Abstract
Shift work can be associated with health and sleep problems, which may lead to cognitive impairment. This study investigated the effects of shift work on sleep, health behaviours and cognitive functions of Polish rescue service workers. We tested 18 paramedics working 12-h shifts, 15 firefighters working 24-h shifts and 17 daytime workers. We measured general sleepiness, workload during shifts and the occurrence of health behaviours. Additionally, we measured attention, executive function and subjective alertness. Paramedics showed lower average sleep duration and quality, and fewer health behaviours than firefighters and the control group. However, no differences were found in performance on cognitive tests between the groups and between the measures. The results indicate that the differences in job specificity may contribute to the effects of shift work on the sleep and health of the workers.
1. Introduction
The arrangement of working hours across the modern world has been changing rapidly over the last several decades. Nowadays, nearly 20% of workers worldwide work non-traditional hours (outside 7:00–18:00) [Citation1]. Shift work is common in many professions where services have to be maintained around the clock (protective services, healthcare professionals, production, etc.). Such 24-h operations are often necessary for public safety and health, which makes such arrangement of working time an indispensable aspect of our social organization. Working non-standard hours, especially night shifts, contends with the natural circadian rhythmicity of the human organism. Numerous scientific studies have demonstrated that this increasing diversification of worktime patterns can be associated with increased stress and other various acute and chronic negative effects on peoples’ health, such as sleep disorders, anxiety, digestive disturbances, diabetes, reproductive difficulties and gastrointestinal and cardiovascular diseases [Citation2–4].
One of the major complaints among shift workers is increased sleepiness and disturbed sleep. Misalignment of natural sleep–wake rhythms with working hours often results in sleep deprivation. Pilcher et al. [Citation5] in a meta-analysis of 36 studies found that permanent night-shift and rotating-shift workers, on average, sleep 1–2 h less than permanent day-shift workers, which affects mainly the second stage of sleep and rapid eye movement (REM) sleep. This is an alarming fact, since numerous studies show that sleep deprivation has strong, adverse effects on alertness and cognitive efficiency, which in consequence can be linked to a higher rate of vehicular and work-related accidents as well as errors on the job [Citation6]. Most noticeable cognitive consequences of sleep deprivation include decrement of attention and working memory, increased reaction time and impaired motor skills [Citation6–9]. It has been established that 17–19 h without sleep affect performance on tasks involving cognitive and motor speed, accuracy, coordination and attention to a level equivalent to that caused by alcohol intoxication at a blood alcohol concentration (BAC) of 0.05% [Citation10]. Moreover, some data suggest that sleep deprivation results in poorer insight into our performance, making us more confident that our answers in cognitive tasks are correct [Citation11], which can be a significant factor contributing to ‘human error’ and leading to work accidents. Overall, the number of errors in performed cognitive tasks is significantly higher on the night shift in comparison with the day shift, which allows us to draw conclusions that this is when the probability of work accidents is the highest [Citation12]. These findings are consistent with the fact that some of the most disastrous industry-related accidents of the last few decades caused by human error (e.g., Chernobyl, Three Mile Island, chemical spill into the Rhine and Valdez) occurred at night.
Maintaining a high level of performance is crucial for public service workers, as the consequences of errors made during work may affect the lives of others. For this purpose, it is extremely important to investigate the factors that may affect their cognitive performance. The current study was focused on two groups of public service workers: paramedics and firefighters. These two groups differ in their shift organization and duration. Paramedics work 12-h day and night shifts (see later), and the order of the shifts is irregular, while the firefighters work 24-h shifts with 48-h rest periods. Therefore, the study gave us the opportunity to compare the functioning of the public service works with regard to the shift-work organization.
The study focuses on the effects of shift work on participants’ cognitive functions in terms of attention, processing speed, inhibitory control and cognitive flexibility in relation to their shift pattern. These cognitive processes were indicated as susceptible to the circadian misalignment that is the consequence of shift work [Citation13–15]. However, the results of the previous studies are not conclusive, which may be a result of the methods applied, such as using self-assessment questionnaires in some of the studies [Citation16,Citation17]. Therefore, in our study we applied both subjective (questionnaires) and objective (cognitive tests) measures. The present study also takes into consideration the individual factors, such as perceived workload during the shift and sleep duration (both average and the night before the cognitive assessment).
