Abstract
Objective: This paper reports the iterative redesign, feasibility and usability of the Comprehensive Mobile Assessment of Pressure (CMAP) system’s mobile app used by Veterans with SCI.
Design: This three-year, multi-staged study used a mixed-methods approach.
Setting: Minneapolis VA Health Care System, Minneapolis, Minnesota.
Participants: Veterans with spinal cord injury (N = 18).
Interventions: Veterans with spinal cord injury engaged in iterative focus groups and personal interviews, sharing their needs and desires for the CMAP app redesign. App developers used these data for the redesign. The redesigned CMAP app was tested for six-weeks in users’ homes.
Outcome Measures: Quantitative (surveys) and qualitative (interviews) methods measured feasibility for self-management of seating pressure. Qualitative data were audio recorded, transcribed, anonymized, and coded. Survey data were analyzed using summary statistics.
Results: After the CMAP system’s redesign, the in-home use interview found: (1) any tool that can assist in prevention and monitoring of skin ulcers is important; (2) the desired key features are present in the app; (3) the main barrier to CMAP use was inconsistent functionality; (4) when functioning as expected, the live pressure map was the central feature, with reminders to weight shift also of high importance. The survey found: power wheelchair users tended to score closer than manual wheelchair users to the positive response end ranges on two separate surveys.
Conclusions: Overall both the power and manual wheelchair users reported that they wanted to use the system, felt confident using the system, and that the functions of the system were well integrated.
Introduction
Spinal cord injuries (SCIs) among soldiers of the United States of America increased to 11% of combat wounds during the wars in Iraq and Afghanistan compared to 1–2% during previous military actions.Citation1 Further, the Veterans Affairs Health Care System treats more than 27,000 Veterans with SCI and related injuries annually.Citation2 Spinal trauma may require the use of a manual or motorized wheelchair for mobility. Use of a wheelchair imposes an almost permanent seated position on the person and creates a daily threat of acquiring a life-threatening sitting-related pressure injury.
Sitting-related pressure injuries result from damage to tissue to the sacral, ischial and sacrococcygeal areas. Risks for injury include but are not limited to pressure, shear, friction, moisture, poor nutrition, immobility, and lack of adherence to acknowledged preventative behaviors.Citation3,Citation4 In the US, 25% of adults with paralysis will have one or more pressure injuries at any given time.Citation5–8 Pressure injuries are a primary reason (secondary only to diseases of the genitourinary system) for hospital readmission for those with a SCI across all time periods (1–20 years post SCI).Citation9,Citation10 With pressure injury recurrence rates as high as 79%Citation11,Citation12 there exists a critical clinical need to target prevention of pressure injury development to avert serious complications and death.Citation13,Citation14
Education is a key component for the prevention of sitting-related pressure injury development.Citation15,Citation16 However, retention of the education provided during their inpatient rehabilitation is a mere 50% after 30 months, contributing to suboptimal adherence to prevention recommendations.Citation15 Even with careful adherence to skin health recommendations and education, pressure injuries still occur from seat cushion failures, inadequate equipment, and poor positioning strategies.Citation17,Citation18 Appropriately fitted equipment and user positioning in a wheelchair can be effectively determined in the rehabilitation clinic using seat interface pressure mapping,Citation19–21 but translation of that information to users’ daily routine is often unsuccessful. Furthermore, routine clinic visits for equipment replacement occur annually or every few years, allowing serious problems with equipment fit to go undetected between those visits.
Our team developed a prototype pressure mapping system for personal daily use to address the more common contributors to pressure injury: infrequent pressure reliefs, undetected cushion failures; incorrect seat positioning by the wheelchair user and their caregivers. The prototype of the Comprehensive Mobile Assessment of Pressure (CMAP) system includes a Bluetooth-enabled pressure mat that sits atop the user’s wheelchair cushion and communicates real-time pressure map images to a personal smartphone via a mobile application.
