ABSTRACT
This study was conducted to evaluate the prevalence and risk factors for work-related respiratory conditions (asthma, farmer’s lung, sinusitis, rhinitis, and environmental allergies, diagnosed by a physician) among farm and ranch operators in the central US. A survey was conducted by the Central States Center for Agricultural Safety and Health (CS-CASH) in 2018, focusing on work-related injuries, illnesses, exposures, and preventive measures in a seven-state region (Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota). Farms and ranches (n = 16,818) with an email address and annual sales exceeding $5,000 were randomly selected for the survey. Agricultural production and weather data were merged with survey responses. The relationship between exposures and respiratory conditions was analyzed using generalized estimating equations. We received responses from 3,268 agricultural operations (19% response rate) containing information on 4,064 individual operators. The life-time prevalence of (any) respiratory conditions among farm/ranch operators was 18%. Risk factors for respiratory conditions included exposures to grain/hay/feed dust (OR 2.41), animal confinement dust (OR 1.57), field/road dust (OR 2.11), manure/silage gasses (OR 1.66), anhydrous ammonia (OR 1.51), fuels/solvents/paints (OR 1.92), older age group >70 vs. <43 (OR 1.40), female gender (OR 1.82), and being primary vs. third operator (OR 1.61). Farmers and ranchers have a high prevalence of respiratory conditions associated with dust and gas exposures at work. More effective protective measures are needed using the hierarchy of controls, including improved use of respiratory protection.
Introduction
According to the 2017 Census of Agriculture, there were 2,042,220 farms and 3,399,834 individual producers (farm operators, excluding hired labor) engaged in the agricultural industry in the United States (US). A total of 6,577,050 persons lived in the producers’ households, being potentially at risk for injuries and illnesses associated with exposures in the agricultural environment.Citation1 The number of farms has remained relatively unchanged for the past three decades, but major changes have occurred in agricultural production, particularly in the livestock sector, which has concentrated into fewer larger units. Nearly half of the farms (43%) still have cattle and calves, but only 3.2% have dairy production, and 2.7% have swine production.Citation1 The number of farms growing field crops has also decreased. The land area used for corn and soybean production has increased while most other crops have decreased. Technology has replaced much of the manual labor, but larger agricultural operations rely increasingly on hired labor.
Respiratory conditions are one of the most important occupational health hazards for farmers, and numerous studies have addressed the prevalence, characteristics, exposures, and prevention of respiratory conditions, especially among livestock producers. A chapter by Donham and ThelinCitation2 provides an overview of respiratory conditions in agriculture, hazards related to dust, gasses, and chemicals in different types of work settings, based on their work, and a review of over 150 studies. Much of this research has focused on exposures and health conditions among confined animal feeding operation (CAFO) workers. With the structural, technological, and demographic changes in agriculture, it is essential to conduct research and surveillance to see if progress has been made and if new hazards may be emerging.
This study focuses on respiratory conditions among self-employed farmers and ranchers who represent most of the agricultural workforce in the US. Farmers have a unique work environment and lifestyle compared to the general population in terms of lower smoking rates, intense physical activity, and exposure to a wide variety of hazards at work.Citation2 These differences have both positive and negative effects on farmers’ health, including respiratory conditions. The average age of the US farm and ranch operators was 57.5 years in 2017,Citation1 and older age adds vulnerability to adverse health outcomes. Respiratory illnesses such as chronic bronchitis, asthma, hay fever, organic dust toxic syndrome, and hypersensitive respiratory symptoms are prevalent in agricultural workers.Citation3,Citation4 Their age, gender, and race adjusted Proportionate Mortality Ratio (PMR) is significantly higher for acute respiratory infections (APMR 124, 95% CI 111–138) and pneumonia/influenza (APMR 109, 95% CI 107–111).Citation5
Respiratory conditions among farmers could be triggered by multiple factors like physiologic (age, gender, genetic factors), occupational (exposure to air contaminants in raising crops and livestock), and environmental (relative humidity, wind, temperature, pollen) factors.Citation6,Citation7
Individuals engaged in the agriculture industry perform tasks that differ from non-farming industries in terms of exposure potential to antigens from plant and animal sources, resulting in high dust hour/day-exposure indices.Citation5 Personal dust exposure concentrations vary daily depending on the work task; for instance, high concentrations have been measured in land preparation (disking),Citation8 cleaning grain bins, and moving and sorting animals.Citation1 Further, low relative humidity, high wind speed, and high soil temperature are associated with higher dust particle exposure in crop and livestock farmers.Citation8,Citation9
Exposure to organic agricultural dust results in an antigen-antibody reaction that can trigger immune responses that lead to respiratory tract inflammation.Citation10 Individuals involved in agricultural activities, due to their exposure to agricultural allergens, often develop hypersensitive IgE immune reactions.Citation11,Citation12 Individuals with genetic factors linked to overexpression of IgE in response to multiple environmental factors are vulnerable to developing hay fever and asthma.Citation13
The current literature is inconsistent in describing the relationship between respiratory conditions and occupational farming exposures. A systematic review to describe the relationship between agricultural organic dust and respiratory illness identified eight studies with a positive association, five studies with a negative association, and two with no effect.Citation14 Many studies did not address physiologic, occupational, and environmental factors in combination.
