ABSTRACT
Objective
: Meditation, mindfulness, and acceptance (MMA) methods have gained popularity among psychotherapists and the public. The impact of these strategies as implemented in treatment packages (e.g., mindfulness-based interventions) has been studied extensively. However, the impact of integrating MMA strategies into individual psychotherapy has not been established.
Methods
: To address this gap in the literature, we conducted a systematic review of empirical (quantitative or qualitative) studies investigating the use of MMA methods during individual psychotherapy in adult samples.
Results
: After reviewing 4671 references, only three studies (one quantitative, two qualitative) met our inclusion criteria. The one experimental study (n = 162) provided no evidence that including mindfulness meditation improved outcomes beyond other active interventions (ds = 0.00–0.12 for effects on general clinical symptoms vs. progressive muscle relaxation and treatment-as-usual, respectively). Two qualitative studies (n = 5 therapist-patient dyads in one study, n = 9 adults in one study) provided preliminary evidence that patients may find MMA methods helpful.
Conclusions
: We highlight future directions for work in this area, including clarifying optimal dosage and timing, identifying patient characteristics associated with beneficial or adverse effects, investigating cultural adaptations, and clarifying how MMA constructs can be measured within individual psychotherapy. We conclude by highlighting training recommendations and therapeutic practices.
Clinical or methodological significance of this article: The study examined the evidence for incorporating meditation, mindfulness, and acceptance strategies within individual psychotherapy outside of treatment packages. Only three studies met our inclusion criteria, and none provided strong empirical support for this integration. However, given the extensive evidence supporting the efficacy of treatment packages that include these strategies, clinicians may find them helpful for patients with common psychological symptoms and those seeking to improve their wellbeing.
For after all, the best thing one can do when it is raining, is to let it rain—Henry Wadsworth Longfellow (Citation1900, p. 398)
Over the past three decades, there has been a dramatic increase in both scientific and popular interest in what has been defined as the third wave of cognitive and behavioural therapies (Hayes, Citation2004). Widely studied third-wave therapies include Acceptance and Commitment Therapy (ACT; Hayes et al., Citation1999), Dialectical Behaviour Therapy (DBT; Linehan, Citation1993), and mindfulness meditation-based therapies, such as Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, Citation2013) and Mindfulness-Based Cognitive Therapy (MBCT; Segal et al., Citation2013). Of course, various forms of meditation have existed for thousands of years in contemplative traditions around the world (Smith, Citation1991). The secularized forms of mindfulness meditation found in MBSR and MBCT are derived from Buddhist practices (Kabat-Zinn, Citation2011). Whereas prior waves of cognitive behavioural therapy (CBT) focused on symptom reduction, these third-wave therapies instead emphasize promotion of behaviours associated with psychological health and wellbeing. Thus, patients are encouraged to shift their emphasis from making unpleasant experiences go away to moving in psychologically healthy and value-driven directions regardless of painful thoughts, emotions, and events that may occur (Block-Lerner et al., Citation2009).
Meditation, mindfulness, and acceptance (MMA) are three central methods included to varying degrees across these third-wave therapies. There is clear evidence these methods have gained strong footholds within the psychotherapy world and broader Western culture (Davis & Hayes, Citation2011; Goldberg, Citation2022; Michalak et al., Citation2020; Van Dam et al., Citation2018). Hundreds of randomized controlled trials (RCTs) have been conducted investigating mindfulness meditation-based interventions alone (Goldberg et al., Citation2022b), and ACT, DBT, and MBCT are all listed as evidence-based treatments by the American Psychological Association's Society of Clinical Psychology (Citationn.d.). Meditation-based smartphone apps are far and away the most popular mental health apps (Wasil et al., Citation2020). To date, the bulk of scientific research on MMA in psychotherapy has emphasized testing treatment packages (e.g., ACT, DBT, MBCT). Consistent with the broader psychotherapy literature (Wampold & Imel, Citation2015), these therapies generally improve psychological symptoms to a similar degree as other interventions that are intended to be therapeutic (i.e., bona fide psychotherapies; Galante et al., Citation2021; Goldberg et al., Citation2018; Öst, Citation2008, Citation2014) ().
Table I. Summary effect sizes from review of meta-analyzes of randomized controlled trials testing mindfulness-based interventions.
While treatment packages have been invaluable for popularizing MMA within psychotherapy, these methods may hold promise for implementation outside of the context of a specific or manualized treatment package. Therapists commonly use a wide variety of methods in actual clinical practice (Cook et al., Citation2010), and many are already using mindfulness (Michalak et al., Citation2020). This chapter focuses on the narrower MMA methods themselves rather than the treatment packages within which these methods are commonly implemented (e.g., ACT, DBT, MBCT).
Definitions and Clinical Description
Meditation has been defined as “a family of complex emotional and attentional regulatory training regimes developed for various ends, including the cultivation of well-being and emotional balance” (Lutz et al., Citation2008, p. 163). Various forms of meditation have been studied scientifically, primarily drawn from Eastern contemplative traditions (e.g., Tibetan, Theravadan, and Zen Buddhism; Hinduism; Harrington & Dunne, Citation2015; Nidich et al., Citation2018). These include practices designed to develop attention regulation (e.g., meta-awareness or awareness of the processes of consciousness), cultivate cognitive and affective patterns conducive to well-being (e.g., kindness, compassion), and foster insight into the nature of the self (e.g., self-inquiry practices; Dahl et al., Citation2015). A wide variety of specific practices are used to support these changes and may include focusing on a single object (e.g., the breath coming in and out of the body), generating feelings of kindness and compassion (e.g., using the repetition of phrases and visualizing directing feelings towards particular people), or reflecting on the changing nature of moment-to-moment experience (Dahl et al., Citation2015).
Mindfulness has been defined as a way of purposefully attending to present-moment experience without judgment (Kabat-Zinn, Citation1994). Mindfulness meditation is a specific form of meditation practice aimed at cultivating the capacity to orient attention nonjudgmentally towards the present moment.
Acceptance methods enhance patients’ experiential acceptance, defined as having or allowing private events (including painful ones) free of attempts at regulation (Block-Lerner et al., Citation2009)—in other words, allowing things to be experienced without needing to change them or push them away. This orientation contrasts with experiential avoidance, where one is “unwilling to remain in contact with particular private experiences (e.g., bodily sensations, emotions, thoughts, memories, behavioural predispositions) and takes steps to alter the form or frequency of these events and the contexts that occasion them” (Hayes et al., Citation1996, p. 1154).
There are many forms of meditation in practice, including mindfulness meditation designed to train one's capacity for experiential acceptance by attending to present-moment private experiences without effort to change them (Block-Lerner et al., Citation2009). Broader still, experiential acceptance has been proposed as a common factor across various forms of psychotherapy which, through methods such as therapists’ unconditional positive regard for their patients, patients turn towards rather than away from painful private experiences (Block-Lerner et al., Citation2009). In contrast, mindfulness meditation, unlike acceptance alone, trains both acceptance and present-moment awareness (i.e., monitoring with acceptance; Lindsay & Creswell, Citation2017).
