Abstract
Context
Although self-management is linked to reduced secondary health complications (SHCs) and enhanced overall quality of life post-spinal cord injury or disease (SCI/D), it is poorly integrated into the current rehabilitation process. Promoting self-management and assuring equity in care delivery is critical. Herein, we describe the selection of Self-Management structure, process and outcome indicators for adults with SCI/D in the first 18 months after rehabilitation admission.
Methods
Experts in self-management across Canada completed the following tasks: (1) defined the Self-Management construct; (2) conducted a systematic search of available outcomes and their psychometric properties; and (3) created a Driver diagram summarizing available evidence related to Self-Management. Facilitated meetings allowed development and selection following rapid-cycle evaluations of proposed structure, process and outcome indicators.
Results
The structure indicator is the proportion of staff with appropriate education and training in self-management principles. The process indicator is the proportion of SCI/D inpatients who have received a self-management assessment related to specific patient self-management goal(s) within 30 days of admission. The outcome indicator is the Skill and Technique Acquisition, and Self-Monitoring and Insight subscores of the modified Health Education Impact Questionnaire.
Conclusion
The structure indicator will heighten awareness among administrators and policy makers regarding the need to provide staff with ongoing training related to promoting self-management skill acquisition. Successful implementation of the Self-Management process and outcome indicators will promote self-management education and skill acquisition as a rehabilitation priority, allow for personalization of skills related to the individual’s self-management goal(s), and empower individuals with SCI/D to manage their health and daily activities while successfully integrating into the community.
Introduction
Damage to the spinal cord following injury or disease causes profound changes in nearly all of the body system, the individual’s functional abilities, and may affect their ability to independently manage their health. In addition to the initial adjustment to the disability (e.g. sensory, motor, autonomic impairments), individuals with spinal cord injury or disease (SCI/D)Citation1 also typically experience a number of secondary health conditions (SHCs) and often undergo psychosocial adjustment to their disability,Citation2 which may include reduced self-esteem and self-efficacy (one’s belief in their abilities to meet the demands of a situation)Citation3 as well as the possibility of dealing with a comorbid mood disorder.Citation2 As a result of the SHCs, individuals with SCI/D and their informal care networks (e.g. family members) may mitigate or manage these health conditions that may arise throughout their lives.Citation4 Furthermore, length-of-stay (LOS) in tertiary SCI/D rehabilitation has significantly reduced over time,Citation5,Citation6 which provides less opportunity to prepare individuals with SCI/D entering the community to attain sufficient knowledge and self-management skills to prevent and/or manage their SHCs.Citation5,Citation7
Common SHCs after SCI/D include urinary tract infections (UTIs), tissue injuries, bowel and bladder dysfunctions, chronic pain, heart disease, sexual disorders, and depression.Citation8,Citation9 SHCs can result in service interruptions during rehabilitation, increase morbidity, and contribute to the observed high physician and emergency department (ED) visit rates in this population.Citation10–12 A recent Ontario (Canada) study found that service interruptions due to SHCs resulted in a mean nine day disruption in inpatient rehabilitation.Citation10 Furthermore, while many SHCs are preventable, they are key contributors to rehospitalization in the post-acute phase,Citation13,Citation14 and are particularly so within the first year post-discharge.Citation9 A Canadian study conducted by Noonan and colleaguesCitation11 identified that individuals with SCI living in the community have high healthcare utilization; multimorbidity being a significant factor associated with inappropriate healthcare utilization, and together were linked with lower health status. With respect to ED visits, Guilcher and colleaguesCitation12 reported that there are high rates of ED use for low acuity and potentially preventable SHCs, suggesting that the ED is being used inappropriately among individuals with traumatic SCI. Even after 20 years post-injury, rehospitalization rates continue to be high (i.e. more than 30%) due to the cumulative effects of SCI-related SHCs as well as the comorbidities related to aging.Citation13 Overall, these studies suggest that individuals with SCI/D are high users of the healthcare system due to their SCI-related health challenges, and are often seeking support in less-than-ideal care settings (e.g. ED); indicating that this population may not be well-prepared to manage their health long-term. Indeed, evidence pointing towards a high prevalence of reported SHCs (e.g. 95.6% of patients with SCI had at least one medical condition at the time of their annual check-up),Citation15 suggests that the majority of individuals with SCI lack sufficient self-management education and skills.Citation16,Citation17 Studies have also reported that family members who provide care to individuals with SCI are not well-equipped to attend to the specialized needs of their injured family member.Citation4,Citation18,Citation19
Considering the health and economic consequences of SCI/D, there have been substantial efforts put forth towards developing interventions enhancing self-management education and knowledge among individuals with SCI/D during rehabilitation care. These interventions have predominately focused on education as the foundation for instilling change;Citation20 and often informed by key self-management components, including problem-solving, decision-making, action planning, self-monitoring/tailoring, resource utilization, and formation of patient-provider partnership.Citation21,Citation22 Several studies have reported that patient education promoting self-management has been effective in addressing a range of issues post-SCI, including decreasing the occurrence of SHCs such as pressure injuries, UTIs,Citation23–25 while promoting better emotional well-being and coping skills,Citation26 fostering health promotion,Citation27 and enhancing community participation.Citation28,Citation29 Similar to self-management approaches used in other chronic disease groups (e.g. stroke, diabetes, traumatic brain injury), there is no “gold standard” on what constitutes self-management in a SCI/D population.Citation30,Citation31 This lack of consensus of what is self-management reflects that it is a rather complex and multifaceted construct, which makes it challenging to measure self-management outcomes.
