are already engaging in human contact regularly, but with no relief. As a result, it appears that when there is a meaningful therapeutic factor, as in the TIPC-FA treatment group, rather than merely social interaction, it may further contribute to FAs and can even make a meaningful difference in patients’ lives.
The one-of-a-kind, stepwise outreach procedure utilized in this study provides a significant advantage in practicability. It has been demonstrated that the conventional method of discussing therapy is ineffective when dealing with FAs. As was previously stated, patients referred to another person may experience feelings of rejection at the hands of that person (Bursztajn & Barsky, Citation1985). There is significant potential in forming a relationship first and only then introducing a therapeutic process within the context of this relationship. However, this intriguing aspect calls for additional research, not only as part of this particular program of TIPC-FA but also in the general approach to dealing with FAs with case managers, nurses, and other paramedical professionals involved in their care.
Taken as a whole, the strength of this study lies in the novel approach used to treat a distinct group of patients who are suffering without relief and are known to refuse psychological treatment for their physical complaints.
Limitations
The primary limitation of this study is the small sample size, which stems from the preliminary nature of the study, limited resources, and difficulty in recruiting participants. Because of the small number of participants, the study was ultimately underpowered; as previously discussed, some results were insignificant. More research with larger samples and a longer-term follow-up is needed to determine whether the potential effects of the intervention are sustained or only become apparent after a long time. The small sample size and the relatively large number of counselors contribute to significant variation in treatment delivery. Second, while the counselor effects were considered in the analysis, no measure of adherence was implemented; thus, further evaluation of counselors’ adherence to the model should be considered in future research.
Furthermore, there were no measurements of change or process mechanisms because the current feasibility study was so limited. As a result, our assumptions that the difference between the support and TIPC-FA groups is due to specific techniques or formulations used only in the TIPC-FA group remain speculative. Future research would benefit from measures to evaluate purported mechanisms of change. These could be IPT-hypothesized change mechanisms like emotional expression, interpersonal skills, social support, and interpersonal stress, or processes like the therapeutic alliance.
Conclusions
To the best of our knowledge, this is the first study to attempt and report on a feasibility and efficacy study using an RCT design involving a new IPC intervention on this population—FAs to primary care. TIPC-FA is only six sessions long and can be delivered by non-expert clinicians over the phone, making it potentially appropriate for FAs. The preliminary evidence from this trial suggests that larger trials in a more controlled environment, testing counselor adherence and the mechanisms of change involved, are needed to confirm these initial findings. Despite the limitations discussed, the tentative results of this study demonstrated the potential of TIPC-FA intervention in reducing psychological distress and medical service misutilization among FAs.
The findings provisionally support the use of psychological interventions, specifically an interpersonal-relational model for FAs (e.g., Barsky, Citation1996; Bowlby, Citation1969; Simon et al., Citation2001; Sullivan, Citation1953), as well as the unique outreach approach used in this study. TIPC-FA appears acceptable to FAs; therefore, this approach warrants further investigation with this patient population. This may be especially important given the population's unique characteristics, namely the need for interpersonal relationships and a lack of knowledge or personal resources to obtain psychological assistance. Our findings also tentatively suggest that other interventions for this population could benefit from addressing interpersonal needs and challenges through formal counseling or as part of the medical system's more integrated approach.
Acknowledgements
The study was conducted with the contribution of Maccabi Health Services, which provided access to patient data and assisted in analyses.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
References
- Allan, B. A., Campos, I. D., & Wimberley, T. E. (2016). Interpersonal psychotherapy: A review and multicultural critique. Counselling Psychology Quarterly, 29(3), 253–273. https://doi.org/10.1080/09515070.2015.1028896
- Andersson, S. O., Mattsson, B., & Lynoe, N. (1995). Patients frequently consulting general practitioners at a primary health care centre in Sweden—A comparative study. Scandinavian Journal of Social Medicine, 23(4), 251–257. https://doi.org/10.1177/140349489502300406
- Barsky, A. J. (1996). Hypochondriasis: Medical management and psychiatric treatment. Psychosomatics, 37(1), 48–56. https://doi.org/10.1016/S0033-3182(96)71598-0
- Barsky, A. J., Bauer, M. R., & Nolido, N. (2013). A randomized trial of treatments for high-utilizing somatizing patients. Journal of General Internal Medicine, 28(11), 1396–1404. https://doi.org/10.1007/s11606-013-2392-6
- Bellón, JÁ, Delgado, A., Luna, J. D., & Lardelli, P. (1999). Psychosocial and health belief variables associated with frequent attendance in primary care. Psychological Medicine, 29(6), 1347–1357. https://doi.org/10.1017/S0033291799008995
- Bernecker, S. L., Coyne, A. E., Constantino, M. J., & Ravitz, P. (2017). For whom does interpersonal psychotherapy work? A systematic review. Clinical Psychology Review, 56, 82–93. https://doi.org/10.1016/j.cpr.2017.07.001
- Bowlby, J. (1969). Attachment and loss. Basic Books.
