ABSTRACT
This study investigated whether parental caregiving burden changed during adjunct multi-family therapy of adolescent anorexia nervosa and eating disorders not otherwise specified (EDNOS) and whether caregiver burden at baseline and changes in caregiver burden during treatment were associated with treatment outcome.
Twenty-four females, 13 to 16 years old, and their parents, participated in the study. Caregiver burden was measured with the Eating Disorders Symptom Impact Scale, by mothers (n = 23) and fathers (n = 22). Treatment outcome was measured by adolescent body mass index, level of global functioning and self-rated eating disorder symptoms by the Eating Disorders Examination Questionnaire 4.0.
All patient outcomes improved and overall caregiver burden decreased significantly during treatment. When broken down in aspects of caregiver burden the decrease in parental perceived isolation, was found to be associated with improvement of BMI and Children’s Global Assessment Scale. When analyzing fathers and mothers separately, we found that maternal feelings of guilt and paternal perceived burden of dysregulated behaviors at base-line were correlated to treatment outcome. Future studies are needed to clarify the role of caregiver burden as a potential mediator of treatment results.
Clinical Implications
Multi-Family Therapy shows preliminary effectiveness as an adjunct treatment for adolescent anorexia nervosa.
Parents’ parental burden decreased pre- to post Multi-family Therapy.
Fathers’ perceived dysregulated behaviors in the patient pre-treatment were associated with decrease of Body Mass Index during treatment.
Fathers are a resource in treatment and should be more specifically supported in the participation of Multi-Family Therapy.
Multi-Family Therapy as an adjunct therapy is related to a physical symptom reduction of the patient as well as to a decrease of caregiver burden for the parents, but no causality can be established in the present study.
Parental involvement in the treatment of anorexia nervosa (AN) is important, especially in younger patients with short duration of the disorder (Brockmeyer, Friederich, & Schmidt, Citation2017; Eisler, Simic, Blessit, & Dodge, Citation2016b; Lock & Le Grange, Citation2013). To care for someone diagnosed with AN often causes mental pain in the caregiver, which can impede the treatment and recovery of the patient. In order to more carefully study this process, the concept of psychological caregiver burden has been formulated (Anastasiadou, Medina-Pradas, Sepúlveda, & Treasure, Citation2014; Hibbs, Rhind, Leppanen, & Treasure, Citation2015; Svensson, Nilsson, Levi, & Suarez Carballeira, Citation2013). Caregiver burden has been defined as carergivers’ subjective and objective perceptions of the caregiving experience (Schene, Citation1990), and refers to the physical, emotional, and social problems associated with caregiving (Platt, Citation1985).
Common reactions of caregivers are worries about the nutritional status of the adolescent, guilt for letting the child down, developing difficulties with one’s own temper, all of which often lead to social isolation (Sepúlveda, Whitney, Hankins, & Treasure, Citation2008). The increase in caregiver burden often contributes to ineffective strategies in managing a patient, and a negative cycle might be set in motion. In this cycle, caregiver reactions and behaviors add to the stress of the adolescents (Goddard et al., Citation2013).
In accordance with the above described processes, a reduction in caregiver burden may lead to more effective treatment and faster patient recovery (Rienecke, Citation2017). Several interventions aim to help caregivers cope with the caregiver burden and make them more effective in supporting their children (Treasure & Nazar, Citation2016). Nine studies in a meta-analysis have shown outcome results from workshop interventions and self-help interventions (books or online) (Hibbs et al., Citation2015). The meta-analysis found a moderate reduction in caregiver burden post-treatment, and the burden continued to decrease at follow-up (from 2 months to 3 years later) moderately. Even though no causality has been established, the decrease in caregiver burden and increase in patient weight seem to occur simultaneously over an in-patient clinic treatment period (Magill et al., Citation2016; Matthews, Peterson, Peugh, & Mitan, Citation2019).
The association between specific aspects of parental burden and treatment outcome are not well understood. Slater with colleagues (Slater, Treasure, Schmidt, Gilchrist, & Wade, Citation2015) examined 12 participants with AN in an outpatient treatment trial and their nominated “significant other.” A positive correlation between a reduction in eating disorder symptoms in individuals with AN during treatment and a decrease in family distress three months after treatment was found. To our knowledge, no articles on caregiver burden (as a specific concept; Sepúlveda et al., Citation2008) and its associations with patient outcome in multi-family therapy (MFT) have been published. There is a gap in knowledge of how caregiver burden is associated with treatment outcome and how the perceived caregiver burden may differ between fathers and mothers and across cultures (Anastasiadou, Sepúlveda, Parks, Cuellar-Flores, & Graell, Citation2016; Gale, Cluett, & Laver-Bradbury, Citation2013).
