ABSTRACT
Background
Cardiac rehabilitation (CR) has been successful in improving exercise capacity (EC) and quality of life (QoL). However, depression and anxiety are highly prevalent among cardiac patients and might represent risk factors for rehabilitation outcomes. The aim of this study was to investigate the role of depression and anxiety as possible independent risk factors for CR outcomes.
Methods
The study applied a pre-post-design. The sample comprised N = 3’434 cardiac disease patients taking part in a Swiss inpatient CR center. Variables measured at the beginning (T1) and end of rehabilitation (T2) included depression and anxiety (HADS), EC, and QoL (MacNew). A path analysis was conducted.
Results
Depression at T1 had a significant negative relationship with improvements in EC and in all aspects of QoL during rehabilitation. Anxiety at T1 was positively related to improvements in EC and in emotional and physical QoL. Improvements in depression during CR were positively related with improvements in all outcomes. Improvements in anxiety showed no significant association with the outcomes.
Conclusion
Depression and anxiety should be screened for during CR. Depression should be treated due to the negative association found with rehabilitation outcomes. Underlying mechanisms of the positive association of anxiety with rehabilitation outcomes need further investigation.
Introduction
Cardiac disease is the most frequent cause of death and disability worldwide (Khan et al., Citation2020). It is mainly caused by a combination of lifestyle risk factors, such as physical inactivity, smoking, leading an unhealthy diet, and stress (Knoll et al., Citation2017). Cardiac rehabilitation (CR) programs aim at providing patients with a strong basis to lead a healthy lifestyle and, thus, at improving exercise capacity, quality of life, and cardiovascular prognosis (Piepoli et al., Citation2016; Rauch et al., Citation2016). Exercise-based CR programs have been successful in improving exercise capacity and health-related quality of life, as well as in reducing the risk of cardiovascular mortality and hospital admissions (Anderson et al., Citation2016; Bierbauer et al., Citation2020; Shepherd & While, Citation2012). Nevertheless, some short- and long-term outcomes remain elusive, such as patients’ adherence to physical activity recommendations (ter Hoeve et al., Citation2015). Taking psychosocial factors, such as depression and anxiety, into account might be crucial in order to optimize CR outcomes (Chauvet-Gelinier & Bonin, Citation2017).
Depression and anxiety have indeed been shown to be detrimental for self-management behaviors in cardiac disease patients after surgery (Fredericks et al., Citation2012). In addition, baseline depression has been associated with the later development of a sedentary lifestyle (Roshanaei-Moghaddam et al., Citation2009), as well as with adverse cardiovascular outcomes (Freedland & Carney, Citation2013) and increased health care costs (Palacios et al., Citation2018). A possible explanation for these relationships might be that depression and anxiety represent important risk factors for CR outcomes during rehabilitation. Moreover, inpatient CR with its multidisciplinary approach offers an ideal opportunity for intervention (Pogosova et al., Citation2015). Nevertheless, the association that depression and anxiety may have with improvements in exercise capacity and in quality of life during inpatient CR has yet to be investigated. These improvements are crucial CR outcomes in order to provide patients with a strong basis to lead a healthy lifestyle (e.g., Piepoli et al., Citation2016). The main goal of the present study is to better understand the role of depression and anxiety as possible detrimental and independent factors for the improvements in exercise capacity and in health-related quality of life during inpatient CR.
Exercise capacity refers to the maximal physical exertion that a patient can endure (Goldstein, Citation1990). Improvements in exercise capacity during rehabilitation are crucial outcomes for CR success (Bierbauer et al., Citation2020) and have been linked to a favorable cardiac prognosis including a reduced risk of new cardiac events and mortality (Sabbag et al., Citation2018). Self-reported health-related quality of life, on the other hand, is a multi-dimensional concept that reflects the patients’ perception of their well-being and functional status relative to their health or disease (Shepherd & While, Citation2012). Health-related quality of life is frequently divided into three dimensions: emotional, physical, and social quality of life (Höfer et al., Citation2004a; Shepherd & While, Citation2012). Aside from the fact, that higher quality of life is a value in itself, it has also been linked to a reduced risk of cardiac events and mortality (Kato et al., Citation2011). Thus, improvements in quality of life during rehabilitation represent a crucial CR success indicator (Piepoli et al., Citation2016).
Depression and anxiety seem to share a common epidemiology with cardiovascular disease (Chauvet-Gelinier & Bonin, Citation2017; Wong et al., Citation2019). The main symptoms of depression include being in a depressed mood (e.g., feeling sad, hopeless, or empty), as well as losing interest or pleasure in activities (American Psychiatric Association – APA, Citation2013). Anxiety symptoms, on the other hand, include feeling restless, keyed up, or on edge, as well as finding it difficult to control the worrying (APA, Citation2013). A recent study found an estimated prevalence of moderate to extremely severe depression symptoms of 18% at the beginning of outpatient CR (Rao et al., Citation2020), which is four times larger than the estimated prevalence of depression in the general population (4.4%; World Health Organization - WHO, Citation2017). In the case of anxiety, the study found an estimated prevalence of anxiety symptoms of 28% among cardiac disease patients entering outpatient CR (Rao et al., Citation2020), which is also substantially higher than the 3.6% prevalence of anxiety found in the general population (WHO, Citation2017). Next to estimating the prevalence of depression and anxiety symptoms at the beginning of inpatient CR, the first goal of the present study is to also estimate the prevalence at the end of CR, and to provide information on the changes in these factors during inpatient CR.