To our knowledge, this study is the first attempt at complex assessment of the shift-work effect in Polish rescue services, as well as the first that compares working 12-h and 24-h shifts. We expected that the duration of shifts might show a significant difference in subjective and objective measures of cognitive performance as well as in the subjective levels of sleepiness reported in both compared groups.
2. Method
2.1. Participants
The present study was carried out among 33 shift workers: 18 paramedics (12 male, 6 female) and 15 firefighters (all male), and 17 white-collar workers (15 male, 2 female) who served as the control group and worked traditional 8-h day shifts. All participants were aged under 45 years and had a minimum 5 years of work experience and did not report any serious physical or mental problems (which were assessed by a survey prior to the study). They were recruited via email notices, electronic postings and information leaflets distributed to Warsaw fire departments, hospital emergency units and ambulance stations. The selection of subjects for the control group was based on demographic data (age, gender, education and work experience) so as to ensure their comparability to the shift-worker groups, thus there was no significant difference in age, level of education and work experience between all three groups (Table ). There were no females in the firefighter group (due to the specificity of this profession), hence the gender distribution in the study groups was unequal (χ2(2) = 7.108, p < 0.029). All participants gave their written consent prior to participation in the study (Table ).
Table 1. Characteristic data of study groups: distribution of gender and mean age, years of education and years of work experience.
There are significant differences in the organization of working time of firefighters and paramedics in Poland, regarding their working hours as well as the length of the shifts. Firefighters work 24-h shifts (8:00–8:00) followed by 48 h of rest. Paramedics work 12-h day or night shifts (7:00–19:00 or 19:00–7:00) and usually do not have a regular shift-rotation system. White-collar workers, who served as a control group in our study, work 8-h dayshifts (8:00–16:00 or 9:00–17:00).
2.2. Materials
The study involved questionnaires and standard psychomotor tests of attention and executive functions. Prior to the study, all participants filled out a 20-item questionnaire developed by the authors, concerning general health issues, demographic data and work schedule details.
2.2.1. Perceived workload
The participants were asked to judge their physical (one question) and psychological (one question) workload on a 5-point scale (1 = very low to 5 = very high).
2.2.2. Sleep and sleepiness measurement
The average sleep duration and sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI) [Citation18]. On the basis of the questionnaire, the average duration of sleep was calculated. Moreover, the PSQI global score was calculated and analysed. The higher the value of the PSQI global score, the poorer the sleep quality. According to the authors of the questionnaire, a global score of 5 or greater indicates poor sleep quality [Citation18]. While filling out the survey, the participants also assessed their level of tiredness on the day of the study and their sleep time duration the night before. They were also asked to complete the Epworth sleepiness scale [Citation19], which allowed us to assess their average sleep propensity in daily life.
2.2.3. Health behaviour
In order to establish pro-health behaviour of the participants, we used the Health Behaviour Inventory (HBI) [Citation20]. The questionnaire consists of 24 statements regarding health-related behaviours. The respondent rates a frequency of each behaviour on a 5-point scale (1 = almost never to 5 = almost always), which allowed us to determine the general severity of behaviour conducive to his health, and also the scores on four subscales: proper nutrition habits, preventive behaviour, health practices and positive mental attitude.
2.2.4. Cognitive functions
Cognitive functions, i.e., attention and executive functions, were measured three times. Each time, two tests were administered: the D2 test of sustained attention [Citation21] and the color trails test (CTT) [Citation22]. In the D2 test, the participant has to cross out all letters ‘d’ with two short lines from a mix of letters ‘d’ and ‘p’ with various numbers of lines (one to three). The test consists of 14 rows of ‘d’ and ‘p’ letters, and each row should be completed within a time of 20 s. We analysed the following parameters of the tests: Corrected Speed (Speedc) – the total number of letters worked through minus the number of errors as an index of processing speed (error-corrected); Error Rate – the percentage of the errors made in the test; Variance – the difference between the row with the maximum number of the letters crossed out and the row with the minimum number of letters crossed out, as an index of processing variability; Correctly Detected – total number of the correctly crossed out letters minus the number of the letters incorrectly crossed out – the index of concentration.
