Abstract
Objective: Context/Objective: Family physicians may lack the knowledge or resources to adequately support patients with spinal cord injury (SCI). Our objectives were to determine patterns of preventive care for patients with SCI in a primary care setting (i.e. cancer screening, influenza vaccinations, general physicals, bone mineral density tests), and determine physicians’ level of comfort with providing primary care to patients with SCI.
Design: i) Retrospective chart review, ii) Survey of physicians in the family practice.
Setting: Six primary care practice sites in Ontario, Canada.
Participants: All adult rostered patients of the family practice with SCI; All family physicians in the six sites.
Outcome Measures: Proportion of patients up-to-date on cancer screening, proportion of patients with influenza vaccinations, general physicals, bone mineral density tests; physicians’ level of comfort with providing care to patients with SCI.
Results: Sixty patients were included in analyses. Rates of cancer screening were generally poor. The highest uptake was seen for cervical cancer screening, where 50% of eligible women were up-to-date on Pap tests. Only 36.7% of patients were up-to-date on colorectal cancer screening. Only 14 (23.3%) patients had a documented general physical exam in their electronic record. There was a recorded flu vaccination for 55% of patients, and of those, there was a median of 19 months since last vaccination. Fifteen physicians (21.4%) responded to the survey. Ten physicians reported at least one patient with SCI, with the maximum being 20 patients. Comfort level in managing SCI-relevant conditions varied and was lowest for spasticity, respiratory issues and autonomic dysreflexia, where only 27.3% of respondents had some level of comfort.
Conclusion There are many opportunities to improve the preventive care of patients living with SCI.
Context/objectives
The literature suggests that individuals living with mobility issues and physical disabilities face significant challenges accessing quality primary and preventive care in Canada.Citation1,Citation2 A recent survey at a primary care practice found that patients with mobility issues were more likely to use the emergency room than their peers and were more likely to report their health status as fair or poor.Citation3 Furthermore, they were more likely to be living with a low income, which is itself associated with less preventive care.Citation3–7 A spinal cord injury (SCI) may be the prototypical example of disability, and people living with SCI often have secondary complications, multiple co-morbidities and significant lifelong impairments.Citation8 Persons with SCI may be particularly vulnerable to the gaps in care experienced by people with disability and mobility issues. The literature suggests that people with SCI face difficulties in accessing primary care due to inadequate examination tables, transportation barriers, inadequate office space to accommodate mobility devices, physical barriers such as stairs, and availability of mechanical lifts for transfers.Citation9–13 In a recent Canadian study, family physicians reported that quality of care for patients with SCI can be affected by lack of appropriate medical equipment, and that there is often a focus on acute rather than preventive care.Citation11 Patients with SCI may even be sent to the emergency room for routine care, solely due to access issues.Citation14 Perhaps not surprisingly, Guilcher et al. found high rates of emergency department use for both low acuity and potentially preventable conditions among people with traumatic SCI, with 50% of emergency room visits falling into these two categories.Citation15 Provider knowledge gaps and attitudinal biases may also be barriers to quality care for patients with SCI.Citation11
Relatively little information exists on patients living with SCI in the context of Canadian primary care, particularly from the perspective of primary care providers. Persons with SCI constitute a small vulnerable population where issues of accessibility and equity in primary care can be highlighted. More literature is needed describing the healthcare needs of these patients and the perspectives of their physicians to ensure patients with SCI receive accessible, timely, equitable, high-quality preventive care.
Screening for breast, cervical and colorectal cancers is an evidence-based approach to reducing cancer incidence, morbidity and mortality,Citation16 and is a core component of primary and preventive care. Population-based studies in Ontario, Canada’s most populous province with nearly 14 million people, have shown that women with severe disability are less likely to be screened for breast and cervical cancer, especially as their level of co-morbidity increases.Citation6,Citation7 Vaccination against infectious diseases such as influenza is another hallmark of preventive care and the Ontario Ministry of Health and Long-Term Care recommends annual influenza vaccine for all, with individuals with neurologic or neurodevelopmental conditions being considered high risk.Citation17 Bone mineral density (BMD) tests screen for osteoporosis and people with SCI have a higher incidence of fragility fractures due to excessive loss of bone mass, and are also at risk for sublesional osteoporosis.Citation18 Therefore, the objectives of this exploratory study were to: i) determine the proportion of patients living with SCI who were up-to-date on routine cancer screening in a primary care setting, ii) describe other patterns of preventive care for these patients (i.e. influenza vaccinations, general physicals, BMD tests), and iii) determine physicians’ level of comfort with providing primary care to patients with SCI.