MMA methods can be implemented in multiple ways within individual psychotherapy of different theoretical orientations (for guidelines for implementing mindfulness meditation, see Michalak et al., Citation2019). Formal meditation practice (in contrast to informal practice implemented in daily life; Kabat-Zinn, Citation2013) involves taking a few moments (or longer) in a session to engage in a specific meditation practice. For example, a therapist may guide the patient in a body scan, in which one turns their attention to the physical sensations occurring in the body (Kabat-Zinn, Citation2013), or a lovingkindness meditation, in which one generates feelings of kindness towards oneself or others (Salzberg, Citation2004). The initial introduction of formal meditation will probably occur with an extended guided practice in the session followed by inquiry, during which the therapist supports the patient reflecting on their practice experience (Michalak et al., Citation2019). This inquiry could start with discussion of physical sensations and allow patients the opportunity to draw linkages between body states and affective experiences.
Mindfulness can also take the form of a guided meditation practice (e.g., body scan). But it may be introduced less formally by inviting patients to pay attention to their internal experience (i.e., physical sensations, affective state, cognitions) with curiosity and acceptance.
Acceptance can likewise be implemented through formal meditation practice or a wide range of other methods. Both ACT and DBT include numerous acceptance methods to provide patients a direct experience of experiential acceptance. These may involve stories or images to express the drawbacks of non-acceptance (e.g., characterizing the relationship between anxiety and struggle as a volleyball game; Forsyth & Eifert, Citation2007) as well as conceptual frameworks (e.g., willingness vs. willfulness) and behavioural methods (e.g., half-smiling) to promote experiential acceptance (Linehan, Citation2015).
As will be discussed, there is limited research evidence to guide the use of meditation within psychotherapy sessions outside of third-wave treatment packages. And, importantly, much of the research on third-wave treatment packages, especially mindfulness, has occurred in group settings (although see studies investigating individual MBCT, e.g., Tovote et al., Citation2014). There are elements in the group setting that may make MMA methods particularly helpful (e.g., opportunity to learn from others’ experience, sense of shared humanity with others experiencing similar difficulties; Yalom & Leszcz, Citation2005). To the extent to which evidence from treatment packages (often delivered in groups) generalizes to implementation in individual therapy, there is evidence that all three methods may effectively reduce common forms of psychological distress (e.g., depression, anxiety, stress) and may be helpful for chronic pain and substance use (Galante et al., Citation2021; Goldberg et al., Citation2022b; Goyal et al., Citation2014; Öst, Citation2008, Citation2014).
In terms of other specific indications, DBT was designed for patients with borderline personality disorder, although it includes many other treatment ingredients beyond acceptance (e.g., training in emotion regulation and interpersonal effectiveness skills; Linehan, Citation2015). There is some evidence that individuals with greater severity of depression may benefit more from MBCT (Kuyken et al., Citation2016). However, on the whole, moderators of method effectiveness are generally unknown.
Formal meditation and mindfulness methods may calm some patients and enhance a sense of alliance, collaboration, and a healing setting. For example, MBCT (Segal et al., Citation2013) conceptualizes mindfulness as a method to detect early signs of relapse and prevent worsening of symptoms through increased awareness and decentring (i.e., ability to dis-identify with internal experience; Bernstein et al., Citation2015).
Care using MMA methods may be particularly important for individuals who find meditation practice aversive and even triggering (Baer et al., Citation2019b; Goldberg et al., Citation2022a). Particular sensitivity should be taken when implementing formal meditation practice for those with trauma histories (Goldberg et al., Citation2022a; Treleaven, 2019). Specific forms of meditation (e.g., compassion practice) may be triggering for patients prone to rumination, who may feel discouraged by their inability to immediately embody the qualities being cultivated through practice (Segal et al., Citation2013). Nonetheless, the available experimental evidence suggests that MMA methods implemented in treatment packages decrease rather than increase the risk of symptom worsening (Goldberg et al., Citation2020a; Hirshberg et al., 2021, Citation2022).
With acceptance strategies, the therapist establishes a validating environment prior to introducing acceptance methods. Indeed, methods for validating and responding to invalidation are included in DBT (Linehan, Citation2015), as many patients with borderline personality disorder are sensitive to perceived emotional invalidation. Patients may reasonably wish to (and be encouraged to) make changes to factors contributing to their distress. Thus, acceptance is best focused on both immediate (e.g., distress in the current moment) and persistent experiences (e.g., chronic illness) that cannot be constructively resolved in another way (i.e., accepting the things one cannot change, changing the things one can; Block-Lerner et al., Citation2009). Therapists implementing acceptance should be sensitive to their patients’ resistance to the perceived message that their life cannot be better. Of course, acceptance does not imply that change will not occur (and Eastern contemplative traditions clearly acknowledge that change is inevitable; Bodhi, Citation2005), and there is strong evidence that acceptance strategies can, somewhat counterintuitively, decrease distress and other symptoms (e.g., pain, substance use; Goldberg et al., Citation2022b; Öst, Citation2008).
Assessment
Several adherence and competence measures have been designed to assess implementation of treatment packages emphasizing MMA methods (e.g., Chawla et al., Citation2010; Hanley & Garland, Citation2021; Harned et al., Citation2021; Segal et al., Citation2002). However, to our knowledge these measures have not been used to evaluate implementation outside the treatment package. In theory, these measures may include relevant items for implementing them in individual psychotherapy. However, it will be vital for future researchers to investigate this possibility directly (e.g., by administering items drawn from existing adherence and competence measures). Developing measures specifically for evaluating the implementation of MMA methods in individual psychotherapy and outside of a treatment package is also an essential step in this area.
In a study investigating the inclusion of mindfulness within psychotherapy, a measure of general psychotherapeutic presence (Therapeutic Presence Inventory; Geller et al., Citation2010) was used to assess therapists’ in-session mindfulness and acceptance based on patient- and therapist-ratings (Mander et al., Citation2019). Mander et al. (Citation2019) also included observer-rated items assessing the therapists’ provision of specific methods (mindfulness or progressive muscle relaxation in this particular study). The authors of this study used a measure designed to assess mindfulness practice quality (Practice Quality-Mindfulness [PQ-M]; Del Re et al., Citation2013) to evaluate patients’ perceived quality of their mindfulness practice. Although Mander et al. (Citation2019) conceptualized the PQ-M as a measure of mindfulness implementation, it could also reasonably be viewed as a measure of outcome (i.e., patient's mindfulness practice quality being an outcome of an effective implementation of a mindfulness method).
