Abstract
Introduction
Spinal cord injury (SCI) is a life-altering injury that leads to a complex constellation of changes in an individual’s sensory, motor, and autonomic function which is largely determined by the level and severity of cord impairment. Available SCI-specific clinical practice guidelines (CPG) address specific impairments, health conditions or a segment of the care continuum, however, fail to address all the important clinical questions arising throughout an individual’s care journey. To address this gap, an interprofessional panel of experts in SCI convened to develop the Canadian Spinal Cord Injury Best Practice (Can-SCIP) Guideline. This article provides an overview of the methods underpinning the Can-SCIP Guideline process.
Methods
The Can-SCIP Guideline was developed using the Guidelines Adaptation Cycle. A comprehensive search for existing SCI-specific CPGs was conducted. The quality of eligible CPGs was evaluated using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) instrument. An expert panel (n = 52) convened, and groups of relevant experts met to review and recommend adoption or refinement of existing recommendations or develop new recommendations based on evidence from systematic reviews conducted by the Spinal Cord Injury Research Evidence (SCIRE) team. The expert panel voted to approve selected recommendations using an online survey tool.
Results
The Can-SCIP Guideline includes 585 total recommendations from 41 guidelines, 96 recommendations that pertain to the Components of the Ideal SCI Care System section, and 489 recommendations that pertain to the Management of Secondary Health Conditions section. Most recommendations (n = 281, 48%) were adopted from existing guidelines without revision, 215 (36.8%) recommendations were revised for application in a Canadian context, and 89 recommendations (15.2%) were created de novo.
Conclusion
The Can-SCIP Guideline is the first living comprehensive guideline for adults with SCI in Canada across the care continuum.
Introduction
Spinal cord injury (SCI) is a life-altering injury that leads to complex changes in sensory, motor, and autonomic function, significantly affecting an individual’s emotional wellbeing, quality of life, community participation, functional abilities, health and life expectancy.Citation1–5 Specialized acute, rehabilitation, and community-based healthcare that necessitates the provision of the best available interprofessional care from time of injury onset and throughout the balance of the individual’s lifetime is required. Further, challenges within the field of SCI internationally include: ongoing difficulties in funding and accruing an adequate sample size within clinical trials, hampering the ability to generate Level I evidence to meet regulatory requirements and inform practice.Citation6,Citation7 A concern within healthcare settings is the underutilization of research by healthcare professionalsCitation8 and the clinical equipoise regarding how best to diagnose or treat patients with complex biopsychosocial issues and medical morbidity such as individuals living with SCI.
Although there is a large and expanding body of clinical research directed toward improving patient care, thirty to forty percent of patients do not receive appropriate evidence-based care.Citation9,Citation10 As the volume of research evidence is rapidly increasing, it is challenging for healthcare professionals to remain informed on the latest research and related clinical recommendations across care domains.Citation8 Clinical Practice Guidelines (CPGs) play an important role in bridging this knowledge gap. CPGs are knowledge tools that assist evidence-based decision-making and are comprised of systematically developed statements that promote high-quality practice across the continuum of care. Evidence-informed practice recommendations within CPGs can reduce practice variation, improve the quality of care, and assist healthcare professionals in making clinical decisions based on evidence and advancing practice.Citation11–13
Within the field of SCI research, existing CPGs focus on specific individual impairments (i.e. skin integrity, bowel management) or a single segment of the care continuum (i.e. prehospital care, MRI diagnosis, surgical intervention, community participation) and do not address all the important clinical questions which arise for individuals throughout an individual’s care journey. Furthermore, few guidelines provide recommendations for all members of the interprofessional care team that are tailored to the individual’s level of injury and severity of injury (i.e. American Spinal Injury Association Impairment Scale, AIS). A CPG that identifies best practices across the entire SCI care continuum is needed.
CPGs with the greatest potential to influence systems of care, in addition to quality care recommendations, should contain recommendations tailored for specific stakeholders including but not limited to healthcare administrators, policymakers and individuals with lived experience. Although well intended, CPGs can adversely affect public policy for patients. For example, recommendations against an intervention may lead service providers and or healthcare funders to reduce access to the intervention and/or withdraw funding for the product or service in a single payer health system. Also, recommendations for costly interventions that are hardly feasible may displace the resources needed for other services (across the care continuum) of greater value to patients in a single payer health system.
Recognizing these aforementioned challenges and limitations, we sought to develop a living guideline that is continuously updated. The Can-SCIP Guideline is the first comprehensive living guideline for adults with SCI in Canada. This article describes the methodology used for the development of the Can-SCIP Guideline intended to highlight its’ unique features and rigor throughout development.