Design
The study had two components: i) a retrospective chart review and ii) a survey sent out to all physicians in the family practice. The study was approved by the Research Ethics Board of St. Michael’s Hospital.
Setting
This study was based within six practice sites that together form a large multidisciplinary Family Health Team in Ontario, Canada with approximately seventy physicians and numerous other health professionals serving over 35,000 enrolled patients. The practice locations are all in relatively close proximity to a large tertiary care hospital, and all use an electronic medical record (EMR) since February 2011. Quality improvement efforts within the Family Health Team have included a focus on increasing cancer screening uptake for patients. As of June 30, 2016, cancer screening uptake for the team of practices were 71% for cervical, 65% for breast, and 70% for colorectal cancer (CRC) screening.
Participants
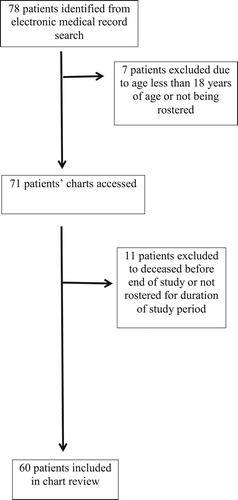
Retrospective chart review
All rostered patients of the family practice aged 18 years and over with SCI and who were alive for all of June 1, 2015 – May 31, 2016 were eligible for inclusion in this retrospective analysis. Patients who are rostered are those who have formally enrolled themselves with their family physician. To determine eligibility, we searched the EMR for any rostered patients with the following terms in their Cumulative Patient Profile (CPP): “spinal cord”, “spinal cord injury”, “paraplegia/ paraplegic”, “quadriplegia/quadriplegic”, “tetraplegia/tetraplegic” and “SCI”. This EMR search was previously validated (by two of the co-authors) against a patient roster at the Centre for Family Medicine, another academic Family Health Team located in Ontario, Canada, which runs a primary care Mobility Clinic that serves patients with SCI. A manual review of the identified charts was then performed to confirm if patients had an SCI. Only those patients with a confirmed SCI on manual chart review were included in the study. Patients who were less than 18 years of age, who were not rostered for the entire study period, and who died before the end of the study period were excluded.
Physician survey
All 70 family physicians in the six sites were eligible for participation in the survey. Physicians were invited to participate in an electronic anonymous survey housed on the FluidSurveysTM website, and an email reminder was sent out two weeks after the initial invitation. We approximated that the survey would take 10-15 minutes to complete.
Outcome measures
Retrospective chart review
The following data were collected from the charts of study participants: age, sex, number of family physician visits in the preceding year, and number of visits to other health professionals in the practice in the preceding year. We also documented the dates of the last Pap test (for women aged 21–69 years), last mammogram (for women aged 50–74 years), last fecal occult blood test (for individuals aged 50–74 years), last colonoscopy (for individuals aged 50–74 years), last general physical exam, last influenza vaccination, and last BMD test, as well as the number of medications. All data extracted were as of May 31, 2016.
We defined eligibility and up-to-date status for cancer screening based on provincial guidelines for “average risk” screening. Current Ontario cancer screening guidelines recommend that women who have ever been sexually active and are over the age of 21 years should have a Pap test once every three years until they reach 70 years.Citation16 They also recommend that women aged 50 to 74 years should have a mammogram every two years for breast cancer screening, and that adults aged 50 to 74 years should have a fecal occult blood test (FOBT) every two years for CRC screening.Citation16 Individuals who have had a normal colonoscopy in the preceding ten years are also considered up-to-date on CRC screening.Citation19
For influenza vaccination, BMD testing and general physical exam, we did not define up-to-date status as guidelines are not as straightforward. Instead, we calculated the number and percentage of patients with a test on record, and the number of months since the last test.
Physician survey
The survey consisted of demographic questions (i.e. age, sex, years in practice, number of patients) questions on comfort with managing care for patients with SCI, and questions on collaborating with specialists for patients with SCI.
