Abstract
Background
There are challenges implementing physical activity interventions for people across the stroke pathway of care. There is a need to understand the intervention content in addition to the effects.
Objective
This scoping review maps out the existing systematic review evidence in relation to five objectives.
Design
Intervention data were extracted to identify and clarify definitions of physical activity as well as key emerging themes, gaps and recommendations for implementation approaches and consensus.
Results
50 systematic reviews fulfilled the predefined inclusion criteria. Most reviews (n = 31) focused on a subset of physical activity rather than day to day physical activity (n = 19). In addition, a description of theories underpinning the interventions were lacking. Only 11 reviews used a definition of physical activity. Physical activity outcome measures were reported in 22 reviews.
Conclusions
Better reporting of physical activity interventions is required to improve implementation. Research should include physical activity outcome measures across the stroke pathway. Determining which physical activity modes and parameters of each intervention would be useful in determining the optimal intervention for stroke survivors with different physical activity capacity levels.
Introduction
The lifetime risk of stroke has increased to one in four people [Citation1], with one-quarter of reported strokes reoccurring [Citation2]. One of the risk factors associated with stroke reoccurrence is the lack of physical activity (PA) post stroke [Citation3]. There is increasing interest in physical activity levels and implementation of physical activity interventions for people across the stroke pathway of care who have varying degrees of physical impairments and physical capacity levels [Citation2]. Physical activity levels, measured in steps per day, remain low in people with stroke, much less than a healthy older adult [Citation2]. The causes of low levels of physical activity post-stroke appear to be multifactorial. Stroke often leads to long term physical impairments such as limited mobility and movement. These impairments may result in difficulty engaging with physical activity [Citation4] and consequently the inability to adhere to physical activity guidance [Citation5].
Clinical guidelines are an essential bridge in translating advice on the effectiveness of a physical activity intervention into clinical practice. The United Kingdom (UK) stroke guidelines [Citation6,Citation7] encourage physical activity without referring specifically to changing physical activity behaviour in people with stroke. The most recent UK Stroke practice guidelines recommend that people with stroke should aim to be active every day and participate in physical activity unless there are contraindications [Citation6,Citation7]. The evidence underpinning the guidelines include primary studies only which focus on, strengthening interventions [Citation8], circuit class therapy [Citation9], cardiorespiratory fitness [Citation10], and aerobic exercise [Citation11]; all of which do not focus on physical activity promotion as a change in long term lifestyle.
The UK physical activity guidelines [Citation12] do not use evidence from the stroke population to inform their guidelines. The 2019 guidelines suggest analogous health benefits for disabled adults engaging in physical activity as for the rest of the adult population. This statement is based on a review completed for the UK Chief Medical Officers' (CMO) physical activity guidelines for disabled persons [Citation13]. These 2018 guidelines do not provide specific guidance for persons following a stroke and do not capture the evidence relevant to the stroke population.
Since the first seminal paper in 1953 by Morris [Citation14], which found an association between increased physical activity levels and reduced incidence of coronary events; the term physical activity has been used interchangeably with various other terms. Physical activity is defined as any movement produced by skeletal muscles resulting in energy expenditure [Citation15], and includes all physical activity done as part of daily living such as social and domestic activities, commuting, recreational and leisure activities [Citation16,Citation17]. Physical activity may or may not include exercise: exercise is a subset of physical activity that is planned, structured or repetitive [Citation16], with a purpose of improvement or maintenance of one or more components of physical fitness as an objective [Citation15]. Currently, there are four dimensions of physical activity, which are widely accepted [Citation18,Citation19]. These include mode or type of activity, frequency of performing activity, duration of performing activity, and intensity of performing activity. In addition, early physical activity research was largely uninformed by behaviour theory [Citation20]. Today, theories of behaviour change are essential to understand physical activity and provide an organizing framework underpinning effective physical activity interventions [Citation20]. Despite the terms of dimensions being widely accepted, there continues to be variation in physical activity terminology used within the literature and clinical guidelines, with most published studies being carried out as a subset of physical activity; for a specific purpose such as improving strength or cardiovascular fitness [Citation17] rather than physical activity promotion as a change in long term lifestyle.
There is an existing large body of work in the promotion of physical activity for the stroke population which demonstrates positive outcomes [Citation9,Citation21–26]. These studies focus on the effects on clinical endpoints such as mobility, function, and pain rather than changing physical activity behaviour as an outcome, of which there is less clarity. In addition, there remain complexities with regards to the reporting of evidence in the area. Poor reporting of heterogeneous and complex evidence as well as the absence of analysis using the latest implementation guidelines has made it difficult for evidence to be implemented into practice [Citation27–29].
Implementation is defined as the promotion and uptake of research findings and identifies ‘how to’ implement evidence to change healthcare practice. Work by Proctor et al. [Citation29] provides a set of guidelines by which the body of evidence would provide sufficient detail in order for it to be more easily implemented; these guidelines were used to guide the data extraction of the current scoping review; specifically naming, defining, and operationalizing strategies in terms of the following criteria: actor (provider of intervention), the action (intervention including definitions), action targets (population demographics, stroke pathway of care) and dose (physical activity dimensions and domains).