An important consideration for successful use of any new assistive technology is the principle of technology abandonment.Citation22 The top factors of technology abandonment are (1) poor device performance, (2) the lack of consideration of user opinion in selection, and (3) changes in user needs or priorities.Citation22 To move the prototype CMAP system forward, the next step was to assess and address these technology abandonment factors. In this current study, we prioritized abandonment factors of user opinions (factor #2) and changes in user needs or priorities (factor #3) to improve the CMAP system’s mobile application.
The objectives of the overall project were to work collaboratively with the targeted end-users, the Veteran with SCI at risk for pressure injury, to: (1) determine the preferred features for redesign of the initial CMAP prototype along with usability of the redesigned app; and (2) determine feasibility and usability of the redesigned system during personal use in the field.
The primary purpose of this paper is to report on the iterative redesign, feasibility and usability of the Comprehensive Mobile Assessment of Pressure (CMAP) system’s mobile app used by Veterans with SCI in their natural environment for six weeks. We hypothesized that by engaging the future user in the design, we could potentially offset the second and third technology abandonment issues.
Methods
This study was funded by the Department of Defense, number W81XWH-15-1-0484, and was conducted at the Minneapolis VA Health Care System (MVAHCS), Minneapolis, Minnesota. The study was approved by the MVAHCS Institution Review Board and the Research and Development Committee, and the US Army Medical Research and Materiel Command, Human Research Protection Office prior to study initiation. All participants signed the approved consent.
Study design
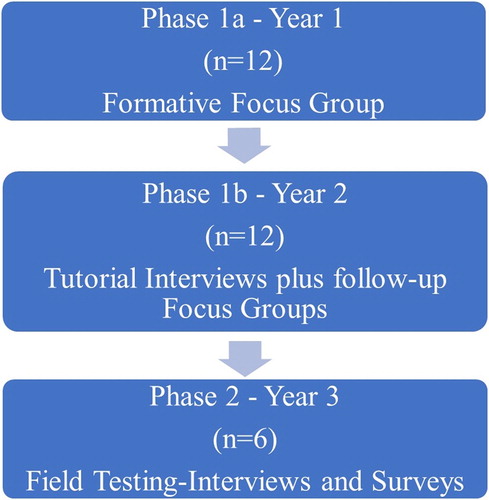
The three-year study was multi-staged and used a mixed methods approach governed by an experience-based design methodology.Citation23 See for study design overview.
The CMAP system
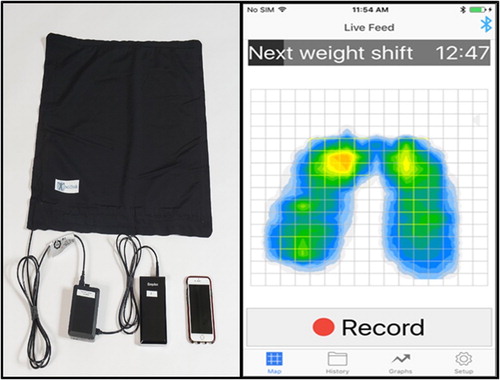
The Comprehensive Mobile Assessment of Pressure (CMAP) system consists of: (1) a pressure mat consisting of a 22 × 22 inch sensor array (BodiTrack Seat System, http://www.vista-medical.com/subsite/stretchseat.php, Vista Medical, Winnipeg, Manitoba) that is commercially available, met basic criteria for longer term useCitation24 and designed for detecting seated pressures in wheelchair users, (2) a portable power bank by Anker (https://www.anker.com/), (3) a mobile app on an iOS mobile phone, and (4) a Raspberry Pi (https://www.raspberrypi.org/) minicomputer coded for pulling pressure data from the pressure mat to the mobile app by a USB cable (for the testing in the MVAHCS) or wireless via Bluetooth (for the at-home testing). See .
Protocol
Veterans from the MVAHCS Spinal Cord Injury and Disorders Center were recruited to participate. See Supplemental Information for Recruitment details. The study consisted of two phases. Phase 1a and 1b were conducted within the Center setting. Phase 2 was conducted in the participant’s home. See Supplemental Information for details of protocol.