A significant number of patients do not respond well to traditional single-family therapy, and therefore, MFT has been developed (Rienecke, Citation2017). MFT can be offered as a stand-alone intervention or as an adjunct therapy and is described more in detail in the method section. There remains a lack of robust evidence for the superior efficacy of MFT (with and without standard family-based treatments or treatment as usual [TAU]), compared to standard family-based treatments (Lock, Citation2018; Richards, Subar, Touyz, & Rhodes, Citation2018), but nevertheless, MFT has shown promising results, especially when it comes to weight gain in AN (e.g. Eisler et al., Citation2016a; Gelin, Fuso, Hendrick, Cook-Darzens, & Simon, Citation2015; Marzola et al., Citation2015). A study of adult patients and their caregivers in MFT found a decrease in burden for family members (Dimitropoulos, Farquhar, Freeman, Colton, & Olmsted, Citation2015), but the study did not address how these changes were related to patient treatment outcome.
The first aim of this one-armed clinical effectiveness study was to investigate whether adolescent self-reported eating disorders symptoms, BMI, and clinician-assessed global function, and parental caregiver burden changed with MFT as an adjunct therapy. The second aim was to study whether the parental burden pre-treatment and change in burden during MFT correlated with treatment outcome. We have the following hypotheses:
The primary outcomes (adolescents’ eating disorder symptoms, BMI, and global function) will improve after MFT.
The parental caregiver burden will decrease after MFT.
The parental caregiver burden pre-treatment will correlate with treatment outcome.
The parental caregiver burden pre- to post-intervention will correlate positively with improvement in primary outcomes.
As an exploratory aim we also investigated whether the caregiver burden of mothers and fathers differed and how this related to treatment outcome.
Method
Study setting
The study was conducted at an outpatient child and adolescent psychiatric (CAP) clinic in Sweden. The project was approved by the Regional Ethical Review Board at Umeå University and followed the Ethical Guidelines of APA and the Declaration of Helsinki.
Procedure
At the same CAP clinic, newly referred patients and patients in on-going AN treatment were clinically assessed for MFT as an adjunct therapy. These families were invited to an information-session and offered participation in MFT. Approximately half of the families accepted the invitation to participate in MFT, and those families were also invited to participate in the present study, other families declined for unknown reasons. Written informed consent was obtained. Base-line data was collected prior to or simultaneously with the first session, and data was also gathered directly after the last session.
Participants
Participants were recruited into five consecutive MFT-treatment groups. Twenty-eight families, including patients, mothers, fathers, and siblings, entered MFT. Two of these families did not give their consent to participate in the study, and two other families were excluded because of incomplete datasets. Twenty-four patients had at least one parent who filled out the parental burden questionnaire (EDSIS) pre- and post-treatment (mothers n = 23, fathers n = 22). Siblings were not included in the present study.
Inclusion criteria for the patients were: (1) primary DSM-IV diagnosis of Anorexia Nervosa (AN), or Eating Disorder Not Otherwise Specified (EDNOS); (2) age 12–17 years; (3) fluency in Swedish (the intervention was conducted in Swedish). Exclusion criteria for the patients were: (1) active substance abuse; (2) severe trauma with, e.g. persistent dissociative symptoms and severe interpersonal difficulties; (3) acute suicidality (suicidal ideation was allowed); (4) psychosis; (5) or any other serious psychiatric comorbidity that hindered group participation, e.g. severe depression. Parents were eligible for study participation if they were capable of functioning in a group setting.
The intervention
MFT has been developed as an adjunct treatment to individual or family treatment (Eisler, Citation2005; Gelin, Cook-Darzens, & Hendrick, Citation2018; Simic & Eisler, Citation2015). The theoretical framework for MFT stems from cognitive behavioral therapy with additional elements of structural and constructivist system therapy. MFT is manualized and structured around four objectives: eating management and weight gain; clear boundaries within the family regarding roles and tasks; communication; and individual development (Eisler et al., Citation2016b).
In our study, MFT was offered to patients and their parents according to Wallin’s manual (Citation2007) and with the above-mentioned four objectives. Patients were seen with their families over a period of one year. First, a four-day intensive group treatment was offered, followed by six and a half days of treatment (approximately three each semester). The treatment had the following phases: (1) The first phase was symptom-oriented with the aim of preventing starvation. The parents were encouraged to take the lead in managing their children’s eating habits with a shift in the approach from parental control to parental care.; (2) The second phase was relationally-oriented. Family-based relational patterns were processed through exercises and group-discussions. Themes, such as transparency, identification with family roles, renegotiations skills, and conflict resolution, were addressed. Improved eating habits were established and maintained during this phase.; (3) The last phase was future-oriented. A new family constellation was formed in which the adolescent gained autonomy and age-appropriate interdependence. Relapse prevention was also addressed.
The group was led by two senior MFT psychotherapists who were assisted by two therapists. Staff from the CAP eating disorder team also participated. The therapists received a total of eight hours of supervision by a licensed MFT supervisor during the treatment period. The participants also received treatment as usual (TAU; see below) at the CAP clinic throughout the duration of the MFT.
Treatment as usual
MFT was added to TAU, which consisted of single-family therapy (n = 24, range 4 to 41 sessions, M = 19.43, SD = 8.84), individual psychotherapy (n = 13, range 3 to 25 sessions, M = 6.65, SD = 7.96), or inpatient care (n = 7, range from 3 to 25 days). The amount of concurrent treatment did not significantly correlate with patient outcomes. We have no detailed information available about the possible treatment offered prior to the participation of MFT, only that most families had a treatment period of TAU before they entered the MFT-study.