The lack of implementation and variation in reporting of this evidence across the stroke pathway warrants further investigation into the content of physical activity interventions. Therefore, a scoping review of systematic reviews within the area of physical activity and stroke is timely to learn more about these interventions, the terminology and outcome measures used and the key emerging themes from all the reviews that need some consensus building.
Our specific objectives are to:
Describe the focus of the reviews (aims, objectives, research questions, physical activity terminology used and theoretical description of the intervention)
Identify the overall level of reporting
Describe the actor (provider of intervention)
Describe the action (intervention including definitions), action targets (population demographics) and dose (physical activity dimensions and domains) across the stroke pathway of care (setting)
Identify physical activity intervention outcome measures (how these interventions were evaluated)
Identify key emerging themes, gaps and recommendations informing future research and clinical implementation
Methods
A scoping review was conducted to identify and describe available systematic review evidence on physical activity in the adult stroke population. The scoping review was reported using the Preferred Reporting Items for Systematic Reviews and Meta-analyses protocols extension for Scoping reviews (PRISMA-ScR) [Citation30]. The Scoping review methods followed the five steps outlined in the framework devised by Arksey and O’Malley [Citation31] and further developed by Levac et al. [Citation32] with additional reference to the recently updated Johanna Briggs Institute (JBI) scoping review guide [Citation33]. The published scoping review protocol is accessible here: https://www.tandfonline.com/doi/abs/10.1080/10833196.2020.1846237 and registered with the Open Science Framework (https://osf.io/vjfp4).
Eligibility criteria
This scoping review’s search and inclusion criteria were based on the dimensions and domains of physical activity outlined by Strath et al. [Citation19] ( and ).
Table 1. Physical activity dimensions: mode, frequency, duration, and intensity [Citation19] (a four section table outlining the definitions according to Strath et al. (2013) used to present information on dimensions of physical activity).
Table 2. Physical Activity Domains [Citation19] (A four section table outlining the definitions according to Strath et al. (2013) used to present information on domains of physical activity).
Study design was limited to systematic reviews, however within those reviews there were no restrictions on primary study design. Included reviews had been determined to be within the field of physical activity and included adults 18 years or older with a diagnosis of stroke. Language was limited to English. Reviews were not excluded based on population demographics such as severity of stroke, physical or cognitive impairment level, gender, variation of time since onset of stroke and settings. Reviews were included as being physical activity related if the core intervention(s) explicitly included a dimension and/or domain of physical activity approach or concept defined in and . Reviews were included if they had primary or secondary physical activity related outcome measures. Reviews that had combined specific rehabilitation (e.g., Constrained Induced Movement Therapy, Dual task training) and physical activity interventions and outcome measures, were only included if over 50% of the interventions were focused on physical activity (determined by research team).
Information sources
Comprehensive literature searches were defined and conducted with support from a research librarian. We searched the following electronic databases from inception until 1st June 2021: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, PsycInfo and Scopus. A set of keywords and Medical Subject Headings (MeSH) was used, related to physical activity and stroke, with search limits to systematic reviews or meta-analysis. The final search strategy for the MEDLINE database including limits is presented in Appendix 1. Additional search strategies are available from the corresponding author, upon request. Reference lists of all identified reviews were also hand searched for additional relevant reviews.
Selection of sources of evidence
Search results were imported into Covidence Systematics [Citation34], an online systematic review software system. 5% of the results titles and abstracts were assessed independently by two the research team (CMcF, KP) to pilot the suitability and clarity of the eligibility criteria [Citation33,Citation35]. The final list of titles and abstracts were divided among the core research team (100% CMcF, 50% NK, 50% KP) for screening using eligibility criteria, followed by a screen of full texts using the eligibility criteria. All screening was performed independently by two of three team members (100% CMcF, 50% NK, 50% KP), and discrepancies were resolved by consensus or involvement of a fourth team member (SMcD). Data was extracted electronically using Microsoft Excel software [Citation35] and supported by Covidence software [Citation34].
Data charting process
The data extraction and charting framework (Appendix 2) aligned to the research objectives [Citation32] were developed and subsequently piloted on a random sample of 10 included papers and modified as required based on feedback from the research team. Aligning with the research objectives, for each of the included reviews, the following data was extracted from the pooled reporting of the results:
Review details: title, citation, review aim and objective(s), review question(s), physical activity terminology or other terms used and the theoretical description underpinning the intervention
Review methods: actual inclusion/exclusion criteria, multi component or single, types of studies, number of studies and sample size.
Intervention characteristics (description of intervention, dimensions and domains of intervention and provider of the intervention and whether there was behaviour change associated with the intervention).