Three parallel forms of the CTT (A, B and C) were used, to minimize the test–retest effect on the scores. We used both parts of the tests: CTT1, where the circles with numbers from 1 to 25 have to be connected as quickly as possible in the ascending order; and CTT2, where the subject has to connect the circles with numbers ascending while alternating between two colours (yellow and pink) in each step. The time to complete each part of the task (in seconds) was analysed, as a measure of performance. Errors in the tests were not taken into the analyses, as very few participants committed them. Additionally, the subjective level of sleepiness of the participants was assessed using the Polish adaptation of the Karolinska sleepiness scale (KSS) [Citation16] with the total score taken into the analyses.
2.3. Study design
In each group, the set of tasks measuring cognitive performance was conducted three times on different days. The order of meetings was randomized to eliminate any influence of the test–retest effect on task performance.
In the group of paramedics, the assessment was carried out after the day shift (ca. 20:00), after the night shift (ca. 8:00) and in the evening on the day off work (ca. 18:00). The firefighters underwent the assessment after the 24-h shift (ca. 9:00), on the day off work in the morning (ca. 9:00) and on the day off work in the evening (ca. 18:00). In the case of day workers from the control group, the study took place on the day off work in the morning (ca. 9:00), on the day off-work in the evening (ca. 18:00) and after work (ca. 18:00).
During each assessment session, the participants filled out the questionnaire concerning their level of tiredness, hours of sleep and the perceived workload during the last shift (if the assessment was performed after work). Afterwards, they filled out the KSS and performed the D2 and CTT tests. The scheme of the measurement times is summarized in Table .
Table 2. Timetable of cognitive measurement performed repeatedly in shift and day workers.
2.4. Statistical analysis
As not all of the results showed a normal distribution (Kolmogorov–Smirnov test), non-parametric tests were applied in the analysis. The variables measured once during the study, such as health behaviour (HBI scores), sleep duration and quality (PSQI scores), as well as subjective workload were compared between the three groups using the Kruskal–Wallis test. The same test was applied to analyse differences in cognitive functions on a day off (three groups). The Dunn–Bonferroni test was applied for pairwise comparisons. The repeated measures that were carried out in each group (D2 test, CTT and KSS) were compared using Friedman analysis of variance (ANOVA) with the Dunn–Bonferroni test applied for pairwise comparison of the groups. Data were analysed using IBM SPSS version 24.0.
3. Results
3.1. Perceived workload
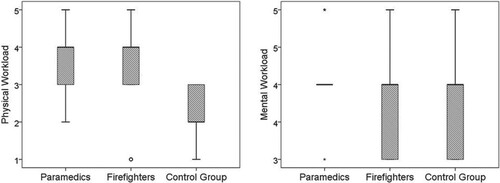
The analysis showed that there were significant differences in perceived physical workload (Figure ) between the groups (H(2) = 21.226, p < 0.001). The post-hoc analysis revealed that both the firefighters and the paramedics had higher physical workload than the control group (paramedics vs control group, p < 0.001; firefighters vs control group, p < 0.001). There were, however, no differences in perceived mental workload between the groups. All three groups judged their work as at least ‘moderately demanding’ (score 3 on the mental workload scale).
3.2. Average sleep duration and sleepiness
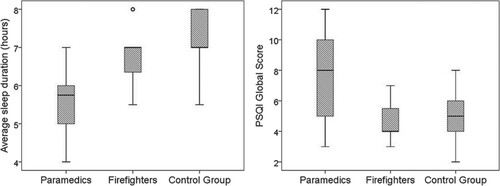
Analysis of the average sleep duration measured with the PSQI questionnaire showed that there was a significant difference in sleep duration between the groups (H(2) = 19.141, p < 0.001) (Figure ). Pairwise comparisons revealed that the average sleep duration among the paramedics (Mdn 5.75 h) was significantly shorter than among the firefighters (Mdn 7 h; p < 0.016) and the control group (Mdn 7 h; p < 0.001). There was no significant difference between sleep duration of the firefighters and the control group. Analysis of the PSQI global score also revealed that the groups differed significantly (H(2) = 9.866, p < 0.007) (Figure ). Pairwise comparisons showed that the paramedics obtained a significantly higher global score than the firefighters (p < 0.12) and the control group (p < 0.042). There were no significant differences in the PSQI global score between the firefighters and the control group. No significant differences between the groups were revealed for the Epworth sleepiness scale.
