Abstract
Context: Emotional Well-Being (EWB) post-spinal cord injury or disease (SCI/D) is a critical aspect of adjustment to disability. Advancing care and assuring equity in care delivery within this rehabilitation care domain is essential. Herein, we describe the selection of EWB structure, process and outcome indicators for adults with SCI/D in the first 18 months after rehabilitation admission.
Methods: A pan-Canadian Working Group completed the following tasks: (1) defined the EWB construct; (2) conducted a systematic review of available outcomes and their psychometric properties; (3) constructed a Driver diagram summarizing available evidence associated with EWB; and, (4) prepared a process map. Facilitated meetings allowed selection and review of feedback following rapid-cycle evaluations of proposed structure, process and outcome indicators.
Results: The structure indicator is the proportion of staff with appropriate education and training in EWB and access to experts and resources. The process indicator is the proportion of SCI/D patients who were screened for depression and anxiety symptoms at rehabilitation admission and rehabilitation discharge. The intermediary outcome is the proportion of SCI/D patients at risk for depression or anxiety at rehabilitation discharge based on screening symptom scores. The final outcomes are: (a) proportion of individuals at risk for depression or anxiety based on screening symptom scores; and (b) proportion of individuals who received referral for EWB services or intervention.
Conclusion: The proposed indicators have a low administrative burden and will ensure feasibility of screening for depression and anxiety at important transition points for individuals with SCI/D. We anticipate that the current structures have inadequate resources for at-risk individuals identified during the screening process.
Introduction
The primary impairments and secondary conditions (e.g. pain, skin ulcers, etc.) associated with spinal cord injury or disease (SCI/D)Citation1–3 can interfere with participation in activities of daily living (e.g. self-care), personal relationships, and community re-integration; each of which are crucial for maintaining quality of life.Citation4 Often, individuals with SCI/D must attempt to relearn new ways to engage in society.Citation5 Understandably, high rates of psychological issues occur following SCI/D are observed,Citation6 including depressiveCitation7,Citation8 and anxiety disorders,Citation9 and other forms of adjustment problems and psychological distress.Citation10
The expression of psychological issues post-SCI/D is not uniform and may be influenced by: demographic or injury-related characteristics; pre-injury behaviors and psychopathology; personality factors; social/environmental factors; and, styles of appraisal.Citation11 Although depression is not a universal occurrence in individuals with SCI/D,Citation12 the observed prevalence rates are higher in the SCI/D population when compared to their non-disabled peers.Citation13 Mood disorders following SCI/D can further impact the experience of disability among affected individualsCitation6 and lead to increased rates of suicide.Citation14–16
The prevalence of depression and anxiety is approximately 30% in individuals with SCI/D.Citation17–23 When psychological issues emerge, the clinical manifestation may follow different trajectories in terms of symptom severity and onset. Some experience depression early post-injury with improvements over time,Citation24–26 while others continue to struggle with it over their lifespan.Citation7 In other cases, individuals without signs of depression and/or anxiety early post-injury did exhibit them many years following their inpatient rehabilitation. For example, Hoffman and colleaguesCitation8 stated that 18% of individuals with SCI reported major depression at five years post-injury. Similarly, individuals with traumatic SCI with an injury severity score of 16 or greater had an almost two fold higher risk of developing depression or anxiety within a three-year follow-up period.Citation27 Overall, depression and anxiety are significant issues post-SCI, with a number of studies highlighting the first year following injury as a time of high vulnerability.Citation27–30
Despite ample research suggesting that depression and anxiety significantly affect health and well-being post-SCI/D, the task of identifying clinical depression is challenging for rehabilitation professionals. Considering the overlap between some physiological changes that occur in SCI/D and the symptoms of depression (e.g. fatigue), some health care professionals may overestimate its occurrenceCitation31 while others may overlook symptoms.Citation32 Although there have been many prior efforts to improve the detection and treatment of depression,Citation7 concerns remain that a significant proportion of inpatients with SCI/D undergoing rehabilitation, as well as outpatients, are not receiving appropriate screening or treatment.Citation33–35 In Canada, a recent environmental scan of rehabilitation hospitals providing care to patients with SCI/D indicated that there is inadequate capacity for sites to serve the emotional well-being (EWB) needs for this population.Citation36 The key recommendation from the environmental scan was the compelling need to assure equity of access to clinical care nationally, which would enhance the quality of care by standardizing the timing and format of EWB assessments during inpatient rehabilitation, and in the community, through use of valid and reliable assessment tools that do not conflate physiological symptoms with those of depression.Citation37
Moving a nationwide care agenda for depression and anxiety for SCI/D is challenging and requires buy-in from key stakeholders including decision-makers and front-line clinical staff. Therefore, it behooves us, as a rehabilitation community, to formulate an approach that builds upon the growing consensus for quality measures to support decision-making in health care.Citation38 Indicators are widely used to identify trends, inform priority setting and policy formulation, and monitor rehabilitation programs and care processes. Quality indicator data can further inform comparisons across different health care settings and support continuous quality improvement (i.e. benchmarking) while building transparency in health care.Citation38,Citation39 Indicators can measure the structure, process or outcome of health care services and their evaluation can facilitate the sustainability of a high quality health care delivery system that is predicated upon evidence-informed programs of relevance to stakeholders.Citation40 Structure indicators are defined by the properties of the setting in which the health care services are deliveredCitation41 while process indicators describe the specific activities in providing and receiving of care.Citation42 Finally, outcome indicators describe the effects of health care provided to a given individual or population (e.g. mortality, health-related quality of life, or patient satisfaction etc.Citation42 Together, they provide a framework for evaluation care.