Methods
Scope and purpose of the Can-SCIP guideline
The Can-SCIP Guideline process was initiated by formation of an interprofessional steering committee who through a collaborative process defined the scope and target audience for the Guideline. The Can-SCIP steering committee was comprised of clinicians, program leaders, knowledge translation experts, researchers, and administrators. The Can-SCIP Guideline is designed to provide evidence-based recommendations for adults 18 years and older with a SCI in all phases of care (from pre-hospital emergency care through acute and rehabilitation care and on to community care), across an individual’s lifetime. The majority of the identified recommendations were obtained from the traumatic SCI literature, acknowledging that some recommendations would only be applicable to the care of individuals with SCI of either traumatic or non-traumatic etiology, within the latter parts of the care continuum such as the rehabilitation and community care aspects of the guideline. The Can-SCIP steering committee agreed that the selected recommendations should be divided into two sections: (1) Components of the Ideal SCI Care System; and (2) Management of Secondary Health Conditions. The key secondary health conditions identified for recommendation development was derived from a 2017 national consensus process.Citation14 The Spinal Cord Injury-High Performance Indicator (SCI-HIGH) Project team identified 11 domains of rehabilitation care where gaps between knowledge generation and clinical practice implementation that were important to clinicians and people with SCI for enhancing care and developing quality indicators existed.Citation14 Neuropathic pain was an additional health condition among the top health conditions in SCI considered.Citation15
Target users
The intended audience of the Can-SCIP Guideline are clinicians, allied healthcare providers, support workers, persons with SCI and their caregivers, administrators, and policy makers. The primary users of the Components of the Ideal SCI Care System section are policy makers and administrators, while the primary users of the Management of Secondary Health Conditions section are healthcare providers, individuals with lived experience and their caregivers. The recommendations are intended to specify feasible single or multimodal interventions that are evidence-informed for an individual based on their spinal cord impairment (neurologic level of injury, AIS, cord syndrome and type of bowel and bladder impairment) within the Canadian healthcare context.
Guideline development cycle
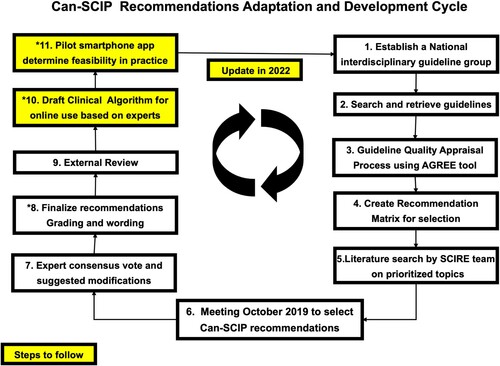
The Can-SCIP Guideline was developed using the Guidelines Adaptation Cycle (ADAPTE) (www.adapte.org) originally derived and modified from a process developed by Graham & Harrison (2005). The steps involved in the process are outlined in and were as follows:
Establish an expert panel: The Can-SCIP expert panel includes clinicians, individuals with lived experience, program directors, knowledge translation experts, researchers, and administrators and other relevant stakeholders (Appendix 1).
Search and retrieval of previously published guidelines: A systematic scoping review was undertaken for CPGs focused on treatment and evidence-based recommendations in the field of SCI. The Can-SCIP steering committee consulted with the Health Sciences Librarian at University of British Columbia to assist with construction of the search. The following databases were searched: PubMed, Medline, Embase, CINAHL, and PsycINFO. In addition, indexes and databases that specifically archive clinical guidelines and medical evidence were also included in the search (NCCIH Clearinghouse,Citation16 Clinical Key,Citation17 Trip Medical Database,Citation18 DynaMed Plus,Citation19 Scottish Intercollegiate Guidelines Network,Citation20 CADTH Grey Matters tool,Citation21 Guidelines International Network,Citation22 and Physiotherapy Evidence Database Ratings).Citation23 The key search terms included ‘spinal cord injury’, ‘spinal cord dysfunction’, ‘tetraplegia’, ‘quadriplegia’, ‘paraplegia’, ‘spinal cord impaired’, ‘spinal cord lesion’ (including truncations of these SCI terms) and ‘clinical practice guidelines’. CPGs published between 2011 and 2018 in English or French, written by four or more authors, applicable to the Canadian health care setting, including evidence-based recommendations for adults over 18 years of age were considered for inclusion. Systematic reviews were excluded, and shorter evidence-based documents were excluded, but their reference lists were hand-searched to find any additional clinical practice guidelines for inclusion. The Can-SCIP steering committee reviewed the existing SCI guidelines to ensure the content of the guideline would be consistent with planned scope of the CPG and to ensure the extracted recommendations could be adapted to the Canadian healthcare context (i.e. health system structure, payor model, available expertise etc.). In addition, the Can-SCIP steering committee reached out to stakeholder organizations to identify CPGs that were currently in development.
Guideline quality appraisal process using AGREE instrument: Each eligible CPG was then evaluated individually by two to four appraisers from the expert panel and/or Can-SCIP steering committee, using the Appraisal of Guidelines for Research and Evaluation II instrument (AGREE II; https://www.agreecollaboration.org). The AGREE II instrument evaluates the guideline development process and quality of the guideline across six domains including: (1) scope and purpose, (2) stakeholder involvement, (3) rigor of development, (4) clarity of presentation, (5) applicability, and (6) editorial independence. Training sessions were held by one of the authors (MB) to ensure all experts were familiar with using the AGREE instrument. Each CPG was given a standardized score ranging from 1 to 100 (100 representing a strong score) by the reviewing appraiser from the expert panel. The AGREE ratings for the selected CPGs are shown elsewhere in this issue.Citation24 As the AGREE User Manual does not specify a minimum score that is considered ‘low-quality,’ the Can-SCIP steering committee set a benchmark of 40% for inclusion; whereby scores higher than 40% represent higher quality, and scores below 40% represent poorer quality. CPGs with an AGREE score below 40% were excluded from the recommendation review process.
