Abstract
The social processes of stigmatization and discrimination can have complex and devastating effects on the health and welfare of families and communities, and thus on the environments in which children live and grow. The authors conducted a literature review to identify interventions for reducing the stigma and discrimination that impede child health and well-being in low- and middle-income countries, with a focus on nutrition, HIV/AIDS, neonatal survival and infant health, and early child development. Despite broad consensus on the importance of stigma and discrimination as barriers to access and uptake of health information and services, the authors found a dearth of research and program evaluations directly assessing effective interventions in the area of child health except in the area of reducing HIV-related stigma and discrimination. While the literature demonstrates that poverty and social exclusion are often stigma-laden and impede adult access to health information and services, and to education relevant to family planning, child rearing, nutrition, health promotion, and disease prevention, the child health literature does not document direct connections between these known mediators of child health and the stigmatization of either children or their caregivers. The child health field would greatly benefit from more research to understand and address stigma as it relates to child health and well-being. The authors suggest applying a framework, adapted from the HIV stigma field, to direct future research and the adaptation of existing strategies to reduce HIV-related stigma and discrimination to address social and health-related stigmas affecting children and their families.
Children's well-being is a function of their environmental experiences and their opportunities to meet their potential. Stigma and discrimination related to social standing and health can significantly affect child health by impeding or diverting child health and development outcomes and pathways. Stigma has been documented in association with a wide range of conditions such as leprosy (van Brakel et al., Citation2012), epilepsy (Viteva, Citation2012), tuberculosis (Courtwright & Turner, Citation2010), disability (Ali, Hassiotis, Strydom, & King, Citation2012) and other mental health diagnoses (Kleinman, Citation1995; O'Driscoll, Heary, Hennessy, & McKeague, Citation2012). Research on stigma associated with these conditions has demonstrated that the social processes of stigmatization and discrimination can have complex and often devastating effects on the health and welfare of individuals, families, and whole communities.
While there is limited published research on stigmatization of children (younger than 5 years old), the health and human development of children is profoundly affected by the environment in which they and their caretakers live, learn, and grow (Wilkinson & Marmot, Citation2003). That is, stigmatization and discrimination of a child's family or community is likely to affect the child's health and life chances. Research concerning children affected by HIV has shown that HIV-related stigma amplifies the negative effects of loss and economic deprivation resulting from parental illness, disability, and death (Foster & Williamson, Citation2000). For example, Cluver and colleagues (Cluver, Citation2011; Cluver, Bowes, & Gardner, Citation2010; Cluver & Gardner, Citation2007; Cluver et al., Citation2013) have shown clearly that children orphaned by AIDS report higher levels of mental health burden than do children orphaned by other means, exacerbated considerably by experiences of stigma (Cluver, Gardner, & Operario, Citation2008).
More broadly, it is well established that HIV stigma, discrimination, and social exclusion impede both provision and uptake of health information and services among young people and adults in contexts ranging from housing and employment to health care (Pulerwitz, Michaelis, Weiss, Brown, & Mahendra, Citation2010; Turan & Nyblade, Citation2013). It is clear that stigma and discrimination are important factors and that interventions which interrupt or reduce the negative manifestations of stigma could actively contribute to health policies, services, and individual behaviors that enhance child health and development outcomes. This review sought to identify research on interventions that aimed to reduce stigma and discrimination in order to promote child health in low- and middle-income countries, with the aim of identifying characteristics of interventions that were effective and could produce population-level impact. The review included stigma related to major causes of child morbidity and mortality, including nutrition, malaria, acute respiratory illness, diarrheal disease, and immunization, but focused primarily on stigma associated with HIV and AIDS because of greater literature in this area. Another review in this issue of the journal addresses studies that have examined gender equity and discrimination against women as it relates to nutrition (Kraft, Wilkins, Morales, Widyono, & Middlestadt, Citation2014), therefore we did not consider that topic in our review.
While children can be directly affected by stigma (e.g., in cases of disability or mental illness), our study explored stigma associated with childhood diseases of high impact in low- and middle-income countries that could negatively influence child health outcomes. Therefore, our review focused on the indirect effects of stigma that children under 5 may experience because of stigmatizing attitudes and actions that directly affect their adult caretakers and community members.
What Is Stigma?
The ability of social groups to assign a stigma (a discrediting mark or negative judgment) to people, attributes and/or behaviors and to sanction people who are so stigmatized is a fundamental mechanism of informal social control in all societies (Giddens, Citation1984; Goffman, Citation1963). Socially defined stigmas are applied through a process that begins when a difference is labeled, then linked to negative stereotypes, leading to a separation of “us” from “them,” and finally to status loss and discrimination for those carrying the trait (Link & Phelan, Citation2001). Stigmas persist because they are reinforced and replicated by a range of interlocking social norms and institutions. Organizational and national policies reflect social values and norms. They may replicate and reinforce social stigma against certain behaviors or groups actively (e.g., through criminalization, or disqualification from services), or passively (e.g., through neglect and lack of investment), according to structural factors ranging from economic and geographic distinctions to differences in ethnicity, occupation, or sexual orientation. Thus, stigma and discrimination can be profoundly political (Parker & Aggleton, Citation2003).
How Does Stigma Affect Infant Mortality and Child Development?
To interrupt the stigmatization process, it is important to understand the different domains of stigma that can be shifted, halted, or reduced through programmatic or structural interventions. A recent global effort to develop standardized indicators of HIV stigma and discrimination led to the development a practical framework that offers an informative model for thinking about how the stigmatization of diseases and marginalized groups may be influencing child health and well-being (see Figure ).
Figure 1 A framework for reducing the stigma and discrimination that influence child health, adapted from the HIV field (Stangl, Go, et al., Citation2010).
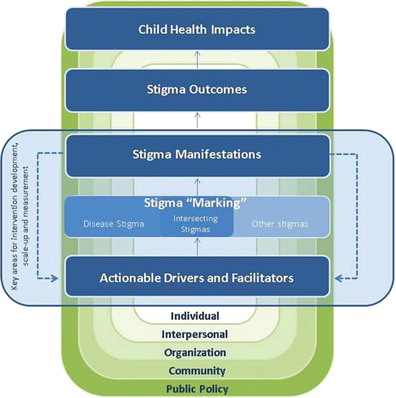
The HIV stigma reduction framework highlights six domains that together constitute the stigmatization process, including drivers, facilitators, intersecting stigmas, manifestations of stigma, outcomes of stigma, and impacts of stigma (Stangl, Go, et al., Citation2010; Stangl, Lloyd, Brady, Holland, & Baral, 2013). Drivers—such as fear of infection, lack of awareness of stigma, and prejudice and stereotypes—negatively influence the stigmatization process at the individual level (Hong, Van Anh, & Ogden, Citation2004; Nyblade et al., Citation2003; Ogden & Nyblade, Citation2005; Mahendra, et al., Citation2007). Facilitators—such as gender and cultural norms, availability of social support services, and protective or punitive laws—influence the stigmatization process either positively or negatively at the societal level (Stangl, Go, et al., Citation2010). Together, drivers and facilitators influence whether a stigma is applied to individuals or groups. Of particular relevance to the child health field are intersecting, or multiple, stigmas that people often face as a result of HIV status, profession, gender, migration, poverty, drug use, marital status, and race (Logie, James, Tharao, & Loutfy, Citation2013; Loutfy et al., Citation2012; Nyblade, Citation2006; Reidpath & Chan, Citation2005).
When a stigma is applied to individuals or groups, a number of immediate, negative manifestations may result, including anticipated stigma—the fear of experiencing humiliating or degrading treatment (Quinn & Chaudoir, Citation2009); perceived stigma—an individual's experience of the negative meanings associated with a stigma (Zelaya et al., Citation2012), internalized or self-stigma—negative self-sanction or judgements when people believe that stigmatizing public attitudes apply to themselves (Rao et al., Citation2012) and shame (Burris, Citation2008). The HIV-related stigma reduction framework distinguishes between experienced stigma and discrimination. Rather than viewing discrimination as the end result of the stigmatization process, experienced stigma and discrimination are considered manifestations of the stigmatization process. Resilience—an individual's ability to overcome threats to health and development after stigma is experienced (Earnshaw, Bogart, Dovidio, & Williams Citation2013)—is the only positive manifestation of stigma included in the HIV-related stigma reduction framework.
The manifestations of stigma can lead to a number of stigma outcomes, such as delayed treatment seeking or poor medication adherence, that ultimately lead to longer term stigma impacts, including poorer quality of life and increased morbidity and mortality. For children under 5 years of age, stigma and discrimination experienced by parents—for example, as a result of having a stigmatized disease such as HIV or belonging to a stigmatized group such as the scheduled caste in India—can impede access to or uptake of available health care services, leading to poor health outcomes for children.