In the current study, based on the 2018 Farm and Ranch Health & Safety Survey (FRHSS) responses, we aimed to evaluate the life-time prevalence of physician-diagnosed respiratory conditions among farmers and ranchers and the relationship between occupational exposures and adverse respiratory conditions. The analysis included physiologic, occupational, environmental, and climatic factors that have the potential to exacerbate farmers’ respiratory conditions. This multi-factorial approach could strengthen the evidence on the association between occupational exposures and respiratory conditions.
Methods
This study used information from three different sources: Farm and Ranch Health and Safety Survey (FRHSS), Farm Market iD (FMiD) database of agricultural operations, and the North American Regional Reanalysis (NARR) climate database.
The Central States Center for Agricultural Safety and Health (CS-CASH) implemented the FRHSS in a seven-state region: Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, and South Dakota. The surveys were conducted via email and mail during the spring and summer of 2018, requesting responses for up to three individual operators on each farm or ranch. The survey included 29 questions on farmer demographics, type/intensity of farm-related activities, farm-related injury and illness outcome information, agricultural occupational and environmental exposures, and personal protective practices.
In the first phase of the study, we emailed operators a link to an online survey, followed by a reminder email to the non-respondents. In the second phase, we conducted a mail survey to a randomly selected subset of the farms/ranches that did not respond to the electronic survey with one mail reminder to non-respondents. All data were entered and stored electronically in REDCap.Citation15
We obtained a dataset from FMiD, which contained farm contact information and crop and animal production data. FMiD is a private organization that collects information on farms and ranches and processes it for use by farmers and organizations that provide products and services to farms and ranches. FMiD selected operations randomly from their grower database, stratified by state, limiting the selection to those farms with a valid email address and gross farm income of $5,000 or more to focus on active farms. FMiD contact information was used for sending email and mail surveys to potential respondents.
The NARR dataset contained temperature, wind, moisture, soil, and other parameters with a spatial resolution of 32 km. From this dataset, we extracted the mean relative humidity (RH) for the year 2017 for each geographic grid point in the US. Further, we calculated the area average of mean relative humidity for each county for the seven states and merged it with the FMiD data set. We then joined FRHSS, FMiD, and NARR data for each operation and constructed an operator-level dataset for analyses using Oracle MySQL Workbench-community edition, version 6.1.7.
The outcome variable was constructed from the question: “Has the operator ever been diagnosed by a physician with any of the following respiratory conditions?”. Possible responses were none, chronic obstructive pulmonary disease (COPD), asthma, farmer’s lung, sinus diseases (sinusitis), nasal inflammation/runny nose (rhinitis), and environmental allergies. The outcome variable was dichotomized as the presence or absence of any respiratory condition after excluding COPD. Among the six respiratory conditions documented in this study, COPD was excluded due to its strong association with smoking, rather than exposure to other air pollutants.
The primary exposure variables were obtained from the question: “Was the operator exposed to high levels of the following air contaminants in the past 12 months?”. Possible responses were none, grain/feed/hay dust, animal confinement dust, field/road dust, manure/silage gases, anhydrous ammonia, fuel/solvent/paints, and others.
Additional exposures included age (converted to 4 categories using K-means clustering: 14–42, 43–58, 59–69, 70–96), gender (male or female), primary occupation (farm/ranch or other), percent of the farmer’s work time involved in farm/ranch activity in the past 12 months (0–24, 25–49, 50–74, 75–99, 100), presence or absence of major crops (e.g., corn, sorghum, wheat) and livestock, and mean relative humidity (in percent) for the year 2017 by county-level geographical information. Respiratory protection was measured with the question: “When exposed to high levels of air contaminants at work, what percentage of that time did the operator use proper respiratory protection (including N95 masks, half masks with dust/gas filter)” and dichotomized as 50% or lower versus greater than 50%.
Descriptive statistics were tabulated to summarize respondent, exposure, and outcome characteristics. Crude and adjusted odds ratios were calculated to identify risk factors for respiratory conditions, including exposure status, age-group, gender, operator’s primary work activity, operator level, farm type, and relative humidity.
The relationships of exposure variables and respiratory conditions were evaluated using generalized estimating equations (GEE) with an exchangeable correlation matrix and with operators clustered within the same farm/ranch operation. The GEE (S-function, version 4.13) function was used from the GEE library version 4.13–20 using R version 3.5.2.Citation16,Citation17 Both crude and adjusted odds ratios were calculated, and the final statistical model was adjusted for age-group, gender, operator’s primary activity, operator level, farm type, relative humidity, animal confinement dust, field/road dust, manure/silage gases, anhydrous ammonia, and fuel/solvents/paint exposures.