The main goal of the present study focuses on the association of depression and anxiety with inpatient CR outcomes. Depression has been linked to reduced exercise capacity and quality of life, as well as to an increased cardiovascular risk and mortality (Cohen et al., Citation2015; McGrady et al., Citation2009; Milani & Lavie, Citation2007; Yohannes et al., Citation2010). Depression was also found to have a detrimental relationship with exercise capacity during outpatient CR (Glazer et al., Citation2002). Anxiety shows a more inconsistent picture in the extant literature. On the one hand, it has also been repeatedly associated with reduced exercise capacity and quality of life, as well as with an increased cardiovascular risk and mortality (Kroenke et al., Citation2013; McGrady et al., Citation2009; Pfaffenberger et al., Citation2010; Tully et al., Citation2016). On the other hand, a Danish 5-year prospective study found no association of anxiety with cardiac hospitalizations and all-cause mortality after controlling for depression (Versteeg et al., Citation2013). Yet another 5-year prospective study from Australia even found a positive effect of generalized anxiety disorder on cardiac outcomes after an acute coronary syndrome after controlling for depression (Parker et al., Citation2011). With the aim of investigating the independent relationship of depression and anxiety with the improvements in exercise capacity and health-related quality of life during inpatient CR, we hypothesized that both depression and anxiety at the beginning of CR would be negatively associated with both rehabilitation outcomes. Finally, we also hypothesized that reductions in depression and anxiety during rehabilitation would be related to higher improvements in exercise capacity and in health-related quality of life.
Methods
The study had a single-group pre–post-design with assessments at the beginning (T1) and at the end (T2) of inpatient CR. The data were collected following the guidelines of the Swiss National Association for Quality Development in Hospitals and Clinics (ANQ; https://www.anq.ch/en/) in order to monitor and ensure rehabilitation’s quality. The measurement of depression and anxiety was an addition to these guidelines. The use of the data for research purposes was approved by the Ethics Committee Zurich (KEK; approval number: REQ-2019-00291).
Sample
The initial sample comprised 3´747 cardiac patients taking part in inpatient CR at the Zürcher RehaZentrum Wald (Switzerland) between November 2011 and December 2018. Age under 18 (n = 2), a rehabilitation duration of less than 7 days (n = 195) or more than 8 weeks (n = 1), as well as missing values in all variables of interest were applied as criteria leading to the exclusion of 313 cases. The final sample, N = 3´434, had a mean age of 68.78 years (SD = 12.83, age range: 18–94 years) with a male proportion of 67.0%. The majority of the sample (57.2%) was married or in a registered partnership, whereas 42.0% were separated, single or widowed. The most frequent main diagnoses were: coronary artery disease (39.8%), aortic valve stenosis (13.1%), mitral insufficiency (5.6%) and dilated cardiomyopathy (3.1%). Included patients did not differ significantly from the excluded sample in terms of age, Welch’s t(365) = −0.49 p = .63, or gender distribution, χ²(1) = 0.77, p = .38. There was, however, a significant difference in marital status distribution, Fisher’s χ² = 6.43, p = .04 (50.2% of the excluded sample was married or in a registered partnership, and 48.6% separated, single or widowed). The most frequent main diagnoses were the same in both samples, that is, in the excluded sample: coronary artery disease (40.3%), aortic valve stenosis (10.9%), mitral insufficiency (5.4%) and dilated cardiomyopathy (2.2%).
Cardiac rehabilitation program
In Switzerland, inpatient CR has a recommended duration of 3 to 4 weeks and its components are determined nationwide by the Swiss Working Group for Cardiovascular Prevention, Rehabilitation and Sports Cardiology (SCPRS; https://www.scprs.ch/). In the present sample, CR had a mean duration of M = 19.3 days (SD = 4.8). The exercise therapy during CR consisted of endurance training (cycling or treadmill 3–6 times per week), gymnastics (5-6 times per week), outdoor walking (2-5 times per week), strength training (2-3 times per week), and, in some patients, inspiratory muscle training (3 times per week), progressive muscle relaxation (once a week), and autogenic training (once a week). The sessions were adapted to the patient’s exercise capacity. Moreover, patients received psychoeducation and counseling regarding the cardiac disease and cardiac risk factors, such as smoking cessation, diet, and stress. Furthermore, in accordance with the SCPRS guidelines each patient participated in at least one group therapy session led by a psychologist. Individual psychological counseling was offered upon interprofessional feedback about potential need for psychological support.
Measures
Depression and anxiety
The German version of the Hospital Anxiety and Depression Scale (HADS-D) was used to screen for depression and anxiety at T1 and T2 (Herrmann-Lingen et al., Citation2005). This self-report screening questionnaire has two subscales: one for depression and one for anxiety with 7 items each. Examples are “I feel as if I am slowed down” and “I feel tense or wound up”, accordingly. Items are rated on a 4-point Likert scale with item-specific labels (e.g., from 0 – not at all to 3 – most of the time). A score is built for each subscale as the sum of the ratings after having reversed the pertinent items. Thus, scores range from 0 to 21. Scores from 0 to 7 can be interpreted as normal, scores from 8 to 10 can be categorized as possibly clinically relevant, and scores above 10 as (highly likely) clinically relevant (Benzer et al., Citation2007). In the present sample the reliability of the anxiety subscale was high with Cronbach’s alphas of 0.82 and 0.85 at T1 and T2 accordingly. The reliability of the depression subscale was lower with Cronbach’s alphas of 0.66 and 0.68.
Quality of life
Patients reported their health-related quality of life at T1 and T2 using the German version of the MacNew Heart Disease Quality of Life Questionnaire (MacNew; Höfer et al., Citation2004a, Citation2004b), which contains 27 items and comprises three subscales corresponding to physical, emotional and social quality of life. Items are rated on a 7-point Likert-scale from 1 (e.g., never) to 7 (e.g., all the time). All scores are calculated as the mean of the corresponding items given that no more than 50% of the items are missing. All scores range from 1 to 7. A value of 0.5 has been identified as the minimal clinically important difference in MacNew scores (Dixon et al., Citation2002). However, there is disagreement in the literature regarding the factorial structure of MacNew (e.g., Friedrich et al., Citation2015; Gramm et al., Citation2012; Höfer et al., Citation2004a, Citation2005, Citation2008, Citation2012; Valenti et al., Citation1996). Therefore, it was important for the quality of the present analyses to find a factorial structure that fits both measurement points in order to ensure that any changes observed between T1 and T2 were actually changes in quality of life and not due to changes in the factorial structure.
