Abstract
Background
Virtual Reality (VR) is an immersive technology, which transports the user to a three-dimensional ‘virtual world’ and is increasingly used as an innovative treatment modality in various aspects of healthcare. The use of immersive VR in the management of musculoskeletal conditions is relatively new and research is required to demonstrate its effectiveness in this field.
Aim
The aim of this narrative review is to explore the effectiveness of immersive VR interventions in the management of musculoskeletal conditions.
Methods
A literature search was carried out on the following databases: Pubmed, Scopus and Medline using the following keywords: Virtual Reality and Pain. Studies of any design were included if they reported clinical outcomes following an immersive VR intervention for individuals with musculoskeletal pain.
Results
Thirteen studies which investigated the effectiveness of immersive VR in the management of musculoskeletal conditions were identified. Studies included people with various musculoskeletal conditions: neck pain (5), low back pain (1), complex regional pain syndrome (4), peripheral nerve injury (1), fibromyalgia (1) and total knee replacement (2). Only five randomized controlled trials were found. Outcome measures included but were not limited to pain, range of motion and disability.
Conclusion
Although the current findings are promising and demonstrate that immersive VR interventions may have a useful role in musculoskeletal management and rehabilitation, no conclusive clinical recommendations can be made based on the low quality of available research. Future research should follow a framework with clear standards leading to robust and meaningful outcomes that will guide clinical practice using immersive VR.
Background
Virtual Reality (VR) is an immersive human-computer interface, designed to immerse a person into a virtual environment. The use of VR in healthcare is increasingly supported by research evidence. Examples include burn injury management [Citation1], upper limb rehabilitation post stroke [Citation2] and treatment of mental health disorders [Citation3]. The use of VR in the management of musculoskeletal conditions is relatively new and research is required to demonstrate its feasibility and utility in this field.
Types of VR technology
Non-immersive VR allows the user to view and interact with a computer-generated image of themselves on a screen using a mouse or various hand-held devices. The user in this case, can see and experience the real world outside of the screen and therefore the user is not immersed completely in a virtual world. Non-immersive VR systems include Nintendo Wii™ and Microsoft Kinect™. Semi-immersive VR systems use more advanced visual displays such as panoramic or curved screens to create a greater sense of immersion. Similar to non-immersive technology, the user can see the real world either side of the screen. Semi-immersive technology is commonly used in education and training such as flight simulation for trainee pilots. Immersive VR is based on the use of a head-mounted display unit that offers a multi-sensory experience for the user. Additional equipment including gesture-sensing gloves, wands, vibrotactile platforms and multidirectional treadmills make it possible for the user to explore and interact with the virtual world as an avatar (a virtual character) that represents the individual within the virtual world.
Embodiment occurs when a user is immersed in VR and processes the avatar’s movements (such as the hands) as though they are the users own body parts [Citation4, Citation5]. To maximize embodiment, the VR user must experience a sense of; (i) location (being somewhere in time and space), (ii) agency (performing an action or intervention that produces an effect) and (iii) body ownership (the VR user believes the avatar is the user) [Citation4]. By providing the VR user with sensory feedback (visual, tactile, vestibular and audible) that is synchronous with the users and avatars actions, the sense of location, agency and body ownership are realized.
Immersive VR allows for somatosensory manipulation that may lead to new opportunities in the assessment and management of people with musculoskeletal conditions. As such a review of the current state of the art of immersive VR interventions in the management of musculoskeletal pain identifying current understanding and knowledge gaps will be useful for clinicians considering adoption in practice, researchers contemplating investigating VR and for people with MSK conditions considering its usefulness in management.
Current applications of VR in healthcare
Pain management
Virtual Reality has been shown to be effective in the management of people experiencing acute pain [Citation6–8]. It is widely used in burn injury and wound care as an alternative or adjunct to analgesic medication [Citation1, Citation9]. Specifically, VR has been used to reduce pain and anxiety experienced during wound dressing and rehabilitation, compared to conventional measures [Citation10]. Sense of presence and immersion achieved with VR leads to greater distraction and reduced awareness of injury and pain during wound care procedures [Citation11]. The success of ‘Snow World™’, the first immersive virtual world created to reduce the experience of pain for people with burn injuries demonstrates that context is also relevant. Snow World™ not only provides an element of distraction but also creates a context or ‘habitat’ counter-posed to that associated with danger for burn injured patients. The context in which potentially tissue damaging signals are received by the brain is critical in the experience of pain [Citation12]. For people with burn injuries, the Snow World™ game portrays an icy, cold environment that is diametrically opposed to images associated with burn injuries; fire and heat [Citation13] and as such the context of the experience is changed. Functional magnetic resonance imaging studies exploring the analgesic effects of VR in thermal pain situations have shown reductions in activity in brain regions associated with the pain experience, such as the thalamus and insula, and this may explain the analgesic mechanisms behind VR in such circumstances [Citation13, Citation14].