Geographic hotspot analysis (Getis-Ord Gi* method) based on the rate of operators diagnosed with respiratory conditions by the farm was conducted using an unsupervised machine learning technique. We used the fixed distance (50 miles) band for the spatial relationship with the Euclidean distance to identify cold spots and hotspots.Citation18 Additionally, the hotspot and cold spot clusters were adjusted using the false discovery rate in ArcGIS Pro version 2.6.0.Citation19
Results
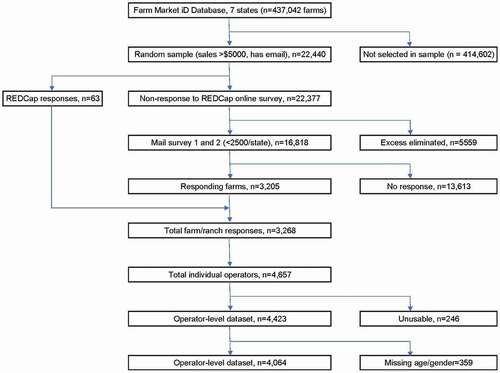
The numbers of responses to the 2018 Farm and Ranch Health and Safety Survey (FRHSS) from phase 1 (email/online survey) and phase 2 (mail survey) are presented in . The overall response rate (calculated from the mail survey population) was 19.4% (n = 3,268 operations and 4,064 operators). The agricultural production characteristics of the responding/non-responding operations were similar: the presence of any livestock 46/46%; cow-calf 16/16%; dairy 5/5%; wheat 40/47%; corn 90/89%; soybeans 86/84%, and hay production 67/69%, respectively. The usable responses included information on 4,064 farmers/ranchers distributed across seven Midwestern states included in the survey as follows: Nebraska (n = 909), Iowa (n = 711), Minnesota (n = 585), South Dakota (n = 558), Kansas (n = 498), North Dakota (n = 448) and Missouri (n = 355). Nearly all responses were received via mail (n = 3,978, 97.8%) vs. email/online (n = 63, 2.2%). About 85% of the respondent sites were farms (n = 3,468), while 11.5% were ranches (n = 471), and 3% were both farming and ranching operations (n = 125).
Figure 1. Study flowchart. This figure provides a systematic overview of the respondents included in this study.
Farm characteristics
The median cereal grain acreages (field corn, rice, sorghum, barley, millet, wheat, rye, oats, and sorghum sweet) were highest in North Dakota (513 acres) and Kansas (377 acres). Nebraska (median acreage: 43) and North Dakota (median acreage: 18) had the most oil crops (sunflowers, canola, castor beans, safflower). Livestock (cow/calf, fed cattle, replacement heifers, dairy, hogs, sheep, horses, goats, mohair, and wool) herds were the largest in South Dakota (median number of animals: 146) and Minnesota (median: 120).
Farmer and exposure characteristics
Among 4,064 operators, 69% were first (primary) operators, 24% second operators, and 7% third operators (). The proportion of male operators was higher among all three operator classes (98%, 52%, and 84% among first, second, and third operators, respectively). The median age of first operators was 61 years, second operators were 53 years, and third operators were 34 years. More than half (57%) of the farmers/ranchers reported exposure to grain/feed/hay dust, including 59% of primary operators, 52% of second operators, and 59% of third operators ().
Table 1. Organic (grain/hay/feed) dust exposure by age, operator status and gender.
Exposure to grain/feed/hay dust was associated with the proportion of work time in farming/ranching (vs. other occupation): 61%, 60%, 57%, 48%, and 25% among operators working full time, 99–75% time, 74–50% time, 50–25% time, and <25% time on the farm/ranch, respectively. Operators who spent more than 50% of their work time on farm/ranch activities were exposed to grain/hay/feed dust more frequently (60%, n = 2,002) than operators primarily engaged in other occupational activities (40%, n = 1,300).
Approximately half of the operators (54% primary, 49% second, and 51% third) reported using appropriate respiratory protection (N95 dust mask or half mask with dust/gas filters) more than 50% of the time when exposed to high levels of air contaminants.
The mean annual relative humidity among the seven Midwestern states ranged between 47.8–78.2%. Among the Midwestern states Minnesota, Iowa and Missouri were with higher RH conditions than the western part of North Dakota, South Dakota, Nebraska, and Kansas, which were low RH. The majority of the farms/ranches included in this study were concentrated in areas with higher relative humidity, 69% operations with RH between 60–70%, and 14% operations with RH 70–78% (S. 1).
Respiratory conditions
Among 4,064 respondents, 734 farmers/ranchers reported being diagnosed with at least one respiratory condition (asthma, farmer’s lung, sinusitis, rhinitis, environmental allergies). The prevalence of (any) respiratory conditions among farmers/ranchers was 18%. Respiratory conditions were more common among primary and secondary operators (18%) than third operators (13%).