The objective of this initiative was to establish a set of structure, process and outcome indicators to assess EWB in adult patients with SCI/D during the initial 18 months following their admission to inpatient rehabilitation. The term “Emotional Well-Being” was selected as the nomenclature to ensure recognition of a broad perspective of elements affecting psychological well-being. Although depression and anxiety are significant clinical issues for individuals with recent onset SCI/D, there are other aspects of EWB (i.e. coping, self-esteem, etc.) that our team felt would merit exploration to determine how to best impact practice and policy. This process is part of a larger initiative to develop, implement and evaluate 11 Domains of rehabilitaiotn care across Canada to improve the quality and equity of SCI rehabilitation care by 2020.Citation43
Methods
A detailed description of the overall SCI-High Project methods and process for identifying EWB as a priority Domains for SCI rehabilitation care are described in related manuscripts in this issue.Citation43 In addition to the SCI-High Project Leaders (www.sci-high.ca), an external advisory committee and national data strategy committee supported the global Project goals and provided oversight regarding the context for implementing all of the planned indicators. The Project Leaders stipulated that the selected indicators must be relevant, concise (<10 minutes to implement), feasible, and aligned to measure critical elements that would drive advances in care within each Domains.
The approach to developing the EWB indicators followed a modified but similar approach to that described by Mainz,Citation38,Citation43 which included the following planning and development phases: (a) formation and organization of the national and local Working Groups;Citation43 (b) defining and/or refining the key Domain-specific construct; (c) providing an overview of existing evidence and practice; (d) developing and interpreting a Driver diagram; (e) selecting indicators; and (f) pilot testing and refininig the Domain-specific structure, process and outcome indicators. Throughout these processes, a facilitated discussion occurred amongst the Domain-specific Working Group and SCI-High Project Leaders to utilize relevant subject matter expertise, while ensuring the broader goals of the SCI-High Project were aligned across the other ten Domain Working Groups (as appropriate).
Domain selection
The selection of EWB as a Domain of interest for developing indicators emerged from a consensus-building activity to select the broader set of key Domains being pursued in the larger initiative.Citation44 EWB, as well as the other selected Domains, originated from the E-Scan project.Citation45 The E-Scan: defined specific domains of adult SCI rehabilitation and the common goals and processes of rehabilitation care specific to the domain; spotlighted a Canadian centre with the best practice in a particular domain of care;Citation45 and provided a national summary report card pertinent to the domain of care outlining gaps in care related to knowledge generation, clinical implementation and health policy. Hence, the initial EWB construct used for this initiative was:
Emotional well-being is a state of mind in which the individual realizes his or her own abilities, is able to cope with the normal stresses of life and can interact and contribute in the community. Enhanced emotional well-being can positively contribute to coping ability, self-esteem, productivity and longevity.Citation46
Emotional Well-Being working group
In organizing a team to develop a set of indicators, it is recommended to have individuals with different perspectives.Citation47 This includes having individuals with expertise in measurement, of the clinical domain, project administration and/or user representatives.Citation48 A caveat is to limit the size of the team so that discussions do not become “unwieldy”.Citation38 A team of eight to 14 individuals from different backgrounds and/or varying expertise is sufficient for expert discussions.Citation38 Hence, the EWB Working Group was comprised of 12 members who were expert clinicians (e.g. clinical psychologists, social workers, patient and family educators, medical doctors, etc.), researchers, and/or community advocates from non-governmental organizations across three provinces (Ontario, Alberta and British Columbia).
Evidence map
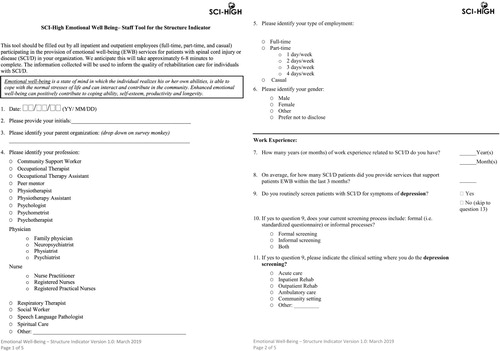
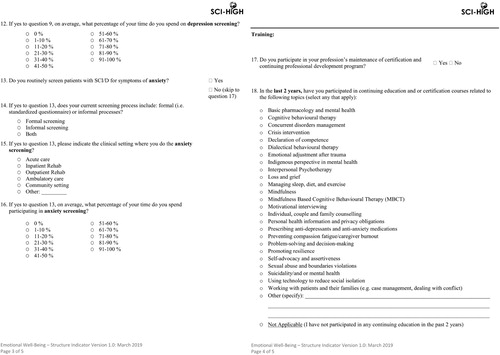
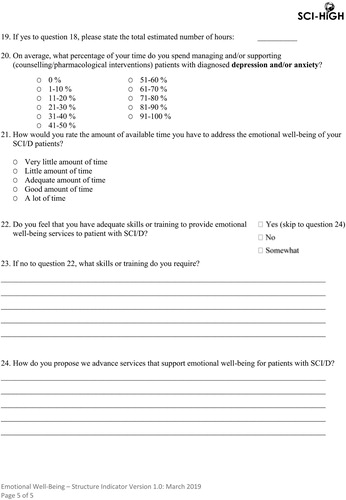
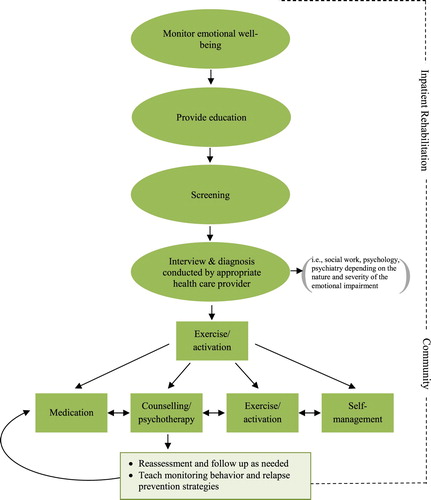