Although knowledge related to self-management preparation (e.g. educational interventions) prior to discharge is emerging within Canada,Citation32 there are inconsistent practices across tertiary rehabilitation hospitals, suggesting there is a lack of equity in national care for this population with regards to this domain. Hence, to ensure a broader approach to self-management skill acquisition across the country, efforts are needed, nationally, to address the current gaps in care and advance self-management education and skill acquisition within rehabilitation settings with the goal of improving standards of SCI/D rehabilitation in Canada. Implementation of quality of care indicators can build equity and access to care, identify trends, and inform policy formulation, and monitor rehabilitation programs and care processes.Citation33,Citation34 Indicators can measure the structure, process or outcome of health care services and their evaluation can facilitate the sustainability of a high-quality health care delivery system that is based on evidence-informed programs and services.Citation33 Structure indicators are defined by the properties of the setting in which the health care services occurCitation35 while process indicators describe the specific activities in providing and receiving of care.Citation36 Finally, outcome indicators evaluate health improvements (or deterioration) that can be attributed to the health care or therapy provided, such as mortality, morbidity, health status, health-related quality of life, patient/family/provider satisfaction, and functional ability.Citation36
The SCI Rehabilitation Care High Performance Indicators or “SCI-High Project” is a nationwide endeavor to develop/select, implement and evaluate consensus derived quality of care indicators for 11 domains of rehabilitation prioritized by clinicians, researchers and individuals living with chronic SCI/D. This report describes the processes involved in the selection, development and implementation of structure, process and outcome indicators related to the Self-Management Domain from rehabilitation admission to 18 months thereafter.
Methods
A detailed description of the overall SCI-High Project methods and process for identifying “Self-Management” as a priority domain for SCI rehabilitation care are described in related manuscripts.Citation37,Citation38 In addition to the SCI-High investigative team (www.sci-high.ca), an external advisory committee and national data strategy committee supported the global project goals and provided oversight regarding the context for implementing all of the planned indicators.
The approach to developing the Self-Management Domain’s structure, process and outcome indicators followed a slightly modified version of the processes described by Mainz,Citation39 which included the following planning and development phases: (a) formation and organization of the national and local Working Groups; (b) defining and refining the key domain and specific target construct; (c) providing an overview/summary of existing evidence and practice; (d) developing and interpreting a Driver diagram (i.e. visual display of a high-level quality improvement goal, and a set of underpinning factors/goalsCitation40); (e) selecting indicators; and (f) pilot testing and refinement of the domain-specific structure, process and outcome indicators. Throughout these processes, a facilitated discussion occurred amongst the domain-specific Working Group and the SCI-High Project Team to capitalize on the relevant expertise of the different stakeholders on the topic while ensuring that the broader goals of the SCI-High Project were aligned across the other 10 domain Working Groups (as appropriate). The selected indicators will be integrated into the larger SCI-High Project framework to create a group of indicators and related best practices for routine implementation within a single rehabilitation program with project-wide report cards enabling cross site comparisons of structure, process and outcomes.
Self-Management Working Group
Experts in self-management and relevant stakeholders were invited to participate in the SCI-High Project as members of the domain-specific Working Group based on their practical or empirical knowledge of SCI/D rehabilitation, self-management, health service delivery and patient education. The group was composed of practitioners, rehabilitation scientists, patient and family educators, partners from community organizations, policy leaders, researchers, and a stakeholder with lived experience. The Working Group met 13 times via conference call over an 18-month period; totaling 17 h of discussion related to the development of the indicators to refine the indicators and discuss manuscript preparation. Outside of the formal meeting, individual members of the Working Group completed an additional review of the prepared materials, shared resources and/or practice standards with one another, or conducted independent evaluations of the proposed indicators.
Driver diagram and construct definition
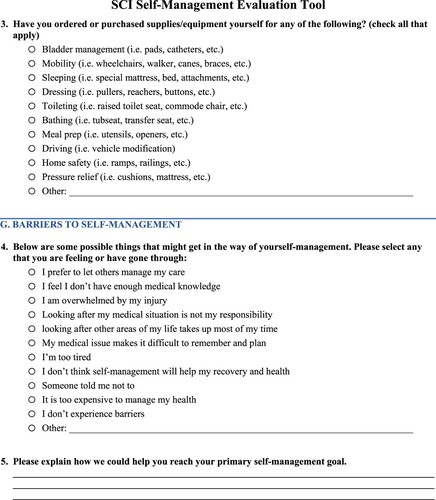
The selection of Self-Management as a domain of interest for developing indicators emerged from a consensus-building activity to select the broader set of domains being pursued within the overarching SCI-High Project.Citation38 This process involved a systematic search to collect information about SCI/D rehabilitation care related to self-management, identification of factors that influence the outcome of rehabilitation interventions, and a scoping synthesis of the data acquired. The MEDLINE, EMBASE and CINAHL databases were searched using the combination of the terms “self-management” and “spinal cord injury” (similar terms were selected for each database). This information was then used to create a Driver diagram to illustrate known drivers or factors that impact self-management among individuals with SCI/D (). The Driver diagram helped to organize change concepts as the Working Group discerned “what changes can we make, that will result in goal attainment”. The branches in red within the final Driver diagram represent the main areas that were the focus for development of indicators based on experts’ opinions.