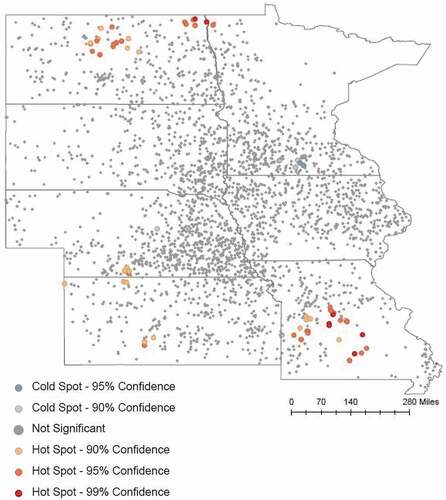
Environmental allergy was the most commonly reported respiratory condition (9%), followed by rhinitis (5%) (). A total of 165 (6%) principal operators, 47 (5%) second operators, and nine (3%) third operators reported being diagnosed with more than one respiratory condition. There were five geographical hotspots in North Dakota, Nebraska, Kansas, and Missouri for respiratory conditions (). Spatial exploratory regression showed that respiratory condition rates were significantly correlated with the number of acres per farm in row crop production and the number of cows/calves livestock on a farm/ranch. Large farm operations (median: 18,047 acres) growing row crops overlapped geographically with the hotspot clusters in North Dakota, Nebraska, and Kansas.
Table 2. Respiratory conditions among operators by state and organic grain/hay/feed) dust exposure.
Figure 2. Hotspot analysis- Rate of respiratory conditions in central states. This figure was generated using the Getis-ord hotspot analysis method. Each dot represents a farm (up to 3 operators), and the clustering is based on the rate of respiratory conditions per farm to identify the hot spot (vulnerable to respiratory illness). The red dots represent vulnerability to respiratory illness, and the blue dots represent protectiveness to respiratory illness.
Risk factors for respiratory conditions
The adjusted odds of respiratory conditions were higher among those exposed to organic plant-based grain/hay/feed dust exposure compared to exposures with other respiratory contaminants. Operators exposed to grain/hay/feed dust had more than twice the odds of developing respiratory conditions than the unexposed group (AOR 2.41, 95% CI 2.00–2.90). The odds for respiratory conditions increased by age and were the highest among 70–96-year-old participants (AOR 1.40; 95% CI 1.01–1.94). Females had higher odds of respiratory conditions compared to male operators (AOR 1.82, 95% CI 1.35–2.45). Participants from dual (farm/ranch) operations had higher odds of reporting respiratory conditions compared to those from single (farms or ranch) operations (). Additionally, the operators exposed to plant-based organic dust had higher odds of developing all the respiratory conditions included in the study (). More frequent use (more than 50% of the time) of respiratory protection during farm/ranch activities was not protective against respiratory conditions (AOR: 0.96, 95% CI 0.79–1.15). The majority (69%) of the farm/ranch operations were located under a geographic area with RH between 60–70%, and regression analyses showed no significant associations between respiratory conditions and RH.
Table 3. Risk factors for respiratory conditionsa (n = 4,064).
Table 4. Association of plant-based organic dust and respiratory conditions (n = 4,064).
Discussion
Agricultural work practices in the US are changing, influenced by technology, ownership changes, and renting of land. Custom contract work has made it possible to do greater proportions of tillage, planting, crop protection, and harvesting work with larger machinery and fewer workers. Much of the crop production work can be done in cabs with air conditioning and filtration, where exposures to air contaminants are well controlled.Citation20 Animal production work has also undergone major changes where the number of livestock operations has fallen, and production has shifted to larger and more specialized operations.Citation21 Many studies have been done in previous years on air contaminants and respiratory conditions in agriculture, particularly among animal confinement workers.Citation22 However, continued changes in work practices create a need for re-evaluating the risk of respiratory conditions and exposures among agricultural workers. This study evaluated the prevalence of common work-related respiratory conditions and the relationship between agricultural air contaminants and respiratory conditions among farmers and ranchers in the central US, adjusted for demographic and production factors.