Measures
Diagnostic procedure
DSM-IV diagnoses of anorexia nervosa (AN) or Eating Disorder Not Otherwise Specified (EDNOS) (APA, Citation1994) were established based on the Structured Eating Disorder Interview (SEDI; De Man Lapidoth & Birgegård, Citation2009), which is a semi-structured diagnostic interview for patients with eating disorders.
Clinical assessment
Weight, height, heart rate, and systolic and diastolic blood pressure were measured by staff at the clinic. Body Mass Index (BMI; Kuczmarski et al., Citation2000) was calculated as weight in kilograms divided by height in meters squared. Expected Body Weight (%EBW; Le Grange et al., Citation2012) was calculated by patient BMI divided by the 50th percentile BMI for normal sample age and height x 100.
The Children’s Global Assessment Scale (CGAS; Shaffer et al., Citation1983) is a clinician rating scale used to assess global functioning in children and adolescents. The scale ranges from 0–100, and higher scores indicate better functioning.
Patient self-reporting
The Eating Disorders Examination Questionnaire, version 4.0 (EDE-Q; Fairburn & Beglin, Citation1994; Forsén Mantilla & Birgegård, Citation2016) measures eating-related pathology, behaviors, and attitudes. The fourth version was developed to suit adolescent populations (Carter, Stewart, & Fairburn, Citation2001). EDE-Q is a 36-item self-report instrument. Each item is rated on a 7-point Likert scale 0 (no day) to 6 (every day). The EDE-Q has four subscales: restraint, eating concern, shape concern, and weight concern. In the present study, we used the global score, which is the mean value of the four subscales. EDE-Q has shown satisfactory psychometric properties, including acceptable to high internal consistency and test-retest reliability (Berg, Peterson, Frazier, & Crow, Citation2012). Internal consistency could not be calculated in the present study due to lack of item-level data.
Parent self-reporting
The Eating Disorders Symptom Impact Scale (EDSIS; Sepúlveda et al., Citation2008) measures the subjective and objective burden of caregivers of patients with eating disorders. The 24-item self-report measure has four subscales: 1. managing nutrition; 2. guilt; 3. dealing with dysregulated behaviors; and 4. social isolation. Scores are rated on a 5-point Likert scale ranging from 1 (never) to 4 (almost always), and higher scores indicate both higher caregiving burden and more negative appraisal of caregiving. Convergent validity has been shown satisfactory, and it is sensitive to a change in symptoms (Sepúlveda et al., Citation2008). The scale has acceptable to high internal consistency (Cronbach’s alpha = 0.84 to 0.91) across the four subscales (Hibbs et al., Citation2014; Sepúlveda et al., Citation2008). In the present study, internal consistency (Cronbach’s alpha) at base-line was 0.62 (mothers) and 0.58 (fathers) for nutrition, 0.88 (mothers) and 0.79 (fathers) for guilt, 0.71 (mothers) and 0.81 (fathers) for dealing with dysregulated behaviors, and 0.83 (mothers) and 0.88 (fathers) for social isolation.
Statistical analysis
Overall, the as-treated analysis method was used in the present study. Intercorrelations between EDSIS and other variables pre-treatment were analyzed with Pearson correlations. Since intercorrelations were found (under recommended values; Tabachnick & Fidell, Citation2013) mixed-design repeated multivariate analysis of variance (MANOVA) was conducted to calculate change scores and to detect interaction effects. Mother and father status was used as the between-subject factor, and EDSIS-scores (four variables) were used as dependent variables in each model. ANOVAS (F-tests) were used to calculate univariate change scores. Paired T-tests were used to calculate pre- to post-changes for patient and parent descriptives. Pretest scores and change scores for parental caregiver burden and difference scores for children’s symptoms and function were calculated with Pearson Correlations.
Following the guidelines of Tabachnick and Fidell (Citation2013), the data was found to meet the assumptions of multivariate analyses in relation to normal distribution, linearity, univariate outliers, multivariate outliers, homogeneity of variance-covariance matrices, and multicollinearity, and singularity. All analyses were conducted using IBM SPSS Statistics for Windows, Version 24.0.
Effect sizes (ES) were expressed in eta squared (i.e. η2) and Cohen’s d. ES η2 of 0.01, 0.06, and 0.14 indicate small, medium, and large effect, respectively. For Cohen’s d, 0.2–0.49 is considered small, 0.05–0.79 is considered medium, and ≥ 0.8 is considered a large effect size (Cohen, Citation1988).
Results
Description of the sample
All patient participants were females, 13 to 16 years old (M = 13.91, SD = 1.12) living with their parents. Nine patients fulfilled criteria for a DSM-IV diagnosis of anorexia nervosa (AN) and 15 of Eating Disorder Not Otherwise Specified (EDNOS). The duration of having the diagnosis prior to entering the study ranged from one to four years (M = 1.82, SD = 1.25). Six patients were hospitalized prior to MFT with a mean duration of 3.52 days (SD = 7.25). Four of the patients had psychiatric comorbidity at baseline, including major depressive disorder, obsessive compulsive disorder, and anxiety disorders, such as social anxiety disorder. All DSM diagnostics were performed by child and adolescent psychiatrists and supported by an internet-based quality assurance system (Birgegård, Björck, & Clinton, Citation2010). 100% of the sample was Caucasian. See more detailed description of the sample in .
