Abstract
Objective
The study objectives were to evaluate the inter-rater and intra-rater reliability; and criterion and construct validity of the 3D printed Toronto Rehabilitation Institute -Hand Function Test (3D TRI-HFT) in individuals with spinal cord injury (SCI).
Design
Observational study.
Setting
Inpatient Rehabilitation Hospital.
Participants
Four individuals with subacute and three individuals with chronic SCI.
Interventions
Reliability and validity of the 3D TRI-HFT was assessed within two interventional studies.
Outcome Measures
Participants performed the 3D TRI-HFT, Graded Redefined Assessment of Strength, Sensibility and Prehension (GRASSP), Functional Independence Measure (FIM) and the Spinal Cord Independence Measure (SCIM) at baseline, after 20 and 40 sessions of therapy and at six month follow-up from baseline. 3D TRI-HFT assessments were graded at the time of performance and re-graded from the video recordings for purpose of reliability testing. Validity testing was done by comparing the scores on 3D TRI-HFT with the scores on the GRASSP, and the FIM and SCIM self care sub-scores.
Results
The 3D TRI-HFT had high intra-rater and inter-rater reliability in sub-acute and chronic SCI with ICC values exceeding 0.99. Moderate to strong correlations were found between 3D TRI-HFT object manipulation scores and the FIM and SCIM self care sub-scores, with r values in the range of 0.7–0.8. Strong correlations were found between the various components of GRASSP and the 3D TRI-HFT, with r values exceeding 0.9.
Conclusions
The 3D TRI-HFT is a reliable and valid measure to assess unilateral hand gross motor function in individuals with SCI.
Introduction
Amongst the spinal cord injury (SCI) population, 59.9% have tetraplegia and their highest priority is to regain upper extremity function.Citation1,Citation2 Rehabilitation is the mainstay of treatment for retraining function. To scientifically evaluate novel interventions, researchers need access to reliable, valid, easy to use and universally accessible clinical outcome assessment tools that can be administered within reasonable time frames. Although there are many tests of hand function, few reliable and valid assessments have been developed for SCI.Citation3–9
Hand function tests such as the Action Research Arm Test and the Jebsen Hand Function test are not recommended for use in the SCI population as they are not developed for the patterns of grasp impairments following SCI. The Grasp and Release Test although developed for SCI, specifically to assess function following use of upper limb orthoses, FES, and reconstructive procedures is a time based measure and does not take into account proximal arm function.Citation10 Thus, there is a need to develop assessments based on the International Classification of Functioning, Disability and Health (ICF) framework and these assessments need to go beyond evaluation of pathophysiology or impairment.Citation11 The first working group of the International Campaign for Cures of SCI Paralysis aptly recognized that “no SCI therapy will be considered effective for the treatment of patients unless it improves the ability of patients to function in their daily routines or activities”.Citation12
In a review done by Jones et al.,Citation13 the authors identified two outcome measures that are SCI specific upper extremity measures in the activity domain. These measures are the Graded Redefined Assessment of Strength, Sensibility and Prehension (GRASSP) and the Capabilities of Upper Extremity Function- Test (CUE-T).
The GRASSP is a quantitative impairment measure designed for use in acute and chronic cervical SCI and was developed to address the void in the availability of SCI measures that detect functional capacity of the hand.Citation14,Citation15 Various sub-components of the GRASSP assess function under the body structure and function domain, and the activity domain of the ICF. The Quantitative Prehension component of the GRASSP is a timed test that does not consider proximal function or quality of movement. The entire test takes approximately 1–1.5 h to administer on bilateral upper extremities and occasionally may have to be completed over two days based on patient tolerance. It is custom manufactured and needs to be purchased for ∼ CAD $2,500. There is a 2-day training module to become certified to perform the test. So, although the psychometric properties of the test have been established in SCI the above barriers reduce its uptake by clinicians and researchers.
