Abstract
Background: High-quality rehabilitation care following spinal cord injury or disease (SCI/D) is critical for optimizing neurorecovery and long-term health outcomes. This manuscript describes the methods used for developing, refining, and implementing a framework of structure, process, and outcome indicators that reflect high-quality rehabilitation among adults with SCI/D in Canada.
Methods: This quality improvement initiative was comprised of the following processes: (1) prioritization of care Domains by key stakeholders (scientists, clinicians, therapists, patients and stakeholder organizations); (2) assembly of 11 Domain-specific Working Groups including 69 content experts; (3) conduct of literature searches, guideline and best practice reviews, and outcome synthesis by the Project Team; (4) refinement of Domain aim and construct definitions; (5) conduct of cause and effect analysis using Driver diagrams; (6) selection and development of structure, process and outcome indicators; (7) piloting and feasibility analysis of indicators and associated evaluation tools; and, (8) dissemination of the proposed indicators.
Result: The Project Team established aims, constructs and related structure, process, and outcome indicators to facilitate uniform measurement and benchmarking across 11 Domains of rehabilitation, at admission and for 18 months thereafter, among adult Canadians by 2020.
Conclusion: These processes led to the selection of a feasible set of indicators that once implemented should ensure that adults with SCI/D receive timely, safe, and effective rehabilitation services. These indicators can be used to assess health system performance, monitor the quality of care within and across rehabilitation settings, and evaluate the rehabilitation outcomes of the population to ultimately enhance healthcare quality and equity.
Introduction
Quality of care can be defined as “the degree to which health care services for individuals and populations increase the likelihood of desired outcomes, and are consistent with current professional knowledge”Citation1 (1161). The Institute of Medicine has defined six key dimensions of a high-quality health care system that are included in the mnemonic, “STEEEP,” which includes: Safety, Timeliness, Efficiency, Equitable Access, Effectiveness and Patient-Centered.Citation2 There is extensive evidence that measurement of indicators by audit and feedback,Citation3–5 can improve quality of care. Measuring high-quality care is not easy, but can be achieved through the development and implementation of appropriate evidence-based quality of care indicators. Best practice recommendations grounded upon evidence-based indicators of quality care are successfully implemented in stroke,Citation6,Citation7 cancer,Citation8 diabetes,Citation9 and cardiac care.Citation10 To date among neurological populations, significant efforts have been made to develop indicators for measuring and reporting the quality of stroke rehabilitation careCitation11,Citation12 and are an explicit example of how the use of indicators can optimize neurorecovery and post-discharge patient outcomes. However, this has not been done in the field of spinal cord injury rehabilitation.
Spinal cord injury or disease (SCI/D) onset results in complex changes in an individual’s physical health, functional abilities, emotional well-being, and financial independence.Citation13 To add insult to injury, individuals with SCI/D often experience barriers to accessing the optimal tertiary rehabilitation care they require. The heterogeneity of SCI/D care in part results from individuals having diverse motor, sensory and autonomic impairments, and the individual’s social and emotional adjustment. In addition, care is delivered across acute, rehabilitation, and community settings, which make measuring quality extremely challenging. Recent research highlights the many inefficiencies in the way care is provided across the continuum from SCI onset to community integration.Citation14,Citation15 Hagglund et al.Citation16 have noted that lack of transportation, physical and architectural barriers, and slow health care reform, further confound an individual’s community reintegration and care if they are living in rural regions. Current outcome tools fail to capture many Domains relevant to SCI/D rehabilitation care.Citation17 The lack of unanimity regarding a comprehensive standard set of quality of care measures is a specific and substantive barrier to advancing the quality of SCI/D rehabilitation care in Canada.
In the last five years, Accreditation Canada, a nationwide not-for-profit organization dedicated to working with patients, policy-makers and the public to improve the quality of health and social services, has developed specific SCI rehabilitation standards.Citation18 With the later advent of the Health Services Organization (HSO),Citation19 and the need for hospitals to demonstrate how they use data to inform SCI/D rehabilitation during the Accreditation process, the development of consensus-derived indicators could be a powerful tool for advancing rehabilitation care if the indicators are embedded in the Accreditation process.Citation20
Indicators can represent key features of the quality improvement process and can be categorized as structure, process, or outcome. Structure indicators are measures of the properties or characteristics of the health care setting that are judged to be necessary resources to ensure the quality of care occurs.Citation21 For example, the attributes of the material resources such as facilities, equipment, and financial and human resources, as well as organizational resources are considered structure indicators. Process indicators examine what is actually done in providing and receiving elements of care judged critical to achieving the desired outcomes. Process indicators are key elements of ensuring quality.Citation7 Outcome indicators are widely used to evaluate the effects of the care provided to a given individual or population on their long-term health and function.Citation7,Citation8 Typical outcome measures include morbidity, health status, health-related quality of life, and patient/family/provider satisfaction.Citation22 An ideal outcome indicator should capture the effect of care on the well-being of individual patients and populations. Outcome indicators are most familiar to SCI/D rehabilitation clinicians and researchers and have been studied extensively in the SCI/D literature.Citation23 The highest priority elements of SCI/D rehabilitation identified by consumers,Citation24 health care professionals, researchersCitation25 and health system leaders that should be measured have not been identified, until recently.Citation26 Routine measurement of indicators can: (1) determine the effects of health care on desired outcomes; (2) assess how well health care processes adhere to scientific evidence or professional consensus; and, (3) ensure the outcomes are consistent with patient preferences.Citation10
The Spinal Cord Injury Rehabilitation Care High Performance Indicators (SCI-High Project) is a bold endeavor which aims to select, implement and evaluate indicators of quality rehabilitation care in Canada in the first 18 months after SCI/D rehabilitation admission, by 2020. This manuscript describes the project leadership structure and steps taken to develop a comprehensive framework of structure, process, and outcome indicators for 11 prioritized Domains of SCI/D rehabilitation. This manuscript is the second in a series of 14 SCI-High Project manuscripts. A detailed description of the process for domain prioritizationCitation26 and the development of Domain-specific indicatorsCitation27–33 are described in related manuscripts in this issue.
Methods
Theoretical underpinnings of the rehabilitation framework and Domain identification
The SCI-High Project is a quality improvement initiative to advance the quality of rehabilitation care, that intuitively followed from a prior scoping review and environmental scan (E-Scan) of SCI/D rehabilitation services in Canada conducted between 2009 and 2012.Citation34,Citation35 The E-Scan involved the collaborative efforts of 17 tertiary SCI/D rehabilitation programs and 224 SCI/D expert clinicians, scientists and policymakers. The theoretical underpinning of the E-scan was based on a hybrid International Classification of Functioning, Disability, and Health modelCitation36 that was developed a priori to E-scan conduct.Citation35 The 37 Domains represented within the SCI Rehabilitation FrameworkCitation37 were used to guide the E-scan data collection, collation, and reporting. Application of the SCI Rehabilitation Framework is customized to the individual and their personal rehabilitation goals within specific rehabilitation Domains, which are typically derived from the individual’s impairments, health beliefs, and life situation.