Population demographics across the stroke pathway of care (gender, age, severity of stroke, physical or cognitive impairment level, classification; acute, subacute, chronic, variation of time since onset of stroke and setting).
Intervention outcome measures used.
Recommendations and key points of review (emerging themes, gaps, recommendations for implementation approaches and areas where a consensus is required).
Full data extraction of each included review was completed by two team members (100% CMcF, 50% NK, 50% KP) independently (using Covidence), and subsequent consensus gained. Discrepancies were resolved by consensus or involvement of a fourth team member (SMcD). Where investigators published several reviews based on data from a single study population, the most recent or most complete review was selected for data extraction. Methodological quality or risk of bias of the included reviews was not completed, which is consistent with guidance on scoping review conduct [Citation33].
Data items
Intervention evaluation (outcome measures)
Evaluation of interventions; the outcome measures reported in the reviews were presented separately for the following: physical activity measures, sedentary behaviour and physical performance and physiological measures.
Outcome measures for physical activity levels (including sedentary behaviour) were identified, including subjective self-report (e.g. International Physical Activity Questionnaire, recall diary) and/or objective measurement using devices (e.g. pedometers, actigraphy, activity monitoring global positioning systems) [Citation16]. Physical performance and physiological measures and outcomes indicate potential physical activity capacity; however, they are not considered a measure of physical activity [Citation36]. Examples identified included walking capacity (6 m Walk Test MWT) and walking speed (10 m Walk Test MWT).
Theoretical descriptions underpinning the intervention
Theoretical descriptions underpinning the intervention were identified from the reporting/interpretation of the authors of each included review.
Data retrieval
Data were extracted directly from the results published from each review (e.g. the results pooled from the studies included in each systematic review). Primary study data was not analysed beyond what was reported within the systematic review. Basic descriptive values were collated in Microsoft excel to gain averages and ranges of values that were reported in the reviews (e.g. reporting of dimensions of physical activity, age of participants).
Analysis of results
The analysis of results included descriptive analysis of both quantitative and qualitative data. These descriptive results were then presented using a diagrammatic or tabular form and/or in a descriptive format that aligns with the objective(s) and scope of the review. Qualitative summary information was extracted directly from the discussion section of each included review. One of the research team (CMcF) synthesised and categorised this information under the following themes: gaps in the research and recommendations for implementation strategies. The research team discussed the themes and made group decisions on the categorisations.
Results
Results have been presented below based on the information included within the systematic reviews, which relate to this scoping review’s objectives. This is information extracted directly from each individual review which reflects the review authors interpretation of their included primary studies (i.e. the studies included in each original systematic review). Topic headings, clear explanations and level of reporting are provided aligned to each objective.
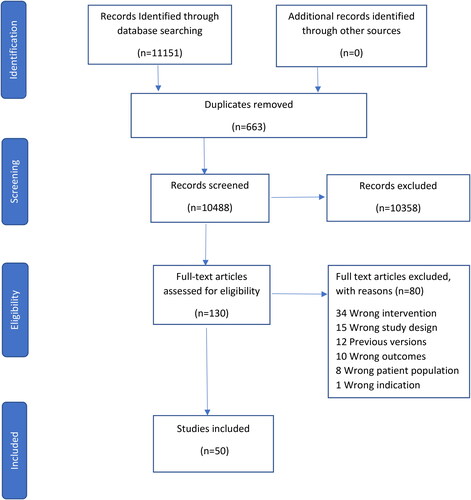
Results of the search
The electronic searches returned 11151 records. After removal of duplicates, 10488 titles and abstracts were screened against the inclusion criteria. In total, 130 records underwent full text review. 50 systematic reviews fulfilled the predefined inclusion criteria ( PRISMA flowchart). The reviews were published between 2014 and 2021 except for one review published in 2006 [Citation8]. Appendix 3 describes an overview of the 50 included systematic reviews.
Study designs
All 50 systematic reviews described whether study design was reported by their included primary studies (n = 935, mean n = 19 and range per review 3 to 103). Of these, 546 were RCT’s (58%), 191 primary study designs were not reported (21%), 77 primary studies were cross sectional (8%) and 35 primary studies were qualitative (4%). The remaining 86 studies were made up of other reported n = 41 (5%); retrospective n = 2, crossover n = 16, cohort n = 8, longitudinal n = 3, mixed methods n = 1, pilot n = 2, non-randomised, repeated measures n = 2, pre/post interventional n = 7 and other not reported n = 45 (5%).
Focus of the reviews
The focus of all reviews (n = 50) was consistent with an aim to change physical activity or a subset of physical activity. There was a broad set of aims, objectives and interventions across the scoping review that included anything pertinent to physical activity and stroke including reviews that focused on physical activity as day to day physical activity (n = 19); and reviews that focused on a subset (e.g. exercise) of physical activity (n = 31); the latter were usually carried out as part of a rehabilitation programme; 16 such reviews did not refer to the term physical activity within their text.