Create a recommendation matrix for selection of CPG recommendations: A recommendations matrix was created to facilitate a comparison of the similar or overlapping recommendations across all included CPGs. The CPG recommendations and evidence statements obtained from SCIRE were divided into twenty-four domains relevant to SCI care and treatment within the matrix (). As various evidence grading systems were used across the different selected CPGs, the Can-SCIP steering committee used a standardized grading system () also used in previous CPG development projects.Citation25
Literature search by SCIRE team on prioritized topics: The search processes were enhanced by systematic searches of the SCI literature conducted by the Spinal Cord Injury Research Evidence (SCIRE) project team (https://scireproject.com/) to ensure the incorporated recommendations are based on the most current evidence. Evidence statements formulated by the SCIRE project team were added to the synthesized materials prior to convening the entire expert panel to facilitate the formulation of de novo recommendations when there were not existing recommendations, or where the existing guidelines were outdated, insufficient or not relevant to the Canadian context.
Consensus Meeting to select and/or adapt Can-SCIP recommendations from published recommendations or develop new ones: The expert panel was convened in a two-day meeting prior to the Canadian Spinal Cord Injury Rehabilitation Association (CSCI-RA) 8th National Conference in Niagara Falls, Ontario, Canada, in October 2019. All expert panel members completed declarations of conflicts of interests. The expert panel members were invited to review domains in which they had established expertise or a unique perspective to contribute. Fifty expert panel members reviewed the recommendations matrix independently prior to the consensus meeting and in small working groups during the meeting. At least two individuals with lived experience with SCI were included within each working group to ensure their views were considered. The key activities undertaken by the expert panel members at the consensus conference were to:
Review the quality assessment of previously published best practice guidelines in the SCI field.
Consider the evidence tables derived from the SCIRE systematic review.
Draft or refine recommendations: Each working group selected recommendations from existing CPGs for inclusion, modification or refinement of existing recommendations based on current evidence (i.e. rewording with Canadian terminology, separated some lengthy recommendations into two separate recommendations), or developed new recommendations based on the most current evidence provided by the SCIRE Project. New recommendations with consensus support were also articulated by the experts in each working group. The working groups reviewed recommendations within each domain. In summary, the recommendations were either adopted with the original wording or revised/reworded based on current evidence/settings.
Assign a level of evidence: The experts reviewed the recommendations and supporting evidence and assigned one of 3 levels of evidence as outlined in .
Individualize guidance: For each selected recommendation, the working group specified (i) the section of the care continuum the recommendations applies to (pre-hospital, acute & surgical, tertiary rehabilitation, community), (ii) the neurological level of injury and AIS to which the recommendation applies, (iii) whether the recommendation applies to an individual with a specific cord syndrome – central cord syndrome, anterior cord syndrome, posterior cord syndrome, Brown-Séquard syndrome or cauda equina syndrome; and, (iv) whether the recommendation applies to a person with an upper motor neuron neurogenic bowel or bladder, and (v) whether there were any groups for whom the recommendation does not apply (Appendix 2).
Identify potential implementation toolkits/resources to assist with implementation. Experts were asked to provide lists of websites, publications, decision rules and other implementation tools that could be used to facilitate recommendation uptake.
Expert consensus vote and final modification suggestions: The expert panel voted on all the recommendations using an online survey tool (Survey Monkey®) (Appendix 2). For each recommendation, the expert panel selected whether the recommend should be included within the Can-SCIP Guideline, whether the recommendation should not be included in the Can-SCIP Guideline, or whether the recommendation should be included in the Can-SCIP Guideline but that further modifications were necessary. Recommendations with less than 80% agreement were excluded from the Can-SCIP Guideline.
Finalize recommendation grading and wording: The Can-SCIP steering committee adapted and refined each draft recommendation based on the feedback received from the expert panel and the established format for the recommendations based on the weight of the evidence underpinning the recommendation.
External review: As part of the validation process, the Can-SCIP Guideline was externally reviewed by recognized international experts in SCI who did not participate in the Can-SCIP Guideline development process (n = 8) (Appendix 3). The purpose of conducting the external review was to gather information on both the reviewer’s overall impression of the Guideline and specific comments addressing the following issues: validity, relevance, awareness of new information, evidence or concerns, scope and purpose, stakeholder involvement, rigor of the methods and clarity of presentation according to some questions from the AGREE II instrument. The steering committee considered revisions to the Can-SCIP Guideline based on the suggestions and comments from the external reviewers, feedback from the expert panel and the CPG aims and structure.
Table 1 Section 1 & 2 domains.
Table 2 Summary of criteria for levels of evidence reported in the Can-SCIP guideline.
Upcoming steps and plans for implementation
Draft clinical algorithm for online use based on experts: To facilitate clinical implementation, multiple algorithms will be drafted to provide clinicians with relevant recommendations for the individual patient based on considerations such as neurological level of injury, AIS and nature of bladder impairment. These algorithms will be incorporated into a web-based application formatted for computers, tablets, and smartphones, displaying the recommendations.