For developing and selecting a set of indicators, it is critical that the evidence informing this process is based on empirical data,Citation48 and not solely based on expert opinion.Citation47 Thus, a comprehensive review of the literature and of existing clinical practice guidelines relevant to the EWB was conducted, and a list of available outcome measures used to assess EWB post-SCI/D was generated (see Supplementary document). Furthermore, the Project Leaders developed Ishikawa or Driver diagrams, which are graphic illustrations used as a brainstorming tools to provide a systematic approach to identifying components of care that contribute to each priority rehabilitation care domain.Citation49 Two Driver diagrams were generated from the systematic literature searches; these included EWB () and depression (). In addition, the Working Group was provided with a proposed care model described in the EWB chapter of the E-Scan;Citation37 () to help stimulate ideas for the selection and refinement of the indicators following pilot testing.
Figure 1 Emotional Well-Being (EWB) Driver diagram. UEMS: Upper-Extremity Motor Score; LEMS: Lower-Extremity Motor Score; NLI: Neurological Level of Injury; HR: Heart Rate; BP: Blood Pressure; PTSD: Post-Traumatic Stress Disorder; UTI: Urinary Tract Infection.
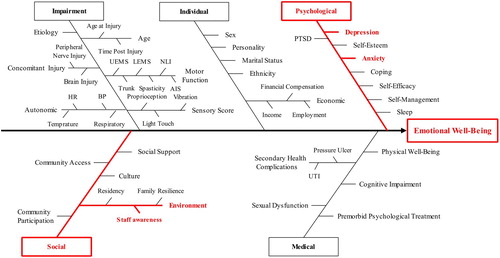
Figure 2 Depression Driver diagram. UEMS: Upper-Extremity Motor Score; LEMS: Lower-Extremity Motor Score; NLI: Neurological Level of Injury; AIS: ASIA Impairment Scale; HR: Heart Rate; BP: Blood Pressure; PIL: Purpose In Life; EROS: Environmental Rewards Observation Scale; CBT: Cognitive Behavioral Therapy. *Personality disorder, substance abuse, bipolar disorder, Schizophrenia, anxiety, and Post-Traumatic Stress Disorder (PTSD). **Intravenous anesthesia, tracheostomy, artificial respiration, and gastrostomy.
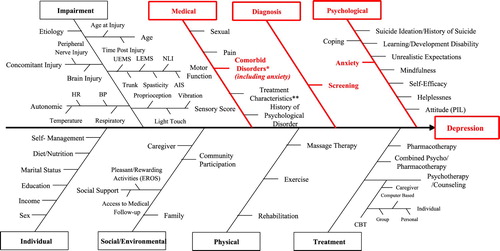
Figure 3 A diagram depicting a potential model for future emotional well-being service provision (taken from the E-Scan Atlas with permission from the authorCitation37).
Selection of indicators
Between September 2016 and November 2018, nine teleconferences with the Working Group were facilitated by a member of the SCI-High investigative team to establish the EWB indicators. The key parameters provided to the team included: the indicators that needed to be collected at admission and then within the first 18 months following inpatient rehabilitation; the indicators should inform one another; and could be feasibly implemented nationally, recognizing that some hospitals varied in their capacity in terms of size, staffing and resources. The goal was to develop a set of three indicators that would improve EWB rehabilitation care for patients with SCI/D by 2020.
Pilot testing
An important step prior to implementing a set of indicators is to conduct pilot testing.Citation38 Following the series of Working Group meetings to develop the indicators, a pilot study was implemented to test the feasibility of the agreed upon indicators (described in the Results section below).
Results
Construct definition
The initial process towards indicator development was to review and refine the construct definition and related Driver diagrams. Throughout these processes, the Working Group felt it was imperative that the construct of EWB was retained to ensure that the focus was not solely on psychopathology. For instance, identifying factors that promoted self-efficacy were discussed as this construct is an important predictor of positive outcomes post-injury.Citation50–52 Similarly, coping styles were of interest, as other authors have reported that how individuals cope early-post injury can predict long-term outcomes. Pollard and KennedyCitation53 conducted a longitudinal study of 87 inpatients with SCI and reported that the rates of anxiety and depression did not significantly change over a decade and that coping strategies used at week 12 explained one third of the variance in depression rates at year ten. Thus, there was a strong impetus to ensure that key factors associated with promoting EWB were included in the national dialogue. Although other EWB definitions were reviewed (e.g. Public Health Agency of CanadaCitation50) to help critically reflect on the construct definition, the team decided to endorse utilizing the construct described in the E-Scan,Citation54 albeit with some modifications. For example, the group agreed to remove “productivity” from the working definition as it denotes employment, which is not available to significant proportions of people with SCI/D. However, the group agreed to add in “economic stability” to recognize the importance of the contribution of economics to EWB in the first 18 months post-SCI/D rehabilitation admission. The final construct definition was:
Emotional well-being is a state of mind in which the individual realizes his or her own abilities, is able to cope with the stresses of life, and can interact and participate in the community. Enhanced emotional well-being is associated with improved mood states, self-esteem, meaningful roles and relationships, resilience, physical and mental health, economic stability and longevity.