The E-Scan contained 17 Domain-specific national report cards summarizing the current state of knowledge generation, clinical application, and policy, which highlighted the gaps between knowledge generation and clinical application in SCI/D rehabilitation.Citation34 The SCI-High Project Leaders chose to use these E-scan Domain-specific national report cards to identify Domains of rehabilitation with an opportunity to substantially advance care by 2020 through reduction of the gap between knowledge generation and clinical application. Recognizing that systematic development of quality indicators requires substantial time and resource, the SCI-High Project Leaders planned to develop quality indicators for ten Domains of SCI/D rehabilitation, necessitating a process to rank the Domains and narrow our focus from 17 Domains with the aforementioned “gaps” contained in rehabilitation framework, to a smaller number of prioritized Domains.
Rehabilitation Domain prioritization
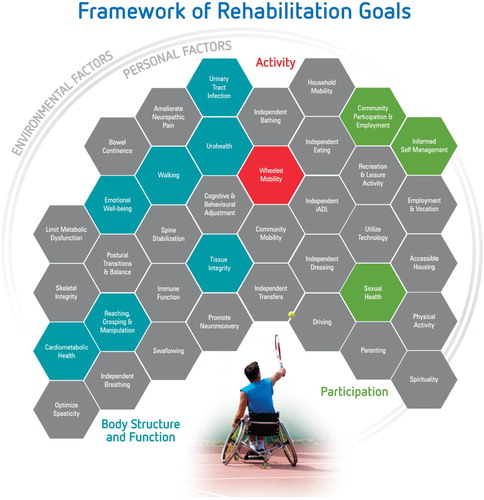
The “Hanlon Method for Prioritizing Health Problems” developed by J.J. Hanlon,Citation38 is a well-respected technique to objectively rank health priorities based on defined priority criteria and feasibility factors. Detailed results of the SCI-High Team’s utilization of a modified Hanlon methodCitation26 for stakeholder ranking of SCI/D rehabilitation Domains based on priority and feasibility scores are described in a related manuscript. Using the modified Hanlon method and UCLA/RAND consensus methods,Citation16,Citation23 the following were the top 11 prioritized SCI/D rehabilitation Domains included: Cardiometabolic Health; Community Participation and Employment; Emotional Well-Being; Reaching, Grasping, and Manipulation; Self-Management; Sexual Health; Tissue Integrity, Urinary Tract Infection (UTI); Urohealth; Walking; and, Wheeled Mobility. displays a modification of the E-Scan SCI Rehabilitation Framework highlighting the prioritized Domains and their distribution within the International Classification of Functioning, Disability and Health framework. Among the 11 prioritized Domains: seven relate to body structure and function, one to activity, and three to participation.
Project Team structure and responsibilities
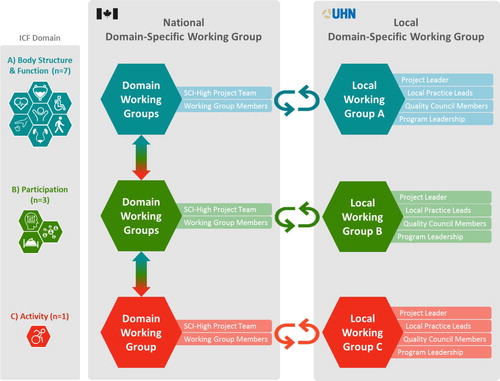
The SCI-High Project Team consists of two senior scientists, one scientist, one advanced practice leader, one project manager, two postdoctoral fellows, and one research analyst. The Team members have extensive experience in SCI/D rehabilitation care and evaluating healthcare quality. The SCI-High Project Leaders’ role (CC, MB, FF) was to guide project progression serving as an administrative, logistical, communication and evaluation hub during the indicator development, implementation, and evaluation processes. The Project Team’s activities were supported by the External Advisory Committee, Minimum Data Set Committee, the Toronto Rehab Spinal Cord Injury Rehabilitation Program (including program leaders, patients, and staff) and the Domain-specific Working Groups (). The project manager was responsible for communication within and among the Committees and Working Groups. The Toronto Rehabilitation Institute’s Lyndhurst Centre (TRI-LC) is home to the Spinal Cord Rehabilitation Program. This site houses Canada’s largest freestanding SCI/D rehabilitation facility, with 60 in-patient beds to serve 300 inpatients per year, and provide support for 20,000 outpatient tertiary clinic visits per year.
Figure 2 Overview of SCI-High Project Team structure which illustrates how the Project Team interacts with and coordinates activities across the Domain-specific Working Groups, External Advisory Committee, Toronto Rehab Spinal Cord Program, and the Data Set Committee.

External Advisory Committee
The External Advisory Committee members were responsible for participating in the ranking of rehabilitation Domains. The External Advisory Committee was comprised of 17 experts including people with lived experience, clinical experts in rehabilitation, scientists with expertise in processing and interpreting administrative data, and representatives from key stakeholder organizations including: Accreditation Canada (www.accreditation.ca), Canadian Spinal Research Organization (www.csro.com), SCI Canada (https://sci-can.ca), Ontario Neurotrauma Foundation (www.onf.org), and the Rick Hansen Institute (www.rickhanseninstitute.org).
Domain-specific Working Groups
Eleven Domain-specific Working Groups of content experts from across the country were formed to develop Domain-specific structure, process, and outcome indicators, aligned with the Domain Construct and Aim. There were 6–9 experts in each Working Group and the SCI-High Project Team members. In total, the Working Groups were comprised of 69 experts [14 physicians, 3 nurses, 5 occupational therapists, 10 physiotherapists, 2 social workers, 3 psychologists and 29 scientists (neuro-rehabilitation, kinesiology, psychology, etc.)], 3 individuals with lived experience, 4 administrative leaders and 2 patient and family educators. Some members contributed more than one area of expertise (e.g. clinician-administrators, advance practice leaders), and participated in more than one Domain-specific Working Group. Meetings were done via a series of 6–11 teleconferences. Indicator selection was based on scientific evidence, practical/clinical considerations, and the context for their decision making stipulated by the SCI-High Project Team. To ensure feasibility, the SCI-High Project Team stipulated that the outcome indicators in their entirety for all Domains should be completed within 60 min, ideally using patient self-report measures at the 18-month time point.
The SCI-High Project Team generated and synthesized documents and resources pre and post each teleconference. Outside of the teleconferences, Working Group members reviewed the prepared materials, shared resources and practice standards with one another, or conducted independent evaluations of the proposed indicators. The SCI-High Leaders actively discussed issues of concern with the Working Groups, clinicians and administrative leaders at the TRI-LC, and with others within the team’s infrastructure.
Toronto Rehab program leaders and staff
From the project outset, the leaders and staff members of the TRI-LC Spinal Cord Rehabilitation Program agreed to provide substantive in-kind support to enable rapid cycle evaluation of potential indicators, provide advice about the feasibility of implementation of proposed indicators and ensure clinical validity of the developed indicators (). As such, seven members of the TRI-LC leadership team chose to participate in the SCI-High Project in a variety of manners including as: members of the External Advisory Committee, Working Groups, local site teams that completed quality improvement Plan-Do-Study-ActCitation39 cycle evaluation of potential indicators and the November 2017 report out meeting. In addition, routine indicator pilot updates were provided to the TRI-LC Spinal Cord Rehabilitation Program’s Quality Council Committee, and at daily inpatient huddles and weekly outpatient huddles during active piloting (i.e. head-to-toe skin checks on inpatient unit or depression screening in outpatient setting).