There is a general consensus among stigma researchers that interventions should target multiple, socioecological levels (Stangl et al., Citation2013), as societal norms and structures influence individual attitudes and behaviors (AIDS 2031 Social Drivers Working Group, Citation2010; Parkhurst, Citation2012). Key levels at which stigma-reduction activities can be targeted include the following: the individual (knowledge, attitudes, skills), interpersonal (family, friends, social networks), organizational (organizations, social institutions, work place), community (cultural values, norms, attitudes), and public policy (national and local laws and policies) levels (Heijnders & van der Meij, Citation2006; McLeroy, Bibeau, Steckler, & Glanz, Citation1988; see Figure ).
While initially developed for the HIV field, we believe this framework can be applied more broadly in order to inform research and programmatic efforts seeking to reduce stigma and discrimination and improve child health outcomes.
Method
This review grew out of the U.S. Government's Evidence Summit on Enhancing Child Survival and Development in Lower- and Middle-Income Countries by Achieving Population-Level Behavior Change organized and supported by the U.S. Agency for International Development (USAID) and the United Nations Children's Fund (UNICEF). The background and rationale for the Evidence Summit is described in another article in this issue (Fox & Obregón Citation2014). The method used to obtain initial documents is also described in detail in another article in this issue (Balster, Levy, & Stammer, Citation2014). Briefly, two strategies were used: (a) an initial literature review conducted by USAID, and (b) a call for evidence issued to members of the evidence review teams.
USAID commissioned a literature review by Knowledge Management Services (Washington, DC) to identify peer-reviewed studies of interventions to achieve behavior change, health, or developmental outcomes related to maternal and child health. The initial literature search and screening process yielded 750 documents (Balster et al., Citation2014). Working group members were given the opportunity to conduct their own relevance reviews of the documents obtained through the literature search. The stigma and discrimination evidence review team (ERT) reviewed the bibliography and determined that none of the articles evaluated stigma or discrimination reduction interventions; however, there were a few articles with limited relevance to stigma and discrimination.
To supplement this initial literature search, a call for evidence (from peer-reviewed and gray literature) was issued to ERT members to expand the range of materials available for preparing their evidence syntheses. The stigma and discrimination ERT relied on their own resources and the additional studies identified through this call for evidence process. The group worked with Knowledge Management Services to broaden the search to include terms such as marginalization, exclusion, shame, blame, and humiliation. As the bulk of research on stigma reduction in the realm of global health has focused on HIV and AIDS, many of the articles identified were related to HIV-related stigma and discrimination reduction. We aimed to identify intervention studies or high-quality evaluations targeting maternal and child health outcomes. Given that few stigma-reduction interventions have been developed to specifically improve child health outcomes, and none have been rigorously evaluated to date, we broadened our review to include stigma reduction intervention studies with any target population. With these refined search criteria, a number of relevant articles from the prevention of mother-to-child (PMTCT) literature emerged.
For the purposes of this review, we also searched for literature exploring the relationship between marginalized populations, disease, prevention and treatment. Populations experience stigma and discrimination as a result of attributes such as color, caste, ethnicity/language, religion, sexual preferences or practices, drug use, and poverty. Marginalized populations are more vulnerable to many diseases as a result of factors such as limited access to education and employment, living in riskier places, having lower access to preventive and curative measures (Castro & Farmer, Citation2005; Gill et al., Citation2013), fewer skills and knowledge, and lower self-efficacy. Some diseases and health conditions to which marginalized populations are more vulnerable are stigmatized (e.g., HIV and AIDS) by virtue of their association with stigmatizing attributes, such as poverty, or involvement in a stigmatized occupation, such as sex work. However, some diseases and conditions prevalent among marginalized populations, such as malnutrition, diarrheal disease, acute respiratory infection, and malaria, do not evoke shame or elicit discrimination.
Findings
The findings are divided into five sections: (a) HIV-related stigma in the context of PMTCT; (b) neonatal survival, and health; (c) healthy early childhood development; (d) nutrition; and (e) marginalized groups; and child survival. It is important to note that interventions directly addressing stigma and discrimination were identified for HIV and not for any of the other listed health conditions.
HIV-Related Stigma in the Context of PMTCT
In the context of HIV, stigma, discrimination, and inequality contribute to negative health outcomes for children and their parents, and disproportionally affect poor or marginalized groups (Castro & Farmer, Citation2005). Limited access to and uptake of services for PMTCT as a result of the fear of or the experience of stigma and discrimination is a prominent example of how child survival can be influenced by stigma.
PMTCT requires the successful uptake and adherence to several constituent steps, often referred to as the PMTCT cascade. These steps include: early HIV diagnosis during pregnancy, women's acceptance of CD4 testing, prompt uptake of either short-term antiretroviral prophylaxis or life-long antiretroviral treatment (depending on CD4 cell count), high adherence to maternal and infant drug regimens, adherence to infant feeding guidelines and early infant diagnosis (World Health Organization, 2012). For women and children to receive the most benefit from PMTCT services, consistent engagement in maternal care and reliable medication adherence are required. Yet, PMTCT programs globally are experiencing challenges in achieving the levels of engagement and adherence needed (Coetzee, Stringer, & Chi, Citation2009). Given that treatment of women with CD4+ cell counts of <350 cells/µl will prevent at least 75% of infant transmissions, as well as most maternal deaths (Kuhn & Coovadia, Citation2012), medication adherence among HIV-positive women during and following pregnancy is critical.
A growing body of literature indicates that each of the linked processes in the PMTCT cascade may be negatively influenced by the stigma that HIV-positive pregnant women face in the health care setting, as well as in their families and communities. Recent research indicates that HIV-related stigma and discrimination affect pregnant women's decisions to enroll in PMTCT programs (Ekouevi et al., Citation2004; Painter et al., Citation2005) and impedes their retention and adherence in these services (Awiti Ujiji et al., Citation2011; Bwirire et al., Citation2008; Duff, Kipp, Wild, Rubaale, & Okech-Ojony, Citation2010; Mepham, Zondi, Mbuyazi, Mkhwanazi, & Newell, Citation2011; Turan et al., Citation2011). It has been estimated that more than half of vertical transmissions in some settings can be attributed to the cumulative effect of stigma at each point in the PMTCT cascade of services (Watts, Zimmerman, Eckhaus, & Nyblade, 2011).
We could find no published studies that evaluated stigma-reduction interventions for pregnant women living with HIV or the direct impact of HIV-related stigma on the uptake of PMTCT services. However, a growing body of literature suggests that interventions to reduce negative attitudes toward people living with HIV (PLHIV) among community members, and anticipated and internalized stigma among HIV-infected pregnant women, may together improve HIV-related care outcomes for this population. Evidence shows that interventions using a combination of sensitization and participatory activities can reduce stigma in health care and community settings (Apinundecha, Laohasiriwong, Cameron, & Lim, Citation2007; Nyblade et al., Citation2008; Oanh, Ashburn, Pulerwitz, Ogden, & Nyblade, Citation2008), but few PMTCT programs have systematically applied these strategies, and no rigorous research has been conducted to measure the impact of these program enhancements on key PMTCT outcomes, including infant seroconversion and postpartum child survival.
There are, however, promising practices to draw upon. Intervention strategies designed to reduce HIV-related stigma and discrimination used in other settings, such as with the general community or within health care settings, could be applied to the PMTCT context. Emerging evidence reveals several key programmatic principals for successful stigma-reduction programs. Successful interventions involve a combination of strategies and approaches, engage a broad range of stakeholders, address intersecting stigmas, and are led by or actively engage communities experiencing stigma (Mahajan et al., Citation2008; Parker & Aggleton, Citation2003; Stangl, Carr, et al., Citation2010). Recent reviews have categorized stigma reduction interventions into four types, including (a) information-based approaches, (b) skills building, (c) counselling/support, and (d) contact with affected groups. These broad categories encompass a range of different intervention activities, such as training sessions, participatory learning, support groups, holding community meetings, using cultural mediums and media channels, and providing written materials with specific information of local relevance (Brown, Macintyre, & Trujillo, Citation2003; Stangl et al., Citation2013). Evaluation data from stigma reduction interventions show that the more activities a respondent reports exposure to, the larger the increase in awareness of stigma, and decrease in fear and social judgment (Nyblade et al., Citation2008). Multiple activities not only reinforce messages, but provide ongoing opportunities to engage on the issue, learn, and begin to change attitudes and behaviors. In addition, different activities reach and appeal to different segments of the community.