Prevalence of respiratory conditions
The life-time prevalence of common agricultural work-related respiratory conditions (asthma, farmer’s lung, sinusitis, rhinitis, and environmental allergies) was evaluated from responses to the 2018 FRHSS survey. Of the respondents, 18% reported having at least one of the listed conditions diagnosed by a physician. The disease-specific prevalence varied, being highest for environmental allergies (8.5%), and followed by rhinitis (5.4%), sinusitis (4.9%), asthma (4.4%), and farmer’s lung (2.2%). Similar results have been reported in studies based on self-reported physician-diagnosed life-time prevalence of respiratory conditions. Asthma was most prevalent (7.2%) and farmer’s lung least prevalent (1.2%) among the 43,548 participants (pesticide applicators and their spouses) in the Agricultural Health Study during 2005–2010.Citation23 The 2011 Farm and Ranch Safety Survey (FRSS) (n = 11,210 primary operators) identified asthma prevalence as 5.1% among all US operators, and 4.3% among midwestern operators.Citation24 In a study of 178 crop farmers from eastern North Carolina, 7% of the participants were diagnosed with asthma by a physician, while 6% had sinusitis and 1% had rhinitis.Citation25
Compared to our finding (5.4%), Mazurek et al. reported a much higher life-time prevalence of rhinitis: 31% among primary operators in the US and 28% in midwestern farmers.Citation24 Other studies have found that rhinitis is prevalent among pesticide applicators.Citation26,Citation27 However, this does not explain the difference between 63% of farmers/ranchers in our study and 40% of farmworkers in Mazurek’s study reported pesticide exposures.
The 1996–2001 Medical Expenditure Panel Survey results showed that farmers often encounter problems finding affordable health insurance, and this could lead to a decline in health care service utilization.Citation28 In 2015, 89.3% of farmers had health insurance; 28.2% from government, 17.6% from private, and 55.6% from employment-based sources.Citation29 As farmers often have high premiums and high deductible health insurance policies, the use of health care services among farmers could be lower than in non-farmers. The factors associated with farmers’ health care accessibility could trigger under-reporting of physician-diagnosed respiratory conditions among farmers in general and in the current study. Additionally, the prevalence rate in this study could be an underestimate, as the FRHSS survey was focused on operators from active farm operations with gross income of at least $5,000. This limitation could result in a ‘healthy worker effect. Previous research has shown that respiratory conditions are more common among those who are not in active employment.Citation30
Respiratory exposures
Agricultural workers are exposed to a variety of air contaminants. In our study, we focused on six types: grain/hay/feed dust (plant-based organic dust), animal confinement dust (mix of animal and plant-based organic dust), field/road dust (inorganic dust including silica), manure/silage gases (gases in animal production), anhydrous ammonia (irritant fertilizer vapor/gas), and fuel/solvents/paints (volatile organic compounds).
We hypothesized that farm/ranch operators are at a higher risk for respiratory conditions if exposed to specific hazardous air contaminants. We could not quantify the exposures in a survey while recognizing that the concentrations can vary, and the exposure duration can range from short-term to intermediate or long-term based on the tasks performed.Citation2,Citation31 The health effects also vary depending on the type of exposure and individual susceptibility. For example, acute exposure to moldy grain, hay, and other organic material can cause organic dust toxic syndrome (ODTS).Citation2 Long-term exposure (regular work) to lower levels of various dust, gases, aerosols, and atmospheric conditions can lead to respiratory hypersensitive reactions.Citation32,Citation33
Our results indicated that the odds of (any) respiratory conditions were significantly higher among operators exposed to each air contaminant in the study. Farm/ranch operators exposed to organic dust from plant sources (grain, feed, hay) had 2.41 times higher adjusted odds of being diagnosed with respiratory conditions than the unexposed. This finding aligns with prior studies.Citation34–36 Dorribo et al. identified an increased risk of acute respiratory symptoms with wheat dust exposure among Swiss farmers.Citation34 A study of 2,203 New Zealand farmers found increased odds of respiratory illness (OR: 1.8–2.2) in operators exposed to grain/hay dust.Citation35 Field wheat dust exposure increased the risk of respiratory symptoms among Swiss farmers compared to farmers handling storage wheat for cattle feeding purposes.Citation36
Organic grain/hay/feed dust exposure was associated with all five specific diseases in this study, with the highest adjusted odds for sinusitis (3.00) and lowest for asthma (1.68). Asthma can be related to various exposures, and the specific occupational exposures in our study could be only a few among many other contributing factors. Occupational exposures may play a prominent role in causing other respiratory illnesses, especially for farmers’ lung.Citation2
The adjusted odds of respiratory conditions among female farm operators were about double compared to male operators. A meta-analysis, which included farm operators, identified similar results where the odds of occupational asthma, sinusitis, throat irritation, nasal dryness, and nasal catarrh were higher among female operators.Citation37
Approximately 50% of the farmers and ranchers had used respiratory protection more than half of the time when exposed to high air contaminant levels at work. This percentage is lower than the results reported in 2006 FRSS (73%) but higher than the 2011 FRSS (35%) for the Midwestern region.Citation38,Citation39 Regression analysis found no association between respiratory protection and respiratory conditions. This finding does not preclude the possibility that healthy farmers may be less inclined to use protection while farmers with symptoms may become motivated about respiratory protection.
