ABSTRACT
Objective
The International Consortium on Manual Therapies (ICMT) is a grassroots interprofessional association open to any formally trained practitioner of manual therapy (MT) and basic scientists promoting research related to the practice of MT. Currently, MT research is impeded by professions’ lack of communication with other MT professions, biases, and vernacular. Current ICMT goals are to minimize these barriers, compare MT techniques, and establish an interprofessional MT glossary.
Methods
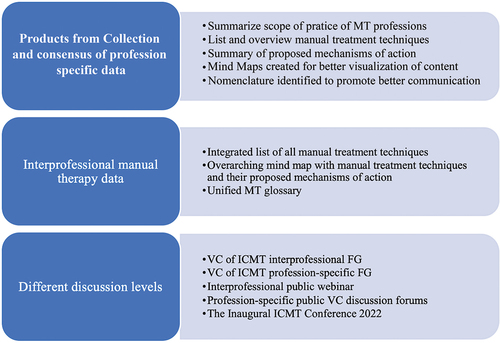
Practitioners from all professions with training in manual therapies were encouraged by e-mail and website to participate (www.ICMTConferene.org). Video conferences were conducted at least bimonthly for 2.5 years by profession-specific and interprofessional focus groups (FGs). Members summarized scopes of practice, technique descriptions, associated mechanisms of action (MOA), and glossary terms. Each profession presented their work to the interprofessional FG to promote dialogue, understanding and consensus. Outcomes were reported and refined at numerous public events.
Results
Focus groups with representatives from 5 MT professions, chiropractic, massage therapy, osteopathic, physical therapy and structural integration identified 17 targeting osseous structures and 49 targeting nonosseous structures. Thirty-two techniques appeared distinct to a specific profession, and 13 were used by more than 1. Comparing descriptions identified additional commonalities. All professions agreed on 4 MOA categories for MT. A glossary of 280 terms and definitions was consolidated, representing key concepts in MT. Twenty-one terms were used by all MT professions and basic scientists. Five terms were used by MT professions exclusive of basic scientists.
Conclusion
Outcomes suggested a third to a half of techniques used in MT are similar across professions. Additional research is needed to better define the extent of similarity and how to consistently identify those approaches. Ongoing expansion and refinement of the glossary is necessary to promote descriptive clarity and facilitate communication between practitioners and basic scientists.
Introduction
Using hands to apply pressure to the body for therapeutic purposes is as old as human history [Citation1,Citation2]. In the 19th century, modern professions incorporating hands-on skills as foundational services began to develop. As their education was formalized in the 20th century, some achieved regulatory support in several regions of the world. Other professions also began incorporating these skills into practice. However, disagreements about approaches and other ideological conflicts resulted in divisions among professions trying to develop distinctive ideologies of practice and establish their utility and value. Relationships between factions within a profession were sometimes acrimonious about ideologies. Professions began isolating themselves and criticizing each other’s systems of practice.
Early publications characterized each profession’s unique identity, defended their reason for existence, or claimed a near 100% success rate for treatment approaches [Citation3–16]. Few studies critically analyzed treatments, identified mechanisms for outcomes, or determined optimization or weaknesses to their approaches. In 1998, the National Institutes of Health established the National Center for Complementary and Alternative Medicine, now the National Center for Complementary and Integrative Health (NCCIH), to guide research for evaluating complementary healthcare fields, including those using hands-on treatment approaches, which they categorized as manual therapies (MT) [Citation17]. Despite numerous programs to establish priorities and resources for research, the lack of communication and collaboration between basic science and MT professions were fundamental barriers to progress [Citation18,Citation19]. Successful communication occurs when shared information is understood by all parties, resulting in positive relationships and strong collaborations [Citation20]. Poor communication occurs when shared information is vague or ambiguous or causes incorrect assumptions about clinical/scientific verbiage. During past interprofessional MT conferences, jargon, imprecise scientific terms, and nomenclature based on original conceptions of professional identity instead of current evidence has undermined progress in this field [Citation19].
In 2018, a grassroots volunteer organization called the International Consortium on Manual Therapies (ICMT) was formed. Its self-selected volunteers came from several MT professions: chiropractic, massage therapy, osteopathic, physiotherapy, and structural integration professions, and basic scientists whose research is relevant to MT. The long-term goal of the ICMT is to improve the practice of MT through promotion of rigorous research within the field. The first step in achieving this goal is to overcome the previously stated hindrance of poor communication related to professional silos, associated jargon, and distrust among professions. Therefore, the ICMT formed 2 working groups. One group, primarily of clinician and basic scientists, was tasked with reviewing the literature and cataloging current evidence on known and postulated mechanisms of action (MOA) across MT professions. The other working group, primarily of clinicians and clinician academics, initiated a process to improve communication by creating focus groups (FGs) that promoted accurate understanding of each profession’s use of MT and their proposed MOA and established an ongoing system for maintaining a unified glossary to facilitate collaborative research. The current article reports the outcomes of these FGs.
Methods
Formation of the international consortium on manual therapies
Administration at the A.T. Still Research Institute, Kirksville, MO., led and coordinated the development and activities of the ICMT. Clinical, academic, and research experts from MT professions and basic scientists whose research focused on the neuromusculoskeletal system were solicited to join the ICMT. MT practitioners without formal training were excluded. The members were from the United States and Europe, representing basic science and 5 MT professions – chiropractic, massage therapy, osteopathic, physiotherapy, and structural integration.
To consolidate the ICMT's interprofessional FG, bimonthly 90-min video conferences established constructive and respectful dialogue and clear, achievable objectives. Members then established profession-specific FGs to draft documents representing their profession. Documents were produced and shared using Google Drive and presented to the interprofessional FG through video conferences. Nominal group technique [Citation21–23] was used to promote dialogue, critique, clarification, understanding, and consensus among professions. In all points of discussion but one, consensus was unanimous with participating members. In that case, one member of a profession with numerous participants expressed cordial disagreement.
On 30 October 2021, the ICMT hosted a 2-h webinar to report progress, receive feedback on profession-specific documents, and solicit participation in continuing ICMT activities. Any MT practitioner, regardless of participation in ICMT involvement, and interested members from the scientific community, could attend. Based on participant comments, interprofessional critique of profession similarities and differences and refinement of documents continued. From January to March 2022, profession-specific discussion forums were held, engaging a broader group of practitioners and researchers for feedback regarding scope and accuracy of content. The FGs further refined documents for dissemination at the Inaugural ICMT Conference ().