Table 1. Means, standard deviations and paired t-tests for adolescents’ outcome data
Twenty-three mothers and 22 fathers participated in the MFT. The maternal age varied between 31 and 52 years (M = 43.73, SD = 5.36), and paternal age varied from 40 to 56 years (M = 46.62, SD = 4.35). 100% of the fathers and 60% of the mothers worked full time. Thirty-five percent of the mothers worked part-time, and 5% of the mothers were unemployed. A majority of the parents (78.50%) had a university degree.
Days of participation in the MFT by any of the parents ranged from 8 to 10 days, (M = 9.75, SD =0.53). Mother’s participation ranged from 8 to 10 days, (M = 9.48, SD = 0.79), and father’s participation ranged from 7 to 10 days (M = 9.61, SD = 0.83).
Baseline comparison between study sample and samples from the normal population
A sample of Swedish 14-year-old females, representative of the normal population, had a mean weight of 53.08 kg (SD = 8.78) (Albertsson Wikland, Luo, Niklasson, & Karlberg, Citation2002). In another Swedish reference study (Karlberg, Luo, & Albertsson-Wikland, Citation2001), the mean BMI was 19.09. Normative Swedish EDE-Q data from a similar age-group showed a total score mean of 1.41 (SD = 1.36) (Forsén Mantilla & Birgegård, Citation2016). The present study sample had significantly lower weight (t(23) = 2.99, p = .007), BMI (t(23) = 2.90, p = .008), and a higher total score of EDE-Q (t(23) = 49.86, p < .001) compared to these normative samples, which validates the clinical status of our sample.
Patient changes in primary and secondary outcomes pre- to post-MFT
The patients improved significantly pre- to post-MFT in physiological parameters, such as weight, height, heart rate, diastolic (but not systolic) blood pressure, BMI, and in global functioning (CGAS) and eating disorder symptoms (EDE-Q), see , . At the end of the MFT intervention, two of the patients fulfilled the DSM-IV-criteria for AN, nine fulfilled criteria for EDNOS, and 13 no longer fulfilled criteria for any eating disorders according to DSM-IV. Pearson correlations showed that the duration of diagnosis prior to entering the study did not affect the change in weight scores (r = .14, p = .555), BMI (r = .12, p = .603), or the total EDE-Q score (r = .22, p < .387).
Pre-treatment differences between mothers and fathers
Mothers and fathers did not differ significantly on the Eating Disorders Symptom Impact Scale (EDSIS) scores at base-line, except for the subscale guilt, which was scored higher by mothers than fathers (t = −2.46, p = .02. d = 0.72).
Parental caregiver burden pre- to post-MFT
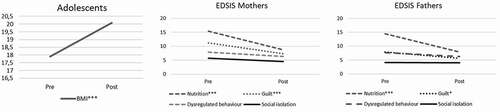
Intercorrelations between study variables in EDSIS were in the expected direction and under recommended values (Tabachnick & Fidell, Citation2013), see . A repeated MANOVA was conducted to investigate within-group differences over time. Four dependent variables were investigated: nutrition, guilt, dysregulated behavior, and social isolation. Time in treatment was chosen as the independent variable, and a for the parent status an interaction effect was tested. A significant change over time was found (Wilks’ Lambda Λ = 0.37, F(4,40) = 16.81, p < .001, eta squared = 0.63), and no interaction effect (Wilks’ Lambda Λ = .96, F(4,40) = .44, p = .78). The interaction effect means that pre- to post-MFT differences in caregiver burden did not depend on parent status. Separate univariate ANOVAs showed that nutrition (F(1,43) = 57.89, p < .001, eta squared = .57), guilt (F(1,43) = 20.15, p < .001, eta squared = .32), and dysregulated behavior (F(1,43) = 5.02, p = .03, eta squared = .10) changed significantly over time, but social isolation (F(1,43) = .76, p = .39, eta squared = .02) did not. See for descriptives and for figures on adolescent BMI and parental caregiver burden (EDSIS) change over time.
Table 2. Summary of intercorrelations for scores on parents’ burden for all parents pre treatment
Table 3. Means and standard deviations, and paired T-tests for mothers’ and fathers’ caregiving burden (eating disorders symptom impact scale)
The relation between maternal and paternal caregiver burden at baseline and treatment outcome
A negative association was found between maternal guilt rated on EDSIS pre-treatment and treatment outcome (EDE-Q). For fathers, on the other hand, the rated burden of perceived dysregulated behaviors on EDSIS pre-treatment negatively correlated with treatment outcome as measured with BMI. A positive correlation was found between paternal base-line scores on perceived isolation on EDSIS and treatment outcome in terms of BMI, see .
