Abstract
Context
Insufficient recruitment is a barrier to research and limits statistical power. We describe an initiative aimed to streamline recruitment and consent processes for inpatients with spinal cord injury or disease (SCI/D) via implementation of a Central Recruitment (CR) process. The CR process adhered to ethical standards, reduced participant burden, and maximized research participation.
Methods
In this CR process, the inpatient’s nurse affirmed suitability for research approach based on fluency, cognition and health stability. A patient research liaison (PRL) was the sole contact for information regarding the research process, and introduced ongoing studies, screened for eligibility, and completed the consent process(es).
Results
Over five and a half years, 1,561 inpatients with SCI/D were screened for eligibility upon admission, of whom 80% (1256/1561) were deemed suitable for the PRL approach. Of those suitable for the CR process, 80% (1001/1256) agreed to discuss current research opportunities, 46% (235/516) consented to participate in one or more studies, and 86% (856/1001) agreed to future research contact.
Conclusion
This process adhered to ethical procedures and reduced the burden of having multiple researchers approach each individual inpatient regarding research participation, with high consent rates for low-risk studies. Future evaluation of the process scalability is underway.
Introduction
Spinal cord injury or disease (SCI/D) results in diverse short- and long-term motor, sensory and autonomic impairments and subsequent comorbidities and secondary health conditions. The incidence of traumatic SCI in Canada has remained stable over the past two decades at approximately 53 injuries per million people,Citation1 while the incidence of non-traumatic SCI has been on the rise, currently residing at 26.3-33.2 injuries per million people.Citation2–4 The frequency and severity of health conditions in the subacute and chronic periods post-injury are significant and often involve persistent secondary health conditions such as musculoskeletal and neuropathic pain, pressure ulcers, depression and anxiety,Citation5–9 impacting physical and mental health, independence, and ultimately willingness and ability to participate in research.Citation10 Like other patient populations with multiple morbidities, those with SCI/D have higher healthcare and polypharmacy utilization,Citation7 and a rehabilitation length of stay, averaging between 78 and 99 days.Citation10–14 Recruitment of individuals with SCI into clinical trials is notoriously difficult due to the sporadic or unpredictable nature of SCI onset and the heterogeneity of impairment and comorbid health conditions.Citation15
Clinical research plays an important role in enabling our understanding of life following SCI/D, the quality of care, health system trajectories, resource requirements and it informs health policy and standards of care.Citation15–20 Anderson et al. have identified the following barriers to participation in clinical trials including: concerns about changes in insurance or disability income eligibility; out of pocket expenses; and, the risk of side-effects or decline in function.Citation21 From a patient’s perspective, Annemie Heselmans, who is both a researcher and person with lived experience, recently discussed her reasons to participate in SCI research in a Lancet Correspondence piece.Citation16 She highlighted meaningful reasons such as to stave-off secondary complications, experiment with aids that encourage movement, prepare for future treatments that might eventually restore spinal cord functionality, and to help guide research priorities. Despite these important aims, clinical research in SCI/D continues to exhibit high screening to recruitment ratios, poor consent rates,Citation15,Citation16 and lacks coordination. These challenges served as the impetus for developing an organizational improvement approach to enhance recruitment – a Central Recruitment (CR) process.
The SCI/D population is particularly vulnerable to both repeated recruitment and over-sampling in research studies, inferring a higher burden of research participation.Citation15,Citation17,Citation18 One reason is due to their life-long engagement with the health care system; patients with SCI may be approached for research studies in the emergency department, at the acute care hospital, multiple times during inpatient rehabilitation and then again each time they attend tertiary clinics, once they have resumed community living. To minimize this risk and ensure best practices, it is important to understand the ways a recruitment process should uphold ethical standards.Citation18,Citation19 The individual obtaining informed consent is required to outline the risks and benefits of a study in a neutral manner to ensure that consent is given voluntarily. The process should also be attentive to justice-related considerations because this process aims to foster access to research for all who desire to participate (not merely those who have a healthcare provider who is attentive to what is happening on the research front). Alternatively, by tracking patient preferences, it is important to be respectful and record the responses of those who express a desire not to participate. Thus, a non-coercive and robust procedure that streamlines the recruitment process for individuals following SCI/D should benefit the patient, research enterprise, and the health care system.