Promising interventions piloted in a wide range of contexts have demonstrated that another key element to successful stigma reduction programs is the involvement of gatekeepers and multiple change agents, such as local government leaders, teachers, police, media, and health care providers (Apinundecha et al., Citation2007; Boulay, Tweedie, & Fiagbey, Citation2008; Young et al., Citation2011). Building commitment to and ownership of the stigma reduction process among community leaders is crucial for obtaining buy-in from the larger community. To cultivate community leaders as champions for stigma reduction, it is important to build their knowledge of HIV, AIDS and stigma; provide opportunities for them to address their own fears, misconceptions, and attitudes; and build their capacity to reduce stigma. These leaders help raise awareness and reduce fear within the community, facilitating a shift in community norms (Nyblade et al., Citation2008; Stangl, Carr, et al., Citation2010). Shifting community norms is likely to inspire more lasting population-level improvement in community attitudes and create an enabling environment for PLHIV to engage in health care and social support systems. As evidence of this, Boulay and colleagues (Citation2008) found that individuals living in communities with more positive attitudes toward PLHIV had significantly better attitudes toward PLHIV than people living in communities with less favourable attitudes.
Research has shown that it is also important to address intersecting stigmas. Stigma and discrimination are particularly harsh for populations that are already socially excluded or have unequal status in society. These groups often experience stigma and discrimination on the basis of intersecting stigmas related to gender, sexuality, ethnicity, and so forth (Logie et al., Citation2013; Loutfy et al., Citation2012; Nyblade et al., Citation2006; Reidpath & Chan, Citation2005). In the context of PMTCT, it is particularly important to address intersecting stigma related to gender. Women and children, for example, are more prone than men to property grabbing, abandonment, and violence as a result of their HIV status (Swaminathan, Walker, & Rugadya, Citation2008).
Last, evidence gathered from community-led interventions highlights the critical role that supportive networks play in helping strengthen capacity of marginalized communities to reduce stigma and discrimination. Involving marginalized communities is essential for strengthening capacity, ensuring appropriate messaging, and maximizing results (Stangl, Carr, et al., Citation2010). Additionally, addressing self-stigma effectively is an important precondition for effective engagement of marginalized communities (Rao et al., Citation2012).
Neonatal Survival and Infant Health
A lack of preventative practices in pregnancy such as iron intake, complications during pregnancy, delivery with unskilled attendants, and a lack of postnatal care all contribute to high rates of neonatal mortality, as well as to the number of children born with disabilities that can threaten their ability to thrive. Risk factors for neonatal death and disability are particularly evident among disadvantaged women living in poor-resource communities (D'Ambruoso, Citation2012). Reducing the risk for death and poor health outcomes during infancy requires that care providers, particularly mothers, receive quality care at the prenatal, birth and postnatal stages (Bhutta, Darmstadt, Haws, Yakoob, & Lawn, 2005).
Barros and colleagues (2012) reported that effective and low-cost interventions that increase the likelihood of neonatal survival and health do exist. Such interventions include promoting early initiation of breastfeeding, treating infections early with antibiotics, and training community-based health workers who oversee births to implement basic resuscitation strategies (Barros et al., Citation2012). However, such interventions are not frequently used. There are many barriers that interfere with access to care, and some of the most significant are associated with stigma and discrimination (Darak et al., Citation2012). Manifestations including perceived stigma and the experience of discrimination in health facilities are particularly pernicious barriers to care for HIV-positive women (Rahangdale et al., Citation2010; Turan et al., Citation2011).
The evidence for effective and sustainable interventions to address stigma and discrimination is moderate to weak. There is a paucity of research examining the effectiveness of programs that implement the aforementioned low-cost interventions to promote neonatal survival and health among poor and marginalized groups, particularly in developing countries (Schiffman, Darmstadt, Agarwal, & Baqui, Citation2010). Studies of interventions that specifically target stigma and discrimination as a means to improve neonatal survival and health are nearly nonexistent, except in the PMTCT literature, where interventions have focused on eliminating barriers to care among pregnant women living with HIV. The PMTCT literature demonstrates that maternal health and newborn outcomes are inextricably linked (Futterman et al., Citation2010; Turan et al., Citation2011). As such, addressing stigma and discrimination at all stages leading up to the newborn's entry into the world, during delivery and shortly after birth are critical to ensuring survival and good health outcomes among neonates.
The limited evidence on stigma and discrimination reduction efforts that impact neonatal survival and health suggest that the provision of information in community settings is an important mechanism to increase knowledge among groups that typically underuse available services. For example, Kumar and colleagues (Citation2012) reported results of a cluster randomized controlled trial to assess the impact of a newborn-focused behavioral intervention on maternal health in rural communities in India. Results suggest that the provision of information targeting marginalized communities promoting birth and emergency preparedness and care seeking from trained providers improves equity in care provision across different religious and caste categories. Improvements were noted in maternal knowledge, behaviors (e.g., care seeking), and birth outcomes.
A reduction in stigma can also be achieved through interventions that attend to where and how information is provided. For example, capitalizing on social support structures appears to facilitate the acquisition of important information relevant for neonatal survival and health among women from disadvantaged backgrounds. There is some evidence from studies of disadvantaged groups in high-income countries that social support plays an important role in behavioral change in mothers. For example, the provision of social support during prenatal visits among Mexican immigrants in the United States increased the likelihood that participants in the intervention group would come in for a postpartum appointment (McGlade, Saha, & Dahlstrom, Citation2004). Similarly, the provision of information to fathers in the United Kingdom regarding maternal care in some communities improved the chances of a safe delivery and implementation of good postbirth practices (Burgess, 2006).
Attending to service location is a widely advocated approach to improving access to care among disadvantaged groups that is centered around eliminating economic barriers. Service location can act as a facilitator in efforts to reduce stigma and discrimination at the structural level. For example, research assessing the impact of PMTCT interventions suggests that location of services is important. Women living with HIV may be reluctant to access services for fear of experiencing stigma and discrimination in contexts that are clearly associated with being HIV positive. In high-income nations, there is increasing support for providing mental health services in schools as a mechanism for facilitating access to care among groups that typically will not access mental health care because of stigma (Clauss-Ehlers, Serpell, & Weist, Citation2013). With respect to neonatal survival and health, there has been a lot of advocacy for integrated services to enable a one-shop stop model where multiple services are accessed in a single location—all of which could contribute to improved maternal and neonatal outcomes.
There is also some evidence that interventions designed to reduce discriminatory practices among health care providers are key to reducing neonatal health and survival. Discrimination against pregnant women living with HIV attempting to access care is widely acknowledged in nations across the economic spectrum. A qualitative study of HIV-positive mothers attempting to access PMTCT care in India (Rahangdale et al., Citation2010) suggests that women living with HIV perceive discrimination at multiple levels, including at the institutional level as well as in their interpersonal interactions with health workers. Turan, Miller, Bukusi, Sande, and Cohen (Citation2008) reported findings from a qualitative study in a Kenyan community with a high rate of HIV infection and low rate of childbirth in a health setting. They concluded that sensitivity training, and increasing knowledge and access to postexposure prophylaxis among health workers, may reduce health care workers' unwillingness to attend births of women who are living with or are suspected to be living with HIV as well as improve the quality of the care they provide. An important implication of this work is that PMTCT interventions should include efforts to reduce stigma at multiple socioecological levels, including the institutional and interpersonal levels, as a mechanism to promote the retention of HIV-positive women in programs that are key to ensuring neonatal survival and health.
Healthy Early Childhood Development
It is well documented that children's developmental outcomes are influenced both by biological and environmental factors. For example, poverty, family stress, caregiver health and mental health status, and exposure to violence have all been documented to have a deleterious impact on child development (Barbarin & Richter, Citation1999, Citation2001; Barbarin, Richter, & deWet, Citation2001; Gottlieb & Blair, Citation2004; Noble, Norman, & Farah, Citation2005). The consequences of many of these risks to child developmental outcomes are stigma and marginalization.
Stigma and discrimination reduction interventions likely to result in improved developmental outcomes in children provide families with appropriate skills (e.g., parenting skills); empower them with knowledge that helps them overcome personal and systemic barriers; and facilitate access to resources necessary for providing safe and health-promoting home environments for children. Few studies examine specific strategies to overcome discrimination and stigma that directly affect children's developmental outcomes, and the studies that do tend not to be empirically strong. However, nearly all efforts to adapt interventions to local contexts, specific cultural groups or family types entail some consideration of issues related to stigma and discrimination. Furthermore, there is moderate evidence that there are interventions targeting HIV stigma that yield positive attitudinal shifts and increased knowledge in families, care providers, and communities (Sengupta, Banks, Jonas, Miles, & Smith, 2011; Stangl et al., Citation2013), and such changes can serve as the basis for behavioral changes that facilitate children's physical, cognitive, and social growth.
As discussed earlier, the socioecological perspective suggests that stigma and discrimination reduction interventions can operate at the individual, interpersonal, and broader structural levels of the institution, community, and/or country. In their comprehensive review of literature on parenting, Richter and Naicker (Citation2013) explained how interventions that are based in human rights and protection from discrimination can be important structural approaches that affect parenting. That is, parents find it very difficult to fulfill their parenting roles in countries where human rights abuses and discrimination are tolerated. These authors drew from studies that describe parents who experience discrimination in their communities as a result of color, caste, ethnicity, language, religion, sexual preference, sexual practice, and drug use (see Beard et al., Citation2010; Rekart, Citation2006; Rhodes, Bernays, & Houmoller, Citation2010) and state that supportive interventions include self-help and solidarity, education and empowerment, care, decriminalization and legal representation, safety and protection, and community-based child protection networks.