Figure 1. Timeline of the International Consortium on manual therapies.
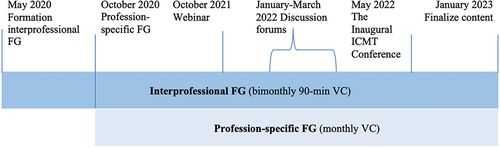
During the conference, presentations summarized ICMT outcomes, and breakout sessions provided opportunities for intraprofessional and interprofessional discussion and vetting of outcomes [Citation24]. Results from these discussions were collated during the following 6 months and informed outcomes presented in the current article.
Specifically, FG outcomes were to (1) summarize the scope of practice of different MT professions to address and overcome possible biases among ICMT members, (2) describe commonly used manual therapeutic techniques of different MT professions, (3) summarize clinician understanding of known and postulated MOA for MT techniques, and (4) generate an interprofessional glossary to improve communication. This qualitative process is illustrated and presented in .
Scope of practice
When available, the legal scope of practice for each MT profession was based on the established practice act that governs the profession’s license and adopted rules pursuant to that act. The scopes of practice also vary within a profession, depending on location or local jurisdictions. Given the international scope of the ICMT, defined scopes of practice were not intended to reflect all possible nuances worldwide and instead focused on consistent language for generalizations and comparisons.
Terms for manual treatment techniques
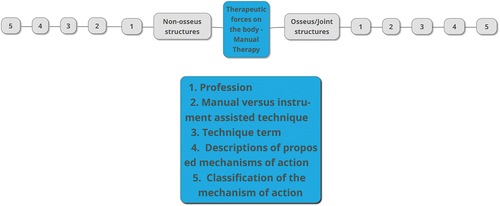
Manual treatment techniques commonly used by each MT profession were cataloged and described by profession-specific FGs. Based on the intended site of action, techniques were subdivided into 2 biologic targets: osseous and nonosseous. Osseous techniques focus on bones, joints, and immediate surrounding tissue; nonosseous techniques focus on myofascial and other connective tissues. We also distinguished between manually delivered and instrument-assisted techniques (i.e. using noninvasive, force-based devices as an extension of the hand). Eponym techniques (e.g. Sutherland, Maitland, Rolf) were avoided when possible in favor of descriptive terms. Terms were placed in a spreadsheet for comparisons. Techniques used by more than 1 MT profession were grouped based on agreement for nomenclature, biomechanical description, and technique performance.
For better visualization, profession-specific mind maps were created to represent techniques and associated proposed MOA. A unified mind map was created for the overall MT field. The paid version of the MindMup software (mindmup.com, United Kingdom) was used for the mind maps.
Proposed mechanisms of action
After unanimous consensus on technique terms was achieved within each profession, FGs described each technique. They also detailed how techniques are performed and provided a summary of known or postulated MOA underlying each technique. This content was incorporated into the mind maps.
Interprofessional glossary
Each profession specific FGs provided a list of terms describing the palpatory approaches, treatment techniques, physical mechanics of technique performance, and practitioners’ perceptions of associated tissue responses when performing the techniques. Basic scientists produced a list of scientific terms for characterization of MT and their influence on the body. Each term was referenced, usually from existing profession-based glossaries. Terms were then placed in a unified interprofessional glossary. The interprofessional FG analyzed terms and identified additional terms used by their professions that they had not originally submitted.
Results
Forty-three ICMT members participated during this 2.5-year project: 3 basic scientists, 7 chiropractors, 1 data manager, 2 librarians, 8 massage therapists, 7 osteopaths, 4 physiotherapists (orthopedic manual physical therapists), 2 staff assistants, and 9 structural integration practitioners. Members were manual therapy practitioners in private practice or contributors to academic programs. Approximately 200 nonmembers participated in the webinar, discussion forums, and conference.
Scope of practice
Key elements for scopes of practice for the 5 MT professions are presented in . Scope of practice for each profession includes legal form, main functional aims, and primary body focus. More complete scope of practice information is available in Supplement 1.
Table 1. Scope of practice for manual therapy (MT) professions.
Terms for manual treatment techniques
Sixty-six terms for manual treatment techniques were identified by the 5 MT professions: 17 were osseous and 49 nonosseous (). Thirty-two were distinct to a profession, and 13 were used by more than 1 profession.
Figure 3. Osseous and nonosseous techniques of the 5 manual therapy (MT) professions.
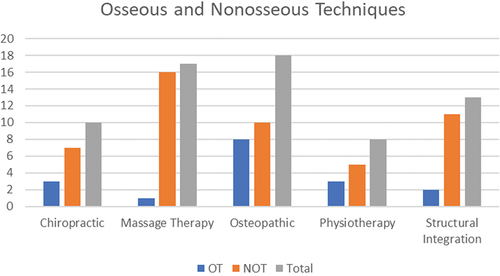
Osseous techniques
Eleven osseous techniques were recorded, ranging from 1 for massage therapy to 8 for osteopathic (). Three manual techniques were commonly described by more than 1 profession: mobilizations; high-velocity, low-amplitude (HVLA); and muscle energy techniques. All MT professions, except structural integration, shared at least 1 osseous technique (chiropractic: 2, massage therapy: 1, osteopathic: 3, physiotherapy: 3) (). An example consensus process for osseous techniques is presented in Supplement 2.
Table 2. Osseous treatment techniques used by the 5 manual therapy (MT) professions.
Nonosseous techniques
Thirty-four nonosseous techniques were recorded, ranging from 5 for physiotherapy to 16 for massage therapy (). Eight manual techniques were used by more than 1 profession. All MT professions, except structural integration, shared terms for at least 4 nonosseous techniques (chiropractic: 6, massage therapy: 7, osteopathic: 7, physiotherapy: 5) (). An example consensus process for non-osseous techniques is presented in Supplement 2.
Table 3. Non-osseous treatment techniques used by 5 manual therapy (MT) professions.
Proposed mechanisms of action
The profession-specific FGs reported the most common MOA for all manual treatment techniques. These clinician-reported MOA, technique descriptions, and information on technique performance are available at the ICMT website (https://www.icmtconference.org/). During interprofessional FGs, all professions acknowledged that these MOA are intertwined, but most reported on the most likely MOAs; structural integration proposed the same cascade of MOA for all their techniques.