Figure 1 Self-management Driver diagram. The impairment branch is common to the 11 SCI-High Project domains. UEMS: Upper-Extremity Motor Score, LEMS: Lower-Extremity Motor Score, NLI: Neurological Level of Injury, AIS: ASIA Impairment Scale, HR: Heart Rate, BP: Blood Pressure, UTI: Urinary Tract Infection. *: Self-Efficacy, although relevant in Self-Management, has been used as an outcome measure for the Community Participation Domain (66).
Following review of the systematic searches, discussions, and multiple refinements of the Driver diagram, the group agreed that self-management skill acquisition to help individuals with SCI/D to manage their health and daily activities towards successful community integration was the driver most likely to advance SCI/D rehabilitation care in the near term. Based on this discussion, and reflection upon current terminologies, the following construct definition was created:
Self-management relates to the tasks and skills that an individual must undertake to live well with a SCI/D. These tasks and skills include having or gaining the confidence and problem-solving abilities to deal with medical management, role management and emotional management.
Selection of indicators
Consistent with the methodology used in the SCI-High Project, the Working Group was asked to develop/select at least one indicator each for structure, process and outcome in relation to the Self-Management Domain. The Project Leaders stipulated that the indicators should be relevant, concise and feasible to implement (10 min or less), and aligned across the structure, process and outcome to achieve a single substantive advance in SCI/D rehabilitation care. The indicators could be measured using established or new measurement tools (i.e. questionnaires, data collection sheets, laboratory exams, and medical record data), depending on the requirements and feasibility of a given indicator. The Working Group felt that the process indicator should inform the specific self-management skills required by individuals with SCI/D post-discharge into the community (e.g. gathering information, medication management, symptom management, self-advocacy, etc.). The Working Group reviewed several skill inventories and identified constructs of importance prior to selecting the process indicator. The Working Group’s intent was to create a process indicator that would inform the outcome indicator and vice-versa, yet allow for individualized goal setting and assure the selected indicators would be of relevance across a variety of individual patient goals. The time constraints for indicator assessment also drove the Working Group’s decision making and indicator selection. The Working Group chose to refine an existing tool (SCI Self-Management Evaluation Tool (SCI-SMET)) acceptable to patient’s with SCI/D rather than creating a new tool de novo.
Indicator piloting and refinement
The refinement of the indicators related to Self-Management were primarily driven by the impetus to promote self-management skill acquisition to ensure individuals with SCI/D can manage their health and daily activities toward successful community integration (as depicted in and the construct definition). The Working Group focused on the structure indicator in order to inform the development of the process and outcome indicators. To promote self-management among people with SCI/D, the feasibility of the structure and process indicators for the Self-Management Domain was pilot tested. The indicator was reviewed and refined through multiple quality improvement Plan-Do-Study-Act (PDSA)Citation34 cycles for quick qualitative evaluations, feedback and refinement. The structure indicator pilot data will be used to create a consensus definition of self-management “training and skills”.
Results
Indicator development
The indicators selected by the Self-Management Working Group are shown in , which specifies the type of indicator, denominators, and timing of measurement for each of the selected indicators.
Table 1 Selected structure, process and outcome indicators for the Self-Management Domain.
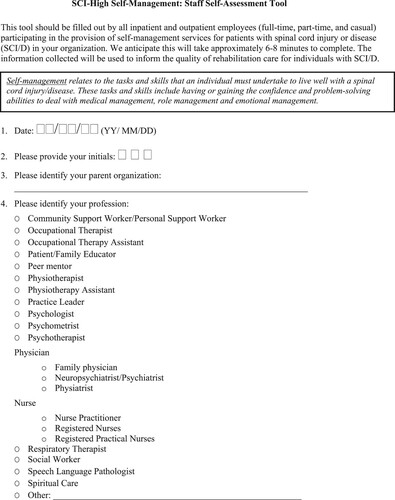
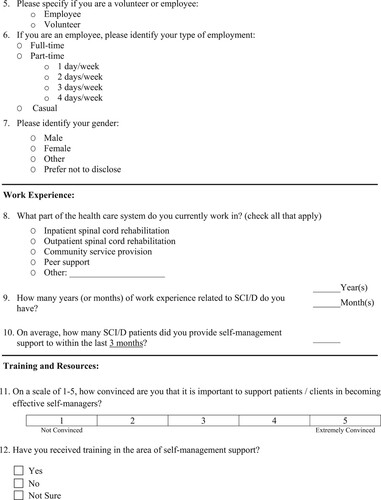
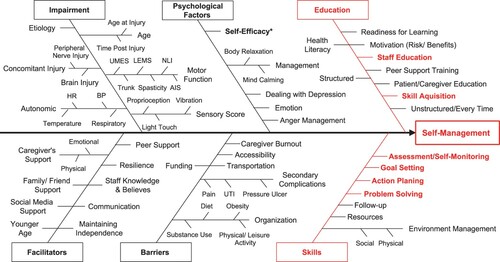
The structure indicator is a self-management staff self-assessment tool, which will be completed by any SCI rehabilitation Health Care Professionals (HCP) or peer mentor to assess their self-management training, skills, level of comfort and confidence to effectively provide self-management support to individuals with SCI/D (structure indicator; ).
Figure 2 SCI-High self-management staff self-assessment tool. Structure indicator SCI-High self-management self-assessment tool to assess self-management training and skills of SCI rehabilitation healthcare professionals and peer mentors involved in the provision of self-management services.