Indicator development
After finalizing the construct, the guiding strategy of ensuring significant clinical impact was used to focus the group's efforts. Given the significance and impact of depression and anxiety following SCI/DCitation9 the group achieved consensus to develop a set of three indicators focused on achievement of a single aim. To substantially impact the EWB needs post-SCI/D, it was agreed that having indicators that could identify the incidence of depression and anxiety symptoms would be invaluable as no national data was available on this topic. As well, it was felt that screening inpatients would lead to a higher likelihood of patients being referred to an appropriate EWB service. The EWB structure, process and outcome indicators are presented in .
Table 1 Selected structure, process and outcome indicators for the Emotional Well-Being Domain.
To assure national generalizability, the Working Group initially focused on the structure indicator in order to inform the process and outcome indicators (). For the structure indicator, the Working Group agreed that any health care professional with appropriate education and training in recognizing and understanding EWB post-SCI/D with access to experts and resources participate in the provision of EWB services, as not all rehabilitation hospitals have on-site access to psychologists, psychiatrists and/or social workers. Pilot data collection of the structure indicator is currently ongoing, and the collected data will use consensus methods to inform a future definition of “appropriate education and training”. The natural process indicator to emerge from this structure indicator was the process of screening for symptoms of depression and anxiety. Recognizing that not all patients with SCI/D within Canada are likely to continue to receive follow-up services at their initial rehabilitation center, the Working Group decided that the two time points for screening would be at admission and discharge from inpatient rehabilitation.
Figure 4 Emotional Well-Being structure indicator tool.
With regard to the outcome indicator, several meetings were focused on discussing publicly available (e.g. no cost) reliable and valid screening measures for depression and anxiety post-SCI/D. Although the Structured Clinical Interview DSM,Citation55 which is the gold standard used by trained mental health professionals for diagnosing major depressive disorders, was ideal; it was not a feasible solution for a national rollout because of the high degree of administrative burden and lack of available expertise. The clinical members of the Working Group used different measures in their practice for screening depression and anxiety, with the Patient Health Questionnaire-9 (PHQ-9),Citation56 the Generalized Anxiety Disorder 7 (GAD-7) scale,Citation57 and the Depression Anxiety Stress Scales 21 (DASS-21)Citation58 being the more commonly used measures. Following a review of available literature, there was not one measure that the team felt best-addressed screening for both depression and anxiety and/or across all patient settings. For instance,Citation59 the team was concerned that the PHQ-9 was not ideally-suited for inpatients, but felt it was appropriate for outpatients. However, Bombardier and colleaguesCitation60 debunked this assumption as their data was collected in an inpatient context. As well, some were concerned the PHQ-9 did not screen for anxiety.
Conversely, the DASS-21 does screen for anxiety but it has a greater level of administrative burden and is not as sensitive for detecting depression as the PHQ-9 in individuals with SCI. A challenge with using depression screening measures in SCI/D is the need to adjust cut-off scores to minimize conflating depressive symptoms with physical symptoms of SCI (e.g. fatigue).Citation61,Citation62 Given the various strengths and weaknesses of each measure, the group decided that the PHQ-9 and DASS-21 (found in the public domain) would be piloted as potential outcome indicators.
Indicator piloting
To trial and optimize workflow, the process of screening for depression utilizing the PHQ-9 measure was implemented in an adult outpatient clinic at a tertiary SCI rehabilitation hospital in a large urban center. Consecutive patients attending routine follow-up appointments with physiatrists were approached by trained evaluators (fellows or senior residents in Physiatry) to complete the PHQ-9 prior to physician assessment. Physical assistance was provided in completing the pen and paper tool when required. A positive screening test was defined as a score of 11 or greater, as defined in the literature,Citation60 which was provided to the physician to incorporate into their management plan. The data collected included the number of positive screens, time required to complete the questionnaire, concordance of the PHQ-9 results and physician clinical impression and actions taken by a regulated health care professional (physician or nurse) due to the identification of depressive symptoms. Additionally, barriers to implementation of the questionnaire were noted.
A similar process of screening for anxiety was performed at the same outpatient clinic using the seven-item Anxiety subscale of the DASS-21. Overall scores for the related subscales of the anxiety construct were calculated, with higher scores indicating greater distress.Citation63 Data collected included the overall scores related to the anxiety subscale, time required to complete the measure, as well as the feasibility and challenges of implementing the measure. There were fewer established processes for treatment of anxiety than depression in this setting.
Pilot study results – PHQ-9
Initial pilot data from 15 individuals with SCI/D approached for screening included 13 patients who completed the PHQ-9. Three patients’ scores fell within the range suggestive of depressed mood. All positive screens were concordant with the physician's clinical assessment. For management of depressive symptoms, all patients were referred for counseling and one was also started on pharmacotherapy. One patient did not complete the measure due to concurrent cognitive and hearing deficits, while another declined the assessment due to an established psychiatric diagnosis. Negative screens were completed in less than two minutes; however, positive screens were completed in 5–10 minutes. Noted barriers to implementation included the impact of cognitive and motor deficits on the ability to independently answer questions, the additional time required to address mental health issues, and the impact of pre-existing psychiatric diagnosis on the interpretation.