Outcome Measures
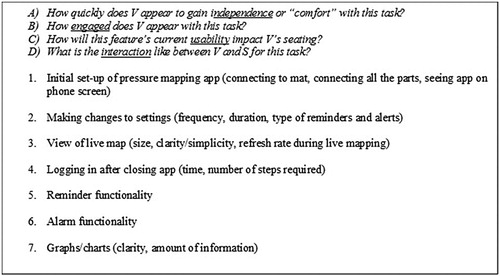
Focus groups and interviews: The Phase 1 focus group semi-structured moderator guide () was developed using the prevailing principles outlined by Krueger and Casey.Citation25 The Phase 1 focus groups and interviews as well as Phase 2 in-home interviews were all shaped by experience-based design methodology.Citation23 See : Overview guides for observation, feasibility, usability and follow-up interviews.
Table 1 Phase 1: Focus group guide.
System Usability Scale (SUS)
The SUS (Digital Equipment Co Ltd., Reading, United Kingdom) is a simple, ten-item scale, completed by the CMAP user to give an overall view of the user’s assessment of usability and learnability.Citation26 Ten statements are presented to the user who selects a response on a scale of 1 (strongly disagree) to 5 (strongly agree). See the Supplemental Information for details on the SUS.
User Experience Questionnaire (UEQ)
The UEQ contains 26 pairs of semantic differential items on six scales: attractiveness, perspicuity, efficiency, dependability, stimulation, and novelty.Citation27 The attractiveness scale contains subjective item relating to general appeal. The items in the perspicuity, efficiency, and dependability scales of the UEQ describe ease of learning and understanding, effort required, and amount of user control, while the remaining scales (stimulation and novelty) are concerned with motivation and interest of the user. See the Supplemental Information for details on the UEQ.
Analysis
Qualitative data analysis
Qualitative data collection and analysis were guided by the experience-based design methodology, where technical experts and end-users iteratively collaborate to optimize the function, fit and feel of health technology. All tutorials, interviews and focus groups were audio recorded, transcribed and anonymized. Transcripts and fieldnotes were entered into specialized qualitative software (NVivo12, QRS International, 2018) for data management and analyzed using the framework method.Citation28 Following the framework method our qualitative researchers (J.E.+ K.C.) categorized and coded transcripts and fieldnotes to develop common themes, then interpreting the coded data in conjunction with the multidisciplinary team.
Quantitative data analysis
Summary statistics were calculated for the survey data. The SUS survey data were analyzed by calculating overall scores for each participant as follows: subtract 1 from odd numbered items and subtract 5 from even numbered items, resulting in 10 scores that range from 0 to 4. These scores were summed and then multiplied by 2.5 to obtain a total usability score. A usability score of 68 is average. The UEQ survey data were analyzed using the UEQ Data Analysis Tool (http://www.ueq-online.org/). Scores were entered into the Excel-based tool for calculation of the scale mean and standard deviation per item, with confidence intervals for the scale means and mean of each item.
Results
Demographics
Twelve male Veterans with SCI participated in Phase 1a and 1b (), with slight imbalance in representation in injury level (paraplegia vs tetraplegia) and wheelchair type (manual, power, or both). The distinct set of six Veterans with SCI participating in Phase 2 were on average slightly older, but had equally distributed injury level and wheelchair type ().
Table 2 Phase 1a and 1b: Participants’ demographics (focus group and interviews).
Table 3 Phase 2: Participants’ demographics (six weeks field testing).
Qualitative research results
Formative Focus Groups (Phase 1a): The two focus groups conducted with Veterans in July of 2016 yielded important direction for the multidisciplinary team. Namely, five key themes emerged from the semi-structured discussion:
Veteran users confirmed that skin ulcer prevention is important and expressed their interest in its prevention through pressure reliefs and reminders.