Figure 2. Results of the PSQI among two groups of shift workers (paramedics and firefighters) and the control group (day workers): average sleep duration (left) and global score (right).
Note: The circle in the box plot indicates outlier data in a particular group. PSQI = Pittsburgh Sleep Quality Index.
3.3. Health behaviour
The analysis of the total score for the HBI revealed significant differences between the groups (H(2) = 7.751, p < 0.021). The pairwise comparisons revealed that the paramedics obtained a significantly lower score than the firefighters (p < 0.032). The results also showed that the total HBI score was lower in the paramedics than in the control group. However, this result turned non-significant after adjustment of the p values to correct the results for multiple comparisons.
The analysis of the scores obtained for the four subscales of the HBI revealed that the groups differed in proper nutrition habits (H(2) = 6.991, p < 0.03) (Figure ) and health practices (H(2) = 16.502, p < 0.001). The pairwise comparisons revealed that the paramedics showed less frequent proper nutrition habits than the firefighters (p < 0.041). The analysis showed also that the frequency of proper nutrition was lower in the paramedics than in the control group, but the result turned non-significant after adjusting the probability value for multiple comparisons.
Figure 3. HBI results: proper nutrition habits score (upper right), health practices score (upper left) and total score (below) among the paramedics, the firefighters and the control group.
Note: The outlier values in a particular group are marked with circles and extreme values are marked with asterisks. HBI = Health Behaviour Inventory.
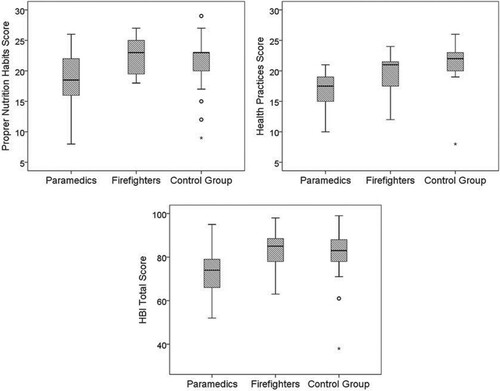
Pairwise comparisons of the scores obtained in the health practices subscale showed that these practices were significantly less frequent in the paramedics than in the other two groups (paramedics vs firefighters, p < 0.038; paramedics vs control group, p < 0.001). The scores obtained in the group of firefighters and the control group did not differ significantly.
3.4. Cognitive functioning
3.4.1. Shift workers vs daytime workers
In order to compare cognitive functions between the groups, the assessment of alertness and executive functions was carried out during the day off at the same time (day off in the afternoon). A between-group comparison of the scores obtained for the KSS as well the two applied cognitive tests (D2 and CTT) did not yield any significant results. The mean results obtained in each group are presented in Table .
Table 3. Scores obtained during consecutive measurements in paramedics and firefighters and in day workers (control group).
3.4.2. Cognitive functioning after the day, night and 24-h shifts and on a day off
In order to assess the impact of working day and night shifts on paramedics’ functioning, the results of the three measurements were compared (after day shift, after night-shift and on the day off). The comparison of the scores obtained for the KSS revealed statistically significant differences in the subjective level of sleepiness during the three sessions (Friedmann ANOVA: χ2 = 19.452, p < 0.001). The paramedics felt more sleepy after the night shift (KSS score: Mdn 6.5) than after the day shift (KSS score: Mdn 4; p < 0.014) and on the day off (KSS score: Mdn 4; p < 0.001). There were no significant differences in the level of sleepiness after the day shift and on the day off in the evening.
The comparison of the D2 and CTT tests performed during the three measurements did not yield any significant results.
In the case of the firefighters as well as the control group there were no differences in the subjective level of sleepiness (as measured by the KSS) between the three sessions. The comparison of the D2 and CTT tests performed during the three measurements did not yield any significant results.
3.4.3. Comparison of the night and 24-h shifts
As both the night shift and the 24-h shift require workers to be awake during night hours, we therefore decided to compare the perceived workload, sleep duration as well as cognitive performance after working a 12-h night shift and a 24-h shift.
The analysis of the perceived physical and cognitive workload yielded no significant differences. However, we found that the paramedics slept significantly less during the night shift (Mdn 3 h) than the firefighters during the 24-h shift (Mdn 5 h; U = 26.5, p < 0.001). This result was followed by a higher level of sleepiness in the paramedics (KSS score: Mdn 6.5) than in the firefighters (KSS score: Mdn 4). There were no group differences between the results of the cognitive tests (CTT and D2).