Far greater work has focused on developing measures to evaluate the distal (e.g., trait mindfulness) and proximal (e.g., state mindfulness) outcomes of MMA methods. Widely-used self-report measures of trait mindfulness (as opposed to mindfulness occurring in the moment, which would be state mindfulness) that could evaluate the distal effects of these methods include the Mindful Attention Awareness Scale (MAAS; Brown & Ryan, Citation2003) and the Five Facet Mindfulness Scale (Baer et al., Citation2006). These measures are responsive to mindfulness meditation training (Goldberg et al., Citation2019; Quaglia et al., Citation2016), and the FFMQ has also been shown to respond to informal mindfulness practice (Hanley et al., Citation2015). Both measures have shown desirable psychometric properties including acceptable internal consistency as well as evidence for construct validity (convergent and discriminant validity) and structural validity (Baer et al., Citation2006; Brown & Ryan, Citation2003). However, it is worth noting that these measures may be responsive not only to mindfulness training, but appear to increase in the context of psychological treatments (Baer et al., Citation2019b; Goldberg et al., Citation2019). The Self-Compassion Scale (Neff, Citation2003) is widely used to measure compassion towards self and has been shown to be responsive to brief lovingkindness meditation training (Smeets et al., Citation2014). The Acceptance and Action Questionnaire-II (Bond et al., Citation2011) is designed to assess experiential avoidance (e.g., “I’m afraid of my feelings”) and is commonly used within the context of ACT.
Although some of these measures have shown responsiveness to short-term training (e.g., mindfulness inductions), they are considered trait measures (i.e., measures that do not vary from moment-to-moment). There has been parallel development of state measures of mindfulness which may be relevant to assessing the impact of mindfulness or meditation methods in a particular session. These include a state version of the MAAS (Brown & Ryan, Citation2003), the Toronto Mindfulness Scale (Lau et al., Citation2006), and the State Mindfulness Scale (Tanay & Bernstein, Citation2013). As noted above, the Practice Quality–Mindfulness scale (PQ-M; Del Re et al., Citation2013) has been used to evaluate within-session implementation of mindfulness practice. Changes in the Practice Quality–Mindfulness scale have been linked to improvements in psychological symptoms and trait mindfulness within mindfulness interventions (Del Re et al., Citation2013; Goldberg et al., Citation2014, Citation2020b).
Previous Reviews
There are dozens of RCTs testing MMA methods as part of larger treatment packages. Meta-analyzes of these RCTs have concluded that these treatment packages, like various forms of psychotherapy (Wampold & Imel, Citation2015), tend to produce moderate-to-large magnitude effects on psychological symptoms when compared to no treatment and produce non-significant effects when compared to other forms of psychotherapy (Goldberg et al., Citation2022b; Goyal et al., Citation2014; Öst, Citation2008, Citation2014).
Meta-analyzes have also examined the effects of stand-alone, without-therapy mindfulness exercises delivered outside of the context of a mindfulness meditation-based intervention as well as brief mindfulness inductions. Results from these meta-analyzes suggest that stand-alone mindfulness exercises produce small-to-moderate reductions in depression and anxiety relative to controls (standardized mean differences = 0.41, 0.39, respectively; Blanck et al., Citation2018). Brief mindfulness inductions may also reduce negative affect, although this effect may be exaggerated due to the lack of publication of non-significant findings (i.e., publication bias; Schumer et al., Citation2018). Despite these promising findings, research on the impact of MMA methods outside a treatment package is just beginning. This was the motivation to conduct the current systematic review.
Research Review
Distal Outcomes of Treatment Packages
Many RCTs and meta-analyzes of RCTs have examined the efficacy of treatment packages implementing MMA methods. The body of research examining mindfulness meditation is particularly large. A recent meta-review examined the evidence for mindfulness-based interventions seen in 44 meta-analyzes of RCTs (Goldberg et al., Citation2022b). This review identified 160 different effect sizes characterizing the effects of mindfulness-based interventions from 336 RCTs (N = 30,483 participants). The mindfulness-based interventions included in these studies all involved the repeated practice of mindfulness meditation. The authors identified effect sizes representing the largest number of studies for a particular combination of population, intervention, comparison group, and outcome (e.g., studies testing MBCT for depressive relapse in adults; Kuyken et al., Citation2016).
Although it is not possible to summarize the details of this vast literature in brief, there were several patterns of findings. On the whole, mindfulness-based interventions produced small to moderate magnitude effects relative to passive control conditions (e.g., waitlist controls) at post-treatment, with many effects persisting although often decreasing at follow-up (Goldberg et al., Citation2022b). These effects were observed across a range of populations, types of mindfulness interventions, and outcomes, although they tended to be most robust for common psychological symptoms (e.g., depression, anxiety). Effect sizes tended to diminish when mindfulness-based interventions were compared with active controls (i.e., other interventions intended to be therapeutic or “placebo” controls that were designed to control for attention but not include therapeutic ingredients), although there was still evidence for superiority in some instances (e.g., on common psychological symptoms). When compared directly, mindfulness-based interventions performed very similarly to frontline, evidence-based treatments (e.g., CBT, antidepressants; Kuyken et al., Citation2016).
The certainty of the evidence for MMA-based treatment packages is not uniform across all demographic groups. Cultural diversity has been understudied and inconsistently reported within meditation research (Eichel et al., Citation2021). The small body of research investigating mindfulness-based methods for racial/ethnic minority participants in the US indicates that these interventions produce modest benefits (standardized mean differences = 0.26 and 0.11 for comparisons with inactive controls and active controls at post-treatment, respectively) with effect sizes potentially smaller than those seen for similar interventions in the general population (Sun et al., Citation2022). A growing number of RCTs have investigated mindfulness in non-Western samples (e.g., Asian, Middle East; Galante et al., Citation2021), although to our knowledge it has not been established the degree to which efficacy varies across countries. Additional dimensions of diversity (gender, sexual orientation, socioeconomic status) remain understudied in relation to these methods, although women are more likely than men to enrol in community-based mindfulness training (Hirshberg et al., 2020). Further, it is generally unknown which, if any, demographic characteristics moderate the impact of these methods. Nonetheless, there are reasons to believe that these approaches may be culturally resonant for some cultural groups (e.g., alignment with African American spiritual values; Biggers et al., Citation2020; Woods-Giscombé & Black, Citation2010).
In-Session Impact of MMA Methods
We designed our search terms to identify articles investigating one or more of the MMA methods. The search terms were: (“mindful*” OR “meditat*” OR “acceptance” OR “dialectical”) AND (“psychother*” OR “in session”). The search was conducted on 18 January 2021 using PubMed. Two doctoral students in counselling psychology supervised by two counselling psychology professors with experience in systematic reviews and meta-analysis completed inclusion/exclusion coding.
