ABSTRACT
Research shows that the Unresolved-disorganized attachment representation (U), resulting from experiences of loss or abuse, is associated with a range of psychiatric conditions. However, clinical implications of U are yet unclear.
Objective: To investigate how U is related to symptoms and recovery of eating disorder (ED) patients.
Method: First, 38 ED patients starting psychotherapeutic treatment were compared to 20 controls without ED on the prevalence of U, assessed with the Adult Attachment Interview. Second, in the patient group relations between U and ED symptoms, depression, anxiety and subjective experience of symptoms were investigated. Third, we compared, 1 year afterwards, recovery of patients with and without U.
Results: The prevalence of U was higher in ED patients than in controls. Symptom severity was not related to U. ED patients with U at the start of treatment improved significantly more regarding anxiety, depression and subjective experience of symptoms than did patients without U.
Discussion: The differential recovery of ED patients with or without U confirms the trauma-related heterogeneity of patients found in other diagnostic groups and calls for further investigation into the treatment needs of patients with different attachment representations.
Clinical implications
Unresolved-disorganized attachment (U) is a risk factor for psychopathology
The prevalence of U is higher in eating disorders (ED) patients than in controls
Symptom severity of ED patients was not related to U
ED patients with U show differential recovery than patients without U
ED patients with U improved more on anxiety, depression and psycho-neuroticism
Introduction
Unresolved-disorganized attachment resulting from traumatic experiences of loss or abuse is an important risk factor for the development of psychopathology. For example, it has been associated with borderline personality disorder, post-traumatic stress disorder, suicidality, substance abuse, anti-social personality disorder, and eating disorders (Kuipers & Bekker, Citation2012; Van IJzendoorn & Bakermans-Kranenburg, Citation2008). Unresolvedness (U) can be measured with the Adult Attachment Interview (AAI) (George et al., Citation1996) and is characterized by signs of disorientation and/or dissociation while discussing deaths of close persons or experiences of physical/sexual abuse. It is considered as a temporarily collapse of attachment strategy due to the ongoing influence of traumatic experiences on mental or behavioral processes (Hesse & Main, Citation2000), which manifests itself in the AAI by lapses in reasoning or discourse (Main et al., Citation2002). For example, unresolved individuals may talk about a deceased person as though he or she were alive, may show signs of visual intrusions while discussing a traumatic event or may suddenly change to a confused way of speaking. These disorganized narratives in case of loss or abuse indicate that the individual is still overwhelmed by incompletely remembered loss experiences or frightening traumatic events (Lyons-Ruth & Jacobvitz, Citation2016). A meta-analysis of over 200 adult attachment studies showed a prevalence of U of 43% in a mixed clinical sample (Bakermans-Kranenburg & van IJzendoorn, Citation2009), which is significantly higher than in normative groups. U is therefore considered a transdiagnostic risk factor that is relevant across psychopathologies and has been suggested to account for patient characteristics within diagnostic categories (Riem et al., Citation2019). However, the clinical implications of the high prevalence of U in psychiatric groups are still unclear. In the current study, we, therefore, examined how U resulting from loss and abuse relates to symptom severity and recovery in ED patients.
The high prevalence of unresolved loss and abuse in ED patients may be due to a relatively higher actual occurrence of potentially traumatic events in their lives. In a Swedish study, however, ED patients did not report greater overall exposure to traumatic experiences (i.e., deaths, sexual or physical abuse, accident or natural disaster) than did non-clinical young adults: in both groups, those exposed were 1:5 (Backholm et al., Citation2013). Nevertheless, the nature of the mostly reported traumatic experiences differed. Non-clinical young adults often reported violence, accidents and bereavement, ED patients more often experiences of sexual abuse. Jacobi et al. (Citation2004) also found higher rates of sexual abuse for patients with anorexia nervosa (AN) or bulimia nervosa (BN) than for community controls (but similar rates to those of psychiatric controls). Sexual abuse, therefore, seems a non-specific risk factor for the development of EDs, possibly because it results in an insecure attachment status. Indeed, Tasca et al. (Citation2013) found that attachment insecurity partly mediated the relation between childhood sexual abuse and ED symptoms later in life (Tasca, Citation2019; Tasca et al., Citation2013).
However, not all children who experience a loss or abuse develop an unresolved status. Resilience factors, such as personality, cognitive functioning, and parenting, may explain individual variability in the pathways from loss or abuse to (mal)adaptation (Masten et al., Citation2008). Moreover, not all ED patients have a history of abuse; some develop ED in the context of other risk factors (Jacobi et al., Citation2004). This etiological heterogeneity may explain individual differences in the clinical presentation of ED. An interesting question is, therefore, whether U is related to ED and co-morbid symptom severity. Although still little is known how U relates to ED’s clinical presentation, some studies indicate that ED patients with a history of trauma show more severe symptoms. For example, Backholm et al. (Citation2013) showed ED patients with a history of trauma (physical assault, sexual trauma, death, natural disaster, accident) had more severe ED as well as comorbid depressive, anxiety and compulsive symptoms than ED patients without trauma, with sexual trauma having the greatest impact. This could be due to the presence of complex trauma symptoms, such as dissociation, inconsistent sense of self, and relationship problems after traumatic events (Bailey et al., Citation2007).
