Abstract
Context
Severe traumatic fractures and dislocations of the lower cervical spine are usually accompanied by irreversible spinal cord injuries. Such patients rarely have mild or no neurological symptoms.
Findings
We report three cases of severe lower cervical dislocation without spinal cord injury and discuss the mechanisms underlying this type of injury. All three patients had severe lower cervical dislocation, but their neurological symptoms were mild. In all cases, the fractures occurred at the bilateral junctions of the lamina and pedicle, resulting in severe cervical spondylolisthesis, whereas the posterior structure remained in place, thereby increasing the cross-sectional area of the spinal canal. After preoperative skull traction for a few days, the patients underwent anterior or combined anterior and posterior cervical surgeries. All surgeries were successfully completed and the patient's symptoms disappeared at the last follow-up.
Conclusion
Severe traumatic dislocation of the lower cervical spine with an intact neurological status is rare in clinical practice. Pathological canal enlargement preserves neurological function, and the most commonly injured segment is C7. Preoperative traction for closed reduction remains controversial. We suggest that if no obvious anterior compression is observed, closed reduction should be pursued. Anterior or combined anterior and posterior cervical surgeries can provide rigid fixation with satisfactory results.
Introduction
Traumatic lower cervical fractures and dislocations are common conditions caused by high-energy accidents. This disease is usually associated with mechanical instability and severe irreversible spinal cord injury. Severe traumatic lower cervical fractures and dislocations with mild or no neurological symptoms are rare. Merianos et al. were the first to report this type of diseases (Citation1–3). Neurologically intact patients with severe cervical spondyloptosis represent a challenging clinical scenario for clinicians because of the need to preserve neurological function during reduction and internal fixation (Citation4). Here, we report three cases of severe traumatic spondylolisthesis with mild neurological symptoms at the cervicothoracic junction. Combined with previous literature, we discuss the mechanism of injury and treatment in this type of case.
Case reports
Case 1
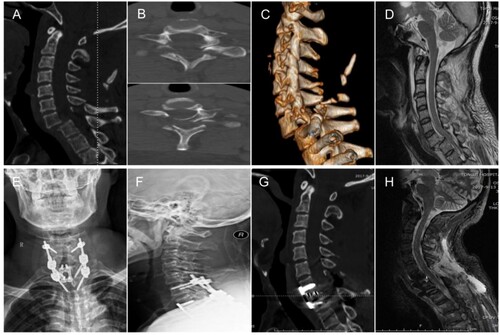
A 52-year-old man accidentally injured his head and neck by using heavy objects. He did not experience disturbance of consciousness but felt severe neck pain, numbness, and a slight loss of muscle strength in his right upper limb, while the sensation and movement of the other limbs were normal. After external immobilization using a neck collar and suturing the scalp wound in the emergency room, radiography, CTs and MRI were performed. Magnetic resonance imaging revealed a small subarachnoid hemorrhage and fractures at the bilateral junction of the lamina and pedicle, with grade III spondylolisthesis of C7 and no spinal cord injury. On the sagittal MRI image, we also observed enlargement of the spinal canal of C7 and prolapse of the intervertebral disc. After hospitalization, skull traction was applied for three days, gradually increasing from 3 to 10 kg to maintain stability and relax the cervical muscles. Then, anterior cervical discectomy was performed, spondylolisthesis was easily reduced with intra-operative traction, and anterior cervical fusion and posterior cervical-thoracic fixation were performed from C6 to T2. The patient's neurological condition did not worsen postoperatively. He was discharged from the hospital two weeks after surgery, with the feeling of his right upper extremity returning to normal. During the 3-year follow-up, the construct was stable and the clinical condition was satisfactory. The patient's right upper limb muscle strength and numbness returned to normal and the neck pain basically disappeared one month after the operation. The postoperative radiography showed that the internal construction was stable and the anterior intervertebral bone graft fusion was good. The imaging examinations are shown in .