Exercise capacity
Exercise capacity was measured at T1 and T2 using the 6-minute walk test (6MWT; Guyatt et al., Citation1985). During this test patients are instructed to walk as far as they can during six minutes. The total distance walked in meters is then used as an indicator of their exercise capacity. In a CR population, the 6MWT showed excellent test-retest reliability (ICC = .97), as well as a high correlation with the maximum metabolic equivalents from a symptom-limited graded exercise test (r=.69) supporting the validity of the test (Hamilton & Haennel, Citation2000). A systematic review found that an increase of 45 meters in the performance in the 6MWT seems to be clinically relevant for CR (Shoemaker et al., Citation2012).
Multimorbidity
Multimorbidity was measured at T1 using the German Version of the Cumulative Illness Rating Scale (CIRS-G; Hock & Nosper, Citation2005; Salvi et al., Citation2008). This measurement tool involves the evaluation by trained practitioners regarding the severity of impairment in 14 organ systems of the patient. Each organ system is evaluated using a 5-point scale from no impairment (0) to extremely impaired (4). The CIRS has shown good intra- and interrater reliability (ICC = .83 and .81, accordingly), as well as good predictive validity regarding hospital admissions and mortality (Salvi et al., Citation2008). For the purposes of this study, the psychiatric system was excluded from analysis, given that it includes impairment due to depression and anxiety. Using the 13 remaining organ systems, a comorbidity index indicating the number of systems with a rating higher than 1 was calculated (Salvi et al., Citation2008). Thus, scores could range between 0 and 13. A score of 3, for example, would indicate that three organ systems of the patient show a moderate or higher impairment. Therefore, higher scores indicate higher comorbidity.
Statistical analyses
First, given the disagreement in the literature regarding the factorial structure of MacNew (e.g., Friedrich et al., Citation2015; Gramm et al., Citation2012), it was crucial to find a factorial structure that fits the present data at T1 and T2. A confirmatory factor analysis was conducted to test the original structure (Model 1; Valenti et al., Citation1996), as well as seven different structures found in the literature using the German version of MacNew (Friedrich et al., Citation2015; Gramm et al., Citation2012; Höfer et al., Citation2004a, Citation2005, Citation2008, Citation2012). For these structures, items were chosen as indicators of one of the subscales (factors), only if the loading in the given study was at least .40 (Höfer et al., Citation2005). For the aims of the present study, it was important to not allow an overlap (i.e., items being part of more than one subscale) between the subscales, since they were outcomes investigated simultaneously in our analyses, given their expected intercorrelations. Therefore, we also only chose items as indicators of one of the subscales, if in the given study they showed the highest loading to that subscale. shows the items contained in each structure found in the literature (Models 1 to 8; Friedrich et al., Citation2015; Gramm et al., Citation2012; Höfer et al., Citation2005, Citation2004a, Citation2012, Citation2008; Valenti et al., Citation1996). Lastly, Model 9 was built by selecting an item for a subscale only, if that item was part of that subscale in the majority of structures found in the literature (that is, in at least 5 from the 8 structures or models found; see ). Note that, as frequently done in the literature, an item pertaining sex life was excluded from all analyses due to a very high percentage of missing values (73.1% at T1 and 81.2% at T2; Höfer et al., Citation2008).
Table 1. Overview of items and factors/subscales contained in each model tested with a confirmatory factor analysis.
A confirmatory factor analysis was conducted for each model taking both measurement points (T1 and T2) into account and allowing for variances and covariances between the items and between measurement points. Missing data was estimated using the full information maximum likelihood method. This method estimates a log-likelihood function for each individual based on the available variables, and has been found to perform well and produce unbiased parameters (Enders & Bandalos, Citation2001). shows the robust fit indices of the confirmatory factor analysis for each model tested. ANOVAs were applied to compare the fit of two models at a time. Model 2 and Model 9 showed the best fit, but there was no significant difference between both models, χ²(61) = 30.23, p = .99 (Gramm et al., Citation2012). Given that Model 9 contained the three subscales theorized from the start, we chose Model 9 for further analyses (Valenti et al., Citation1996). Moreover, to ensure temporal stability of the factors across both measurements, the factorial model was tested for weak invariance, meaning that the loadings of each item to a subscale were fixed across measurement points (Model 9.2). The model still showed a good fit (see ). Therefore, the factorial structure of Model 9 was chosen to build the score for each subscale. This structure included 11 items forming the emotional subscale, 5 items the physical subscale, and 3 items the social subscale. Cronbach’s alphas for the emotional, physical and social subscale were 0.93, 0.74 and 0.64 accordingly at T1, and 0.93, 0.73 and 0.70 at T2.
Table 2. Robust fit indices of the confirmatory factor analysis of each model.
In order to analyze improvements in depression, anxiety and rehabilitation outcomes, paired sample t-tests comparing scores at T1 and T2 were carried out. Effect sizes were calculated using Cohen’s d. A Cohen’s d of 0.2 can be interpreted as a small effect size, a d = 0.5 and d = 0.8 represent a medium and a large effect size (Cohen, Citation1992). Moreover, Pearson bivariate correlations were calculated for all variables relevant for the present study.
In order to investigate the relationship between depression and anxiety (at T1, as well as changes during CR) with improvements in rehabilitation outcomes, a path analysis was conducted. The independent variables were depression and anxiety scores at T1, as well as the changes in depression and anxiety (score at T2 minus score at T1) during rehabilitation. The dependent variables were the changes in exercise capacity and in emotional, physical and social quality of life. Control variables were the multimorbidity index, age, gender, T1 score of the outcome and days between T1 and T2 of each outcome. The model accounted for missing values by applying full information maximum likelihood to estimate values. The model also allowed for covariances between predictor variables, as well as between outcome variables.