Community-based interventions often address discrimination and improve equity by increasing service provision to underserved or marginalized groups. There are a few randomized control studies of community-level interventions for which stigma and discrimination reduction is a secondary outcomes but not the direct target of intervention activities. For example, in a randomized controlled trial in rural India, Pandey, Sehgal, Riboud, Levine, and Goyal (Citation2007) demonstrated that the provision of information to community members about their entitlement to child-related services increased service delivery to potentially stigmatized groups (low caste) and may therefore have inadvertently reduced discrimination. Similarly in another trial in India, the provision of information promoting birth and emergency preparedness, and care-seeking from trained providers improved maternal knowledge and care seeking regardless of religious and caste categories (Kumar et al., Citation2012). As such, these interventions improved the capacity of families likely to experience stigma and discrimination to access care for their children and thereby improve child health and developmental outcomes.
There is some evidence on interventions that build good parenting skills to reduce stigma and discrimination in low-income countries. The majority of evidence on parenting interventions is drawn from high-income countries, specifically Europe and North America. However, evidence from both low- and high-income countries demonstrates how poverty can significantly endanger the well-being of children and families (Yoshikawa, Aber, & Beardslee, Citation2012). For example, Abosede, Campbell, Okechukwu, Salako-Akande, and Onyenwenyi (Citation2010) found that poverty makes it difficult for disadvantaged parents in Nigeria to pay the high fees charged by child development centers. Such early education centers have the promise for improving healthy child development through intensive stimulation and learning, and provide opportunities for poor mothers to gain income by working outside the home. These authors found that providing community support for free early education increased the likelihood that mothers would enroll their under-5 children in the education program, and also increased their participation in income-generating work.
At the individual level, maternal health and emotional status are known to affect infant functioning. Maternal depression is strongly associated with many risk factors that may be stigmatized, and depression itself is a stigmatized mental health condition. The impact of maternal depression may be particularly powerful during the early years of life, given that this is a time when young children are more dependent on nurturing, stimulation, and support from primary caregivers. Concomitant stigma associated with maternal risk factors for depression may exacerbate the impact of maternal depression on child outcomes. Tripathy and colleagues (Citation2010) examined the role of participatory intervention with groups of women as a mechanism for reducing maternal depression in a rural population in three districts in eastern India. In this randomized clinical trial, women were assigned to either a control group or an intervention group where education about maternal and infant health was provided. Maternal outcomes including depression were monitored for both groups. A large and sustained reduction in maternal depression was observed in the intervention group. The authors suggested that social support for women in the intervention group resulted in reduced risk of depression and increased problem-solving skills. While the intervention did not directly seek to reduce stigma, empowering women to become more active participants in their health care may reduce barriers to care including the potential for experiencing stigma and discrimination.
A few studies were identified that suggest a benefit to child health and development from parent disclosure of HIV status to their children. Blasini and colleagues (Citation2004) developed a model to address many of the barriers to open communication about pediatric HIV. The investigators found that their model promoted healthy psychological adjustment and better adherence in children living with HIV. Nostlinger and colleagues (2004) noted that disclosure of HIV status by parents to their children may promote improved developmental outcomes for children by reducing stigma. That is, dispelling misconceptions about the disease and fostering an openness that can help ameliorate the potential impact of stigma on children's developmental outcomes after their parents have died.
Nutrition
Stigma and discrimination experienced by caregivers or parents (especially mothers), can negatively affect children's access to resources related to health and nutrition. Our review noted the absence of interventions directly or indirectly addressing stigma in the domain of nutrition. We did not identify any studies that specifically addressed the stigmas around childhood nutrition, although we did find intervention on stigmas around food insecurity more broadly (Dutta, Citation2012). Some studies tangentially reported the broader social and cultural contexts around childhood nutrition (Khatun, Stelund, & Hornell, Citation2004). In other studies, context was addressed in the form of gender inequality (Ghosh, Kilaru, & Ganapathy, Citation2002; Khatun et al., Citation2004) and marginalization of women in society.
Dutta, Anaele, and Jones (Citation2013) reported an intervention in the United States that directly addressed the stigma around food insecurity, documenting qualitative indicators such as greater access to food pantries and the quality of food available at food pantries that appeared to be beneficial to food insecure populations. Study authors suggested that the absence of advocates and broader participation from the food insecure community in work to reduce food insecurity was both a marker of and a result of the stigma associated with food insecurity (Dutta, Citation2012). The relationship of nutrition to the broader sociocultural and economic context is also documented in some literature. For example, Alderman, Hoogeveen, and Rossi (Citation2006) analyzed data from a panel of children in Tanzania to document that malnourished children had less education and delayed entry into school.. The authors also suggested the impact of malnutrition on the lack of economic opportunity. Similarly, in a report of Jamaican studies in nutrition and child development, Grantham-McGregor and Cumper (Citation1992) noted the association between malnutrition and school achievement. There is a need for systematically documenting the relationship of malnutrition to the broader social, cultural, and economic outcomes. This is important in understanding the cycles of disenfranchisement and marginalization that are connected to childhood malnutrition. This is also important in understanding how stigmatization plays out in cycles of poverty and structural barriers to food access, manifested in early childhood in a variety of experiences, including malnutrition, with consequences for the rest of the life cycle.
Marginalized Groups and Child Survival
Marginalization is the process of discrimination and exclusion of stigmatized groups, and falls under the umbrella of manifestations in the stigma reduction framework (Figure ). Marginalized groups have decreased access to health services. They have limited resources and consequent high relative risk for morbidity and premature mortality (Flaskerud et al., Citation1998). In turn, children of parents belonging to marginalized groups have decreased access to health services and increased morbidity and mortality. As a consequence, unhealthy birth spacing, diarrheal diseases and pneumonia disproportionately affect poor and marginalized groups. In many developing countries, the poor and the marginalized are often uninformed of the mortality and morbidity risks associated with short childbearing intervals. They may understand generally that spacing pregnancies is a healthy behavior, but most do not know that mortality, morbidity, and poor nutritional status are often associated with short birth intervals, and are preventable. In addition, some women may not know that they can control the pace of births, and may be unaware of the various options to achieve longer childbearing intervals, including breastfeeding, modern contraceptive methods, abstinence, and natural family planning (Norton, Citation2005).
Diarrhea and acute respiratory infections are other examples of health issues that disproportionately affect poor and marginalized groups. Millions of children die unnecessarily from pneumonia and diarrhea, and mortality from these illnesses is increasingly concentrated in resource-poor settings (Walker et al., Citation2013). Many interventions to prevent diarrhea and pneumonia exist within present health systems, but their coverage and availability to poor and marginalized populations varies greatly (Gill et al., Citation2013).
Access to health services is a human right, and a pillar of human rights principles is non-discrimination. Human rights principles dictate the necessity to strive for equal opportunity for health for children and parents who suffer marginalization or discrimination. Braveman and Gruskin (Citation2003) suggested that governance and health institutions deal with marginalization, poverty and health within a framework encompassing equity and human rights concerns by implementing equitable health care financing (which should help reduce poverty while increasing access to health services for the poor, including children living in poverty); ensuring that health services respond effectively to the major causes of preventable ill-health among poor and disadvantaged children and adults; and taking action to address the potential health equity and human rights implications of policies in all sectors affecting health (Braveman & Gruskin, Citation2003).
Three Millennium Development Goals deal with combatting extreme poverty and improving children's life chances through access to education and health information and services. In 2012, countries committed to implement a social protection floor that would guarantee that their populations have access to a basic package of health, education and income benefits (ECA, ILO, UNCTAD, UNDESA, & UNICEF, Citation2012). If implemented equitably and inclusively, such high level policy interventions could overcome discrimination and exclusion of stigmatized groups, and create an enabling environment for behaviors which improve child health and development.
Discussion
Despite broad consensus on the importance of stigma and discrimination as potential barriers to access and uptake of health information and services, this review found surprisingly little empirical research on interventions that directly aimed to reduce stigma and discrimination to improve child health outcomes in low- and middle-income countries. This is partly a matter of semantics. There is a wealth of research demonstrating that poverty and social exclusion impede adult access to health information and services, as well as to the education and skills relevant to family planning, child rearing, nutrition, health promotion, disease prevention, and uptake of health care. However, there is a failure to connect such exclusion and disadvantage to the social and political distinctions, prejudices, stereotypes and “shame and blame” that are the heart of stigma research. There is a small but growing body of research that demonstrates that a number of intervention strategies can reduce stigma and discrimination and increase inclusiveness in allocation of social services. These include information, education and communication, skills building, community mobilization and mutual support, and strategic advocacy for equity, participation, and human rights.