Low recruitment rates associated with clinical trials constitute one of the biggest and most global challenges in SCI research.Citation15,Citation20,Citation22 Published work identifies existing infrastructure, research study design, recruiter and participant characteristics as the main factors influencing successful recruitment. Effective remedial strategies are cited as reducing participant burden, supporting individuals who do not speak English, and forming collaborations with the patients’ circle of care teams.Citation23–27 Studies have shown that screening to recruitment ratios for subacute SCI patients can be high even with favorable study design (e.g. short travel time, non-invasive protocols) and minimal inclusion/exclusion criteria.Citation15,Citation17,Citation28 The idea of recruiting for multiple studies simultaneously has been suggested as a means to reduce participant burden and increase the efficiencies of patient recruitment in other hard-to-recruit patient populations, such as stroke survivors, cancer patients, and those undergoing unscheduled hospital admissions.Citation27,Citation29–31 Recruitment efficiency for organizations can be realized by incorporating recommendations cited in research such as using fewer staff to recruit and avoiding building redundant infrastructure for each new study.Citation15,Citation31 Our study protocol was developed with these efficiencies in mind. To-date, no such standardized inpatient rehabilitation research recruitment process has been reported in the literature.
The purpose of this pilot study was to develop a novel CR process based on ethical principles, which maximized participation by reducing recruitment barriers, eliminated redundancy in research infrastructure, and increased organizational efficiency.
Objectives
To develop a process to streamline SCI inpatient recruiting, consistent with the ethical framework of the Tri-Council Policy Statement (TCPS2),Citation32 and the International Council for Harmonization of Technical Requirements of Pharmaceuticals for Human Use Good Clinical Practice (GCP) Guidelines.Citation33
To pilot the process with inpatients at a tertiary SCI rehabilitation center and recruit participants into clinical research studies of varied designs.
To evaluate the effectiveness of the process based on outcome measures such as rates of inpatient willingness to learn about research opportunities, consent to participate, screening to recruitment ratios, and rates of agreement to future research contact.
Methods
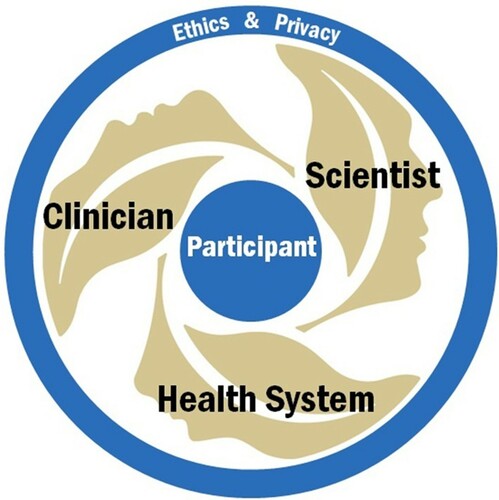
The CR pilot process was designed using a patient-centered model (). The model was predicated upon the TCPS2 and GCP guidelines, and firmly rooted in the principles of ethical research conduct to minimize patient harm or risk. Principles of autonomy, beneficence, non-maleficence, and justice were incorporated to ensure equal opportunities for inpatients to learn about research and for researchers to have access to potential participants.Citation32 Canadian ethical guidelines concerning research with humans suggest that the initial approach regarding research participation should be made by someone from a patient’s Circle of Care (CoC). This practice ensures that the initial screening is done by someone familiar to the patient and with insight into the patient’s health history and capacity to meaningfully consider research participation. Our process utilized the primary registered nurse (RN) as the inpatient’s CoC representative as the RN was most familiar with the inpatient's suitability and was routinely accessible to the CR staff. The RNs were provided with training regarding the constructs of research suitability, and their role in the CR process.