Climate conditions, including temperature, relative humidity, and rainfall, could exacerbate adverse respiratory conditions among farmers directly. Climate can also have indirect effects on occupational exposures as climate influences agricultural practices and types of crops and animals raised in a particular geographic area. Most (~70%) of the operations included in this study were concentrated in an area with RH between 60–70%. We found no association between respiratory conditions and relative humidity. This could be due to the low sample size in low and high humidity regions and relatively similar agricultural practices on most operations in this study area. A study design comparing operators from inland and coastal regions could provide further insights into the risk of respiratory conditions attributable to climate conditions.
Finally, we applied the hotspot analysis as an alternative approach to assess the differences in the prevalence of respiratory conditions in smaller geographic areas that could be influenced by the climate and local agricultural practices. We observed five hotspot clusters for respiratory conditions in the seven Midwestern states. The driving factors behind these respiratory condition hotspots would require further study with additional agricultural production and environmental exposure data. Each hotspot may have unique exposures, as the identified areas overlap with different production types, including grain, sugar beet, feed yard, poultry, and hog. As the associations were based on a spatial exploratory regression approach, the results could be uncertain, and a robust spatial-temporal model would be required to identify the factors associated with respiratory condition hotspots.
Strengths and limitations
The strengths of this study include having a well-defined randomly selected study population in a large geographical area that represents about one-fifth of the farms/ranches in the US. Our survey method enabled conducting a short survey while merging existing agricultural production and climate information from secondary databases. Another strength was the ability to compare agricultural production profiles between respondents and non-respondents. While the response rate was low (19.4%), the differences in agricultural production variables between respondents and non-respondents were small. This could suggest that the risk of biases from non-response is fairly low. A previous analysis of non-response bias in the 2018 sample found no evidence that responders differed from non-responders on farm or ranch characteristics Respondents were more likely to be married than non-responders, but no other demographic differences were identified.Citation40 Overall, the merged combined research dataset contained detailed information on operator demographics, crops, animals raised, hazardous agricultural exposures, and adverse health outcomes from a large analytic sample of 4,064 farm/ranch operators.
The FRHSS questions addressed several common respiratory health outcomes (asthma, farmer’s lung, sinusitis, rhinitis, and environmental allergies) and several common agricultural occupational exposures (grain/feed/hay dust, animal confinement dust, field/road dust, manure/silage gases, anhydrous ammonia, and fuel/solvent/paint exposures). We excluded chronic obstructive pulmonary disease (COPD), which is primarily caused by cigarette smoking and genetic susceptibility.Citation41 Our primary outcomes (asthma, farmer’s lung, sinusitis, rhinitis, and environmental allergies) are more clearly associated with occupational exposures.
The limitations of the study include self-reporting, which could introduce biases that we could not quantify. The response for the respiratory outcomes was based on “ever” diagnosed by a physician, whereas the exposure information was based on the “past 12 months” and this, along with the cross-sectional study design, does not enable establishing a temporal connection between cause and effect. It is uncertain how well self-reporting exposure conditions reflect real-life exposures vs. quantifying them with standard industrial hygiene methods, which would be exceedingly expensive for this size study.
Additionally, the FRHSS survey does not contain information on smoking or vaping tobacco products or second-hand smoke exposure, which are significant contributors to respiratory conditions.Citation42–44 The results from this study could be influenced by information bias due to missing information on smoking habits, which could result in nondifferential exposure misclassification. As the study results are not adjusted for the confounding effect of smoking or vaping, the study results could be influenced by type-1 error.
Missing information affected the analyses to some extent; missingness being 5.5% for farm operation information, 0.5% for age, 1.2% for gender, 1.5% for occupation, 1.6% for percent of the total work time in farm/ranch activities, and 20.3% for the usage of personal protective equipment. The information related to respiratory exposures and outcomes was complete among all responses received.
Conclusion
This study assessed the relationship between occupational exposures and respiratory conditions among farmers and ranchers in a seven-state region of the central US. We received responses from 3,268 farm operations (rate 19.4%) that included information on 4,064 individual operators. The prevalence of (any) respiratory conditions among farm/ranch operators was 18%. Respiratory exposure to grain/feed/hay dust more than doubled the odds (AOR: 2.41, 95% CI 2.00–2.90) of respiratory condition. Older age increased the odds of respiratory conditions, and the odds were twice as high for female operators compared to males. Primary operators had higher odds of respiratory conditions compared to second and third operators. All six air contaminant types in the study increased to odds of respiratory conditions. The annual average relative humidity varied only slightly in the study region and had no association with respiratory conditions.
Overall, farmers and ranchers have a high prevalence of respiratory conditions, which are associated with dust and gas exposures at work. More effective protective measures are needed using the hierarchy of controls, including improved use of respiratory protection.
Acknowledgments
We would like to acknowledge Kaeli Samson, Dr. Abadi, and the CS-CASH team for supporting the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- USDA. 2017. Census of agriculture. United States. Summary and state data. Volume 1. Geographic Area Series. Part 51. https://www.nass.usda.gov/Publications/AgCensus/2017/Full_Report/Volume_1,_Chapter_1_US/usv1.pdf.