Figure 3 Relationship between national Working Groups and local teams that piloted indicators and provided feedback iteratively between the two groups.
During the pilot processes, groups of local staff typically by profession were invited to participate in the indicator vetting and piloting processes (i.e. occupational therapists inform the reaching and grasping indicator, physical therapists discuss limitations and challenges with the Standing and Walking Assessment Tool - SWAT)Citation40 and provide advice about implementation barriers and facilitators of the proposed indicators. Local staff at TRI-LC were actively engaged in leading or participating in collaborative activities that helped to bootstrap the efforts of the Working Groups including but not limited to: the Knowledge Mobilization Network,Citation41 Rick Hansen Spinal Cord Injury Registry (RHSCIR 2.0),Citation42 Ontario Neurotrauma Foundation-funded Urology Summit,Citation43 the Electrical Stimulation Therapy Collaborative,Citation44 the SCI Solutions Alliance (alliance.sciontario.org/sci-solutions-alliance), a systematic review of Depression Screening tools,Citation45 and dissemination of the Standing and Walking Assessment Tool.Citation40 Leaders from TRI-LC and the SCI-High project leaders met with designates from HSO and Accreditation Canada to examine the overlap and synergies between the proposed indicators and current SCI Accreditation Standards to inform the activities of the Minimum Data Set Committee.
Minimum Data Set Committee
Early in SCI-High project implementation, the need for a core minimum dataset was recognized. The minimum data set will assist with determining whether an individual with SCI/D received the right treatment at the correct time. To help achieve this goal, a Minimum Data Set Committee was established, which was comprised of experts in SCI/D rehabilitation, health services and several data custodians including the RHSCIR team.Citation46 This Committee’s role was to select data elements from available patient administrative databases, registries, and clinical workload tools deemed critical for indicator inclusion to allow for national data collection. Key data elements considered were the individual’s age, sex/gender, postal code, relationship, and employment status, admission and discharge dates, impairment (International Standards for Neurological Classification of Spinal Cord Injury)Citation47 and Spinal Cord Independence Measure (SCIM)Citation48 disability scores which are sensitive to functional change among impairment subgroups. These variables are essential for identifying the numerator and denominator for indicator calculations and reporting.
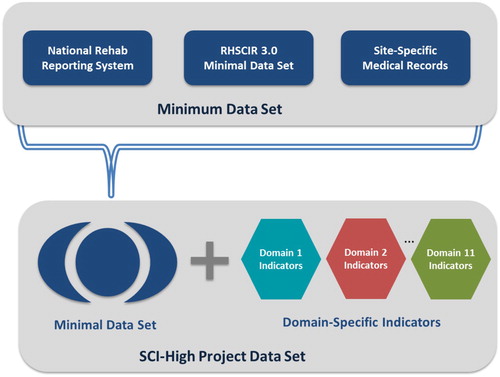
A priori, the Project Leaders determined that data for all patients with SCI/D was to be collected from the time of rehabilitation admission to 18 months thereafter. The rationale for this decision was that: (1) the current case-finding strategies for patients with non-traumatic SCICitation49 are not well established and an international classification of diseases codes for case finding was proposed for the first time in 2018;Citation50,Citation51 (2) the Project Team wanted to allow for data collection beyond one year post-injury due to the current lack of community datasetsCitation52 describing patient outcomes following rehab discharge; (3) recognizing that the median 78 day length-of-stay in Canada, and current length-of-stay targetsCitation53,Citation54 may limit the time for outcome indicator data collection; and (4) recognizing the high rates of divorce rates in the first 3 years after injury,Citation55 and the high rates of depression onset 6 months post dischargeCitation56 and the role for poor coping skills to impede self-managementCitation57 in the first few months following discharge from the inpatient rehabilitation setting. is a conceptual diagram illustrating how elements from the Canadian Institute for Health Information National Rehabilitation Reporting System (www.cihi.ca/en/national-rehabilitation-reporting-system-metadata), RHSCIR 3.0 (www.rickhanseninstitute.org) and local site health records are planned to be combined with indicator data to enable reporting in the fiscal year 2019–2020. The Project Leaders intent is to incrementally move toward transparent annual reporting of indicators and development of benchmarks of quality care.
Figure 4 The Minimum Data Set Committee will be comprised of data from the National Rehab Reporting System, RHSCIR 3.0 minimal data set, and site-specific medical records. This data will be merged with the Domain-specific indicators to form the SCI-High Project data set to evaluate the quality of SCI/D rehabilitation care.
Process for development and selection of Domain-specific indicators
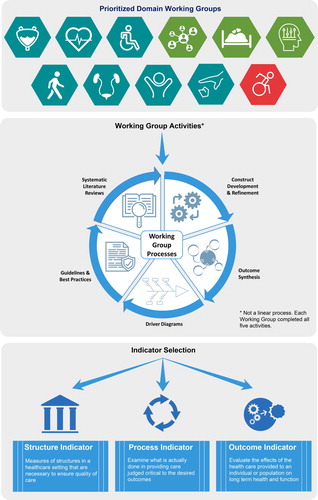
The approach to the Working Group (see section 3.b) development of Domain-specific structure, process, and outcome indicators followed a modified, but substantially similar, approach to that described by Mainz (Citation2003).Citation21 This included the following planning and development phases: (a) selecting the Domain to investigate (see Domain prioritization); (b) forming the national and local Working Groups (see section 3.b); (c) refining the Domain construct originally derived from the E-scan;Citation20 (d) identifying an aim linked to the Domain construct; (e) reviewing a summary of existing evidence and practice; (f) developing and interpreting a Driver diagram; (g) selecting indicators; and (h) pilot testing and refinement of the Domain-specific structure, process and outcome indicators. Although similar across groups, the processes as outlined above did not occur in a linear fashion, nor in the same order, across Working Groups as shown in .
Figure 5 Common processes summarizing the development of structure, process and outcome indicators for each of the 11 Domains of care.
Throughout these processes, a facilitated discussion occurred amongst the SCI-High Project Team (see section 3.a) and the Domain-specific Working Groups (see section “Domain-specific Working Groups”) in order to best utilize the relevant expertise of members, while ensuring the broader goals of the SCI-High Project were aligned across the 11 Domain Working Groups.
Working Group tools
Construct definitions and aim
The Domain-specific Working Groups (see section “Domain-specific Working Groups”) began their activities with review and discussion of the E-scan derived Domain constructs prior to creating a precise Construct definition. Developing and/or refining the Construct definition was a simple task for some groups, and very complex for others groups depending on the nature of the construct or the evolving scientific literature pertaining to a Construct (i.e. Cardiometabolic Health, Sexual Health, Community Participation), or the absence of a prior Construct. The UTI Working Group had a challenging task, as UTI was originally a component of the Urohealth construct and was added as a new Domain at the request of the study sponsor. Many groups defined a concept that was a broad idea and then defined an Aim that was the target for incremental changes in care by 2020. For example, Emotional Well-Being was broadly defined as “Emotional well-being is a state of mind in which the individual realizes his or her own abilities, is able to cope with the stresses of life, and can interact and participate in the community … ”; while the Aim was to initiate routine depression and anxiety screening as their near term goal.