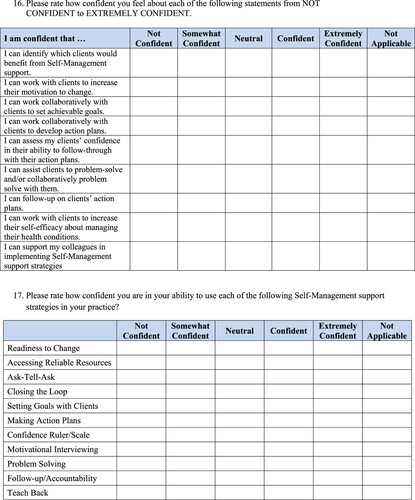
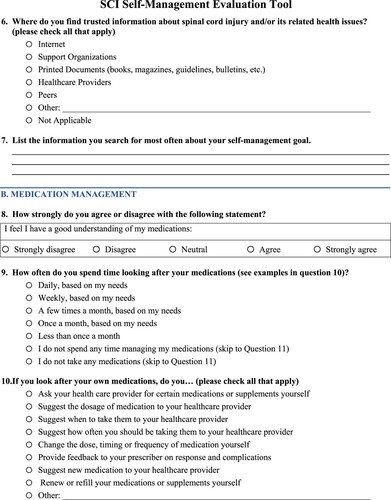
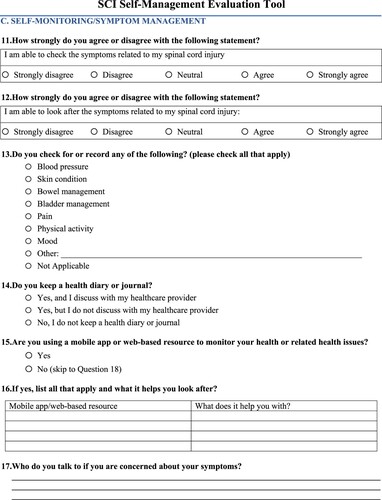
The process indicator related to Self-Management is the proportion of SCI/D inpatients who have received a self-management assessment within 30 days of admission (process indicator; ). The Working Group refined the SCI-SMET (i.e. based on the above-mentioned requirements and restrictions) of the original tool developed by Dr. Gary Linassi (author) and colleagues from the Saskatchewan Health Authority. The SCI-SMET was developed with specific self-management constructs in mind, including: goal setting, problem-solving, action planning, and self-monitoring. Goal setting is the process by which one identifies specific goals and determines how they will be achieved.Citation41 Problem-solving implies a behavioral process which (a) makes available a variety of response alternatives for dealing with a problematic situation and (b) increases the probability of selecting the most effective response from among these alternatives.Citation42 Action planning denotes where, when, and how a goal will be implemented and help individuals plan the specific actions they will take to achieve their overarching goal.Citation41 Finally, self-monitoring is part of managing many chronic conditions, and comprises of two major attributes or central components: (1) awareness of bodily symptoms, sensations, daily activities, and cognitive processes and (2) measurements, recordings, or observations that inform cognition and provide information for independent action or consultation with care providers.Citation43 Together, these constructs could drive behavior change and enhance patient self-management. The SCI-SMET allows HCPs to document and have facilitated conversations regarding specific patient self-management goals, as well as a level of confidence in carrying out self-management behaviors and barriers to self-management.
Figure 3 SCI self-management evaluation tool (SCI-SMET). Process indicator SCI-SMET for healthcare professionals to document specific patient self-management goals and assess level of confidence in carrying out self-management behaviors and barriers to self-management.
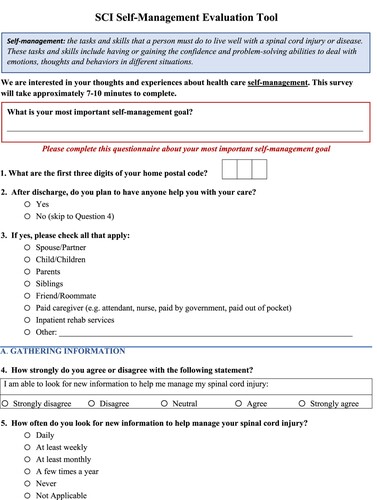
With respect to the outcome indicator, several meetings were held discussing relevant, valid and reliable tools to measure the effect of self-management/patient education programs (e.g. self-management skills acquisition; refer to for the outcome measures table). Following a review of available literature, a relevant tool was agreed upon: Health Education Impact Questionnaire (heiQ).Citation49 The heiQ is a user-friendly, appropriate and psychometrically sound tool designed to measure the effect of self-management/health education programs based on patients’ perspectives. The heiQ offers a new approach to measuring behavioral, cognitive and emotional responses and fills a vital gap in patient-centered outcome assessment related to self-management. Studies using heiQ found that it captured various aspects (i.e. dimensions mentioned below) other than standard measures typically used to assess self-management,Citation65 such as self-efficacy (e.g. Moorong Self-Efficacy Scale (MSES)). Furthermore, the Working Group felt that since the Community Participation Domain (manuscript submitted for publication)Citation66 will use the MSES to assess and collect data on self-efficacy of individuals with SCI/D as the outcome measure, the Self-Management outcome indicator should focus on a tool that measures the effect of self-management/health education programs. The heiQ consists of eight independent dimensions, including: Positive and Active Engagement in Life; Health Directed Behaviour; Skill and Technique Acquisition; Constructive Attitudes and Approaches; Self-Monitoring and Insight; Health Service Navigation; Social Integration and Support; and Emotional Wellbeing.
Table 2 Self-management outcome measures.