The CUE-T is intended to evaluate functional limitations as described by Marino RJCitation16 and is validated in SCI. It consists of 19 items, 17 of which are unilateral and test basic upper limb actions and grasp patterns. It evaluates upper extremity actions such as reaching, lifting, pulling, and pushing in addition to various grasp patterns. Most items are scored based on time or number of repetitions in 30 s. The test takes approximately 1 h to administer and unlike the 3D TRI-HFT does not integrate the use of the arm and hand during task execution. The test intends to assess the action, not the task.Citation16
Amongst the other widely used measures are the Functional Independence Measure (FIM);Citation17 and the Spinal Cord Independence Measure (SCIM), both of which have been validated in the SCI population.Citation18 Both these scales measure function in the activity domain. However, both scales are administered as questionnaires and hence are subjective in nature. Despite the subjective nature of the SCIM-III measure, the subjective results on the self-care subcategory are found to have a high level of agreement with the scores obtained when this part of the test is objectively administered.Citation19
In light of the above, we developed the Toronto Rehabilitation Institute-Hand Function Test (TRI-HFT) in 2008.Citation20 The TRI-HFT is a test to measure unilateral gross motor function of the upper extremity and has been validated in individuals with sub-acute SCI.Citation20 It consists of 2 parts and is designed to assess both proximal and distal upper extremity function. The first part of the test assesses the individuals’ ability to manipulate the following objects: (1) mug, (2) book, (3) soda can, (4) isosceles triangular sponge, (5) wireless home telephone, (6) paper sheet, (7) Ziploc bag filled with five golf balls, (8) dice, (9) credit card, (10) pencil and (11) nine rectangular blocks in sets of 3 × 100 g, 3 × 200 g and 3 × 300 g. Each of the three blocks in each weight category have surfaces with different levels of friction. The second part measures the ability to withstand eccentric forces (Bar test), the strength of lateral pinch in Newtons using a dynamometer (instrumented credit card test) and the strength of palmar grasp in Nm using a dynamometer (instrumented cylinder). The scoring system for the first part of the test considers ability to reach, grasp and manipulate and is done on a scale of 0–7, where greater scores indicate better performance. Further details on the original test objects, administration and scoring are described in Kapadia et al.Citation20
While the TRI-HFT has potential for high clinical utility (i.e. low cost, minimal training required to administer), a limitation to its use has been accessibility. To make it more easily accessible we replicated the test in a 3D printed format and demonstrated that the 3D printed objects were within 10% error margin of the original test objects. For details of the 3D printed version please refer to Kapadia et al.Citation21
The objective of the current study was to test the psychometric properties of the 3D printed Toronto Rehabilitation Institute-Hand Function Test (3D TRI-HFT) in individuals with sub-acute and chronic SCI. Specifically, we assessed the inter-rater reliability, intra-rater reliability and construct (convergent) and criterion validity of the 3D TRI-HFT within two interventional studies.
Methods
The current study was designed to evaluate the psychometric properties of the 3D TRI-HFT in sub-acute and chronic SCI populations. This study was a sub-study conducted within two single arm interventional studies that aimed at assessing the feasibility and efficacy of EEG-Triggered Functional Electrical Stimulation Therapy for Upper Limb Rehabilitation.Citation22 Inclusion criteria for study 1 were: (a) traumatic SCI classified as American Spinal Injury Association Impairment Scale (AIS) B-D, (b) SCI less than six months prior to baseline assessment, (c) neurological level of injury between C4 to C7 and (d) expected length of stay of at least 80 days at the time of study initiation. The exclusion criteria were (a) history of seizure disorder not effectively managed by seizure medications, (b) an existing electrical stimulation device (e.g. Implantable Cardioverter Defibrillator, Pacemaker, Spinal Stimulation), (c) rash or open wound at electrode site, (d) denervation of the targeted muscles, (e) poorly controlled autonomic dysreflexia, (f) botulinum toxin injection into affected upper extremity within three months prior to the study start, and (g) currently enrolled in another upper limb study. Inclusion criteria for study 2 were: (a) traumatic SCI classified as AIS B-D and (b) SCI at least 24 months prior to the baseline assessment. The exclusion criteria were same as the sub-acute study.