Results
shows the mean scores of depression, anxiety, exercise capacity and emotional, physical and social quality of life at T1 and T2, as well as the results on their improvement during CR.
Table 3. Assessments at T1 and T2, and their change during rehabilitation.
shows the frequencies of the categorized depression and anxiety HADS scores. The percentages of patients categorized as (highly likely) clinically relevant, represent the estimated prevalence in the sample. Thus, at T1 there was a prevalence of depression of 9.3%. At T2 the prevalence had gone down to 5.0%. Indeed, as expected, depression scores showed a significant improvement from T1 to T2 with a small effect size (see ).
Figure 1. Frequencies of depression and anxiety categories at T1 and T2. Note. HADS depression and anxiety scores between 0 and 7 were categorized as normal, between 8 and 10 as possibly clinically relevant, and above 10 as (highly likely) clinically relevant. The latter group indicates the screening-based prevalence of depression and anxiety.
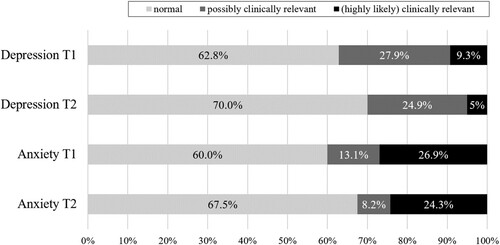
For anxiety there was a prevalence of 26.9% and 24.3% at T1 and T2, respectively (see ). Anxiety scores also showed a significant improvement during rehabilitation with a small effect size (see ).
Moreover, 5.2% (n=136) of patients at T1 and 3.0% (n=69) at T2, showed (highly likely) clinically relevant levels of both depression and anxiety. And 29.5% (n=770) at T1 and 25.9% (n=596) at T2 had at least possibly clinically relevant scores of both depression and anxiety.
Pearson bivariate correlations for all variables relevant for the present study can be found in . Whereas these correlations do not pertain the hypotheses and research questions directly, they emphasize the need to take predictors, control variables and outcomes simultaneously into account when analyzing the relevant relationships (due to intercorrelations).
Table 4. Pearson bivariate correlations.
The association of depression and anxiety with CR outcomes
The results of the path analysis investigating the associations between depression and anxiety with changes in exercise capacity and in emotional, physical and social health-related quality of life are shown in .
Table 5. Results from path analysis with the change in exercise capacity (6MWT) and change in emotional, physical and social quality of life (MacNew) as outcomes.
Depression
Depression at T1 was negatively and significantly associated with improvements in exercise capacity, as well as in emotional, physical and social quality of life during rehabilitation (see ). Based on the results, a one unit increase in the scale of depression at T1 would be associated with 3.4 meters (b = −3.40, see ) less improvement in the 6MWT. Given that the depression scale ranges from 0 to 21, this would mean that a patient with the highest depression score (21) at T1 would show 71.4 meters less improvement in the 6MWT than a patient with the lowest depression score (0), if all other variables in the model are held constant. Also, for each point higher in the scale of depression at T1 the emotional, physical and social quality of life would show 0.1, 0.07 and 0.07 (b parameters in ) less improvement, accordingly. This would mean that a patient with the highest depression score would show 2.1, 1.47 and 1.47 less improvement in emotional, physical and social quality of life accordingly, compared to a patient with the lowest depression score, given that all other variables in the model are held constant. Note that the highest possible improvement in the quality of life subscales is 6.
Moreover, changes in depression during CR were significantly and negatively related to changes in exercise capacity, and in emotional, physical and social quality of life. This means that decreases in depression during CR were related to greater improvements in exercise capacity, and in emotional, physical and social quality of life.
Anxiety
Contrary to our hypotheses, anxiety at T1 was positively and significantly associated with improvements in exercise capacity, as well as in emotional and physical quality of life (see ). There was no significant association of anxiety at T1 with improvements in social quality of life. Moreover, changes in anxiety during rehabilitation showed no significant relationship with changes in exercise capacity or in emotional, physical or social quality of life.
Discussion
The main goal of the present study was to investigate the independent relationship of depression and anxiety at the beginning of CR, as well as their change during CR, with the improvements in exercise capacity and emotional, physical and social quality of life. As expected, higher depression scores at the beginning of rehabilitation were associated with less improvement in exercise capacity and in emotional, physical and social quality of life during rehabilitation. Moreover, greater improvements in depression during rehabilitation were related to higher improvements in all outcomes. These findings highlight the importance and fruitfulness of screening for and treating depression in patients taking part in inpatient CR. A recent state-of-the-art review indeed highlights the necessity for all patients to be screened for depression and points to cognitive behavioral therapy, exercise, or pharmacotherapy as possible effective treatment options (Jha et al., Citation2019).