An unresolved status with respect to loss or trauma may also matter for treatment response and recovery. Regarding treatment outcome, cognitive behavioural therapy appeared less effective in reducing ED- and comorbid symptoms for ED patients with a history of childhood abuse than for those without (Castellini et al., Citation2018). This is consistent with studies examining treatment response in other clinical groups of patients with and without trauma. For example, depressed patients with a history of trauma (especially, parental loss) did not benefit from pharmacotherapy as did patients without trauma (Nanni et al., Citation2012; Nemeroff et al., Citation2003), but they responded better to psychotherapy. In addition, patients with depressive, anxiety, and substance use disorders and a history of childhood maltreatment showed higher illness severity and poorer treatment response than did non-maltreated patients with the same diagnoses (Teicher & Samson, Citation2013). These authors introduced the concept of ‘maltreated ecophenotype’ to explain this abuse-related heterogeneity within diagnostic classifications (see also Teicher & Samson, Citation2016). This pattern of findings raises the question whether also ED patients with or without a history of trauma show different recovery rates or respond differently to treatment. ED patients with trauma may benefit less from treatment, particularly in case of unresolved trauma. Thus, U could call for a different therapeutic approach. Notice that caregivers with an unresolved attachment status indeed responded less well to parenting interventions (Moran et al., Citation2005; Routh et al., Citation1995); in general, however, the role of U in response to treatment in psychiatric groups is still scarcely examined.
Therefore, the first aim of the present study was to (1) explore differences between ED patients and controls regarding the frequency of reports of experiences of loss and abuse during the AAI, and regarding U for loss or abuse. U with respect to loss and abuse were examined separately, because most studies combine both unresolved subtypes for analysis and only few studies examined U-abuse and U-loss separately regarding their associations with psychiatric conditions. In addition, we aimed to (2) investigate the association between U and symptoms in ED patients, and (3) investigate whether the recovery in ED patients differed between those with and without U at the start of treatment. Our hypotheses were that (1) experiences of loss and abuse would be more frequent in ED patients than in controls; (2) U for loss or abuse would be more frequent in ED patients than in controls; (3) ED symptoms, anxiety, subjective experience of symptoms and depression would be more severe in patients with U; and (4) recovery would be less for patients with U.
Method
Participants
This study is part of a longitudinal project on attachment, mentalization, and symptoms of ED patients, approved by The Netherlands’ medical ethical committee for mental health institutions (METIGG). Details on the sample have also been described elsewhere (see Kuipers et al., Citation2016, Citation2017). Participants were ED patients who completed 1 year of treatment in one of two specialized ED treatment centers in the southern part of The Netherlands; and controls.
Clinical group
Of the original 50 (all female) patients who were included at the start of treatment (T1), 38 also participated 1 year later at T2 (completers), and 12 patients participated only at T1 (dropouts). Dropouts were older (M = 28.7 years, SD = 11.4) than completers (M = 22.2 years, SD = 3.45; t(48) = −3.16, p =.003); they did not differ from completers regarding level of education, attachment, mentalization, ED or comorbidity. Compared with both completers and controls, the dropouts scored higher on the AAI-subscale Unresolvedness (F(2, 68) = 7.463, p = .001). At the start of treatment, 73% of the completers had AN, 10.5% BN, and 16.5% ED NOS (American Psychiatric Association, Citation2000).
The treatment consisted of 6 months’ 4–5 day/week group treatment followed by 3 months of 2 day/week group treatment, and 3 months of individual outpatient psychotherapy, respectively. “Group treatment” here included group and individual Mentalization-Based Treatment (MBT: Bateman and Fonagy, Citation2004), daily meals, art therapy, and psychomotor therapy. Therapists and nurses were trained and supervised by MBT trainers (De Viersprong/Stichting MBT Nederland). In addition to the original MBT format, ED patients set targets for the restoration of eating behaviours and weight, and underwent regular somatic assessment (Skårderud & Fonagy, Citation2012). Treatment aims were to normalize eating behavior and weight; to enhance the capacity to understand mental states in self and others (i.e., “mentalization”; Bateman & Fonagy, Citation2004); to improve the recognition, expression, and regulation of emotions; to improve body awareness and body satisfaction; and to improve social skills and relationships. Treatment groups were open and slowly changing because patients moved on to different therapeutic phases on a regular basis.
Controls. The control group consisted of 20 undergraduate students from Tilburg University, School of Social and Behavioral Sciences (19 women) without any ED who were recruited online using the Research Participation system of Tilburg University. They participated for course credits. The mean age of patients (M = 22.2, SD = 3.5) and controls (M = 21.4, SD = 5.8) did not differ significantly. Educational level was, however, higher in the control group because only 46% of the patients had a university level of education.