4. Discussion
The present study focused on the effects of shift work on cognitive performance, as well as pro-health behaviours of Polish public service workers, i.e., paramedics and firefighters. The study investigated factors related to the organization of shift work and the shift duration. Both subjective and objective measures of cognitive performance were applied in this study. The analysis of the perceived workload revealed that only the physical demands of the shift work are judged higher than the day work. Interestingly, we found no group differences in perceived cognitive workload.
The analysis of the average sleep duration and quality (PSQI) showed that the paramedics, on average, sleep less and have a poorer sleep than the firefighters and the control group. This group also obtained the lowest score in the HBI questionnaire measuring pro-health behaviours. They obtained a lower score for the proper nutrition score as well as pro-health practices (such as exercise, healthy eating habits, etc.).
The comparisons of the cognitive performance after work (after a day shift, night shift and 24-h shift) and on the day off showed that there were differences in the subjective measure of alertness (KSS score) only in the paramedic group. There were no significant differences between the results of the cognitive tests performed after shifts and on the day off in none of the groups.
The comparison of the performance after the 12-h night shift and the 24-h shift also showed that the paramedics slept significantly less during the night before the cognitive assessment and felt significantly more sleepy (KSS) during the cognitive assessment. However, we found no significant differences between the groups in the cognitive test results.
To sum up, our results indicate that the paramedic group was the most affected by the consequences of shift work in terms of duration and quality of sleep. However, we found no differences between the groups either in the subjective or the objective measures of cognitive performance. Such a result may suggest that this group of workers may maintain their cognitive abilities despite prolonged sleep deprivation. Some of the previous studies show no evident association between shift work and cognitive impairment. For example, a study conducted among emergency physicians working day and night shifts did not reveal any changes in their performance on the trial making test before and after day and night shifts [Citation23].
On the other hand, numerous studies suggest that shift work can be associated with both short and long-term cognitive impairment (e.g., [Citation24–26]). Shift workers are often not only exposed to acute sleep deprivation (resulting from being kept awake for prolonged periods of time) but also to chronic sleep restriction. Results of a VISAT longitudinal cohort study [Citation25] of more than 3000 workers showed that long-term exposure to circadian disruption is associated with chronic deterioration of cognition and that this effect is positively correlated with the number of years of exposure to shift work. It appears that such abnormal work schedules may have long-term consequences with regards to cognitive abilities. The fact that we did not observe the differences in this study does not necessarily mean that they will not appear in the future as long-term consequences.
Our results could relate to the length of the tests performed during particular studies, because it has been established that lapses of attention caused by fatigue and sleep deprivation are more pronounced in sustained or continuous work lasting more than 3 min [Citation27]. The tests carried applied in our study (D2 and CTT) are relatively short and this factor could contribute to the lack of differences in the scores obtained by the participants. Another factor that could influence the obtained results is the relatively young age of the studied groups as well as their experience. More than one-third (35%) of our study group were aged under 30 years and 94% were under 40 years, so they may not yet experience chronic, long-term effects of their non-traditional working hours. Younger subjects are able to maintain relatively constant performance on both day and night shifts, while there was a significant change in performance across the shifts in older subjects [Citation28]. On the other hand, all of the participants had at least 5 years of work experience. This criterion was used to ensure that the cognitive performance of the participants might have already been influenced by the shift work. However, at the same time, 5 years is long enough for the self-selection to have taken place. It has been proven that there are differences among employees in tolerance to shift work and individuals with specific sleep behaviours tend to cope with this job type more effectively than other people [Citation29]. About 20% of workers are not capable of tolerating non-traditional working hours and return to day work within the first 2–3 years [Citation30].
Moreover, the obtained results could be explained in relation to the phenomenon called the ‘healthy shift-worker effect’ [Citation29,Citation30], which poses that shift workers may be healthier than the general population of workers and cope better with demands of working non-standard hours. It is possible that due to the inclusion criteria of this study (5 years of experience), our sample consisted of workers who were already adapted to shift work, and therefore they could maintain the performance despite tiredness. The future studies should focus more on the process of adaptation to shift work, i.e., include participants with varying work experience.