Systematic searches and fishbone (Ishikawa) or Driver diagrams
Systematic searches were conducted by Project Team members (MO and MA) of Medline, Embase, and CINAHL, to identify factors influencing the desired rehabilitation outcomes, and to summarize the available clinimetric properties of published Domain-specific outcome assessment tools. The search results were synthesized and tabulated to facilitate comparison between outcomes, content, and face validity review. In addition, review of available published systematic reviews from SCIRE (scireproject.com) and current clinical practice guidelines relevant to the Canadian context were independently conducted for each Domain. These literature reviews were reviewed and refined by the Working Groups; thereby, providing an overview of the strength of evidence for each Domain.
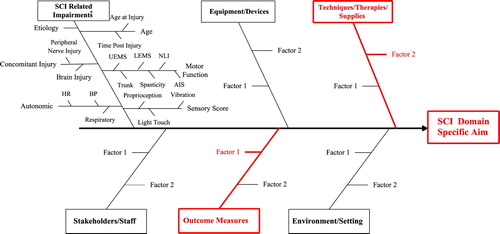
Identify factors relevant to outcomes and display in Driver diagram
The Driver diagram (Ishikawa or fishbone diagram) is one of the seven basic tools of quality control. In this diagram the ‘fish head’ represents the main problem and potential causes of the problem usually derived from brainstorming sessions or literature search, are indicated in the ‘fish bones’.Citation58 The cause and effect or Driver diagrams are a graphic illustration which convey the relationships between the Domain and factors that influence the outcome. These diagrams can be used as a brainstorming tool to identify components of care or care processes that contribute to the outcome of interest.Citation59 All Working Groups used the standard categories in this cause and effect framework that included: Equipment, Process, Personnel, Materials, and Environment, although modifications to the factors were allowed to facilitate the development of a relevant picture for each Domain (see ). The driver diagram and literature syntheses were used to inform the Working Groups selection of the most important and feasible drivers for the Domain-specific outcome.
Figure 6 Typical structure for Driver (Ishikawa) diagram. UEMS: upper-extremity motor score; LEMS: lower-extremity motor score; NLI: neurological level of injury; AIS: ASIA impairment scale; HR: heart rate; BP: blood pressure; * This part of the fishbone is common to all SCI-High project's fishbone diagrams (11 Domains).
Guided by the Domain-specific Driver diagrams and using the RAND/UCLA Appropriateness Method,Citation60 each Working Group was instructed to prioritize the key elements of care that should be measured. The Working Groups used several criteria for selecting the arms of the Driver diagram, including, the strength of the evidence for the factors’ importance, and the extent to which it was within the control of clinicians, At the outset, the Project Team planned to develop and implement a collection of one structure, process and outcome indicator for each Domain. Anticipating that development of a total of 33 indicators across 11 domains would be a substantial burden for clinical programs to implement and wanting to ensure indicator feasibility Working Groups were instructed to develop/select indicators requiring 6–10 min to administer at any time point admission, discharge or 18 months after admission.
Select structure indicator
Structure indicators are measures of the properties or characteristics of the health care setting that are judged to be necessary resources to ensure the quality of care.Citation61 For example, the attributes of the material resources such as facilities, equipment, financial and human resources, as well as organizational resources. Each Working Group was asked to select one structure indicator that could be administered annually. These indicators could be administered by accreditors or self-reported by programs to determine whether there were sufficient resources to provide high-quality care in each Domain.
Select process indicator
Process indicators examine what is actually done in providing and receiving elements of care judged critical to result in the desired outcomes. These are often overlooked as key elements of ensuring quality.Citation1 To select the process indicator, Working Groups were advised to consider measures that could be administered during rehabilitation typically for each patient and should be embedded in day-to-day care. The SCI-High Team stipulated that only one or maximum two process indicators could be selected for each Domain. Some measurements were dichotomous where the answers are “yes” or “no” such as “Completion of the daily head to toe skin check” as a process indicator for the Skin Integrity Domain, and some were more quantitative such as number of minutes of wheelchair skills training.
Select outcome indicator
Outcomes are widely used to evaluate the effects of the health care provided to a given individual or population on long-term health and function.Citation1,Citation14 These indicators are most familiar to SCI/D clinicians and researchers as they have been extensively studied in the SCI/D literature. Typical outcome measures include morbidity, health status, health-related quality of life, and patient/ family/ provider satisfaction.Citation62 An ideal outcome indicator captures the effect of care on the well-being of patients and populations. To ensure feasibility, the SCI-High Project Team stipulated that the outcome indicators for all Domains should be completed within 60 min, ideally using self-report measures, by the individual patient at the 18-month timeframe. An intermediary outcome could be administered at rehabilitation discharge. For both outcome indicators, the experts were strongly encouraged to select published measures with established reliability and validity. The majority of the Domains will require indicator collection at rehabilitation admission, rehabilitation discharge, and 18-months post rehabilitation admission.
Pilot testing
Preliminary testing of the defined indicators and measurement tools helped to determine relative bias, precision, and reliability. Preliminary testing used quality improvement iterative cycles (i.e. Plan-Do-Study-Act cycles, or audit and feedback) that included using small samples of SCI/D individuals or staff (n = 5–10) and rehabilitation centers (n = 1–2), considering eligibility for each indicator.
Finalize definitions and technical aspects of all indicators
The results from these Plan-Do-Study-Act cycles of preliminary testing informed refinement of the constructs and indicators, for different environments to fulfill the SCI-High Project needs not previously identified by the Working Groups. Many operative definitions, diagnostic and treatment thresholds, and interpretations of tools were determined prior to SCI-High tool inclusion.
Stakeholder engagement
Stakeholders participated in the aforementioned prioritization of rehabilitation Domains, and during a formal National Report-Out meeting in November 2017, where stakeholders were presented potential indicators for the prioritized Domains and then asked to rate their importance and feasibility using an audience response system. Following the meeting, administrative leaders from 15 tertiary SCI/D rehabilitation centers participated in telephone interviews to confirm their rankings of Domain importance and feasibility from their organizational perspective. A summary report and executive summary from the National Report-Out meeting is available on the project website (www.sci-high.ca). The feedback from this consultation process was used to refine the indicators prior to publication of the Domain-specific manuscripts, and inform the strategic planning for the order of Domain deployment provincially and nationally.
Results
The aforementioned Working Group processes led to the development of 11 rehabilitation Domain Constructs and Working Group Aims () and 52 indicators derived from the rehabilitation framework (see ). The Cardiometabolic Health, Emotional Well-Being, Tissue Integrity, Sexual Health, UTI, Walking and/or Wheeled Mobility are detailed in separate manuscripts in this issue. These six Domains have been selected for provincial deployment at five sites in Ontario in 2019–2020, and the Cardiometabolic Health indicators will be piloted in Ontario and Quebec in this same time period. The relevant discussions, definitions, literature reviews, and final decisions about outcomes and indicators are outlined in subsequent manuscripts.