Pilot study results – DASS-21
The pilot data on anxiety screening includes results from 21 individuals with SCI/D that completed the DASS-21. While majority of the patients’ scores fell within the range suggestive of normal (0–7) and moderate anxiety (10–14) levels, three patients had scores indicating extremely severe anxiety (20+) levels. The DASS-21 tools were completed on average in less than two minutes. Noted feasibility issues and challenges experienced when the patients self-administered the tool included: (1) the impact of motor deficits on the ability to self-administer the tool; and (2) inability to understand certain aspects of the tool (i.e. clarifications needed on the timeframe of the questions being asked). Feasibility issues and challenges when the evaluator conducted the interview included: (1) the additional time taken by patients to discuss the responses in-depth; and (2) potential response bias, whereby some patients responded in a positive way (i.e. providing responses that made themselves look favorable to the evaluator).
Discussion
The SCI-High initiative established a set of structure, process and outcome indicators to assess EWB in adults with SCI/D in the first 18 months after inpatient rehabilitation admission. Although the conceptual focus of this Domain of care is intended to represent a broad construct of what constitutes EWB, the resulting indicators are designed to identify symptoms of depression and anxiety following SCI/D, and to capture whether individuals are receiving appropriate treatment referrals. These EWB Domains were selected by the Working Group since they were determined to likely have the most impact on making a meaningful change in inpatient rehabilitation practice for the SCI/D population. Depression and anxiety are prevalent conditions post-SCI/D, which can subsequently affecting health and quality of life.Citation6 Addressing depression and anxiety during inpatient rehabilitation might provide opportunities to mitigate its effects, given that early adjustment following SCI/D is a positive predictor of long-term outcomes.Citation53 Regardless, the decision to keep the EWB nomenclature to encompass this rehabilitation Domain construct will ensure on-going national recognition that other aspects of EWB (e.g. coping styles, life satisfaction, etc.) should be addressed to optimize outcomes following SCI/D in subsequent indicator interactions.
The selected indicators on depression and anxiety will provide an opportunity to decrease stigma associated with mental health issues,Citation64 consistent with the goals of several national health programs.Citation65 Although the social stigma associated with experencing depression post-SCI/D has not been investigated extensively, preliminary findings suggest it exists.Citation22 Accordingly, raising awareness with universal screening may help individuals with SCI/D to seek various supports during inpatient rehabilitation and once discharged home.
Potential challenges associated with the implementation of the proposed indicators include the costs associated with identifying large numbers of individuals with depression and/or anxiety. It is well-established that the economic burden post-SCI/D in Canada is substantial, with lifetime estimates ranging from $1.5 million for individuals with incomplete paraplegia to $3.0 million for those with complete tetraplegia.Citation66 Similarly, the economic burden of mental illness in Canada will increase six-fold over the next 30 years, with costs likely to exceed 2.7 trillion CAD.Citation67 Within the Canadian finite-envelope health care funding system, the ability to adequately meet all of the physical and mental health needs of individuals with SCI/D will be challenging given the substantial costs associated with SCI/D and mental health services. As well, there is inequity in the availability of resources across the country, with urban centers having more access to specialized services within both hospital and the community setting to meet the needs of individuals with SCI/D compared to rural regions.Citation45 We further foresee a potential constraint associated with determining a protocol for referring at-risk patients (post-screening for symptoms of depression and anxiety) to appropriate resources. The Working Group is currently in discussion as to whether to develop such a protocol to enhance implementation. In addition, there may be potential feasibility challenges with respect to obtaining informed consent from patients to share anonymized results and allow for widespread reporting of indicator data. Although there are challenges, it is critical to implement the EWB indicators to ensure people with SCI/D at risk for depression and/or anxiety have their mental health needs met to maximize coping, improve quality of life, enhance community reintegration, and engage in meaningful roles and relationships.
It is imperative to recognize that one-size rehabilitation does not fit all patients with SCI/D.Citation68 In fact, rehabilitation treatment interventions are context-specific for the individual with SCI/D (i.e. patient and injury characteristics) and are influenced by the hospital/ site's access to resources (e.g. availability of health care professionals trained to provide care related to depression and anxiety).Citation68 There are guidelines for the management of mental health in Canada (http://www.canmat.org/), but unlike other countries, these are not SCI/D specific. While our study does not dictate how health care professionals should provide treatment to their patients with SCI/D within their setting, it has provided a set of quality indicators that would be feasible for all centers to adopt to facilitate routine screening. This ensures that patients “at-risk” for depression and anxiety are not overlooked in the rehabilitation process. If a better understanding of the extent of depression and anxiety post-SCI/D is established, this could help stimulate the development of SCI-specific clinical guidelines for Canada and reallocation of mental health resources.