Previous studies regarding the ethics of conducting research during rehabilitation have suggested that the extended time inpatients interact with their health care providers’ influences their desire to participate in research, as a way to please or repay them for the hours of care provided.Citation18 An important ethical concern is that inpatients may consent out of a sense of obligation, or by falsely conflating the aims of research with those of clinical care.Citation48 The potential for therapeutic misconception is significant in this population due to the highly disabling nature of the condition, absence of a cure, and raised hope that the experimental intervention offered in the same setting as their clinical treatment will be beneficial.Citation18–49 To mitigate these risks, the CR process used a single, non-clinical point of contact between research and the inpatient. The Patient Research Liaison (PRL) was a research staff member who was a neutral third party, not biased towards any one study, and did not report directly to the Principal Investigators (PIs) responsible for the studies. The PRL was able to clearly delineate the difference between clinical care and research participation to address therapeutic misconception, making sure that the inpatient understands the distinctions between the two. The PRL’s training was comprised of 1:1 training with a clinician and senior scientists on the consent process which included role playing, successful completion of research quality integration training (roles and responsibilities of PI, delegation of research procedures, informed consent, documentation, Standard Operating Procedures, institutional annual certification, and training for research personnel).
Procedures
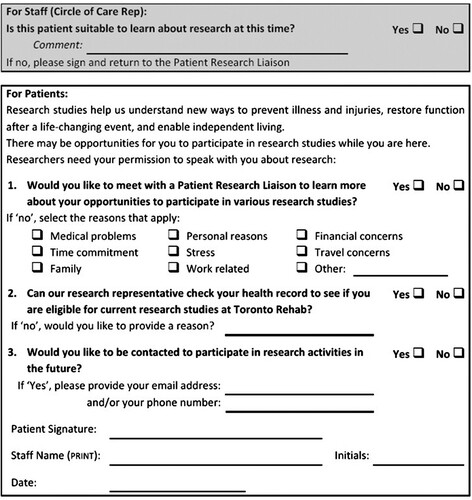
The CR process began with a screening tool called the Research Interest Form (RIF). The first section of this form was designed for the CoC representative to determine if the inpatient was ‘suitable’ for research approach. This concept of suitability was based on multiple aspects including the individual inpatient’s English proficiency, cognitive capacity, and medical stability. If suitable, the CoC representative proceeded to have the inpatient complete the form, obtaining yes or no answers to three (3) questions about research (see ).
The completed forms were returned to the PRL for processing. If the CoC representative found the inpatient to be suitable and they answered ‘Yes’ to questions #1 and #2, the PRL followed up appropriately by introducing research to the inpatient and auditing their medical record to screen for study eligibility. If the inpatient answered ‘No’ they did not want to meet with the PRL or want to have their medical record reviewed, then the CR screening process was not initiated by the PRL. The answer to question #3 was considered independently of the first two; if the inpatient answered ‘Yes’, then the PRL met with them to confirm that their contact information will be stored for future research consideration. No action was taken by the PRL if the answer was ‘No’. Interactions with the inpatient were recorded in the medical chart, and where appropriate, it was noted if the inpatient declined research approach or screening.
The CR pilot study received Research Ethics Board (REB) approval in July 2011 and began with three REB approved studies at Toronto Rehabilitation Institute (TRI) – Lyndhurst Center. Lyndhurst Centre is the largest free-standing SCI rehabilitation facility in Canada, and is a tertiary academic rehabilitation hospital within the University Health Network (UHN), a member of the Toronto Academic Health Science Network. Clinical research is ongoing in the acute, subacute and chronic phases of SCI. Clinical research is a multi-faceted process, which requires a commitment on the part of the organization for infrastructure, a research team for funding and staffing, as well as a sufficient population of potential research participants.