Retrieved references were first coded at the title and abstract level. Full text articles were retrieved for studies that passed the title and abstract level of screening. Studies were eligible if they (a) investigated the use of MMA methods during individual psychotherapy and (b) were conducted using an adult sample. Both qualitative and quantitative studies were eligible. Studies were excluded if they (a) focused on a treatment package (e.g., MBSR, MBCT, DBT, ACT, or stand-alone modules from these packages that were not delivered in the context of general psychotherapy), (b) implemented MMA as an intervention for therapists (i.e., not patients), (c) occurred outside psychotherapy (e.g., analogue studies, mindfulness induction), and (d) examined mindfulness and/or acceptance as a mechanism (e.g., changes in trait mindfulness) but did not manipulate these characteristics (e.g., changes in trait mindfulness measured in routine psychotherapy within application of a MMA method). All coding was done independently by the two coders, with disagreements discussed by all four authors.
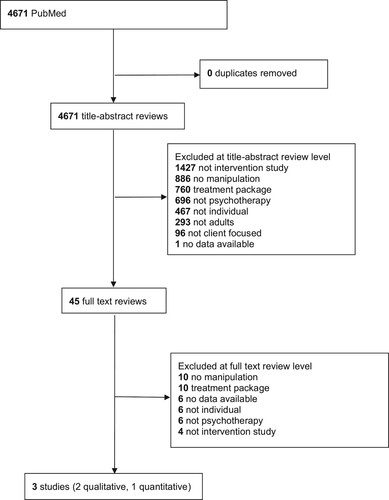
Our search returned 4671 references, which were reviewed at the title and abstract level. Forty-five of these were reviewed at the full text level. Three studies were ultimately deemed eligible for inclusion, two of which were qualitative studies and one of which was quantitative. presents the PRISMA flow diagram. Thus, there were an insufficient number of studies to perform a meta-analysis. Given the small number of studies retrieved, we discuss them briefly here.
The one quantitative study was an RCT that directly evaluated the impact of including MMA methods in individual psychotherapy outside the context of a treatment package (Mander et al., Citation2019). This study included 162 adults with depressive or anxiety disorders who were being treated by 48 therapists in an outpatient CBT training clinic in Germany. Patients were randomly assigned to receive 5-min introductions to audio-guided mindfulness meditation (adaptation of the breathing space from MBCT), audio-guided progressive muscle relaxation, or treatment-as-usual (therapist and patient were free to use the first 5 min of sessions however they would like) at the beginning of each session over a 25-session course of treatment. Therapists were trained to deliver the active interventions through two expert-led workshops, separated by 6-weeks during which the therapists were asked to practice the method (mindfulness meditation or progressive muscle relaxation) at home.
The primary outcome of the 5-min psychotherapy session introductions was patients’ general clinical symptoms assessed at four time points. The study had a large sample to detect small effects for between-group differences. Several secondary outcomes were assessed, including therapeutic alliance, depression, anxiety, and mindfulness. Therapists’ adherence (self-report and observer rated) was also assessed on their assigned session introduction, therapeutic presence, mindfulness practice quality, allegiance, and CBT competence.
This is an exemplary study in many respects. It included random assignment conducted by an independent research assistant; assessed clinically relevant outcomes in a clinical sample (Mander et al., Citation2015); featured patient-, therapist-, and observer-rated outcomes; provided training from experts and opportunities for therapist home practice; had an adequate sample size (i.e., was statistically powered) to detect small effects; and incorporated statistical analyzes accounting for the nested data structure (multilevel models).
Within this unusually rigorous context, Mander et al. (Citation2019) reported no evidence for differences across types of session introductions. All groups showed moderate to large improvements across their primary outcome and all secondary outcomes. Moreover, the researchers found no evidence that assignment to the mindfulness condition moderated the alliance-outcome association, nor that baseline demographic or mindfulness-related measures moderated the impact of condition assignment on outcomes.
The effect sizes for between-group differences on the primary outcome (general clinical symptoms) were Cohen's d = 0.00 (for mindfulness vs. progressive muscle relaxation) and d = 0.12 (for mindfulness vs. treatment-as-usual). Across the secondary outcomes, the maximum between-group differences for mindfulness vs. progressive muscle relaxation was d = 0.31 (for therapist-rated therapeutic alliance) and for mindfulness vs. treatment-as-usual d = 0.20 (for patient-rated mindfulness). Although between-group effects were not significant, these effect sizes were in the small range (i.e., d ≥ 0.20; Cohen, Citation1988). This raises the question (not raised by Mander et al., Citation2019) as to whether statistical power may have impacted their detection of certain between-group contrasts—in other words, the same magnitude effect may have been statistically significant in a larger sample. Understandably, Mander et al. were conservative in not testing and reporting between-group differences when omnibus tests of differences were not significant.
Rigorously obtained evidence that all introductions worked equally well should, of course, be taken seriously. Thus, the most conservative interpretation is that mindfulness as an introduction to a psychotherapy session did not improve clinical outcomes or alliance relative to other active introductions. Further, this study provided no indication that some patients may benefit more from mindfulness than the other interventions tested (treatment-as-usual and progressive muscle relaxation). In other words, no patient-level characteristics (e.g., demographic or diagnostic variables) moderated the treatment effects (Mander et al., Citation2019).
From our perspective, a key question in interpreting the results of Mander et al. (Citation2019) is did their study test whether integrating mindfulness meditation into individual psychotherapy proved helpful. There are probably more individualized and flexible ways of including these methods. In routine practice, therapists can flexibly apply mindfulness (or meditation, acceptance) within the course of psychotherapy for a particular patient and/or at a particular time. This naturalistic implementation is, of course, harder to study experimentally. In addition, the study included a relatively modest dose of mindfulness training—5 min at the beginning of each session. Thus, it is unclear whether a more intensive inclusion of mindfulness training (perhaps coupled with home practice assignments) would have yielded different results. A future study could randomly assign therapists to integrate one or more of MMA methods within their course of treatment with specific patients and not others.
We found two qualitative studies in our systematic review on the use of MMA methods in individual therapy (Horst et al., Citation2013; Michaelis et al., Citation2018). Horst et al. most directly examined the impact of incorporating mindfulness in individual psychotherapy. This study was conducted with trainee therapists and adult psychotherapy patients. The authors recruited five therapist-patient dyads in which the therapist had implemented a mindfulness exercise at least twice. The trainee therapists had some training in mindfulness before implementing these methods in session, either in the form of an 8-week group practicum or through their own independent study (e.g., books, other resources).
On the whole, both therapists and patients in the Horst et al. (Citation2013) study found these practices to be helpful. The dyads reported numerous ways in which mindfulness facilitated the therapeutic experience, including reducing the presenting problem (e.g., managing pain), helping with transitions (starting and ending sessions), facilitating conversations, producing a calming effect, and slowing the session pace. Both patients and therapists, however, noted a lack of confidence in their ability to effectively implement mindfulness, particularly the first time, although they became more comfortable with practice.
Patients and therapists identified features that made these practices more or less successful (Horst et al., Citation2013). The helpful features included having mindfulness as a shared experience (therapists and patients practicing together and discussing their shared apprehensions), continued practice, mutual trust, and the importance of flexibility (e.g., “moving on” from the exercise if a patient did not find it helpful). It also appeared helpful to preface/process the experience in the form of conversations before and after the exercise. Echoing concerns raised with implementing lovingkindness practice for patients with depression (Segal et al., Citation2013), one patient remarked that “you don't want to make someone feel like they aren't doing this right” (Horst et al., Citation2013, p. 377).