The bulk of research directly on stigma and global health has focused on HIV and AIDS. There has been a significant increase in quantitative as well as qualitative research on interventions to combat stigma and discrimination in that area, but little of it connects stigma with child health directly. The two topics where this has been explored directly are: orphans and vulnerable children, and prevention of mother to child transmission of HIV. In these areas there is weak to moderate evidence of the effectiveness of interventions to reduce stigma on a range of outcomes.
An extensive range of tools and models now exist for identifying and measuring HIV-related stigma in specific communities and institutions, such as health care facilities (Stangl et al., Citation2013) and for designing, evaluating and reporting on interventions to combat three interlocking sources of stigma: lack of awareness of stigma's hurtful effects, misinformation about HIV transmission, and social judgment about people and behaviors associated with HIV and AIDS. These models could be adapted to address stigma and discrimination affecting marginalized populations more broadly (Stangl et al., Citation2013).
The paucity of strong evidence on how to intervene to reduce stigma and discrimination is the result of several factors: anti-stigma interventions are often poorly described; interventions addressing stigma are usually part of a larger package, so that parsing out the effect of the antistigma element is difficult; and there is a lack of standardization in definitions and measurement of stigma and discrimination, which impedes meta-analysis and learning from program experience. Furthermore, while the causal chain linking structural and individual factors to stigma marking, stigma manifestations, and finally to negative health outcomes is increasingly clear, that causal chain is long and complex, and few studies endeavour to tackle its entirety. It can be argued that to achieve population-level changes that support child health interventions, the social and political factors that shape public health and social welfare policies may be our most important target. Structural interventions to reduce stigma and discrimination call attention to underlying power structures and ideologies that enable the stigmatization process. Examining and shifting harmful social and political conditions, such as gender inequality or racism, may engender more lasting and widespread change (Aggleton et al., 2003; Link et al., Citation2001). Yet, stigma and discrimination tend to be studied largely in small-scale projects, and structural factors such as policies and laws are rarely included in studies of stigma mitigation interventions (Sengupta et al., Citation2011; Stangl et al., Citation2013).
Findings from research in multiple countries and contexts have shown that HIV-related stigma—which involves social judgments about gender, poverty and risk-taking, as well as about HIV per se—is much less varied and context-specific than one may think (Ogden et al., Citation2005). There are more similarities than differences across contexts in the key causes of stigma associated with HIV, tuberculosis, poverty, and marginalized groups, as well as in the forms stigma takes, and the consequences of stigma in all of these cases. Thus, while the thematic content must be grounded in specific problems and places, promising practices and intervention strategies designed to reduce stigma could, in many cases, be applied across contexts and cultures.
Stigma is part of a larger picture of inequity as a result of marginalization. Results of the review suggest that addressing access and empowerment related to marginalization could improve child health outcomes in marginalized populations. For health and development programs to be rights-based and people-centered, they must be alert to, and prepared to combat, ignorance, fear and social judgment that lead to stigma and discrimination. This means that increased attention to stigma and discrimination is needed in all areas affecting child health. Concern and action on stigma and discrimination may have arisen in the global HIV movement, but the ethical concerns and the structure of stigma processes and responses are general, and should be assimilated into child health research and practice.
For this to happen efficiently, a consensus conceptual model of stigma and antistigma interventions, such as the one proposed in this paper, is needed to support a common language, as well as standardized measures of stigma levels and processes. Consensus around a practical framework of the stigmatization process would allow researchers and practitioners to (a) articulate the pathway connecting structural and individual causes and effects; (b) support identification of standard, core measures of stigma drivers, facilitators and manifestations, including anticipated, perceived, internalized and experienced stigma, discrimination, and resilience; (c) address all program areas influenced by stigma and discrimination that are relevant to child health, including nutrition, healthy early childhood development, immunizable diseases and HIV and AIDS; (d) explicitly include interventions that affect children by reducing consequences of stigma for their parents; (e) explicitly include interventions addressing pathways through which stigma influences outcomes, such as disclosure, adherence, access and empowerment; (f) include red flags and guidance regarding ethical issues and ways to avert stigma as a negative unintended consequence of interventions; and (g) be developed with full participation of affected community members.
Increased investment in stigma and discrimination reduction interventions and program evaluations is also needed to overcome the evidence gap regarding stigma and discrimination reduction interventions. Program implementers should prioritize regular inclusion of measures that assess stigma and discrimination in evaluations of all interventions targeting neonatal and child health and healthy early childhood development, including interventions addressing integrated care of mother and child. The field would also benefit from improved, more detailed reporting about the content of community engagement, communication and counseling inputs in randomized controlled trials of interventions to facilitate replication of successful strategies. For example, creating a standard such as the CONSORT statement (http://www.consort-statement.org) would be very beneficial to the field. In addition, to improve reporting about randomized controlled trials, alternative or new evaluation methodologies should be more widely considered in child health studies that seek to address social determinants and structural interventions. Use of qualitative evaluation methods grounded in systems thinking and complexity science, and quantitative analysis using propensity scores, causal inference and structural equation modeling (Seeley et al., 2012) have untapped potential for bridging qualitative and quantitative analysis of complex social, political, economic and biomedical factors that influence child health. Last, research to document the relational and sociocultural contexts of stigma surrounding interventions to improve child health should be expanded. Beyond the documentation of the effects numerically, there is a need for more qualitative, in-depth data that offer contextual information as well as richer insights into the structural aspects of stigma surrounding child health and development.
Limitations
There are several limitations to the approach used here. The primary one being that this paper is not an attempt at a systematic review of current literature on stigma and discrimination; rather it is focused on examining the direct and indirect influences of interventions related to stigma and discrimination on the health of children. Most of the studies reviewed provided minimal information about the interventions assessed, which made it difficult to ascertain whether and how directly intervention activities interrupted or reversed the stigmatization process. In addition, the complex nature of stigma and discrimination requires multifaceted interventions that target multiple stigma domains and socioecological levels (Stangl et al., Citation2013; Khumalo-Sakutukwa et al., Citation2008), which makes it difficult to discern the discrete elements that might have affected stigma. We did not consider interventions that might inadvertently stigmatize. For example, interventions that focus on children orphaned by parental death from HIV may intend to provide care and support services to orphans, but may inadvertently stigmatize the children by identifying them as AIDS orphans in their communities. We also did not include interventions that sought to reduce stigma directly experienced by children under 5 years of age, such as interventions to reduce stigma toward disabled children or children with mental health issues. Lastly, interventions that did not directly or indirectly seek to reduce stigma and discrimination, such as disease awareness campaigns and biomedical prevention approaches (e.g., treatment as prevention for HIV), were excluded from this review. Despite these limitations, our review is one of the first to explore stigma and discrimination reduction interventions that could improve child health and well-being and to propose a framework for future research and programmatic efforts in this area.
Conclusions
Stigma and discrimination, social exclusion and their impact on children should not be viewed in isolation, as they interact in every level of society. In every society, the disadvantages of stigmatized groups are experienced in varied forms by their children, who sometimes are trapped by them into intergenerational cycles of poverty and marginalization. Like societies, national policies are programs can be rated in terms of how they treat the least powerful and most marginalized members of their intended audience.
Moving forward, it is critical for the research community and policy planners to (a) evaluate the success of interventions that proactively include marginalized groups and respect their knowledge and dignity; (b) use the presence of stigma and discrimination, including differential neglect and exclusion, as indicators of quality in child health intervention programs; (c) explore and expand upon the domains of stigma that have been defined from the HIV field, to inform programming and research on stigma and social exclusion in an array of child health outcomes; and (d) deal head on with the phenomena of stigma and discrimination as a significant barrier to a child's heath. It is critical that stigma and discrimination not be relegated to the background as a result of perceived complexities of this ubiquitous social process.
Acknowledgments
This article would not have been completed without the expertise, knowledge, and, above all, immense support of the following evidence review team members: Susan Zimicki, FHI 360; Kim Seifert-Ahanda, USAID; Mohan J. Dutta, National University of Singapore; Katherine Fritz, International Center for Research on Women; Zewelanji N. Serpell, Virginia Commonwealth University; Lorraine Sherr, University College London; Janet Shriberg, USAID; and Vicki Tepper, University of Maryland. The authors extend thanks to Benjamin Isquith and Elizabeth Anderson at USAID for their administrative assistance to the team. The authors also thank their colleagues who initiated this project and supported it in every way: Elizabeth Fox, USAID; Rafael Obregón, UNICEF; Robert L. Balster, Virginia Commonwealth University; and Stephanie Levy, USAID.
Notes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/uhcm.