Data analysis
We conducted descriptive analyses to characterize the patient and physician participants. Research policies at the study practice sites require that any individual cells in a table with a numerical value less than 5 cannot be reported to reduce the risk of identifying participants. As such, all cell sizes less than 5 were suppressed. All statistical analyses were conducted using SPSS 20.0.
Results
Retrospective chart review
There were 78 patients identified from the initial EMR search as potentially living with SCI. After exclusion criteria were applied, a total of 60 patients were included in analyses (). There were no participants identified from the search that did not have an SCI. Participants ranged in age from 26 to 94 years of age, with an average age of almost 54 years (). The number of visits to the family practice varied widely (range 0–35 visits, median 3, mean 5.4), as did the number of medications listed in the chart, with a median of 6 medications and a range of 0 to 20 medications. The majority (63.3%) of patients were male.
Table 1 Demographic and healthcare utilization characteristics of the 60 patients with spinal cord injury in the study sample.
Rates of cancer screening were generally poor among patients with SCI. The highest uptake was seen for cervical cancer screening, where 50% of eligible women with SCI were up-to-date on Pap tests. Only 36.7% of patients were up-to-date on CRC screening. Only 14 (23.3%) patients had a documented general physical exam in their electronic record and only 40% had a BMD test recorded. Flu vaccination was on record for 55% of patients; among those who did have a recorded vaccination, there had been a median of 19 months since the last vaccination.
Physician survey
There were 15 physicians who responded to the survey (21.4% response rate), 7 of whom reported being female. The median number of patients in their practices was 650. Ten physicians reported that they had at least one patient with SCI, with the maximum number of patients with SCI being 20. Seven of these physicians reported that their patients were co-managed by specialists. Of those physicians who reported having female patients with SCI eligible for cervical cancer screening, 60% reported performing these patients’ Pap tests themselves.
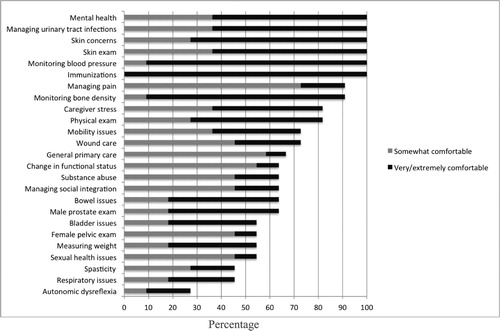
Comfort level in managing conditions in patients with SCI varied (). All respondents reported some level of comfort with mental health, urinary tract infections, skin concerns, providing immunizations and monitoring blood pressure. However, comfort levels were lowest for managing spasticity, respiratory issues and autonomic dysreflexia, where only 27.3% of respondents had some level of comfort.
Figure 2 Responses of the 15 physicians who participated in the online study survey regarding comfort with medical conditions or procedures for patients with spinal cord injury.
Note: Percentages represent those who reported being extremely/very or somewhat comfortable, where the denominator is those who answered the question. No question was answered by less than 11 physicians.
Discussion
In this multi-method study performed within a multi-site Family Health Team, we have found that there are many opportunities to improve the preventive care of patients living with SCI. Patients with SCI had low cancer screening rates, with CRC rates being the lowest at 36.7%, and with rates much lower than in the practices as a whole (e.g. CRC screening at 70% for general patients within practice sites). Many patients had no record of a flu shot. Physicians tended to have few patients with SCI, with the median among survey respondents being one patient. Most physician respondents co-managed care with specialists, and although comfort was high with managing some conditions for patients with SCI, there were opportunities for improving comfort in spasticity, respiratory issues and autonomic dysreflexia.
Interestingly, all physicians in the sample felt comfortable managing blood pressure of patients with SCI but most were not comfortable managing autonomic dysreflexia. Autonomic dysreflexia is a common and serious condition that can occur in patients with an SCI at the T6 level or higher, yet many primary care physicians have never heard of the condition.Citation20,Citation21 Briefly, the condition is triggered by a noxious stimulus below the level of the lesion, usually bladder or bowel irritation, which then leads to activation of sympathetic nerves below the level of injury and parasympathetic input above the level of injury. Sympathetic activation results in massive vasoconstriction and an increase in blood pressure. Signs and symptoms of autonomic dysreflexia include elevated blood pressure and may include headache, dyspnea, flushing, and sweating. Treatment involves removing the noxious stimulus and may involve acute lowering of blood pressure. Consequences can be serious, including seizure, stroke and death.Citation20,Citation21 It is possible that more education to primary care providers treating patients with SCI about this serious and potentially life-threatening emergency could increase their comfort level.