The Working Group felt two of the dimensions and their related items (Skill and Technique Acquisition, and Self-Monitoring and Insight) were the most relevant to our goal of acquisition of specific self-management skills required by individuals with SCI/D, which is consistent with the process indicator tool (outcome indicator; see for the modified heiQ). The participants will be asked to rate their confidence in their ability to complete specific tasks on 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The Skill and Technique dimension captures the knowledge-based skills and techniques that help patients manage disease-related symptoms and health problems more effectively. High scores are characteristic of an individual who has highly developed skills related to symptom relief and techniques to manage their own health. The Self-Monitoring and Insight dimension captures the patients’ ability to monitor their conditions, and their physical and/or emotional responses that lead to insight and appropriate actions to self-manage. High scores identify self-monitoring, self-management, setting reasonable targets, and insight into living with a health problem.Citation49 Recognizing that individuals with SCI/D are likely to continue to acquire self-management skills post-discharge, the Working Group decided that the two time points for completing the modified heiQ would be prior to rehabilitation discharge and 18 months post-rehabilitation admission. The heiQ has high construct validity and has reliable measures of key dimensions related to self-management behaviors, which could be easily incorporated into assessment practice in a rehabilitation setting in order to advance goals of self-management programs.Citation65,Citation67,Citation68
Table 3 Self-management outcome indicator tool- modified Health Education Impact Questionnaire (m-heiQ).
Self-Management indicator piloting
Pilot study results- structure indicator
The pilot data regarding the self-management training and skills includes results from six SCI rehabilitation HCPs who completed the staff self-assessment tool. The tool was completed within an average of 14 min. The majority of the participants reported they received training in the area of self-management support, and have participated in educational opportunities for the purpose of learning about self-management in SCI (e.g. Clinician Influence and Patient Action, Stages of Change, Teach Back, etc.). Regarding the level of confidence in effectively providing self-management support to patients with SCI, the majority reported they are confident (on a scale from 1-not confident to 5-extremely confident). Feasibility issues and challenges experienced included: (1) more time required when tracking down specific education and training-related information (e.g. courses attended); (2) tool was not applicable considering the individual did not receive formal training due to limited work experience; (3) required clarifications (e.g. how much time needs to be allocated with each patient to be considered providing self-management support); and (4) difficulty completing the tool in electronic form.
Pilot study results- process indicator
To optimize workflow (i.e. conducting self-management assessments), the feasibility of the SCI-SMET was pilot tested in an adult outpatient clinic at a tertiary SCI rehabilitation hospital in a large urban center. Consecutive patients attending routine follow-up appointments, as well as inpatients, were approached by trained evaluators to complete the tool. The pilot data includes results from eight patients. The tools were completed within an average of 7–10 min. Noted feasibility issues and challenges included: (1) the impact of cognitive and motor deficits on the ability to self-administer the tool; (2) inability to understand certain aspects of the tool (i.e. clarifications needed on specific language [e.g. emotional management]); and (3) additional time taken by patients to discuss the responses in depth.
Discussion
Self-management is a critical skill for enabling persons with SCI/D to maintain their health and wellbeing long-term in the community. Despite the growing awareness of self-management practices within Canada,Citation32 these practices are inconsistently applied across tertiary rehabilitation hospitals. To help address this inequity, the SCI-High Self-Management Working Group selected and developed structure, process and outcome indicators intended to: (1) identify learning gaps and improve capacity among rehabilitation HCPs and peer mentors in self-management; (2) promote documentation and integration of self-management skill acquisition into the rehabilitation process; and (3) help individuals with SCI/D acquire the necessary skills to manage their health and daily activities toward successful community integration.
It is vital to recognize that in order to enhance self-efficacy and practice self-management, individuals with SCI must first have appropriate knowledge and skills pertinent to managing their injury.Citation17,Citation69 The first step towards addressing this issue of enhancing self-management education and skills is enabling facilitated conversations regarding specific patient self-management priorities and learning needs. The selected process indicator will provide an opportunity for HCPs to assess and understand patients’ individual self-management goals, barriers to self-management and level of confidence in carrying out self-management behaviors, in order to direct care accordingly. The patients’ responses are intended to guide self-management education provided by a rehabilitation professional by focusing on what they report are most important to them. Targeted and personalized management along with patient-mediated strategies are critical in implementing a self-management intervention (i.e. interventions enhancing self-management education and knowledge).Citation70 This should begin in the inpatient setting prior to discharge from rehabilitation and carry over as they reintegrate into the community.Citation32
Although the importance of educating individuals with SCI/D and their family members about self-management is recognized, including how to prevent SHCs, there is a shortage of qualified HCPs to provide such self-management education.Citation71 Due to the relatively low prevalence of individuals with SCI/D, only a few primary HCPs have individuals with SCI/D in their practice.Citation72 Thus, the majority of the primary care providers do not often have much opportunity to obtain adequate training and sufficient knowledge and skills to provide self-management education to their patients.Citation73 To assist the various disciplines of HCPs in the rehabilitation setting in providing self-management education and helping the individuals with SCI/D to manage their health and daily activities toward successful community integration, the Self-Management Working Group felt there should be an initiative to enhance staff capacity- in other words, continuing education hours toward developing/enhancing their training and skills specific to self-management. A first step to enhancing capacity in this domain of care across Canada is to determine what extent staff training incorporates the best methods to facilitate self-management skill development among individuals with SCI/D, and whether these processes are conducted and/or documented appropriately during inpatient rehabilitation. Doing so will provide important knowledge about the state of self-management across Canada in SCI/D rehabilitation where there is an increasing need to ensure equity of access to clinical care across the country.Citation38 Further, it will help build capacity in HCPs working in rehabilitation, as well as foster a culture conducive to self-management across the continuum of care. The indicators developed by the Working Group are projected to create a new minimum threshold of self-management knowledge and skills among HCPs to identify and address the self-management needs of individuals with SCI/D and their family members in the first 18 months post inpatient rehabilitation admission.