The recruitment foci for the initial three studies active between 2011 and 2013 were individuals with SCI/D enrolled in the inpatient rehabilitation program at Lyndhurst Center.Citation34–39 From 2013 to 2016, three additional studies began using the CR process for recruitment.Citation35,Citation40–42 Each study had its own unique set of inclusion and exclusion criteria which were used by the PRL to screen for during audit of the medical record. The screening criteria are listed in . If the inpatient met the screening criteria for one or more of the studies, the PRL met with them to review the informed consent form (ICF), and answer any questions pertaining to study participation. The consent documents were given to the inpatient, to review and share with family members, as appropriate, prior to making a decision about research participation. The inpatient could take as long as desired to make a decision regarding research consent within the time period before eligibility expiration. For low-risk studies with simple inclusion criteria, the PRL obtained consent and then notified the appropriate study coordinator to commence the study. For high-risk studies with complex inclusion criteria, the PRL introduced the inpatient to the study-specific research coordinator for secondary screening, followed by consent and enrollment.
Table 1 TRI – Lyndhurst Center: screening criteria by study.
Outcomes
The metrics of evaluation of the CR process included: length of time from CoC representative approach to RIF completion, number of inpatients eligible or not eligible for each study, number of eligible inpatients who consented to or declined a study, and number of inpatients willing to be contacted for future research opportunities after discharge. Data was recorded daily, and descriptive statistics were maintained for the six studies carried out between July 2011 and December 2016.
Results
During the 66-month period, a total of 1561 new inpatients were admitted to the Lyndhurst Center SCI/D rehabilitation program. On average, inpatients took 4 days (SD = 4.5) to complete the RIF after being approached by the CoC representative. A total of 80% (1256/1561) of all inpatients were deemed suitable for research approach. The predominant reason for lack of suitability was poor English fluency (more than 80% of all those unsuitable). Other reasons included early discharge, cognitive impairment, and having a palliative status. Of all suitable inpatients, 86% (1074/1256) consented to medical record review and 80% (1001/1256) agreed to discuss research studies with the PRL. After meeting the PRL, 86% agreed to future research contact after discharge, a percentage which remained relatively consistent over time. Across all studies, 46% (235/516) of inpatients consented to participate in research. Of those eligible, 51% (178/346) consented to participate in one study, 34% (57/170) in two studies and 15.4% (8/52) in three studies, where concurrent enrollment was feasible and did not undermine the scientific integrity of one study vs another (see ).
Table 2 Time of Research Interest Forms (RIF) completion relative to admission and response statistics July 2011 to December 2016.
Participants in this study were representative of the typical demographic of SCI/D inpatients in Canada during this time period (see for overview). The majority of participants were males in their 50s with traumatic SCI. The mean age of inpatients increased over time from an average of 50 years at year one to 58 years of age by year six. In addition, we noticed a trend towards more nontraumatic SCI/D admissions over time, with a 7% increase in nontraumatic cases over the 5.5 year period, reflecting the changing demographics of SCI rehabilitation patients in Canada.Citation1
Table 3 Demographic information of inpatients with Spinal Cord Injury (SCI) who agreed to medical record review.
The six studies that utilized the CR process covered a variety of designs, as detailed in . Simpler designs requiring minimal time commitment (e.g. registry, observational) had higher screening to consent rates, ranging between 55-85%. More involved designs associated with greater time-commitment and more complex, multimodal assessments had lower consent rates ranging between 10-44%. The use of the streamlined CR process with a single PRL approaching inpatients for all studies instead of six individual study coordinators approaching them was a significant reduction in burden to our inpatients.
Table 4 Study details: design, recruitment duration, consent rate.