To support the national implementation of the SCI-High indicators, a meeting was held with managers of Canadian rehabilitation centers providing care to patients with SCI/D to review the proposed indicators for all care Domains, including EWB. The outcome of that meeting was a commitment to explore the inclusion of the potential indicators at the individual rehabilitation hospitals. However, MainzCitation38 notes “Before clinical indicators are implemented they should be thoroughly tested” (p. i10). At this stage, the pilot testing of the EWB indicators has not yet been fully vetted due to some noted patient and system barriers encountered in the pilot testing described above. A limitation of our pilot data was that it was obtained at a large specialized tertiary site that was dedicated to SCI/D rehabilitation. As a result, this site had wide access to medical residents, a psychologist, and social workers who could support the testing of our indicators. Other sites across Canada are either smaller or may have a mixed patient-population due to inequities of services,Citation54 which will necessitate that other sites enrolling into the SCI-High initiative might need to modify how these indicators are implemented. An implementation science approach (i.e. specifying what, when and howCitation69) will be utilized to help identify facilitators and barriers that different sites will need to consider in adopting the EWB indicators. Regardless, our pilot data suggests mental health screening is feasible for individuals with SCI/D at important rehabilitation transition points, which has helped to set the stage for nationwide validation and benchmarking to advance knowledge and access to proper care.
Conclusions
In summary, the use of structure, process and outcome indicators to support EWB across Canadian SCI rehabilitation hospitals holds the potential for advancing knowledge about the incidence and clinical course of depression and anxiety and will ensure that more individuals with SCI/D have access to proper care. Moreover, Elliott and KennedyCitation12 have noted the research on interventions for depression is not as well-developed and that there is a need for more research to bolster the evidence underlying various treatments. Raising further awareness regarding EWB might stimulate further research on the topic to refine current approaches to be more targeted for individuals with SCI/D. More importantly, addressing depression and anxiety early-post injury will likely lead to better physical health outcomes and reduce the burden to the larger health care system since patients better equipped to self-manage their injuries in the community.
Disclaimer statements
Contributors None.
Disclosure of Interest Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation and receipt of consulting fees from The Rick Hansen Institute. Dr. S. Mohammad Alavinia, Patricia Bain, Teren Clarke, Farnoosh Farahani, Heather Flett, Dr. Sander L. Hitzig, Dr. Gaya Jeyathevan, Sandra Mills, Dr. Vanessa K. Noonan, Dr. Steven Orenczuk, Dr. Rebecca Titman, and Dr. Matheus J. Wiest report no conflicts of interest.
Supplemental data
Supplemental data for this article can be accessed http://dx.doi.org/10.1080/10790268.2019.1605750.
Supplemental Material
Download MS Word (21.7 KB)Acknowledgements
The authors would like to thank Dr. Cheryl Bradbury, Dr. Mark Bayley and Maryam Omidvar from Toronto Rehabilitation Institute – University Health as well as Stacey Guy from Parkwood Institute Research and Dr. Swati Mehta from University of Regina, for their valuable contributions during the development of the Emotional Well-Being indicators.
ORCID
Sander L. Hitzig http://orcid.org/0000-0002-9139-9250
Rebecca Titman http://orcid.org/0000-0001-9950-744X
Heather Flett http://orcid.org/0000-0001-9444-8006
Vanessa K Noonan http://orcid.org/0000-0003-3226-9218
Farnoosh Farahani http://orcid.org/0000-0002-3937-7708
Matheus Joner Wiest http://orcid.org/0000-0003-1444-4828
Gaya Jeyathevan http://orcid.org/0000-0001-5525-3214
S. Mohammad Alavania http://orcid.org/0000-0002-5503-9362
B. Catharine Craven http://orcid.org/0000-0001-8234-6803
Additional information
Funding
References
- Furlan JC, Fehlings MG. Cardiovascular complications after acute spinal cord injury: pathophysiology, diagnosis, and management. Neurosurg Focus. 2008;25(5):E13. doi: 10.3171/FOC.2008.25.11.E13
- Krassioukov A. Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol. 2009;169(2):157–64. doi: 10.1016/j.resp.2009.08.003
- Yezierski RP. Spinal cord injury pain: spinal and supraspinal mechanisms. J Rehabil Res Dev. 2009;46(1):95–107. doi: 10.1682/JRRD.2008.06.0074
- Tonack M, Hitzig SL, Craven BC, Campbell KA, Boschen KA, McGillivray CF. Predicting life satisfaction after spinal cord injury in a Canadian sample. Spinal Cord. 2008;46(5):380–5. doi: 10.1038/sj.sc.3102088
- Trieschmann R. Spinal Cord Injuries: Psychological, Social, and Vocational Rehabilitation. 2nd ed. New York: Demos Publishing; 1988.
- Orenczuk S, Mehta S, Slivinski J, Teasell RW. Depression following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al., (eds.) Spinal Cord Injury Rehabilitation Evidence Version 5.0. Vancouver, BC: Rick Hansen Institute & Ontario Neurotrauma Foundation; 2014. p. 1–35. Available from https://scireproject.com/evidence/rehabilitation-evidence/depression-following-spinal-cord-injury/.
- Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG. Symptoms of major depression in people with spinal cord injury: implications for screening. Arch Phys Med Rehabil. 2004;85(11):1749–56. doi: 10.1016/j.apmr.2004.07.348
- Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):411–18. doi: 10.1016/j.apmr.2010.10.036
- Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil. 2000;81(7):932–7. doi: 10.1053/apmr.2000.5580
- Victorson D, Tulsky DS, Kisala PA, Kalpakjian CZ, Weiland B, Choi SW. Measuring resilience after spinal cord injury: development, validation and psychometric characteristics of the SCI-QOL Resilience item bank and short form. J Spinal Cord Med. 2015;38(3):366–76. doi: 10.1179/2045772315Y.0000000016
- Elliott TR, Rivera P. Spinal cord injury. In: Nezu A, Maguth C, Geller P, editor. Handbook of Psychology: Health Psychology. Hoboken, NJ: John Wiley & Sons Inc.; 2003. p. 415–35.