Based on similarities among proposed mechanisms, 4 hypothesized MOA categories – local biomechanical, neurophysiologic, fluid/circulatory, and biochemical – were identified and labeled in mind maps. Biomechanical mechanisms involve structural changes at the local tissue level. Neurophysiologic mechanisms involve spinal reflexes or changes in the central nervous system. Fluid/circulatory mechanisms indicate changes in tissue perfusion at an intercellular or circulatory level, and biochemical mechanisms involve changes in biomarkers or second messenger signaling within the cells and tissues. An example consensus process for proposed MOA is presented in Supplement 2.
Mind maps
Mind maps of treatment techniques and proposed MOA commonly accepted in the clinical community for each MT profession are presented in Supplements 3–7. An overview of mind map content is presented in . Massage therapy and structural integration had a predominance for nonosseous treatment techniques; chiropractic, osteopathic, and physiotherapy had a more balanced technical profile with a slight predominance of nonosseous techniques (see and ). An integrated mind map of all MT professions is available at the ICMT website (https://www.icmtconference.org/).
Interprofessional glossary
The chiropractic [Citation25,Citation26], osteopathic [Citation27], and physiotherapy [Citation28] professions already had profession-sanctioned glossaries that were used as a starting point. Other sources included articles, textbooks, and website documents. The interprofessional glossary is presented in Supplement 8.
Chiropractic included 187 terms in the interprofessional glossary, massage therapy 171, osteopathic 134, physiotherapy 129, and structural integration 84. The basic science community provided 103. Twenty-one terms were used or mentioned by all MT professions and basic scientists. Another 5 were mentioned by all MT professions exclusive of basic scientists. Twenty-four terms have more than 1 description; manipulation has 4.
presents examples of several related glossary terms of manipulation with multiple descriptions. The description of manipulation can be very general or more specific, referring to such terms as HVLA and thrust. It can also be specific to profession or technique. Basic scientists recently redefined manipulation to include the adjective force-based, which supports the general meaning. Thrust also has 2 descriptions, which physiotherapy combines with HVLA to define manipulation. Although thrust was in the osteopathic glossary [Citation27], it was not included as a separate entry but as synonymous for HVLA and used as such by the profession. Osteopathic considers HVLA or thrust as a category of manipulation, whereas chiropractic and physiotherapy consider them synonymous. Chiropractic uses 3 meanings for adjustment, and one refers to thrust and another to HVLA.
Table 4. Examples of interprofessional glossary definitions of manipulation and related terms with multiple descriptions as defined by the 5 manual therapy professions and basic scientists.
Discussion
From a healthcare perspective, the goal of the scientific process is to identify effective and safe treatments, so practitioners with appropriate scopes of practice can cure disease and improve patient health. In the MT field, professional isolation and lack of clarity and consistency regarding terminology have hampered dissemination of new knowledge and reduced the impact of research on practice. Studies already have been conducted in which the terms and practices of MT professions have been compared [Citation29–31], a common treatment package for a particular condition was offered [Citation32] and common nomenclature for important anatomical structures across professions was promoted [Citation33]. A model was also proposed for standardizing and more objectively characterizing technique terminology for the physiotherapy profession [Citation34]. To our knowledge, the ICMT’s goal to improve communication by promoting better communication and understanding of the nomenclature and performance of MT procedures is unprecedented. Ideally, this ongoing collaborative process will continue to advance individual and collective evidenced-based professional skills, unify clinician and basic scientist understanding of MOA for treatment techniques, and establish a living interprofessional MT glossary.
Scope of practice
Scope of practice evolves from educational standards within a profession and reflects its research, expert opinion, innovation, and collaborative process to meet societal needs. Educational standards are considered consistent with legal scopes of practice. However, changes in those standards can expand a profession’s legal scope of practice. As such, the scope of practice is often disputed among professions, and any modifications are typically viewed as encroachment on practice and economic security [Citation3,Citation35]. Given the worldwide diversity in licensure and scope of practice between and within healthcare professions, ICMT discussions were crucial in addressing ignorance, misinformation and fostering collaboration. Despite uncomfortable moments, increased knowledge of the scope of practice reduced previous biases and supported respectful relationships. Although there will always be challenges associated with economics, politics, and innovations among healthcare professions, patient-centered practitioners should be committed to overcoming obstacles that inhibit patient care.
Terms for manual treatment techniques
Technique descriptions and mind maps were created by profession-specific FGs and vetted during several online events. Thus, these outcomes should represent the categorization and description of each profession’s commonly used treatment techniques, highlighting commonalities and distinctiveness among professions. Because descriptions provide only a general description of actions performed with the hands during MT, they are not intended as a training guide or comprehensive report of technique nuances. Consequently, less commonly used techniques are not represented in the current article.
In 2010, Evans and Lucas [Citation36] differentiated between definition and description while investigating a robust definition for manipulation. Their criteria [Citation37] for new definitions overlapped with the framework our FGs struggled through to describe techniques. Specifically, Evans and Lucas [Citation37] listed 11 criteria commonly used for definitions for manipulation, but eliminated 6 for being inconsistent, imprecise, and speculative. Our FGs serendipitously excluded the same 6 criteria and did not use 2 additional criteria. The first, mechanical response, overlapped with MOA, and we deemed it inappropriate to include in technique descriptions since MOA for many techniques are unknown or poorly defined. The second, taxonomic consistency, is our eventual target. Currently, we are collaboratively identifying accepted terms with various taxonomic origins. Consequently, ICMT technique descriptions were based on three criteria: biological target (osseous or nonosseous), action (how the technique is performed), and universality (a technique that is sufficient for one tissue or structure (biological target) should be sufficient for any other).
Based on our outcomes, 3 of 12 osseous and 10 of 36 nonosseous techniques were reported by more than 1 MT profession, suggesting more technical differences than similarities among the professions. However, additional comparisons between terms and technique descriptions are necessary for more definitive conclusions.
Regarding osseous techniques, chiropractic, massage therapy, and physiotherapy had name and technique descriptions that were similar to 1–3 osteopathic techniques. The osteopathic profession listed 4 additional distinct techniques. The description of the compress, hold, and release technique of structural integration appeared similar to balanced ligamentous tension technique performed by osteopathic practitioners. The reported instrument-assisted techniques appeared unique to each profession.