A second qualitative study examined the use of mindfulness-based relaxation methods within individual CBT-informed treatment for managing seizures in nine adults (Michaelis et al., Citation2018). Patients were given the option of learning about mindfulness during the initial session and were then advised to practice it regularly. Seven of the nine patients chose to learn about mindfulness. Adherence to home practice was not reported.
The authors’ qualitative analysis focused on patients’ sense of self-efficacy and mastery. Interestingly, mention of mindfulness was rare within the data reported. Two participants noted benefits from mindfulness under a theme focused on “shaping everyday life in a way that is good for oneself,” while one mentioned mindfulness exercises were not necessary as they were engaging in yoga practice. Acceptance appeared more frequently. One participant remarked that “the word ‘accepting’ has become my mantra’” (Michaelis et al., Citation2018, p. 157). Several participants mentioned acceptance as a helpful strategy under the “coping with seizures” theme. Self-acceptance also appeared under the “epilepsy as a means of increasing self-knowledge and control over one's life” theme: “I accept epilepsy […]. It is still an illness, […] but people with epilepsy are valuable anyway” (Michaelis et al., Citation2018, p. 158).
Given our search returned only three studies, in lieu of a meta-analysis, we estimated box scores (i.e., summary judgment of the evidence for effects of MMA methods on in-session outcomes) for each of the three studies. We used +1, −1, and 0 to denote positive, neutral, and negative effects, respectively. To get a weighted box score, we multiplied the box score by the sample size for each finding and then computed an average box score across the studies. We interpreted box scores between −1 and -.5 as negative, between .5 and +1 as positive, and between -.49 and + .49 as neutral. For the one quantitative study (Mander et al., Citation2019), we assigned a score of 0 to reflect the null effects observed for the use of mindfulness as a session-introducing exercise in a sample of 162 patients. For Horst et al. (Citation2013), we assigned a score of +1 for mindfulness in a sample of five therapy dyads (n = 10). For Michaelis et al. (Citation2018), we assigned a score of 0 for mindfulness and +1 for acceptance in a sample of nine people with epilepsy. The weighted box score for mindfulness was neutral [(0 × 162 = 0 for Mander et al.) + (+1 × 10 = 10 for Horst et al.) + (0 × 9 = 0 for Michaelis et al.) = 10/181 across both studies = 0.06 weighted box score]. The weighted box score for acceptance was positive [(1 × 9 = 9 for Michaelis et al.) = 9/9 across one study = 1 weighted box score]. Taken together, these studies provide inconclusive evidence regarding the impact of these methods on in-session outcomes.
Possible Negative Effects and Harm
Systematic evaluation of harm and adverse effects in meditation-based methods is lacking (Baer et al., Citation2019a). To our knowledge, no systematic evaluation of harm and adverse effects of informal mindfulness or acceptance methods implemented outside of a treatment package exists. Thus, we focus here on what is known about meditation practice generally.
It is widely recognized within the contemplative traditions that these practices can have challenging consequences (Lindahl et al., Citation2017). There is now strong scientific evidence that intensive meditation practice (i.e., meditation retreats) in particular can produce a host of perceptual, affective, and behavioural shifts that can cause varying degrees of distress, even as these experiences may be viewed as natural consequences of spiritual development and even as indicators of spiritual progress (Baer et al., Citation2019a; Lindahl et al., Citation2017).
It does appear that “unpleasant experiences” are fairly common within meditation-based methods (e.g., 67–73% of participants in MBCT; Baer et al., Citation2020). The estimates of harm (defined as worsening) range from 2 to 7% (Baer et al., Citation2020; Britton et al., Citation2021; Hirshberg et al., Citation2022). Moreover, 32–50% of individuals in the general population who have been exposed to meditation report having had meditation-related challenges, most commonly anxiety, traumatic re-experiencing, and increased emotional sensitivity (Goldberg et al., Citation2022a). These experiences seem to be more common for individuals with proneness toward negative affect (depression, anxiety, loneliness) and with early childhood adversity (Goldberg et al., Citation2022a).
These results highlight the need for clinicians to apply meditation with caution and sensitivity, especially when patients have a trauma history. In our view, the available data suggest the benefits of meditation generally outweigh the potential harm. Indeed, these negative consequences are not associated with whether an individual feels glad to have practiced meditation (Goldberg et al., Citation2022a), suggesting distressing consequences usually do not overshadow the potential benefits. Furthermore, results from RCTs testing meditation apps indicate that they decrease (rather than increase) risk for symptom worsening relative to wait-list controls (Goldberg et al., Citation2020a; Hirshberg et al., 2021). However, as with any intervention, clinicians are encouraged to attend closely to how a particular patient is responding to a given intervention approach.
Limitations of the Research
Research on the use of MMA methods in individual psychotherapy outside of treatment packages is just beginning. The three studies we identified investigating the use of MMA in this way had important limitations, some of which were discussed above. Mander et al. (Citation2019) used a brief (5-min) audio-guided mindfulness meditation practice, but did not examine either a more flexible or therapist-led implementation of mindfulness nor the impact of more intensive mindfulness practice (e.g., longer session introductions, home practice assigned to patients). The two qualitative studies (Horst et al., Citation2013; Michaelis et al., Citation2018) included small samples and did not involve randomization, making causal inferences not possible. An important limitation across all three studies was a lack of evaluation of MMA effects on outcomes theoretically sensitive to MMA methods immediately following their implementation. The closest to this was Mander et al. who assessed therapeutic alliance at the end of each psychotherapy session. However, this was following a 50-min session (not immediately following the mindfulness practice) and therapeutic alliance may or may not be sensitive to mindfulness training. It may well be that there are short-term but nonetheless important effects of these methods that are not captured by retrospective assessments. Taken together, it remains scientifically uncertain whether promising findings drawn from the treatment package literature will apply.
We highlight several future directions for future research on MMA methods. There is a need to clarify the optimal dosage for incorporating these methods, as they could range from very minimal (e.g., mentioning a meditation app as adjunctive support, including an informal acceptance method) to central (e.g., applying these methods once or more every session). It may be valuable to investigate the impact of assigning homework outside of session. As noted, examining effects on more proximal outcomes (e.g., immediately following the application of a MMA method) may be helpful here. It will also be important to clarify when and for whom these methods may be most effective as well as when they may be contraindicated. It is also important to investigate cultural adaptation of these methods (Sun et al., Citation2022), given that culturally-adapted treatments outperform non-adapted treatments for racial/ethnic minority groups in psychotherapy generally (Benish et al., Citation2011). Lastly, it will be important to clarify the necessary therapist training for implementing these strategies (Michalak et al., Citation2019), including whether and how training might be incorporated into graduate education. At a minimal, it will be helpful for researchers studying these methods to clearly report the training therapists delivering MMA methods have both delivering these methods as well as cultivating these capacities through their own personal practice (e.g., attending meditation classes and retreats).