Pilot website to determine feasibility in practice: The Can-SCIP 2 Implementation website will be the first of its kind within SCI and provide clinicians and learners with a valuable user-friendly and easy to follow tool to find best-practice treatments for the patient sitting in front of them. The application will link users to relevant implementation tools and resources (i.e. SCI-FX fracture risk assessment tool, SCI-U, Canadian C-Spine Rule tip card, International Standards for Neurological Classification of SCI (ISNCSCI) algorithm) and rehabilitation and community stakeholders to relevant structure, process and outcome health indicators developed by the SCI-HIGH project.Citation26
Results
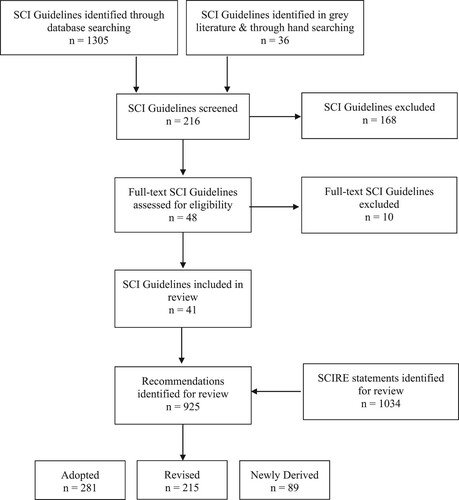
As shown in the PRISMA flow diagram (), the systematic search identified 41 SCI-specific CPGs that met our inclusion criteria (see ). Following expert review and vetting of recommendations, the Can-SCIP Guideline includes 585 total recommendations, 96 recommendations that pertain to the Components of the Ideal SCI Care System () and 489 recommendations that pertain to the Management of Secondary Health Conditions section (). and provide an overview of each domain and subheadings, the associated number of recommendations, and provides a summary of both the level of evidence and whether the recommendations were adopted, revised, or newly derived. The majority of recommendations 281 (48%) were adopted from other CPGs without revision, 215 (36.8%) recommendations were revised to ensure application in a Canadian context and 89 (15.2%) were created de novo during the expert panel discussions from the SCIRE statements and or reflections on current established best practices. The majority of the recommendations (n = 382, 65.3%) are based on level C evidence, 126 (21.5%) are based on level B evidence, and a minority 77 (13.2%) are based on level A evidence.
Table 3 SCI clinical practice guidelines selected for inclusion.
Table 4 Can-SCIP domain summary – Section 1.
Table 5 Can-SCIP domain summary – Section 2.
Within the Components of the Ideal SCI Care System, 39 recommendations (40.6%) pertain to prehospital care, 18 (18.8%) that pertain to diagnostic imaging, 9 (9.4%) pertain to early acute care, 20 (20.8%) that pertain to specialized rehabilitation and community transitions, and 10 (10.4%) that pertain to education for clinicians, patients and caregivers across the care continuum. In the health systems portion of the guideline, the majority of the 21 new recommendations pertain to community-based rehabilitation.
In the Secondary Health Conditions section, there were over 68 new recommendations. There was a total of 249 recommendations that were adopted without revision and 172 recommendations that were revised. Across the Secondary Health Conditions section, the aspects of care with the most recommendations, pertain to common and severe complications including skin integrity (97 recommendations), autonomic dysreflexia (88 recommendations), emotional well-being (54 recommendations) and sexual health, relationships, and fertility (53 recommendations).
A substantial proportion of the recommendations (86%) were felt to be generic for application to the entire SCI community regardless of impairment. The majority of the recommendations are applicable across the rehabilitation and community settings; whereas for prehospital care and surgical interventions there was greater specificity based on the mechanism of injury and associated impairments (data not shown). This data will be used to inform the design of the Can-SCIP Guideline website and will be presented in a future manuscript with the associated algorithms.
Discussion
SCI results in a complex constellation of impairments that require tertiary care across the health system and the individual’s lifespanCitation27,Citation28 to reduce morbidity and mortality and augment functional recovery, health and well-being. The Can-SCIP Guideline is the first comprehensive guideline for adults with SCI in Canada that has integrated recommendations from 41 guidelines and has validated the guideline content for implementation in Canada.
A total of 585 recommendations were explicitly adopted (n = 281), adapted (n = 215) or newly developed (n = 89) to align with the Canadian healthcare environment, providing a set of recommendations that cover the continuum from pre-hospital to community-based care that are customized for the individual based on their impairment. Due to the sheer number of recommendations, and the diverse audiences for sections of the Guideline content, the Can-SCIP steering committee a priori elected to divide the recommendations into two sections: the first section addressing recommendations for the components of the ideal SCI care system and the second section addressing the management of secondary health conditions. The target audience for this section is health system leaders who make decisions about human resources, capital equipment, staff training, physical space, and specialized equipment needed for optimal care. The second section provides recommendations to address secondary health conditions within prioritized domains for rehabilitation care deemed important by SCI stakeholders. The target audiences for this section are individuals with SCI and their regulated healthcare professionals.
There are gaps in the number and complexity of recommendations in the latter part of the healthcare continuum that in part reflect the design and resourcing of the health system and existence of available community sector administrative data sources.Citation29 Areas in which new recommendations were developed to reflect burgeoning science. also reflect the presence of local champions in Canada who are leading the development of innovations in SCI care including: hemodynamic monitoring,Citation30 early surgical spinal cord decompression,Citation31 upper limb rehabilitation including the selection of patient appropriate for tenodesis or peripheral nerve transplant surgery,Citation32 bone health,Citation33 autonomic dysreflexia,Citation34 respiratory care,Citation35,Citation36 and sexual health.Citation37
Not surprisingly, the greatest number of recommendations pertain to skin integrity, autonomic dysreflexia and neurogenic bladder management that are the most frequent secondary health conditions which have a profound adverse impact on an individual’s health, resource requirements and mortality.