Mental health
Maples-Keller et al. [Citation3] reported that the greatest strength of evidence for VR in mental healthcare is Virtual Reality Exposure Therapy (VRE). VRE is used for treating anxiety disorders and phobias by placing individuals in a VR world and exposing them to stressful environments e.g. fear of flying, heights or spiders. Rothbaum et al. [Citation15–17], demonstrated symptom reduction and behavioral change in those with fear of flying with VR exposure that is equivalent to in-vivo exposure groups and significantly greater than control groups. An RCT comparing VRE to in-vivo standard exposure (SE) and waiting list (WL) controls (n = 75) found that reduction in scores on the Fear of Flying Inventory (FFI) were significantly greater for both exposure groups compared to controls (VRE = 16.69, SE = 16.45, WL = −14.46, p = 0.009). VR exposure therapy appears to be a safe, cost-effective, more practical intervention and was preferred by patients compared to in vivo exposure therapy [Citation3].
Education
Virtual Reality may have a role in patient education and health literacy awareness. The Oculus™ Study assessed whether VR movie-based education was effective at increasing participants (n = 100) knowledge about atrial fibrillation (AF), stroke prevention strategies including pharmacological treatments [Citation18]. Awareness of AF as a risk factor for stroke increased from 22% to 83% immediately after intervention (p < 0.0001). At one-year follow-up 72.2% participants reported using oral anticoagulant medication compared to 55.6% at baseline (p = 0.006). Similarly, Saab et al. [Citation19] used VR as a platform for educating men about testicular disorders and found a significant improvement in knowledge, awareness, help-seeking intentions and behaviors that lasted at least one-month post intervention. Mean knowledge scores (12 item questionnaire) increased from 6.2 at baseline to 9.8 post intervention (p < 0.001), while awareness scores (Testicular Awareness Scale) increased from 3.6 at baseline to 3.8 post intervention (p < 0.001). VR is a tool that may be applied to many areas of healthcare and may be particularly useful in educating patients around lifestyle factors and long-term management for persistent conditions such as musculoskeletal conditions.
Musculoskeletal conditions
A number of systematic reviews into the use of VR in musculoskeletal conditions have been conducted. Ahern et al. [Citation20] evaluated the effectiveness of VR interventions for the management of musculoskeletal spinal pain. They included seven randomized controlled trials (RCT) in their review, four of which used immersive VR technology, and all were identified as being of high risk of bias. Results indicated that there was an overall small effect size of VR for spinal pain. They concluded that there is potential for VR to have a future role in back pain management but more robust research involving long-term follow-up is needed. Gumaa and Youssef [Citation21] conducted a systematic review of the literature investigating the effectiveness of VR for orthopedic rehabilitation and included 19 RCT’s which explored spinal, upper and lower quadrant musculoskeletal pain, fibromyalgia, osteoarthritis and rheumatoid arthritis. Three out of 19 studies investigated immersive VR. The authors state that studies included were limited by the heterogeneity in type of VR, control interventions and outcome measures used. They stated that 26% of included studies were of high quality, 58% were of moderate quality and 16% were of low quality. They concluded that there was promising evidence to support the effectiveness of VR for neck and shoulder pain but for all other conditions, the evidence was inconclusive. A scoping review by Lin et al. [Citation22] explored the effect of VR on numerous outcomes relevant to musculoskeletal disorders and burn related pain in 14 RCTs. In Lin et al.’s [Citation23] review, there was considerable heterogeneity across the included RCTs in terms of study design, population, and type of VR investigated, with five studies examining the effect of immersive VR. The quality of included studies was considered moderate (mean PEDro score 6.14). The authors conclude that VR intervention appears to have a significant effect on pain, joint mobility and motor function for people with musculoskeletal conditions. However, they state that further research in needed in the area, specifically to explore whether different types of VR have different effects on clinical outcomes. The current research investigating the effectiveness of VR interventions for musculoskeletal conditions is of low-moderate quality and reviews to date are heterogenous in terms of type of VR, control intervention, outcome measures used and clinical population included. Ahern et al. [Citation20] include people with spinal pain but have found that the studies identified are of high risk of bias. Lin et al. [Citation22] include people with musculoskeletal conditions and burn injuries. All the reviews discussed include a mix of immersive and non-immersive VR intervention. This review will be the first to focus on immersive VR in people with musculoskeletal conditions.
Aim
The aim of this review is to explore the effectiveness of immersive VR interventions in the management of musculoskeletal conditions.
Methods
A literature search was carried out on the following databases: Pubmed, Scopus and Medline using the following keywords: Virtual Reality and Pain. Where appropriate, MeSH terms were used for individual databases. The reference lists of relevant articles were screened to identify additional studies for inclusion. Once duplicates were removed the remaining articles underwent further screening for eligibility. Title and abstracts were screened, and full text articles were then assessed for those considered to be eligible. Articles were considered for inclusion if they were published in English in a peer-reviewed journal up to August 2020.