Our analysis revealed no differences in perceived mental workload between shift workers and the control group, as both groups judged their work as ‘moderately demanding’ or ‘higher’. Existing data suggest that people who join emergency-services professions have personality characteristics that allow them to cope more effectively with high level of stressors (e.g., higher extraversion and excitement-seeking), thus they may underestimate the psychological strain of their jobs [Citation31]. Perceived physical workload, however, was higher among firefighters and paramedics than in the control group. These results can be associated with the specificity of tasks related with each profession. Our control group consisted of white-collar workers whose job consists mainly of strictly intellectual tasks, whereas both shift-worker groups in our study perform activities causing mental as well as physical strain.
The significant differences between the consecutive measurements after work and on a day off showed only that in the group of paramedics was the sleepiness higher after the night shift than after the day shift and on the day off. It was also higher than the declared sleepiness among the firefighters after the 24-h shift. Further analyses revealed that there were significant differences in average sleep duration (PSQI; Figure ) between our study groups, with paramedics sleeping less than both the firefighters and the control group. The paramedics also obtained a higher PSQI global score, which means that their perceived sleep quality is poorer than in the two other groups. These results can be associated with the shift organization in this group, as their work was less regular and shift rotation was faster.
It has been proven that the possibility of napping is one of the factors improving reaction time and alertness and mitigating the effects of fatigue from extended work hours and night-shift work [Citation32,Citation33]. What is interesting, however, is that neither paramedics nor firefighters in our study scored higher than the control group on the Epworth sleepiness scale, which is a tool designed to estimate a person’s ‘average sleep propensity’ across a wide range of activities in their daily lives [Citation34]. This result is consistent with other studies. For example, Garbarino et al. [Citation35] evaluated the sleepiness and sleep disorders among police officers working shifts and among daytime workers, and they found no differences in the ESS score, despite a significantly higher rate of sleep disorders among shift workers than in the non-shift-worker group. It is possible that the ESS score, which is a subjective measure of sleepiness, may be influenced by confounding factors such as particularly stressful work associated with high responsibility, which may lead to underestimate the possibility of falling asleep or even actually lead to maintaining a high level of vigilance in many conditions. This could also be the case for the participants in our study.
Our analysis revealed that only the paramedics had a lower level of declared health behaviours than the two other study groups, especially with regard to proper nutrition habits. These results are consistent with many previous studies showing adverse effects of shift work on daily life-style behaviours, eating and exercise habits [Citation36,Citation37]. A systematic review by Zhao and Turner [Citation38] revealed that shift work can be associated with poor dietary intake, smoking and becoming overweight. In our study, the aforementioned effect was not observed in the group of firefighters, which can be explained by the fact this one of their job requirements is a high level of physical fitness. However, a steady shift pattern (24-h shift, 48 h of rest) may also be the factor that facilitates maintaining healthy habits. Moreover, the paramedics reported less possibilities of napping during their night shifts (less hours of sleep). This can promote imbalance in appetite hormones, leading to increased feelings of hunger and metabolic changes resulting in obesity, insulin resistance and reduced lipid tolerance [Citation39]. It has been proven that the adverse effects of shift work can be reduced by appropriate matching between workers’ circadian rhythm and the shift pattern (regarding the rotation and length of shifts). Studies have shown that most often people find it easier to adapt to slowly rotating shifts and the likelihood of committing a human error is lower among these workers [Citation40]. The results of our study are consistent with these findings, as the firefighters, whose shift pattern is more regular and slower rotating, tend to suffer less adverse effects of this non-traditional working schedule than the paramedics. It must be noted, however, that the results of some other studies (e.g., [Citation41]) indicate better tolerance of fast-rotation shifts.