Participants in both studies underwent a battery of assessments at baseline, after 20 sessions of therapy (sessions were carried out 3–5 times a week), at discharge (after 40 sessions of therapy) and at 6-month follow-up. Assessment conducted at each time point for each participant for the right and the left upper extremity was treated as an independent data point. These assessments included: (a) FIM,Citation17 (b) SCIM,Citation23 (c) 3D TRI-HFT,Citation21 and (d) GRASSP,Citation14 and were completed in one session for both studies. The 3D TRI-HFT was video recorded for assessing inter and intra-rater reliability. For construct (convergent) validity, scores on the 3D TRI-HFT were correlated with scores on the self-care sub-scale of the FIM and SCIM. For the assessment of criterion validity, scores on the 3D TRI-HFT were correlated with scores on the different components of the GRASSP, i.e. strength, sensation, qualitative and quantitative prehension. The strong psychometric properties of the GRASSP have resulted in its use in clinical trials to evaluate primary endpoints related to hand function,Citation24–27 and so we choose to use this test for validity testing. The FIM and SCIM are validated measures in SCI population.Citation14,Citation17,Citation23 For testing reliability and validity, scores of the left and right upper extremities as well as scores at each time point were treated as separate independent data points.
Assessors: Two assessors with extensive experience in SCI research were involved in the psychometric testing of the 3D TRI-HFT. Specifically, assessor AB is a researcher working in the field of SCI research for 20 years and assessor CD is a clinician researcher working in the field of SCI for 12 years. All in-person assessments for both the studies were carried out by assessor AB and all video recorded assessments were rated by assessor CD. Both assessors have eight years on and off experience with the use of original version of the TRI-HFT however they did not receive any additional training for the use of the 3D printed version.
Statistical Analysis were independently performed for the sub-acute and the chronic SCI participants as below:
Inter-rater Reliability: The inter-rater reliability of the first component of the test, i.e. object manipulation component which includes the ten objects and the set of nine rectangular blocks, was assessed. For inter-rater reliability, the de-identified video recording from both studies were reviewed by CD and each task was scored. The scores were than compared to the scores from the original testing performed by AB. Intraclass correlation coefficient (ICC) was calculated using SPSS version 16 (SPSS, Inc., USA).
Intra-rater Reliability: For the purpose of intra-rater reliability, AB and CD reviewed the participant videos from both the studies, one month apart and re-rated the participant performance on individual tasks at both time points. ICC was calculated using SPSS version 16 (SPSS, Inc., USA).
Construct (convergent) and Criterion Validity: The construct (convergent) validity of the 3D TRI-HFT was evaluated by computing Spearman’s correlation coefficient with the FIM self-care sub-score and the SCIM self-care sub-score. The criterion validity of the 3D TRI-HFT was established by computing Spearman’s correlation coefficient’s with the strength, sensation, qualitative prehension and quantitative prehension scores of the GRASSP. An r value of 0.0–0.4 was considered as weak correlation, 0.4–0.7 was considered as moderate correlation, and anything above 0.7 was considered as strong correlation.Citation28
For all statistical procedures, α was set at <0.01.
Results
For the sub-acute study, 4 of the 5 participant’s data were assessed at 3 time points in the study. The 5th participant dropped out of the study after 12 sessions. The remaining 4 participants completed all the outcome assessments at all time points except one participant who missed one assessment. Inter-rater reliability was determined using 22 datasets (n = (4 participants x3 time points)-1missed appointment X 2 (left and right UE)). For intra-rater reliability AB and CD re-assessed the participant videos and scored them again (n = 44). For assessing construct validity and criterion validity, scores on right and left hand as well as at each time point were treated as independent data points (n = 22).
For the chronic study, 3 participants were recruited and assessed at 4 time points except one participant who missed one assessment. Inter-rater reliability was determined using 22 datasets and intra-rater reliability was determined using 44 datasets (both AB and CD reassessed the videos). For assessing construct validity and criterion validity scores on right and left hand as well as at each time point were treated as independent data points (n = 22).
Participant demographics, FIM and SCIM self-care sub-scores for both the studies are described in whereas raw scores on the 3D TRI-HFT and GRASSP are presented in and .
Table 1 Participant demographics.
Table 2 3D Toronto Rehabilitation Institute – Hand Function Test scores.
Table 3 Graded redefined assessment of strength, sensibility and prehension scores.
