?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Introduction
Spinal cord injury (SCI) is a complex condition with substantial adverse personal, social and economic impacts necessitating evidence-based inter-professional care. To date, limited studies have assessed the quality of clinical practice guidelines (CPGs) within SCI. The aim of this study is to evaluate the quality of the development process and methodological rigour of published SCI CPGs across the care continuum from pre-hospital to community-based care.
Methods
Electronic health databases and indexes were searched to identify English or French language CPGs within SCI published within the last nine years with specific evidence-based recommendations applicable to the Canadian health care setting. Eligible CPGs were evaluated using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) instrument.
Results
A total of forty-one CPGs that met the inclusion criteria were appraised by at least four raters. There was high variability in quality. Twenty-seven CPGs achieved a good rigour of development domain score of >70%. Other standardized mean domain scores were scope and purpose (85.32%), stakeholder involvement (65.03%), clarity of presentation (84.81%), applicability (55.55%) and editorial independence (75.83%). The agreement between appraisers (intraclass correlation coefficient) was high (intraclass correlation coefficient > 0.80).
Conclusion
There is a paucity of CPGs that address community-based specialized rehabilitation and community reintegration. Furthermore, many CPGs only focus on a single impairment at one time point in the care continuum. As SCI is a complex condition that results in multimorbidity and requires health monitoring and intervention across the lifespan, a rigorously developed CPG that addresses high-quality, interprofessional comprehensive care is needed.
Introduction
Spinal cord injury (SCI) is a traumatic event that impacts an individual’s quality of life, sensory, motor and autonomic function, and social independence.Citation1 Worldwide, the incidence of traumatic SCI is estimated to range from 10 to 83 people per million.Citation2 Studies have estimated the worldwide prevalence of traumatic SCI to range from 8 to 246 per million.Citation3 The direct lifetime costs for SCI onset at age 25 range from USD $2.1 to 5.4 million depending on injury severity.Citation4 The estimated incidence of traumatic SCI is 1,785 cases in Canada each year.Citation2 Thus, traumatic SCI is a complex condition, with substantial adverse personal, social and economic impacts necessitating evidence-informed inter-professional care.
A consistent finding within health services research is that the translation of research knowledge into practice is a “slow and haphazard process.”Citation5 Clinical practice guidelines (CPGs) play an important role in bridging this knowledge gap. Field and LohrCitation6 define CPGs as “systematically developed statements to assist practitioners’ and patients’ decisions about appropriate health care for specific clinical circumstances”. CPGs have the ability to improve the quality and consistency of health care provided by clinicians leading to improvements in patient health outcomes.Citation7 However, the identification of rigorously developed CPGs is a “daunting task” for clinicians, policymakers and other stakeholders.Citation7 The AGREE instrument was developed by an international group of guideline developers and researchers in 2003 to assess the ‘Quality of guidelines’ or “the confidence that the potential biases of guideline development have been addressed adequately and that the recommendations are both internally and externally valid and are feasible for practice.”Citation8
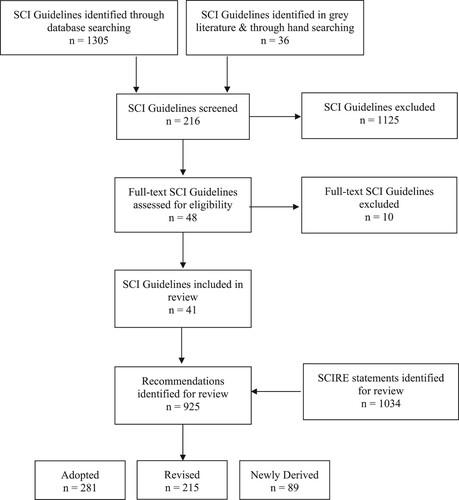
Within the field of traumatic SCI, existing CPGs focus on specific health complicationsCitation9,Citation10 or care within specific segments of the care continuumCitation11,Citation12 and do not address all the important clinical questions which arise during care provision. As SCI is a complex condition that results in multimorbidityCitation13 and requires health monitoring and intervention across the lifespan, a rigorously developed CPG that addresses high-quality, interprofessional comprehensive care is needed. Recognizing these challenges and limitations, we sought to form an interprofessional panel of experts in SCI to develop the Canadian Spinal Cord Injury Best Practice (Can-SCIP) Guideline. The Can-SCIP Guideline is the first comprehensive living guideline for adults with SCI in Canada that is adapting, updating, integrating 585 recommendations from 41 CPGs () and has validated the content of existing SCI guidelines with stakeholders for implementation in Canada.