Studies of any design were included if they reported clinical outcomes following an immersive VR intervention for individuals with musculoskeletal pain. We defined musculoskeletal pain as pain originating from a joint and it’s surrounding tissue, as well as muscle, tendon and nerve sources. We excluded studies involving people with burn injury, procedural pain, phantom limb pain, spinal cord injury and experimental pain. Screening was completed by two independent reviewers (NB and TD) and consensus was reached through discussion. Where consensus could not be reached a third reviewer (JL) contributed to the decision process. The following data were extracted and are presented in : authors, year of publication, musculoskeletal condition, intervention, control, primary outcome measure, results. A narrative synthesis was carried out on the effectiveness of immersive VR interventions in the management of musculoskeletal conditions.
Table 1. Data extraction table.
Results
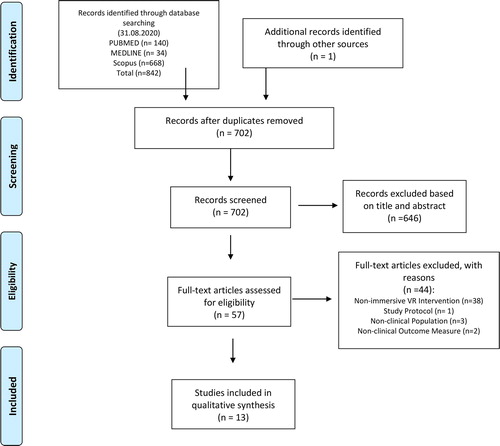
A flowchart of the search is shown in . Our initial search retrieved 842 studies (VR and Pain). After duplicates were removed, a total of 702 articles were identified. One additional article was identified from a reference list of a separate review. After the screening process a total of 57 articles were identified which evaluated VR in musculoskeletal conditions. Of these 56 studies, 19 used immersive VR and 37 used non-immersive VR. Following review of the mode of VR used, we were left with 13 studies which investigated the effectiveness of immersive VR in the management of musculoskeletal conditions.
Of the 13 studies identified, five included people with neck pain, one study investigated people with low back pain, four studies included people with complex regional pain syndrome (CRPS) and peripheral nerve injury (PNI), one study recruited people with fibromyalgia and two studies used VR in rehabilitation following total knee replacement surgery. In terms of study design, five studies were RCTs and the others were non-randomized clinical trials, pilot studies, experimental studies, case series and a single case report. All studies involved immersive VR, in isolation or in combination with another treatment. Outcome measurement varied considerably. The most commonly measured outcome was pain, followed by range of motion and disability. Other outcomes included strength, balance, body perception, exercise capacity, kinesiophobia, joint kinematics and quality of life.
Neck pain
Bahat et al. [Citation25] compared VR Kinematic training (VRKT) to non-VR kinematic training (KT) in both supervised and home settings in patients with persistent neck pain (n = 90). They found significant improvements in Neck Disability Index (NDI) scores in both groups but greater improvement in the VRKT group (Mean: VRKT Pre-intervention: 29.6, Post-intervention 21.7, 3 p < 0.01, three month follow up 18.6 p < 0.01, KT Pre-intervention: 28.2, Post-intervention 25.1 p > 0.05, three month follow up 23.6 p < 0.05). However, when groups were compared, there was no significant difference in disability scores. Both groups showed significant improvements in mean cervical movement velocity in all directions post intervention and at three month follow up (p < 0.05), with one exception; the KT did not show significant improvements in left rotation mean velocity at 3 month follow up (p < 0.05). The VRKT group showed significantly greater improvements in flexion and left rotation velocity compared to the KT group (p < 0.05) An earlier pilot study by Bahat et al. [Citation36] found similar effects when comparing VRKT to KT for people with neck pain. Both groups showed improvements in several outcomes (range of movement, velocity of movement), however, only the VRKT group-maintained improvements in Neck Disability Index scores at three-month follow-up. In addition, the VRKT group alone showed significant improvement in global perceived effect at three-month follow-up (p < 0.05).
Harvie et al. [Citation24] investigated the use of VR for manipulating somatosensory input to influence perceived cervical movement. They used a technique termed ‘re-directed walking’ to provide altered visio-kinetic input to users, thus altering body perception. In a group of 24 participants with persistent, movement induced neck pain, VR was used to provide a visual illusion that either exaggerated or understated the range of actual movement [Citation23]. During visual feedback that understated true rotation (by 20%), pain-free motion was increased by 6% (95% CI 2–11%); during visual feedback that overstated true rotation (by 20%), pain-free range of motion decreased by 7% (95% CI 3–11%). A more recent study by Harvie et al. [Citation26] required people with neck pain to use VR twice daily at home. Participants progressed through two phases of VR exercise, one without a visual illusion and another that provided a visual illusion to exaggerate the range of movement that the individual performed. The authors hypothesized that the illusion would lead to a reduction in neck pain intensity. However, no significant between phase differences were found for movement evoked pain threshold or pain intensity (p > 0.05).