Figure 1 Imaging examinations of case 1. (A) Sagittal image of the cervical spine CT demonstrated grade III spondylolisthesis of C7. (B) Axial image of C7 displayed bilateral fractures at the junction of the bilateral lamina and pedicle. (C) Three-dimension reconstruction image of the cervical spine. (D) MRI of the cervical spine showed mild compression and no edema signal of the spinal cord. (E–H) Postoperative X-ray films, CT and MRI showed that the cervical spine was well realigned and compression of the spinal cord was relieved
Case 2
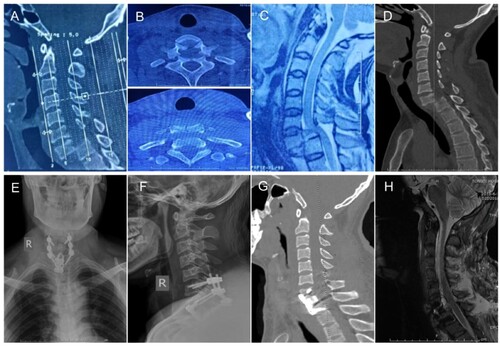
A 40-year-old man presented to our hospital after a motorcycle accident. He experienced mild numbness and weakness in his limbs, without any disturbance of consciousness. After external fixation of the neck with a brace, imaging was performed at a local hospital. Examination revealed grade IV spondylolisthesis of C7, with no spinal cord injury. In the sagittal MRI images, we also observed enlargement of the spinal canal at C7. Skull traction was applied at a local hospital and was gradually increased from 3 kg to 10 kg. After traction, his symptoms were slightly relieved, and the dislocation was slightly reduced. He was transferred to our department where skull traction was performed. We performed an anterior cervical discectomy, and the dislocation was easily reduced with intra-operative traction. We then performed anterior cervical fusion and posterior cervical thoracic fixation from C6 to T1. The patient's neurological condition did not worsen postoperatively. The patient was discharged 12 days after the surgery, and his symptoms disappeared. During the 2.5-year follow-up, the construct was stable and the clinical condition was satisfactory. All imaging findings are shown in .
Figure 2 Imaging examinations of case 2. (A) Sagittal CT of the cervical spine showed grade IV spondylolisthesis of C7. (B) Axial image of C7 displayed bilateral fractures at the junction of the bilateral lamina and pedicle. (C) MRI of the cervical spine showed mild compression and no edema signal of the spinal cord. (D) Sagittal CT of the cervical spine after traction showed the dislocation was slightly reduced. (E–H) Postoperative X-ray films, CT and MRI showed that the cervical spine was well realigned and compression of the spinal cord was relieved
Case 3
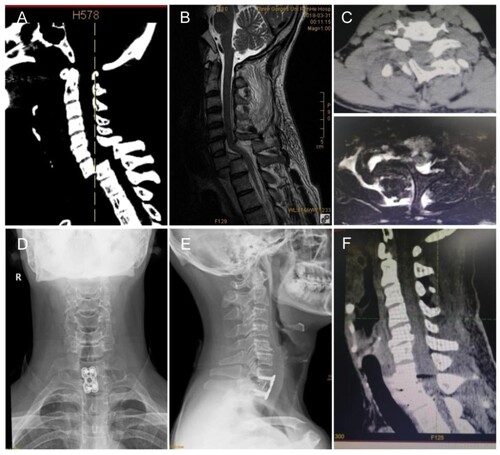
A 48-year-old man presented with numbness and weakness in his upper limbs and severe neck pain after a car accident; his lower limbs and consciousness were normal. He was immediately sent to a local hospital for imaging examinations. Computed tomography revealed C7 grade IV spondylolisthesis and fractures at the bilateral junctions of the lamina and pedicle. On MRI sagittal images, we observed no signs of spinal cord edema, and the spinal canal at C7 was enlarged. We performed an anterior cervical discectomy, and the spondylolisthesis was easily reduced with intra-operative traction. We then used a cage and plate for anterior fusion surgery. No deterioration in neurological function was observed after surgery, and his symptoms were relieved when he was discharged. At the 2-year follow-up, the construct was stable, and the clinical symptoms disappeared. All imaging examinations are shown in .
Figure 3 Imaging examinations of case 3. (A–B) Sagittal CT and MRI of the cervical spine showed grade IV spondylolisthesis and pathological enlargement of the spinal canal at C7. (C) Axial image of C7 displayed bilateral fractures at the junction of the bilateral lamina and pedicle. (D–F) Postoperative X-ray films and CT showed that the cervical spine was well realigned and width of the spinal canal had been restored
Discussion
Spondylolisthesis refers to the slippage of the upper vertebral body relative to its adjacent lower vertebral body (anterior or posterior spondylolisthesis). Lumbar spondylolisthesis is the most common type of spondylolisthesis, and its most frequent etiologies are congenital and high-energy traumas (Citation5). Traumatic cervical spondyloptosis is very common and is usually followed by narrowing of the spinal canal due to the displacement of the whole or part of the vertebra into the spinal canal. Traumatic cervical spondyloptosis is typically associated with complete and irreversible spinal cord injury. However, the literature rarely describes cases of grade III or more severe lower cervical spine spondylolisthesis with mild or no neurological deficits.