Table 1 SCI Clinical Practice Guidelines selected for inclusion.
The objective of this study, therefore, is to evaluate the quality of the development process and methodological rigour of published CPGs within SCI across the care continuum from pre-hospital to community-based care.
Methods
Guideline search and selection
A scoping review was undertaken for CPGs focused on treatment and evidence-based recommendations for individuals with traumatic SCI. The Can-SCIP steering committee consulted with the Health Sciences Librarian at the University of British Columbia (UBC) to assist with the construction of the search. Thirteen electronic health databases and indexes were searched to identify CPGs within SCI. These include but were not limited to: PubMed, Medline, Embase, CINAHL, and PsycINFO, NCCIH Clearinghouse,Citation52 Clinical Key,Citation53 Trip Medical database,Citation54 DynaMed Plus,Citation55 Scottish Intercollegiate Guidelines Network,Citation56 CADTH Grey Matters tool,Citation57 Guidelines International Network,Citation58 and Physiotherapy Evidence Database Ratings (PEDro).Citation59
The key search terms included ‘spinal cord injury,’ ‘spinal cord dysfunction,’ ‘tetraplegia,’ ‘quadriplegia,’ ‘paraplegia,’ ‘spinal cord impaired,’ ‘spinal cord lesion’ (including truncations of these SCI terms) and ‘clinical practice guidelines.’ The inclusion criteria for the CPGs included:
Adults (> 18 years of age)
CPG published in last 9 years (2011–2020)
Written by 4 or more authors
Written in English or French language
Inclusion of specific evidence-based recommendations
Applicable to the Canadian health care setting
Quality Appraisal
The Appraisal of Guidelines for Research and Evaluation (AGREE II) instrument was used to evaluate eligible guidelines. The AGREE instrument is composed of twenty-three items organized in six quality domains: (1) scope and purpose, (2) stakeholder involvement, (3) rigour of development, (4) clarity of presentation, (5) applicability, and (6) editorial independence. An additional item rates the overall quality of the guideline when considering the criteria within the six domains. Each domain is specific to a unique dimension of guideline quality. Each item within the instrument is rated on a 7-point scale. A score of 1 (“strongly disagree”) is given when the concept is “very poorly reported,” or the appraiser cannot find any information relevant to a particular AGREE II item, or the guideline authors indicate that a specific criterion was not met. A score of 7 (“strongly agree”) is assigned when all criteria and considerations in the AGREE User ManualCitation60 are met. A score between 2 and 6 is given when the information related to a specific item does not meet the full criteria and consideration discussed in the AGREE User Manual. The AGREE II instrument has demonstrated construct validity,Citation61 inter-rater reliabilityCitation62 and was found to be a significant positive predictor of guideline adoption.Citation62
Each CPG was independently evaluated by three to five appraisers from the Can-SCIP expert panel (Appendix A). Each expert panel member was required to disclose to the Can-SCIP steering committee if they have developed or served as an external reviewer of any of the CPGs within SCI. Each panel member was assigned approximately four or five CPGs to appraise. Expert panel members who participated in the development of an included CPG or served as an external reviewer for the CPG were asked to rate other CPGs. As described in the AGREE II User Manual,Citation60 the six domains scores are independent and were not be combined into a single score. For each CPG, a standardized score was calculated using the following formula for each domain:
Intra-class correlation coefficients (2-way random model) were used to assess appraiser agreement.
As the AGREE User ManualCitation60 does not specify a minimum score that is considered ‘low-quality,’ the Can-SCIP steering committee set a benchmark of 40% for inclusion, whereby scores higher than 40% represent higher quality, and scores below 40% represent poorer quality.