Physical activity terminology
Of the 50 reviews, 11 reviews defined physical activity (22%). Seven of these reviews referenced the Casperson 1985 definition; “Physical activity is defined as any bodily movements produced by the contractions of the skeletal muscles, that increase energy expenditure, such as those executed during leisure activities, at work, at home, or while travelling” [Citation15]. Three reviews did not reference their definition of physical activity, and within these there was little commonality. One additional review had an unreferenced definition specific to stroke [Citation37].
Theoretical description underpinning the intervention
Data on theories underpinning interventions was not dominant across the included reviews. 26% of reviews (n = 13) described whether behaviour change theories were reported by their included primary studies. Of those, behaviour change theories were not reported by the primary studies in 4 reviews. Of the remaining nine reviews that reported, there were four theories used to underpin a total of seven primary study interventions (Transtheoretical n = 4, Health belief n = 1, Social Cognitive Theory n = 1 and Health action n = 1). In addition, there were several broadly defined individual constructs of these theories (e.g. goal setting, action planning) targeted by intervention components described across 30 primary studies (of a total of 935).
Population demographics
Participant sex was reported in 30% of reviews (n = 15). The average percentage ratio of male and female participants ratio was 58:42. Participant age was reported in 70% (n = 35), the range was 48–75 (n = 21) and mean was 63 years (n = 20).
Time since onset of stoke
64% of reviews (n = 32) described whether the participants time since onset (TSO) of Stroke was reported by their included primary studies. 26 of 32 reviews reported the range (2.9- 89.3 months), five of these reviews also reported an average TSO (22 months).
Classification
40% of reviews (n = 20) described whether classification of participants in terms of acute, sub-acute and chronic was reported by their included primary studies. Of these 20 reviews, there were reviews that included a mix of classifications n = 11 and reviews that reported only one classification n = 7 (acute n = 1, chronic = 6). Of the 20 reviews, classifications were reported as follows: acute (n = 10), subacute (n = 4), chronic (n = 16).
Severity
28% of reviews (n = 14) described whether classification of participants in terms of stroke severity at baseline was reported by their included primary studies. How severity was measured also varied; the Barthel index (n = 6) as a measure of impairment to indicate severity, was the most reported (see ).
Table 3. Frequency of measures of impairment severity used by included systematic reviews (a two section table presenting descriptions of measurement of impairment and the numerical number of reviews aligned to each. Most instances occur for the Barthel index measurement).
Ambulatory status of participants
72% of reviews (n = 36) reported or implied ambulatory status. 92% of these reviews (n = 33) were based on ambulant participants. 22 reviews reported participants were ambulant, with 11 additional reviews implying the participants were of ambulant status. This implication was based on the requirements to undertake the intervention, i.e. walking intervention. Three reviews focused on non-ambulant participants specifically and five reviews stipulated a mix of all ambulatory statuses.
Cognitive impairment
49 of 50 reviews did not report on cognitive impairment level. One review reported participants were ‘able to communicate with investigators and follow a two-stage command’. One further review reported participants were ‘across the spectrum’ of cognitive impairment. Neither used a validated cognitive assessment. No review stipulated cognitive status within their inclusion/exclusion criteria.
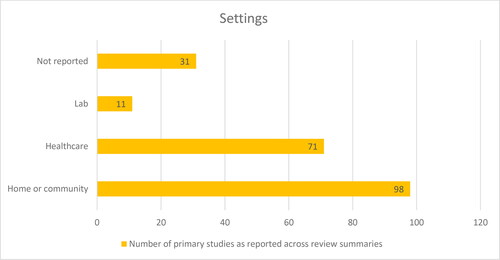
Setting
A similar number of reviews reported the setting (n = 23) as did not report it (n = 27). Of the 23 reviews that reported, a total of 211 primary studies were within those reviews (23% of overall primary studies). The most prevalent setting was in a home or community setting (n = 98 primary studies) rather than in a healthcare setting (see ).
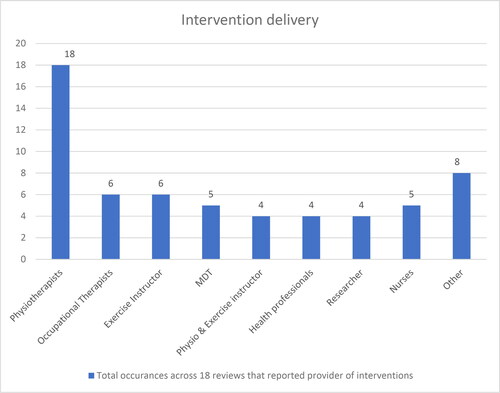
Intervention delivery
See for the number of occurrences across 18 reviews (36%) that reported the provider of interventions. Most instances occur for physiotherapists
Intervention characteristics
Physical activity dimensions: Mode, frequency, duration, and intensity (Strath et al. 2013)
There were 27 modes of physical activity interventions described across the 50 included systematic reviews (see ). Mode(s) were described in every review. The most prevalent included cycle ergometry (n = 11) and treadmill training (n = 10) (see ). For reviews that included general physical activity (n = 6), this was described as; time spent in activity and inactivity, multimodal lifestyle interventions including any type of exercise (aerobic, strengthening, progressive, tailored, group), or any type of activity aimed at improving a skill or ability.