In a recent RCT, VR rehabilitation was compared to standard rehabilitation for neck pain management [Citation27]. Participants in each group completed two training session per week for four weeks. Participants in the VR group (n = 22) played games that involved neck movements of varying levels of challenge, while participants in the control group (n = 22) completed three sets of 10 of each neck exercise in each training session. Both groups demonstrated significant improvement in pain intensity at all time points (p < 0.01) but there was no significant difference between groups. Similarly, both groups showed significant improvements in NDI scores at all time points (p < 0.01) but there was no significant difference between the groups. The VR group showed significant improvement in rotation at 1-month (p < 0.05) and lateral flexion at 3-months (p < 0.05) compared to the control group.
Low back pain
Igna et al. [Citation28] designed a clinical trial to compare the effect of mindfulness-based cognitive behavioral therapy (MBCBT) to VR-enhanced CBT (VRCBT) and standard physiotherapy for patients with chronic low back pain. For the VRCBT group, classical CBT was followed by a 5-minute session of using the Snow World game which is an immersive software designed for patients with burn injury pain. Igna et al.’s [Citation28] findings demonstrated that VRCBT was no more effective than standard physiotherapy for reducing pain as measured by a visual analogue scale (VAS) and the McGill Pain Questionnaire (p > 0.05).
Complex regional pain syndrome
Four studies investigated the effect of VR interventions for management of Complex Regional Pain Syndrome as well Peripheral Nerve Injury. One study also included patients with peripheral nerve injury [Citation31]. Solcà et al. [Citation29] recruited 24 participants with CRPS and a further 24 age and sex-matched controls. VR was used to present an image of a heart, beating synchronously or asynchronously with their own heartbeat. For patients with CRPS, it was found that when the virtual heart was beating synchronously with the participant’s actual heart, pain levels decreased (F(1,94.09) = 4.63, p = 0.033) and grip strength increased (t(17) = 2.5, p = 0.023, mean 0.85 kg, 95% CI 0.072–1.63, SEM 0.37). Jeon et al. [Citation30] included ten participants in a pilot study to investigate whether virtual body swapping is applicable to patients with CRPS. Body swapping is an illusion that the virtual body is perceived as the person’s own body. All participants viewed a video clip through VR and five participants were instructed to do a mental rehearsal exercise of the movements presented in the video. Body perception disturbance scores improved significantly in the mental rehearsal group compared to the control group (F(1,8) = 16.22, p = 0.01), while significant differences were found in virtual body swapping scores between the groups in favor of the mental rehearsal group (T(8) = 2.40, p = 0.04). For patients with CRPS and PNI (N = 19), Matamala-Gomez et al. [Citation31] used VR to manipulate characteristics (size and transparency) of a virtual arm. They found that in all conditions where the virtual arm was manipulated (in size or transparency), pain was reduced by at least 50%. Chau et al. [Citation32] investigated the effect of VR on pain and function in eight patients with CRPS. Participants were asked to perform various tasks within a virtual three-dimensional kitchen. They also performed guided visualization exercises in a virtual environment. Authors state that for all participants who completed the study (n = 6), there was an overall increase in pain intensity post-intervention, as demonstrated by the Visual Analogue Scale and Short-form McGill Pain Questionnaire despite participants reporting reduced symptoms within sessions.
Fibromyalgia
Gulsen et al. [Citation33] carried out a small RCT (n = 16) to evaluate the effects of VR and exercise compared to exercise alone in a group of patients with fibromyalgia. Both groups completed 30 min aerobic exercise plus 30 min Pilates exercise twice weekly for eight weeks. In addition, the VR group played VR games for 20 min. The VR group showed significantly greater improvement compared to the to exercise alone group in pain (VAS mean change VR group −4, Control group −2.05 p = 0.021), kinesiophobia (VR group −12, Control group −10, p = 0.034), fatigue (VR Group −2.82, Control (−1.16), level of physical activity (VR Group 1797.25, Control Group 528.5, p = 0.001) and mental component of quality of life (VR Group 148, Control Group 70.25, p = 0.016).