Results
Included Guidelines
The systematic search yielded 1,305 documents in addition to thirty-three grey literature documents. Of the 1338 documents, 216 full-text documents were reviewed, and 48 were shortlisted for evaluation. The experts continued to scan literature and became aware that the Paralyzed Veterans of America was in the final stages of completing 3 CPGs that were to be published in 2020, and these CPGs were evaluated after the initial set.Citation49–51 A total of forty-one CPGs met the inclusion criteria. provides an output of the search process.
provides an overview of the included guidelines, the topics covered and the phase of the continuum of care involved. Fifteen originated in the United States, eight CPGs originated in Canada, six from the United Kingdom, one CPG was from Australia, one was from Norway, one joint collaboration of Canada and the United Kingdom, and 9 CPGs were international collaborations. There was a total of 925 recommendations within the forty-one CPGs. The CPGs fit under 24 health domains ().
Quality Appraisal
outlines the standardized domain scores. “Rigor of development” is considered one of the most important indicators of methodological quality as it indicates the link between the strength of the clinical trial evidence that supports each recommendation. The median score for “rigor of development” was 79.17%. Thirty-nine CPGs achieved a domain score greater than 40%, and 2 guidelines achieved a score below 40%.
Table 2 Standardized domain scores (%).
Domains with High Scores
Domain scores were relatively higher for “rigour of development”, “clarity of presentation,” “editorial independence,” and “stakeholder involvement,” with mean scores of 73.90%, 84.81% and 75.83%, 65.03, respectively. The highest domain score was achieved in domain 1, “scope and purpose,” with a median score of 85.32%.
Domains with Low Scores
Standardized scores for domain 5 of the AGREE II tool (“applicability”) were low, with a median of 56.67. “Applicability” had the greatest number of standardized domain scores less than 40% (n=10). Three CPGs had a standardized “applicability” domain score between 30 and 39 percent, one CPG between 20 and 29 percent and one CPG with a score between 10 and 19 percent. The lowest standardized domain scores were under “stakeholder involvement” (domain 2) at 7.8% for two CPGs.
Interrater Reliability.
Interrater reliability score was measured using the Interclass Correlation Coefficient (ICC). All ICCs indicated high agreement (ICC > 0.80), except for one domain, which indicated was moderate agreement (ICC < 0.80) among expert panel members with varied clinical expertise across all guidelines assessed. The table below shows the interrater reliability for each domain ().
Table 3 Appraiser agreement.
Discussion
To our knowledge, this is the first comprehensive search and evaluation of the methodological quality of published CPGs across the SCI care continuum from pre-hospital and emergency care to community-based rehabilitation. CPGs are an important tool to improve the quality of medical care and assist healthcare professionals in making clinical decisions based on evidence.Citation63–65 Based on the standardized domains scores, the CPGs that scored the highest rating within all six domains included Wounds Canada Best Practice Recommendations,Citation45 Evidence-Based Scientific Exercise Guidelines for Adults with SCI,Citation34 Home Mechanical Ventilation: A Canadian Thoracic Society CPG,Citation16 CPG for the Management of Patients With Acute SCI: Recommendations on the Type and Timing of Rehabilitation,Citation39 and Management of Neurogenic Bowel Dysfunction in Adults after SCI: CPG for Health Care Providers.Citation50
Further, an important domain within the AGREE II tool for clinicians is “rigour of development.”Citation66 Twenty-seven CPGs (65%) achieved a standardized domain score of over 70%. The findings are similar to Hurdowar and colleagues (2007)Citation66, who noted that 62% of evaluated CPGs received a standardized domain score of over 74%. The domain scores achieved are higher than previous CPG assessments. Cranney and colleaguesCitation67 appraised the quality of osteoporosis guidelines that received a “rigour of development” score of 23%. Graham and colleagues (2001) assessed the quality of drug therapy CPGs and received a “rigour of development” score of 30%.Citation68 Variation in the other AGREE standardized domain scores within the other categories was also observed. Similar to HurdowarCitation66 and others, the mean and median scores on stakeholder involvement and applicability domains were lower. Future guideline development groups should clearly describe the facilitators and barriers to implementing the CPG, tools and resources to facilitate dissemination and implementation of the CPG, and the strategies used to incorporate the views and preferences of persons with lived experience throughout the CPG development process. Further, only 3 CPGs presented the cost implications (i.e. economic evaluation, drug acquisition costs for each treatment) of applying the recommendations. This finding is similar to previous studies, which noted that economic evaluations are overlooked.Citation45 Additional research on the resource implications and cost-effectiveness during CPG development and implementation is needed. Future CPG development groups should also consider incorporating the evaluation content within each AGREE II domain to develop high-quality CPGs using a systematic and rigorous process.