Figure 4. Modes of physical activity interventions (A column chart plotting the description of the mode of physical activity and the number of reviews that reported for each mode. There is a wide range of modes presented with marginally most instances occurring in cycle ergometry).
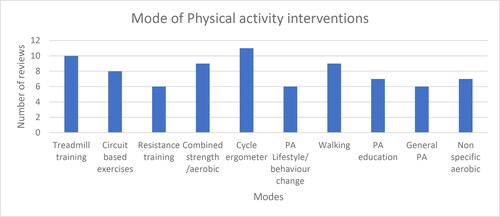
Figure 5. Reporting of frequency, duration and intensity of physical activity interventions (A bar chart plotting three dimensions of physical activity and the number of reviews that reported each dimension data. Significantly less instances occur for the dimension intensity).
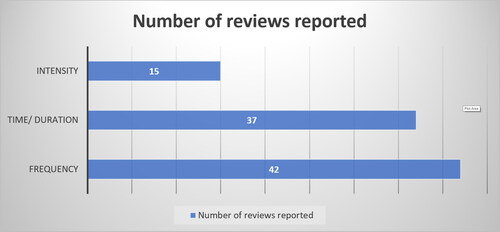
Figure 6. Most used self-reported physical activity outcome measures (A column chart plotting the description of self reported physical activity outcome measures and the number of reviews that reported for each. Most instances occurring for the Physical Activity Scale for the Elderly (PASE)).
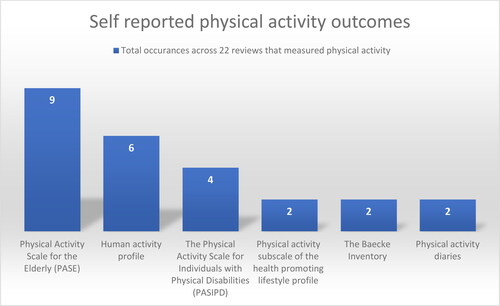
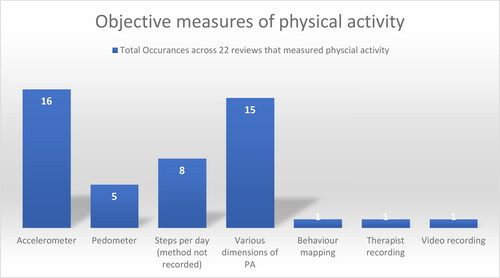
Figure 7. Most used objective physical activity outcome measures (A column chart plotting the description of device based physical activity outcome measures and the number of occurrences for each. Most instances occurring for Accelerometers).
Frequency was the most reported dimension of physical activity (see ) in 84% of reviews (n = 42). Time/duration was reported in 74% of reviews (n = 37). The intensity was the least reported dimension of physical activity in 30% of reviews (n = 15).
Physical activity domains
The domains in which physical activity occurred (i.e. occupational; work-related, domestic; housework, transportation; the purpose of going somewhere and leisure time; recreational activities) were not explicitly reported in any review. However, many could have been defined as leisure time as they consisted of an exercise or some other form of class.
Intervention evaluation (outcome measures)
Results of outcome measures used are presented separately for the following: physical activity measures, sedentary behaviour and physical performance and physiological measures.
Physical activity measures
Physical activity measures were reported in 44% of reviews (n = 22). Of those, there was a total of 36 types of outcomes measuring physical activity. There were 30 types of self-report measures reported including validated tools (see for most prevalent). Self-reported measures occurred 62 times across the 22 reviews that measured physical activity.
Objective measures of physical activity occurred 47 times across the 22 reviews that measured physical activity. There were six types of objective measures of physical activity reported e.g. accelerometers (n = 16 reviews) and pedometers (n = 5 reviews). Eight reviews reported physical activity measured as steps per day, although the device or method to measure was not reported. Behavioural mapping was reported in three reviews, therapist recording (n = 1) and video recording (n = 1); all of which were completed in inpatient settings. Various dimensions of physical activity were reported e.g. time spent in light intensity (n = 3); time spent in moderate -vigorous intensity (n = 4); change in number engaging in regular physical activity (n = 4); number meeting minimum requirements of physically activity for 30 mins/5 days a week (n = 2) and change from passive to active stage of physical activity (n = 2) (see ).
Sedentary behaviour
Three (6%) reviews [Citation2,Citation38,Citation39] defined sedentary behaviour as activities expending <1.5 metabolic equivalents (METs) and measured it via behavioural mapping, wearable devices, and questionnaires.