Procedure
This study was part of a larger project on changes in attachment representation in patients with ED. In the current study, we focus on the role of Unresolvedness in recovery. Details on changes in attachment status have been described elsewhere (see Kuipers et al., Citation2016, Citation2017). Both groups were screened with the section on psychotic symptoms of the Mini–International Neuropsychiatric Interview (MINI; Sheehan et al., Citation1998) to guarantee that no participant suffered from a psychosis. We administered the Structured Clinical Interview for DSM Axis I disorders (SCID-I; First et al., Citation1996) to diagnose EDs, and depression. To classify the state of mind with regard to attachment, the Adult Attachment Interview (AAI; George et al., Citation1996; Dutch translation by Van IJzendoorn et al., Citation1999) was administered. Symptom severity was measured with self-report questionnaires regarding ED symptoms, state and trait anxiety, and subjective experience of symptoms at T1 and T2.
Measures
The AAI (George et al., Citation1996; Van IJzendoorn et al., Citation1999) is a structured interview of 20 questions that concern childhood experiences with parents/parental figures, and lifetime experiences of loss or traumatic abuse as defined in the AAI scoring manual (Main et al., Citation2002). Using this interview, an attachment classification can be assigned to participants, based on the coherence of the narrative that is told during this interview. The category Unresolvedness/disorganization is assigned to transcripts that show lapses of reasoning and discourse surrounding the discussion of loss or abuse during the AAI, such as moments of absorption or dissociation, or, for example, irrational beliefs or guilt while dwelling upon these experiences in the interview. The following questions are asked to discuss loss experiences: “Did you experience the loss of a parent or other close loved one while you were a young child, for example, a sibling or a close family member? Did you lose any other important persons during your childhood? Have you lost other close persons in adult years?” Abuse is asked with the following questions: “Some people have memories of threats or some kind of behavior that was abusive. Did anything like this ever happen to you?” According to AAI criteria, abuse is defined as physical or sexual abuse, not emotional abuse or neglect. The severity of signs of disorganization in the interview is scored on a 9-point scale. Individuals with scores above the score of 5.5 are assigned the classification U. “U” is not classified in case of recent loss (<1 year prior to the interview). An independent person who was blind for participants’ status (control or patient, T1 or T2) scored the AAI transcripts (S. den Hollander, trained by D. Pederson & D. Jacobvitz and reliable since 2001; again followed AAI Institute by J. Sroufe, in 2012). G. Kuipers (trained by D. Pederson & D. Pederson, and reliable since 2011) also classified 10 AAI interviews. The estimated interrater reliability was good: κ = .74. It should be noted that U cannot be assessed with self-report questionnaires for measuring adult attachment, as the AAI has the advantage, unlike self-report questionnaires, of accessing information on attachment that the interviewed individual is not consciously aware of (Steele et al., Citation2009).
The Eating Disorder Inventory-II (EDI–II; Garner, Citation1991; Dutch translation by Van Strien, Citation2002) short version is a self-report, 64-items questionnaire. Each item has six answering categories, ranging from 1 (never) to 6 (always). The EDI–II short version consists of eight subscales on behaviors and personality traits associated with EDs. The total score on the EDI–II short version reflected the severity of ED symptoms. In our sample, test-score reliability estimated by Cronbach’s alpha was .91 for the total EDI score.
The State Trait Anxiety Inventory (STAI; Spielberger, Citation1983; Dutch translation by Van der Ploeg et al., Citation1979) is a self-report questionnaire that consists of two subscales: State Anxiety and Trait Anxiety, i.e., level of anxiety and proneness to anxiety, respectively. Both scales consist of 20 items that are scored on a 4-point scale, ranging from 1 (not at all) to 4 (very much). In our sample, Cronbach’s alpha was .97 for State Anxiety and .96 for Trait Anxiety.
The Symptom Checklist-90 (SCL-90; Derogatis, Citation1977; Dutch version by Arrindell & Ettema, Citation1986) is a self-report questionnaire consisting of 90 items. In each item, the respondent indicates the prevalence of a psychological symptom during the previous week on a 5-point scale, ranging from 1 (not at all) to 5 (very much). Eight dimensions of psychopathology are assessed: agoraphobia, anxiety, depression, somatization, insufficient thinking and acting, interpersonal sensitivity, hostility, and sleeping problems. In this study, the total score was used as a measure of the subjective experience of symptomatic distress; reliability estimated by Cronbach’s alpha was .98 in our sample.
Current depression was assessed with the SCID-I (First et al., Citation1996); severity of depressive symptoms ranging from 0 (none), 1 (mild), 2 (moderate), to 3 (severe).