The evaluation of recently published CPGs with SCI highlighted several gaps in the literature. There is a paucity of CPGs that address community-based specialized rehabilitation and community reintegration. As well, only several community-based studies that address the needs of people with SCI over their lifetime are available.Citation69 In addition, many CPGs only focus on a single impairment or organ system at a particular time point in the care continuum (i.e. specialized rehabilitation).
As SCI is a complex condition that results in multimorbidity and requires health monitoring and intervention across the lifespan, a rigorously developed CPG that addresses high-quality, interprofessional comprehensive care is needed. The Can-SCIP Guideline was developed to address the gaps in the literature. The Guideline is the first comprehensive living guideline for adults with SCI in Canada that is adapting, updating, integrating, and validating the content of existing SCI guidelines with stakeholders for implementation in Canada. The Guideline has been explicitly adapted to align with the Canadian health care environment, providing a set of recommendations that cover the continuum from pre-hospital to community-based care.
Study Strengths & Limitations
One of the strengths of the study is that a high interrater reliability score was achieved (mean ICC = 0.84) among expert panel members. As well, the CPGs included for evaluation were published within the last 9 years and represent the most recent literature in SCI.
A known limitation is that the AGREE instrument does not provide benchmark cutoff values, and the values selected in this study (benchmark of 40%) were selected by the Can-SCIP steering committee. Other CPG appraisers may interpret the AGREE domain scores differently. Furthermore, the inclusion of only CPGs in English may have excluded high-quality CPGs. Further, there are several factors that may influence the interpretation of the AGREE II appraisal. One factor that may alter scores is that CPGs that are published within large peer-reviewed journals may not have disclosed all methodology because of page and word limitations, which may have affected the ability of the Can-SCIP expert panel to find the level of detail required to receive a score of ‘7’ using the AGREE II tool.
Conclusions
While there are many published SCI guidelines, no single CPG provides recommendations that cover the optimal system of care across the continuum from pre-hospital, acute, rehabilitation and community care, and we did not find a CPG that covered all SCI complications deemed important by individuals with SCI and other relevant stakeholders. About two-thirds of CPGs were developed using a rigorous methodology, although there was variability, and few guidelines provide tools for implementation and applicability. The Can-SCIP Guideline will aim to address these gaps in the currently published guidelines.
Disclosures Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation, and receipt of consulting fees from the Rick Hansen Institute. Vanessa Noonan and Christiana Cheng are employees of the Praxis Spinal Cord Institute. Eleni Patsakos, Janice Eng, Matthew Querée, Chester Ho and Ailene Kua report no conflicts of interest. Dr. M. Bayley receives a stipend from UHN- Toronto Rehabilitation Institute for his role as Medical Director but has no other conflicts of interests.
Disclaimer statements
Conflict of interest: Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation, and receipt of consulting fees from the Rick Hansen Institute now Praxis Spinal Cord Institute. Vanessa Noonan and Christiana Cheng are employees of the Praxis Spinal Cord Institute. Eleni Patsakos, Janice Eng, Matthew Querée, Chester Ho and Ailene Kua report no conflicts of interest. Dr. M. Bayley receives a stipend from UHN- Toronto Rehabilitation Institute for his role as Medical Director but has no other conflicts of interests.
Disclosure statement: No potential conflict of interest was reported by the author(s).
Funding: This work was supported by the Praxis Spinal Cord Institute (former Rick Hansen Institute under Grant #G2019-11).
References
- Fehlings MG, Tetreault LA, Wilson JR, Kwon BK, Burns AS, Martin AR, et al. A clinical practice guideline for the management of acute spinal cord injury: introduction, rationale, and scope. Los Angeles, CA: SAGE Publications Sage CA; 2017.
- Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology 2012;38(4):219–226.
- Furlan JC, Sakakibara BM, Miller WC, Krassioukov A V. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci 2013;40(4):456–464.
- Thomas R, Barnes M. Life expectancy for people with disabilities. NeuroRehabilitation 2010;27(2):201–209.
- Graham ID, Brouwers M, Davies C, Tetroe J. Ontario doctors’ attitudes toward and use of clinical practice guidelines in oncology. J Eval Clin Pract 2007;13(4):607–615.