References
- Abosede , O. A. , Campbell , P. C. , Okechukwu , E. I. , Salako-Akande , A. O. , & Onyenwenyi , A. O. ( 2010 ). Sustainable poverty amelioration through early life education in a peri-urban community of Lagos, Nigeria . African Journal of Primary Health Care & Family Medicine , 2 ( 1 ), 80 – 89 .
- AIDS 2031 Social Drivers Working Group . ( 2010 ). Revolutionizing the AIDS response: Building AIDS resilient communities . Clark University and International Center for Research on Women . Retrieved from http://www.aids2031.org/pdfs/social%20drivers%20report%201st%20pg_merged.pdf
- Alderman , H. , Hoogeveen , H. , & Rossi , M. ( 2006 ). Reducing child malnutrition in Tanzania. Combined effects of income growth and program interventions . Economics & Human Biology , 4 ( 1 ), 1 – 23 .
- Ali , A. , Hassiotis , A. , Strydom , A. , & King , M. ( 2012 ). Self stigma in people with intellectual disabilities and courtesy stigma in family carers: A systematic review . Research in Developmental Disabilities , 33 , 2122 – 2140 .
- Apinundecha , C. , Laohasiriwong , W. , Cameron , M. P. , & Lim , S. (2007). A community participation intervention to reduce HIV/AIDS stigma, Nakhon Ratchasima province, northeast Thailand. AIDS Care , 19, 1157–1165.
- Awiti Ujiji , O. , Ekström , A. M. , Ilako , F. , Indalo , D. , Wamalwa , D. , & Rubenson , B. ( 2011 ). Reasoning and deciding PMTCT-adherence during pregnancy among women living with HIV in Kenya . Culture, Health & Sexuality , 13 , 829 – 840 .
- Balster , R. L. , Levy , S. , & Stammer , E. ( 2014 ). Evidence acquisition and evaluation for evidence summit on population-level behavior change to enhance child survival and development in low- and middle-income countries . Journal of Health Communication , 19 ( Suppl 1 ), 10 – 24 .
- Barros , A. J. , Ronsmans , C. , Axelson , H. , Loaiza , E. , Bertoldi , A. D. , França , G. V. , … Victora , C. G. ( 2012 ). Equity in maternal, newborn, and child health interventions in Countdown to 2015: A retrospective review of survey data from 54 countries . The Lancet , 379 , 1225 – 1233 .
- Barbarin , O. A. , Richter , L. , & DeWet , T. ( 2001 ). Exposure to violence, coping resources, and psychological adjustment of South African children . American Journal of Orthopsychiatry , 71 , 16 – 25 .
- Barbarin , O. A. , & Richter , L. ( 1999 ). Adversity and psychosocial competence of South African children . American Journal of Orthopsychiatry , 69 , 319 – 327 .
- Barbarin , O. A. , & Richter , L. ( 2001 ). Economic status, community danger and psychological problems among South African children . Childhood , 8 , 115 – 133 .
- Beard , J. , Biemba , G. , Brooks , M. I. , Costello , J. , Ommerborn , M. , Bresnahan , M. , … Simon , J. L. ( 2010 ). Children of female sex workers and drug users: A review of vulnerability, resilience and family-centered models of care . Journal of the International AIDS Society , 13 ( Suppl 2 ), S6 .
- Bhutta , Z. A. , Darmstadt , G. L. , Hasan , B. S. , & Haws , R. A. ( 2005 ). Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence . Pediatrics , 115 ( Suppl 2 ), 519 – 617 .
- Blasini , I. , Chantry , C. , Cruz , C. , Ortiz , L. , Salabarria , I. , Scalley , N. , … Diaz , C. ( 2004 ). Disclosure model for pediatric patients living with HIV in Puerto Rico: Design, implementation, and evaluation . Journal of Developmental & Behavioral Pediatrics , 25 , 181 – 189 .
- Boulay , M. , Tweedie , I. , & Fiagbey , E. ( 2008 ). The effectiveness of a national communication campaign using religious leaders to reduce HIV-related stigma in Ghana . African Journal of AIDS Research , 7 , 133 – 141 .
- Boyes , M. E. , Mason , S. J. , & Cluver , L. D. ( 2013 ). Validation of a brief stigma-by-association scale for use with HIV/AIDS-affected youth in South Africa . AIDS Care , 25 , 215 – 222 .
- Braveman , P. , & Gruskin , S. ( 2003 ). Defining equity in health . Journal of Epidemiology and Community Health , 57 , 254 – 258 .
- Brown , L. , Macintyre , K. , & Trujillo , L. ( 2003 ). Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention , 15 , 49 – 69 .
- Burgess , A. ( 2007 ). The costs and benefits of active fatherhood: Evidence and insights to inform the development of policy and practice . Retrieved from http://www.men-care.org/data/Costs%20and%20Benefits.pdf
- Burris , S. ( 2008 ). Stigma, ethics and policy: A commentary on Bayer's “Stigma and the ethics of public health: Not can we but should we.” Social Science & Medicine , 67 , 473 – 475 .
- Bwirire , L. D. , Fitzgerald , M. , Zachariah , R. , Chikafa , V. , Massaquoi , M. , Moens , M. , … Schouten , E. J. ( 2008 ). Reasons for loss to follow-up among mothers registered in a prevention-of-mother-to-child transmission program in rural Malawi . Transactions of the Royal Society of Tropical Medicine and Hygiene , 102 , 1195 – 1200 .
- Castro , A. , & Farmer , P. ( 2005 ). Understanding and addressing AIDS-related stigma: From anthropological theory to clinical practice in Haiti . American Journal of Public Health , 95 , 53 – 59 .
- Clauss-Ehlers , C. S. , Serpell , Z. N. , & Weist , M. D. (Eds.). (2013). Handbook of culturally responsive school mental health: Advancing research, training, practice, and policy . New York , NY : Springer.
- Cluver , L. ( 2011 ). Children of the AIDS pandemic . Nature , 474 , 27 – 29 .
- Cluver , L. , Bowes , L. , & Gardner , F. ( 2010 ). Risk and protective factors for bullying victimization among AIDS-affected and vulnerable children in South Africa . Child Abuse & Neglect , 34 , 793 – 803 .
- Cluver , L. , & Gardner , F. ( 2007 ). Risk and protective factors for psychological well-being of children orphaned by AIDS in Cape Town: A qualitative study of children and caregivers' perspectives . AIDS Care , 19 , 318 – 325 .
- Cluver , L. , Gardner , F. , & Operario , D. ( 2008 ). Effects of stigma on the mental health of adolescents orphaned by AIDS . Journal of Adolescent Health , 42 , 410 – 417 .
- Cluver , L. , Orkin , M. , Boyes , M. E. , Sherr , L. , Makasi , D. , & Nikelo , J. ( 2013 ). Pathways from parental AIDS to child psychological, educational and sexual risk: Developing an empirically-based interactive theoretical model . Social Science & Medicine , 87 , 185 – 193 .
- Coetzee , D. , Stringer , E. , & Chi , B. H. ( 2009 , July 19–22 ). Evaluation of PMTCT coverage in four African countries: The PEARL study. Paper presented at the 5th IAS Conference on HIV Pathogenesis and Treatment, Cape Town, South Africa. Retrieved from http://www.ias2009.org
- Courtwright , A. , & Turner , A. N. ( 2010 ). Tuberculosis and stigmatization: Pathways and interventions . Public Health Reports , 125 ( Suppl 4 ), 34 – 42 .
- D'Ambruoso , L. ( 2012 ). Relating the construction and maintenance of maternal ill-health in rural Indonesia . Global Health Action , 5 . doi: 10.3402/gha.v5i0.17989
- Darak , S. , Panditrao , M. , Parchure , R. , Kulkarni , V. , Kulkarni , S. , & Janssen , F. ( 2012 ). Systematic review of public health research on prevention of mother-to-child transmission of HIV in India with focus on provision and utilization of cascade of PMTCT services . BMC Public Health , 12 ( 1 ), 320 .
- Duff , P. , Kipp , W. , Wild , T. C. , Rubaale , T. , & Okech-Ojony , J. ( 2010 ). Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda . Journal of the International AIDS Society , 13 ( 1 ), 37 .
- Dutta , M. J. ( 2012 ). Hunger as health: Culture-centered interrogations of alternative rationalities of health . Communication Monographs , 79 , 366 – 384 .
- Dutta , M. J. , Anaele , A. , & Jones , C. ( 2013 ). Voices of hunger: Addressing health disparities through the culture‐centered approach . Journal of Communication , 63 , 159 – 180 .
- Earnshaw , V. A. , Bogart , L. M. , Dovidio , J. F. , & Williams , D. R. ( 2013 ). Stigma and racial/ethnic HIV disparities: Moving toward resilience . American Psychologist , 68 , 225 – 236 .