Statistical analyses
First, the frequencies of experiences of loss or abuse, and of classification U in the patient group were compared to those in the control group using chi-square tests. In addition, the mean scores on the AAI subscales Unresolvedness for abuse, Unresolvedness for loss and Unresolvedness total were compared between control group and patient group using two-sided t-tests for independent samples of unequal size. Second, we compared mean scores on the EDI–II and SCL-90, STAI subscales Trait anxiety and State Anxiety and mean severity of depression between ED patients with or without AAI-classification U, using two-sided t-tests for independent samples of unequal size. Third, a repeated-measures ANOVA was performed in order to examine whether response to treatment differed between patients with or without U. Dependent variables were mean total EDI–II score, mean total SCL-90 score, mean Trait anxiety, mean State anxiety, and mean severity of depression, time (T1 and T2) was the within-subject factor and subgroups (U versus non-U) the between-subjects factor.
Results
Loss, abuse and unresolvedness for patients and controls
We found no differences between ED patients and controls with regard to the prevalence of experiences of loss or abuse: 85% (N = 17) of the controls had experienced loss vs. 71.1% (N = 27) of the patients; χ2(1) = 1.39, p = .24. Compared to 15% (N = 3) of the controls, 26.3% (N = 10) of the ED patients had experienced sexual and/or physical abuse; χ2(1) = .96, p = .33. Patients did not report sexual abuse more often than controls; 13.2% vs. 10%; χ2(1) = .12, p = .73.
In line with our expectation, ED patients were more often classified as Unresolved for loss or abuse compared to healthy controls. The percentage U was higher in the patient group (60.5%) than in the control group (10.0%), χ2(1) = 5.49, p = .019, φ = .30. In the control group 1 of the 15 persons who reported loss, received classification U; and 1 of the 3 persons reporting abuse, was classified U. In the patient group, 7 of the 22 persons who reported only loss, were classified U; and 8 of the 10 persons who reported abuse—with or without loss—received classification U. shows the distribution of classification U for ED patients and controls.
Table 1. Frequency of AAI classification U for controls and eating disorder patients (with adjusted residuals in parentheses)
shows the mean scores and standard deviations on the AAI subscales Unresolvedness for abuse, Unresolvedness for loss and the total score for Unresolvedness, for both ED patients and controls, and the results of two-sided statistical testing. Contrary to our expectation, the mean score on Unresolvedness for abuse was not higher in ED patients than in controls. However, both the mean score on subscale Unresolvedness for loss and the mean total score for Unresolvedness were higher in the patient group than in the controls.
Table 2. Mean scores and standard deviation on AAI-subscales for Unresolvedness in 38 eating disorder patients compared to 20 healthy controls
Unresolvedness and symptoms of eating disorder patients
As is shown in there were no differences between ED patients (N = 15) who were classified U and patients who were not (N = 23) with regard to the mean total scores on EDI–II and SCL-90, mean Trait anxiety and mean State anxiety scores. The severity of depression (not tabulated) did not differ between ED patients with or without U; t(36) = −.852, p = .40.
Table 3. Means and standard deviations of test scores of EDI–II, STAI, and SCL-90 for 38 ED patients with or without AAI-classification U
Recovery
The repeated-measures ANOVA with total EDI–II scores as dependent variable showed a significant effect of time on ED symptom severity, F(1,36) = 17.89, p < .001, partial ɳ2 = .322, but no significant effect of Unresolvedness, F(1,36) = 0.383, p = .540, partial ɳ2 = .11. Neither was there a significant interaction between Unresolvedness and time, F(1,36) = 1.471, p = .233, partial ɳ2 = .39, indicating that the change in ED symptom severity during treatment did not differ for patients with and without classification U.
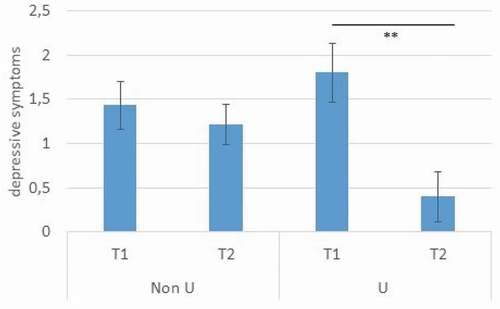
The repeated-measures ANOVA with total SCL-90 scores as dependent variable showed a significant effect of time, F(1,36) = 18.592, p < .001, partial ɳ2 = .341, but no significant effect of Unresolvedness, F(1,36) = 0.75, p = .786, partial ɳ2 = .2. However, there was a significant interaction between Unresolvedness and time, F(1,36) = 4.413, p = .043, partial ɳ2 = .109. Patients with classification U showed a significantly stronger decrease in the subjective experience of symptoms over time compared patients without this status (see ).