Inter-rater reliability
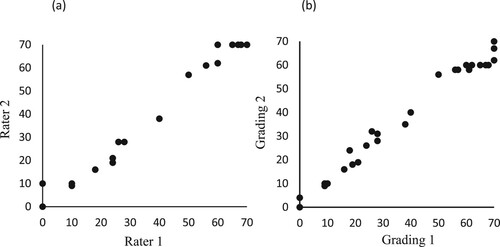
For both the sub-acute and chronic SCI study, we found a statistically significant strong correlation between the two assessors for the 10-object manipulation component of the 3D TRI-HFT with an ICC = 0.994 (95% CI: 0.985–0.998; P < 0.000) ((a)) and ICC = 0.990 (95% CI:0.976–0.996; P < 0.000) respectively. The inter-rater reliability for the 9 rectangular blocks could not be assessed for both studies as the assessor had difficulty identifying the blocks based on their weight and texture from the video recorded assessments.
Intra-rater reliability
We found statistically significant strong correlation between the first and second rating on the 10-object manipulation component of the TRI-HFT within each assessor. ICC values for the sub-acute and chronic study are ICC = 0.995 (95% CI: 0.992–0.998; P < 0.000) ((b)) and ICC = 0.999 (95% CI: 0.999–1.00; P < 0.000) respectively.
Construct and criterion validity
Sub-acute SCI Study
The results showed a moderately strong correlation between the FIM selfcare sub-score and the 10-object manipulation component of the 3D TRI HFT with an r = 0.770 (95% CI: 0.567–0.890, P = 0.01) and the rectangular blocks with an r = 0.760 (95% CI: 0.535–0.887, P = 0.01). Similarly, we found a moderately strong correlation between the SCIM self-care sub-score and the 10-object manipulation component with an r = 0.769 (95% CI: 0.547–0.894, P = 0.01) and the rectangular blocks with an r = 0.758, (95% CI: 0.533–0.875, P = 0.01).
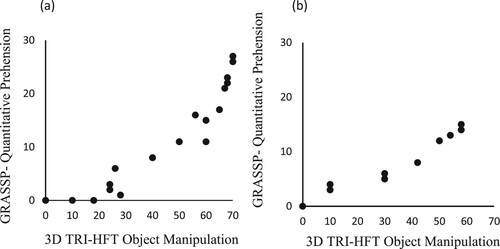
The 10-object manipulation component showed very strong correlation with the Strength (r = 0.946; 95% CI: 0.830–0.986 P = 0.01), Qualitative Prehension (r = 0.951; 95% CI: 0.856–0.982 P = 0.01) and Quantitative Prehension (r = 0.974; 95% CI: 0.0.920–0.991 P = 0.01) components of the GRASSP. However, it had a moderate correlation with the Sensation component of the GRASSP (r = 0.523; 95% CI: 0.126–0.740 P = 0.05). Similarly, the rectangular blocks showed a very strong correlation with the Strength (r = 0.918; 95% CI: 0.770–0.968, P = 0.01), Qualitative Prehension (r = 0.941; 95% CI: 0.854–0.978 P = 0.01) and Quantitative Prehension (r = 0.938; 95% CI: 0.830–0.976 P = 0.01) components of the GRASSP, but had a moderate correlation with the Sensation component (r = 0.512; 95% CI: 0.115–0.749 P = 0.05). The instrumented cylinder, instrumented credit card and the bar also showed strong to very strong correlations with all components of the GRASSP except sensation with which it showed only weak correlations.
For correlations with individual test components please refer to .
Table 4 Concurrent and criterion validity of the 3D TRI-HFT.
Chronic SCI study
The results showed a moderately strong correlation between the FIM selfcare sub-score and the 10-object manipulation component of the 3D TRI HFT with an r = 0.756 (95% CI: 0.497–0.898, P = 0.01) and the rectangular blocks with an r = 0.759 (95% CI: 0.530–0.895, P = 0.01). Similarly, we found a moderately strong correlation between the SCIM self-care sub-score and the 10-object manipulation component with an r = 0.725 (95% CI: 0.419–0.888, P = 0.01) and the rectangular blocks with an r = 0.726 (95% CI: 0.448–0.890, P = 0.01).