Table 1 SCI-High Domains, construct definitions, and aims.
Discussion
To our knowledge, this is the first concerted effort to identify priority indicators of quality care for SCI/D rehabilitation that could be incorporated into usual clinical care. The process benefits from a unique engagement of clinicians, consumers, health care leaders and decision-makers throughout multiple steps in the process. The modified Hanlon methodology provided a rigorous and novel approach to identify and rank key rehabilitation Domains for indicator development from the SCI rehabilitation framework.
Each step in the process led to important developments. The Construct definition process assured Working Group members were clear on the core concept for each Domain. The identification of Aim, and review of related best practices, and existing measures ensured that available relevant outcomes, which were psychometrically sound, and had been tested in the SCI/D population, were reviewed for inclusion. Driver diagram development ensured that all relevant factors that influence outcomes were displayed in an easily comprehensible form and allowed for group consideration of near term rehabilitation priorities. The selection of a structure indicator ensured that the right characteristics and resources are present in the environment to provide high-quality interventions. The process indicators measured key processes that ultimately are critical for the outcomes. The outcome measures selected were chosen because of their feasibility to be administered at rehabilitation discharge and at 18 months after rehabilitation admission to look at the explanatory relationship between the structure and processes of care and how they result in the expected rehabilitation outcomes.
A key strength of the process was the prioritization of Domains for evaluation. Further narrowing of the set of indicators challenged the expert Working Groups to identify key drivers of outcomes and select related measures based on the Driver diagrams. There has been a number of prior initiatives to measure the outcomes of inpatient care.Citation63 Furthermore, given the dearth of evidence-based indicators of quality care, particularly in outpatient settings (i.e. lack of community/long-term follow-up),Citation52 there is a case to be made for the development, implementation, and evaluation of indicators to measure the quality of SCI/D rehabilitation care. An approach to advancing this initiative is to first determine indicators during the early post-discharge stage (i.e. initial 18 months). Currently, the trend of decreasing length-of-stay in tertiary SCI/D rehabilitation centers in North AmericaCitation64 has led to individuals with SCI/D entering the community after a limited time for adjustment to the physical and psychological changes post-injury. Certainly, discharge from inpatient rehabilitation is a crucial transition in the care path for individuals with SCI/D, as well as their informal networks (e.g. family members/caregivers) as there is initial fear and anxiety in attempting to undertake and manage clinical, logistic and organizational issues.Citation65–67 Low-incidence conditions such as SCI do not create enough of a market to support development of specialized services in remote areas.Citation68 Factors threatening sustainability of health services in general include: populations of insufficient in size to support traditional models of care, difficulties recruiting and retaining an adequate health workforce, geographic isolation of individuals living in remote areas, and reliance on periodic visiting services due to insufficient access to rehabilitation centers. Furthermore, most family disintegration and divorce occurs during the early stages of injury when care demands are the highestCitation69–71 due to the challenges in adjusting to new physical functions, creating new normalcy, and maintaining relationships. It is apparent that, at the initial stage of injury (18 months post-discharge), both explicit and implicit needs and challenges arise from individuals with SCI/D, and there is a need to enhance care delivery across the continuum.Citation52
Indicators development is an iterative process
Beyond the initial implementation of indicators, it must be clearly stated that these quality indicators are intended to be iterative in design, and will continually evolve with audit and feedback informing alterations in health service delivery and best practice over time. A benchmark of care is setting a threshold or expectation for quality care of a specific type, magnitude or timing thereby allowing the reviewer to compare their facility’s care to quality benchmarks (peer and national) to identify areas where they are performing well, and those that merit immediate attention and action. As the selected indicators provide relevant evaluative information about the health system, the SCI-High Project Team will conduct ongoing appraisal of the information provided and, as appropriate, refine the indicators and related benchmarks in order to enhance their overall effectiveness. The SCI-High Project Team intends to conduct the appraisal of the indicators at regular, pre-determined time points to harness the capabilities of indicators to create a rapidly responding framework that will create and reinforce a learning health system for individuals with SCI/D living in the community.
Moving from outcomes to health surveillance with indicators
Clinical research falls into the broader field of outcomes research, which sets out to develop knowledge that is useful in guiding health care decisions and optimizing care through preventative, diagnostic, prognostic, and therapeutic interventions. Outcomes research has been a focus of the rehabilitation community and can be categorized into three types: discovery science, application studies (i.e. development, use and evaluation of interventions), and surveillance.Citation72 To date, most of the focus of outcomes research has been on discovery science and application studies. As a result, health care decision-makers have neglected the benefits of health surveillance. Functioning as a learning health system goes beyond data collection and report generation, and involves a continuous monitoring of distributions or trends in indicator outcomes by thoroughly collecting, consolidating and evaluating all relevant information as proposed in the SCI-High Project.Citation73 The outcomes of interest in health surveillance are: health indicators; “a measure designed to summarize information about a given priority topic in population health or health system performance.”Citation64 The goal of health indicators is to “provide comparable and actionable information across different geographic, organizational or administrative boundaries and/or can track progress over time.”Citation64 This is differentiated from metrics collected in most application studies because indicators are comparable through adjustment or standardization; by placing the information into context.Citation64 The current impact of outcomes research on the quality of rehabilitation care for the SCI/D population is unknown. However, with few resources dedicated to health surveillance following rehabilitation discharge, there is no doubt that the benefits of this type of initiative are not being maximized. Thus, increased resources invested into the development of a more sophisticated rehabilitation surveillance system through the use of rehabilitation indicators has the potential to rapidly augment the quality of care and wellbeing of the SCI/D population.
Some limitations are worthy of discussion prior to generalizing the indicators. First, since there are numerous indicators for the 11 prioritized Domains, the Working Group attempted to choose the most feasible indicators; therefore, it is possible that the selected indicators may not be optimal for health care assessment. Second, aspects of care assessed by indicators must relate to enough patients to ensure data comparison is feasible. However, as SCI/D is a rare event,Citation74 feasibility testing and implication of these indicators for comparison would be difficult, due to small sample sizes and heterogeneity in impairment within the SCI/D population. Finally, we used a limited group of experts (a minimum of 12 and a maximum 17 members) for each Domain; thus, it is possible that a different group of experts might disagree on the Construct definition and selected indicators. To address this problem, we plan to measure the reliability and validity of the indicators for quality improvement over time.
In terms of next steps, these indicators alone are meaningless without appropriate interpretation and suitable actions taken to improve priority setting, policy formulation, and care processes. A sustained effort to enhance care processes and implement the indicators in a variety of sites will be required. The widespread implementation and collection of the indicators will allow the development of achievable benchmarks of care as similarly developed for stroke care.Citation51 Implementation tools for the indicators will also be critical. Some Domain-specific Working Groups developed flow diagrams for clinical implementation, for example, screening of depression and anxiety, or dyslipidemia. We also partnered with consumer advocacy groups: the Ontario SCI network and the Ontario SCI Alliance. These two groups will facilitate the creation of site-specific methodologies for indicator implementation, creation, and adoption of best clinical practices, and the approximation between the SCI-High goals and consumer’s priorities. We expect that the appropriate measurement of indicators will help to understand gaps in SCI/D rehabilitation care and identify strengths and weaknesses of each rehabilitation program. In this context, strengths can be shared between different sites with the long-term aim of increasing equity in healthcare. Therefore, timely and transparent reporting of indicators is key to success. There is also an opportunity to link the indicators with the HSO and Accreditation Canada for the development of a distinction program, creating an environment where indicator data collection becomes a routine part of day-to-day practices.