As discussed above, there are fewer recommendations supported by high-quality randomized controlled trials, reflecting the low proportion of level A recommendations. This reflects the nature of the SCI evidence, the relatively low incidence and prevalence and the challenge of studying complex interventions in this population with heterogeneous impairments. Further, challenges within the field of SCI internationally include: ongoing difficulties in funding and accruing an adequate sample size within clinical trials, restricting our ability to generate Level I evidence to inform practice.Citation6,Citation7
The Can-SCIP Guideline development process had multiple benefits:
Instead of duplicating the solid work of other guideline groups, it allowed for the Can-SCIP group to conduct a quality assessment of existing SCI CPGs that allowed the expert panel members to adopt the highest quality recommendations for inclusion. This process allowed for many important clinical questions which arise for individuals throughout an individual’s care journey to be addressed and may be used by all members of an interprofessional care team.
Each working group had access to the SCIRE systematic literature review evidence tables to ensure all evidence that had not been incorporated into previous guidelines were considered for each domain.
We adhered to the processes for engaging individuals with lived experience described by Gainforth and colleaguesCitation38 throughout the guideline development process.
The expert panel members specified which recommendations apply to specific impairments groups which will allow clinicians to quickly identify recommendations relevant to the patient in front of them.
As the current model used to update CPGs involves revising the entire CPG within a specific time interval (e.g. every two years), some recommendations may be out of date by the time the CPG is updated, thereby affecting the validity of specific recommendations.Citation39 Further, the evidence base for some recommendations may not vary significantly between CPG updates; thereby, slowing the efficiency of the update process. To overcome these challenges, living guidelines are an alternative to standard guideline development methods which will allow recommendations within a CPG to be updated as new and relevant evidence is published.Citation39 The Can-SCIP Guideline Living Guideline Panel will adopt a living guideline process to provide target users with up-to-date and high-quality advice. This process will involve a living systematic review, living evidence profiles, living evidence-to-decision tables, ongoing participation from a living guideline panel, timely peer review processes, with routine publication and dissemination, with a sustainable source of funding. These processes and associated work plan will be discussed in a subsequent publication. In brief, Can-SCIP Guideline recommendations will be prioritized for revision and dissemination based on the following criteriaCitation39:
“The recommendation is a priority for decision-making”Citation39 which may be affected by increased prevalence of morbidity and mortality or emergent interventions or therapies.
There is a moderate-to-high probability that emerging evidence may improve the level of a particular intervention (i.e. in instances when the level of evidence is a “B” or “C” within the Guideline).
There is active research within a particular topic area of interest to the field.
Conclusion
The Can-SCIP Guideline recommendations were developed using a systematic and rigorous process of evaluating previously published rigorously developed CPGs. The recommendations are pertinent to the care of individuals with SCI over their lifespan from injury onset to healthy aging in the community. The 585 guideline recommendations are intended to assist clinicians, administrators, and policy makers within interdisciplinary teams to provide evidence-informed multidisciplinary care to individuals with SCI within the Canadian healthcare context.
Disclaimer statements
Contributors None.
Funding This work was supported by the Praxis Spinal Cord Institute (former Rick Hansen Institute) [grant number G2019-11].
Declaration of interest Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation, and receipt of consulting fees from the Praxis Spinal Cord Institute. Vanessa Noonan and Christiana Cheng are employees of the Praxis Spinal Cord Institute. Eleni Patsakos, Janice Eng, Matthew Querée, Chester Ho and Ailene Kua report no conflicts of interest. Dr. M. Bayley receives a stipend from UHN- Toronto Rehabilitation Institute for his role as Medical Director but has no other conflicts of interests.
Conflicts of interest Authors have no conflict of interests to declare.
Supplemental Material
Download Zip (349.2 KB)Acknowledgements
We extend our particular gratitude to the entire expert panel for their expertise, dedication and support of the Can-SCIP Guideline: Andrea Townson, Andréanne Richard-Denis, Andrei Krassioukov, Blayne Welk, Brian Kwon, Christine Short, Christopher West, Colleen O'Connell, Daryl Forney, Deena Lala, Denise Hill, Graham Jones, Heather Flett, Jamie Milligan, Jeff Wilson, Joanne Smith, John Chernesky, John Cobb, John Shepherd, Karen Ethans, Katharina Kovacs Burns, Kristin Musselman, Kristine Cowley, Laurent Bouyer, Leanna Ritchie, Lise Bélanger, Louise Russo, Marie-Thérèse Laramée, Michael Fehlings, Milos Popovic, Pamela Houghton, Peter Athanasopoulos, Richard Fox, Sean Christie, Sera Nicosia, Shane McCullum, Shea Hocaloski, Sonja McVeigh, Stacy Elliot, Steve Casha, Sukhvinder Kalsi-Ryan, Susan Jaglal, Teren Clarke.
References
- Hitzig SL, Escobar EMR, Noreau L, Craven BC. Validation of the reintegration to normal living index for community-dwelling persons with chronic spinal cord injury. Arch Phys Med Rehabil 2012;93(1):108–14.
- Carr JJ, Kendall MB, Amsters DI, Pershouse KJ, Kuipers P, Buettner P, et al. Community participation for individuals with spinal cord injury living in Queensland, Australia. Spinal Cord 2017;55(2):192–7.