- Elliott TR, Kennedy P. Treatment of depression following spinal cord injury: an evidence based review. Rehabil Psychol. 2004;49:134–9. doi: 10.1037/0090-5550.49.2.134
- Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Depression following traumatic spinal cord injury. Neuroepidemiology. 2005;25(2):55–61. doi: 10.1159/000086284
- Charlifue SW, Gerhart KA. Behavioral and demographic predictors of suicide after traumatic spinal cord injury. Arch Phys Med Rehabil. 1991;72(7):488–92.
- DeVivo MJ, Black KJ, Richards JS, Stover SL. Suicide following spinal cord injury. Paraplegia. 1991;29(9):620–7.
- Hartkopp A, Bronnum-Hansen H, Seidenschnur AM, Biering-Sorensen F. Suicide in a spinal cord injured population: its relation to functional status. Arch Phys Med Rehabil. 1998;79(11):1356–61. doi: 10.1016/S0003-9993(98)90227-1
- Craven C, Hitzig SL, Mittmann N. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med. 2012;35(5):361–70. doi: 10.1179/2045772312Y.0000000046
- Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42(9):513–25. doi: 10.1038/sj.sc.3101629
- Hancock KM, Craig AR, Dickson HG, Chang E, Martin J. Anxiety and depression over the first year of spinal cord injury: a longitudinal study. Paraplegia. 1993;31(6):349–57.
- Hitzig SL, Campbell KA, McGillivray CF, Boschen KA, Craven BC. Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord. 2010;48(4):330–5. doi: 10.1038/sc.2009.135
- Krause JS, Bombardier C, Carter RE. Assessment of depressive symptoms during inpatient rehabilitation for spinal cord injury: is there an underlying somatic factor when using the PHQ? Rehabil Psychol. 2008;53:513–20. doi: 10.1037/a0013354
- Migliorini C, Tonge B, Taleporos G. Spinal cord injury and mental health. Aust N Z J Psychiatry. 2008;42(4):309–14. doi: 10.1080/00048670801886080
- Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil. 2015;96(1):133–40. doi: 10.1016/j.apmr.2014.08.016
- Kishi Y, Robinson RG, Forrester AW. Prospective longitudinal study of depression following spinal cord injury. J Neuropsychiatry Clin Neurosci. 1994;6(3):237–44. doi: 10.1176/jnp.6.3.237
- Richards JS. Psychologic adjustment to spinal cord injury during first postdischarge year. Arch Phys Med Rehabil. 1986;67(6):362–5.
- Richardson EJ, Richards JS. Factor structure of the PHQ-9 screen for depression across time since injury among persons with spinal cord injury. Rehabil Psychol. 2008;53:243–9. doi: 10.1037/0090-5550.53.2.243
- Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, et al. Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS One. 2017;12(1):e0169623. doi: 10.1371/journal.pone.0169623
- Bombardier CH, Adams LM, Fann JR, Hoffman JM. Depression trajectories during the first year after spinal cord injury. Arch Phys Med Rehabil. 2016;97(2):196–203. doi: 10.1016/j.apmr.2015.10.083
- Craig AR, Hancock KM, Dickson HG. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia. 1994;32(10):675–9.
- Mehta S, Orenczuk S, Hansen KT, Aubut J-AL, Hitzig SL, Legassic M, et al. An evidence-based review of the effectiveness of cognitive behavioral therapy for psychosocial issues post-spinal cord injury. Rehabil Psychol. 2011;56(1):15–25. doi: 10.1037/a0022743
- Cushman LA, Dijkers MP. Depressed mood in spinal cord injured patients: staff perceptions and patient realities. Arch Phys Med Rehabil. 1990;71(3):191–6.
- Kemp B, Mosqueda L. Aging with a Disability: What the Clinician Needs to Know. Boston: John Hopkins University Press; 2004.
- Faber RA. Depression and spinal cord injury. Neuroepidemiology. 2005;25(2):53–4. doi: 10.1159/000086283
- Kemp BJ, Krause JS. Depression and life satisfaction among people ageing with post-polio and spinal cord injury. Disabil Rehabil. 1999;21(5-6):241–9. doi: 10.1080/096382899297666
- Smith BM, Weaver FM, Ullrich PM. Prevalence of depression diagnoses and use of antidepressant medications by veterans with spinal cord injury. Am J Phys Med Rehabil. 2007;86(8):662–71. doi: 10.1097/PHM.0b013e318114cb6d
- Craven C, Verrier M, Balioussis C, Wolfe D, Hsieh J, Noonan V, et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation. Vancouver, BC: Rick Hansen Institute; 2012. Available from http://rickhanseninstitute.org/images/stories/ESCAN/RHESCANATLAS2012WEB_2014.pdf.