Although our results suggest many opportunities for educating physicians on the needs of patients with SCI, including autonomic dysreflexia, the fact remains that SCI is not a common condition in medical practice.Citation20 This is reflected in our study findings where only 60 of 35,000 patients were identified as having an SCI in the EMR. This relative rarity likely hinders family physicians’ ability to develop knowledge, expertise and self-efficacy in providing primary care for persons with SCI. Not surprisingly, people living with disabilities have reported that it is rare to find primary care providers with knowledge in enough areas to provide them with high quality primary care.Citation22 In a recent scoping review, McColl et al. found that information needs for patients with SCI are often poorly met in primary care.Citation2 Many of the providers in our urban sample reported co-managing patients with specialists, and ideally patients would be co-managed with a physiatrist with expertise in SCI, but for primary care providers who do not have good access to such specialists, perhaps online resources or timely communication access to experts (e.g. enabled via technology) could help to improve care. Two good examples of online resources are those found at https://scireproject.com (the Spinal Cord Injury Research Evidence Project) and at http://www.pva.org/publications/clinical-practice-guidelines (Paralyzed Veterans of America). The former compiles relevant literature relevant to SCI rehabilitation and concisely summarizes it for health professionals and the latter includes evidence-based clinical practice guidelines for patients with SCI.
Regardless of specific expertise in SCI, we also observed opportunities to improve basic preventive care, such as cancer screening, flu shot uptake, and BMD test training. These preventive actions are well within the realm of primary care, as opposed to specialist care. Interestingly, the highest cancer screening uptake was seen for cervical cancer screening, which can often be quite cumbersome due to the requirements for the patient transfer, positioning, and need for appropriate accessible equipment. The involved practices are affiliated with a large hospital and have good access to gynaecology services, so this may have influenced screening rates. However, opportunities exist to continue to increase Pap test use, in line with previous literature,Citation23 and perhaps to work with local mammography sites to better accommodate patients with SCI. As well, how to best facilitate CRC screening for patients with SCI needs to be urgently explored, as rates were particularly low for both colonoscopy and FOBT use. Colonoscopies present unique challenges for patients with SCI, as the bowel preparation for colonoscopies requires frequent transfers, necessitates close attention to avoid skin-related complications, and can be a trigger for autonomic dysreflexia.Citation24 Adequate bowel cleansing presents another obstacle in the setting of neurogenic bowel. This limits diagnostic yield of the screening colonoscopy. However, rates were still low for FOBT use, which are more feasible for patients with SCI to complete. Patients averaged more than five visits for the 1-year study period, suggesting that there are ample opportunities to broach prevention for those living with SCI.
The Ontario Ministry of Health and Long-Term Care recommends annual influenza vaccine for all, including high-risk individuals with neurologic or neurodevelopmental conditions,Citation17 yet only 55% of patients had a flu shot on record, and for those who did, the median time since the last vaccination was 19 months. Increasing influenza uptake in this population seems like an initiative that would be relatively easy to undertake with high potential gains, particularly as all respondents reported comfort with providing immunizations.
Only 40% of patients had a BMD test on record, and there had been a median of 4 years since the last test. However, measuring and monitoring of bone density are considered essential in this patient population to detect both osteoporosis and sublesional osteoporosis.Citation18 Uncertainty with BMD testing is understandable as many individuals will be young and not fall into the general population guidelines. Again, comfort among physicians was quite high for monitoring bone density so increasing monitoring seems like an achievable goal with provider education.