Table 4. Summary of pearson correlations between pretest scores on the parents’ caregiving burden and difference scores on children’s symptoms and function
The relation between change in mother- and father-perceived caregiver burden and treatment outcome
The change in caregiver burden (EDSIS) in terms of social isolation showed a significant negative correlation with the primary treatment outcomes, BMI, and global function (CGAS).
For fathers, the change in self-rated guilt and worries about the child’s nutritional status pre- to post-MFT was negatively associated with changes in BMI and CGAS. The change scores of fathers for perceived dysregulated behaviors were negatively associated with changes in CGAS, see .
Table 5. Summary of pearson correlations between difference scores on the parents’ caregiving burden and difference scores on children’s symptoms and function
Discussion
Clinical studies of adolescent anorexia nervosa (AN) and their caregivers are rare, and the data is difficult to obtain due to the long treatment periods and the complex nature of the disorder. The present study attempted to bring more in-depth knowledge of the role of parental caregiver burden with regard to outcome of treatment. Even though no causality can be claimed due to purely correlational data and no proof of efficacy can be stated due to the lack of control conditions, this clinical study provides new insights into the different aspects of caregiver burden and how it is perceived by mothers and fathers. The study also implicates new research questions for future studies.
According to our first hypothesis, adolescent girls with AN or EDNOS significantly improved in self-rated eating disorder symptoms, BMI, and global function pre- to post-adjunct MFT, which is in line with previous findings (Richards et al., Citation2018).
In line with our second hypothesis, both mothers and fathers reported a significant reduction in caregiver burden pre- to post-MFT, especially for nutrition-related parental caregiver burden, such as effort of noticing, arguing about, and checking food intake. Parents also reported that their feelings of guilt decreased (i.e. the experience that they were responsible for the illness and that they had let their child down). No significant difference between the mother and father groups were found. Dimitropoulos et al. (Citation2015) have also found the highest impact on the variables nutrition and guilt (EDSIS) at the end of family intervention. Sepúlveda et al. (Citation2012) have found that the impact of nutrition-related burden, as measured with EDSIS, was the major predictor of anxiety and depression in caregivers, and feelings of guilt and social isolation predicted increased anxiety in the caregivers.
Pre-treatment parental caregiver burden in relation to patient outcome
Our third hypothesis that parental caregiver burden pre-treatment would be associated with treatment outcome was also supported. Interestingly, a high level of maternal guilt before treatment was associated with positive treatment outcome in eating disorder symptoms. A study by Stillar et al. (Citation2016) demonstrates a link between fear, self-blame, and low self-efficacy in caregivers, and those authors concluded that these emotional experiences could lead to inflexibility, reactiveness, and difficulties in accessing their instincts and acquired skills. Our previous study (present author reference) showed that parents often feel responsible for their child’s eating disorder, and many parents feel insecure about their competence as parents. However, meeting other parents in the same situation gave them a sense of relief from guilt and shame and parents expressed statements like: “The affirmation that it was not my fault, we had not done anything evil. Nobody knows why it (AN) turns out this way. It just happens.”
Paternal reports of the burden of their daughter’s dysregulated behaviors pre-treatment (manipulative, aggressive, and lying) correlated negatively with an improvement of BMI, implying that a more trustful relationship between the daughter and the father, were associated with better treatment outcome in length and weight. This could be compared with the Wallis et al. (Citation2017) study of family functioning that found that higher levels of father-reported behavioral control (e.g. rules and expected behaviors) at the commencement of treatment were positively related to remission status over time.
In addition, there was an association between a higher sense of isolation among fathers before treatment and greater improvement in BMI in the patients. One explanation could be that fathers, who felt more isolated at base-line, were better able to take advantage of the treatment and were more supportive of their daughters.
Change in parental caregiver burden in relation to patient outcomes
In line with our fourth hypothesis, we found correlations between parental caregiver burden pre- to post-intervention and improvement in the primary outcomes. Major associations were found between a decrease in parental burden of social isolation and adolescent recovery in BMI and daily function during treatment. For both mothers and fathers, the decrease in social isolation was strongly associated with physical treatment outcome. Singh, Accurso, Hail, Goldschmidt, and Le Grange (Citation2018) have found that mothers experienced the physical recovery of their children most important.
We found a concurrent change in parental caregiver burden, specifically social isolation and the physical recovery of the patients Slater et al. (Citation2015) have found that a reduction in eating pathology in 12 women preceded the reduction in psychological distress of caregivers, and they found reduced psychological distress in the care-givers three months after the end of treatment. The Slater study differed in many ways from our study, which makes comparison difficult. Most importantly, their patients were adults (mean age 27), and the intervention was delivered in individual sessions and was less intense than the group-based MFT.
One aspect that needs to be taken into consideration is the age of our sample since adolescence is a developmentally sensitive period regarding identity and autonomy. The closeness between adolescents and their parents in more intensive treatment may have influenced the simultaneous and stronger correlations in our study.
Furthermore, BMI was moderately low in our sample, and possibly, carergivers could have assimilated more easily in the treatment group because they did not have to face life threatening AN. It is, however, not clear which effect comes first, i.e. improvements in the physical symptoms of the AN patients, or the decrease in caregiver burden. Future longitudinal and well-powered studies could sort this out.