- Donham KJ, Thelin A. Agricultural respiratory diseases. In: Donham KJ, Thelin A, eds. Agricultural Medicine: Rural Occupational and Environmental Health, Safety, and Prevention. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc; 2016:95–154.
- Iversen M, Dahl R, Korsgaard J, Hallas T, Jensen EJ. Respiratory symptoms in Danish farmers: an epidemiological study of risk factors. Thorax. 1988;43(11):872–877. doi:10.1136/thx.43.11.872.
- Respiratory disease in agricultural workers: mortality and morbidity statistics. Nat Inst Occup Safe Health (NIOSH). 2007. https://www.cdc.gov/niosh/docs/2007-106/pdfs/2007-106.pdf?id=10.26616/NIOSHPUB2007106.
- Wu JD, Nieuwenhuijsen MJ, Samuels SJ, Lee K, Schenker MB. Identification of agricultural tasks important to cumulative exposures to inhalable and respirable dust in California. AIHA J. 2003;64(6):830–836. doi:10.1080/15428110308984879.
- Cooper JD. Occupational asthma, byssinosis, and industrial bronchitis. In: Grippi MA, Elias JA, Fishman JA, et al., eds. Fishman’s Pulmonary Diseases and Disorders. 5th ed. https://accessmedicine-mhmedical-com.ezproxy.unmc.edu/content.aspx?bookid=1344§ionid=81194770.
- Balmes JR. Occupational lung diseases. In: LaDou J, Harrison RJ, eds. CURRENT Diagnosis & Treatment: Occupational & Environmental Medicine. 6th ed. McGraw-Hill. https://accessmedicine-mhmedical-com.ezproxy.unmc.edu/content.aspx?bookid=3065§ionid=255652307. Accessed May 19, 2021.
- Nieuwenhuijsen MJ, Schenker MB. Determinants of personal dust exposure during field crop operations in California agriculture. Am Ind Hyg Assoc J. 1998;59(1):9–13. doi:10.1080/15428119891010271.
- Papanastasiou DK, Fidaros D, Bartzanas T, Kittas C. Monitoring particulate matter levels and climate conditions in a Greek sheep and goat livestock building. Environ Monit Assess. 2011;183(1–4):285–296. doi:10.1007/s10661-011-1921-1.
- Kishiyama JL, Chang JJ, Donovan SM. Disorders of the immune system. In: Hammer GD, and McPhee SJ, eds. Pathophysiology of Disease: An Introduction to Clinical Medicine, 8th Vol. China: McGraw-Hill Education, 31–60; 2019.
- Barrett KE, Barman SM, Brooks HL, Yuan JXJ. Immunity, infection, & inflammation. In: Ganong’s Review of Medical Physiology, 26th Vol. USA: McGraw-Hill Education, 67–84; 2019.
- Poole JA. Farming-associated environmental exposures and effect on atopic diseases. Ann Allergy Asthma Immunol. 2012;109(2):93–98. doi:10.1016/j.anai.2011.12.014.
- Janeway CA, Travers P, Walport M, Shlomchik MJ. Immunobiology: The Immune System in Health and Disease. 5th ed. New York, USA: Garland Science; 2001.
- Wunschel J, Poole JA. Occupational agriculture organic dust exposure and its relationship to asthma and airway inflammation in adults. J Asthma. 2016;53(5):471–477. doi:10.3109/02770903.2015.1116089.
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208–103208. doi:10.1016/j.jbi.2019.103208.
- Generalized Estimation Equation Solver. CRAN. https://cran.r-project.org/web/packages/gee/gee.pdf. 2019. Accessed Oct 9, 2019.
- Agresti A. An Introduction to Categorical Data Analysis. Vol. 3. Hoboken, NJ: John Wiley & Sons; 2018.
- Ord JK. The analysis of spatial association by use of distance statistics. Geog Anal. 2010;24(3):189–206. doi:10.1111/j.1538-4632.1992.tb00261.x.
- Caldas de Castro M, Singer BH. Controlling the false discovery rate: a new application to account for multiple and dependent tests in local statistics of spatial association. Geog Anal. 2006;38(2):180–208. doi:10.1111/j.0016-7363.2006.00682.x.
- Conkin PK. A Revolution down on the Farm: The Transformation of American Agriculture since 1929. Lexington, KY: University Press of Kentucky; 2008.
- USDA ERS. 2020. Livestock production practices. US Department of Agriculture. https://www.ers.usda.gov/topics/farm-practices-management/crop-livestock-practices/livestock-production-practices/.
- Mazurek JM, White GE, Rodman C, Schleiff PL. Farm work-related asthma among US primary farm operators. J Agromedicine. 2015;20(1):31–42. doi:10.1080/1059924X.2014.976729.