Regarding nonosseous techniques, chiropractic, osteopathic, and physiotherapy described soft tissue techniques as soft tissue mobilization/method. Massage therapy classified at least 6 unique techniques commonly used, understood, and identified by chiropractic, osteopathic, and physiotherapy practitioners as soft tissue techniques. Of instrument-assisted techniques, 1 was shared by massage therapy and chiropractic.
Multiple unresolved issues identified by the interprofessional FGs involved myofascial release, soft tissue methods, all structural integration techniques, and the osteopathic fascial distortion model. These terms propose targeting specific components of soft tissue (fascial vs myofascial)promoting technique distinctiveness, yet the FG review identified that the technique descriptions appeared very similar, possibly indicating that these terms are more related to professional dogma than anatomical specificity. It seems obvious that forces applied to soft tissues can not be isolated to one specific type of tissue (muscle, fascia, adipose, etc). In the interprofessional glossary, the soft tissue method for the osteopathic profession was historically defined as a myofascial treatment, calling into question the distinctiveness of these terms. Another example of overlapping terms is muscle energy techniques and proprioceptive neuromuscular facilitation. Both engage the patient in contracting their muscles against practitioner resistance [Citation38]. However, forces and the point in the joint’s range of motion where contraction takes place may differ [Citation39,Citation40,]. This brings into question what is necessary to make techniques distinct and is an important area for future research.
Collapsing similar techniques into consistently used descriptive terms across MT professions should facilitate communication by providing a quick and clear picture of universal characteristics of basic manual techniques. Conversely, collapsed terms may be inadequate for outlining specific nuances of techniques necessary for reproducibility in research modeling or clinical practice. Continued collaboration is needed to determine how to best modify current technique nomenclature to promote understanding and translation between research and clinical practice.
Comparing technique terms, a third or less appeared similar across professions for osseous and nonosseous techniques. Comparing technique descriptions, this similarity may increase to 50%–60%, indicating substantial overlap and distinctiveness in biomechanical characteristics of care provided by MT professions. Findings also indicated that current nomenclature hinders appreciation of comparable aspects of MT and that updating terminology to descriptive, consistently applied terms would improve formation, understanding, and translation of research in this field.
Proposed mechanisms of action
There was marked uniformity among MT professions and basic and clinical scientists when independently reporting known and proposed MOA associated with MT. The consistent outcome of 4 proposed MOA categories provides common ground for collaborative research by clinicians and scientists. When consistent nomenclature is used, there should be an improved understanding of clinical procedures and the strengths and limitations of research designs. Animal model and human research are necessary to advance the understanding of these MOA, and better communication between basic scientists and clinicians will improve the quality, efficiency, translation, and impact of this research.
Considering the 4 MOA categories, direct consequences of mechanical forces on circulatory/fluid mechanisms seem widely understood and accepted. For neurophysiologic mechanisms, underlying mechanisms are less clear; MOA could be related to mechanical forces or psychosocial factors [Citation41,Citation42]. Since body systems do not function in isolation, MT mechanisms may be a cascade of physical and psychological responses, as promoted by those in structural integration. Clarifying neurophysiologic MOA will be challenging and require a wide array of basic science expertise.
Interprofessional glossary
The interprofessional glossary collated by the ICMT contains extensive contributions from 5 MT professions and basic scientists. This unified interprofessional MT glossary is critical for ongoing evaluation of the efficacy and safety of MT approaches [Citation43–45] and for improving translation of research questions and outcomes between practitioners and basic scientists. This tool impacts far beyond research. Because it is based on current evidence and input from the MT community, this glossary is a foundation for education in MT [Citation46] and can minimize communication errors among healthcare providers [Citation47], in medical records, and across MT professions [Citation48,Citation49]. However, individual professions need to continue addressing internal nomenclature inconsistencies and disagreements as they participate in the collaborative refinement of glossary content. Intraprofessional and interprofessional communication needs to be sustained, continuing to advance this interprofessional glossary. In short, the glossary needs ongoing, wide-ranging input, sustained collaboration and widespread acceptance for advancing clinical, educational and research activities.
Our living interprofessional glossary of MT terms is necessary because terms and practice are continuously evolving. For example, a common term-like manipulation should be easily understood by all practitioners. However, Evans and Lucas [Citation36,Citation37] reported major differences between professions regarding the use and understanding of manipulation, as is identified in the interprofessional glossary. The work of Evans and Lucas [Citation36,Citation37] and the work of the ICMT illustrate the necessity of sustaining an interprofessional glossary.
Some professions have modernized technique names to more descriptive terminology, i.e. effleurage and petrissage updated to gliding and kneading. The ICMT supports this trend and recommends every MT profession collaborate to modernize terms that describe technique mechanics, thereby eliminating inconsistent, imprecise, and speculative terms.
Strengths and limitations
The work of the ICMT represents the first systematic attempt to break down a century of MT professional isolation. Given the large number of interprofessional contributors, outcomes should be reasonably representative of each profession. The outcomes also provide a foundation for ongoing work to refine and standardize nomenclature in the MT field.
There are several limitations for reported outcomes. Because professions are at different stages of development, data from profession-specific FGs may have different levels of generalizability. Another limitation is potential bias related to the small number of self-selected ICMT contributors from the United States and a few European countries. Primary contributors of the ICMT review and consensus process were practitioners and academics, so some views may have been omitted through lack of awareness and representation. Further, active engagement of the physiotherapy profession was limited to practitioners in the United States. Another limitation may be related to our level of detail, which we intentionally restricted to commonalities and general patterns of biomechanical properties of manual techniques to promote generalizability and relevance of outcomes to mainstream practice.
Recommendations and roadmap for the future
The ICMT is only starting to reach its overall goal. To succeed, the ICMT workforce should be expanded, and additional interprofessional MT and basic science groups must address identified issues that inhibit advancement of the science and clinical practice of MTs. For better consistency, transparency, and communication, we need to continue unifying technique terms and standardizing descriptions for MTs, especially for techniques that target soft tissues. Once general categories for MT techniques are accepted, objectively quantifying nuances of professional and individual performance of techniques should be considered. We also support the development of reproducible descriptive subcategories that highlight distinct aspects of the consolidated terms. Subcategories are necessary to identify variations in techniques performed by different professions or providers and how techniques are modified for different patients.