Figure 1. Decrease in mean total score of SCL-90 after 1 year of treatment for ED patients with or without classification Unresolvedness
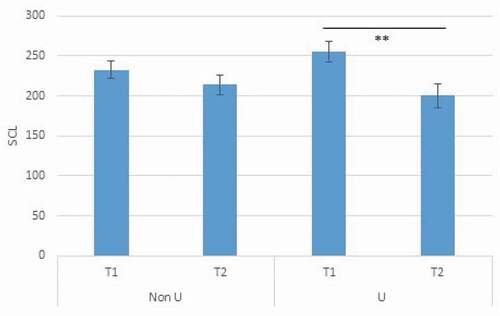
The repeated-measures ANOVAs with anxiety showed significant effects of time on trait anxiety, F(1,36) = 16.286, p < .001, partial ɳ2 = .311, and state anxiety, F(1,36) = 6.103, p = .018, partial ɳ2 = .145. Unresolvedness did not significantly affect trait, F(1,36) = 0.237, p = .622, partial ɳ2 = .7, or state anxiety, F(1,36) = 0.270, p = .606, partial ɳ2 = .7. Neither was there a significant interaction between Unresolvedness and time in the analysis with state anxiety, F(1,36) = 0.702, p = .408, partial ɳ2 = .19. However, the analysis with trait anxiety revealed a significant interaction between Unresolvedness and time, F(1,36) = 5.443, p = .025, partial ɳ2 = .131. Patients with U showed a significantly stronger decrease in trait anxiety over time than did patients without U (see ).
Figure 2. Decrease in mean score on Trait Anxiety after 1 year of treatment for ED patients with or without classification Unresolvedness
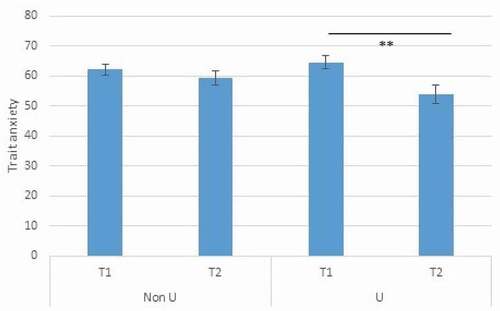
The repeated-measures ANOVA with depression showed a significant effect of time F(1,36) = 1.489, p = .003, partial ɳ2 = .225 and a significant interaction between time and unresolvedness, F(1,36) = 5.608, p = .023, partial ɳ2 = .135. Again, patients with U showed a significantly stronger decrease in depressive symptoms compared to patients without classification U (see ). There was no significant effect of unresolvedness, F(1,36) = 0.532, p = .47, partial ɳ2 = .015.
Discussion
The current study aimed to examine frequencies of unresolved loss and abuse in ED patients compared to non-clinical controls; and whether Unresolvedness (U) in the clinical group is related to symptom severity and recovery. Confirming previous research (Fonagy et al., Citation1996; Kuipers et al., Citation2016; Ward et al., Citation2001), the prevalence of AAI classification U appeared higher in the ED patients than in the controls. Contrary to our expectations, ED and co-morbid symptoms did not differ between patients with and without U. However, ED patients with U changed differently during treatment than did ED patients without U: They improved more regarding depression, trait anxiety and subjective experience of symptoms.
Interestingly, our finding that ED patients were more often classified with U than controls, was not due to a higher number of reported loss or abuse experiences. This is consistent with previous research: also Backholm et al. (Citation2013) showed similar frequencies of overall traumatic experiences in ED patients and in a community sample (Backholm et al., Citation2013), except for sexual abuse. However, this result regarding sexual abuse was not confirmed in our study. This may be due to the use of different trauma measures. Backholm et al. (Citation2013) defined trauma according to DSM-criteria, while we used the AAI. Notice that, according to Bailey et al. (Citation2007), the AAI may underestimate the prevalence of abuse experiences, by letting respondents (subjectively) evaluate whether an experience was abusive. If abuse is denied, the topic is not explored further. This contrasts to the detailed probes for loss (see Measures).
As the higher prevalence of U in the ED patients in this study could not be explained by higher numbers of reported loss or abuse experiences, other factors should be considered. In general, it is an attachment insecurity that raises the risk for U (Bailey et al., Citation2007). However, in our study ED patients and controls did not differ in insecure attachment classifications (Kuipers et al., Citation2016). Low quality of relationships is another risk factor for U (Aikins et al., Citation2009). ED patients often suffer from interpersonal difficulties; this could also be true for our sample, thus partly explaining the higher prevalence of unresolvedness. Another, possibly relevant factor is mentalization, that is, the ability to understand the actions of oneself and others as meaningful on the basis of intentional mental states such as personal desires, needs, feelings, believes and reasons (Bateman & Fonagy, Citation2004).” ED patients, especially those with AN, often show mentalizing deficits (Kuipers & Bekker, Citation2012). Poor mentalization incapacitates the ability to process the emotions, pain, confusion and questions raised by traumatic loss or abuse. Moreover, traumatic events themselves tend to impair mentalization (Allen, Lemma & Fonagy, Citation2012).