Discussion
The aim of the Central Recruitment pilot process was to design an ethically robust process that streamlined inpatient participant recruitment for rehabilitation-focused clinical research studies, increased organizational efficiency by eliminating the need to create new research infrastructure for each study, and, perhaps most importantly, reduced inpatient burden of meeting multiple research personnel during recruitment. The results indicate that CR is an effective and feasible recruitment strategy for rehabilitation studies in the SCI/D population. By standardizing the process on the front end, with the RN as the CoC representative, and with the addition of the PRL as an unbiased single point of contact, this process maximized research participation among inpatients, reduced research resource redundancy and inpatient burden.
The basic architecture of the model used in this investigation focused on inpatients and their priorities. By keeping the needs of patients at the center of the process, it was successful in reducing the number of research personnel that met with inpatients for the purpose of recruitment, as historically at least one research coordinator per study has been assigned to recruit. SCI/D inpatients have many interactions with numerous members of the interprofessional rehabilitation team, hence reducing the number of research personnel, which presumably contributes to role clarity and limits inpatient confusion.
Further, the CR model addressed an opportunity to increase organizational efficiency during research recruitment. In the literature, Nasser et al. have commented on the need to professionalize and automate the process of recruitment and provide an infrastructure of experienced professional recruiters in academic medicine.Citation45 They found that most academic health centers still rely on traditional study staff with little training or experience in recruitment and concluded that a centralized process would benefit both the participants and research organization. This is consistent with our findings, which extend the benefits of the CR model to the research enterprise by demonstrating feasibility in being able to support a large quantity of diverse studies. During the implementation of the CR process, our efforts were bootstrapped by the academic mandate of the University Health Network. The Corporate UHN Balanced Scorecard of 2012 set an organizational objective to “Become the Research Hospital of the Future” and identified areas for improvement, such as maximizing patient engagement in research and timely study recruitment.Citation46 Between 2011 and 2012, the scorecard reported that 18.1% of research studies within the organization recruited zero participants within the first year. The CR process was well-received and supported by administrative leaders, as it was an important initiative aimed to mitigate recruitment barriers, establish centralized admission-to-enrollment infrastructure, ultimately lowering the percentage of studies with zero accrual in the first year.
From a clinical point of view, the CR process did not disrupt clinical care and medical appointments took priority over research participation. Clinicians gained a heightened awareness of inpatient research enrollment based on routine documentation in the medical record. The PIs benefitted from the systematic approach to inpatient screening through access to a centralized dataset and timely recruitment of desired sample sizes, powering the studies that advance the SCI/D field.
Given the success of this pilot, the logical next step is to test the scalability of the CR process by increasing the complexity and number of studies and extending the scope to include a broader range of clinical populations in both inpatient and outpatient groups. Future research can additionally explore whether there is an optimal number of studies a single PRL can manage and how the number may be influenced by complexity of study design and screening criteria, both quantitatively and qualitatively (e.g. interviews with stakeholders such as the PIs, CoC representatives, study coordinators, inpatients).
There is an opportunity to apply learnings from the SCI/D population to other inpatient and outpatient tertiary rehabilitation populations (e.g. brain injury, stroke, dementia), recognizing there may be additional nuances to the process depending on the impairment group. This scale of implementation should be built into the infrastructure of the research institute, requiring support from the Director of the Research Institute and the hospital Executive and Medical Directors. Resources in the form of staff and funding to support the training and retention of the PRLs are required to ensure the successful implementation of this system at similar Institutes or Centres. Implementing the CR process in the outpatient setting would provide an exceptional opportunity to study the influence of managed care on the complex multi-morbidity of SCI/D. In order to scale this process to support all local studies, a database that automates the process is needed given the large number of patients and studies.
Issues and limitations
A major limitation of the CR process is its exclusion of inpatients who did not speak English. While many health care facilities offer translation services for inpatients during research consent, access to such services is typically lost upon study enrollment due to the limited availability of translators, lack of a budget to pay for ongoing research translation services, and methodological shortcomings associated with data analysis and interpretation.Citation47 Studies in this project did not have funding to cover such costs. From an equity and diversity perspective, having a centralized process allows us to track those that may be systematically excluded from research based on English proficiency, allowing for an opportunity to address this limitation in the future.