Mintken et al [Citation34] proposed 6 parameters for reporting MT: (1) rate of force application, (2) location in range of available movement, (3) direction of force, (4) target of force (anatomical structure), (5) relative structural movement, and (6) patient position. We recommend that MT professions reconsider these parameters and consider adding the magnitude of force in research and clinical practice. Adding magnitude of force applied during a technique should enable the identification of generalizable and distinct technique characteristics and MOA. For basic scientists, laboratory instrumentation can capture these parameters producing continuous data which will allow for unprecedented rigorous research. Since access and use of most instruments in clinical practice is currently unrealistic, developing consistent biomechanical measures using categorical standards should be developed, such as those established for reporting grades of mobilization. The challenge for the clinical and scientific communities is to collaboratively establish standardized and reliable parameters that are feasible for clinical practice. Once established, these standards can be used by clinician researchers to define and calibrate the MT arm of a study. Educational programs can use these standards to advance the training and skills of practitioners.
Conclusions
The outcomes described in the current article reflect the current status regarding treatment techniques in the MT professions. When comparing technique terms, up to one third of the described techniques appear similar between at least 2 MT professions for osseous and nonosseous techniques. When comparing technique descriptions, there was an increase in similarities. Overall, there is a notable lack of specificity associated with techniques directed to soft tissues. The work of the ICMT provides the first steps toward resolution of fundamental nomenclature issues among MT professions. However, to advance the field of MT, additional development and refinement of nomenclature is necessary to reach descriptive clarity and transparency for designing reproducible clinical and basic science research, improving translation of research findings, and promoting meaningful discourse among students, academicians, researchers, and clinicians.
Resubmission Supplement 1 Scope of Practice 4.docx
Download MS Word (27.5 KB)Resubmission Supplement 6 Mind Map Physical Therapy.pdf
Download PDF (14.2 KB)Resubmission Supplement 4 Mind Map Massage Therapy.pdf
Download PDF (26.7 KB)Resubmission Supplement 2 Consensus Examples.docx
Download MS Word (13.1 KB)Resubmission Supplement 5 Mind Map Osteopathic.pdf
Download PDF (21.1 KB)Resubmission Supplement 8 Interprofessional Glossary.docx
Download MS Word (78.6 KB)Resubmission Supplement 3 Mind Map Chiropractic.pdf
Download PDF (14 KB)Resubmission Supplement 7 Mind Map Structural Integration.pdf
Download PDF (442.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10669817.2023.2288495
Additional information
Funding
Notes on contributors
Brian Degenhardt
Brian Degenhardt, DO I am the assistant vice president for osteopathic research at A. T. Still University, director of the Center for Research in Osteopathic Manipulative Medicine (OMM) at the A.T. Still Research Institute, professor in the Department of OMM at the Kirksville College of Osteopathic Medicine and an Osteopathic Heritage Foundation Endowed Chair. I oversee numerous areas of research, particularly directing research in palpatory diagnosis and Osteopathic Manipulative Treatment. I am the director of the practice-based research network called DO-Touch.NET. I am also the co-founded the grass roots organization called the International Consortium on Manual Therapies, a multi-professional organization of manual therapy professionals whose goal is to improve communication and understanding between manual therapy professions, and to establish an ongoing system that promotes collaborative research to advance scientific understanding of the effectiveness and safety of manual therapies. I am a graduate of the Des Moines University College of Osteopathic Medicine and Surgery, completed my residency in OMM and am board certified in Neuromusculoskeletal Medicine/Osteopathic Manipulative Medicine.
Patrick L.S. van Dun
Patrick L.S. van Dun, MSc, DO I have a private practice as an osteopath in Mechelen (Belgium) and Habichtswald (Germany). I received my M.Sc. degree in Rehabilitation and Physical Therapy at the Catholic University Leuven in 1989 and completed my osteopathy studies at COC, organized at the Free University of Brussels, in 1993. I am a researcher and Board of Trustees member of the Centre for Osteopathic MEdicine Collaboration (COME), Pescara (Italy), a non-profit research institute. I have a broad interest in osteopathic research but in recent years have focused on osteopathic professional identity, the practice characteristics of European osteopaths and the health economic value of osteopathy.
Eric Jacobson
Eric Jacobson, PhD, MPH I investigate alternative medicine and teach medical anthropology at Harvard Medical School. My dissertation topic was classical Tibetan medicine’s approach to psychiatric illnesses. I was trained by Ida Rolf in 1974 and am the current president of the Ida P. Rolf Research Foundation. In 2015, I completed an NIH-funded clinical trial of Structural Integration as an adjunct to outpatient rehabilitation for chronic low back pain. Prior to that I was a co-investigator on multiple studies of the placebo effect and diagnostic reasoning in acupuncture.
Sandy Fritz
Sandy Fritz, MS LMT, BCTMB I am a licensed massage therapist, board certified through the National Certification Board for Therapeutic Massage & Bodywork and Certified Massage and Bodywork Educator by the Alliance for Massage Therapy Education. I have a Bachelor of Science in Health Sciences and a Master’s in Organizational Leadership. Since 1994 I have authored academic textbooks on massage therapy with Elsevier publishing.
Paul Mettler
Paul Mettler, PT, DPT I graduated from the University of North Dakota with my degree in physical therapy in 1981 and doctor of physical therapy in 2006. I have practiced for 40 years focusing on the care of orthopedic and musculoskeletal conditions. In 1991, I discovered a way to rapidly identify and undo the damage caused by connective tissue inflammatory process. This innovative technique was originally published in Physical Therapy Today titled “The Mettler Release Technique®: A New Manual Therapy,” but since 2018, is now known as Dermal-Fascial Restoration® or DFR®. Through High Frequency Shear Wave Elastography imaging and other imaging approaches, I have been able to show that DFR reduces skin and fascial stiffness and precisely restructures (or restores) the scar tissue that connects injured tissue without causing further injury. This work has been presented at the Fourth International Fascia Research Congress (FRC) in 2015 and at the International Consortium of Manual Therapies (ICMT) Conference in 2022. It was awarded 2nd place for overall clinical usefulness at the FRC and was the overall winner at the ICMT Conference. My current focus is on dermal and fascial clinical research and education through the non-for-profit DFR Therapy Institute in downtown Chicago.