One challenge is that some healthcare providers at tertiary rehabilitation centers have adequate self-management education and training, but there may not be any appropriate documentation of their practice. There is an increasing need to ensure equity of access to clinical care nationally to optimize the quality of care by standardizing the timing and format of self-management assessments during inpatient rehabilitation, as well as in the community using valid and reliable assessment tools. Therefore, our developed process indicator aims to address this gap by ensuring appropriate documentation of the facilitated conversations with patients regarding specific self-management goals.
A few potential barriers with the proposed indicators should be considered. First, self-management is a complex and challenging construct to measure in a condensed timeframe. For example, each individual with SCI/D goes through a unique journey (based on specific injury conditions, age, sex, etc.), and self-management education and skill needs will be continuously evolving depending on the timing and setting across the care trajectory and the individuals psychosocial and environmental context. Thus, the assessment of self-management needs and accompanying strategies during these time points in an individual’s journey are unique to the individual and vary in complexity. Furthermore, the Project Leaders agreed that the indicators should be concise and feasible to implement (i.e. within 10 min), which may have compromised a comprehensive assessment. In addition, these indicators were designed for use by any health care professional, not just someone with a psychology background, therefore, they are grounded in skill acquisition, not theory. Although this approach allows for universal usability, it does not deter a psychologist/social worker from conducting an intimate comprehensive assessment in addition to the indicators and related practices. To add, readiness to receive self-management education is difficult to assess due to the fact that individuals with SCI/D also evolve in their readiness to gain new information related to managing their health and integrating back into the community post-SCI. At this stage, the Working Group is aiming to identify tools to assess “readiness” (to receive self-management education). Regardless, these initial indicators were intentionally developed to be feasible at critical SCI rehabilitation transition points, which can help to set the stage for nationwide validation and benchmarking to advance access to appropriate care.
Conclusion
Successful implementation of the selected structure, process and outcome indicators and related best practices for Self-Management will simultaneously promote self-management education and skill acquisition as a rehabilitation priority and empower individuals with SCI/D to manage their health and daily activities towards successful community integration. Moreover, self-management interventions are not well-developed and there is a pressing need for directed research to bolster evidence underlying the service delivery gaps to better integrate self-management education into SCI/D rehabilitation care process. More importantly, providing self-management education when the individual is ready to engage in this learning as soon after injury as possible will likely lead to a decrease in the onset of SHCs as individuals with SCI/D will be better equipped to self-manage their health in the community, and in return, reduce the burden on the Canadian healthcare system.
Disclaimer statements
Contributors None.
Funding This work is embedded in the larger SCI-High Project funded by Praxis Spinal Cord Institute (former Rick Hansen Institute – Grant #G2015-33), Ontario Neurotrauma Foundation (ONF – Grant #2018-RHI-HIGH-1057), Ontario Neurotrauma Foundation (Consortium TRI Site Grant#2019-RHI-SITE1-1065), Ontario Neurotrauma Foundation (Consortium Implementation Grant #2019-RHI-IMPLEM-1064), and the Toronto Rehab Foundation.
Conflicts of interest Dr. Gaya Jeyathevan is funded by the Craig H. Neilsen Foundation (G#594918). Dr. B. Catharine Craven acknowledges support from the Toronto Rehab Foundation as the Toronto Rehabilitation Institute Chair in Spinal Cord Injury Rehabilitation, and receipt of consulting fees from the Praxis Spinal Cord Institute. Dr. Vanessa K. Noonan is an employee of the Praxis Spinal Cord Institute. Dr. Susan B. Jaglal, Dr. Sander L. Hitzig, Sandra Mills, Karen Anzai, Teren Clarke, Dr. Dalton Wolfe, Dr. Mark Bayley, Lubna Aslam, Dr. S. Mohammad Alavinia, Farnoosh Farahani, and Maryam Omidvar report no conflicts of interest.
Acknowledgements
We would like to thank Dr. Matheus J. Wiest and Heather Flett from the Toronto Rehabilitation Institute (University Health Network), and Peter Athanasopoulos from the Spinal Cord Injury Ontario for their valuable contributions during the development of the Self-Management indicators.
References
- Hou S, Rabchevsky AG. Autonomic consequences of spinal cord injury. Compr Physiol 2014;4(4):1419–53.
- Migliorini C, Tonge B, Taleporos G. Spinal cord injury and mental health. Aust N Z J Psychiatry 2008;42(4):309–14.
- Luszczynska A, Schwarzer R. Social cognitive theory. In: Predicting health behaviour. 2nd ed. New York (NY): Open University Press, McGraw Hill; 2005. p. 127–69.
- McColl MA, Aiken A, McColl A, Sakakibara B, Smith K. Primary care of people with spinal cord injury: scoping review. Can Fam Physician 2012;58(11):1207–16. e626–35.
- Crewe NM, Krause JS. Spinal cord injury. In: Medical, psychosocial and vocational aspects of disability. 3rd ed. Athens: Elliott & Fitzpatrick, Inc.; 2009. p. 289–304.
- Whiteneck G, Gassaway J, Dijkers M, Backus D, Charlifue S, Chen D, et al. The SCIRehab project: treatment time spent in SCI rehabilitation. inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med 2011;34(2):133–48.