- Burckhardt, C. S., & Anderson, K. L. (2003). The Quality of Life Scale (QOLS): Reliability, validity, and utilization. Health and Quality of Life Outcomes, 1(1), 60–65. https://doi.org/10.1186/1477-7525-1-60
- Bursztajn, H., & Barsky, A. J. (1985). Facilitating patient acceptance of a psychiatric referral. Archives of Internal Medicine, 145(1), 73–75. https://doi.org/10.1001/archinte.1985.00360010097015
- Castro, A., Gili, M., Ricci-Cabello, I., Roca, M., Gilbody, S., Perez-Ara, MÁ, Seguí, A., & McMillan, D. (2020). Effectiveness and adherence of telephone-administered psychotherapy for depression: A systematic review and meta-analysis. Journal of Affective Disorders, 260, 514–526. https://doi.org/10.1016/j.jad.2019.09.023
- Cuijpers, P., Donker, T., Weissman, M., Ravitz, P., & Cristea, I. A. (2016). Interpersonal psychotherapy for mental health problems: A comprehensive meta-analysis. American Journal of Psychiatry, https://doi.org/10.1176/appi.ajp.2015.15091141
- Dowrick, C. F., Bellón, J. A., & Gómez, M. J. (2000). GP frequent attendance in Liverpool and Granada: The impact of depressive symptoms. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 50(454), 361–365.
- Flanagan, J. C. (1978). A research approach to improving our quality of life. American Psychologist, 33(2), 138–147. https://doi.org/10.1037/0003-066X.33.2.138
- Foster, A., Jordan, K., & Croft, P. (2006). Is frequent attendance in primary care disease-specific? Family Practice, 23(4), 444–452. https://doi.org/10.1093/fampra/cml019
- Gili, M., Luciano, J. V., Serrano, M. J., Jiménez, R., Bauza, N., & Roca, M. (2011). Mental disorders Among frequent attenders in primary care: A comparison with routine attenders. The Journal of Nervous and Mental Disease, 199(10), 744. https://doi.org/10.1097/NMD.0b013e31822fcd4d
- Given, B., Goddeeris, J., Smith, R. C., Gardiner, J. C., Lyles, J. S., Sirbu, C., Dwamena, F. C., Hodges, A., Collins, C., Lein, C., & Given, C. W. (2005). Exploration of DSM-IV criteria in primary care patients with medically unexplained symptoms. Psychosomatic Medicine, 67(1), 123–129. https://doi.org/10.1097/01.psy.0000149279.10978.3e
- Hammerman, O., Halperin, D., Tsalihin, D., Greenberg, D., Kushnir, T., & Ezra, Y. (2021). Characteristics and economic burden of frequent attenders with medically unexplained symptoms in primary care in Israel. European Journal of General Practice, 27(1), 294–302. https://doi.org/10.1080/13814788.2021.1985997
- Huhtakangas, M., Tuomikoski, A.-M., Kyngäs, H., & Kanste, O. (2021). Frequent attenders’ experiences of encounters with healthcare personnel: A systematic review of qualitative studies. Nursing & Health Sciences, 23(1), 53–68. https://doi.org/10.1111/nhs.12784
- Hunter, J. J., & Maunder, R. G. (2001). Using attachment theory to understand illness behavior. General Hospital Psychiatry, 23(4), 177–182. https://doi.org/10.1016/S0163-8343(01)00141-4
- Irvine, A., Drew, P., Bower, P., Brooks, H., Gellatly, J., Armitage, C. J., Barkham, M., McMillan, D., & Bee, P. (2020). Are there interactional differences between telephone and face-to-face psychological therapy? A systematic review of comparative studies. Journal of Affective Disorders, 265, 120–131. https://doi.org/10.1016/j.jad.2020.01.057
- Kapur, N., Hunt, I., Macfarlane, G., McBeth, J., & Creed, F. (2004). Childhood experience and health care use in adulthood: Nested case—Control study. The British Journal of Psychiatry: The Journal of Mental Science, 185(2), 134–139. https://doi.org/10.1192/bjp.185.2.134
- Karlsson, H., Lehtinen, V., & Joukamaa, M. (1995). Are frequent attenders of primary health care distressed? Scandinavian Journal of Primary Health Care, 13(1), 32–38. https://doi.org/10.3109/02813439508996732
- Kersnik, J., Svab, I., & Vegnuti, M. (2001). Frequent attenders in general practice: Quality of life, patient satisfaction, use of medical services and GP characteristics. Scandinavian Journal of Primary Health Care, 19(3), 174–177. https://doi.org/10.1080/028134301316982405