- Guilcher SJT, Catharine Craven B, Bassett-Gunter RL, Cimino SR, Hitzig SL. An examination of objective social disconnectedness and perceived social isolation among persons with spinal cord injury/dysfunction: a descriptive cross-sectional study. Disabil Rehabil 2019;43(1):1–7.
- Craven BC, Balioussis C, Verrier M. The tipping point: perspectives on SCI rehabilitation service gaps in Canada. Int J Phys Med Rehabil 2013;1(8):1–4.
- DeVivo MJ, Savic G, Frankel HL, Jamous MA, Soni BM, Charlifue S, et al. Comparison of statistical methods for calculating life expectancy after spinal cord injury. Spinal Cord 2018;56(7):666–73.
- Blight AR, Hsieh J, Curt A, Fawcett JW, Guest JD, Kleitman N, et al. The challenge of recruitment for neurotherapeutic clinical trials in spinal cord injury. Spinal Cord 2019;57(5):348–59.
- Mulcahey MJ, Jones LAT, Rockhold F, Rupp R, Kramer JLK, Kirshblum S, et al. Adaptive trial designs for spinal cord injury clinical trials directed to the central nervous system. Spinal Cord 2020;58(12):1–14.
- Peters S, Bussières A, Depreitere B, Vanholle S, Cristens J, Vermandere M, et al. Facilitating guideline implementation in primary health care practices. J Prim Care Community Health 2020;11:2150132720916263.
- Ketelaar M, Russell DJ, Gorter JW. The challenge of moving evidence-based measures into clinical practice: lessons in knowledge translation. Phys Occup Ther Pediatr 2008;28(2):191–206.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362(9391):1225–30.
- Ciliska DK, Pinelli J, DiCenso A, Cullum N. Resources to enhance evidence-based nursing practice. AACN Adv Crit Care 2001;12(4):520–8.
- Davies BL. Sources and models for moving research evidence into clinical practice. J Obstet Gynecol Neonatal Nurs 2002;31(5):558–62.
- Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 2001;39(8):II46–54.
- Alavinia SM, Hitzig SL, Farahani F, Flett H, Bayley M, Craven BC. Prioritization of rehabilitation domains for establishing spinal cord injury high performance indicators using a modification of the Hanlon method: SCI-high project. J Spinal Cord Med 2019;42(Suppl. 1):43–50.
- Marion TE, Rivers CS, Kurban D, Cheng CL, Fallah N, Batke J, et al. Previously identified common post-injury adverse events in traumatic spinal cord injury—validation of existing literature and relation to selected potentially modifiable comorbidities: a prospective Canadian cohort study. J Neurotrauma 2017;34(20):2883–91.
- NCCIH Clearinghouse [Internet]. Available from https://nccih.nih.gov/health/clearinghouse.
- Clinical Key [Internet]. Available from https://www.elsevier.com/solutions/clinicalkey.
- Trip Medical Database [Internet]. Available from https://www.tripdatabase.com.
- DynaMed Plus [Internet]. Available from https://www.dynamed.com/home/.
- Scottish Intercollegiate Guidelines Network [Internet]. Available from https://www.sign.ac.uk/.
- CADTH Grey Matters Tool [Internet]. Available from https://www.cadth.ca/resources/finding-evidence/grey-matters.
- Guidelines International Network [Internet]. Available from https://www.g-i-n.net/home.
- Physiotherapy Evidence Database Ratings (PEDro) [Internet]. Available from https://www.pedro.org.au/.
- Patsakos EM, Bayley MT, Kua A, Cheng C, Eng J, Ho C, et al. Quality of published SCI clinical practice guidelines: results from Can-SCIP panel appraisal of guidelines for research and evaluation (AGREE) evaluation. J Spinal Cord Med 2020.
- Lindsay P, Bayley M, Kelloway L. P75–recommendations are not enough: creating a toolbox to support stroke guideline uptake. Otolaryngol Neck Surg 2010;143(1_suppl):117.
- Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-high project. J Spinal Cord Med 2019;42(Suppl. 1):51–67.
- Cadel L, Everall AC, Packer TL, Hitzig SL, Patel T, Lofters AK, et al. Exploring the perspectives on medication self-management among persons with spinal cord injury/dysfunction and providers. Res Soc Adm Pharm 2020;16(12):1775–84.
- Noonan V, Fallah N, Park S, Dumont F, Leblond J, Cobb J, et al. Health care utilization in persons with traumatic spinal cord injury: the importance of multimorbidity and the impact on patient outcomes. Top Spinal Cord Inj Rehabil 2014;20(4):289–301.
- Rowan CP, Chan BCF, Jaglal SB, Catharine Craven B. Describing the current state of post-rehabilitation health system surveillance in Ontario–an invited review. J Spinal Cord Med 2019;42(Suppl. 1):21–33.
- Kong CY, Hosseini AM, Belanger LM, Ronco JJ, Paquette SJ, Boyd MC, et al. A prospective evaluation of hemodynamic management in acute spinal cord injury patients. Spinal Cord 2013;51(6):466–71.
- Badhiwala JH, Ahuja CS, Fehlings MG. Time is spine: a review of translational advances in spinal cord injury: JNSPG 75th anniversary invited review article. J Neurosurg Spine 2018;30(1):1–18.