Norman Kettner
Norman Kettner, DC I am a chiropractic physician and board-certified chiropractic radiologist. I served as chair of radiology at Logan Health Centers, Logan University for 35 years. I am currently professor emeritus in the department of radiology. Research work includes functional brain imaging of neuroplastic dynamics in clinical pain with non-pharmaceutical interventions such as acupuncture and manual therapy. My work has been published in journals include Brain, PAIN, Human Brain Mapping and Brain Stimulation.
G. Franklin
G. Franklin, MBA, I am the Data Manager for A. T. Still Research Institute. I am an applied data scientist evaluating methods for delivering scientific content to the general public. My personal goal is to promote the creation of partnerships for diverse viewpoints in the scientific community to ensure equitable access to data.
Kendi Hensel
Kendi Hensel, DO, PhD I am an osteopathic physician, professor and Vice chair of the Department of Family and Osteopathic Manipulative Medicine at the Texas College of Osteopathic Medicine (TCOM), and a Osteopathic Neuromusculoskeletal Medicine (ONMM) residency director. I completed a Combined Family Medicine/ONMM residency at the University of New England. In 2004, I joined the faculty at the TCOM. I have been an investigator and treatment provider on several research studies on Osteopathic Manipulative Medicine (OMM). I received a K23 Mentored Patient-Oriented Research Career Development Award (2006) from the NIH-NCCIH, studying the effects of OMM on pregnant women. I received my PhD in OMM Clinical Research and Education in 2009 from the University of North Texas Health Science Center-Graduate School of Biomedical Sciences. I served as the 2019- 2020 President of the American Academy of Osteopathy, and served 6 years as a Section Editor of the Journal of the American Osteopathic Association. I am currently involved in clinical, educational and research activities at TCOM, and in national efforts to improve the evidence base and utilization of OMT in patient care. My research interests center around mechanistic and clinical effectiveness studies of OMM.
David Lesondak
David Lesondak, BCSI, ATSI I am an Allied Health Member in the Department of Family and Community Medicine at the University of Pittsburgh Medical Center (UPMC). I am the Senior Structural Integrator and Myofascial Specialist at UPMC’s Center for Integrative Medicine. I am the author of Fascia: What it is and Why it Matters. My follow up work as editor, Fascia, Function, and Medical Applications was nominated for a 2021 British Medical Association award. My podcast, BodyTalk with David Lesondak, is listened to in 49 countries. I was also an invited speaker at the 2020 NIH Conference on Myofascial Pain.
Giacomo Consorti
Giacomo Consorti, DO, MSc (Ost) I am an Italian osteopath, professor and researcher. I am the co-founder of the thematic working group Osteopathy Track & Field and coordinator of the Education Department of the Istituto Superiore di Osteopatia (ISO) in Milan. Currently I am an Italian register of Osteopaths board delegate for Osteopathy Europe (OE) and a member of the OE education committee. I am also an ISO delegate to manage relationships with the European Osteopathic Academic Network (OsEAN). In 2012, I began my training in the field of medical pedagogy through the Italian Society of Medical Pedagogy (SIPeM) of which I am currently a member. Within this position, I collaborate in developing and putting on faculty development events at some Italian and European universities. I have participated in the working groups for the drafting of the Core Competence proposal of the Italian osteopath of the ROI and also participated in the working groups for the drafting of the Core Curriculum proposal developed by the Italian Association of Osteopathy Schools (AISO). I enjoy carrying out research activities for the ISO research department and in collaboration with COME Collaboration. Currently I am the official osteopath of Rovellasca Athlethics.
Leah Frank
Leah Frank, DO I am an osteopathic physician, board-certified in Neuromusculoskeletal Medicine and Osteopathic Manipulative Medicine. I currently work in a private practice in Germany and teach regularly with the Deutsch-Amerikanische Akademie für Osteopathie (DAAO, German-American Academy of Osteopathy). I serve on the DAAO advisory board, leading the task force regarding training German osteopathic physicians in cranial osteopathy. I graduated medical school at the AT Still University Kirksville College of Osteopathic Medicine, where I completed an academic fellowship in Osteopathic Theory and Methods and later held a faculty appointment in the Osteopathic Manipulative Medicine department.
William R. Reed
William R. Reed DC, PhD I am an Associate Professor in the Physical Therapy Department and the Director of the Rehabilitation Science Program at the University of Alabama at Birmingham. My background is as a manual therapy clinician (chiropractor) who after 14 years left a successful private practice to pursue a research career investigating physiological mechanisms underlying manual therapy and physical rehabilitation approaches aimed at alleviating pain and the improving human health. I received a NIH Career Development Award in 2010 to investigate the effects of spinal joint dysfunction on lumbar muscle spindle primary afferent discharge during spinal manipulation in animal models, followed by an NIH R21 award continuing this line of research. I have worked to characterize various animal models of muscular low back pain, so as to investigate mechanisms responsible for musculoskeletal pain relief related to manual therapy interventions. In 2022, my colleagues and I received a NIH U24 award to develop a sustainable research network (ForceNET; https://sites.duke.edu/forcenet/) aimed at developing interdisciplinary collaborations to address current mechanistic knowledge gaps and successfully overcome long-standing barriers in the field of manual therapy.
Cameron MacDonald
Cameron MacDonald, PT, DPT I am currently an associate professor in the Regis University School of Physical Therapy in Denver CO. Following Physiotherapist training in Australia with a musculoskeletal focus, I obtained my Doctorate in Physical Therapy and also completed the Fellowship in Orthopaedic Manual Therapy in 2006 with Regis and currently direct that program and the Orthopaedic Residency. I am dual certified as an orthopedic and geriatric board specialist by the ABPTS. I am currently a PhD candidate University Newcastle, Australia, focusing on the history of manual therapy across professions. Additional lines of research are in dry needling, hip, spinal, shoulder and foot/ankle management. I have 20 publications including regional OMPT management, dry needling and the genesis of manual therapy. I am currently the President of the Program Directors SIG within the AAOMPT. I have presented over 100 posters/platforms/papers at conferences including multiple international presentations with 30 years of clinical practice experience.
Vaclav Kremen
Vaclav Kremen, MScEng, EMBA, PhD I serve as an Associate Professor in the Department of Biomedical Engineering and an Assistant Professor of Neurology at Mayo Clinic in Rochester, MN, USA. In my multifaceted role, I hold the position of Principal Engineer and Research Fellow within the Neurology Department. I am also a Rolfer, have been trained at the European Rolf Association, and actively engage in Rolfing Structural Integration. My commitment to this field extends to my current membership and chairmanship of the Research Committee at the Dr. Ida P. Rolf Institute. My academic contributions include co-authoring over 100 peer-reviewed research papers and several patents. My research interests are rooted in the translation of scientific discoveries into clinical applications.