Veteran users’ desired CMAP to be simple to use, especially because some users may have limited experience with Smartphones. Veterans welcomed app customization to the extent that it not make things more complex.
Veterans’ desired a more integrated system where the many components of the technology integrate and work reliably.
Veteran users viewed the real-time pressure mapping as the primary asset of the app as it could be seen and responded to almost-automatically.
Veteran users saw CMAP as a medical adjunct that their doctor/therapist would introduce to them and instruct them on. There were no major concerns about privacy or sharing any data that would be collected with their health care provider.
Table 4 Phase 1b: Participant feedback: topic and the protocol and design response.
Field Use Feasibility Interviews (Phase 2): Six in-home interviews took place in the winter of 2017–2018. While some topics of discussion were similar to findings from Phase 1, other themes emerged as participants used the app at home:
Skin ulcers are serious and unwelcome, so any tool that can assist in prevention and monitoring is key.
The desired key features are in the app, and unnecessary ones were minimal.
The main barrier to in-home use was the inconsistency of function due to many components requiring interconnectivity (wireless/Bluetooth connection, wires, batteries, app, cushion, mat).
When it worked, the live pressure map was seen as the central feature, with reminders to weight shift also of high importance.
Suggestions for dissemination of the technology.
Want to be able to use on other surfaces that put their skin at risk.
Survey results
System Usability Scale (SUS): The SUS scores for the six at-home pressure map users ranged from 47.5 to 100; Mean = 72.1, SD = 19.07 (). Items with the poorest scores reflected challenges users faced with the technology functioning consistently. For example, the lowest score overall was for Item 6, “I thought there was too much inconsistency in the system”. The highest scored response reflected users’ confidence using technology: Item 10 “I felt very confident using the system.”
Table 5 System Usability Scale (SUS)*
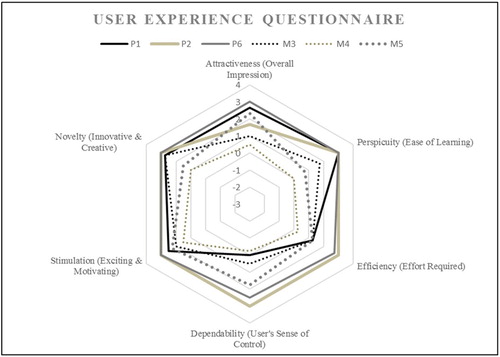
User Experience Questionnaire (UEQ): The mean UEQ scores for each of the 6 scales were all above 0.8 () indicating a positive experience. UEQ scores range from −3.0 to 3.0. Scores between −0.8 and 0.8 represent neutral responses. Scores above 0.8 indicate a positive response and those below −0.8 represent a negative response. “Dependability” was ranked as the lowest scale (M = 1.23, SD 1.088) and within that scale, Dependability was impacted greatest by the specific item for “Predictability”. Scale items “Novelty” (M = 2.33, SD = 0.86) and “Stimulation” (M = 2.79, SD = 1.14) were ranked the highest by the Veterans who used the CMAP system at home ().
Table 6 User Experience Questionnaire (UEQ): Scores, means, and standard deviations.
Skin Checks: By placing the pressure sensing mat between the seat cushion and the person, there is risk that the additional material could wrinkle or otherwise change the pressure-relieving properties of the cushion by reducing immersion or changing the microclimate. In this study, participants conducted daily self-examinations of their skin after sitting on the mat and no changes in skin integrity were reported.
Discussion
Pressure mapping performed in rehabilitation clinics can effectively determine appropriate seating equipment and positioning strategies for wheelchair users,Citation19–21 but translation of that same information integrated with a wheelchair user’s daily routine has not been previously addressed. The CMAP system is a seat interface pressure monitoring system that provides real-time imaging 24 h/day to the wheelchair users with SCI. This real-time biofeedback tool, compensating for absent or reduced sensation via visual images, may have the potential to prevent pressure injuries, facilitate potential remote monitoring of seating needs, and limit unnecessary medical visits.