Total knee replacement
Jin et al. [Citation34] carried out a RCT (n = 66), comparing standard rehabilitation combined with immersive VR rowing to standard rehabilitation combined with regular passive range of motion exercises following TKR. They reported significantly greater improvement in knee range of motion and function, as measured by the Western Ontario McMaster University Osteoarthritis Index (WOMAC) 1-month post TKA:VR group 32.00, Control group 35.06 (p = 0.02); 3-month post TKA: VR group 25.79, Control group 29.67 (p = 0.002); 6-month post TKA: VR group 21.58, Control group 26.33 (p = 0.000) and Hospital for Special Surgery Knee Score (HSS) 1-month post TKA: VR group 68.39, Control group 60.45 (p = 0.000), 3-month post TKA: VR group 77.73, Control Group 67.94 (p = 0.000); 6-month post TKA: VR group 87.55, Control Group 80.39 (p = 0.000), and significant reductions in pain at seven days following surgery in the immersive VR group compared to the control group VR group 3.87, Control Group 4.42 (p = 0.002). A single case report by Hong and Lee [Citation35] demonstrated the application of VR in a multifaceted rehabilitation programme for a patient following total knee replacement. In addition to 20 min of VR training, the patient completed range of motion exercise, isometric exercise and received both thermotherapy and electrotherapy. After two weeks of five-weekly sessions, the patient showed a 32% increase in lower limb muscle strength, a 45% improvement in proprioception and a return of walking speed to pre-surgical level.
Risks and adverse effects associated with VR technology
Four studies reported adverse effects related to the VR intervention. The most commonly reported adverse effect of using immersive VR is motion sickness [Citation25, Citation26, Citation36]. Motion sickness occurs due to a mismatch of sensory information between the virtual and real world. Devices with reduced accuracy in motion tracking may lead to feelings of nausea, dizziness and headache [Citation37]. Improved technology that optimizes congruency of movement with visual feedback may minimize this risk. Another adverse effect that was experienced by one participant [Citation32] was an increase in self-reported nervous system sensitivity. It is difficult to say whether this effect resulted from immersive VR exposure or the exercise itself.
Discussion
This is the first review to explore the effectiveness of immersive VR in the management of musculoskeletal conditions. The review identified considerable variation of protocol interventions. Programs ranged from passive (watching a video using VR) to interactive (games that require whole body movement and cognitive attention). Some studies used VR as a standalone intervention and in other cases VR was used in combination with other management tools. For patients with neck pain, VR was well tolerated and was at least as effective as standard rehabilitation for all outcomes [Citation25, Citation36]. The experiment by Harvie et al. [Citation23] suggests that VR could be used to influence pain threshold and movement for individuals with movement-induced neck pain. VR was only a minor component of the VRCBT intervention for LBP patients and the VR software used was possibly not ideal for a LBP population [Citation28]. In addition, the authors did not state what usual physiotherapy comprised of. Therefore, the findings must be interpreted with caution and cannot be used to guide the application of VR in musculoskeletal practice.
For patients with CRPS, there were mixed findings. A virtual heartbeat had the potential to modify pain intensity and grip strength in a small group of participants [Citation29]. Virtual body swapping was effective for patients with CRPS, however, results improved when participants were actively completing a mental task [Citation30]. This may suggest that participation in the VR intervention has an added effect, perhaps by focusing attention on the task. Matamala-Gomez et al. [Citation31] demonstrated a reduction in pain intensity for patients with CRPS and PNI by manipulating the transparency and size of a virtual arm. For both studies mentioned above, it would be valuable to replicate this protocol in a clinical trial and compare outcomes with a control group intervention. The VR intervention used by Chau et al. [Citation32] involved both active tasks and visualization exercises in a virtual environment. Pain outcomes worsened post-intervention despite participants informally reporting within sessions that the intervention was beneficial. These paradoxical findings and the fact that only six participants completed the study, make it challenging to draw conclusions on the effectiveness of VR for pain in patients with CRPS. For patients with fibromyalgia, VR was added to a programme of aerobic and Pilates exercise and positively impacted on several outcomes when compared to exercise alone [Citation33]. However, this RCT included a small sample size (n = 16), and results must be interpreted with caution. For patients following TKR, Jin et al. [Citation34] demonstrated significant improvements in favor of the VR group in pain, range of motion and function. However, the VR group intervention required participants to actively flex their knee, while the control group were instructed to passively flex their knee, two very different types of exercise. For one patient following TKR [Citation35], VR was added to a multifaceted intervention and was tolerated well. While it is difficult to say what components of rehabilitation contributed most to overall improvement, the VR training duration (30 min) accounted for half of the overall intervention duration (60 min) per session.
The current review identified 13 studies that investigated the effectiveness of immersive VR for managing musculoskeletal conditions, with mixed study design. Of the five RCTs included sample size ranged from 16 to 92 participants. Other study designs included non-randomised trials, pilot studies, experimental studies, case series and a single case study which is the lowest form of research evidence. In addition, none of the included articles report on the minimal clinically important difference (MCID) for outcomes. While some promising results have been presented, limitations in quality of studies included impacts on interpretation of results. Heterogeneity of clinical population, interventions and outcome measures makes it difficult to draw comparisons between studies and conclusions regarding the effectiveness of immersive VR for the management of musculoskeletal conditions.