- Kivelä, K., Elo, S., & Kääriäinen, M. (2018). Frequent attenders in primary health care: A concept analysis. International Journal of Nursing Studies, 86, 115–124. https://doi.org/10.1016/j.ijnurstu.2018.06.003
- Klerman, G. L., Budman, S., Berwick, D., Weissman, M., Damico-White, J., Demby, A., & Feldstein, M. (1987). Efficacy of a brief psychosocial intervention for symptoms of stress and distress among patients in primary care. Medical Care, 25(11), 1078–1088. https://doi.org/10.1097/00005650-198711000-00006
- Klerman, G. L., Weissman, M., Rounsaville, B. J., & Chevron, E. S. (1984). Interpersonal psychotherapy of depression. Basic Books.
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., & Löwe, B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32(4), 345–359. https://doi.org/10.1016/j.genhosppsych.2010.03.006
- LaCalle, E., & Rabin, E. (2010). Frequent users of emergency departments: The myths, the data, and the policy implications. Annals of Emergency Medicine, 56(1), 42–48. https://doi.org/10.1016/j.annemergmed.2010.01.032
- Lipsitz, J. D., & Markowitz, J. C. (2013). Mechanisms of change in interpersonal therapy (IPT). Clinical Psychology Review, 33(8), 1134–1147. https://doi.org/10.1016/j.cpr.2013.09.002
- Matalon, A., Yaphe, J., Nahmani, T., Maoz, B., & Portuguez-Chitrit, N. (2009). The effect of a multi-disciplinary integrative intervention on health status and general health perception in primary care frequent attenders. Families, Systems & Health: The Journal of Collaborative Family Healthcare, 27(1), 77–84. https://doi.org/10.1037/a0014769
- Menchetti, M., Bortolotti, B., Rucci, P., Scocco, P., Bombi, A., Berardi, D., & DEPICS Study Group. (2010). Depression in primary care: Interpersonal counseling vs selective serotonin reuptake inhibitors. The DEPICS study. A multicenter randomized controlled trial. Rationale and design. BMC Psychiatry, 10(1), 97. https://doi.org/10.1186/1471-244X-10-97
- Montgomery, P., Grant, S., Mayo-Wilson, E., Macdonald, G., Michie, S., Hopewell, S., Moher, D., Lawrence Aber, J., Altman, D., Bhui, K., Booth, A., Clark, D., Craig, P., Eisner, M., Fraser, M. W., Gardner, F., Grant, S., Hedges, L., Hollon, S. … on behalf of the CONSORT-SPI Group (2018). Reporting randomised trials of social and psychological interventions: The CONSORT-SPI 2018 extension. Trials, 19(1), 407. https://doi.org/10.1186/s13063-018-2733-1
- Neugebauer, R., Kline, J., Bleiberg, K., Baxi, L., Markowitz, J. C., Rosing, M., Levin, B., & Keith, J. (2007). Preliminary open trial of interpersonal counseling for subsyndromal depression following miscarriage. Depression and Anxiety, 24(3), 219–222. https://doi.org/10.1002/da.20150
- Patel, S., Kai, J., Atha, C., Avery, A., Guo, B., James, M., Malins, S., Sampson, C., Stubley, M., & Morriss, R. (2015). Clinical characteristics of persistent frequent attenders in primary care: Case–control study. Family Practice, 32(6), 624–630. https://doi.org/10.1093/fampra/cmv076
- Rafaeli, A. K., Bar-Kalifa, E., Verdeli, H., & Miller, L. (2021). Interpersonal counseling for college students: Pilot feasibility and acceptability study. American Journal of Psychotherapy, Appi-psychotherapy, 74(4), 165–171. https://doi.org/10.1176/appi.psychotherapy.202120200038
- Rasmussen, N. H., Furst, J. W., Swenson-Dravis, D. M., Agerter, D. C., Smith, A. J., Baird, M. A., & Cha, S. S. (2006). Innovative reflecting interview: Effect on high-utilizing patients with medically unexplained symptoms. Disease Management, 9(6), 349–359. https://doi.org/10.1089/dis.2006.9.349
- Ravitz, P., Watson, P., Lawson, A., Constantino, M. J., Bernecker, S., Park, J., & Swartz, H. A. (2019). Interpersonal psychotherapy: A scoping review and historical perspective (1974–2017). Harvard Review of Psychiatry, 27(3), 165–180. https://doi.org/10.1097/HRP.0000000000000219