- Craven BC, Verrier M, Balioussis C, DW P, Hsieh J, Noonan V, et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation, Emotional Wellbeing. Vancouver, BC: Rick Hansen Institute; 2012. Available from: http://rickhanseninstitute.org/RHI/J__Emotional_Wellbeing/J__Emotional_Wellbeing/index.html#/1/.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care. 2003;15(Suppl 1):5i–11. doi: 10.1093/intqhc/mzg084
- Rubin HR, Pronovost P, Diette GB. The advantages and disadvantages of process-based measures of health care quality. Int J Qual Health Care. 2001;13(6):469–74. doi: 10.1093/intqhc/13.6.469
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord. 2013;51(2):165–9. doi: 10.1038/sc.2012.91
- Idvall E, Rooke L, Hamrin E. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs. 1997;25(1):6–17. doi: 10.1046/j.1365-2648.1997.1997025006.x
- Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, et al. Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Med Care. 2002;40(3):237–45. doi: 10.1097/00005650-200203000-00007
- Craven BC, Alavinia SM,Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-high Project. J Spinal Cord Med. 2019;42(Suppl 1):S51–S67.
- Craven BC, Flett H, Hitzig SL, Farahani F, Alavinia SM, Omidvar M, et al. Moving from prioritization to implementation: the spinal cord injury rehabilitation care high performance indicators (SCI-high) project. J Spinal Cord Med. 2017;40(6):WCA162, 865.
- Craven BC, Verrier M, Balioussis C, Wolfe D, Hsieh J, Noonan V, et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation. Vancouver: Rick Hansen Institute; 2012.
- Herrman H, Shekhar S, Moodie R. Promoting Mental Health: Concepts, Emerging Evidence, Practice. A Report of the World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. Geneva, Switzerland: World Health Organization; 2005.
- Mainz J, Bartels PD, Laustsen S. The national indicator project to monitoring and improving of the medical technical care. Ugeskr Laeger. 2003;163:6401–6.
- Rubin HR, Pronovost P, Diette GB. From a process of care to a measure: the development and testing of a quality indicator. Int J Qual Health Care. 2001;13(6):489–96. doi: 10.1093/intqhc/13.6.489
- Phillips J, Simmonds L. Using fishbone analysis to investigate problems. Nurs Times. 2013;109(15):18–20.
- Kennedy P, Taylor N, Hindson L. A pilot investigation of a psychosocial activity course for people with spinal cord injuries. Psychol Health Med. 2006;11(1):91–9. doi: 10.1080/13548500500330494
- Middleton J, Tran Y, Craig A. Relationship between quality of life and self-efficacy in persons with spinal cord injuries. Arch Phys Med Rehabil. 2007;88(12):1643–8. doi: 10.1016/j.apmr.2007.09.001
- Nicholson Perry K, Nicholas MK, Middleton J. Spinal cord injury-related pain in rehabilitation: a cross-sectional study of relationships with cognitions, mood and physical function. Eur J Pain. 2009;13(5):511–7. doi: 10.1016/j.ejpain.2008.06.003
- Pollard C, Kennedy P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol. 2007;12(Pt 3):347–62. doi: 10.1348/135910707X197046
- Noonan VK, Hitzig SL, Orenczuk S, Bain P, Bradbury C, Craven BC, et al. Emotional wellbeing. In: Craven BC, Verrier M, Balioussis C, Wolfe DL, Hsieh J, Noonan VK, et al., (eds.) Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian Spinal Cord Injury Rehabilitation. Vancouver, BC: Rick Hansen Institute; 2012. Available from http://rickhanseninstitute.org/RHI/R__Community_Participation/R__Community_Participation/index.html#/1/.
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. doi: 10.1016/0005-7967(94)00075-U
- Bombardier CH, Smiley J. Measurement characteristics and clinical utility of the Patient Health Questionnaire-9 among individuals with spinal cord injury. Rehabil Psychol. 2015;60(2):211–12. doi: 10.1037/rep0000042
- Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR. Validity of the Patient Health Questionnaire-9 in assessing major depressive disorder during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil. 2012;93(10):1838–45. doi: 10.1016/j.apmr.2012.04.019
- Kalpakjian CZ, Bombardier CH, Schomer K, Brown PA, Johnson KL. Measuring depression in persons with spinal cord injury: a systematic review. J Spinal Cord Med. 2009;32(1):6–24. doi: 10.1080/10790268.2009.11760748
- Sakakibara BM, Miller WC, Orenczuk SG, Wolfe DL, Team SR. A systematic review of depression and anxiety measures used with individuals with spinal cord injury. Spinal Cord. 2009;47(12):841–51. doi: 10.1038/sc.2009.93
- Vignola RC, Tucci AM. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. Journal of affective disorders. 2014;155:104–9. doi: 10.1016/j.jad.2013.10.031
- Stuart H, Patten SB, Koller M, Modgill G, Liinamaa T. Stigma in Canada: results from a rapid response survey. Can J Psychiatry. 2014;59(10 Suppl 1):27–33. doi: 10.1177/070674371405901S07
- Stuart H, Chen SP, Christie R, Dobson K, Kirsh B, Knaak S, et al. Opening minds in Canada: background and rationale. Can J Psychiatry. 2014;59(10 Suppl 1):8–12. doi: 10.1177/070674371405901S04
- Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33(3):113–22.
- Doran CM, Kinchin I. A review of the economic impact of mental illness. Aust Health Rev. in press.
- Whiteneck G, Gassaway J. The SCIRehab project: what rehabilitation interventions are most strongly associated with positive outcomes after spinal cord injury? J Spinal Cord Med. 2012;35(6):482–3. doi: 10.1179/2045772312Y.0000000083
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50