- ECA , ILO , UNCTAD , UNDESA , & UNICEF . ( 2012 ). Social protection: A development priority in the post-2015 UN development agenda–thematic think piece. Economic Commission for Africa, International Labour Organization, UN Conference on Trade and Development, UN Department for Economic and Social Affairs, and UNICEF. Retrieved from http://www.un.org/millenniumgoals/pdf/Think%20Pieces/16_social_protection.pdf
- Ekouevi , D. K. , Leroy , V. , Viho , I. , Bequet , L. , Horo , A. , Rouet , F. , & Dabis , F. ( 2004 ). Acceptability and uptake of a package to prevent mother-to-child transmission using rapid HIV testing in Abidjan, Cote d'Ivoire . AIDS , 18 , 697 – 700 .
- Flaskerud , J. H. , & Winslow , B. J. ( 1998 ). Conceptualizing vulnerable populations health-related research . Nursing Research , 47 , 69 – 78 .
- Foster , G. , & Williamson , J. ( 2000 ). A review of current literature on the impact of HIV/AIDS on children in sub-Saharan Africa . AIDS , 14 , S275 – S284 .
- Fox , E. , & Obregón , R. ( 2014 ). Population-level behavior change to enchance child survival and development in low- and middle-income countries . Journal of Health Communication , 19 ( Suppl 1 ), 3 – 9 .
- Futterman , D. , Shea , J. , Besser , M. , Stafford , S. , Desmond , K. , Comulada , W. S. , & Greco , E. (2010). Mamekhaya: A pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care , 22, 1093–1100.
- Ghosh , S. , Kilaru , A. , & Ganapathy , S. ( 2002 ). Nutrition education and infant growth in rural Indian infants: Narrowing the gender gap? Journal of the Indian Medical Association , 100 , 483 – 490 .
- Giddens , A. ( 1984 ). The constitution of society: Introduction of the theory of structuration . Oakland : University of California Press .
- Gill , C. J. , Young , M. , Schroder , K. , Carvajal-Velez , L. , McNabb , M. , Aboubaker , S. , … Bhutta , Z. A. ( 2013 ). Bottlenecks, barriers, and solutions: Results from multicountry consultations focused on reduction of childhood pneumonia and diarrhoea deaths . The Lancet , 381 , 1487 – 1498 .
- Goffman , E. ( 1963 ). Stigma: Notes on the management of spoiled identity . New York , NY : Simon & Schuster .
- Gottlieb , G. , & Blair , C. ( 2004 ). How early experience matters in intellectual development in the case of poverty . Prevention Science , 5 , 245 – 252 .
- Grantham-McGregor , S. M. , & Cumper , G. ( 1992 ). Jamaican studies in nutrition and child development, and their implications for national development . Proceedings of the Nutrition Society , 51 , 71 – 79 .
- Heijnders , M. , & Van Der Meij , S. ( 2006 ). The fight against stigma: An overview of stigma-reduction strategies and interventions . Psychology, Health & Medicine , 11 , 353 – 363 .
- Hong , K. T. , Van Anh , N. T. , & Ogden , J. ( 2004 ). “Because this is the disease of the century”: Understanding HIV and AIDS-related stigma and discrimination . Retrieved from http://www.icrw.org/files/publications/Understanding-HIV-and-AIDS-related-Stigma-and-Discrimination-in-Vietnam.pdf
- Khatun , M. , Stenlund , H. , & Hörnell , A. ( 2004 ). BRAC initiative towards promoting gender and social equity in health: A longitudinal study of child growth in Matlab, Bangladesh . Public Health Nutrition , 7 , 1071 – 1079 .
- Khumalo-Sakutukwa , G. , Morin , S. F. , Fritz , K. , Charlebois , E. D. , van Rooyen , H. , Chingono , A. , & Coates , T. J. ( 2008 ). Project Accept (HPTN 043): A community-based intervention to reduce HIV incidence in populations at risk for HIV in sub-Saharan Africa and Thailand . Journal of Acquired Immune Deficiency Syndromes , 49 ( 4 ), 422 .
- Kleinman , A. ( 1995 ). The social course of epilepsy: Chronic course of illness as social experience in interior China . In A. Kleinman (Ed.), Writing at the margins: Discourse between anthropology and medicine (pp. 147 – 172 ). Berkeley : University of California Press .
- Kraft , J. M. , Wilkins , K. G. , Morales , G. J. , Widyono , M. , & Middlestadt , S. E. ( 2014 ). An evidence review of gender-integrated interventions in reproductive and maternal-child health . Journal of Health Communication , 19 ( Suppl 1 ), 122 – 141 .
- Kuhn , L. , & Coovadia , H. M. ( 2012 ). Protecting infants of HIV-positive mothers in Malawi . The Lancet , 379 , 2405 – 2407 .
- Kumar , V. , Kumar , A. , Das , V. , Srivastava , N. M. , Baqui , A. H. , Santosham , M. , & Darmstadt , G. L. ( 2012 ). Community-driven impact of a newborn-focused behavioral intervention on maternal health in Shivgarh, India . International Journal of Gynecology & Obstetrics , 117 , 48 – 55 .
- Link , B. G. , & Phelan , J. C. ( 2001 ). Conceptualizing stigma . Annual Review of Sociology , 363 – 385 .
- Logie , C. , James , L. , Tharao , W. , & Loutfy , M. ( 2013 ). Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black women in Ontario, Canada . AIDS Patient Care and STDs , 27 , 114 – 122 .
- Loutfy , M. R. , Logie , C. H. , Zhang , Y. , Blitz , S. L. , Margolese , S. L. , Tharao , W. E. , … Raboud , J. M. ( 2012 ). Gender and ethnicity differences in HIV-related stigma experienced by people living with HIV in Ontario, Canada . PloS One , 7 ( 12 ), e48168 .
- Mahajan , A. P. , Sayles , J. N. , Patel , V. A. , Remien , R. H. , Ortiz , D. , Szekeres , G. , & Coates , T. J. (2008). Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS , 22(Suppl. 2), S67–S79.
- Mahendra , V. S. , Gilborn , L. , Bharat , S. , Mudoi , R. , Gupta , I. , George , B. , … Pulerwitz , J. ( 2007 ). Understanding and measuring AIDS-related settings: A developing country perspective . SAHARA Journal (Journal of Social Aspects of HIV/AIDS Research Alliance) , 4 , 616 – 625 .
- McGlade , M. S. , Saha , S. , & Dahlstrom , M. E. ( 2004 ). The Latina paradox: An opportunity for restructuring prenatal care delivery . American Journal of Public Health , 94 , 2062 – 2065 .
- McLeroy , K. R. , Bibeau , D. , Steckler , A. , & Glanz , K. ( 1988 ). An ecological perspective on health promotion programs . Health Education & Behavior , 15 , 351 – 377 .
- Mepham , S. , Zondi , Z. , Mbuyazi , A. , Mkhwanazi , N. , & Newell , M. L. ( 2011 ). Challenges in PMTCT antiretroviral adherence in northern KwaZulu-Natal, South Africa . AIDS Care , 23 , 741 – 747 .
- Noble , K. G. , Norman , M. F. , & Farah , M. J. ( 2005 ). Neurocognitive correlates of socioeconomic status in Kindergarten children . Developmental Science , 8 , 74 – 87 .
- Norton , M. ( 2005 ). New evidence on birth spacing: Promising findings for improving newborn, infant, child, and maternal health . International Journal of Gynecology & Obstetrics , 89 , S1 – S6 .
- Nöstlinger , C. , Jonckheer , T. , De Belder , E. , Van Wijngaerden , E. , Wylock , C. , Pelgrom , J. , & Colebunders , R. ( 2004 ). Families affected by HIV: Parents' and children's characteristics and disclosure to the children . AIDS Care , 16 , 641 – 648 .
- Nyblade , L. ( 2006 ). Measuring HIV stigma: Existing knowledge and gaps . Psychology, Health & Medicine , 11 , 335 – 345 .
- Nyblade , L. , Hong , K. T. , Anh , N. V. , Ogden , J. , Jain , A. , Stangl , A. , … Ashburn , A. ( 2008 ). Communities confront HIV stigma in Viet Nam: Participatory interventions reduce HIV-related stigma in two provinces . Retrieved from http://www.icrw.org/files/publications/Communities-Confront-HIV-Stigma-in-Vietnam.pdf
- Nyblade , L. , Pande , R. P. , Mathur , S. , MacQuarrie , K. , Kidd , R. , Banteyerga , H. , … Bond , V. ( 2003 ). Disentangling HIV and AIDS stigma in Ethiopia, Tanzania and Zambia . Retrieved from http://www.icrw.org/files/publications/Disentagling-HIV-and-AIDS-Stigma-in-Ethiopia-Tanzania-and-Zambia.pdf
- Nyblade , L. , Stangl , A. , Weiss , E. , & Ashburn , K. ( 2009 ). Combating HIV stigma in health care settings: what works? Journal of the International AIDS Society , 12 , 15 : 1 – 7 .