- Chen D, Nussbaum SB. The gastrointestinal system and bowel management following spinal cord injury. Phys Med Rehabil Clin N Am 2000;11(1):45–56. viii.
- Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K, et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil 2008;87(7):545–55.
- Paker N, Soy D, Kesiktas N, Nur Bardak A, Erbil M, Ersoy S, et al. Reasons for rehospitalization in patients with spinal cord injury: 5 years’ experience. Int J Rehabil Res 2006;29(1):71–6.
- Bhide R, Rivers C, Kuerban D, Chen J, Farahani F, Flett H, et al. Service interruptions’ and their impact on rehabilitation length of stay among Ontarians with traumatic, subacute spinal cord injury. Crit Rev Phys Rehabil Med 2018;30:45–66.
- Noonan VK, Fallah N, Park SE, Dumont FS, Leblond J, Cobb J, et al. Health care utilization in persons with traumatic spinal cord injury: the importance of multimorbidity and the impact on patient outcomes. Top Spinal Cord Inj Rehabil 2014;20(4):289–301.
- Guilcher SJ, Craven BC, Lemieux-Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil 2013;35(11):894–906.
- DeVivo MJ, Chen Y. Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehabil 2011;92(3):332–8.
- Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004;42(9):513–25.
- Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996;19(1):55–66.
- Pang MY, Eng JJ, Lin KH, Tang PF, Hung C, Wang YH. Association of depression and pain interference with disease-management self-efficacy in community-dwelling individuals with spinal cord injury. J Rehabil Med 2009;41(13):1068–73.
- Piatt JA, Nagata S, Zahl M, Li J, Rosenbluth JP. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. J Spinal Cord Med 2016;39(6):693–8.
- Jeyathevan G, Catharine Craven B, Cameron JI, Jaglal SB. Facilitators and barriers to supporting individuals with spinal cord injury in the community: experiences of family caregivers and care recipients. Disabil Rehabil 2020;42(13):1844–54.
- Robinson-Whelen S, Rintala DH. Informal care providers for veterans with SCI: who are they and how are they doing? J Rehabil Res Dev 2003;40(6):511–6.
- McIntyre A, Marrocco SL, McRae SA, Sleeth L, Hitzig S, Jaglal S, et al. A scoping review of self-management interventions following spinal cord injury. Top Spinal Cord Inj Rehabil 2020;26(1):36–63.
- Hirsche RC, Williams B, Jones A, Manns P. Chronic disease self-management for individuals with stroke, multiple sclerosis and spinal cord injury. Disabil Rehabil 2011;33(13-14):1136–46.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26(1):1–7.
- Barber DB, Woodard FL, Rogers SJ, Able AC. The efficacy of nursing education as an intervention in the treatment of recurrent urinary tract infections in individuals with spinal cord injury. SCI Nurs 1999;16(2):54–6.
- Garber SL, Rintala DH, Rossi CD, Hart KA, Fuhrer MJ. Reported pressure ulcer prevention and management techniques by persons with spinal cord injury. Arch Phys Med Rehabil 1996;77(8):744–9.
- Kroll T, Neri MT, Ho PS. Secondary conditions in spinal cord injury: results from a prospective survey. Disabil Rehabil 2007;29(15):1229–37.
- Craig A, Hancock K, Chang E, Dickson H. The effectiveness of group psychological intervention in enhancing perceptions of control following spinal cord injury. Aust N Z J Psychiatry 1998;32(1):112–8.
- Chen HY, Wu TJ, Lin CC. Improving self-perception and self-efficacy in patients with spinal cord injury: the efficacy of DVD-based instructions. J Clin Nurs 2015;24(11-12):1666–75.
- Craig AR, Hancock K, Dickson H, Chang E. Long-term psychological outcomes in spinal cord injured persons: results of a controlled trial using cognitive behavior therapy. Arch Phys Med Rehabil 1997;78(1):33–8.
- Curcoll ML. Psychological approach to the rehabilitation of the spinal cord injured: the contribution of relaxation techniques. Paraplegia 1992;30(6):425–7.
- Delparte JJ, Chau BA, Mills S, Burns AS. Spinal cord essentials: the development of an individualized, handout-based patient and family education initiative for people with spinal cord injury. Spinal Cord 2014;52(5):400–6.
- Houlihan B, DeJoie C, Williams S. The internet as a treatment modality: a model program for clients with SCI. OT Pract 2007;12(19):10.
- Wolfe DL, Mills S, Shepherd J, Craven BC. Informed self-management. In: Rehabilitation environmental scan atlas: capturing capacity in Canadian SCI rehabilitation. Rick Hansen Institute; 2012. p. 159–66.
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord 2013;51(2):165–9.
- Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. John Wiley & Sons; 2009.
- Idvall E, Rooke L, Hamrin E. Quality indicators in clinical nursing: a review of the literature. J Adv Nurs 1997;25(1):6–17.
- Selim AJ, Berlowitz DR, Fincke G, Rosen AK, Ren XS, Christiansen CL, et al. Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Med Care 2002;40(3):237–45.
- Alavinia SM, Hitzig SL, Farahani F, Flett H, Bayley M, Craven BC. Prioritization of rehabilitation domains for establishing spinal cord injury high performance indicators using a modification of the hanlon method: SCI-High project. J Spinal Cord Med 2019;42(sup1):43–50.
- Craven BC, Alavinia SM, Wiest MJ, Farahani F, Hitzig SL, Flett H, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High project. J Spinal Cord Med 2019;42(sup1):51–67.