Currently there is uncertainty around the mechanisms underlying the effect that VR has on pain and range of movement. Persistent pain is associated with sensory changes and functional reorganization of the somatosensory cortex. Melzack [Citation38] proposed that the neurosignature for pain experience is determined by the synaptic architecture of the neuromatrix, which is produced by genetic and sensory influences. The neurosignature projects to various areas of the brain to create a sense of awareness of self, feelings, emotions, and activation of behavior. Riva et al. [Citation5] describe a brain mechanism called ‘embodied simulations’, which contribute to the body neuromatrix. VR technology shares this basic mechanism [Citation5]. Like the brain, VR technology maintains a simulation of the body and the space around it so that it can accurately predict the consequences of an individual’s actions within the virtual world. By doing this, VR may be able to trick the predictive coding mechanisms used by the brain [Citation5], generating the feeling of presence in the virtual body and altering the experience of the body, including the pain experience. Riva et al. [Citation5] suggest that VR as an embodied medicine may offer a new platform for augmenting the experience of the body for clinical goals and may explain the mechanisms behind clinical improvements demonstrated in VR literature to date. In addition, using VR to demonstrate the change in experience of neck pain reported by Harvie et al. [Citation23] or other types of pain may offer a valuable education tool for explaining pain.
Limitations and uncertainties relating to VR research
Clinical VR research may be described as ‘heterogeneous’ and lacking in robust experimental design [Citation39]. There is uncertainty regarding its use in people with musculoskeletal conditions and there remain many unanswered questions. For example, it is not clear if the effectiveness of immersive VR is limited to the time spent using VR as long-term studies have not yet been conducted. It is also unclear whether various contexts can be used to modulate pain sensitivity in those with musculoskeletal conditions. Harvie et al. [Citation40] investigated whether pain sensitivity would be increased if the context associated with previously painful stimuli were presented using VR to healthy, asymptomatic participants, however, no change in pain sensitivity was demonstrated using VR. Further research is required to investigate the importance of context to modulate pain using VR.
To date there is little understanding of individual characteristics that influence tolerance, acceptability, enjoyment, and overall success with VR delivered therapy. Characteristics such as age, sex, immersive tendencies, technological literacy, and socioeconomic status may all be important to consider when deciding whether VR is an appropriate tool in clinical practice. Qualitative data from Tsekleves et al. [Citation41] suggest that the ability to personalize the game or program so that it targets the interests and ability of the user are important. It has also been suggested that providing encouragement, positive feedback and rewards to users based on their participation has a positive effect on engagement and motivation [Citation42]. However, most of these qualitative studies were with individuals using VR for stroke rehabilitation. Further research is needed to investigate whether similar features are advantageous for those using VR for musculoskeletal conditions. None of the included studies provided a cost-effective analysis for immersive VR intervention. Further research is needed to evaluate whether immersive VR interventions can lead to reduction in healthcare costs while providing a similar effect or even superior effect to traditional musculoskeletal management and rehabilitation.
Birkhead et al. [Citation39] have suggested a framework to assist with standardization of VR clinical research, which includes three phases: (i) development of the VR therapy intervention, (ii) feasibility and acceptability studies and (iii) randomized controlled trials. This framework may guide future research in musculoskeletal clinical practice.
Future research
There is a need for both qualitative and quantitative research methods to fully explore the role of immersive VR in the management of musculoskeletal questions. To date, no study has examined the acceptability to both clinicians and patients of using this technology in clinical practice. There is a large potential for the development of software to target specific conditions and body regions using evidence-based principles of musculoskeletal management and rehabilitation. Software development should involve a collaborative approach with input from both patients and clinicians [Citation39]. There is a need for both feasibility and pilot studies to establish initial clinical efficacy as well as tolerability before designing large and robust RCT’s with both short and long-term follow up. Future research should involve experimental work to explore the mechanisms by which VR technology modulates pain and behavior. This may be dependent on the type of VR application employed, of which there are many. Knowledge of these mechanisms may help us understand how various VR applications may be appropriate to achieve specific clinical outcomes so that we can use VR technology to its maximum potential.