Merianos et al. first reported their observations in 17 patients with bilateral neural arch fractures associated with cervical fractures and dislocation (Citation3). It is worth noting that in these cases, 13 patients had no neurological symptoms, and 2 patients had only mild root lesions (Citation3). They attributed this phenomenon to fractures of the bilateral neural arch and anterior displacement of the body of the injured vertebra, while the posterior elements of the vertebra remained in place, thereby enlarging the cross-sectional area of the spinal canal (Citation3). Ramieri et al. also reported two similar cases, including one grade IV case (Citation6). In the present case, bilateral pedicle fractures occurred (Citation6). Due to the same mechanism of injury, the patient had no neurological symptoms before surgery (Citation6). After preoperative traction and partial reduction, the patient underwent combined anterior and posterior cervical surgeries under intraoperative traction (Citation6). The results were satisfactory during the 3-year follow-up period, the result was satisfactory (Citation6). Menku et al. have reported a case of grade IV C6 traumatic anterior spondylolisthesis with bilateral pedicle fractures (Citation7). The patient had no neurological symptoms before the surgery (Citation7). Owing to traumatic disc herniation, the patient did not undergo preoperative traction and underwent combined anterior and posterior internal fixation surgery after anterior decompression and reduction (Citation7). Tumialán et al. and Acikbas et al. reported a grade IV case of C7 traumatic anterior spondylolisthesis (Citation4, Citation8). No possible compression was found in front of the spinal cord; therefore, inline cervical traction was applied, and reduction was achieved before surgery (Citation4, Citation8). Both patients underwent combined anterior and posterior internal fixation without any new deficits (Citation4, Citation8). Munakomi et al. and Nguyen et al. reported grade IV cases of C7 spondylolisthesis in which preoperative traction was applied (Citation9, Citation10). However, there was no sign of reduction in either case, possibly due to locking of the bilateral facet joints; therefore, combined anterior and posterior cervical surgery was finally performed (Citation9, Citation10).
As summarized by Allen et al., the mechanism of injury in these patients is compressive extension injury (Citation11). These patients were in accordance with their definition of stage 4 and 5 injuries, which were described as bilateral vertebral arch fractures with partial or full vertebral body width displacing forward while the posterior portion of the vertebral arch remained in place (Citation11). Merianos et al. reported 17 cases of lower cervical spinal injuries with traumatic spinal canal (Citation3). They found that most patients had an injury to the forehead, indicating that the applied force resulted in a hyperextension injury (Citation3). During the injury, the neural arch of the vertebra was fractured, whereas the anterior displacement of the vertebra occurred during flexion, similar to the two patients described by Ramieri (Citation3, Citation6). In a review by Nguyen et al., 15 patients had high-grade traumatic cervical dislocation and minimal neurological deficits, and they found that C7/T1 was the most frequently affected level (9 cases) (Citation12). We believe that the cervical-thoracic junction is the transitional area between the rigid thoracic spine and movable cervical spine. In a hyperextension injury of the cervical spine, a huge shearing force may be generated, which can lead to fracture of the posterior arch of the C7. Without direct evidence, this must be confirmed by mechanical experiments.
For this type of injury, closed reduction itself may lead to devastating neurological compromise; therefore, preoperative traction to pursue closed reduction is still under debate (Citation13, Citation14). Surgeons who favor preoperative traction believe that the more preoperative alignment is achieved, the less invasive the surgery. Tumialan et al. performed closed reduction using inline traction with the patient awake before surgery (Citation4). After preoperative reduction, anterior surgery was limited to single-level discectomy and fusion, and only a two-stage surgery (anterior-posterior) was performed (Citation4). Ramieri et al. reported that a bipedicular fracture was easier to align than locked facets (Citation6). They obtained preoperative realignment through halo traction when the patient was awake, and the traction weight did not exceed 20 lb (Citation6). They did not observe deterioration of neurological function due to disc herniation, and the spondylolisthesis was well realigned (Citation6). In spondyloptosis, traction only achieves C6 distraction and C7 elevation without effective reduction (Citation6). Many studies do not recommend the use of cervical traction in the presence of significant traumatic disc herniation on preoperative MRI. Dahdaleh et al. recommended a post-traumatic cervical spondyloptosis treatment algorithm in which if significant anterior compression was present, closed reduction with preoperative traction was not pursued (Citation15). Preoperative traction and closed reduction can be conducted (Citation15). From a biomechanical point of view, these fractures are considered highly unstable; therefore, we suggest that if there is obvious anterior compression, preoperative and intraoperative traction can be conducted to relax the muscle, maintain stability of the cervical spine, and assist reduction during surgery, not for preoperative reduction. If no obvious anterior compression is found, preoperative traction and closed reduction can be performed when patients are awake, and should be performed under constant fluoroscopy to ensure safety.