Physical performance and physiological measures
There was a total of 57 types of Physical Performance and Physiological outcome measures reported across the scoping review (n = 50). The most prevalent of these were 6MWT (n = 28), VO2 Peak/Max (n = 22), 10MWT (n = 21), BBS (n = 17), Timed Up and Go (n = 12), Heart rate (n = 6) and walking ability measured using the Holden functional ambulation category scale (n = 4).
Key emerging themes; gaps in the research and recommendations for implementation strategies
Each theme was explored with supporting text provided in and .
Table 4. Themes in relation to gaps in physical activity research (a three section table presenting descriptive information on seven themed gaps mapped from the results. Each themed gap has quotation text examples from the included reviews).
Table 5. A summary of the key findings of this review (a seven section table presenting descriptive summary information on the key findings from the results).
Summary of key findings
Discussion
We conducted a comprehensive scoping review that included a total of 935 primary studies within 50 systematic reviews. 58% of these primary studies were RCTs indicating a vastly growing evidence base in this area. In response to the low level of physical activity occurring in the stroke population, coupled with the large volume of research completed in this area, this scoping review mapped out the existing systematic review evidence to better understand the heterogeneity in reporting of research in this area, as well as the intervention content indicating emerging gaps and themes embedded throughout this discussion.
We used Proctor et al. [Citation29] implementation reporting guidelines like TIDieR (Template for Intervention Description and Replication) [Citation45] in terms of intervention detail but extracted additional implementation detail such as implementation outcomes affected. This reporting guideline was used to collate what is known and not known from the systematic review evidence. This included the focus, terminology, characteristics, and outcome measures used in the physical activity and post stroke body of knowledge. Our review has been successful in outlining where there are inconsistencies and gaps in the current research knowledge. Given there were no published reviews that focused on implementation of existing evidence, our findings in terms of implementation are more limited.
Focus of the reviews
Many reviews focused on a subset of physical activity (n=31) rather than day to day physical activity (n=19). In addition, a description of theories underpinning the interventions was lacking. There is extensive evidence that the most effective physical activity interventions are based on behaviour change that supports people to incorporate physical activity into their daily routines [Citation46]. From our scoping review there is emerging evidence that this applies also to people with stroke. Moore et al. (2018) [Citation42] outlined six trials that showed an increase in physical activity behaviour (very or quite promising). These interventions were explicitly designed to increase physical activity in daily living such as counselling-based physical activity promotion. Most reviews in this scoping review, however, are focused on a subset of physical activity intervention that do not include behaviour change. The reason for this remains unclear.
Future physical activity interventions and programmes should move away from repeating what is already known and from adopting strategies that are less likely to lead to sustainable behaviour change across the stroke pathway of care [Citation47].
Across the scoping review, only 11 reviews used a definition of physical activity: seven of those reviews referenced the well renowned Casperson 1985 definition [Citation15] and one review outlined a specific definition appropriate for those on the stroke pathway of care who were non-ambulant [Citation37] called ‘Adapted Physical activity (APA)’; “APA is a form of non-medical movement activity especially designed for individuals with specific health status alterations or chronic diseases. It is aimed to prevent disabilities mainly caused by immobility and to maintain residual motor skills (muscular tropism, joint flexibility, cardio-respiratory function, balance, ambulation, bone mass), bringing lifestyle changes”. Morris (2012) [Citation40] reported a variation in physical activity definitions across studies, however did not determine a definition within the review text. These results highlight the use of a physical activity definition is not prevalent in research for this population. This may be linked to the lack of reporting and clarity in defining physical activity intervention dimensions and domains across all of the stroke pathway (including varying levels of physical capacities) and population demographics. Future research should focus on which physical activity measures (i.e. self-reported, device-based measures) are most appropriately aligned to the various physical capacity levels of the stroke population.
Population demographics
There is an overall lack of reporting of key demographics, such as gender (30% reported); age (41% reported); classification (41% reported); severity (27% reported) and cognitive impairment (2% reported). As a result, we are unable to decide what works well and for whom, particularly for those with cognitive impairments which make up a pooled prevalence of 53.4% (16% with a major impairment) of the stoke population yet only considered in one review [Citation43,Citation48].
The 32 reviews that reported the participants time since onset of stroke indicated that although research is being conducted across the whole stroke pathway (range 2.9–89.3 months), the average participant was 22 months post stroke. Whilst most reviews were based on the ambulant population (n = 33), some research has been conducted with non-ambulant participants specifically (n = 3), again indicating the wide scope of research overall, however with a clear majority of ambulant participants.
The main provider of physical activity interventions is Physiotherapists and given that the context of these reviews is generating evidence rather than implementation, there is a need to review what is happening in clinical practice. The qualitative review summaries frequently highlight the need for increased support for stroke survivors to engage with physical activity, such as peer and professional support. In addition, the roles of non-therapy staff in physical activity promotion, and collaboration with other exercise providers in providing physical activity interventions has been explored. The resulting conclusion is that physical activity promotion, as part of an intervention, should be a generic skill across health care and does not belong to one profession. Positively, many studies reported research being conducted in a home or community setting enhancing the likelihood of their findings being implementable.