Our expectation that symptom severity would be related to U was based on studies showing links between symptom severity and a history of trauma in ED patients (Backholm et al., Citation2013), and patients with depression, anxiety and substance disorders (Teicher & Samson, Citation2013). However, we did not find a full association of U with loss and/or trauma: only 31% of ED patients who experienced loss, and 80% of the patients who experienced abuse, were classified Unresolved. This finding is consistent with previous research showing that attachment status and childhood experiences represent different constructs (Waters et al., Citation2000). Interestingly, U for abuse seemed to overlap more strongly with actual reports of abuse than U for loss with reports of loss. Similarly, Bailey et al. (Citation2007) also found a stronger association between abuse and unresolvedness than between loss and unresolvedness. In their study 55% of women reporting physical abuse, 71% of women reporting sexual abuse, and 15% reporting loss were classified with U. This suggests that the experience of loss is in itself not necessarily traumatic; it might be in the context of, e.g., lack of close relationships or impaired capacity to cope with emotions that a loss becomes an unresolved experience.
Furthermore, we hypothesized that there would be an association between U and change in symptoms during treatment. Surprisingly, the effects we found were in another direction than we had expected. More specifically, patients who were unresolved at the start of treatment improved significantly more on anxiety, depression and subjective experience of symptoms than patients who were not. Although this effect should be interpreted with caution because of the small sample and attrition, it is in line with recent suggestions that ED patients with a history of trauma—for whom CBT had less effect than for ED patients without trauma—would need a treatment that explicitly targeted their problems with social information processing (Monteleone et al., Citation2018). In line with this suggestion, Tasca (Citation2019) describes a model in which traumatic experiences may lead to attachment insecurity, differential emotion regulation strategies and interpersonal styles, and low mentalization, which together confer the vulnerability for developing ED symptoms. In his view, treatment should focus on emotion regulation, interpersonal difficulties and mentalization. Indeed, in our study, the MBT we provided with its focus on the (emotional) meaning of actual interactions and events against the background of past (attachment) experiences might have helped particularly the patients who were unresolved to overcome their affective symptoms. Whereas in CBT improvement is sought in cognitive restructuring, in MBT the capacity to understand mental states in attachment contexts is strengthened in order to improve emotion regulation and interpersonal functioning (Bateman & Fonagy, Citation2009). Interestingly, we did not find a different response to treatment with regard to ED symptoms in patients who were unresolved, which may be explained by the complex, self-perpetuating nature of ED symptoms in which both psychosocial and neurobiological mechanisms are involved (Treasure et al., Citation2010).
Limitations and conclusion
This study’s results confirm the trauma-related heterogeneity of patients with the same psychiatric diagnosis for a sample of ED patients. U in our sample partly reflects the impact of trauma, but other factors contribute to it as well, especially in the case of loss. A limitation of the study is the use of a control group of healthy students. Comparing a sample of ED patients with another patient sample (e.g., personality or anxiety disorders) would have been more informative on the question whether unresolvedness is related to mental distress in general, or to specific psychopathology. The differential course of comorbid symptoms in ED patients with or without classification U during psychotherapeutic treatment (MBT) calls for further investigation into the treatment needs of patients with different attachment representations. Dropouts in our study scored higher on unresolvedness than completers, which implies the associations we found between unresolvedness and greater improvement in anxiety, depression and subjective experience of symptoms after 1 year of treatment might have been different with lower attrition. Also, the suggestion that MBT would especially benefit patients with unresolved experiences of loss or abuse should be viewed with caution. Further investigations in other diagnostic groups could shed more light on this matter. Future research could compare the effect of CBT versus attachment-oriented psychotherapy for subgroups of ED patients with regard to trauma and unresolved-disorganized attachment.
Disclosure statement
The authors declare no conflicts of interest.
Data Availability Statement
Data is not available due to privacy and ethical restrictions.
References
- Aikins, J. W., Howes, C., & Hamilton, C. (2009). Attachment stability and the emergence of unresolved representations during adolescence. Attachment & Human Development, 11(5), 491–512. https://doi.org/10.1080/14616730903017019
- Allen, J. G., Lemma, A., & Fonagy, P. (2012). Trauma. In A. W. Bateman & P. Fonagy (Eds.), Handbook of mentalizing in mental health practice (pp. 419–444). American Psychiatric Publishing.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th, text revision ed).
- Arrindell, W. A., & Ettema, J. H. M. (1986). SCL-90: Handleiding bij een multidimensionele psychopathologie-indicator [Manual for the multi-dimensional psychopathology indicator]. Swets & Zeitlinger.