Contrary to our hypothesis, higher anxiety levels at the beginning of rehabilitation were related to greater improvements in exercise capacity and in emotional and physical quality of life. Note that all associations of depression and anxiety were analyzed while adjusting for the other. The necessity to investigate any associations of depression and anxiety independent from each other was highlighted by the high overlap and correlations between them found in our sample. Given previous findings relating anxiety to reduced physical activity and quality of life, as well as with increased cardiovascular risk and mortality, our findings regarding the positive associations of anxiety should be taken with caution (Kroenke et al., Citation2013; McGrady et al., Citation2009; Pfaffenberger et al., Citation2010; Tully et al., Citation2016). However, anxiety had also been previously linked to more positive cardiac outcomes (Parker et al., Citation2011). Additionally, high anxiety symptoms have also been associated to greater improvements in overall quality of life during outpatient CR (Lavie & Milani, Citation2004). Speculatively, a possible explanation for our findings might be that patients with higher levels of anxiety might be taking their illness more seriously and, therefore, adhering more closely to the rehabilitation program. Another possibility could be that patients high in anxiety might intuitively be using exercise as an emotion regulation strategy, since exercise has been found to be an effective treatment for anxiety, anxiety sensitivity and stress (Broman-Fulks & Storey, Citation2008; Herring et al., Citation2010; Milani & Lavie, Citation2009). Yet another possible explanation could be that anxious patients might be more restless or overactive. Supporting this notion are findings of comorbidity between anxiety and attention deficit hyperactivity disorder (Melegari et al., Citation2018). Future research should address the underlying mechanisms of the relationship of anxiety with rehabilitation outcomes.
Furthermore, the prevalence of depression and anxiety was estimated and changes in these factors during inpatient CR were investigated. Results showed a prevalence of depression of 9.3% at the beginning of rehabilitation. This prevalence, while high, was lower than the 18% found in a recent study at the beginning of outpatient CR (Rao et al., Citation2020). By the end of rehabilitation this prevalence had dropped to 5%, thus, approaching the prevalence of 4.4% in the general population (WHO, Citation2017). Indeed, as expected, results found a small effect for the reduction in depressive scores during rehabilitation, thus, replicating previous findings (Benzer et al., Citation2007; Kulcu et al., Citation2007; Yohannes et al., Citation2010). In the case of anxiety, there was a prevalence of 26.9% at the beginning and of 24.3% at the end of CR. These prevalences are close to the 28% prevalence of moderate to extremely severe anxiety symptoms previously found among patients at the beginning of outpatient CR (Rao et al., Citation2020), but are substantially higher than the 3.6% prevalence in the general population or the 16% found in cardiovascular disease patients in general (Tully et al., Citation2016; WHO, Citation2017). As expected, anxiety scores improved during CR with a small effect size in the present sample (Benzer et al., Citation2007; Kulcu et al., Citation2007; Yohannes et al., Citation2010). Importantly, the results regarding anxiety show that there is still room for improvement in the efforts to ameliorate anxiety symptoms in patients. It should be noted, however, that any differences found in the literature regarding prevalences may be due to different screening instruments or diagnostic methods used. Indeed, the present study used a screening instrument (HADS) to estimate the prevalence of depression and anxiety in our sample and an actual diagnosis would require further assessments.
Strengths and limitations
The present study has several strengths, for example, the large sample size and the use of validated instruments to measure the main constructs, as well as the longitudinal nature of the study in form of a pre- and a post-measurement during inpatient CR. Moreover, the associations of depression and anxiety with rehabilitation outcomes were investigated independently, thus, allowing insights of unique effects despite the comorbidity between the disorders. Our analyses also accounted for correlations between changes in exercise capacity and in the different types of quality of life by implementing a path analysis and allowing for covariance between the outcomes. Furthermore, the study addressed issues found in the literature pertaining the factorial structure of MacNew (e.g., Friedrich et al., Citation2015; Höfer et al., Citation2012), thus, ensuring that any changes investigated were changes in quality of life and not merely temporal changes in the factorial structure.
On the other hand, an important limitation of the present study is the lack of a control group, which means that we cannot be certain that any changes observed were actually due to the rehabilitation program. It is, for example, possible that the improvements observed were simply due to natural recovery over time. Nevertheless, previous research including randomized controlled trials have already found exercise-based cardiac rehabilitation to be effective in improving exercise capacity, quality of life, depression and anxiety (e.g., Smart et al., Citation2018; Yohannes et al., Citation2010). Yet another limitation of the present study is the correlational nature of the data preventing any causal inferences. For example, improvements in rehabilitation outcomes could help patients with depressive symptoms to ameliorate their mood. Alternatively, it is possible that improvements in depression and rehabilitation outcomes co-occur or that other unmeasured variables are involved. Given the nature of the problem at hand, experimental data that would help in clarifying causal relations are impossible in these settings. Thus, the present study provides important insights into the associations despite these limitations.
Conclusion
The present study identifies research gaps that should be addressed by future research such as the underlying mechanisms in the differential relationships of depression and anxiety with CR outcomes, as well as the long-term effects that improvements in depression and anxiety during CR could have on cardiac prognosis and mortality. Overall, the results of this study highlight the relevance of psychosocial factors such as depression and anxiety in CR, thus emphasizing the necessity to screen for and treat depression in order to optimize rehabilitation outcomes. Furthermore, results also point to the need for future research to focus on the relationship between anxiety and CR outcomes.