This study is the first research to investigate the effect of shift work on Polish public service workers. The results show that not only the mere length of the shift (12 or 24 h) but also the differences in job specificity (e.g., possibilities to napping during shifts) of shift workers may influence the obtained results. There are, however, some limitations to the study. First, the study sample is relatively small. A larger population should be studied in the future to confirm the results obtained. Moreover, although we applied cognitive tests as objective measures of the performance, a lot of data were still collected using subjective measures (questionnaires). This applies especially to data such as sleep duration and quality. In future studies, it would be recommendable to use objective measures of sleep such as physiological markers. Although such a measurement and analysis is more demanding, the data obtained would be more precise. Finally, as already mentioned, future studies could include groups with different work experience (e.g., 1–3, 5–8, 10 years and more) to compare the shift-work effect in different groups.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Wright KP Jr, Bogan RK, Wyatt JK. Shift work and the assessment and management of shift work disorder (SWD). Sleep Med Rev. 2013;17(1):41–54. doi: https://doi.org/10.1016/j.smrv.2012.02.002
- Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. Bmj. 2016;355:i5210. doi: https://doi.org/10.1136/bmj.i5210
- Proper KI, van de Langenberg D, Rodenburg W, et al. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med. 2016;50(5):e147–e157. doi: https://doi.org/10.1016/j.amepre.2015.11.013
- Srivastava UR. Shift work related to stress, health and mood states: a study of dairy workers. J Health Manag. 2010;12(2):173–200. doi: https://doi.org/10.1177/097206341001200205
- Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23:1–9. doi: https://doi.org/10.1093/sleep/23.2.1b
- Dinges DF, Douglas SD, Zaugg L, et al. Leukocytosis and natural killer cell function parallel neurobehavioral fatigue induced by 64 hours of sleep deprivation. J Clin Invest. 1994;93(5):1930–1939. doi: https://doi.org/10.1172/JCI117184
- Caruso NC, Radovanovic B, Kennedy JD, et al. Sleep, executive functioning and behaviour in children and adolescents with type 1 diabetes. Sleep Med. 2014;15(12):1490–1499. doi: https://doi.org/10.1016/j.sleep.2014.08.011
- Doran SM, Van Donge HPA, Dinges DF. Sustained attention performance during sleep deprivation: evidence of state instability. Archives italiennes de biologie. 2001;139(3):253–267.
- Wright KP Jr, Badia P. Effects of menstrual cycle phase and oral contraceptives on alertness, cognitive performance, and circadian rhythms during sleep deprivation. Behav Brain Res. 1999;103(2):185–194. doi: https://doi.org/10.1016/S0166-4328(99)00042-X
- Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57(10):649–655. doi: https://doi.org/10.1136/oem.57.10.649
- Harrison Y, Horne JA. The impact of sleep deprivation on decision making: a review. J Exp Psychol Appl. 2000;6(3):236–249. doi: https://doi.org/10.1037/1076-898X.6.3.236
- Kazemi R, Haidarimoghadam R, Motamedzadeh M, et al. Effects of shift work on cognitive performance, sleep quality, and sleepiness among petrochemical control room operators. J Circad Rhyth. 2016;14:1. doi:https://doi.org/10.5334/jcr.134.
- Akerstedt T. Psychological and psychophysiological effects of shift work. Scand J Work Environ Health. 1990;16(Suppl 1):67–73. doi: https://doi.org/10.5271/sjweh.1819
- Arendt J. Shift work: coping with the biological clock. Occup Med. 2010;60(1):10–20. doi: https://doi.org/10.1093/occmed/kqp162
- Markwald RR, Wright KP. Circadian misalignment and sleep disruption in shift work: implications for fatigue and risk of weight gain and obesity. Sleep loss and obesity. New York (NY): Springer; 2012.
- Åkerstedt T, Fredlund P, Gillberg M, et al. Work load and work hours in relation to disturbed sleep and fatigue in a large representative sample. J Psy Res. 2002;53(1):585–588. doi: https://doi.org/10.1016/S0022-3999(02)00447-6
- Gold DR, Rogacz S, Bock N, et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Pub Health. 1992;82(7):1011–1014. doi: https://doi.org/10.2105/AJPH.82.7.1011
- Buysse DJ, Reynolds CF III, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psy Res. 1989;28(2):193–213. doi: https://doi.org/10.1016/0165-1781(89)90047-4
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: https://doi.org/10.1093/sleep/14.6.540
- Juczyński Z. Narzędzia pomiaru w promocji i psychologii zdrowia [Measurement tools in health psychology and promotion]. Warszawa: Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego; 2001. pp. 167–174. Polish.
- Bates ME, Lemay EP. The D2 test of attention: construct validity and extensions in scoring techniques. J Int Neuropsychol Soc. 2004;10(3):392–400. doi: https://doi.org/10.1017/S135561770410307X
- D’Elia LF, Satz P, Uchiyama CL, et al. Color trails test. Odessa: Psychological Assessment Resources; 1996.