The 10-object manipulation component showed very strong correlation with the Strength (r = 0.936; 95% CI: 0.813–0.980 P = 0.01) ((b)), Qualitative Prehension (r = 0.965; 95% CI: 0.821–0.999 P = 0.01) and Quantitative Prehension (r = 0.997; 95% CI: 0.985–1.0 P = 0.01) components of the GRASSP but had a weak correlation with the Sensation component of the GRASSP (r = 0.274; 95% CI: −0.245–0.709 P = 0.217).
Figure 2 (a) Criterion Validity of the 3D TRI-HFT 10-object manipulation component with the GRASSP Quantitative Prehension component in sub-acute SCI. (b) Criterion Validity of the 3D TRI-HFT 10-object manipulation component with the GRASSP Quantitative Prehension component in chronic SCI.
Similarly, the rectangular blocks also showed a very strong correlation with the Strength (r = 0.938; 95% CI: 0.813–0.980 P = 0.01), Qualitative Prehension (r = 0.965; 95% CI: 0.849–0.999 P = 0.01) and Quantitative Prehension (r = 0.995; 95% CI: 0.974–1.0 P = 0.01) components of the GRASSP but had a statistically non-significant weak correlation with the Sensation component (r = 0.284). The instrumented cylinder, instrumented credit card and the bar also showed moderately strong to strong correlations with all components of the GRASSP except sensation with which it showed only weak correlations.
For correlations with individual test components please refer to .
Discussion
In this study, we assessed the psychometric properties of the 3D TRI-HFT within a small number of individuals with sub-acute and chronic SCI. Despite the small sample size, to the best of our knowledge this is the first 3D printed tool to be validated for use in SCI. The 3D printed test can be accessed from anywhere and hence it practically eliminates variability related to test manufacturing, which may often affect the test scoring, accuracy and ultimately reproducibility of test results.Citation21
Whilst the 10-object manipulation component of the 3D TRI-HFT showed high inter- and intra-rater reliability, the rectangular blocks could not be assessed as it was difficult to identify the blocks based on weight and texture on the videos. The 9 blocks are now numbered for easy identification.
The moderately strong correlations of 3D TRI-HFT with the FIM and SCIM selfcare sub-scores is an expected finding given that FIM and SCIM also measure function at an activity level. In the study by Kalsi-Ryan et al., which looked at the psychometric properties of the GRASSP, the authors showed similar correlations between GRASSP and the FIM and SCIM selfcare sub-scores.Citation29 The FIM and SCIM have documented floor and ceiling effects,Citation18,Citation30 and are unable to detect change at either end of the functional spectrum.
The first part of the 3D TRI-HFT showed strong correlations with the strength, qualitative and quantitative components of the GRASSP, in both sub-acute and chronic SCI studies. This finding affirms that it produces the same information about a person’s upper extremity function as the Qualitative and Quantitative components of the GRASSP. The first part of the 3D TRI-HFT showed moderate correlations with sensation component of the GRASSP in sub-acute SCI population. This finding is not surprising as literature has shown poor correlations between sensory impairment and motor function. These findings are supported by Kalsi-Ryan et al., as well where the authors showed moderate correlations between International Standard for Neurological Classification of Spinal Cord Injury-Upper Extremity Motor Scores (ISNCSCI-UEMS) and sensation.Citation5
Advances in medical science has led to a significant improvement in life expectancy in individuals with SCI. It is upon the rehabilitation community to develop tools that can help improve quality of life and independence of this population. Research aimed at developing new rehabilitation therapies require reliable and valid outcome assessment tools that take into account practical aspects such as time needed to administer the test and personnel and financial resources.Citation31 Amongst the current validated upper extremity activity measures in SCI the main limitations are: (1) self-fabrication of test objects, which often compromises standardization of the test; (2) expensive (average cost ∼$2,500); (3) takes up to or more than 1 h to administer; and (4) requires extensive training on part of the assessor to administer the test correctly, which means that if the assessment is not used for a longer duration than the reliability of the test might be questionable.