- Backholm, K., Isomaa, R., & Birgegård, A. (2013). The prevalence and impact of trauma history in eating disorder patients. European Journal of Psychotraumatology, 4(1), 22482. https://doi.org/10.3402/ejpt.v4i0.22482
- Bailey, H. N., Moran, G., & Pederson, D. R. (2007). Childhood maltreatment, complex trauma symptoms, and unresolved attachment in an at-risk sample of adolescent mothers. Attachment and Human Development, 9(2), 139–161. https://doi.org/10.1080/14616730701349721
- Bakermans-Kranenburg, M. J., & van IJzendoorn, M. H. (2009). The first 10,0 adult attachment interviews: Distributions of adult attachment representations in clinical and non-clinical groups. Attachment and Human Development, 11(3), 223–263. https://doi.org/10.1080/14616730902814762
- Bateman, A., & Fonagy, P. (2004). Psychotherapy for borderline personality disorder: Mentalization based treatment. Oxford University Press.
- Bateman, A., & Fonagy, P. (2009). Randomized-control trial of outpatient mentalization based treatment versus structured clinical management of borderline personality disorder. American Journal of Psychiatry, 166(12), 1355–1364. https://doi.org/10.1176/appi.ajp.2009.9040539
- Castellini, G., Lelli, L., Cassioli, E., Ciampi, E., Zamponi, F., Campone, B., Monteleone, A. M., & Ricca, V. (2018). Different outcomes, psychopathological features, and comorbidities in patients with eating disorders reporting childhood abuse: A 3-year follow-up study. European Eating Disorders Review, 26(3), 217–229. https://doi.org/10.1002/erv.2586
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum.
- Derogatis, L. R. (1977). SCL-90-:Administration,scoring, and procedures manual. Clinical Psychometrics Research.
- First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1996). Structured clinical interview for DSM-IV Axis I Disorders, Clinician Version (SCID—CV). American Psychiatric Press.
- Fonagy, P., Leigh, T., Steele, M., Steele, H., Kennedy, R., Mattoon, G., Target, M., & Gerber, A. (1996). The relation of attachment status, psychiatric classification, and response to psychotherapy. Journal of Consulting and Clinical Psychology, 64(1), 22–31. https://doi.org/10.1037/22-6X.64.1.22
- Garner, D. M. (1991). Eating disorder inventory-2, professional manual. Psychological Assessment Resources.
- George, C., Kaplan, N., & Main, M. (1996). Adult attachment interview 3. Department of Psychology, University of California at Berkeley.
- Hesse, E., & Main, M. (2000). Disorganized infant, child, and adult attachment: Collapse in behavioral and attentional strategies. Journal of the American Psychoanalytic Association, 48(4), 1097–1127. https://doi.org/10.1177/30651000480041101
- Jacobi, C., Hayward, C., De Zwaan, M., Kraemer, H. C., & Agras, W. S. (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19–65. https://doi.org/10.1037/33-2909.130.1.19
- Kuipers, G. S., & Bekker, M. H. J. (2012). Attachment, mentalization and eating disorders: A review of studies using the Adult Attachment Interview. Current Psychiatry Reviews, 8(4), 326–336. https://doi.org/10.2174/157340012803520478
- Kuipers, G. S., Van Loenhout, Z., Van der Ark, L. A., & Bekker, M. H. J. (2016). Attachment insecurity, mentalization and their relation to symptoms in eating disorder patients. Attachment and Human Development, 18(3), 250–272. https://doi.org/10.1080/14616734.2015.1136660
- Kuipers, G. S., Van Loenhout, Z., Van der Ark, L. A., & Bekker, M. H. J. (2017). Is reduction of symptoms in eating disorder patients after one year of treatment related to attachment security and mentalization? Eating Disorders: the Journal of Treatment and Prevention. 26(3), 263–269. https://doi.org/10.1080/10640266.2017.1384916
- Lyons-Ruth, K., & Jacobvitz, D. (2016). Attachment disorganization from infancy to adulthood. In J. Cassidy & P. R. Shaver (Eds.), Handbook of attachment (pp. 667–695). Guilford.
- Main, M., Goldwyn, R., & Hesse, E. (2002). Adult attachment scoring and classification systems. Department of Psychology, University of California at Berkeley.