Data sharing statement
The data and material that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgements
Tania Bermudez and Walter Bierbauer were fellows of the International Max Planck Research School on the Life Course (LIFE, www.imprs-life.mpg.de; participating institutions: Max Planck Institute for Human Development, Freie Universität Berlin, Humboldt-Universität zu Berlin, University of Michigan, University of Virginia, University of Zurich).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®) (5th ed.). American Psychiatric Pub. https://doi.org/https://doi.org/10.1176/appi.books.9780890425596
- Anderson, L., Oldridge, N., Thompson, D. R., Zwisler, A.-D., Rees, K., Martin, N., & Taylor, R. S. (2016). Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. Journal of the American College of Cardiology, 67(1), 1–12. https://doi.org/https://doi.org/10.1016/j.jacc.2015.10.044
- Benzer, W., Platter, M., Oldridge, N. B., Schwann, H., Machreich, K., Kullich, W., Mayr, K., Philippi, A., Gassner, A., Dörler, J., & Höfer, S. (2007). Short-term patient-reported outcomes after different exercise-based cardiac rehabilitation programmes. European Journal of Cardiovascular Prevention and Rehabilitation, 14(3), 441–447. https://doi.org/https://doi.org/10.1097/HJR.0b013e32802bf7ae
- Bierbauer, W., Scholz, U., Bermudez, T., Debeer, D., Coch, M., Fleisch-Silvestri, R., Nacht, C.-A., Tschanz, H., Schmid, J.-P., & Hermann, M. (2020). Improvements in exercise capacity of older adults during cardiac rehabilitation. European Journal of Preventive Cardiology, 27(16), 1747–1755. https://doi.org/https://doi.org/10.1177/2047487320914736
- Broman-Fulks, J. J., & Storey, K. M. (2008). Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety, Stress, & Coping, 21(2), 117–128. https://doi.org/https://doi.org/10.1080/10615800701762675
- Chauvet-Gelinier, J.-C., & Bonin, B. (2017). Stress, anxiety and depression in heart disease patients: A major challenge for cardiac rehabilitation. Annals of Physical and Rehabilitation Medicine, 60(1), 6–12. https://doi.org/https://doi.org/10.1016/j.rehab.2016.09.002
- Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. https://doi.org/https://doi.org/10.1111/1467-8721.ep10768783
- Cohen, B. E., Edmondson, D., & Kronish, I. M. (2015). State of the art review: Depression, stress, anxiety, and cardiovascular disease. American Journal of Hypertension, 28(11), 1295–1302. https://doi.org/https://doi.org/10.1093/ajh/hpv047
- Dixon, T., Lim, L. Y., & Oldridge, N. B. (2002). The MacNew heart disease health-related quality of life instrument: Reference data for users. Quality of Life Research, 11(2), 173–183. https://doi.org/https://doi.org/10.1023/A:1015005109731
- Enders, C., & Bandalos, D. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. https://doi.org/https://doi.org/10.1207/S15328007SEM0803_5
- Fredericks, S., Lapum, J., & Lo, J. (2012). Anxiety, depression, and self-management: A systematic review. Clinical Nursing Research, 411–430. https://doi.org/https://doi.org/10.1177/1054773812436681
- Freedland, K. E., & Carney, R. M. (2013). Depression as a risk factor for adverse outcomes in coronary heart disease. BMC Medicine, 11(1), 1–9. https://doi.org/https://doi.org/10.1186/1741-7015-11-131
- Friedrich, O., Sipötz, J., Benzer, W., Kunschitz, E., & Höfer, S. (2015). The dimensional structure of the MacNew Health Related Quality of Life questionnaire: A mokken scale analysis. Journal of Psychosomatic Research, 79(1), 43–48. https://doi.org/https://doi.org/10.1016/j.jpsychores.2015.04.007
- Glazer, K. M., Emery, C. F., Frid, D. J., & Banyasz, R. E. (2002). Psychological predictors of adherence and outcomes among patients in cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation, 22(1), 40–46. https://doi.org/https://doi.org/10.1097/00008483-200201000-00006
- Goldstein, R. E. (1990). Exercise capacity. In H. K. Walker, W. D. Hall, & J. W. Hurst (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed.). Butterworth-Heinemann. https://doi.org/https://doi.org/10.7326/0003-4819-113-7-563_2
- Gramm, L., Farin, E., & Jaeckel, W. H. (2012). Psychometric properties of the German version of the MacNew heart disease health-related quality of life questionnaire. Health and Quality of Life Outcomes, 10(83), 1–9. https://doi.org/https://doi.org/10.1186/1477-7525-10-83
- Guyatt, G. H., Sullivan, M. J., Thompson, P. J., Fallen, E. L., Pugsley, S. O., Taylor, D. W., & Berman, L. B. (1985). The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Canadian Medical Association Journal, 132(8), 919–923.
- Hamilton, D. M., & Haennel, R. G. (2000). Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. Journal of Cardiopulmonary Rehabilitation, 20(3), 156–164. https://doi.org/https://doi.org/10.1097/00008483-200005000-00003
- Herring, M. P., O'Connor, P. J., & Dishman, R. K. (2010). The effect of exercise training on anxiety symptoms among patients: A systemativ review. Archives of Internal Medicine, 170(4), 321–331. https://doi.org/https://doi.org/10.1001/archinternmed.2009.530
- Herrmann-Lingen, C., Buss, U., & Snaith, R. P. (2005). Hospital anxiety and depression scale: HADS-D; deutsche Version; ein Fragebogen zur Erfassung von Angst und Depressivität in der somatischen Medizin; Testdokumentation und Handanweisung. Huber.
- Hock, G., & Nosper, N. (2005). Manual CIRS-G. Cumulative Illness Rating Scale. Skala zur kumulierten bewertung von erkrankungen. MDK Rheinland-Pfalz.