The purpose of this study was to redesign the CMAP system’s mobile app, and iteratively test feasibility and usability of the system. Further, we specifically addressed two known factors for technology abandonmentCitation22 by (1) engaging the future user in the redesign and (2) implementing the future user’s opinions, needs, and priorities for the CMAP system. We utilized Krueger and Casey’s focus group methodsCitation25 during Phase 1a of the study to solicit Veteran users (n = 12) opinions about the CMAP system. Participants shared how important skin issues are to Veterans with SCI, that the Veteran user wanted a simple design with a more integrated system with quick access to their live pressure map. They also envision the CMAP system as a technology available to them through the VA HealthCare System. This information guided the CMAP initial redesign team’s actions, simplifying the app information available to the Veteran user and ensuring that the live pressure map was the first information to be viewed when the app was opened up. The follow-up interviews and focus groups in the usability study in Phase 1b revealed to researchers they were successful meeting many of the Veteran user requests. However, many priorities were identified by the participants for improvement prior to the field testing. The design was advanced through improved accessibility and user control of app alerts. Additionally, training and a user manual assisted in reducing the perceived complexity. During Phase 2 of the study, a distinct set of Veteran’s with SCI (n = 6) used the redesigned CMAP system in their home.
Phase 2 participants completed SUS and UEQ surveys after using the CMAP system in their homes for 4 weeks. Overall, results of the self-reported SUS and UEQ scales indicated the CMAP technology is innovative, useful and liked by the Veteran users. Specifically, there was strong agreement on the SUS () regarding confidence using the system and that the parts of the system were well integrated. This can be interpreted to mean the initial focus group requirements were met. On the UEQ survey, scales for stimulation and novelty scored high, which may reflect continued interest in this type of technology for managing pressure injury prevention, validated by data from the initial focus groups.
Pattern variations on both surveys, between power and manual wheelchair users are worthy of discussion. On the UEQ survey (), power wheelchair users tended to score closer to the positive response end ranges for each word choice whereas the manual wheelchair users tended to score more moderately between the two given words. This is similar to the pattern observed on SUS for both groups of wheelchair users. This may indicate that power wheelchair users are more inclined to use the CMAP system possibly because they have less control over body movement in comparison with manual wheelchair users who have more movement control. Also, on the UEQ survey, the power wheelchair users responded that the system was easy to use, that they would like to use it frequently, and that it would be simple to learn. This was surprising given they also had less finger/hand dexterity in some cases which made phone navigation more challenging. It would be expected the power wheelchair user would have less difficulty managing the actual mat positioning/smoothing because they used a lift system for transfers versus the manual wheelchair user who did self-transfers. Power wheelchair users also had caregivers available to facilitate equipment charging, cord management, and mat repositioning if needed. Further, power wheelchair users appear to adopt technologies to supplement their limitations and to enhance their daily living, compared to manual wheelchair users, who have fewer limitations. The manual wheelchair users reported the system was cumbersome to use possibly reflecting the movement of the mat on the cushion during their self-transfers and possibly self-management of the multiple parts and cords. These survey data were validated in the in-home interviews. Another interesting finding in the UEQ survey was the dependability scale, which was the lowest scored scale for both groups. These scores were validated during the in-home interviews with the users mentioning multiple times the difficulty with system’s hardware.
Some of the Veteran users had difficulties with the hardware management. This aspect was not part of this redesign study. The lowest scores on the surveys were on “inconsistency” (SUS) and “dependability” (UEQ) of the system. However, the average score in these domains remained favorable. The content of the weekly phone calls from Veteran users to the study nurse validated the SUS and UEQ findings, as the issues were primarily related to the hardware functionality of the CMAP system. Specifically, Veteran users identified inconsistency in connectivity between the pressure map and the app.