Crystal Martin
Crystal Martin, DO I am an osteopathic physician board certified in Neuromusculoskeletal Medicine and Osteopathic Manipulative Medicine. My background prior to medical school is in public health and I completed my residency at AT Still University Kirksville College of Osteopathic Medicine. I am on the faculty of Pacific Northwest University of Health Sciences in Yakima, Washington as the Director of Osteopathic Curriculum within the Department of Family Medicine and Osteopathic Principles and Practice. My current research projects involve chronic pain management, fascia, and adaptive sports medicine. My hobbies include rock climbing, ice climbing, skiing, trail running, and playing the violin.
Bernie Landels
Bernie Landels, BHS. BCSI I am a Board-Certified Structural Integration Practitioner (IASI) and hold a Bachelor of Health Studies majoring in Massage & Neuromuscular Therapy. As a qualified adult educator, I have taught massage for over 25 years and was the Owner/Director of the New Zealand College of Massage (2007-2011). As winner of the Ida P Rolf Research Foundation case study competition, I subsequently had my case study “Structural Integration Case Report: a Global Intervention Challenging the Limitations of Local Rehabilitation” published in the International Journal of Therapeutic Massage and Bodywork. I have served on the Ida P Rolf Research Foundation Board of Directors and am currently a member of the Anatomy Trains Structural Integration teaching faculty. I have published a book for parents and professionals on the importance of movement and milestones with a focus on the structure and function of the feet as a child grows.
Paul Standley
Paul Standley, PhD I earned my doctoral degree in medical physiology at Wayne State University School of Medicine in Detroit, Michigan then completed a post-doctoral fellowship in the Division of Endocrinology and Hypertension at the same institution. I moved to Arizona to become a founding faculty member at Midwestern University’s Arizona College of Osteopathic Medicine where I continued NIH-, AHA -, and AOA-funded research on biomechanical modeling of arterial pressure waveforms and developing in vitro models of myofascial release and other manual therapies. As a founding faculty member of the University of Arizona College of Medicine-Phoenix, I have served 12 years as the founding curricular dean. I am currently a tenured professor of basic medical sciences and physiology and director of the Research Office for Medical Education. I have published extensively in the areas of hypertension, vascular biology, effects of biomechanics on gene expression in bioengineered tissues, and medical education research.
References
- Houdeleck J, De Mare J. L’historique des manipulations. In: Hérisson C, and Vautravers P, editors Les Manipulations Vertébrales: Collection de Pathologie Locomotrice 29. Paris, Franc: Elsevier Masson; 1994. p. 1.
- Ottoson A. Wurde die Geschichte der Manipulation von Wirbelsäule und Gelenken manipuliert? Manuelletherapie. 2012;16(4):192–196. doi: 10.1055/s-0032-1327032
- Gevitz N. The DOs: osteopathic Medicine in America. 3rd ed. Baltimore, MD: Johns Hopkins University Press; 2019.
- Leach RA. Doing the same thing and expecting a different outcome: it is time for a questioning philosophy and theory-driven chiropractic research. J Chiropr Humanit. 2019;26:60–74. doi: 10.1016/j.echu.2019.08.002
- Cyriax EF Henrik Kellgren and his methods of manual treatment. John Bale, Sons & Danielsson; 1908. Available from: https://wellcomecollection.org/works/qk5nuet9
- Collins CP, Ling PH A few words on the Curative Power of Systematized Exercises; or the movement cure. Groombridge; 1880. Available from: https://wellcomecollection.org/works/he6zuj6z
- Hulett GD A text book of the principles of osteopathy. 4th ed. Journal Printing Co; 1906. Available from: https://wellcomecollection.org/works/hpszjce9
- Georgii A The movement cure. H. Baillière; 1852. Available from: https://wellcomecollection.org/works/vp7q5xz2
- Still AT, Graves F The Philosophy and mechanical principles of osteopathy. Hudson-Kimberly; 1902. Available from: https://wellcomecollection.org/works/ccfj87sx.
- De Betou IGI. Therapeutic manipulations: or, a successful treatment of various disorders of the human body. Simpkin, Marshall & Co.; 1851. Available from: https://wellcomecollection.org/works/bb454vyj
- Palmer DD. The science of chiropractic. Palmer School Of Chiropractic. 1906. Available from: https://centerforinquiry.org/wp-content/uploads/sites/33/quackwatch/science_of_chiropractic.pdf
- Palmer DD The Chiropractor. Press of Beacon Light, Los Angeles, CA; 1914. Available from: https://welcomecollection.org/works/vhdfhv6c
- Graham D. Massage, manual treatment, remedial movements, history, modes of application, and effects: indications and contra-indications. J.P. Lippincott Company; 1913. Available from: https://welcomecollection.org/works/y5j3fxz8
- Harlan WL. Osteopathy, the new science. Donohue & Henneberry; 1898. Available from: https://welcomecollection.org/works/macgrjjf
- Kellgren A Technic of Ling’s system of manual treatment as applicable to surgery and medicine. Arvid Kellgren. William Wood; 1892. Available from: https://welcomecollection.org/works/prb9k5ft
- Cyriax EF Henrik Kellgren and His Methods of Manual Treatment. John Bale, Sons & Danielsson, 1908. Accessed January 1, 1AD. Available from: https://search.wellcomelibrary.org/iii/encore/record/C__Rb1269548__Skellgren__P3__Orightresult_U?lang=eng&suite=cobalt
- National Center for Complementary and Integrative Health. NCCIH strategic plan FY 2021-2025. [cited 2023 June 23]. Available from: https://www.nccih.nih.gov/about/nccih-strategic-plan-2021-2025.
- National Center for Complementary and Integrative Health. Neurocircuitry of force-based manipulations workshop. Published September 2019. [cited 2023 June 23]. Available from: https://files.nccih.nih.gov/force-workshop-summary-110920-508-updated.pdf.
- Standley PR. My personal journey that led to the crossroads of interdisciplinary manual medicine research: serendipitous opportunities afforded a basic scientist. J Osteopath Med. 2013;113(2):179–183. doi: 10.7556/jaoa.2013.113.2.179
- Hall S. The importance of communication. Prof Payroll Pensions Reward. March 2022;(78);24–25.