The 3D TRI-HFT is one of the first upper extremity measures that can assess reaching, grasping and manipulation and addresses each of the above concerns. With respect to standardization, the test is open source (files will be made available on www.kite-uhn.com) and hence every time the test objects will be manufactured in the same fashion. With respect to cost effectiveness, 3D printing technology is becoming popular, accessible and cost effective, we estimate that today the objects of the 3D TRI-HFT can be printed for ∼CAD $500 and this cost should decrease over time. The test takes approximately 15 mins to administer on one upper extremity (). With respect to training needed to administer the test, the 3D TRI-HFT requires minimal training on part of the assessor,Citation20 and this is in the form of self- training by reading a two page manual (available in the TRI-HFT original test publication).Citation20
Table 5 Time taken (in minutes) to complete the 3D TRI-HFT* for B/L upper extremities for all study participants.
An added benefit of the 3D TRI-HFT is that since the tasks are routinely used in everyday life the results of the test are meaningful to the patients and their care providers too. By successfully completing a component of the 3D TRI-HFT the patient is shown that they can perform a particular object grasping and manipulation task. The other advantage, specifically in research settings, is that since it is universally accessible, if used uniformly across clinical trials, it will enable researchers across the globe to compare interventions that affect upper limb function and share the data.
Conclusion
In summary, the 3D TRI-HFT is an open-source test that is simple, reliable, valid and takes up to 15 min to administer. It assesses function at an activity level. In the context of interventional trials, it may be recommended to be used as an adjunct measurement to strength and sensibility measurements. It can be easily incorporated in SCI rehabilitation clinics worldwide with minimal expense to the user and since the objects are everyday objects they can double-up as therapy tools where appropriate.
Disclaimer statements
Contributors None.
Funding Financial support for the study was obtained from Ontario Neurotrauma Foundation (in partnership with the Praxis Spinal Cord Institute, formerly Rick Hansen Institute) and Morton Cure Paralysis Fund. The funding body did not play a role in the design of the study, data collection, analysis, and interpretation of data or in writing the manuscript. The primary author on the paper is funded by CIHR Frederick Banting Fellowship.
Conflicts of interest Authors NK, LJ, KM, RW and CMC have no conflicts to declare. Dr. Milos R Popovic is the Chief Technology Officer and Director of Myndtec, Inc. a company that manufactures transcutaneous functional electrical stimulators.
Supplemental Material
Download PDF (200 KB)Acknowledgements
The authors would like to acknowledge Dr. Vera Zivanovic, Dr. Sukhvinder Kalsi-Ryan, Janelle Unger, Hope Jarvis Rademeyer, Dr. Parvin Eftekhar, Alexandra Chen and Dr. Cindy Gauthier for providing assistance with participant recruitment and with delivery of research therapy to the study participants.
Data availability statement
The raw data of all participants is included in the manuscript.
References
- Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004;21(10):1371–83.
- Simpson LA, Eng JJ, Hsieh JTC, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma 2012;29(8):1548–55.
- Coates SK, Harvey LA, Dunlop SA, Allison GT. The AuSpinal: a test of hand function for people with tetraplegia. Spinal Cord 2011;49(2):219–29.
- Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil 1969;50(6):311–9.
- Kalsi-Ryan S, Beaton D, Curt A, Popovic MR, Verrier MC, Fehlings MG. Outcome of the upper limb in cervical spinal cord injury: profiles of recovery and insights for clinical studies. J Spinal Cord Med 2014;37(5):503–10.
- Post MWM, Van Lieshout G, Seelen HAM, Snoek GJ, Ijzerman MJ, Pons C. Measurement properties of the short version of the Van Lieshout test for arm/hand function of persons with tetraplegia after spinal cord injury. Spinal Cord 2006;44(12):763–71.
- Sollerman C, Ejeskar A. Sollerman hand function test. A standardised method and its use in tetraplegic patients. Scand J Plast Reconstr Surg Hand Surg 1995;29(2):167–76.
- Velstra IM, Ballert CS, Cieza A. A systematic literature review of outcome measures for upper extremity function using the international classification of functioning, disability, and health as reference. PM & R 2011;3(9):846–60.
- Wuolle KS, Van Doren CL, Thrope GB, Keith MW, Peckham PH. Development of a quantitative hand grasp and release test for patients with tetraplegia using a hand neuroprosthesis. J Hand Surg Am 1994;19(2):209–18.