Training Implications
There are widely available clinical training programmes for learning to implement the treatment packages (e.g., MBSR, MBCT, DBT, ACT) from which these MMA methods are drawn. Interested clinicians would be well served by participating in MBSR or MBCT as participants, trainees, or co-therapists (Michalak et al., Citation2019). Personal practice probably enhances implementing meditation strategies and skillfully managing challenges that arise for patients. Indeed, developers of both MBSR and MBCT have emphasized the importance of instructors’ personal meditation practice when delivering these approaches (Kabat-Zinn, Citation2011; Segal et al., Citation2013). As with most novel strategies, clinicians may benefit from working with supervisors who have experience implementing these methods in individual therapy.
Therapeutic Practices
The plentiful research evidence on the effectiveness of MMA methods embedded within omnibus treatment packages indicates that they can be used successfully. The scant research on in-session outcomes on using these methods in individual therapy also suggests that patients may find the methods helpful, as do their clinicians. We provide a clinical example of how these strategies might be used in session in Supplemental Materials Table 1. Based on this research evidence, we offer the following practice recommendations:
Consider offering MMA methods to those patients seeking to “accept” or “lean into” presenting problems.
Recommend MMA to patients with common psychological symptoms (e.g., depression, anxiety) as well as those seeking to improve their wellbeing; these groups may be most likely to benefit. Consider integrating MMA methods into individual psychotherapy of various theoretical orientations.
Monitor potential adverse reactions, especially to formal meditation practice, as approximately half of those practicing meditation experience some “unpleasant” effects along with their benefits.
Consider obtaining personal experience and training with MMA methods as they may enable you to anticipate and manage these unpleasant experiences among clients.
Consider administering instruments to assess the effects of MMA methods, monitor client progress, and adjust interventions accordingly (routine outcome monitoring).
Given the limited research related to diversity in MMA methods, clinicians may be advised to apply research-informed principles from the broader multicultural counselling and cultural adaptation literature (e.g., cultural humility and curiosity)
Acknowledgments
This article is adapted, by special permission of Oxford University Press, by the same authors in C. E. Hill & J. C. Norcross (Eds.) (2023), Psychotherapy skills and methods that work. New York: Oxford University Press. The interorganizational Task Force on Psychotherapy Methods and Skills was cosponsored by the APA Division of Psychotherapy/Society for the Advancement of Psychotherapy. The authors are grateful for correspondence with Dr. Kate Morrison regarding the role of acceptance in third-wave cognitive behavioural therapies.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10503307.2023.2209694.
Additional information
Funding
References
- *Studies included in systematic review
- Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
- Baer, R., Crane, C., Miller, E., & Kuyken, W. (2019a). Doing no harm in mindfulness-based programs: Conceptual issues and empirical findings. Clinical Psychology Review, 71, 101–114. https://doi.org/10.1016/j.cpr.2019.01.001
- Baer, R., Crane, C., Montero-Marin, J., Phillips, A., Taylor, L., Tickell, A., & Kuyken, W. (2020). Frequency of self-reported unpleasant events and harm in a mindfulness-based program in two general population samples. Mindfulness, 12(3), 763–775. https://doi.org/10.1007/s12671-020-01547-8
- Baer, R., Gu, J., Cavanagh, K., & Strauss, C. (2019b). Differential sensitivity of mindfulness questionnaires to change with treatment: A systematic review and meta-analysis. Psychological Assessment, 31(10), 1247–1263. https://doi.org/10.1037/pas0000744
- Benish, S. G., Quintana, S., & Wampold, B. E. (2011). Culturally adapted psychotherapy and the legitimacy of myth: A direct-comparison meta-analysis. Journal of Counseling Psychology, 58(3), 279–289. https://doi.org/10.1037/a0023626
- Bernstein, A., Hadash, Y., Lichtash, Y., Tanay, G., Shepherd, K., & Fresco, D. M. (2015). Decentering and related constructs: A critical review and metacognitive processes model. Perspectives on Psychological Science, 10(5), 599–617. https://doi.org/10.1177/1745691615594577
- Biggers, A., Spears, C. A., Sanders, K., Ong, J., Sharp, L. K., & Gerber, B. S. (2020). Promoting mindfulness in African American communities. Mindfulness, 11(10), 2274–2282. https://doi.org/10.1007/s12671-020-01480-w
- Blanck, P., Perleth, S., Heidenreich, T., Kröger, P., Ditzen, B., Bents, H., & Mander, J. (2018). Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: Systematic review and meta-analysis. Behaviour Research and Therapy, 102, 25–35. https://doi.org/10.1016/j.brat.2017.12.002
- Block-Lerner, J., Wulfert, E., & Moses, E. (2009). ACT in context: An exploration of experiential acceptance. Cognitive and Behavioral Practice, 16(4), 443–456. https://doi.org/10.1016/j.cbpra.2009.04.005
- Bodhi, B. (2005). In the Buddha’s words: An anthology of discourses from the Pali canon. Wisdom Publications, Inc.
- Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., Waltz, T., & Zettle, R. D. (2011). Preliminary psychometric properties of the acceptance and action questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. https://doi.org/10.1016/j.beth.2011.03.007
- Britton, W. B., Lindahl, J. R., Cooper, D. J., Canby, N. K., & Palitsky, R. (2021). Defining and measuring meditation-related adverse effects in mindfulness-based programs. Clinical Psychological Science, 9(6), 1185–1204. https://doi.org/10.1177/2167702621996340
- Brown, K., & Ryan, R. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822
- Chawla, N., Collins, S., Bowen, S., Hsu, S., Grow, J., Douglass, A., & Marlatt, G. A. (2010). The mindfulness-based relapse prevention adherence and competence scale: Development, interrater reliability, and validity. Psychotherapy Research, 20(4), 388–397. https://doi.org/10.1080/10503300903544257
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum.
- Cook, J., Biyanova, T., Elhai, J., Schnurr, P., & Coyne, J. (2010). What do psychotherapists really do in practice? An internet study of over 2000 practitioners. Psychotherapy Theory, Research, Practice, Training, 47(2), 260–267. https://doi.org/10.1037/a0019788
- Dahl, C. J., Lutz, A., & Davidson, R. J. (2015). Reconstructing and deconstructing the self: Cognitive mechanisms in meditation practice. Trends in Cognitive Sciences, 19(9), 515–523. https://doi.org/10.1016/j.tics.2015.07.001
- Davis, D. M., & Hayes, J. A. (2011). What are the benefits of mindfulness? A practice review of psychotherapy-related research. Psychotherapy, 48(2), 198–208. https://doi.org/10.1037/a0022062
- Del Re, A. C., Flűckiger, C., Goldberg, S. B., & Hoyt, W. T. (2013). Monitoring mindfulness practice quality: An important consideration in mindfulness practice. Psychotherapy Research, 23(1), 54–66. https://doi.org/10.1080/10503307.2012.729275
- Eichel, K., Gawande, R., Acabchuk, R. L., Palitsky, R., Chau, S., Pham, A., Cheaito, A., Yam, D., Lipsky, J., Dumais, T., & Britton, W. (2021). A retrospective systematic review of diversity variables in mindfulness research, 2000–2016. Mindfulness, 12, 2573–2592.