We looked at the rate of performing a general physical examination as there is support in the literature for regular comprehensive examinations in SCI and other disabilities due to the chronic complexity and unmet needs.Citation2 The annual physical examination of asymptomatic patients in primary care has been a topic of much debate and has been found to be resource intensive and likely not of health benefit. Instead there has been a shift to utilizing focused periodic preventative health visits.Citation25 The rate of general physical examination in our study was low (23%), which may reflect whether it could accurately be searched in the EMR (how it was recorded or defined), or may reflect physicians adopting an approach more towards focused periodic preventative health visits and differences in ages and risks of the patients. In patients that have increased complexity, it is unclear if a general assessment or focused health visits or combination of both might be beneficial.
The retrospective chart review had several limitations, largely influenced by the fact that we were only able to track what was documented in patient charts. First, patients may have obtained their screening tests through specialists or other health professionals. For example, patients may have received flu shots at their local pharmacies, or specialists may have performed cancer screening or other preventive tests and not provided this information back to the primary care provider. Ideally, this information would have been recorded in the chart even if performed outside of the clinic but this is not always the case. Second, the reasons why the tests were not done are not available. Patients may have been offered the test and made an informed decision to decline, or the patient and provider may have mutually decided the test was inappropriate (e.g. for the Pap test, if a patient had never been sexually active). Third, the electronic charts only go back to 2011 so we were not able to track any tests or procedures prior to that date. Fourth, although the search for SCI has been validated, there can be complete lack of recording of SCI in some charts so it is possible we missed some patients. Fifth, this study examined rostered patients within the practices and it is possible that some patients with SCI were not rostered. Finally, we had no information on level or completeness of SCI, which could potentially affect accessibility, as well as selection of individual for tests (e.g. one might not order a BMD for an ambulatory SCI patient). Our physician survey also had limitations. First, we had a low response rate, with only 21.4% of physicians participating in the survey. We cannot know the reason for the low response rate but speculate that if physicians knew little about the content area or had no patients with SCI, they would be less likely to participate. Second, as noted above, comfort level does not equate with knowledge of the best evidence or with acting on best evidence. Physicians may have been comfortable treating some conditions for their patients with SCI, but this does not mean that they were aware of the best recommendations or nuances specific to the SCI population.
Conclusions
Although SCI is a condition of relatively low prevalence in primary care, individuals living with this condition are a vulnerable group who are in need of, and have the right to, quality primary and preventive care. Numerous opportunities exist to improve care for this patient group, particularly as they have higher health needs than many others. Future research should explore how primary care providers could be best supported to provide care for these patients and other patients with physical disabilities.
Disclaimer statements
Contributors None.
Conflicts of interest The authors have no conflicts of interest to declare.
Ethics approval None.
Disclosures None.
Funding This study was funded by a research grant from the Centre for Family Medicine and the Ontario Neuro-trauma Foundation. Dr. Lofters is supported by a Canadian Institutes for Health Research (CIHR) New Investigator Award, and as a Clinician Scientist by the University of Toronto Department of Family and Community Medicine. Dr. Guilcher is supported by a CIHR Embedded Clinician Scientist Award.
ORCID
Aisha Lofters http://orcid.org/0000-0002-7322-0894
Maha Chaudhry http://orcid.org/0000-0001-5382-8280
References
- McColl MA, Aiken A, Schaub M. Do people with disabilities have difficulty finding a family physician? Int J Environ Res Public Health 2015;12(5):4638–51. doi: 10.3390/ijerph120504638
- McColl MA, Aiken A, McColl A, Sakakibara B, Smith K. Primary care of people with spinal cord injury: scoping review. Can Fam Physician 2012;58(11):1207–16, e626–35.
- Lofters A, Guilcher S, Maulkhan N, Milligan J, Lee J. Patients living with disabilities: The need for quality primary care. CFP 2016; 62 (8): e457–e464.
- Vahabi M, Lofters A, Kumar M, Glazier RH. Breast cancer screening disparities among immigrant women by world region of origin: a population-based study in Ontario, Canada. Cancer Med 2016. DOI: 10.1002/cam4.700.