- Kwon BK, Liu J, Messerer C, Kobayashi NR, McGraw J, Oschipok L, et al. Survival and regeneration of rubrospinal neurons 1 year after spinal cord injury. Proc Natl Acad Sci 2002;99(5):3246–51.
- Morse LR, Biering-Soerensen F, Carbone LD, Cervinka T, Cirnigliaro CM, Johnston TE, et al. Bone mineral density testing in spinal cord injury: 2019 ISCD official position. J Clin Densitom 2019;22(4):554–66.
- Cowan H, Lakra C, Desai M. Autonomic dysreflexia in spinal cord injury. Br Med J 2020;371: m3596,1–4.
- McKim DA, Avendano M, Abdool S, Côté F, Duguid N, Fraser J, et al. Home mechanical ventilation: a Canadian thoracic society clinical practice guideline. Can Respir J 2011;18:197–215.
- Rose L, McKim D, Leasa D, Nonoyama M, Tandon A, Kaminska M, et al. Monitoring cough effectiveness and use of airway clearance strategies: a Canadian and UK survey. Respir Care 2018;63(12):1506–13.
- Elliott SL. Problems of sexual function after spinal cord injury. Prog Brain Res 2006;152:387–99.
- Gainforth HL, Hoekstra F, McKay R, McBride CB, Sweet SN, Ginis KAM, et al. Integrated knowledge translation guiding principles for conducting and disseminating spinal cord injury research in partnership. Arch Phys Med Rehabil 2021;102(4):656–63.
- Akl EA, Meerpohl JJ, Elliott J, Kahale LA, Schünemann HJ, Agoritsas T, et al. Living systematic reviews: 4. Living guideline recommendations. J Clin Epidemiol 2017;91:47–53.
- Hebert D, Lindsay MP, McIntyre A, Kirton A, Rumney PG, Bagg S, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke 2016;11(4):459–84.
- Academy of Nutrition and Dietetics. Spinal Cord Injury Evidence-Based Nutrition Practice Guideline [Internet]. 2009. Available from https://www.andeal.org/topic.cfm?cat=3485.
- Consortium for Spinal Cord Medicine. Sexuality and reproductive health in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med [Internet]. 2010;33(3):281–336. Available from https://pubmed.ncbi.nlm.nih.gov/20737805.
- Home mechanical ventilation: a Canadian thoracic society CPG, 2011.
- Evidence-based guideline update: intraoperative spinal monitoring with somatosensory and transcranial electrical motor evoked potentials, 2011.
- UK National Clinical Guideline Centre. Urinary incontinence in neurological disease: management of lower urinary tract dysfunction in neurological disease, 2012; Available from https://pubmed.ncbi.nlm.nih.gov/23638496/.
- Ontario Neurotrauma Foundation. Canadian best practice guidelines for the prevention and management of pressure ulcers in people with spinal cord injury. Available from https://onf.org/wp-content/uploads/2019/04/Pressure_Ulcers_Best_Practice_Guideline_Final_web4.pdf.
- Multidisciplinary Association of Spinal Cord Injury Professionals. Clinical guideline for standing in adults following spinal cord injury [Internet]. 2013. Available from https://www.mascip.co.uk/wp-content/uploads/2015/05/Clinical-Guidelines-for-Standing-Adults-Following-Spinal-Cord-Injury.pdf.
- Development of clinical guidelines for the prescription of a seated wheelchair or mobility scooter for people with TBI or SCI [Internet], 2013. Available from https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0003/167286/Guidelines-on-Wheelchair-Prescription.pdf.
- Ryken T, Hadley M, Aarabi B, Sanjay S, Gelb D RJH, et al. Management of acute combination fractures of the atlas and axis in adults. Neurosurgery 2013;72(suppl_3):151–8.
- Gelb DE, Hadley MN, Aarabi B, Dhall SS, Hurlbert J, Rozzelle C, et al. Initial closed reduction of cervical spinal fracture-dislocation injuries. Neurosurgery 2013;72(suppl_3):73–83.
- Dhall SS, Hadley MN, Aarabi B, Gelb DE, Hurlbert RJ, Rozzelle CJ, et al. Deep venous thrombosis and thromboembolism in patients with cervical spinal cord injuries. Neurosurgery 2013;72(suppl_3):244–54.
- Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update, 2013.
- Consortium for Spinal Cord Medicine. Pressure ulcer prevention and treatment following SCI, 2nd ed., [Internet], 2014. Available from https://www.mascip.co.uk/wp-content/uploads/2015/05/CPG_Pressure-Ulcer.pdf.
- NCGC UK. The prevention and management of pressure ulcers in primary and secondary care [Internet]. 2014. Available from https://pubmed.ncbi.nlm.nih.gov/25340232/.
- Prevention and treatment of pressure ulcers: individuals with spinal cord injury [Internet], 2014. Available from https://www.internationalguideline.com/static/pdfs/08-NPUAP-EPUAP-PPPIAIndividualswithSCIExtractoftheCPG 2017.pdf
- PCI Statements. Prevention of venous thromboembolism in individuals with spinal cord injury: clinical practice guidelines for health care providers. Top Spinal Cord Inj Rehabil 2016;22(3):209–40.
- Guy SD, Mehta S, Casalino A, Côté I, Kras-Dupuis A, Moulin DE, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: recommendations for treatment. Spinal Cord [Internet] 2016;54(1):S14–23. Available from https://doi.org/https://doi.org/10.1038/sc.2016.90.