- Mulcahey MJ, Hutchinson D, Kozin S. Assessment of upper limb in tetraplegia: considerations in evaluation and outcomes research. J Rehabil Res Dev 2007;44(1):91–102.
- Sinnott KA, Dunn JA, Rothwell AG. Use of the ICF conceptual framework to interpret hand function outcomes following tendon transfer surgery for tetraplegia. Spinal Cord 2004;42(7):396–400.
- Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007;45(3):190–205.
- Jones LAT, Bryden A, Wheeler TL, Tansey KE, Anderson KD, Beattie MS, et al. Considerations and recommendations for selection and utilization of upper extremity clinical outcome assessments in human spinal cord injury trials. Spinal Cord 2018;56(5):414–25.
- Kalsi-Ryan S, Beaton D, Curt A, Duff S, Popovic MR, Rudhe C, et al. The graded redefined assessment of strength sensibility and prehension: reliability and validity. J Neurotrauma 2012;29(5):905–14.
- Kalsi-Ryan S, Curt A, Fehlings MG, Verrier MC. Assessment of the hand in tetraplegia using the graded redefined assessment of strength, sensibility and prehension (GRASSP): impairment versus function. Top Spinal Cord Inj Rehabil 2009;14:34–46.
- Marino RJ, Shea JA, Stineman MG. Capabilities of upper extremity test manual of administration. Version 1.1. ed. Philadelphia: Thomas Jefferson University; 2016.
- Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil 1993;74(5):531–6.
- Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the functional independence measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1471–6.
- Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Lüthi H, et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2013;51(1):40–7.
- Kapadia N, Zivanovic V, Verrier M, Popovic MR. Toronto rehabilitation institute-hand function test: assessment of gross motor function in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil 2012;18(2):167–86.
- Kapadia N, Myers M, Musselman K, Wang RH, Yurkewich A, Popovic MR. 3-Dimensional printing in rehabilitation: feasibility of printing an upper extremity gross motor function assessment tool. Biomed Eng Online 2021;20(1):2.
- Jovanovic LI, Kapadia N, Zivanovic V, Rademeyer HJ, Alavinia M, McGillivray C, et al. Brain-computer interface-triggered functional electrical stimulation therapy for rehabilitation of reaching and grasping after spinal cord injury: a feasibility study. Spinal Cord 2021;7(1):24.
- Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM – spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997;35(12):850–6.
- Zariffa J, Kapadia N, Kramer JL, Taylor P, Alizadeh-Meghrazi M, Zivanovic V, et al. Relationship between clinical assessments of function and measurements from an upper-limb robotic rehabilitation device in cervical spinal cord injury. IEEE Trans Neural Syst Rehabil Eng 2012;20(3):341–50.
- Zariffa J, Kapadia N, Kramer JLK, Taylor P, Alizadeh-Meghrazi M, Zivanovic V, et al. Feasibility and efficacy of upper limb robotic rehabilitation in a subacute cervical spinal cord injury population. Spinal Cord 2012;50(3):220–6.
- Zbogar D, Eng JJ, Miller WC, Krassioukov AV, Verrier MC. Movement repetitions in physical and occupational therapy during spinal cord injury rehabilitation. Spinal Cord 2017;55(2):172–9.
- Sinnott KA, Dunn JA, Wangdell J, Johanson ME, Hall AS, Post MW. Measurement of outcomes of upper limb reconstructive surgery for tetraplegia. Arch Phys Med Rehabil 2016;97(6 Suppl):S169–81.
- Dawson-Saunders BTR. Basic and clinical biostatistics. 2nd ed. East Norwalk (CT): Appleton & Lange; 1994.
- Velstra I-M, Curt A, Frotzler A, Abel R, Kalsi-Ryan S, Rietman JS, et al. Changes in strength, sensation, and prehension in acute cervical spinal cord injury: European multicenter responsiveness study of the GRASSP. Neurorehabil Neural Repair 2015;29(8):755–66.
- Coster WJ, Haley SM, Jette AM. Measuring patient-reported outcomes after discharge from inpatient rehabilitation settings. J Rehabil Med 2006;38(4):237–42.
- Tyson S, Connell L. The psychometric properties and clinical utility of measures of walking and mobility in neurological conditions: a systematic review. Clin Rehabil 2009;23(11):1018–33.