- Reho, T., Atkins, S., Korhonen, M., Siukola, A., Sumanen, M., Viljamaa, M., Uitti, J., & Sauni, R. (2021). Sociodemographic characteristics and disability pensions of frequent attenders in occupational health primary care – a follow-up study in Finland. BMC Public Health, 21(1), 1847. https://doi.org/10.1186/s12889-021-11873-8
- Ronalds, C., Kapur, N., Stone, K., Webb, S., Tomenson, B., & Creed, F. (2002). Determinants of consultation rate in patients with anxiety and depressive disorders in primary care. Family Practice, 19(1), 23–28. https://doi.org/10.1093/fampra/19.1.23
- Scaife, B., Gill, P., Heywood, P., & Neal, R. (2000). Socio-economic characteristics of adult frequent attenders in general practice: Secondary analysis of data. Family Practice, 17(4), 298–304. https://doi.org/10.1093/fampra/17.4.298
- Shukla, D. M., Faber, E. B., & Sick, B. (2020). Defining and characterizing frequent attenders: Systematic literature review and recommendations. Journal of Patient-Centered Research and Reviews, 7(3), 255. https://doi.org/10.17294/2330-0698.1747
- Simon, G. E., Manning, W. G., Katzelnick, D. J., Pearson, S. D., Henk, H. J., & Helstad, C. S. (2001). Cost-effectiveness of systematic depression treatment for high utilizers of general medical care. Archives of General Psychiatry, 58(2), 181–187. https://doi.org/10.1001/archpsyc.58.2.181
- Sledge, W. H., Wieland, M., Sells, D., Walden, D., Holmberg, C., Lin, Z., & Davidson, L. (2011). Qualitative study of high-cost patients in an urban primary care centre. Chronic Illness, 7(2), 107–119. https://doi.org/10.1177/1742395310388673
- Smits, F. T., Brouwer, H. J., Zwinderman, A. H., Mohrs, J., Smeets, H. M., Bosmans, J. E., Schene, A. H., Van Weert, H. C., & ter Riet, G. (2013). Morbidity and doctor characteristics only partly explain the substantial healthcare expenditures of frequent attenders: A record linkage study between patient data and reimbursements data. BMC Family Practice, 14(1), 1–8. https://doi.org/10.1186/1471-2296-14-138
- Stuart, S. P., & Noyes, R. (2006). Interpersonal psychotherapy for somatizing patients. Psychotherapy and Psychosomatics, 75(4), 209–219. https://doi.org/10.1159/000092891
- Stuart, S. P., & Robertson, M. D. (2003). Interpersonal psychotherapy: A clinician’s guide. CRC Press.
- Sullivan, H. S. (1953). The interpersonal theory of psychiatry. Norton.
- Taylor, R. E., Mann, A. H., White, N. J., & Goldberg, D. P. (2000). Attachment style in patients with unexplained physical complaints. Psychological Medicine, 30(4), 931–941. https://doi.org/10.1017/S0033291799002317
- Taylor, R. E., Marshall, T., Mann, A., & Goldberg, D. P. (2012). Insecure attachment and frequent attendance in primary care: A longitudinal cohort study of medically unexplained symptom presentations in ten UK general practices. Psychological Medicine, 42(4), 855–864. https://doi.org/10.1017/S0033291711001589
- Thompson, D., & Ciechanowski, P. S. (2003). Attaching a new understanding to the patient-physician relationship in family practice. The Journal of the American Board of Family Practice, 16(3), 219–226. https://doi.org/10.3122/jabfm.16.3.219
- Van Hees, M. L., Rotter, T., Ellermann, T., & Evers, S. M. (2013). The effectiveness of individual interpersonal psychotherapy as a treatment for major depressive disorder in adult outpatients: A systematic review. BMC Psychiatry, 13(1), 1–10. https://doi.org/10.1186/1471-244X-13-22
- Vedsted, P., Christensen, M. B., Sørensen, H. T., Fink, P., & Olesen, F. (2002). Special status consultation for frequent attenders. Who are the candidates? Journal of Public Health Medicine, 24(1), 53–57. https://doi.org/10.1093/pubmed/24.1.53
- Vedsted, P., & Olesen, F. (2005). Social environment and frequent attendance in danish general practice. The British Journal of General Practice, 55(516), 510–515.