- Field MJ, Lohr KN. Clinical practice guidelines. Dir a new Program Washingt Natl Acad Pr 1990:1–168.
- Graham ID, Calder LA, Hébert PC, Carter AO, Tetroe JM. A comparison of clinical practice guideline appraisal instruments. Int J Technol Assess Health Care 2000;16(04):1024–1038.
- Brouwers M, Consortium ANS. Appraisal of guidelines for research & evaluation II. Agree Next Steps Consort 2009: 1–56.
- Professionals MA of SCI. Guidelines for management of neurogenic bowel dysfunction in individuals with central neurological conditions. Aylesbury: MASCIP Middlesex; 2012.
- Nash MS, Groah SL, Gater Jr DR, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Identification and management of cardiometabolic risk after spinal cord injury: Clinical practice guideline for health care providers. Top Spinal Cord Inj Rehabil [Internet] 2018;24(4):379–423. Available from: https://pubmed.ncbi.nlm.nih.gov/30459501.
- Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery 2013;60(CN_suppl_1):82–91.
- NICE. Spinal injury: assessment and initial management. Retrieved from World Wide web [Internet] 2017;17(01). Available from: https://www.ncbi.nlm.nih.gov/books/NBK344254/.
- Craven BC, Balioussis C, Verrier M. The tipping point: perspectives on SCI rehabilitation service gaps in Canada. Int J Phys Med Rehabil 2013;1(8):1–4.
- Academy of Nutrition and Dietetics. Spinal Cord Injury Evidence-Based Nutrition Practice Guideline [Internet]. 2009. Available from: https://www.andeal.org/topic.cfm?cat=3485.
- Consortium for Spinal Cord Medicine. Sexuality and reproductive health in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med [Internet] 2010;33(3):281–336. Available from https://pubmed.ncbi.nlm.nih.gov/20737805.
- McKim DA, Avendano M, Abdool S, Côté F, Duguid N, Fraser J, et al. Home mechanical ventilation: a Canadian Thoracic Society clinical practice guideline. Can Respir J 2011;18(4):197–215.
- Evidence-Based Guideline Update: Intraoperative Spinal Monitoring with Somatosensory and Transcranial Electrical Motor Evoked Potentials. 2011.
- UK National Clinical Guideline Centre. Urinary Incontinence in Neurological Disease: Management of Lower Urinary Tract Dysfunction in Neurological Disease. 2012; Available from: https://pubmed.ncbi.nlm.nih.gov/23638496/.
- Ontario Neurotrauma Foundation. Canadian Best Practice Guidelines for the Prevention and Management of Pressure Ulcers in People with Spinal Cord Injury. Available from: https://onf.org/wp-content/uploads/2019/04/Pressure_Ulcers_Best_Practice_Guideline_Final_web4.pdf.
- Multidisciplinary Association of Spinal Cord Injury Professionals. Clinical Guideline for Standing in Adults Following Spinal Cord Injury [Internet]. 2013. Available from: https://www.mascip.co.uk/wp-content/uploads/2015/05/Clinical-Guidelines-for-Standing-Adults-Following-Spinal-Cord-Injury.pdf.
- Development of Clinical Guidelines for the Prescription of a Seated Wheelchair or Mobility Scooter for People with TBI or SCI [Internet]. 2013. Available from https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0003/167286/Guidelines-on-Wheelchair-Prescription.pdf
- Ryken T, Hadley M, Aarabi B, Sanjay S, Gelb D RJH, et al. Management of acute combination fractures of the atlas and axis in adults. Neurosurgery 2013;72(suppl_3):151–158.
- Gelb DE, Hadley MN, Aarabi B, Dhall SS, Hurlbert J, Rozzelle C, et al. Initial closed reduction of cervical spinal fracture-dislocation injuries. Neurosurgery 2013;72(suppl_3):73–83.
- Dhall SS, Hadley MN, Aarabi B, Gelb DE, Hurlbert RJ, Rozzelle CJ, et al. Deep venous thrombosis and thromboembolism in patients with cervical spinal cord injuries. Neurosurgery 2013;72(suppl_3):244–254.
- Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries: 2013 Update. 2013.
- Consortium for Spinal Cord Medicine. Pressure Ulcer Prevention and Treatment Following SCI, 2nd edition [Internet]. 2014. Available from: https://www.mascip.co.uk/wp-content/uploads/2015/05/CPG_Pressure-Ulcer.pdf.