The Subaxial Cervical Spine Injury Classification (SLIC) has important guiding significance in the treatment of lower cervical spine fractures (). According to the total score, surgery is recommended for a score greater than or equal to 5, conservative treatment is recommended for a score less than or equal to 3. When the SLIC score is 4, the choice of conservative or surgical treatment depends on the surgeon's preference. Patients with bilateral pedicle fractures and traumatic anterior spondylolisthesis are technically classified as “rotation/translation” injury in the SLIC system and get a score of at least 4. Usually, a discoligamentous complex (DLC) injury has a score of 2 or more, giving this type of injury a score of at least 6 even in neurologically intact individuals. Therefore, surgery is recommended to restore mechanical stability (Citation16).
Table 1 The Subaxial Cervical Spine Injury Classification. Scores are consisted of the 3 injury parts. Sum score greater than 4 is indicated for surgery, while scores less than 4 can be managed conservatively. Treatment option for patients with a score of 4 depends on surgeon's preference and other patient factors. DLC, discoligamentous complex.
The selection of a surgical approach depends on a combination of factors, including the surgeon's preference, patient factors, injury morphology, and the inherent advantages and disadvantages of the approach. Decompression of a traumatic disc herniation may require an anterior approach (Citation16). Another important consideration for anterior fixation is the presence of superior endplate or facet fractures (Citation17). Additionally, the state of the ligamentum flavum is a rare factor that must be considered. If this ligament is folded, it may cause spinal cord impingement upon reduction of the dislocation; therefore, anterior surgery is required (Citation18). A posterior approach may provide decompression and a stronger fixation. Although there is no additional advantage for neurological recovery, the combined approach can provide the strongest fixation and increase the fusion rate (Citation19, Citation20). Patients with poor bone quality, such as osteoporosis, ankylosing spondylitis, or other chronic conditions, may also be candidates for a combined approach (Citation21). Because of spondylolisthesis in the cases we reported, damage to the intervertebral disc was inevitable; therefore, anterior surgery was required to remove the damaged disc and perform intervertebral fusion, and reduction was easy to achieve after clearance of the intervertebral space. In addition, there was a fracture of the middle and posterior columns along with serious injury of the posterior ligaments and posterior internal fixation and bone graft fusion to achieve a strong fixation. Because fractures or soft tissues may recompress the spinal cord after reduction, the posterior approach can also decompress the spinal canal to relieve possible compression (Citation22). Therefore, we chose combined anterior and posterior surgery for case 1 and case 2. However, in case 3, we did not perform posterior surgery because reduction was successfully achieved after anterior surgery, and the patient's bone quality was satisfactory. The constructs were stable and the clinical conditions were satisfactory in all three cases.
Conclusion
High-grade traumatic cervical spondylolisthesis with intact neurological status is rare. Pathological canal enlargement appears to protect the spinal cord from damage during trauma. Based on a literature review, the cervicothoracic junction is the most commonly injured segment. A huge shearing force is generated in cervical hyperextension injuries, which leads to fractures of the posterior arch or bilateral pedicle. Preoperative traction for closed reduction remains controversial. We recommend that if no obvious anterior compression is found, closed reduction should be pursued. Anterior or combined anterior-posterior surgeries can provide firm fixation and achieve satisfactory results.
Abbreviations: CT: computer tomography, MRI: magnetic resonance imaging, SLIC: Subaxial Ceivical Spine Injury Classification, DLC: discoligamentous complex
Disclaimer statements
Contributors All mentioned authors contributed to the study conception and design. Literature search and data collection were performed by Z.C.Y. and Q.Y. Data analysis and writing of the manuscript draft were performed by C.X.L. and H.Z.
Funding This work was supported by the National Natural Science Foundation of China [grant number 82000659] and Hubei Natural Science Foundation [grant number 2022CFB924].
Declaration of interest None.
Conflicts of interest No potential conflict of interest was reported by the author(s).