The Veteran participants had varying previous experiences with using technology. Further the average age of the first formative focus group was 61.5 years and the average age was even older (64.3 years) for the in-home users. Five out of the six Veteran user in-home participants had very little previous experience using a mobile app on a smart phone. Our surveys indicated that the participants found the CMAP useful. This positive attitude towards use of assistive technology in older adults is supported by Mitzner et al.Citation29 findings which disputed the stereotypes that older adults are afraid or unwilling to use assistive technology.Citation29 Pape et al.,Citation30 suggests that knowing the meaning and context of the assistive technology influences the users’ adoption of the device. Specifically, persons with acquired disabilities (SCI) need a sense of control when using the device.Citation30 Our findings, supported by the Tung et al.Citation31 review of literature,Citation31 suggest that the participants in this study, despite their older age and lack of previous exposure to the mobile apps, maintained a high level of interest in this assistive technology because it is intended to help manage their skin health, a very meaningful endeavor to them.
Limitations of the study deserve discussion. The small sample and older users does not represent all Veterans with SCI or the non-veteran with SCI. Further, the sample does not represent the sex of Veterans or non-veteran with SCI. Female Veterans with SCI represent 3% of the Veterans with SCI population.Citation32 Within the population of adults with SCI, about 22% of new injuries are women.Citation33 Results obtained from a convenience sample such as used in this study must be taken in context, and a larger study is indicated for future study to ensure the redesign iterations of the technology include the desired features and to allow successful transfer to other age groups, race and ethnic groups and women, who represent the SCI population. There was no comparison technology in this study design. That said, the Virtual Seating Coach (Permobil, Inc., Lebanon, TN) is a mobile app that provides feedback to a power wheelchair user on their use of the power seat functions of tilt and recline to perform pressure relieving weight shifts. The app is similar in that it provides cues and information about past behavior for self-tracking and differs in that it does not provide real-time visual feedback about the distribution of pressure between the user and their seat cushion, is not used on manual wheelchairs, and is designed to work with exclusively with one power wheelchair manufacturer. A comparable system may be challenging as the apps currently available are primarily aimed at helping healthcare providers manage existing pressure injuries, not the person with SCI. One system (SENSIMAT) provides basic weight shifting feedback through a mobile app, yet it is different from the CMAP in that it does not provide a continuous visual display of their body and the pressure map. This lack of available technologies for future comparison is clearly an indication need for the CMAP system.
Conclusion
The primary purpose of this paper was to report on the iterative redesign, feasibility and usability of the CMAP system’s mobile app according to the desires and priorities of Veterans with SCI. The multi-staged, mixed methods approach proved to be successful and informative for the app development. The iterative approach was crucial to the study completion and success in that it provided timely feedback for improvements to the mobile app and the interdisciplinary study team (qualitative experts, clinicians, and engineers). Despite minor to moderate challenges with the hardware and connectivity, overall both the power and manual wheelchair users reported that they wanted to use the system, felt confident using the system, and that the functions of the system were well integrated. Power wheelchair users reported in both the survey and qualitative results a higher interest in and satisfaction with the CMAP system compared to the manual wheelchair users. Power and manual wheelchair user responses on the user experience surveys and in the interviews suggested that they may use the system differently. Responses by power wheelchair users suggested a desire to use a pressure mapping system continuously, every day while manual wheelchair user response implied stronger motivation for using pressure mapping for spot checks of their seating system as well as testing pressure on different seating surfaces. Future development and testing will focus on understanding specific user needs; for example, between manual and power wheelchair users and addressing hardware challenges based on the specific feedback received from the Veteran users.
Abbreviations and symbols
| CMAP | = | Comprehensive Mobile Assessment of Pressure |
| MVAHCS | = | Minneapolis VA Health Care System |
| OT/AT | = | Occupational Therapist/Assistive Technology |
| PCP | = | Primary Care Provider |
| PVA | = | Paralyzed Veterans of America |
| SCI | = | Spinal Cord Injury |
| SCI/D | = | Spinal Cord Injury and Disorder |
| SUS | = | System Usability Scale |
| UEQ | = | User Experience Questionnaire |
Disclaimer statements
Contributors None.