- Oanh , K. T. H. , Ashburn , K. , Pulerwitz , J. , Ogden , J. , & Nyblade , L. ( 2008 ). Improving hospital-based quality of care in Vietnam by reducing HIV-related stigma and discrimination . Retrieved from http://www.icrw.org/files/publications/Improving-hospital-based-quality-of-care-in-Vietnam-by-reducing-HIV-related-stigma-and-discrimination.pdf
- O'Driscoll , C. , Heary , C. , Hennessy , E. , & McKeague , L. ( 2012 ). Explicit and implicit stigma towards peers with mental health problems in childhood and adolescence . Journal of Child Psychology and Psychiatry , 53 , 1054 – 1062 .
- Ogden , J. , & Nyblade , L. ( 2005 ). Common at its core: HIV-related stigma across contexts . Retrieved from http://www.icrw.org/files/publications/Common-at-its-Core-HIV-Related-Stigma-Across-Contexts.pdf
- Painter , T. M. , Diaby , K. L. , Matia , D. M. , Lin , L. S. , Sibailly , T. S. , Kouassims , M. K. , … Wiktor , S. Z. ( 2005 ). Sociodemographic factors associated with participation by HIV-1-positive pregnant women in an intervention to prevent mother-to-child transmission of HIV in Cote d'Ivoire . International Journal of STD & AIDS , 16 , 237 – 242 .
- Pandey , P. , Sehgal , A. R. , Riboud , M. , Levine , D. , & Goyal , M. ( 2007 ). Informing resource-poor populations and the delivery of entitled health and social services in rural India . JAMA , 298 , 1867 – 1875 .
- Parker , R. , & Aggleton , P. ( 2003 ). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action . Social Science & Medicine , 57 , 13 – 24 .
- Parkhurst , J. O. (2012). HIV prevention, structural change and social values: The need for an explicit normative approach . Journal of the International AIDS Society , 15(3 Suppl. 1), 17367.
- Pulerwitz , J. , Michaelis , A. , Weiss , E. , Brown , L. , & Mahendra , V. ( 2010 ). Reducing HIV-related stigma: Lessons learned from Horizons research and programs . Public Health Reports , 125 , 272 – 281 .
- Quinn , D. M. , & Chaudoir , S. R. ( 2009 ). Living with a concealable stigmatized identity: The impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health . Journal of Personality and Social Psychology , 97 , 634 – 651 .
- Rahangdale , L. , Banandur , P. , Sreenivas , A. , Turan , J. M. , Washington , R. , & Cohen , C. R. ( 2010 ). Stigma as experienced by women accessing prevention of parent-to-child transmission of HIV services in Karnataka, India . AIDS Care , 22 , 836 – 842 .
- Rao , D. , Desmond , M. , Andrasik , M. , Rasberry , T. , Lambert , N. , Cohn , S. E. , & Simoni , J. ( 2012 ). Feasibility, acceptability, and preliminary efficacy of the unity workshop: An internalized stigma reduction intervention for African American women living with HIV . AIDS Patient Care and STDs , 26 , 614 – 620 .
- Reidpath , D. D. , & Chan , K. Y. ( 2005 ). A method for the quantitative analysis of the layering of HIV-related stigma . AIDS Care , 17 , 425 – 432 .
- Rekart , M. L. ( 2006 ). Sex-work harm reduction . The Lancet , 366 , 2123 – 2134 .
- Rhodes , T. , Bernays , S. , & Houmoller , K. ( 2010 ). Parents who use drugs: Accounting for damage and its limitation . Social Science & Medicine , 71 , 1489 – 1497 .
- Richter , L. M. , & Naicker , S. ( 2013 ). A review of published literature on supporting and strengthening child-caregiver relationships (parenting) . USAID's AIDS Support and Technical Assistance Resources, AIDSTAR-One, Task Order 1 . Retrieved from http://www.aidstar-one.com/sites/default/files/AIDSTAROne_Parenting_LitReview_finalweb.pdf
- Schiffman , J. , Darmstadt , G. L. , Agarwal , S. , & Baqui , A. H. ( 2010 ). Community-based intervention packages for improving perinatal health in developing countries: A review of the evidence . Seminars in Perinatology , 34 , 462 – 476 .
- Sengupta , S. , Banks , B. , Jonas , D. , Miles , M. S. , & Smith , G. C. ( 2011 ). HIV interventions to reduce HIV/AIDS stigma: A systematic review . AIDS and Behavior , 15 , 1075 – 1087 .
- Stangl , A. , Carr , D. , Brady , L. , Eckhaus , T. , Claeson , M. , & Nyblade , L. ( 2010 ). Tackling HIV-related stigma and discrimination in South Asia . Retrieved from http://siteresources.worldbank.org/SOUTHASIAEXT/Resources/223546-1192413140459/4281804-1231540815570/5730961-1235157216166/5849907-1279637337320/Tackling_HIV_Stigma_July_2010.pdf
- Stangl , A. , Go , V. , Zelaya , C. , Brady , L. , Nyblade , L. , & Stackpool-Moore , L. ( 2010 , July 18–23 ). Enabling the scale-up of efforts to reduce HIV stigma and discrimination: A new framework to inform program implementation and measurement. Poster presented at the XVIII International AIDS Conference, Vienna, Austria.
- Stangl , A. L. , Lloyd , J. K. , Brady , L. M. , Holland , C. E. , & Baral , S. ( 2013 ). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society , 16 ( 3 Suppl 2 ), 18734 .
- Swaminathan , H. , Walker , C. , Rugadya , M. A. ( 2008 ). Women's property rights, HIV and AIDS & domestic violence: Research findings from two districts in South Africa and Uganda . Pretoria , South Africa : Human Services Research Council Press . Retrieved from http://www.hsrcpress.ac.za/product.php?cat=1&sort=price&sort_direction=&page=1&productid=2232
- Tripathy , P. , Nair , N. , Barnett , S. , Mahapatra , R. , Borghi , J. , Rath , S. , … Costello , A. ( 2010 ). Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: A cluster-randomized controlled trial . The Lancet , 375 , 1182 – 1192 .
- Turan , J. M. , Bukusi , E. A. , Onono , M. , Holzemer , W. L. , Miller , S. , & Cohen , C. R. (2011). HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: Results from the MAMAS Study. AIDS and Behavior , 15, 1111–1120.
- Turan , J. M. , Miller , S. , Bukusi , E. A. , Sande , J. , & Cohen , C. R. ( 2008 ). HIV/AIDS and maternity care in Kenya: How fears of stigma and discrimination affect uptake and provision of labor and delivery services . AIDS Care , 20 , 938 – 945 .
- Turan , J. M. , & Nyblade , L. ( 2013 ). HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: A review of the evidence . AIDS and Behavior , 17 , 2528 – 2539 .
- van Brakel , W. H. , Sihombing , B. , Djarir , H. , Beise , K. , Kusumawardhani , L. , Yulihane , R. , & Wilder-Smith , A. ( 2012 ). Disability in people affected by leprosy: The role of impairment, activity, social participation, stigma and discrimination . Global Health Action , 5 .
- Viteva , E. ( 2012 ). Impact of stigma on the quality of life of patients with refractory epilepsy . Seizure , 22 , 64 – 69 .
- Walker , C. L. F. , Rudan , I. , Liu , L. , Nair , H. , Theodoratou , E. , Bhutta , Z. A. , & Black , R. E. ( 2013 ). Global burden of childhood pneumonia and diarrhoea . The Lancet , 381 , 1405 – 1416 .
- Watts , C. , Zimmerman , C. , Eckhaus , T. , & Nyblade , L. ( 2010 ). Modelling the impact of stigma on HIV and AIDS programmes: Preliminary projections for mother-to-child transmission . Washington , DC : International Center for Research on Women (ICRW) and London School of Hygiene and Tropical Medicine .
- Wilkinson , R. G. , & Marmot , M. G. ( 2003 ). Social determinants of health: The solid facts . Geneva , Switzerland : World Health Organization .
- Yoshikawa , H. , Aber , J. L. , & Beardslee , W. R. ( 2012 ). The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention . American Psychologist , 67 , 272 .
- Young , S. D. , Konda , K. , Caceres , C. , Galea , J. , Sung-Jae , L. , Salazar , X. , & Coates , T. ( 2011 ). Effect of a community popular opinion leader HIV/STI intervention on stigma in urban, coastal Peru . AIDS and Behavior , 15 , 930 – 937 .
- Zelaya , C. E. , Sivaram , S. , Johnson , S. C. , Srikrishnan , A. K. , Suniti , S. , & Celentano , D. D. ( 2012 ). Measurement of self, experienced, and perceived HIV/AIDS stigma using parallel scales in Chennai, India . AIDS Care , 24 , 846 – 855 .
- Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/uhcm.