HSO and Accreditation Canada
The HSO is a group that is focused on constructing standards and assessment methodologies (e.g. instruments, benchmarking, training, and coaching) to improve health care quality.Citation69 Standards are developed using the highest quality evidence available and with the collaboration of policymakers, clinicians, health care providers, patients, patient family members, and community leaders.Citation68 These standards are then used by Accreditation Canada to form a basis for evaluating whether health and social service organizations meet a level of excellence in delivering services to individuals in need of care. Through their accreditation program, Accreditation Canada provides confirmation that an organization has achieved or exceeded the standards set by HSO.Citation67 The goal of providing accreditation is to promote an organizational culture of improvement that will result in improved safety and efficiency and outcomes of care.Citation70 Accreditation Canada has an established Trauma Distinction and Stroke Distinction program, for trauma and stroke organizations. Organizations with an “Accredited” status can achieve Distinction if they meet trauma/stroke specific standards, and meet the threshold for specific performance indicators, have care protocols in place, and are involved with a project or initiative that has enhanced the quality of services delivered.Citation75 The performance indicators of the Trauma Distinction Program are the foundation for the development of a revised Distinction program that will be more relevant to the SCI population.Citation65 The Rick Hansen Institute will facilitate this planned future work of HSO and Accreditation Canada through the Access to Care and Timing Workshop. The development of an SCI-specific Distinction Program is part of a national strategy to improve the care of Canadians with SCI/D.Citation65 The SCI-High Project is well positioned to inform a future distinction program based on the planned development of benchmarks for the prioritized Domains of SCI/D rehabilitation care.
Looking to the future
The indicators resulting from the described processes, are intended for implementation in a Canadian “universal payer” health system, and may not be appropriate in other SCI/D settings. The current changing demographics of the adult SCI/D population (rising incidence of non-traumatic injury) and the associated increased service demands of individuals with incomplete injuries and a good prognosis for neurological recovery, are likely to challenge and potentially overwhelm rehabilitation resources in our resource-constrained health system, with requests to provide (1) an adequate volume of therapy within appropriate timeframes, and (2) services for those aging with secondary health conditions. The economic resource requirements for the developed indicators has yet to be developed. The developed indicators are intended to capture changes in processes of care and the health outcomes of patients’ with SCI/D, as they transition to community living. Although the incidence of SCI is relatively low: in 2010 only 3,675 new cases occurred in Canada (estimated prevalence of 85,556), with 40% of this population residing in the province of Ontario.Citation74 However, the mean five-year (2005–2010) direct health system costs of incident SCI cases in Ontario was $213,800 CAD, and the direct lifetime costs for SCI onset at age 25, range from $2.1 to 5.4 million USD depending on injury severity.Citation76 Thus, SCI/D is a complex, relatively rare condition, with substantial adverse personal, health system and economic impacts for which implementation of quality indicators are urgently needed to advance accountability, transparency and rehabilitation care for stakeholders through implementation of audit and feedback relative to evolving health system structure, process and outcome benchmarks in the next decade.
Conclusion
The results from this process can be used for different purposes, including assessing the quality of care provided to individuals and populations with SCI/D within and across health care settings and monitoring the effects of changes on patients’ health status. Using these indicators for evaluating rehabilitation care can ensure continuous quality improvement (i.e. benchmarking) and ultimately lead to evidence-based advances in SCI/D rehabilitation practice and improvements in healthcare equity.
Disclaimer statements
Conflicts of interest Dr. Mark Bayley acknowledges support from the Saunderson Family Chair in Acquired Brain Injury Research, the Toronto Rehab Chair in SCI Rehabilitation, and the Toronto Rehab Foundation. Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation and receipt of consulting fees from the Rick Hansen Institute. Dr. S. Mohammad Alavinia, Farnoosh Farahani, Heather Flett, Dr. Sander L. Hitzig, Dr. Gaya Jeyathevan, Maryam Omidvar and Dr. Matheus J. Wiest report no conflicts of interest.
Acknowledgments
We wish to acknowledge the knowledge, expertise and volunteer services of the members of the External Advisory Committee and Domain-specific Working Groups, the leadership team, and staff and patients affiliated with the Toronto Rehab Spinal Cord Rehabilitation Program. We want to thank Maureen Pakosh University Health Network librarian for her time, energy, and valuable contributions to the systematic literature searches, and Joanne Zee for her administrative willingness to tackle advances in quality care. We wish to acknowledge the assistance of Victoria Kim and Eleni Patsakos for their assistance in producing the diagrams contained within this manuscript.
ORCID
B. Catharine Craven http://orcid.org/0000-0001-8234-6803
S. Mohammad Alavinia http://orcid.org/0000-0002-5503-9362
Matheus J. Wiest http://orcid.org/0000-0003-1444-4828
Farnoosh Farahani http://orcid.org/0000-0002-3937-7708
Sander L. Hitzig http://orcid.org/0000-0002-9139-9250
Heather Flett http://orcid.org/0000-0001-9444-8006
Gaya Jeyathevan http://orcid.org/0000-0001-5525-3214
Maryam Omidvar http://orcid.org/0000-0003-2415-8921
Mark T. Bayley http://orcid.org/0000-0001-7860-9463
Additional information
Funding
References
- Runciman W, Hibbert P, Thomson R, Van Der Schaaf T, Sherman H, Lewalle P. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care. 2009;21(1):18–26. doi: 10.1093/intqhc/mzn057
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press (US). 2001.
- Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ Open. 2015;5(9):e008592. doi: 10.1136/bmjopen-2015-008592
- Tuti T, Nzinga J, Njoroge M, Brown B, Peek N, English M, et al. A systematic review of electronic audit and feedback: intervention effectiveness and use of behaviour change theory. Implement Sci. 2017;12(1):61. doi: 10.1186/s13012-017-0590-z
- Ivers NM, Grimshaw JM, Jamtvedt G, Flottorp S, O'Brien MA, French SD, et al. Growing literature, stagnant science? Systematic review, meta-regression and cumulative analysis of audit and feedback interventions in health care. J Gen Intern Med. 2014;29(11):1534–1541. doi: 10.1007/s11606-014-2913-y
- Duncan PW, Horner RD, Reker DM, Samsa GP, Hoenig H, Hamilton B, et al. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke. 2002;33(1):167–177. doi: 10.1161/hs0102.101014
- Lindsay MP, Kapral MK, Gladstone D, Holloway R, Tu JV, Laupacis A, et al. The Canadian stroke quality of care Study: establishing indicators for optimal acute stroke care. CMAJ. 2005;172(3):363–365. doi: 10.1503/cmaj.045310
- Kowalski C, Schulte H, Wesselmann S. Reporting program for cancer care quality indicators. J Oncol Pract. 2015;11(2):158–160. doi: 10.1200/JOP.2014.001339
- Aron DC. Quality indicators and performance measures in diabetes care. Curr Diab Rep. 2014;14(3):472. doi: 10.1007/s11892-013-0472-y
- Canadian Institute for Health Information. Cardiac Care Quality Indicators Report. Ottawa, ON: CIHI. 2017.