Funding This study was funded by the Department of Defense, number W81XWH-15-1-0484.
Conflicts of interest Dr. Vos-Draper, Dr. Morrow and Mayo Clinic have a financial interest related to this research. This research has been reviewed by the University of Minnesota and Mayo Clinic Conflict of Interest Review Board and is being conducted in compliance with both policies. The materials presented here solely represent the views of the authors and does not represent the view of the U.S. Department of Veterans Affairs or the United States Government. The views expressed in the submitted article are the authors’ alone and not an official position of the institutions or funders.
Supplemental Material
Download MS Word (21.7 KB)Acknowledgments
This study was funded by the Department of Defense (W81XWH-15-1-0484). Additional support for XX was provided by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. This material is the result of work supported by and conducted at the Minneapolis VA Health Care System.
ORCID
Christine M. Olney http://orcid.org/0000-0003-3940-6107
Tamara Vos-Draper http://orcid.org/0000-0002-9038-2764
John Ferguson http://orcid.org/0000-0002-9944-1003
Katherine Carroll http://orcid.org/0000-0002-9110-1354
References
- Schoenfeld AJ, Laughlin MD, McCriskin BJ, Bader JO, Waterman BR, Belmont PJ. Jr. Spinal injuries in United States military personnel deployed to Iraq and Afghanistan: an epidemiological investigation involving 7877 combat casualties from 2005 to 2009. Spine 2013;38(20):1770–8. doi: 10.1097/BRS.0b013e31829ef226
- Spinal Cord Injury Fact Sheet. Found on-line on 7/9/2018. Available from https://www.research.va.gov/pubs/ docs/va_factsheets/sci.pdf.
- Garber SL, Rintala DH. Pressure ulcers in veterans with spinal cord injury: a retrospective study. J Rehab Res Dev 2003;40(5):433–42. doi: 10.1682/JRRD.2003.09.0433
- Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord 1996;34(5):255–63. doi: 10.1038/sc.1996.46
- Krause JS. Skin sores after spinal cord injury: relationship to life adjustment. Spinal Cord 1998;36(1):51–6. doi: 10.1038/sj.sc.3100528
- Raghavan P, Raza WA, Ahmed YS, Chamberlain MA. Prevalence of pressure sores in a community sample of spinal injury patients. Clin Rehabil 2003 Dec;17(8):879–84. doi: 10.1191/0269215503cr692oa
- National Spinal Cord Injury Statistical Center. 2016 Annual statistical report for the spinal cord injury model systems public version. Birmingham, Alabama: University of Alabama at Birmingham. [cited 2018 April]. Available from https://www.nscisc.uab.edu.
- Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993;74(11):1172–7.
- Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis1. Arch Phys Med Rehabil 2004;85(11):1757–63. doi: 10.1016/j.apmr.2004.03.016
- Gelis A, Dupeyron A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord 2009;47(9):651–61. doi: 10.1038/sc.2009.32
- Bates-Jensen BM, Guihan M, Garber SL, Chin AS, Burns SP. Characteristics of recurrent pressure ulcers in veterans with spinal cord injury. J Spinal Cord Med 2009;32(1):34–42. doi: 10.1080/10790268.2009.11760750
- Niazi ZB, Salzberg CA, Byrne DW, Viehbeck M. Recurrence of initial pressure ulcer in persons with spinal cord injuries. Adv Wound Care J Prev Healing. 1997;10(3):38–42.
- Staas WE, Jr. Cioschi HM. Pressure sores–a multifaceted approach to prevention and treatment. West J Med 1991;154(5):539.