Ethical parameters The Ethics Committee of Wuhan Tongji Hospital had confirmed that no ethical approval was required. Informed consent to participate was obtained from all individual participants included in the study.
Data availability statement The authors declare that the data supporting the findings of this study are available within the article.
References
- Ido K, Murakami H, Kawaguchi H, Urushidani H. An unusual reduction technique prior to surgical treatment for traumatic spondylolisthesis in the lower cervical spine. J Clin Neurosci 2002;9(6):664–666.
- Hagen T, Roser T, Linke G, Fegg M, Borasio G. The surgical management of traumatic C6 - C7 spondyloptosis in a patient without neurological deficits. Minimally Invasive Neurosurgery Min 2004;47(04):242–244.
- Merianos P, Manousidis D, Samsonas P, Baltopoulos P, Pateras N, Mavroudis G. Injuries of the lower cervical spine associated with widening of the spinal canal. Injury 1994;25(10):645–648.
- Tumialán LM, Dadashev V, Laborde DV, Gupta SK. Management of traumatic cervical spondyloptosis in a neurologically intact patient: case report. Spine 2009;34(19):E703–E708.
- Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am 2019;30(3):299–304.
- Ramieri A, Domenicucci M, Cellocco P, Lenzi J, Dugoni DE, Costanzo G. Traumatic spondylolisthesis and spondyloptosis of the subaxial cervical spine without neurological deficits: closed re-alignment, surgical options and literature review. Eur Spine J 2014;23(6):658–663.
- Menku A, Kurtsoy A, Tucer B, Oktem IS, Akdemir H. The surgical management of traumatic C6 - C7 spondyloptosis in a patient without neurological deficits. Minimally invasive neurosurgery: MIN 2004;47(4):242–244.
- Acikbas C, Gurkanlar D. Post-traumatic C7-T1 Spondyloptosis in a patient without neurological deficit: a case report. Turk Neurosurg 2010;20(2):257.
- Munakomi S, Bhattarai B, Cherian I. Traumatic cervical spondyloptosis in a neurologically stable patient: a therapeutic challenge. Case Rep Crit Care 2015;2015:540919.
- Nguyen HS, Doan N, Lozen A, Gelsomino M, Shabani S, Kurpad S. Traumatic spondyloptosis at the cervico-thoracic junction without neurological deficits. Surg Neurol Int 2016;7(Suppl 13):366–369.
- Allen BL, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine 1982;7(1):1–27.
- Nguyen HS, Soliman H, Kurpad S. Traumatic high-grade spondylolisthesis at C7-T1 with no neurological deficits: Case series, literature review, and biomechanical implications. J Craniovertebr Junction Spine 2017;8(1):74.
- Lee JY, Nassr A, Eck JC, Vaccaro AR. Controversies in the treatment of cervical spine dislocations. Spine J 2009;9(5):418–423.
- Gelb DE, Hadley MN, Aarabi B, Dhall SS, Hurlbert RJ, Rozzelle CJ, et al. Initial closed reduction of cervical spinal fracture-dislocation injuries. Neurosurgery 2013;72(Suppl 2):73–83.
- Dahdaleh NS, Dlouhy BJ, Greenlee JDW, Smoker WRK, Hitchon PW. An algorithm for the management of posttraumatic cervical spondyloptosis. J Clin Neurosci 2013;20(7):951–957.
- Khezri N, Ailon T, Kwon BK. Treatment of facet injuries in the cervical spine. Neurosurg Clin N Am 2017;28(1):125–137.
- Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine 2004;29(24):2815–2820.
- Rhee JM, Kimmerly WS, Smucker JD. Infolding of the ligamentum flavum: a cause of spinal cord compression after reduction of cervical facet injuries. Clin Spine Surg 2006;19(3):208–212.
- Bartels RHMA, Donk R. Delayed management of traumatic bilateral cervical facet dislocation: surgical strategy. Report of three cases. J Neurosurg 2002;97(3):362–365.
- Song K-J, Lee K-B. Anterior versus combined anterior and posterior fixation/fusion in the treatment of distraction-flexion injury in the lower cervical spine. J Clin Neurosci 2008;15(1):36–42.
- Lins CC, Prado DT, Joaquim AF. Surgical treatment of traumatic cervical facet dislocation: anterior, posterior or combined approaches? Arq Neuropsiquiatr 2016;74(9):745–749.
- Hiroaki N, Yasutsugu Y, Keigo I, et al. Posterior approach for cervical fracture–dislocations with traumatic disc herniation. Eur Spine J 2010;20(3):387–394.