- Grube MM, Dohle C, Djouchadar D, Rech P, Bienek K, Dietz-Fricke U, et al. Evidence-based quality indicators for stroke rehabilitation. Stroke. 2012;43(1):142–146. doi: 10.1161/STROKEAHA.111.627679
- Hall RE TA, Khan F, McCormack D, Levi J, Verrilli S, Quant S, et al. Ontario Stroke Evaluation Report 2018: Stroke Care and Outcomes in Complex Continuing Care and Long-Term Care. Toronto, ON: Institute for Clinical Evaluative Sciences/CorHealth Ontario. 2018.
- Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res. 2001;11(6):795–811. doi: 10.1177/104973201129119541
- Guilcher SJ, Parsons D, Craven BC, Jaglal SB, Verrier M. Developing quality of care indicators for patients with traumatic and non-traumatic spinal cord injury (SCI): a feasibility study using administrative health data. J Spinal Cord Med. 2015;38(6):765–776. doi: 10.1179/2045772315Y.0000000043
- Fehlings MG, Cheng CL, Chan E, Thorogood NP, Noonan VK, Ahn H, et al. Using evidence to inform practice and policy to enhance the quality of care for persons with traumatic spinal cord injury. J Neurotrauma. 2017;34(20):2934–2940. doi: 10.1089/neu.2016.4938
- Hagglund K, Clay D, Acuff M. Community reintegration for persons with spinal cord injury living in rural America. Top Spinal Cord Inj Rehabil. 1998;4(2):28–40. doi: 10.1310/3502-06MD-F2NK-LBGK
- Stadhouder A, Buckens CF, Holtslag HR, Oner FC. Are existing outcome instruments suitable for assessment of spinal trauma patients? J Neurosurg Spine. 2010;13(5):638–647. doi: 10.3171/2010.5.SPINE09128
- The Qmentum Accreditation Process, Standards Spinal Cord Injury Rehabilitation Services. [Internet]. Accreditation Canada. Available from https://accreditation.ca/accreditation/process/.
- https://healthstandards.org/about/. [Internet]. Health Standards Organization. Available from https://healthstandards.org/about/.
- Accreditation Canada. Available from: https://accreditation.ca/.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care. 2003;15(Suppl 1):i5–11. doi: 10.1093/intqhc/mzg084
- Bianchi V, Spitale A, Ortelli L, Mazzucchelli L, Bordoni A, Group QCW. Quality indicators of clinical cancer care (QC3) in colorectal cancer. BMJ Open. 2013;3(7): pii: e002818. doi: 10.1136/bmjopen-2013-002818
- Whiteneck G, Gassaway J, Dijkers M, Jha A. New approach to study the contents and outcomes of spinal cord injury rehabilitation: the SCIRehab Project. J Spinal Cord Med. 2009;32(3):251–259. doi: 10.1080/10790268.2009.11760779
- Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371–1383. doi: 10.1089/neu.2004.21.1371
- Van Middendorp JJ, Allison HC, Ahuja S, Bracher D, Dyson C, Fairbank J, et al. Top ten research priorities for spinal cord injury: the methodology and results of a British priority setting partnership. Spinal Cord. 2016;54(5):341–346. doi: 10.1038/sc.2015.199
- Alavinia SM, Hitzig SL, Farahani F, Flett H, Bayley M, Craven BC. Prioritization of rehabilitation Domains for establishing spinal cord injury high performance indicators using a modification of the Hanlon method: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S43–S50.
- Bayley MT, Kirby RL, Titus L, Smith C, Routhier F, Gagnon D, et al. Development of Wheeled Mobility indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S130–S140.
- Craven BC, Alavinia SM, Gajewski JB, Parmar R, Disher S, Ethans K, et al. Conception and development of Urinary Tract Infection indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S205–S214.
- Elliott S, Jeyathevan G, Hocalski S, O’Connell C, Gulasingam S, Mills S, et al. Conception and development of Sexual Health indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S68–S84.
- Flett H, Wiest MJ, Mushahwar V, Ho C, Hsieh J, Farahani F, et al. Development of Tissue Integrity quality indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S196–S204.
- Hitzig SL, Titman R, Orenczuk S, Clarke T, Flett H, Vanessa N, et al. Development of Emotional Well-Being indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S85–S98.
- Wiest MJ, West C, Ditor D, Furlan J, Miyatani M, Farahani F, et al. Development of Cardiometabolic Health indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S166–S175.
- Musselman K, Verrier M, Flett H, Nadeau S, Yang JF, Farahani F, et al. Development of Walking indicators to advance the quality of spinal cord injury rehabilitation: SCI-High Project. J Spinal Cord Med. 2019;42(Suppl 1):S119–S129.
- Craven BC, Verrier M, Balioussis C, Wolfe D PhD, Hsieh J, Noonan V, et al. rehabilitation environmental scan atlas: capturing capacity in Canadian SCI Rehabilitation; Rick Hansen Institute; 2012. Available from http://rickhanseninstitute.org/e-scan-atlas.
- Craven C, Balioussis C, Verrier MC, Hsieh JT, Cherban E, Rasheed A, et al. Using scoping review methods to describe current capacity and prescribe change in Canadian SCI Rehabilitation service delivery. J Spinal Cord Med. 2012;35(5):392–399. doi: 10.1179/2045772312Y.0000000045
- WHO. How to use the ICF: a practical manual for using the International Classification of Functioning, disability and health (ICF). Exposure draft for comment. Geneva: World Health Organization; October 2013.
- Craven B, Balioussis C, Verrier MM, and the E-Scan Investigative Team. The tipping point: perspectives on SCI rehabilitation service gaps in Canada. Int J Phys Med Rehabil. 2013;1(8):165. doi: 10.4172/2329-9096.1000165
- Hanlon J, Pickett G. Public health administration and practice. 8th ed. St. Louis: C.V. Mosby; 1984.
- Langley GM, Nolan K, Nolan T, Norman C, Provost L. The improvement guide: A practical approach to Enhancing organizational performance. 2nd ed. San Francisco, CA: Jossey-Bass; April 2009.
- Musselman KE, Lemay JF, Walden K, Harris A, Gagnon D, Verrier M. The standing and walking assessment tool for individuals with spinal cord injury: a qualitative study of validity and implementation. J Spinal Cord Med. 2019;42(Suppl 1):S108–S118.
- Scovil CY, Delparte JJ, Walia S, Flett HM, Guy SD, Wallace M, et al. Implementation of pressure injury prevention best practices across six Canadian rehabilitation sites: results from the Spinal Cord Injury Knowledge Mobilization Network. Arch Phys Med Rehabil. 2019;100(2):327–335. doi: 10.1016/j.apmr.2018.07.444
- Noonan VK, Thorogood NP, Joshi PB, Fehlings MG, Craven BC, Linassi G, et al. Meeting the privacy requirements for the development of a multi-centre patient registry in Canada: the Rick Hansen Spinal Cord Injury Registry. Healthc Policy. 2013;8(4):87–99.