Another issue was a potential selection bias against two groups of inpatients: (1) those who were re-admitted and changed their minds in favor of research participation; and (2) those who were not suitable for research upon assessment, but became suitable later in their stay. Regarding the former, it was decided not to re-screen inpatients re-admitted within one year based on the assumption that they were asked about research interest upon first admission. This could have affected a number of individuals who may have changed their minds as we observed the number of re-admissions rise from 2% of all admissions in the first 6 months of the project, to 6% by 24 months. Regarding the latter, inpatient suitability assessments took place within the first three days following admission, a timeframe based on research study needs (e.g. the need to collect data early in the rehabilitation stay, or at a specific time post-injury). There were some instances where three days was too soon to assess suitability as some inpatients may have needed time to process their traumatic SCI experience and/or manage major health complications such as dealing with high levels of pain which require narcotic analgesia that affect alertness, coping with anxiety and depression, or complex family or social situations. This pilot demonstrated that the three-day target deadline was not always feasible and that starting the CR process seven days post admission might be more appropriate for inpatients with SCI/D.
Conclusion
The Central Recruitment process reduced the burden of consent for subacute inpatients as: (1) study eligibility was rigorously delineated prior to meeting with inpatients; (2) a single patient research liaison interacted with the individual inpatient; (3) the CR process provided more efficient research screening with stable recruitment rates in a center where multiple research studies were occurring simultaneously; and, (4) provided stable research infrastructure which avoided the creation of unique infrastructure for each new study. Scalability of the CR process needs to be evaluated further and customized for a range of spinal cord injuries and pathologies in order to accommodate the secondary sequelae and comorbidities. The ultimate goal of expansion is to support multi-center trials to address the important research questions which impede the delivery of exemplary health care across the life course.
Disclaimer statements
Contributors: None.
Funding: This work was funded by the Ontario Neurotrauma Foundation ONF Grant 2011-SCI MENTOR-884 and the KITE Research Institute, University Health Network.
Declaration of interest: The authors declare that no competing interests exist. Furthermore, the authors wish to acknowledge the leadership and procedural support provided by UHN-TRI leadership including Gaetan Tardif, Susan Jewell, Alexander Karabanow, Mark Bayley and Joanne Zee.
Conflicts of interest: The authors declare that no competing interests exist.
Acknowledgements
All study procedures were reviewed and received approval from the local REB, and the Hospital Quality Assurance and Safety Board. The authors wish to acknowledge the leadership and procedural support provided by UHN-TRI leadership including Gaetan Tardiff, Susan Jewell, Alexander Karabanow, Mark Bayley and Joanne Zee. First author wishes to acknowledge the support of the UHN Foundation as Toronto Rehabilitation Institute Chair of Spinal Cord Injury Rehabilitation.
References
- Noonan VK, Fingas M, Farry A, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. NED 2012;38:219–26.
- Guilcher SJT, Voth J, Ho C, et al. Characteristics of non-traumatic spinal cord dysfunction in Canada using administrative health data. Top Spinal Cord Inj Rehabil 2017;23:343–52.
- New PW, Sundararajan V. Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord 2008;46:406–11.
- Government of Canada SC. Population estimates on July 1st, by age and sex [Internet]. 2017 [cited 2020 Aug 27]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501.
- McKinley WO, Tewksbury MA, Godbout CJ. Comparison of medical complications following nontraumatic and traumatic spinal cord injury. J Spinal Cord Med 2002;25:88–93.
- Hagen EM. Acute complications of spinal cord injuries. World J Orthop 2015;6:17–23.
- Guilcher SJT, Craven BC, Lemieux-Charles L, et al. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil 2013;35:894–906.