- Waller, E., Scheidt, C. E., & Hartmann, A. (2004). Attachment representation and illness behavior in somatoform disorders. The Journal of Nervous and Mental Disease, 192(3), 200–209. https://doi.org/10.1097/01.nmd.0000116463.17588.07
- Wammes, J. J. G., van der Wees, P. J., Tanke, M. A., Westert, G. P., & Jeurissen, P. P. (2018). Systematic review of high-cost patients’ characteristics and healthcare utilisation. BMJ Open, 8(9), e023113. https://doi.org/10.1136/bmjopen-2018-023113
- Wampold, B. E., & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge. https://doi.org/10.4324/9780203582015
- Weissman, M., Hankerson, S. H., Scorza, P., Olfson, M., Verdeli, H., Shea, S., Lantigua, R., & Wainberg, M. (2014). Interpersonal counseling (IPC) for depression in primary care. American Journal of Psychotherapy, 68(4), 359. https://doi.org/10.1176/appi.psychotherapy.2014.68.4.359
- Weissman, M., & Klerman, G. L. (1993). Interpersonal counseling for stress and distress in primary care settings. In G. L. Klerman, & M. Weissman (Eds.), New applications of interpersonal psychotherapy (pp. 295–318). American Psychiatric Press.
- Weissman, M., & Verdeli, H. (2012). Interpersonal psychotherapy: Evaluation, support, triage. Clinical Psychology & Psychotherapy, 19(2), 106–112. https://doi.org/10.1002/cpp.1775
- Wyke, S., Hunt, K., Walker, J., & Wilson, P. (2003). Frequent attendance, socioeconomic status and burden of ill health: An investigation in the west of Scotland. European Journal of General Practice, 9(2), 48–55. https://doi.org/10.3109/13814780309160402
- Yamamoto, A., Tsujimoto, E., Taketani, R., Tsujii, N., Shirakawa, O., & Ono, H. (2018). The effect of interpersonal counseling for subthreshold depression in undergraduates: An exploratory randomized controlled trial. Depression Research and Treatment, 2018. https://doi.org/10.1155/2018/4201897
Appendices
Appendix A: Equations for Multilevel Modeling Predicting Scale Scores (Symptoms and Quality of Life)
The 3-level models were based on these equations:
Level-1 Model:
Level-2 Model:
Level-3 Model:
Where:
represents the outcome measure (e.g., depression, anxiety, somatization, or quality of life score) for subject i with therapist j at time t
is a variable representing the time point (pre-intervention or post-intervention) for subject i with therapist j at time t
and
are dummy variables for the TIPC-FA and Support groups, respectively, for subject i with therapist j (compared to the TAU group)
and
are Level-2 intercept and slope parameters, respectively, for subject i with therapist j
are Level-3 fixed-effect parameters for therapist j
are the fixed-effect coefficients at Level-3
is the Level-1 residual for subject i with therapist j at time t, assumed to be normally distributed with a mean of 0 and variance
is the Level-2 random effect for the intercept for subject i with therapist j, assumed to be normally distributed with a mean of 0 and variance
and
are Level-3 random effects for the intercept and slope, respectively, for therapist j, assumed to be multivariate normally distributed with a mean vector of 0 and a covariance matrix defined by
and
Appendix B: Equations for Multilevel Modeling Predicting Measures of Healthcare Utilization
The 2-Level models were based on these equations for assessing the various outcome measures:
Level-1 Model:
Level-2 Model:
Where:
represents the utilization score for subject i at time t
is a variable representing the monthly time point starting from a month before the intervention and follow-up until eight months after the intervention
and
are dummy variables for the IPC and Support groups, respectively, for subject i (compared to TAU as a reference category)
and
are Level-2 intercept and slope parameters, respectively, for subject i
are Level-2 fixed-effect parameters
is the Level-1 residual for subject i at time t, assumed to be normally distributed with a mean of 0 and variance
and
are Level-2 random effects for the intercept and slope, respectively, for subject i, assumed to be multivariate normally distributed with a mean vector of 0 and a covariance matrix defined by
and