Conclusion
Immersive VR has been successfully used with various clinical populations for the purpose of acute pain management, anxiety management, rehabilitation, and education. Its ability to provide the user with convincing multi-sensory illusions gives potential for rehabilitation and management of persistent pain. However, many studies relating to musculoskeletal pain are of low quality, with small sample sizes, short-term follow-up and do not include control groups. Therefore, although the current findings are promising and demonstrate that immersive VR interventions may have a useful role in musculoskeletal management and rehabilitation, no conclusive clinical recommendations can be made based on the quality of available research. Future research should follow a framework with clear standards leading to robust and meaningful outcomes that will guide clinical practice using immersive VR. Immersive VR technology is evolving; devices and applications are increasingly reliable, affordable, and sensitive, providing a truly immersive and inter-active experience. Combining current musculoskeletal research evidence, pain neuroscience and behavioral science in the design of modern VR software is an exciting challenge that has the potential to contribute to and potentially change how we manage musculoskeletal pain.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Niamh Brady
Niamh Brady, MPhty BSc (hons) Physiotherapist, Lecturer in Anatomy, PhD Candidate, Discipline of Physiotherapy, School of Clinical Therapies, College of Medicine and Health, University College Cork., Department of Anatomy and Neuroscience, University College Cork, Cork, Ireland., Evolve Health, Physiotherapy and Rehabilitation Clinic, Cork, Ireland. Niamh’s research interests are musculoskeletal shoulder pain and rehabilitation, pain neuroscience and virtual reality applications in musculoskeletal care.
Joseph G. McVeigh
Dr Joseph G. McVeigh, Head of Discipline of Physiotherapy, School of Clinical Therapies, University College Cork, Ireland. Dr McVeigh’s research interest are broadly the rehabilitation of long-term musculoskeletal conditions.
Karen McCreesh
Dr Karen McCreesh, Discipline Lead Physiotherapy, School of Allied Health, University of Limerick, Ireland. Dr McCreesh’s research interest are musculoskeletal disorders, pain, and ultrasound imaging.
Ebonie Rio
Dr Ebonie Rio, PhD MPhty Ba Phys(Hons) Ba App Sci, Post-Doctoral Researcher, La Trobe University, Melbourne, Australia. Dr. Rio’s research interests are musculoskeletal disorders, tendon pain and virtual reality rehabilitation.
Thomas Dekkers
Thomas Dekkers, MPhty MSc BSc (hons), Physiotherapist and Director, Evolve Health, Skibbereen, Co. Cork., PhD Candidate, Technological University Dublin, Ireland. Thomas’ research interests are athletic back pain and exercise science.
Jeremy S. Lewis
Jeremy Lewis, PhD FCSP is Professor of Musculoskeletal Research, University of Hertfordshire, UK and Consultant Physiotherapist, Central London Community Healthcare NHS Trust, UK. He is also an MSK sonographer and independent non-medical prescriber. He is Special Features Editor for the JOSPT and editor and author for Grieve’s 4th and 5th editions and The Shoulder: Theory & Practice (Handspring).
References
- Scapin S, Echevarria-Guanilo ME, Junior PRBF, et al. Virtual reality in the treatment of burn patients: a systematic review. Burns. 2018;44(6):1403–1416.
- Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11:CD008349
- Maples-Keller JL, Bunnell BE, Kim SJ, et al. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry. 2017;25(3):103–113.
- Kilteni K, Groten R, Slater M. The sense of embodiment in virtual reality. Presence Teleoper Virtual Environ. 2012;21(4):373–387.
- Riva G, Wiederhold BK, Mantovani F. Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychol Behav Soc Netw. 2019;22(1):82–96.
- Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053–2085.
- Pourmand A, Davis S, Marchak A, et al. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep. 2018;22(8):53.
- Won AS, Bailey J, Bailenson J, et al. Immersive virtual reality for pediatric pain. Children. 2017;4(7):52.
- Kipping B, Rodger S, Miller K, et al. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns. 2012;38(5):650–657.
- Schmitt YS, Hoffman HG, Blough DK, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011;37(1):61–68.
- Hoffman HG, Doctor JN, Patterson DR, et al. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain. 2000;85(1-2):305–309.
- Moseley GL, Arntz A. The context of a noxious stimulus affects the pain it evokes. Pain. 2007;133(1-3):64–71.
- Hoffman HG, Richards TL, Bills AR, et al. Using FMRI to study the neural correlates of virtual reality analgesia. CNS Spectr. 2006;11(1):45–51.
- Li A, Montano Z, Chen VJ, et al. Virtual reality and pain management: current trends and future directions. Pain Manag. 2011;1(2):147–157.
- Rothbaum BO, Hodges L, Smith S, et al. A controlled study of virtual reality exposure therapy for the fear of flying. J Consult Clin Psychol. 2000;68(6):1020–1026.
- Rothbaum BO, Hodges L, Anderson PL, et al. Twelve-month follow-up of virtual reality and standard exposure therapies for the fear of flying. J Consult Clin Psychol. 2002;70(2):428–432.
- Rothbaum BO, Anderson P, Zimand E, et al. Virtual reality exposure therapy and standard (in vivo) exposure therapy in the treatment of fear of flying. Behav Ther. 2006;37(1):80–90.
- Balsam P, Borodzicz S, Malesa K, et al. OCULUS study: virtual reality-based education in daily clinical practice. Cardiol J. 2019;26(3):260–264.