- NCGC UK. The Prevention and Management of Pressure Ulcers in Primary and Secondary Care [Internet]. 2014. Available from: https://pubmed.ncbi.nlm.nih.gov/25340232/.
- Statements PCI. Prevention of venous thromboembolism in individuals with spinal cord injury: clinical practice guidelines for health care providers. Top Spinal Cord Inj Rehabil 2016;22(3):209–240.
- Guy SD, Mehta S, Casalino A, Côté I, Kras-Dupuis A, Moulin DE, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: Recommendations for treatment. Spinal Cord [Internet] 2016;54(1):S14–S23. Available from: https://doi.org/https://doi.org/10.1038/sc.2016.90.
- Mehta S, Guy SD, Bryce TN, Craven BC, Finnerup NB, Hitzig SL, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: screening and diagnosis recommendations. Spinal Cord [Internet] 2016;54(1):S7–S13. Available from: https://doi.org/https://doi.org/10.1038/sc.2016.89.
- Guy SD, Mehta S, Harvey D, Lau B, Middleton JW, O’Connell C, et al. The CanPain SCI clinical practice guideline for rehabilitation management of neuropathic pain after spinal cord: recommendations for model systems of care. Spinal Cord [Internet] 2016;54(1):24–27. Available from: https://doi.org/https://doi.org/10.1038/sc.2016.91.
- Critical Care Services Ontario. Provincial Guidelines for Spinal Cord Assessment [Internet]. 2016. Available from: https://criticalcareontario.ca/wp-content/uploads/2020/11/Guidelines-for-Adult-Spinal-Cord-Assessment-May-2016.pdf.
- Yue JK, Chan AK, Winkler EA, Upadhyayula PS, Readdy WJ, Dhall SS. A review and update on the guidelines for the acute management of cervical spinal cord injury-part II. J Neurosurg Sci 2015;60(3):367–384.
- Ginis KAM, Van Der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord 2018;56(4):308–321.
- Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (≤ 24 h versus> 24 h) of decompressive surgery. Glob Spine J 2017;7(3_suppl):195S–202S.
- Fehlings MG, Wilson JR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the use of methylprednisolone sodium succinate. Glob Spine J 2017;7(3_suppl):203S–211S.
- Fehlings MG, Tetreault LA, Aarabi B, Anderson P, Arnold PM, Brodke DS, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the type and timing of anticoagulant thromboprophylaxis. Glob Spine J 2017;7(3_suppl):212S–220S.
- Fehlings MG, Martin AR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, et al. CPG for the Management of patients with acute SCI: Recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Glob Spine J [Internet] 2017;7(3_suppl):221S–230S. Available from: https://journals.sagepub.com/doi/pdf/https://doi.org/10.1177/2192568217703089.
- Fehlings M, Tetreault L, Aarabi B, Anderson P, Arnold PM, Brodke D, et al. CPG for the Management of patients with acute SCI: Recommendations on the type and timing of rehabilitation. Glob Spine J [Internet] 2017;7(3 suppl):231S–238S. Available from https://doi.org/10.1177/2192568217701910.
- Rehabilitation in Health Systems [Internet]. 2017. Available from https://www.who.int/disabilities/rehabilitation_health_systems/en/
- WHO. International Perspectives on SCI [Internet]. 2013. Available from https://www.who.int/disabilities/policies/spinal_cord_injury/en/.
- Schurch B, Iacovelli V, Averbeck MA, Carda S, Altaweel W, Finazzi Agrò E. Urodynamics in patients with spinal cord injury: A clinical review and best practice paper by a working group of The International Continence Society Urodynamics Committee. Neurourol Urodyn 2018;37(2):581–591.
- Occupational Therapists and Physiotherapists In the Community Setting (Northern Ireland). Guidelines for the Rehabilitation of Patients with Metastatic Spinal Cord Compression [Internet]. 2017. p. 1–96. Available from https://www.rqia.org.uk/RQIA/files/cb/cba33182-deab-46ae-acd1-d27279d9847c.pdf.
- Kornhall DK, Jørgensen JJ, Brommeland T, Hyldmo PK, Asbjørnsen H, Dolven T, et al. Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med 2017;25(1):1–11.