- Fernandes KA, Sutradhar R, Borkhoff CM, Baxter N, Lofters A, Rabeneck L, et al. Small-area variation in screening for cancer, glucose and cholesterol in Ontario: a cross-sectional study. CMAJ Open 2015;3(4):E373–81. doi: 10.9778/cmajo.20140069
- Lofters A, Guilcher S, Glazier RH, Jaglal S, Voth J, Bayoumi AM. Screening for cervical cancer in women with disability and multimorbidity: a retrospective cohort study in Ontario, Canada. CMAJ Open 2014;2(4):E240–7. doi: 10.9778/cmajo.20140003
- Guilcher SJ, Lofters A, Glazier RH, Jaglal SB, Voth J, Bayoumi AM. Level of disability, multi-morbidity and breast cancer screening: does severity matter? Prev Med 2014;67:193–8. doi: 10.1016/j.ypmed.2014.07.025
- Guilcher SJ, Parsons D, Craven BC, Jaglal SB, Verrier M. Developing quality of care indicators for patients with traumatic and non-traumatic spinal cord injury (SCI): A feasibility study using administrative health data. J Spinal Cord Med 2015;38(6):765–76. doi: 10.1179/2045772315Y.0000000043
- Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord 2010;48(1):45–50. doi: 10.1038/sc.2009.78
- Hwang K, Johnston M, Tulsky D, Wood K, Dyson-Hudson T, Komaroff E. Access and coordination of health care service for people with disabilities. J Disabil Policy 2009;20(1):28–34. doi: 10.1177/1044207308315564
- McMillan C, Lee J, Milligan J, Hillier LM, Bauman C. Physician perspectives on care of individuals with severe mobility impairments in primary care in Southwestern Ontario, Canada. Health & social care in the community 2016;24(4):463–72. doi: 10.1111/hsc.12228
- Kroll T, Jones GC, Kehn M, Neri MT. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: a qualitative inquiry. Health & social care in the community 2006;14(4):284–93. doi: 10.1111/j.1365-2524.2006.00613.x
- Veltman A, Stewart DE, Tardif GS, Branigan M. Perceptions of primary healthcare services among people with physical disabilities - Part 1: Access issues. Medscape Gen Med 2001;3(2):18.
- Milligan J, Lee J. Enhancing primary care for persons with spinal cord injury: More than improving physical accessibility. J Spinal Cord Med 2016;39(5):496–9. doi: 10.1179/2045772315Y.0000000041
- Guilcher SJ, Craven BC, Calzavara A, McColl MA, Jaglal SB. Is the emergency department an appropriate substitute for primary care for persons with traumatic spinal cord injury? Spinal Cord 2013;51(3):202–8. doi: 10.1038/sc.2012.123
- CancerCareOntario. Screening - CCO [Available from: https://http://www.cancercare.on.ca/pcs/screening/.
- Universal Influenza Immunization Program: Ministry of Health and Long-Term Care; [Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/flu/uiip/.
- Craven C, Lynch C, Eng J. Bone Health Following Spinal Cord Injury. In: Eng J, Teasell R, Miller W, Wolfe D, Townson A, Hsieh J, et al., editors. Spinal Cord Injury Rehabilitation Evidence Version 50. Vancouver 2014. p. 1–37.
- Cervical Cancer Screening: Cancer Care Ontario; [February 9, 2016]. Available from: https://http://www.cancercare.on.ca/pcs/screening/cervscreening/.
- Milligan J, Lee J, McMillan C, Klassen H. Autonomic dysreflexia: recognizing a common serious condition in patients with spinal cord injury. Can Fam Physician 2012;58(8):831–5.
- Krassioukov A, Warburton DE, Teasell R, Eng JJ, Team SCIRER. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil 2009;90(4):682–95. doi: 10.1016/j.apmr.2008.10.017
- Bowers B, Edmond S, Lutz B, Jacobson N. Improving primary care for persons with disabilities: the nature of expertise. Disabil Soc 2003;18(4):443–55. doi: 10.1080/0968759032000080995
- Guilcher SJT, Newman A, Jaglal SB. A comparison of cervical cancer screening rates among women with traumatic spinal cord injury and the general population. Journal of Women's Health 2010;19(1):57–63. doi: 10.1089/jwh.2008.1319
- Song SH, Svircev JN, Teng BJ, Dominitz JA, Burns SP. A safe and effective multi-day colonoscopy bowel preparation for individuals with spinal cord injuries. J Spinal Cord Med 2017:1–8.
- Birtwhistle R, Bell NR, Thombs BD, Grad R, Dickinson JA. Periodic preventive health visits: a more appropriate approach to develivering preventive services. CFP 2017; 63: 824–6.