- Hoppin JA, Umbach DM, Long S, et al. Respiratory disease in United States farmers. Occup Environ Med. 2014;71(7):484–491. doi:10.1136/oemed-2013-101983.
- Mazurek JM, Henneberger PK. Life-time allergic rhinitis prevalence among US primary farm operators: findings from the 2011 farm and ranch safety survey. Int Arch Occup Environ Health. 2017;90(6):507–515. doi:10.1007/s00420-017-1217-z.
- Akpinar-Elci M, Pasquale DK, Abrokwah M, Nguyen M, Elci OC. United airway disease among crop farmers. J Agromedicine. 2016;21(3):217–223. doi:10.1080/1059924X.2016.1179239.
- Patel O, Syamlal G, Henneberger PK, Alarcon WA, Mazurek JM. Pesticide use, allergic rhinitis, and asthma among US farm operators. J Agromedicine. 2018;23(4):327–335. doi:10.1080/1059924X.2018.1501451.
- Slager RE, Poole JA, LeVan TD, Sandler DP, Alavanja MC, Hoppin JA. Rhinitis associated with pesticide exposure among commercial pesticide applicators in the agricultural health study. Occup Environ Med. 2009;66(11):718–724. doi:10.1136/oem.2008.041798.
- Zheng X, Zimmer DM. Farmers’ health insurance and access to health care. Am J Agric Environ. 2008;90(1):267–279. doi:10.1111/j.1467-8276.2007.01041.x.
- USDA Economic Research Service. Health insurance coverage. 2019. https://www.ers.usda.gov/topics/farm-economy/farm-household-well-being/health-insurance-coverage/. Accessed July 11, 2021.
- Senthilselvan A, Coonghe WVL, Beach J. Respiratory health, occupational and the healthy worker effect. Occup Med. 2020;70(3):191–199. doi:10.1093/occmed/kqaa023.
- Schenker MB, Christiani D, Cormier Y, et al. Respiratory health hazards in agriculture. Am J Respir Crit Care Med. 1998 Nov;158(5):S1–S76. doi:10.1164/ajrccm.158.supplement_1.rccm1585s1.
- Guillam MT, Pédrono G, Le Bouquin S, et al. Chronic respiratory symptoms of poultry farmers and model-based estimates of long-term dust exposure. Ann Agric Environ Med. 2013;20:307–311.
- Arcury TA, Quandt SA. Chronic agricultural chemical exposure among migrant and seasonal farmworkers. Soc Nat Resour. 1998;11(8):829–843. doi:10.1080/08941929809381121.
- Dorribo V, Wild P, Pralong JA, et al. Respiratory health effects of fifteen years of improved collective protection in a wheat-processing worker population. Ann Agric Environ Med. 2015;22(4):647–654. doi:10.5604/12321966.1185768.
- Kimbell-Dunn MR, Fishwick RD, Bradshaw L, Erkinjuntti-Pekkanen R, Pearce N. Work-related respiratory symptoms in New Zealand farmers. Am J Ind Med. 2001;39(3):292–300. doi:10.1002/1097-0274(200103)39:3<292::aid-ajim1017>3.0.co;2-f.
- Barrera C, Wild P, Dorribo V, et al. Exposure to field vs. storage wheat dust: different consequences on respiratory symptoms and immune response among grain workers. Int Arch Occup Environ Health. 2018;91(6):745–757. doi:10.1007/s00420-018-1322-7.
- Schachter EN, Zuskin E, Moshier EL, et al. Gender and respiratory findings in workers occupationally exposed to organic aerosols: a meta analysis of 12 cross-sectional studies. Environ Health. 2009;8(1):1. doi:10.1186/1476-069X-8-1.
- Syamlal G, Schleiff PL, Mazurek JM, Doney B, Greskevitch M. Respirator use among US farm operators: evidence from the 2006 Farm and Ranch Safety Survey. J Agromedicine. 2013;18(1):27–38. doi:10.1080/1059924X.2012.743379.
- Casey ML, Mazurek JM. Respirator use among US farm operators with asthma: results from the 2011 farm and ranch safety survey. J Agromedicine. 2017;22(2):78–88. doi:10.1080/1059924X.2017.1282904.
- Beseler C, Rautiainen RH. Assessing nonresponse bias in farm injury surveillance data. J Agri Safe Health. In press. doi:10.13031/jash.14554.
- Silverman EK, Crapo JD, Make BJ. Chronic obstructive pulmonary disease. In: Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, and Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 20th ed. USA: McGraw-Hill Education 1990–1998 ; 2018.
- National Center for Chronic Disease Prevention Health Promotion. Office on Smoking Health. Health Effects of Cigarette Smoking (Updated Jan. 2008). Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2008.
- Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. doi:10.1161/CIRCULATIONAHA.114.007667.
- Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2017 Feb 1;46(1):32–43. doi:10.1093/ije/dyw021.