In our study, mothers and fathers presented different correlations (see ). For fathers, their feelings of guilt, worries about their daughters’ nutritional status and dysregulated behavior were associated with a change in patient BMI and global function. This possibly indicates that, for fathers, the physical health of daughters is strongly related to their burden.
Method discussion
Several limitations should be noted in this study. First, the modest sample size limited statistical power and generalizability, and our preliminary findings should be replicated in more well-powered future studies. Also, no correction for familywise error rate was done in this preliminary explorative study, risking Type I Error. Second, in our naturalistic design, we had no control group, and therefore, we cannot dismantle the effects of treatment-as-usual from the effects of MFT. Third, the duration of illness and the length of treatment before MFT varied in our sample. and most of the patients recruited to our study had already been subjected to other eating disorder-focused treatment before they entered MFT. Some patients may possibly have already begun to gain weight before entering MFT since our patients had a higher BMI at baseline than in several other studies (Richards et al., Citation2018). Nevertheless, in comparison with normative data, our study sample was clearly a clinical sample.
The strengths of the present study are the use of manualized treatment, assessment with well-validated measures, and statistical analyses that accounted for multicollinearity and different sample sizes. Furthermore, the data consisted of mainly complete family units, and there are few studies with the participation of an equal amount of mothers and fathers (Hibbs et al., Citation2015), and studies that specifically address paternal self-report are rare (Gale et al., Citation2013).
Conclusions
Despite the different aspects of parental caregiver burden and how it may impede treatment results and clinical work, it is important to emphasize that the patients, in general, benefited from having their parents and significant others involved in the treatment.
The results can further aid the development of interventions aimed at supporting caregivers. In future studies, it is important to carefully monitor how each parent/caregiver responds to and copes with treatment (Wallis et al., Citation2018).
Furthermore, a need to specifically improve support for fathers during treatment has been identified, and the question of how to best encourage and support them to participate actively in the treatment needs to be addressed. We suggest that parents sometimes should be divided into groups of the same gender because especially fathers had had the need to share their experience with someone equal (author). It is also important to support parental collaboration and shared responsibility for their child to unburden the one who is most responsible (author). Shared responsibility can be reached, through more information about the disease.
Finally, improved social interactions between families, as offered by MFT, were strongly associated with physical patient outcomes and may be a uniquely important component of MFT to address guilt and stigma and to build communities of support. Eating is not only eating but also an important social activity that can be practiced within the framework of MFT.
Acknowledgments
This study was supported by clinical research funding (ALF) from Västerbotten county council. The authors want to thank all the families and therapist who participated in the project. Many thanks to Ana Sepúlveda for valuable comments on the Swedish version of EDSIS.
Additional information
Funding
References
- Albertsson Wikland, K., Luo, Z. C., Niklasson, A., & Karlberg, J. (2002). Swedish population-based longitudinal reference values from birth to 18 years of age for height, weight and head circumference. Acta Paediarica, 91, 739–754. doi:https://doi.org/10.1111/j.1651-2227.2002.tb03322.x
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, DSM-IV (4th ed.). Washington, DC: Author.
- Anastasiadou, D., Medina-Pradas, C., Sepúlveda, A. R., & Treasure, J. (2014). A systematic review of family caregiving in eating disorders. Eating Behaviors, 15, 464–477. doi:https://doi.org/10.1016/j.eatbeh.2014.06.001
- Anastasiadou, D., Sepúlveda, A. R., Parks, M., Cuellar-Flores, I., & Graell, M. (2016). The relationship between dysfunctional family patterns and symptom severity among adolescent patients with eating disorders: A gender-specific approach. Women & Health, 56, 695–712. doi:https://doi.org/10.1080/03630242.2015.1118728
- Berg, K., Peterson, C., Frazier, P., & Crow, S. (2012). Psychometric evaluation of the eating disorder examination and eating disorder examination‐questionnaire: A systematic review of the literature. International Journal of Eating Disorders, 45(3), 428–438. doi:https://doi.org/10.1002/eat.20931
- Birgegård, A., Björck, C., & Clinton, D. (2010). Quality assurance of specialised treatment of eating disorders using large-scale internet-based collection systems: Mathods, results and lessons learned from designing the stepwise database. European Eating Disorders Review, 18, 251–259. doi:https://doi.org/10.1002/erv.1003
- Brockmeyer, T., Friederich, H., & Schmidt, U. (2017). Advances in the treatment of anorexia nervosa: A review of established and emerging interventions. Psychological Medicine, 48(8), 1228–1256. doi:https://doi.org/10.1017/S0033291717002604
- Carter, J. C., Stewart, D. A., & Fairburn, C. G. (2001). Eating disorder examination questionnaire: Norms for young adolescent girls. Behaviour Research and Therapy, 39(5), 625–632. doi:https://doi.org/10.1016/s0005-7967(00)00033-4
- Cohen, J. (1988). Statistical power analysis for behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum associates.