- Welk B. The Canadian Spinal Cord Injury Urohealth Summit, Final report 2017. Available from: http://onf.org/system/attachments/476/original/SCI_Urohealth_Summit.pdf.
- Houghton P. The E-Stim collaboration project: a national pressure ulcer implementation program. Wound Care Canada. 2018;16(1). Available from https://www.woundscanada.ca/docman/public/wound-care-canada-magazine/2018-16-no1/1270-wcc-summer-2018-v16n1-final-p-44-49-e-stim/file.
- Titman R, Liang J, Craven BC. Diagnostic accuracy and feasibility of depression screening in spinal cord injury: a systematic review. J Spinal Cord Med; 2019;42(Suppl 1):S99–S107. DOI:10.1080/10790268.2019.1606556].
- Noonan VK, Kwon BK, Soril L, Fehlings MG, Hurlbert RJ, Townson A, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50(1):22–27. doi: 10.1038/sc.2011.109
- Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34(6):535–546. doi: 10.1179/204577211X13207446293695
- Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29(24):1926–1933. doi: 10.1080/09638280601046302
- Ho C, Guilcher SJT, McKenzie N, Mouneimne M, Williams A, Voth J, et al. Validation of algorithm to identify persons with non-traumatic spinal cord dysfunction in Canada using administrative health data. Top Spinal Cord Inj Rehabil. 2017;23(4):333–342. doi: 10.1310/sci2304-333
- Guilcher SJT, Voth J, Ho C, Noonan VK, McKenzie N, Thorogood NP, et al. Characteristics of non-traumatic spinal cord dysfunction in Canada using administrative health data. Top Spinal Cord Inj Rehabil. 2017;23(4):343–352. doi: 10.1310/sci2304-343
- Jaglal SB, Voth J, Guilcher SJT, Ho C, Noonan VK, McKenzie N, et al. Creation of an algorithm to identify non-traumatic spinal cord dysfunction patients in Canada using administrative health data. Top Spinal Cord Inj Rehabil. 2017;23(4):324–332. doi: 10.1310/sci2304-324
- Rowan CP, Chan BCF, Jaglal SB, Craven BC. Describing the current state of postrehabilitation health system surveillance in Ontario – an invited review. J Spinal Cord Med. 2019;42(Suppl 1):S21–S33. doi:10.1080/10790268.2019.1605724.
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord. 2013;51(2):165–169. doi: 10.1038/sc.2012.91
- Craven B C, Kurban D, Farahani F, Rivers CS, Ho C, Linassi AG, et al. Predicting rehabilitation length of stay in Canada: it’s not just about impairment. J Spinal Cord Med. 2017;40(6):676–686. doi: 10.1080/10790268.2017.1368962
- Kreuter M. Spinal cord injury and partner relationships. Spinal Cord. 2000;38(1):2–6. doi: 10.1038/sj.sc.3100933
- Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, et al. Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS One. 2017;12(1):e0169623. doi: 10.1371/journal.pone.0169623
- Craig A, Nicholson Perry K, Guest R, Tran Y, Middleton J. Adjustment following chronic spinal cord injury: determining factors that contribute to social participation. Br J Health Psychol. 2015;20(4):807–823. doi: 10.1111/bjhp.12143
- Wong KC. Using an Ishikawa diagram as a tool to assist memory and retrieval of relevant medical cases from the medical literature. J Med Case Rep. 2011;5(120):1–3.
- Tomson CR, van der Veer SN. Learning from practice variation to improve the quality of care. Clin Med Lond. 2013;13(1):19–23. doi: 10.7861/clinmedicine.13-1-19
- Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR. The RAND/UCLA appropriateness method user’s manual. Available from https://apps.dtic.mil/dtic/tr/fulltext/u2/a393235.pdf. 2001.
- Idvall E, Rooke L, Hamrin E. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs. 1997;25(1):6–17. doi: 10.1046/j.1365-2648.1997.1997025006.x
- Kruk ME, Freedman LP. Assessing health system performance in developing countries: a review of the literature. Health Policy. 2008;85(3):263–276. doi: 10.1016/j.healthpol.2007.09.003
- Whiteneck GG, Gassaway J. SCIRehab uses practice-based evidence methodology to associate patient and treatment characteristics with outcomes. Arch Phys Med Rehabil. 2013;94(4 Suppl):S67–S74. doi: 10.1016/j.apmr.2012.12.022
- Whiteneck G, Gassaway J, Dijkers M, Backus D, Charlifue S, Chen D, et al. The SCIRehab project: treatment time spent in SCI rehabilitation. Inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med. 2011;34(2):133–148. doi: 10.1179/107902611X12971826988011
- Lucke KT, Coccia H, Goode JS, Lucke JF. Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res. 2004;13(1):97–110. doi: 10.1023/B:QURE.0000015284.95515.17
- Marini MG, Reale L. Bisogni e costi delle persone con lesione midollare e dei nuclei familiari di riferimento. IAS. 2010.
- Schulz R, Czaja SJ, Lustig A, Zdaniuk B, Martire LM, Perdomo D. Improving the quality of life of caregivers of persons with spinal cord injury: a randomized controlled trial. Rehabil Psychol. 2009;54(1):1–15. doi: 10.1037/a0014932
- Middleton JW, McCormick M, Engel S, Rutkowski SB, Cameron ID, Harradine P, et al. Issues and challenges for development of a sustainable service model for people with spinal cord injury living in rural regions. Arch Phys Med Rehabil. 2008;89(10):1941–1947. doi: 10.1016/j.apmr.2008.04.011
- Chan RC. Stress and coping in spouses of persons with spinal cord injuries. Clin Rehabil. 2000;14(2):137–144. doi: 10.1191/026921500675826560
- DeVivo MJ, Hawkins LN, Richards JS, Go BK. Outcomes of post-spinal cord injury marriages. Arch Phys Med Rehabil. 1995;76(2):130–138. doi: 10.1016/S0003-9993(95)80022-0
- Kreuter M, Sullivan M, Dahllof AG, Siosteen A. Partner relationships, functioning, mood and global quality of life in persons with spinal cord injury and traumatic brain injury. Spinal Cord. 1998;36(4):252–261. doi: 10.1038/sj.sc.3100592
- Krumholz HM. Real-world imperative of outcomes research. JAMA. 2011;306(7):754–755. doi: 10.1001/jama.2011.1170
- Langmuir AD. The surveillance of communicable diseases of national importance. N Engl J Med. 1963;268:182–192. doi: 10.1056/NEJM196301242680405
- Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology. 2012;38(4):219–226. doi: 10.1159/000336014
- Trauma Distinction Information Package: Accreditation Canada. 2014. Available from https://accreditation.ca/files/trauma-info-package-en.pdf.
- Shavelle R, T Katz R, MacKenzie R, Rosenbloom L, DeVivo M, Hutton J, et al. Life expectancy for people with disabilities 2011. p. 161.
- WHO. Defining sexual health: report of a technical consultation on sexual health. Geneva: World Health Organization; 2002.