Intervention characteristics and intervention evaluation (outcome measures)
27 modes of physical activity interventions were described across the scoping review, indicating a range of domains that could be implemented with this population. The most used mode (cycle ergometry) which in terms of current physical activity definition, is not considered a day-to-day activity. The most prevalent mode that people can fit into daily activities was walking (n = 11) and is therefore not implementable for the 20% of the stroke population who are non-ambulant [Citation49,Citation50].
There has been a predominance of studies measuring physical function and physical capacity (n = 31) without also then measuring how these translate into day to day increases in physical activity. This would suggest that those delivering the interventions (mainly physiotherapists), may have challenges implementing physical activity interventions and/or measuring their outcomes across the stroke pathway of care. There is a current gap in knowing what these challenges are in current practice. However, this trend is starting to change with more recent reviews also including self-report and device-based measures of physical activity which can inform both on the domains in which physical activity takes places and its dimensions. Physical activity dimensions such as intensity in relation to physical capacity levels need to be defined, measured, and clearly reported to determine the optimum dose (and guidelines) for specific stroke capacity levels. Additionally, a consensus is required to determine terminology when describing physical capacity levels i.e. ambulation, severity, classification, weakness.
Limitations of the review
There are some limitations of this review. All non-English studies were excluded from the search strategy which may have led to incomplete synthesis of data in this area. Heterogeneity in reporting of reviews also made the interpretation of results challenging. Due the nature of this review, the authors did not go to the original papers for raw data if it was not reported within the systematic review. As the aim of this review was to look at a wide breadth of literature, reviews were included regardless of quality. Although the search strategy did not include implementation as a key term, a subsequent use of a more comprehensive framework such as the Consolidated Framework for Implementation Research (CFIR) [Citation51] may have extracted more implementation detail. Given the volume and value of the information retrieved within this review, there is an opportunity for future research to follow on from this and include such implementation detail.
Conclusion
Better reporting of physical activity interventions is required to allow implementation and a clear focus for future research. In addition, future research should include physical activity outcome measures to measure the effects of different physical activity interventions across the stroke pathway. Determining which physical activity modes of interventions and establishing the physical activity parameters of each intervention would be useful in determining the optimal intervention for stroke survivors with different physical activity capacity levels and at each stage of the stroke pathway. Defining physical activity, specific to the stroke population, is uncommon and therefore an appropriate definition should be determined which aligns to the various physical capacity levels of the stroke population. Research into clinician knowledge and routine practice of physical activity promotion and its outcomes should be completed in the first instance as a starting point of implementation.
Disclosure statement
The authors report there are no competing interests to declare.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Feigin V, Brainin M, Norrving B, et al. World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18–29.
- Fini N, Holland A, Keating J, et al. How physically active are people following stroke? Systematic review and quantitative synthesis. Phys Ther. 2017;97(7):707–717.
- Chaturvedi S, Turan T, et al. reviewing Neurology 2016. The Importance of Physical Activity in Preventing Recurrent Stroke. 2017. Available at https://www.jwatch.org/na43192/2017/01/04/importance-physical-activity-preventing-recurrent-stroke. (Accessed 02/04/20)
- National Audit Office. Reducing brain damage: faster access to better stroke care. 2005. London: NAO.
- Fletcher S, Kulnik ST, Demain S, et al. The problem with self-management: problematising self-management and power using a foucauldian lens in the context of stroke care and rehabilitation. PLoS One. 2019;14(6):e0218517. Gordon N, Gulanick M, Costa F, American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council, et al. Physical activity and exercise recommendations for stroke survivors. A scientific statement from the American heart association. Circulation. 2004;109(16):2031–2041.
- National Institute for Clinical Care and Excellence (NICE). Stroke rehabilitation: long term rehabilitation after stroke. 2013. Clinical guideline 162. Retrieved from http: https://www.nice.org.uk/guidance/cg162/evidence/full-guideline-pdf-190076509.
- Royal College of Physicians (RCP). National clinical guideline for stroke. 2016. Retrieved from https://www.strokeaudit.org/Guideline/Full-Guideline.aspx.
- Ada L, Dorsch S, Canning CG. Strengthening interventions increase strength and improve activity after stroke: a systematic review. Aust J Physiother. 2006;52(4):241–248.
- English C, Hillier SL. Circuit class therapy for improving mobility after stroke. London, United Kingdom: Cochrane Database of Systematic Reviews, 2010. CD007513.
- Marsden DL, Dunn A, Callister R, et al. Characteristics of exercise training interventions to improve cardiorespiratory fitness after stroke: a systematic review with Meta-analysis. Neurorehabil Neural Repair. 2013;27(9):775–788.
- Kendall BJ, Gothe NP. Effect of aerobic exercise interventions on mobility among stroke patients: a systematic review. American Journal of Physical Medicine & Rehabilitation. 2016;95(3):214–224.