- Höfer, S., Anelli-Monti, M., Berger, T., Hintringer, F., Oldridge, N., & Benzer, W. (2005). Psychometric properties of an established heart disease specific health-related quality of life questionnaire for pacemaker patients. Quality of Life Research, 14(8), 1937–1942. https://doi.org/https://doi.org/10.1007/s11136-005-4347-9
- Höfer, S., Benzer, W., Brandt, D., Laimer, H., Schmid, P., Bernardo, A., & Oldridge, N. B. (2004a). MacNew Heart disease Lebensqualitätsfragebogen nach Herzinfarkt. Zeitschrift Für Klinische Psychologie Und Psychotherapie, 33(4), 270–280. https://doi.org/https://doi.org/10.1026/1616-3443.33.4.270
- Höfer, S., Lim, L., Guyatt, G., & Oldridge, N. (2004b). The MacNew heart disease health-related quality of life instrument: A summary. Health and Quality of Life Outcomes, 2(3), 1–8. https://doi.org/https://doi.org/10.1186/1477-7525-2-3
- Höfer, S., Saleem, A., Stone, J., Thomas, R., Tulloch, H., & Oldridge, N. (2012). The MacNew heart disease health-related quality of life questionnaire in patients with angina and patients with ischemic heart failure. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 15(1), 143–150. https://doi.org/https://doi.org/10.1016/j.jval.2011.07.003
- Höfer, S., Schmid, J.-P., Frick, M., Benzer, W., Laimer, H., Oldridge, N., & Saner, H. (2008). Psychometric properties of the MacNew heart disease health-related quality of life instrument in patients with heart failure. Journal of Evaluation in Clinical Practice, 14(4), 500–506. https://doi.org/https://doi.org/10.1111/j.1365-2753.2007.00905.x
- Jha, M. K., Qamar, A., Vaduganathan, M., Charney, D. S., & Murrough, J. W. (2019). Screening and management of depression in patients with cardiovascular disease: Jacc State-of-the-Art review. Journal of the American College of Cardiology, 73(14), 1827–1845. https://doi.org/https://doi.org/10.1016/j.jacc.2019.01.041
- Kato, N., Kinugawa, K., Seki, S., Shiga, T., Hatano, M., Yao, A., Hirata, Y., Kazuma, K., & Nagai, R. (2011). Quality of life as an independent predictor for cardiac events and death in patients with heart failure. Circulation Journal: Official Journal of the Japanese Circulation Society, 75(7), 1661–1669. https://doi.org/https://doi.org/10.1253/circj.cj-10-1308
- Khan, M. A., Hashim, M. J., Mustafa, H., Baniyas, M. Y., Al Suwaidi, S. K. B. M., AlKatheeri, R., Alblooshi, F. M. K., Almatrooshi, M. E. A. H., Alzaabi, M. E. H., Al Darmaki, R. S., & Lootah, S. N. A. H. (2020). Global epidemiology of Ischemic heart disease: Results from the Global Burden of disease study. Cureus, 12(7), e9349. https://doi.org/https://doi.org/10.7759/cureus.9349
- Knoll, N., Scholz, U., & Rieckmann, N. (2017). Einführung Gesundheitspsychologie (4th ed.). Ernst Reinhardt Verlag.
- Kroenke, K., Outcalt, S., Krebs, E., Bair, M. J., Wu, J., Chumbler, N., & Yu, Z. (2013). Association between anxiety, health-related quality of life and functional impairment in primary care patients with chronic pain. General Hospital Psychiatry, 35(4), 359–365. https://doi.org/https://doi.org/10.1016/j.genhosppsych.2013.03.020
- Kulcu, D. G., Kurtais, Y., Tur, B. S., Gülec, S., & Seckin, B. (2007). The effect of cardiac rehabilitation on quality of life, anxiety and depression in patients with congestive heart failure; a randomized controlled trial, short-term results. Europa Medicophysica, 43(4), 1–9.
- Lavie, C. J., & Milani, R. V. (2004). Prevalence of anxiety in coronary patients with improvement following cardiac rehabilitation and exercise training. The American Journal of Cardiology, 93(3), 336–339. https://doi.org/https://doi.org/10.1016/j.amjcard.2003.10.015
- McGrady, A., McGinnis, R., Badenhop, D., Bentle, M., & Rajput, M. (2009). Effects of depression and anxiety on adherence to cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation and Prevention, 29(6), 358–364. https://doi.org/https://doi.org/10.1097/HCR.0b013e3181be7a8f
- Melegari, M. G., Bruni, O., Sacco, R., Barni, D., Sette, S., & Donfrancesco, R. (2018). Comorbidity of attention deficit hyperactivity disorder and Generalized anxiety disorder in children and adolescents. Psychiatry Research, 270, 780–785. https://doi.org/https://doi.org/10.1016/j.psychres.2018.10.078
- Milani, R. V., & Lavie, C. J. (2007). Impact of cardiac rehabilitation on depression and its associated mortality. The American Journal of Medicine, 120(9), 799–806. https://doi.org/https://doi.org/10.1016/j.amjmed.2007.03.026
- Milani, R. V., & Lavie, C. J. (2009). Reducing psychosocial stress: A novel mechanism of improving survival from exercise training. The American Journal of Medicine, 122(10), 931–938. https://doi.org/https://doi.org/10.1016/j.amjmed.2009.03.028
- Palacios, J., Khondoker, M., Mann, A., Tylee, A., & Hotopf, M. (2018). Depression and anxiety symptom trajectories in coronary heart disease: Associations with measures of disability and impact on 3-year health care costs. Journal of Psychosomatic Research, 104, 1–8. https://doi.org/https://doi.org/10.1016/j.jpsychores.2017.10.015
- Parker, G., Hyett, M., Hadzi-Pavlovic, D., Brotchie, H., & Walsh, W. (2011). Gad is good? Generalized anxiety disorder predicts a superior five-year outcome following an acute coronary syndrome. Psychiatry Research, 188(3), 383–389. https://doi.org/https://doi.org/10.1016/j.psychres.2011.05.018
- Pfaffenberger, N., Doering, S., Puffinger, P., Höfer, S., Alber, H., Ruttmann, E., Günther, V., & Kopp, M. (2010). Gesundheitsbezogene Lebensqualität, Angst und Depression vor und nach einer aortokoronaren Bypass-Operation [Health-related quality of life, anxiety and depression before and after coronary artery bypass grafting]. Wiener Medizinische Wochenschrift, 160(1–2), 44–53. https://doi.org/https://doi.org/10.1007/s10354-009-0722-4