- De Man Lapidoth, J., & Birgegård, A. (2009). Validation of the Structured Eating Disorder Interview (SEDI) against the Eating Disorder Examination (EDE), Swedish. Stockholm, Sweden: Socialstyrelsen Dnr 21–4549
- Dimitropoulos, G., Farquhar, J. C., Freeman, V. E., Colton, P. A., & Olmsted, M. P. (2015). Pilot study comparing multi-family therapy to single family therapy for adults with anorexia nervosa in an intensive eating disorder program. European Eating Disorders Review, 23, 294–303. doi:https://doi.org/10.1002/erv.2359
- Eisler, I. (2005). The empirical and theoretical base of family therapy and multiple family day therapy for adolescent anorexia nervosa. Journal of Family Therapy, 27, 104–131. doi:https://doi.org/10.1111/joft.2005.27.issue-2
- Eisler, I., Simic, M., & Blessit, E., & Dodge, L.; team . (2016b). Maudsley service manual for child and adolescent eating disorders. London: Child and Adolescent Eating Disorders Service, London: England, South London and Maudsley NHS Foundation Trust
- Eisler, I., Simic, M., Hodsoll., J., Asen, E., Berelowitz, M., Connan, F., … Landau, S. (2016a). A pragmatic randomised multi-centre trial of multi-family and single-family therapy for adolescent anorexia nervosa. BMC Psychiatry, 16(1), 422–436. doi:https://doi.org/10.1186/s12888-016-1129-6
- Fairburn, C. G., & Beglin, S. J. (1994). Assessment of eating disorders: Interview or self‐report questionnaire? International Journal of Eating Disorders, 16, 363–370.
- Forsén Mantilla, E., & Birgegård, A. (2016). Eating disorder examination questionnaire: Norms and clinical reference data from adolescent boys and girls in Sweden. Psychiatry Research, 239, 156–162. doi:https://doi.org/10.1016/j.psychres.2016.03.022
- Gale, C. J., Cluett, E. R., & Laver-Bradbury, C. (2013). A review of the father-child relationship in the development and maintenance of adolescent anorexia and bulimia nervosa. Issues in Comprehensive Pediatric Nursing, 36(1–2), 48–69. doi:https://doi.org/10.3109/01460862.2013.779764
- Gelin, Z., Cook-Darzens, S., & Hendrick, S. (2018). The evidence-base for multiple family therapy in psychiatric disorders: A review (part 1). Journal of Family Therapy, 40, 302–325. doi:https://doi.org/10.1111/joft.2018.40.issue-3
- Gelin, Z., Fuso, S., Hendrick, S., Cook-Darzens, S., & Simon, Y. (2015). The effects of a multiple family therapy on adolescents with eating disorders: An outcome study. Family Process, 54(1), 160–172. doi:https://doi.org/10.1111/famp.12103
- Goddard, E., Salerno, L., Hibbs, R., Raenker, S., Naumann, U., Arcelus, J., … Treasure, J. (2013). Empirical examination of the interpersonal maintenance model of anorexia nervosa. International Journal of Eating Disorders, 46, 867–874. doi:https://doi.org/10.1002/eat.22172
- Hibbs, R., Rhind, C., Leppanen, J., & Treasure, J. (2015). Interventions for caregivers of someone with an eating disorder: A meta-analysis. International Journal of Eating Disorders, 48, 349–361. doi:https://doi.org/10.1002/eat.22298
- Hibbs, R., Rhind, C., Sallis, H., Goddard, E., Raenker, S., Ayton, A., & Treasure, J. (2014). Confirmatory factor analysis for two questionnaires of caregiving in eating disorders. Health Psychology and Behavioral Medicine: an Open Access Journal, 2, 322–334. doi:https://doi.org/10.1080/21642850.2014.894889
- Karlberg, J., Luo, Z. C., & Albertsson-Wikland, K. (2001). Body mass index reference values (mean and SD) for Swedish children. Acta Paediatrica, 90, 1427–1434. doi:https://doi.org/10.1080/08035250152708851
- Kuczmarski, R. J., Ogden, C. L., Grummer-Strawn, L. M., Flegal, K. M., Guo, S. S., Wei, R., … Johnson, C. L. (2000). CDC growth charts: United States. Advance Data, 314, 1–27.
- Le Grange, D., Doyle, P. M., Swanson, S. A., Ludwig, K., Glunz, C., & Kreipe, R. (2012). Calculation of expected body weight in adolescents with eating disorders. Pediatrics, 129(2), e438–e446. doi:https://doi.org/10.1542/peds.2011-1676
- Lock, J. (2018). Family therapy for eating disorders in youth: Current confusions, advances, and new directions. Current Opinion in Psychiatry, 31, 431–435. doi:https://doi.org/10.1097/YCO.0000000000000451
- Lock, J., & Le Grange, D. (2013). Treatment manual for anorexia nervosa: A family - based approach (2nd ed.). New York, NY: The Guilford Press.