- Mainz J. Developing evidence-based clinical indicators: a state of the art methods primer. Int J Qual Health Care 2003;15(Suppl 1):5i–11.
- Phillips J, Simmonds L. Using fishbone analysis to investigate problems. Nurs Times 2013;109(15):18–20.
- Bailey RR. Goal setting and action planning for health behavior change. Am J Lifestyle Med 2019;13(6):615–8.
- D'Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol 1971;78(1):107–26.
- Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs 2007;57(3):339–50.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 1965;14:61–5.
- Cress ME, Petrella JK, Moore TL, Schenkman ML. Continuous-scale physical functional performance test: validity, reliability, and sensitivity of data for the short version. Phys Ther 2005;85(4):323–35.
- Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing 1983;12(2):166–70.
- Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the functional independence measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1471–76.
- Masedo AI, Hanley M, Jensen MP, Ehde D, Cardenas DD. Reliability and validity of a self-report FIM (FIM-SR) in persons with amputation or spinal cord injury and chronic pain. Am J Phys Med Rehabil 2005;84(3):167–76; quiz 77-9, 98.
- Osborne RH, Elsworth GR, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns 2007;66(2):192–201.
- Klein R. The Klein–Bell ADL scale manual. Seattle (WA): University of Washington Medical School; 1979.
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9(3):179–86.
- Middleton JW, Tate RL, Geraghty TJ. Self-Efficacy and spinal cord injury: psychometric properties of a new scale. Rehabil Psychol 2003;48(4):281–8.
- Jensen MP, Nielson WR, Kerns RD. Toward the development of a motivational model of pain self-management. J Pain 2003;4(9):477–92.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39(4 Pt 1):1005–26.
- Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav 1978;19(1):2–21.
- Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 2002;83(2):193–200.
- Gresham GE, Labi ML, Dittmar SS, Hicks JT, Joyce SZ, Stehlik MA. The Quadriplegia index of function (QIF): sensitivity and reliability demonstrated in a study of thirty quadriplegic patients. Paraplegia 1986;24(1):38–44.
- Marino RJ, Goin JE. Development of a short-form Quadriplegia index of function scale. Spinal Cord 1999;37(4):289–96.
- Boss BJ, Barlow D, McFarland SM, Sasser L. A self-care assessment tool (SCAT) for persons with a spinal cord injury: an expanded abstract. Axone 1996;17(3):66–7.
- Tulsky DS, Jette AM, Kisala PA, Kalpakjian C, Dijkers MP, Whiteneck G, et al. Spinal cord injury-functional index: item banks to measure physical functioning in individuals with spinal cord injury. Arch Phys Med Rehabil 2012;93(10):1722–32.
- Pruitt SD, Wahlgren DR, Epping-Jordan JE, Rossi AL. Health behavior in persons with spinal cord injury: development and initial validation of an outcome measure. Spinal Cord 1998;36(10):724–31.
- Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM – spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997;35(12):850–6.
- Hoenig H, Hoff J, McIntyre L, Branch LG. The self-reported functional measure: predictive validity for health care utilization in multiple sclerosis and spinal cord injury. Arch Phys Med Rehabil 2001;82(5):613–8.
- Eikelenboom N, Smeele I, Faber M, Jacobs A, Verhulst F, Lacroix J, et al. Validation of self-management screening (SeMaS), a tool to facilitate personalised counselling and support of patients with chronic diseases. BMC Fam Pract 2015;16:165.
- Schuler M, Musekamp G, Faller H, Ehlebracht-Konig I, Gutenbrunner C, Kirchhof R, et al. Assessment of proximal outcomes of self-management programs: translation and psychometric evaluation of a German version of the Health Education Impact Questionnaire (heiQ™). Qual Life Res 2013;22(6):1391–403.
- Hitzig SL, Jeyathevan G, Farahani F, Linassi G, Routhier F, Jetha A, et al. Development of community participation indicators to advance the quality of spinal cord injury rehabilitation: SCI-High project. J Spinal Cord Med 2021 [Forthcoming in this special issue].
- Maunsell E, Lauzier S, Brunet J, Pelletier S, Osborne RH, Campbell HS. Health-related empowerment in cancer: validity of scales from the health education impact questionnaire. Cancer 2014;120(20):3228–36.
- Pozza A, Osborne RH, Elsworth GR, Gualtieri G, Ferretti F, Coluccia A. Evaluation of the Health Education Impact Questionnaire (heiQ), a self-management skill assessment tool, in Italian chronic patients. Psychol Res Behav Manag 2020;13:459–71.
- Jedeloo S, Leenders J. Carebasics: self-management. Amsterdam: Boom Lemma; 2013.
- Kennedy A, Rogers A, Chew-Graham C, Blakeman T, Bowen R, Gardner C, et al. Implementation of a self-management support approach (WISE) across a health system: a process evaluation explaining what did and did not work for organisations, clinicians and patients. Implement Sci 2014;9(129).
- Franklin M, Lewis S, Willis K, Rogers A, Venville A, Smith L. Controlled, constrained, or flexible? How self-management goals are shaped by patient-provider interactions. Qual Health Res 2019;29(4):557–67.
- Munce SE, Fehlings MG, Straus SE, Nugaeva N, Jang E, Webster F, et al. Views of people with traumatic spinal cord injury about the components of self-management programs and program delivery: a Canadian pilot study. BMC Neurol 2014;14:209.
- Bloemen-Vrencken JH, de Witte LP, Post MW. Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation. Spinal Cord 2005;43(8):462–75.