- Forsyth, J. P., & Eifert, G. H. (2007). The mindfulness and acceptance workbook for anxiety: A guide to breaking free from anxiety, phobias, and worry using acceptance and commitment therapy. New Harbinger Publications, Inc.
- Galante, J., Friedrich, C., Dawson, A. F., Modrego-Alarcón, M., Gebbing, P., Delgado-Suárez, I., Gupta, R., Dean, L., Dalgleish, T., White, I. R., & Jones, P. B. (2021). Mindfulness-based programmes for mental health promotion in adults in nonclinical settings: A systematic review and meta-analysis of randomised controlled trials. PLoS Medicine, 18(1), e1003481. https://doi.org/10.1371/journal.pmed.1003481
- Geller, S. M., Greenberg, L. S., & Watson, J. C. (2010). Therapist and client perceptions of therapeutic presence: The development of a measure. Psychotherapy Research, 20(5), 599–610. https://doi.org/10.1080/10503307.2010.495957
- Goldberg, S. B. (2022). A common factors perspective on mindfulness-based interventions. Nature Reviews Psychology, 1(10), 605–619. https://doi.org/10.1038/s44159-022-00090-8
- Goldberg, S. B., Del Re, A. C., Hoyt, W. T., & Davis, J. M. (2014). The secret ingredient in mindfulness interventions? A case for practice quality over quantity. Journal of Counseling Psychology, 61(3), 491–497. https://doi.org/10.1037/cou0000032
- Goldberg, S. B., Imhoff-Smith, T., Bolt, D. M., Wilson-Mendenhall, C. D., Dahl, C. J., Davidson, R. J., & Rosenkranz, M. A. (2020a). Testing a multi-component, self-guided, smartphone-based meditation app: Three-armed randomized controlled trial. JMIR Mental Health, 7(11), e23825. https://doi.org/10.2196/23825
- Goldberg, S. B., Knoeppel, C., Davidson, R. J., & Flook, L. (2020b). Does practice quality mediate the relationship between practice time and outcome in mindfulness-based stress reduction? Journal of Counseling Psychology, 67(1), 115–122. https://doi.org/10.1037/cou0000369
- Goldberg, S. B., Lam, S., Britton, W. B., & Davidson, R. J. (2022a). Prevalence of meditation-related adverse effects in a population-based sample in the United States. Psychotherapy Research, 32(3), 291–305. https://doi.org/10.1080/10503307.2021.1933646
- Goldberg, S. B., Riordan, K., Sun, S., & Davidson, R. J. (2022b). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science, 17(1), 108–130. https://doi.org/10.1177/1745691620968771
- Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/j.cpr.2017.10.011
- Goldberg, S. B., Tucker, R. P., Greene, P. A., Simpson, T. L., Hoyt, W. T., Kearney, D. J., & Davidson, R. J. (2019). What can we learn from randomized clinical trials about the construct validity of self- report measures of mindfulness? A meta-analysis. Mindfulness, 10(5), 775–785. https://doi.org/10.1007/s12671-018-1032-y
- Goyal, M., Singh, S., Sibinga, E. M., Gould, N. F., Rowland-Seymour, A., Sharma, R., Berger, Z., Sleicher, D., Maron, D. D., Shihab, H. M., Ranasinghe, P. D., Linn, S., Saha, S., Bass, E. B., & Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368. https://doi.org/10.1001/jamainternmed.2013.13018
- Hanley, A. W., & Garland, E. L. (2021). The mindfulness-oriented recovery enhancement fidelity measure (MORE-FM): development and validation of a New tool to assess therapist adherence and competence. Journal of Evidence-Based Social Work, 18(3), 308–322. https://doi.org/10.1080/26408066.2020.1833803
- Hanley, A. W., Warner, A. R., Dehili, V. M., Canto, A. I., & Garland, E. L. (2015). Washing dishes to wash the dishes: Brief instruction in an informal mindfulness practice. Mindfulness, 6(5), 1095–1103. https://doi.org/10.1007/s12671-014-0360-9
- Harned, M. S., Korslund, K. E., Schmidt, S. C., & Gallop, R. J. (2021). The dialectical behavior therapy adherence coding scale (DBT ACS): psychometric properties. Psychological Assessment, 33(6), 552–561. https://doi.org/10.1037/pas0000999
- Harrington, A., & Dunne, J. D. (2015). When mindfulness is therapy: Ethical qualms, historical perspectives. American Psychologist, 70(7), 621–631. https://doi.org/10.1037/a0039460
- Hayes, S. C. (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35(4), 639–665.
- Hayes, S. C., Strosahl, K., & Wilson, K. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. Guilford Press.
- Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., & Strosahl, K. (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. https://doi.org/10.1037/0022-006X.64.6.1152
- Hirshberg, M. J., Frye, C., Dahl, C. J., Riordan, K. M., Vack, N. J., Sachs, J., Goldman, R., Davidson, R. J., & Goldberg, S. B. (2022). A randomized controlled trial of a smartphone-based well-being training in public school system employees during the COVID-19 pandemic. Journal of Educational Psychology, 114(8), 1895–1911. https://doi.org/10.1037/edu0000739
- Hirshberg, M. J., Goldberg, S., Rosenkranz, M. A., & Davidson, R. J. (2022). Prevalence of harm in mindfulness-based stress reduction. Psychological Medicine, 52, 1080-1088. https://doi.org/10.1017/S0033291720002834
- *Horst, K., Newsom, K., & Stith, S. (2013). Client and therapist initial experience of using mindfulness in therapy. Psychotherapy Research, 23(4), 369–380. https://doi.org/10.1080/10503307.2013.784420
- Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. Hyperion.
- Kabat-Zinn, J. (2011). Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemporary Buddhism, 12(1), 281–306. https://doi.org/10.1080/14639947.2011.564844
- Kabat-Zinn, J. (2013). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation (Revised ed.). Piatkus.
- Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., Hayes, R., Huijbers, M., Ma, H., Schweizer, S., Segal, Z., Speckens, A., Teasdale, J. D., Van Heeringen, K., Williams, M., Byford, S., Byng, R., & Dalgeish, T. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: An individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. https://doi.org/10.1001/jamapsychiatry.2016.0076
- Lau, M. A., Bishop, S. R., Segal, Z. V., Buis, T., Anderson, N. D., Carlson, L., Shapiro, S., Carmody, J., Abbey, S., & Devins, G. (2006). The Toronto mindfulness scale: Development and validation. Journal of Clinical Psychology, 62(12), 1445–1467. https://doi.org/10.1002/jclp.20326
- Lindahl, J. R., Fisher, N. E., Cooper, D. J., Rosen, R. K., & Britton, W. B. (2017). The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLOS ONE, 12(5), e0176239. https://doi.org/10.1371/journal.pone.0176239
- Lindsay, E. K., & Creswell, J. D. (2017). Mechanisms of mindfulness training: Monitor and acceptance theory (MAT). Clinical Psychology Review, 51, 48–59. https://doi.org/10.1016/j.cpr.2016.10.011
- Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford Press.
- Linehan, M. M. (2015). DBT skills training manual (2nd ed.). Guilford.
- Longfellow, H. W. (1900). Poems of Henry W. Longfellow. A. L. Burt Company.
- Lutz, A., Slagter, H., Dunne, J., & Davidson, R. (2008). Attention regulation and monitoring in meditation. Trends in Cognitive Science, 12(4), 163–169. https://doi.org/10.1016/j.tics.2008.01.005
- *Mander, J., Blanck, P., Neubauer, A. B., Kröger, P., Flückiger, C., Lutz, W., Barnow, S., Bents, H., & Heidenreich, T. (2019). Mindfulness and progressive muscle relaxation as standardized session – introduction in individual therapy: A randomized controlled trial. Journal of Clinical Psychology, 75(1), 21–45. https://doi.org/10.1002/jclp.22695
- Mander, J., Kröger, P., Heidenreich, T., Flückiger, C., Lutz, W., Bents, H., & Barnow, S. (2015). The process-outcome mindfulness effects in trainees (PrOMET) study: Protocol of a pragmatic randomized controlled trial. BMC Psychology, 3(1), 1–13. https://doi.org/10.1186/s40359-015-0082-3
- *Michaelis, R., Niedermann, C., Reuber, M., Kuthe, M., & Berger, B. (2018). “Seizures have become a means of somehow learning things about myself”—A qualitative study of the development of self-efficacy and mastery during a psychotherapeutic intervention for people with epilepsy. Epilepsy & Behavior, 84, 152–161. https://doi.org/10.1016/j.yebeh.2018.04.019
- Michalak, J., Crane, C., Germer, C. K., Gold, E., Heidenreich, T., Mander, J., Meibert, P., & Segal, Z. V. (2019). Principles for a responsible integration of mindfulness in individual therapy. Mindfulness, 10(5), 799–811. https://doi.org/10.1007/s12671-019-01142-6
- Michalak, J., Steinhaus, K., & Heidenreich, T. (2020). (How) do therapists use mindfulness in their clinical work? A study on the implementation of mindfulness interventions. Mindfulness, 11(2), 401–410. https://doi.org/10.1007/s12671-018-0929-9
- Neff, K. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027
- Nidich, S., Mills, P. J., Rainforth, M., Heppner, P., Schneider, R. H., Rosenthal, N. E., Salerno, J., Gaylord-King, C., & Rutledge, T. (2018). Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: A randomised controlled trial. The Lancet Psychiatry, 5(12), 975–986. https://doi.org/10.1016/S2215-0366(18)30384-5
- Öst, L. G. (2008). Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behaviour Research and Therapy, 46(3), 296–321. https://doi.org/10.1016/j.brat.2007.12.005
- Öst, L. G. (2014). The efficacy of acceptance and commitment therapy: An updated systematic review and meta-analysis. Behaviour Research and Therapy, 61, 105–121. https://doi.org/10.1016/j.brat.2014.07.018
- Quaglia, J. T., Braun, S. E., Freeman, S. P., McDaniel, M. A., & Brown, K. W. (2016). Meta-analytic evidence for effects of mindfulness training on dimensions of self-reported dispositional mindfulness. Psychological Assessment, 28(7), 803–818. https://doi.org/10.1037/pas0000268
- Salzberg, S. (2004). Lovingkindness: The revolutionary art of happiness. Shambala.
- Schumer, M. C., Lindsay, E. K., & Creswell, J. D. (2018). Brief mindfulness training for negative affectivity: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 86(7), 569–583. https://doi.org/10.1037/ccp0000324
- Segal, Z. V., Teasdale, J. D., Williams, J. M., & Gemar, M. C. (2002). The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology and Psychotherapy, 9(2), 131–138. https://doi.org/10.1002/cpp.320
- Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2013). Mindfulness-based cognitive therapy for depression (2nd ed.). Guilford Press.
- Smeets, E., Neff, K., Alberts, H., & Peters, M. (2014). Meeting suffering with kindness: Effects of a brief self-compassion intervention for female college students. Journal of Clinical Psychology, 70(9), 794–807. https://doi.org/10.1002/jclp.22076
- Smith, H. (1991). The world’s religions. HarperCollins Publishers.
- Society of Clinical Psychology. (n.d.). Psychological treatments. https://div12.org/treatments/
- Sun, S., Goldberg, S. B., Loucks, E., & Brewer, J. (2022). Mindfulness-based interventions among racial/ethnic minorities: A systematic review and meta-analysis. Psychotherapy Research, 32(3), 277–290. https://doi.org/10.1080/10503307.2021.1937369
- Tanay, G., & Bernstein, A. (2013). State mindfulness scale (SMS): development and initial validation. Psychological Assessment, 25(4), 1286–1299. https://doi.org/10.1037/a0034044
- Tovote, K. A., Fleer, J., Snippe, E., Peeters, A. C., Emmelkamp, P. M., Sanderman, R., Links, T. P., & Schroevers, M. J. (2014). Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: Results of a randomized controlled trial. Diabetes Care, 37(9), 2427–2434. https://doi.org/10.2337/dc13-2918
- Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., Meissner, T., Lazar, S. W., Kerr, C. E., Gorchov, J., Fox, K. C. R., Field, B. A., Britton, W. B., Brefczynski-Lewis, J. A., & Meyer, D. E. (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. https://doi.org/10.1177/1745691617709589
- Wampold, B., & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge.
- Wasil, A. R., Gillespie, S., Patel, R., Petre, A., Venturo-Conerly, K. E., Shingleton, R. M., Weisz, J. R., & DeRubeis, R. J. (2020). Reassessing evidence-based content in popular smartphone apps for depression and anxiety: Developing and applying user-adjusted analyses. Journal of Consulting and Clinical Psychology, 88(11), 983–993. https://doi.org/10.1037/ccp0000604
- Woods-Giscombé, C. L., & Black, A. R. (2010). Mind-body interventions to reduce risk for health disparities related to stress and strength among African American women: The potential of mindfulness-based stress reduction, loving-kindness, and the NTU therapeutic framework. Complementary Health Review, 15(3), 115–131. https://doi.org/10.1177/1533210110386776
- Yalom, I. D., & Leszcz, M. (2005). The theory and practice of group psychotherapy (5th ed.). Basic Books.