- Harvey N, Holmes CA. Nominal group technique: an effective method for obtaining group consensus. Int J Nurs Pract. 2012;18(2):188–194. doi: 10.1111/j.1440-172X.2012.02017.x
- Olsen J. The nominal group technique (NGT) as a tool for facilitating pan-disability focus groups and as a new method for quantifying changes in qualitative data. Int J Qual Methods. 2019;18:18. doi: 10.1177/1609406919866049
- Vande Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health. 1972;62(3):337–342. doi: 10.2105/ajph.62.3.337
- International Consortium on Manual Therapies. Conference. 2022. [cited 2023 June 21]. Available from: https://www.icmtconference.org/international-congress-on-manual-therapies/.
- Glossary. In: Himelfarb I, Hayland JK, Ouzts NE, editors. Practice Analysis of Chiropractic 2020. Greeley, CO: National Board of Chiropractic Examiners; 2020. pp. 134–154
- Harrison DD, Siskin LA. eds. Best practices and practice guidelines. Falls Church, VA: International Chiropractors Association; 2009. pp. 271–282.
- Giusti R, ed. Glossary of Osteopathic terminology. 3rd ed. Bethesda, MD: American Association of Colleges of Osteopathic Medicine; 2017.
- Glossary. In: Rushton A, Beeton K, Jordaan R, editors. Education standards in orthopaedic manipulative therapy. Part A: educational standards 2016. Albany, Aukland: International Federation of Orthopaedic Manipulative Physical Therapists; Vol. 2016. pp. 26–36
- Pincus T, Foster NE, Vogel S, et al. Attitudes to back pain amongst musculoskeletal practitioners: a comparison of professional groups and practice settings using the ABS-mp. Man Ther. 2007;12(2):167–175. doi: 10.1016/j.math.2006.06.005
- van de Veen EA, de Vet HC, Pool JJ, et al. Variance in manual treatment of nonspecific low back pain between orthomanual physicians, manual therapists, and chiropractors. J Manipulative Physiol Ther. 2005;28(2):108–116. doi: 10.1016/j.jmpt.2005.01.008
- Carlesso LC, Macdermid JC, Gross AR, et al. Treatment preferences amongst physical therapists and chiropractors for the management of neck pain: results of an international survey. Chiropr Man Therap. 2014 Mar 24;22(1):11. PMID: 24661461; PMCID: PMC3987839. doi: 10.1186/2045-709X-22-11.
- Harvey E, Burton AK, Moffett JK, et al. UK BEAM trial team. Spinal manipulation for low-back pain: a treatment package agreed to by the UK chiropractic, osteopathy and physiotherapy professional associations. Man Ther. 2003;8(1):46–51. doi: 10.1054/math.2002.0472
- Kumka M, Bonar J. Fascia: a morphological description and classification system based on a literature review. J Can Chiropr Assoc. 2012;56(3):179–191. doi: 10.1007/s00276–010–0757–7
- Mintken PE, DeRosa C, Little T, et al. American Academy of Orthopaedic manual physical therapists. AAOMPT clinical guidelines: a model for standardizing manipulation terminology in physical therapy practice. J Orthop Sports Phys Ther. 2008;38(3):A1–A6. doi: 10.2519/jospt.2008.0301
- Wagner C Exploring European Osteopathic Identity: An Analysis Of The Professional Websites Of European Osteopathic Organizations. Danube University Krems; 2009. [cited 2023 June 21]. Available from: https://www.osteopathicresearch.com/files/original/c0755d065b5fc5fc48efcad8bc44673622a52011.pdf
- Evans DW, Lucas N. What is ‘manipulation’? A reappraisal. Man Ther. 2010;15(3):286–291. doi: 10.1016/j.math.2009.12.009
- Evans DW, Lucas N. What is manipulation? A new definition. BMC Musculoskelet Disord. 2023;24(1):194. doi: 10.1186/s12891-023-06298-w
- Thomas E, Bianco A, Paoli A, et al. The relation between stretching typology and stretching duration: the effects on range of motion. Int J Sports Med. 2018;39(4):243–254. doi: 10.1055/s-0044-101146
- Chaitow L, Liebenson C. Muscle energy techniques. 2nd ed. London, UK: Churchill Livingstone; 2001.
- Ptaszkowski K, Slupska L, Paprocka-Borowicz M, et al. Comparison of the short-term outcomes after postisometric muscle relaxation or kinesio taping application for normalization of the upper trapezius muscle tone and the pain relief: a preliminary study. Evid Based Complement Alternat Med. 2015;2015:721938. doi: 10.1155/2015/721938
- Esteves JE, Cerritelli F, Kim J, et al. Osteopathic care as (En)active inference: a theoretical framework for developing an integrative hypothesis in osteopathy. Frontiers In Psychology. 2022;13:812926. doi: 10.3389/fpsyg.2022.812926
- Lederman E. Fundamentals of manual therapy: physiology, neurology and psychology. London, UK: Churchill Livingstone; 1997.
- Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001;28(2):431–438.
- Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19. doi: 10.1016/j.pain.2004.09.012
- Nabhan M, Elraiyah T, Brown DR, et al. What is preventable harm in healthcare? A systematic review of definitions. BMC Health Serv Res. 2012;12:128. doi: 10.1186/1472-6963-12-128
- Woolf S, Schunemann HJ, Eccles MP, et al. Developing clinical practice guidelines: types of evidence and outcomes; values and economics, synthesis, grading, and presentation and deriving recommendations. Implement Sci. 2012;7(1):61. doi: 10.1186/1748-5908-7-61
- Leysen P, Bombeke K, Remmen R. Osteopathic manual treatment and ultrasound therapy for chronic low back pain: an illustration of osteopathic semantic confusion. J Am Osteopath Assoc. 2013;113(9):660–661. doi: 10.7556/jaoa.2013.030
- de Vet HC, Heymans MW, Dunn KM, et al. Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine (Phila Pa 1976). 2002;27(21):2409–2416. doi: 10.1097/00007632-200211010-00016
- Stanton TR, Latimer J, Maher CG, et al. How do we define the condition ‘recurrent low back pain’? A systematic review. Eur Spine J. 2010;19(4):533–539. doi: 10.1007/s00586-009-1214-3