- Adriaansen JJE, Ruijs LEM, van Koppenhagen CF, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med 2016;48:853–60.
- Chan BC-F, Cadarette SM, Wodchis WP, et al. The lifetime cost of spinal cord injury in Ontario, Canada: a population-based study from the perspective of the public health care payer. J Spinal Cord Med 2019;42:184–93.
- Craven C, Hitzig SL, Mittmann N. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med 2012;35:361–70.
- Juul-Larsen HG, Christensen LD, Bandholm T, et al. Patterns of multimorbidity and differences in healthcare utilization and complexity among acutely hospitalized medical patients (≥65 years) – a latent class approach. Clin Epidemiol 2020;12:245–59.
- Johnston MC, Crilly M, Black C, et al. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health 2019;29:182–9.
- Catharine Craven B, Kurban D, Farahani F, et al. Predicting rehabilitation length of stay in Canada: it’s not just about impairment. J Spinal Cord Med 2017;40:676–86.
- Cheng CL, Plashkes T, Shen T, et al. Does specialized inpatient rehabilitation affect whether or Not people with traumatic spinal cord injury return home? J Neurotrauma 2017;34:2867–76.
- Blight AR, Hsieh J, Curt A, et al. The challenge of recruitment for neurotherapeutic clinical trials in spinal cord injury. Spinal Cord 2019;57:348–59.
- Heselmans A. Research participation for patients with spinal cord injury. The Lancet Neurology 2020;19(2):109.
- Craven BC, Balioussis C, Hitzig SL, et al. Use of screening to recruitment ratios as a tool for planning and implementing spinal cord injury rehabilitation research. Spinal Cord 2014;52:764–8.
- Blackmer J. The unique ethical challenges of conducting research in the rehabilitation medicine population. BMC Med Ethics 2003;4(E2). doi:https://doi.org/10.1186/1472-6939-4-2.
- Rose MA, Neil JA, Castles R, et al. Research in the rehabilitation unit presents challenges to nurse researchers. Rehabil Nurs 2017;42:104–8.
- Cardenas DD, Yilmaz B. Recruitment of spinal cord injury patients to clinical trials: challenges and solutions. Top Spinal Cord Inj Rehabil 2006;11:12–23.
- Anderson KD, Cowan RE, Horsewell J. Facilitators and barriers to spinal cord injury clinical trial participation: multi-national perspective of people living with spinal cord injury. J Neurotrauma 2016;33:493–9.
- Tuszynski MH, Steeves JD, Fawcett JW, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord 2007;45:222–31.
- Newington L, Metcalfe A. Factors influencing recruitment to research: qualitative study of the experiences and perceptions of research teams. BMC Med Res Methodol 2014;14(10). doi:https://doi.org/10.1186/1471-2288-14-10.
- Phelps EE, Tutton E, Griffin X, et al. Facilitating trial recruitment: a qualitative study of patient and staff experiences of an orthopaedic trauma trial. Trials 2019;20(1):492. doi:https://doi.org/10.1186/s13063-019-3597-8.
- Dorstyn D, Roberts R, Murphy G, et al. Work and SCI: a pilot randomized controlled study of an online resource for job-seekers with spinal cord dysfunction. Spinal Cord 2019;57:221–8.
- Fletcher B, Gheorghe A, Moore D, et al. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2012;2(e000496). doi:https://doi.org/10.1136/bmjopen-2011-000496.
- Cramer SC, Wolf SL, Adams HP, et al. Stroke recovery and rehabilitation research: issues, opportunities, and the national institutes of health StrokeNet. Stroke 2017;48:813–9.
- Nary DE, Froehlich-Grobe K, Aaronson L. Recruitment issues in a randomized controlled exercise trial targeting wheelchair users. Contemp Clin Trials 2011;32:188–95.