- Masten, A. S., Best, K. M., & Garmezy, N. (2008). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology, 2(4), 425–444. https://doi.org/10.1017/S0954579400005812
- Monteleone, A. M., Patriciello, G., Ruzzi, V., Cimino, M., Del Giorno, C., Steardo, L., Jr., Monteleone, P., & Maj, M. (2018). Deranged emotional and cortisol responses to a psychosocial stressor in anorexia nervosa women with childhood trauma exposure: Evidence for a “maltreated ecophenotype”?. Journal of Psychiatric Research, 104, 39–45. https://doi.org/10.1016/j.jpsychires.2018.6.13
- Moran, G., Pederson, D. R., & Krupka, A. (2005). Maternal unresolved attachment status impedes the effectiveness of interventions with adolescent mothers. Infant Mental Health Journal, 26(3), 231–249. https://doi.org/10.1002/imhj.20045
- Nanni, V., Uher, R., & Danese, A. (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry, 169(2), 141–151. https://doi.org/10.1176/appi.ajp.2011.11020335
- Nemeroff, C. B., Heim, C. M., Thase, M. E., Klein, D. N., Rush, A. J., Schatzberg, A. F., Keller, M. B., Ninan, P. T., McCullough, J. P., Weiss, P. M., Dunner, D. L., Rothbaum, B. O., Kornstein, S., & Keitner, G. (2003). Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proceedings of the National Academy of Sciences of the USA, 100(24), 14293–14296. https://doi.org/10.1073/pnas.2336126100
- Riem, M. M. E., van Hoof, M. J., Garrett, A. S., van der Wee, N. J. A., van IJzendoorn, M. H., & Vermeiren, R. R. J. M. (2019). General psychopathology factor and unresolved-disorganized attachment uniquely correlated to white matter integrity using diffusion tensor imaging. Behavioural Brain Research, 359, 1–8. https://doi.org/10.1016/j.bbr.2018.10.14
- Routh, C. P., Hill, J. W., Steele, H., Elliott, C. E., & Dewey, M. E. (1995). Maternal attachment status, psychosocial stressors and problem behaviour: Follow-up after parent training courses for conduct disorder. Journal of Child Psychology and Psychiatry and Allied Disciplines, 36(7), 1179–1198. https://doi.org/10.1111/j.1469-7610.1995.tb01364.x
- Sheehan, D. V., Lecubrier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., & Dunbar, G. C. (1998). Mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(suppl. 20), 22–33.
- Skårderud, F., & Fonagy, P. (2012). Eating disorders. In A. W. Bateman & P. Fonagy (Eds.), Handbook of mentalizing in mental health practice (pp. 347–383). American Psychiatric Publishing.
- Spielberger, C. D. (1983). Manual for the state trait anxiety inventory. Consulting Psychologists Press.
- Steele, H., Steele, M., & Murphy, A. (2009). Use of the adult attachment interview to measure process and change in psychotherapy. Psychotherapy Research, 19(6), 633–643. https://doi.org/10.1080/10503300802609698
- Tasca, G. (2019). Attachment and eating disorders: A research update. Current Opinion in Psychology, 25, 59–64. https://doi.org/10.1016/j.copsyc.2018.3.3
- Tasca, G. A., Ritchie, K., Zachariades, F., Proulx, G., Trinneer, A., Balfour, L., Demidenko, N., Hayden, G., Bissada, H., & Wong, A. (2013). Attachment insecurity mediates the relationship between childhood trauma and eating disorder psychopathology in a clinical sample: A structural equation model. Child Abuse & Neglect, 37(11), 926–933. https://doi.org/10.1016/j.chiabu.2013.3.4
- Teicher, M. H., & Samson, J. A. (2013). Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry, 170(10), 1114–1133. https://doi.org/10.1176/appi.ajp.2013.12070957
- Teicher, M. H., & Samson, J. A. (2016). Annual research review: Enduring neurobiological effects of childhood abuse and neglect. Journal of Child Psychology and Psychiatry, 57(3), 241–266. https://doi.org/10.1111/jcpp.12507
- The McKnight Investigators. (2003). Risk factors for the onset of eating disorders in adolescent girls: Results of the Mcknight longitudinal risk factor study. American Journal of Psychiatry, 160(2), 248–254. https://doi.org/10.1176/ajp.160.2.248
- Treasure, J., Claudino, A. M., & Zucker, N. (2010). Eating disorders. The Lancet, 375(9714), 583–593. https://doi.org/10.1016/S0140-6736(9)61748-7
- Van der Ploeg, H. M., Defares, P. B., & Spielberger, C. D. (1979). Zelf- beoordelingsvragenlijst [State trait anxiety inventory]. Swets & Zeitlinger.
- Van IJzendoorn, M. H., & Bakermans-Kranenburg, M. J. (2008). The distribution of adult attachment representations in clinical groups. In H. Steele & M. Steele (Eds.), Clinical applications of the adult attachment interview (pp. 68–98). Guilford Press. https://openaccess.leidenuniv.nl/bitstream/handle/1887/830/7_168_168.pdf?sequence=1
- Van IJzendoorn, M. H., Bakermans-Kranenburg, M. J., Schuengel, C., & Juffer, F., 1999. Gehechtheidsbiografisch interview [Adult attachment interview] [Unpublished Manuscript]. University of Leiden. https://openaccess.leidenuniv.nl/bitstream/handle/1887/1449/168_115.pdf
- Van Strien, T. (2002). EDI-II-NL, handleiding [EDI-II-NL, manual]. Swets & Zeitlinger.
- Ward, A., Ramsay, R., Turnbull, S., Steele, M., Steele, H., & Treasure, J. (2001). Attachment in anorexia nervosa: A transgenerational perspective. British Journal for Medical Psychology, 74(4), 497–505. https://doi.org/10.1348/711201161145
- Waters, E., Hamilton, C. E., & Weinfield, N. S. (2000). The stability of attachment security from infancy to adolescence and early adulthood: General introduction. Child Development, 71(3), 678–683. https://doi.org/10.1111/1467-8624.175