- Saab MM, Landers M, Cooke E, et al. Enhancing men’s awareness of testicular disorders using a virtual reality intervention: a pre-post pilot study. Nurs Res. 2018;67(5):349–358.
- Ahern MM, Dean LV, Stoddard CC, et al. The effectiveness of virtual reality in patients with spinal pain: a systematic review and meta-analysis. Pain Pract. 2020;20(6):656–675.
- Gumaa M, Rehan Youssef A. Is virtual reality effective in orthopedic rehabilitation? A systematic review and meta-analysis. Phys Ther. 2019;99(10):1304–1325.
- Lin HT, Li YI, Hu WP, et al. A scoping review of the efficacy of virtual reality and exergaming on patients of musculoskeletal system disorder. J Clin Med. 2019;8(6):791.
- Harvie DS, Broecker M, Smith RT, et al. Bogus visual feedback alters onset of movement-evoked pain in people with neck pain. Psychol Sci. 2015;26(4):385–392.
- Harvie DS, Smith RT, Hunter EV, et al. Using visuo-kinetic virtual reality to induce illusory spinal movement: the MoOVi Illusion. PeerJ. 2017;5:e3023.
- Bahat HS, Croft K, Carter C, et al. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J. 2018;27(6):1309–1323.
- Harvie DS, Smith RT, Moseley GL, et al. Illusion-enhanced virtual reality exercise for neck pain: a replicated single case series. Clin J Pain. 2020;36(2):101–109.
- Tejera DM, Beltran-Alacreu H, Cano-de-la-Cuerda R, et al. Effects of virtual reality versus exercise on pain, functional, somatosensory and psychosocial outcomes in patients with non-specific chronic neck pain: a randomized clinical trial. Int J Environ Res Public Health. 2020;17(16):5950–5969.
- Igna R, Stefan S, Onac I, et al. Mindfulness-based cognitive-behavior therapy (MCBT) versus virtual reality (VR) enhanced CBT, versus treatment as usual for chronic back pain. A clinical trial. J Evid Based Psychother. 2014;14:229–247.
- Solcà M, Ronchi R, Bello-Ruiz J, et al. Heartbeat-enhanced immersive virtual reality to treat complex regional pain syndrome. Neurology. 2018;91(5):e479–e489.
- Jeon B, Cho S, Lee J-H. Application of virtual body swapping to patients with complex regional pain syndrome: a pilot study. Cyberpsychol Behav Soc Netw. 2014;17(6):366–370.
- Matamala-Gomez M, Diaz Gonzalez AM, Slater M, et al. Decreasing pain ratings in chronic arm pain through changing a virtual body: different strategies for different pain types. J Pain. 2019;20(6):685–697.
- Chau B, Phelan I, Ta P, et al. Immersive virtual reality for pain relief in upper limb complex regional pain syndrome: a pilot Study. Innov Clin Neurosci. 2020;17(4-6):47–52.
- Gulsen C, Soke F, Eldemir K, et al. Effect of fully immersive virtual reality treatment combined with exercise in fibromyalgia patients: a randomized controlled trial. Assistive Technol. 2020;1–8.DOI:10.1080/10400435.2020.1772900
- Jin C, Feng Y, Ni Y, Shan Z. Virtual reality intervention in postoperative rehabilitation after total knee arthroplasty: a prospective and randomized controlled clinical trial. Int J Clin Exp Med. 2018;11(6):6119–6124.
- Hong S, Lee G. Effects of an immersive virtual reality environment on muscle strength, proprioception, balance, and gait of a middle-aged woman who had total knee replacement: a case report. Am J Case Rep. 2019;20:1636–1642.
- Sarig Bahat H, Takasaki H, Chen X, et al. Cervical kinematic training with and without interactive VR training for chronic neck pain – a randomized clinical trial. Manual Therapy. 2015;20(1):68–78.
- Regan C. An investigation into nausea and other side-effects of head-coupled immersive virtual reality. Virtual Reality. 1995;1(1):17–31.
- Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001;65(12):1378–1382.
- Birckhead B, Khalil C, Liu X, et al. Recommendations for methodology of virtual reality clinical trials in health care by an International Working Group: iterative study. JMIR Ment Health. 2019;6(1):e11973.
- Harvie DS, Sterling M, Smith AD. Do pain-associated contexts increase pain sensitivity? An investigation using virtual reality. Scand J Pain. 2018;18(3):525–532.
- Tsekleves E, Paraskevopoulos IT, Warland A, et al. Development and preliminary evaluation of a novel low cost VR-based upper limb stroke rehabilitation platform using Wii technology. Disability Rehabil Assistive Technol. 2016;11(5):413–422.
- Warland A, Paraskevopoulos I, Tsekleves E, et al. The feasibility, acceptability and preliminary efficacy of a low-cost, virtual-reality based, upper-limb stroke rehabilitation device: a mixed methods study. Disability Rehabil. 2019;41(18):2119–2134.