- Piepoli, M. F., Hoes, A. W., Agewall, S., Albus, C., Brotons, C., Catapano, A. L., Cooney, M.-T., Corra, U., Cosyns, B., Deaton, C., Graham, I., Hall, M. S., Hobbs, F. D. R., Lochen, M.-L., Lollgen, H., Marques-Vidal, P., Perk, J., Prescott, E., Redon, J., … Verschuren, W. M. M. (2016). 2016 European guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice. European Heart Journal, 37(29), 2315–2381. https://doi.org/https://doi.org/10.1093/eurheartj/ehw106
- Pogosova, N., Saner, H., Pedersen, S. S., Cupples, M. E., McGee, H., Höfer, S., Doyle, F., Schmid, J.-P., & Känel, R. v. (2015). Psychosocial aspects in cardiac rehabilitation: From theory to practice. A position paper from the cardiac rehabilitation section of the European association of Cardiovascular Prevention and rehabilitation of the European Society of cardiology. European Journal of Preventive Cardiology, 22(10), 1290–1306. https://doi.org/https://doi.org/10.1177/2047487314543075
- Rao, A., Zecchin, R., Newton, P. J., Phillips, J. L., DiGiacomo, M., Denniss, A. R., & Hickman, L. D. (2020). The prevalence and impact of depression and anxiety in cardiac rehabilitation: A longitudinal cohort study. European Journal of Preventive Cardiology, 478–489. https://doi.org/https://doi.org/10.1177/2047487319871716
- Rauch, B., Davos, C. H., Doherty, P., Saure, D., Metzendorf, M.-I., Salzwedel, A., Völler, H., Jensen, K., & Schmid, J.-P. (2016). The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and meta-analysis of randomized and non-randomized studies - The Cardiac Rehabilitation Outcome Study (CROS). European Journal of Preventive Cardiology, 23(18), 1914–1939. https://doi.org/https://doi.org/10.1177/2047487316671181
- Roshanaei-Moghaddam, B., Katon, W. J., & Russo, J. (2009). The longitudinal effects of depression on physical activity. General Hospital Psychiatry, 306–315. https://doi.org/https://doi.org/10.1016/j.genhosppsych.2009.04.002
- Sabbag, A., Mazin, I., Rott, D., Hay, I., Gang, N., Tzur, B., Goldkorn, R., Goldenberg, I., Klempfner, R., & Israel, A. (2018). The prognostic significance of improvement in exercise capacity in heart failure patients who participate in cardiac rehabilitation programme. European Journal of Preventive Cardiology, 25(4), 354–361. https://doi.org/https://doi.org/10.1177/2047487317750427
- Salvi, F., Miller, M. D., Grilli, A., Giorgi, R., Towers, A. L., Morichi, V., Spazzafumo, L., Mancinelli, L., Espinosa, E., Rappelli, A., & Dessì-Fulgheri, P. (2008). A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. Journal of the American Geriatrics Society, 56(10), 1926–1931. https://doi.org/https://doi.org/10.1111/j.1532-5415.2008.01935.x
- Shepherd, C. W., & While, A. E. (2012). Cardiac rehabilitation and quality of life: A systematic review. International Journal of Nursing Studies, 49(6), 755–771. https://doi.org/https://doi.org/10.1016/j.ijnurstu.2011.11.019
- Shoemaker, M. J., Curtis, A. B., Vangsnes, E., & Dickinson, M. G. (2012). Triangulating clinically miningful change in the six-minute walk test in individuals with chronic heart failure: A systematic review. Cardiopulmonary Physical Therapy Journal, 23(3), 5–15. https://doi.org/https://doi.org/10.1097/01823246-201223030-00002
- Smart, N. A., King, N., Lambert, J. D., Pearson, M. J., Campbell, J. L., Risom, S. S., & Taylor, R. S. (2018). Exercise-based cardiac rehabilitation improves exercise capacity and health-related quality of life in people with atrial fibrillation: A systematic review and meta-analysis of randomised and non-randomised trials. Open Heart, 5(2), e000880. https://doi.org/https://doi.org/10.1136/openhrt-2018-000880
- ter Hoeve, N., Huisstede, B. M. A., Stam, H. J., van Domburg, R. T., Sunamura, M., & van den Berg-Emons, R. J. G. (2015). Does cardiac rehabilitation after an acute cardiac syndrome lead to changes in physical activity habits? Systematic review. Physical Therapy, 95(2), 167–179. https://doi.org/https://doi.org/10.2522/ptj.20130509
- Tully, P. J., Harrison, N. J., Cheung, P., & Cosh, S. (2016). Anxiety and cardiovascular disease risk: A review. Current Cardiology Reports, 18(12), 120. https://doi.org/https://doi.org/10.1007/s11886-016-0800-3
- Valenti, L., Lim, L., Heller, R. F., & Knapp, J. (1996). An improved questionnaire for assessing quality of life after acute myocardial infarction. Quality of Life Research, 5(1), 151–161. https://doi.org/https://doi.org/10.1007/bf00435980
- Versteeg, H., Hoogwegt, M. T., Hansen, T. B., Pedersen, S. S., Zwisler, A.-D., & Thygesen, L. C. (2013). Depression, not anxiety, is independently associated with 5-year hospitalizations and mortality in patients with ischemic heart disease. Journal of Psychosomatic Research, 75(6), 518–525. https://doi.org/https://doi.org/10.1016/j.jpsychores.2013.10.005
- WHO. (2017). Depression and other common mental disorders: Global health estimates. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?sequence=1.
- Wong, B. C.-F., Chau, C. K.-L., Ao, F.-K., Mo, C.-H., Wong, S.-Y., Wong, Y.-H., & So, H.-C. (2019). Differential associations of depression-related phenotypes with cardiometabolic risks: Polygenic analyses and exploring shared genetic variants and pathways. Depression and Anxiety, 36(4), 330–344. https://doi.org/https://doi.org/10.1002/da.22861
- Yohannes, A. M., Doherty, P., Bundy, C., & Yalfani, A. (2010). The long-term benefits of cardiac rehabilitation on depression, anxiety, physical activity and quality of life. Journal of Clinical Nursing, 19(19–20), 2806–2813. https://doi.org/https://doi.org/10.1111/j.1365-2702.2010.03313.x