- Machi MS, Staum M, Callaway CW, et al. The relationship between shift work, sleep, and cognition in career emergency physicians. Emerg Med. 2012;19(1):85–91.
- Ansiau D, Wild P, Niezborala M, et al. Effects of working conditions and sleep of the previous day on cognitive performance. Appl Ergonom. 2008;39(1):99–106. doi: https://doi.org/10.1016/j.apergo.2007.01.004
- Marquié JC, Tucker P, Folkard S, et al. Chronic effects of shift work on cognition: findings from the VISAT longitudinal study. Occup Environ Med. 2015;72(4):258–264. doi: https://doi.org/10.1136/oemed-2013-101993
- Titova OE, Lindberg E, Elmståhl S, et al. Association between shift work history and performance on the trail making test in middle-aged and elderly humans: the EpiHealth study. Neurob Aging. 2016;45:23–29. doi: https://doi.org/10.1016/j.neurobiolaging.2016.05.007
- Balkin TJ, Bliese PD, Belenky G. Comparative utility of instruments for monitoring sleepiness-related performance decrements in the operational environment. J Sleep Res. 2004;13:219–227. doi: https://doi.org/10.1111/j.1365-2869.2004.00407.x
- Reid K, Dawson D. Comparing performance on a simulated 12 hour shift rotation in young and older subjects. Occup Environ Med. 2001;58:58–62. doi: https://doi.org/10.1136/oem.58.1.58
- Saksvik IB, Bjorvatn B, Hetland H. Individual differences in tolerance to shift work – a systematic review. Sleep Med Rev. 2011;15(4):221–235. doi: https://doi.org/10.1016/j.smrv.2010.07.002
- Knutsson A, Akerstedt T. The healthy-worker effect: self-selection among Swedish shift workers. Work Stress. 1992;6(2):163–167. doi: https://doi.org/10.1080/02678379208260350
- Salters-Pedneault K, Ruef A M, Orr SP. Personality and psychophysiological profiles of police officer and firefighter recruits. Personal Ind Diff. 2010;49(3):210–215. doi: https://doi.org/10.1016/j.paid.2010.03.037
- McDonald J, Potyk D, Fischer D, et al. Napping on the night shift: a study of sleep, performance, and learning in physicians-in-training. J Grad Med Educ. 2013;5(4):634–638. doi: https://doi.org/10.4300/JGME-D-12-00324.1
- Smith-Coggins R, Howard SK, Mac DT, et al. Improving alertness and performance in emergency department physicians and nurses: the use of planned naps. Ann Emerg Med. 2006;48(5):596–604. doi: https://doi.org/10.1016/j.annemergmed.2006.02.005
- Chen NH, Johns MW, Li HY, et al. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res. 2002;11(8):817–821. doi: https://doi.org/10.1023/A:1020818417949
- Garbarino S, de Carli F, Nobili L, et al. Sleepiness and sleep disorders in shift workers: a study on a group of Italian police officers. Sleep. 2002;25(6):642–647.
- Geliebter A, Gluck ME, Tanowitz M, et al. Work-shift period and weight change. Nutrition. 2000;16(1):27–29. doi: https://doi.org/10.1016/S0899-9007(99)00228-2
- Reeves SL, Newling-Ward E, Gissane C. The effect of shift-work on food intake and eating habits. Nutr Food Sci. 2004;34(5):216–221. doi: https://doi.org/10.1108/00346650410560398
- Zhao I, Turner C. The impact of shift work on people’s daily health habits and adverse health outcomes. Austr J Adv Nurs. 2008;25(3):8.
- Spiegel K, Tasali E, Leproult R. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol. 2009;5(5):253–261. doi: https://doi.org/10.1038/nrendo.2009.23
- San Chang Y, Wu YH, Hsu CY, et al. Impairment of perceptual and motor abilities at the end of a night shift is greater in nurses working fast rotating shifts. Sleep Med. 2011;12(9):866–869. doi: https://doi.org/10.1016/j.sleep.2011.03.018
- Fischer FM, Bruni AC, Berwerth A, et al. Do weekly and fast-rotating shiftwork schedules differentially affect duration and quality of sleep? Int Arch Occup Environ Health. 1997;69(5):354–360. doi: https://doi.org/10.1007/s004200050160