- Mehta S, Guy SD, Bryce TN, Craven BC, Finnerup NB, Hitzig SL, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: screening and diagnosis recommendations. Spinal Cord [Internet] 2016;54(1):S7–13. Available from https://doi.org/https://doi.org/10.1038/sc.2016.89.
- Guy SD, Mehta S, Harvey D, Lau B, Middleton JW, O’Connell C, et al. The CanPain SCI clinical practice guideline for rehabilitation management of neuropathic pain after spinal cord: recommendations for model systems of care. Spinal Cord [Internet] 2016;54(1):S24–7. Available from https://doi.org/https://doi.org/10.1038/sc.2016.91.
- Critical Care Services Ontario. Provincial guidelines for spinal cord assessment [Internet], 2016. Available from https://criticalcareontario.ca/wp-content/uploads/2020/11/Guidelines-for-Adult-Spinal-Cord-Assessment-May-2016.pdf.
- NICE. Spinal injury: assessment and initial management. Retrieved from world wide web [Internet]. 2017;17(01). Available from https://www.ncbi.nlm.nih.gov/books/NBK344254/.
- Yue JK, Chan AK, Winkler EA, Upadhyayula PS, Readdy WJ, Dhall SS. A review and update on the guidelines for the acute management of cervical spinal cord injury-part II. J Neurosurg Sci 2015;60(3):367–84.
- Ginis KAM, Van Der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord 2018;56(4):308–21.
- Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (≤24 hours versus >24 hours) of decompressive surgery. Glob Spine J 2017;7(3_suppl):195S–202S.
- Fehlings MG, Wilson JR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the use of methylprednisolone sodium succinate. Glob Spine J 2017;7(3_suppl):203S–11S.
- Fehlings MG, Tetreault LA, Aarabi B, Anderson P, Arnold PM, Brodke DS, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the type and timing of anticoagulant thromboprophylaxis. Glob Spine J 2017;7(3_suppl):212S–20S.
- Fehlings MG, Martin AR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, et al. CPG for the management of patients with acute SCI: recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Glob Spine J [Internet] 2017;7(3_suppl):221S–30S. Available from https://journals.sagepub.com/doi/pdf/https://doi.org/10.1177/2192568217703089.
- CPG for the management of patients with acute SCI: recommendations on the type and timing of anticoagulant thromboprophylaxis, 2017.
- Rehabilitation in health systems [Internet], 2017. Available from https://www.who.int/disabilities/rehabilitation_health_systems/en/.
- WHO. International perspectives on SCI [Internet], 2013. Available from https://www.who.int/disabilities/policies/spinal_cord_injury/en/.
- Schurch B, Iacovelli V, Averbeck MA, Carda S, Altaweel W, Finazzi Agrò E. Urodynamics in patients with spinal cord injury: a clinical review and best practice paper by a working group of the international continence society urodynamics committee. Neurourol Urodyn 2018;37(2):581–91.
- Occupational therapists and physiotherapists in the community setting (Northern Ireland). Guidelines for the rehabilitation of patients with metastatic spinal cord compression [Internet], 2017. p. 1–96. Available from https://www.rqia.org.uk/RQIA/files/cb/cba33182-deab-46ae-acd1-d27279d9847c.pdf
- Kornhall DK, et al. Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med 2017;25(1):1–11.
- Wounds Canada. Wounds Canada Best Practice Recommendations [Internet]. 2017. Available from https://www.woundscanada.ca/health-care-professional/resources-health-care-pros/12-healthcare-professional/110-supplements
- NICE. Neuropathic Pain in Adults: Pharmacological Management in Non-Specialist Settings (CG173) [Internet]. 2018. Available from https://www.nice.org.uk/guidance/cg173
- Nash MS, Groah SL, Gater Jr DR, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Identification and management of cardiometabolic risk after spinal cord injury: clinical practice guideline for health care providers. Top Spinal Cord Inj Rehabil [Internet] 2018;24(4):379–423. Available from https://pubmed.ncbi.nlm.nih.gov/30459501.
- Kavanagh A, Baverstock R, Campeau L, Carlson K, Cox A, Hickling D, et al. Canadian urological association guideline: diagnosis, management, and surveillance of neurogenic lower urinary tract dysfunction–full text. Can Urol Assoc J 2019;13(6):E157.
- Krassioukov A, Linsenmeyer TA, Beck LA, Elliott S, Gorman P, Kirshblum S, et al. Evaluation and management of autonomic dysreflexia and other autonomic dysfunctions: preventing the highs and lows: management of blood pressure, sweating, and temperature dysfunction. Top Spinal Cord Inj Rehabil 2021;27(2):225–90.
- Johns J, Krogh K, Rodriguez GM, Eng J, Haller E, Heinen M, et al. Management of neurogenic bowel dysfunction in adults after spinal cord injury: clinical practice guideline for health care providers. J Spinal Cord Med 2021;44(3):442–510.
- Bombardier CH, Azuero CB, Fann JR, Kautz DD, Richards JS, Sabharwal S. Management of mental health disorders, substance use disorders, and suicide in adults with spinal cord injury: clinical practice guideline for healthcare providers. Top Spinal Cord Inj Rehabil 2021;27(2):152–224.