- Magill, N., Rhind, C., Hibbs, R., Goddard, E., Macdonald, P., Arcelius, J., … Treasure, J. (2016). Two‐year follow‐up of a pragmatic randomised controlled trial examining the effect of adding a carer’s skill training intervention in inpatients with anorexia nervosa. European Eating Disorders Review, 24, 122–130. doi:https://doi.org/10.1002/erv.2422
- Marzola, E., Knatz, S., Murray, S. B., Rockwell, R., Boutelle, K., Eisler, I., & Kaye, W. H. (2015). Short-term intensive family therapy for adolescent eating disorders: 30-month outcome. European Eating Disorders Review, 23, 210–218. doi:https://doi.org/10.1002/erv.2353
- Matthews, A., Peterson, C. M., Peugh, J., & Mitan, L. (2019). An intensive family-based treatment guided intervention for medically hospitalized youth with anorexia nervosa: Parental self-efficacy and weight-related outcomes. European Eating Disorders Review, 27, 67–75. doi:https://doi.org/10.1002/erv.2632
- Platt, S. (1985). Measuring the burden of psychiatric illness on the family: An evaluation of some rating scales. Psychological Medicine, 15(2), 383–393. doi:https://doi.org/10.1017/s0033291700023680
- Richards, I. L., Subar, A., Touyz, S., & Rhodes, P. (2018). Augmented approaches in family-based treatment for adolescents with restrictive eating disorders: A systematic review. European Eating Disorders Review, 26, 92–111. doi:https://doi.org/10.1002/erv.2577
- Rienecke, R. D. (2017). Family-based treatment of eating disorders in adolescents: Current insights. Adolescent Health, Medicine and Therapeutics, 8, 69–79. doi:https://doi.org/10.2147/AHMT.S115775
- Schene, A. H. (1990). Objective and subjective dimensions of family burden. Towards an integrative framework for research. Social Psychiatry and Psychiatric Epidemiology, 25(6), 289–297.
- Sepúlveda, A. R., Graell, M., Berbel, E., Anastasiadou, D., Botella, J., Carrobles, J. A., & Morandé, G. (2012). Factors associated with emotional well-being in primary and secondary caregivers of patients with eating disorders. European Eating Disorders Review, 20, e78–e84. doi:https://doi.org/10.1002/erv.1118
- Sepúlveda, A. R., Whitney, J., Hankins, M., & Treasure, J. (2008). Development and validation of an Eating Disorder Symptom Impact Scale (EDSIS) for carers of people with eating disorders. Health and Quality of Life Outcomes, 6, 28. doi:https://doi.org/10.1186/1477-7525-6-28
- Shaffer, D., Gould, M., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., & Aluwahlia, S. (1983). A Children’s Global Assessment Scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. doi:https://doi.org/10.1001/archpsyc.1983.01790100074010
- Simic, M., & Eisler, I. (2015). Multi-family therapy. In K. L. Loeb, D. Le Grange, & J. Lock (Eds.), Family therapy for adolescent eating and weight disorders: New applications (pp. 110–138). New York, NY: Routledge.
- Singh, S., Accurso, E. C., Hail, L., Goldschmidt, A. B., & Le Grange, D. (2018). Outcome parameters associated with perceived helpfulness of family-based treatment for adolescent eating disorders. International Journal of Eating Disorders, 51, 574–578. doi:https://doi.org/10.1002/eat.22863
- Slater, J., Treasure, J., Schmidt, U., Gilchrist, P., & Wade, T. D. (2015). A pilot study of associations between treatment for anorexia nervosa and carers ́ distress. Clinical Psychology and Psychotherapy, 22, 372–376. doi:https://doi.org/10.1002/cpp.1895
- Stillar, A., Strahan, E., Nash, P., Files, N., Scarborough, J., Mayman, S., … Lafrance Robinson, A. (2016). The influence of carer fear and self-blame when supporting a loved one with an eating disorder. Eating Disorders, 24, 173–185. doi:https://doi.org/10.1080/10640266.2015.1133210
- Svensson, E., Nilsson, K., Levi, R., & Suarez Carballeira, N. (2013). Parents ́ experiences of having and caring for a child with an eating disorder. Eating Disorders, 21, 395–407. doi:https://doi.org/10.1080/10640266.2013.827537
- Tabachnick, B. G, & Fidell, L. S. (2013). Using multivariate statistics, 6th. Boston, MA:Pearson Education, Inc.
- Treasure, J., & Nazar, B. P. (2016). Interventions for the carers of patients with eating disorders. Current Psychiatry Reports, 18(2), 16. doi:https://doi.org/10.1007/s11920-015-0652-3
- Wallin, U. (2007). Multi-family therapy with anorexia nervosa. A treatment manual. Lund: Lund University.
- Wallis, A., Miskovic-Wheatley, J., Madden, S., Rhodes, P., Crosby, R. D., Cao, L., & Touyz, S. (2017). How does family functioning effect the outcome of family-based treatment for adolescents with severe anorexia nervosa? Journal of Eating Disorders, 5, 5–9. doi:https://doi.org/10.1186/s40337-017-0137-3
- Wallis, A., Miskovic-Wheatley, J., Madden, S., Rhodes, P., Crosby, R. D., Cao, L., & Touyz, S. (2018). Family functioning and relationship quality for adolescents in family-based treatment with severe anorexia nervosa compared with non-clinical adolescents. European Eating Disorders Review, 26, 29–37. doi:https://doi.org/10.1002/erv.2562