- Thomas DR. Prevention and treatment of pressure ulcers: what works? What doesn’t? Cleve Clin J Med 2001;68(8):704–7. doi: 10.3949/ccjm.68.8.704
- Thietje R, Giese R, Pouw M, Kaphengst C, Hosman A, Kienast B, Van De Meent H, Hirschfeld S. How does knowledge about spinal cord injury-related complications develop in subjects with spinal cord injury? A descriptive analysis in 214 patients. Spinal Cord 2011;49(1):43–8. doi: 10.1038/sc.2010.96
- Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care proffessionals. J Spinal Cord Med 2001;24:S40–101. doi: 10.1080/10790268.2001.11753592
- Clark FA, Jackson JM, Scott MD, Carlson ME, Atkins MS, Uhles-Tanaka D, Rubayi S. Data-based models of how pressure ulcers develop in daily-living contexts of adults with spinal cord injury. Arch Phys Med Rehabil 2006;87(11):1516–25. doi: 10.1016/j.apmr.2006.08.329
- Dunn CA, Carlson M, Jackson JM, Clark FA. Response factors surrounding progression of pressure ulcers in community-residing adults with spinal cord injury. Am J Occup Ther 2009;63(3):301–9. doi: 10.5014/ajot.63.3.301
- Stinson MD, Porter-Armstrong AP, Eakin PA. Pressure mapping systems: reliability of pressure map interpretation. Clin Rehabil 2003 Aug;17(5):504–11. doi: 10.1191/0269215503cr643oa
- Crawford SA, Strain B, Gregg B, Walsh DM, Porter-Armstrong AP. An investigation of the impact of the force sensing array pressure mapping system on the clinical judgement of occupational therapists. Clin Rehabil 2005;19(2):224–31. doi: 10.1191/0269215505cr826oa
- Norman D. Measuring interface pressure: validity and reliability problems. J Wound Care 2004;13(2):78–80. doi: 10.12968/jowc.2004.13.2.26576
- Phillips B, Zhao H. Predictors of assistive technology abandonment. Assist Technol 1993;5(1):36–45. doi: 10.1080/10400435.1993.10132205
- Bate P, Robert G. Bringing user experience to healthcare improvement: the concepts, methods and practices of experience-based design. Abingdon, UK: Radcliffe Publishing; 2007.
- Vos-Draper T. Poster 29 wireless seat interface pressure mapping on a smartphone: feasibility study in users with SCI. Arch Phys Med Rehabil 2013;94(10):e21–2. doi: 10.1016/j.apmr.2013.08.075
- Krueger RA, Casey MA. Focus groups: a practical guide for applied research. Singapore: Sage publications; 2014 Jul 22.
- Brooke J. Sus: a retrospective. J Usability Stud 2013;8(2):29–40.
- Laugwitz, B., Schrepp, M. and Held, T. Construction and evaluation of a user experience questionnaire. In: Holzinger A, (ed.) USAB 2008, LNCS 5298, 63–76.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13(1):117. doi: 10.1186/1471-2288-13-117
- Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, Dijkstra K, Fisk AD, Rogers WA, Sharit J. Older adults talk technology: technology usage and attitudes. Comput Human Behav 2010;26(6):1710–21. doi: 10.1016/j.chb.2010.06.020
- Pape TL, Kim J, Weiner B. The shaping of individual meanings assigned to assistive technology: a review of personal factors. Disabil Rehabil 2002;24(1–3):5–20. doi: 10.1080/09638280110066235
- Tung JY, Stead B, Mann W, Pham B, Popovic MR. Assistive technologies for self-managed pressure ulcer prevention in spinal cord injury: a scoping review. J Rehab Res Dev 2015;52(2):121–147. doi: 10.1682/JRRD.2014.02.0064
- Curtin CM, Suarez PA, Di Ponio LS, Frayne SM. Who are the women and men in Veterans Health Administration’s current spinal cord injury population? J Rehabil Res Dev 2012;49(3):351–60. doi: 10.1682/JRRD.2010.11.0220
- National Spinal Cord Injury Statistical Center. Facts and figures at a glance. Birmingham, AL: University of Alabama at Birmingham, 2018. Available from https://www.nscisc.uab.edu.