- Lloyd G, Dean CM, Ada L. Issues in recruiting community-dwelling stroke survivors to clinical trials: the AMBULATE trial. Contemp Clin Trials 2010;31:289–92.
- Rowlands C, Rooshenas L, Fairhurst K, et al. Detailed systematic analysis of recruitment strategies in randomised controlled trials in patients with an unscheduled admission to hospital. BMJ Open 2018;8:e018581.
- Cox K, Avis M, Wilson E, et al. An evaluation of the introduction of clinical trial officer roles into the cancer clinical trial setting in the UK. Eur J Cancer Care (Engl). 2005;14:448–56.
- Government of Canada IAP on RE. Tri-council policy statement: ethical conduct for research involving humans – TCPS 2 (2018) – Introduction [Internet]. 2019 [cited 2020 Jul 22]. Available from: https://ethics.gc.ca/eng/tcps2-eptc2_2018_introduction.html.
- International council for harmonisation of technical requirements of pharmaceuticals for human use. GUIDELINE FOR GOOD CLINICAL PRACTICE.:66.
- Noonan VK, Thorogood NP, Joshi PB, et al. Meeting the privacy requirements for the development of a multi-centre patient registry in Canada: the rick Hansen spinal cord injury registry. Healthc Policy 2013;8:87–99.
- Gagnon DH, Roy A, Gabison S, et al. Effects of seated postural stability and trunk and upper extremity strength on performance during manual wheelchair propulsion tests in individuals with spinal cord injury: an exploratory study. Rehabil Res Pract 2016;2016:6842324.
- Zbogar D, Eng JJ, Miller WC, et al. Physical activity outside of structured therapy during inpatient spinal cord injury rehabilitation. J Neuroeng Rehabil 2016;13:99.
- Zbogar D, Eng JJ, Noble JW, et al. Cardiovascular stress during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil 2017;98:2449–56.
- Zbogar D, Eng JJ, Miller WC, et al. Reliability and validity of daily physical activity measures during inpatient spinal cord injury rehabilitation. SAGE Open Med 2016;4:2050312116666941.
- Zbogar D, Eng JJ, Miller WC, et al. Movement repetitions in physical and occupational therapy during spinal cord injury rehabilitation. Spinal Cord 2017;55:172–9.
- Gabison S, Hayes K, Campbell KE, et al. Ultrasound imaging of tissue overlying the ischial tuberosity: does patient position matter? J Tissue Viability 2019;28:179–85.
- ANZCTR – Registration [Internet]. [cited 2020 Jul 22]. Available from: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=373729.
- AusCAN risk assessment for sitting acquired pressure ulcers [Internet]. Research Data Australia. [cited 2020 Aug 27]. Available from: http://purl.org/au-research/grants/nhmrc/634388.
- Gabison S, Verrier MC, Nadeau S, et al. Trunk strength and function using the multidirectional reach distance in individuals with non-traumatic spinal cord injury. J Spinal Cord Med 2014;37:537–47.
- Singh A, Tetreault L, Kalsi-Ryan S, et al. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 2014;6:309–31.
- Nasser N, Grady D, Balke CW. Commentary: Improving participant recruitment in clinical and translational research. Acad Med 2011;86:1334–5.
- Bell B, Hirji S. Balanced scorecard highlights: highlights from 2012–13 fourth quarter (January to March) [Internet]. [cited 2020 Jul 22]. Available from: https://www.uhn.ca/corporate/AboutUHN/Purpose_Performance/Documents/BSC_2012-13_Q4_Report.pdf.
- Squires A. Methodological challenges in cross-language qualitative research: a research review. Int J Nurs Stud 2009;46:277–87.
- The therapeutic misconception: informed consent in psychiatric research. Int J Law Psychiatry. 1982;5:319–29.
- Appelbaum PS, Roth LH, Lidz C. The therapeutic misconception: informed consent in psychiatric research. Int J Law Psychiatry 1982;5(3–4):319–29.