- Wounds Canada. Wounds Canada Best Practice Recommendations [Internet]. 2017. Available from: https://www.woundscanada.ca/health-care-professional/resources-health-care-pros/12-healthcare-professional/110-supplements.
- NICE. Neuropathic Pain in Adults: Pharmacological Management in Non-Specialist Settings (CG173) [Internet]. 2018. Available from https://www.nice.org.uk/guidance/cg173.
- Kavanagh A, Baverstock R, Campeau L, Carlson K, Cox A, Hickling D, et al. Canadian urological association guideline: diagnosis, management, and surveillance of neurogenic lower urinary tract dysfunction–full text. Can Urol Assoc J 2019;13(6):E157.
- Morse LR, Biering-Soerensen F, Carbone LD, Cervinka T, Cirnigliaro CM, Johnston TE, et al. Bone mineral density testing in spinal cord injury: 2019 ISCD official position. J Clin Densitom 2019;22(4):554–566.
- Krassioukov A, Linsenmeyer TA, Beck LA, Elliott S, Gorman P, Kirshblum S, et al. Evaluation and management of autonomic dysreflexia and other autonomic dysfunctions: Preventing the highs and lows: Management of blood pressure, sweating, and temperature dysfunction. Top Spinal Cord Inj Rehabil 2021;27(2):225–290.
- Johns J, Krogh K, Rodriguez GM, Eng J, Haller E, Heinen M, et al. Management of neurogenic bowel dysfunction in adults after spinal cord injury: Clinical practice guideline for health care providers. J Spinal Cord Med 2021;44(3):442–510.
- Bombardier CH, Azuero CB, Fann JR, Kautz DD, Richards JS, Sabharwal S. Management of mental health disorders, substance use disorders, and suicide in adults with spinal cord injury: Clinical practice guideline for healthcare providers. Top Spinal Cord Inj Rehabil 2021;27(2):152–224.
- NCCIH Clearinghouse [Internet]. Available from https://nccih.nih.gov/health/clearinghouse
- Clinical Key [Internet]. Available from https://www.elsevier.com/solutions/clinicalkey
- Trip Medical Database [Internet]. Available from https://www.tripdatabase.com
- DynaMed Plus [Internet]. Available from http://www.dynamed.com/home/
- Scottish Intercollegiate Guidelines Network [Internet]. Available from https://www.sign.ac.uk/
- CADTH Grey Matters Tool [Internet]. Available from https://www.cadth.ca/resources/finding-evidence/grey-matters
- Guidelines International Network [Internet]. Available from https://www.g-i-n.net/home
- Physiotherapy Evidence Database Ratings (PEDro) [Internet]. Available from https://www.pedro.org.au/
- Consortium ANS. Appraisal of Guidelines for Research & Evaluation II - User Manual [Internet]. Available from: https://www.agreetrust.org/wp-content/uploads/2013/06/AGREE_II_Users_Manual_and_23-item_Instrument_ENGLISH.pdf.
- Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. Development of the AGREE II, part 1: performance, usefulness and areas for improvement. Cmaj 2010;182(10):1045–1052.
- Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. Development of the AGREE II, part 2: assessment of validity of items and tools to support application. Cmaj 2010;182(10):E472–E478.
- Ciliska DK, Pinelli J, DiCenso A, Cullum N. Resources to enhance evidence-based nursing practice. AACN Adv Crit Care 2001;12(4):520–528.
- Davies BL. Sources and models for moving research evidence into clinical practice. J Obstet Gynecol Neonatal Nurs 2002;31(5):558–562.
- Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 2001;39(8, Supplement II):II46–II54.
- Hurdowar A, Graham ID, Bayley M, Harrison M, Wood-Dauphinee S, Bhogal S. Quality of stroke rehabilitation clinical practice guidelines. J Eval Clin Pract 2007;13(4):657–664.
- Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C, et al. IX: Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 2002;23(4):570–578.
- Graham ID, Beardall S, Carter AO, Glennie J, Hébert PC, Tetroe JM, et al. What is the quality of drug therapy clinical practice guidelines in Canada? Cmaj 2001;165(2):157–163.
- Gerber LH, Bush H, Cai X“, Morse L, Worobey L, Garfinkel S. Scoping review of peer reviewed publications addressing rehabilitation for people sustaining traumatic spinal cord injury. J Spinal Cord Med 2020;43(4):421–427.