- UK Chief Medical Officers’ (CMO). Physical Activity Guidelines. 2019. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf.
- UK Chief Medical Officers’ (CMO). Physical Activity for general health benefits in disabled adults. 2018. Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/748126/Physical_activity_for_general_health_benefits_in_disabled_adults.pdf.
- Morris JN, Heady JA, Raffle PAB, et al. Coronary heart disease and physical activity of work. Lancet. 1953;262(6796):1111–1120.
- Caspersen C, Powell K, Christenson G. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131.
- Marley J. Improving the effectiveness of physical activity and exercise interventions in the management of low back pain (E-pub ahead of print). International Society for the Study of the Lumbar Spine: Lumbar Spine Online Textbook. Maryland, United States: Wheeless Texbook of Orthopaedics, Section 10. 2018.
- Rausch Osthoff AK, Niedermann K, Braun J, et al. EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(9):1251–1260.
- Kohl H, Murray T, Salvo D. Foundations of physical activity and public health. 2019. 2nd Ed. Champaign, United States: Human Kinetics.
- Strath S, Kaminsky L, Ainsworth B, American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health and Cardiovascular, Exercise, Cardiac Rehabilitation and Prevention Committee of the Council on Clinical Cardiology, and Council, et al. Guide to the assessment of physical activity: clinical and research applications. A scientific statement from the American heart association. Circulation. 2013;128(20):2259–2279.
- Rhodes RE, McEwan D, Rebar AL. Theories of physical activity behaviour change: a history and synthesis of approaches. Psychol Sport Exercise. 2019;42:100–109.
- Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2020;3:CD003316.
- Lynch E, Jones T, Simpson D, on behalf of the ACTIOnS Collaboration, et al. Monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst Rev. 2018.
- Barclay R, Stevenson T, Poluha W, Cochrane Stroke Group, et al. Interventions for improving community ambulation in individuals with stroke. Cochrane Database Syst Rev. 2015.
- Lawrence M, Celestino F, Jr Matozinho H, Cochrane Stroke Group, et al. Yoga for stroke rehabilitation. Cochrane Database Syst Rev. 2017;2017(12):1465–1858.
- Laver K, Schoene D, Crotty M, Cochrane Stroke Group, et al. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2013;(1):1465–1858.
- Vloothuis J, Mulder M, Veerbeek J, Cochrane Stroke Group, et al. Caregiver‐mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev. 2016;2016(12):1465–1858.
- Kim Y, Byron Lai MS, Mehta T, et al. Exercise training guidelines for multiple sclerosis, stroke, and parkinson disease. Am J Phys Med Rehabil. 2019;98(7):613–621.
- Morris J, Bernhardsson S, Bird M, et al. Implementation in rehabilitation: a roadmap for practitioners and researcher. Disability Rehabilitation. 2020;42(22):3210–3265.
- Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-447ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Intern J Social Res Method. 2005;8(1):19–32.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
- Peters M, Marnie C, Tricco A, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126.
- Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org.
- Microsoft Corporation. 2018. Microsoft Excel. Retrieved from https://office.microsoft.com/excel.
- Portegijs E, Karavirta L, Saajanaho M, et al. Assessing physical performance and physical activity in large population-based aging studies: home-based assessments or visits to the research Centre? BMC Public Health. 2019;19(1):1570.
- Belfiore P, Miele A, Gallè F, et al. Adapted physical activity and stroke: a systematic review. J Sports Med Phys Fitness. 2018;58(12):1867–1875.
- English C, Manns PJ, Tucak C, et al. Physical activity and sedentary behaviors in people with stroke living in the community: a systematic review. Phys Ther. 2014;94(2):185–196.
- Kringle EA, Barone Gibbs B, Campbell G, et al. Influence of interventions on daily physical activity and sedentary behavior after stroke: a systematic review. PM&R. 2020;12(2):186–201.
- Morris J, Oliver T, Kroll T, et al. The importance of psychological and social factors in influencing the uptake and maintenance of physical activity after stroke: a structured review of the empirical literature. Stroke Res Treat. 2012;2012:195249.
- Thilarajah S, Mentiplay B, Bower K, et al. Factors associated with Post-Stroke physical activity: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(9):1876–1889.
- Moore S, Hrisos N, Flynn D, et al. How should long-term free-living physical activity be targeted after stroke? A systematic review and narrative synthesis. Int J Behav Nutr Phys Act. 2018;15(1):100.
- Barbay M, Diouf M, Roussel M, GRECOGVASC study group, et al. Systematic review and Meta-analysis of prevalence in post-stroke neurocognitive disorders in hospital-based studies. Dement Geriatr Cogn Disord. 2018;46(5-6):322–334.
- Nicholson S, Sniehotta FF, van Wijck F, et al. A systematic review of perceived barriers and motivators to physical activity after stroke. Int J Stroke. 2013;8(5):357–364.
- Hendrickx W, Vlietstra L, Valkenet K, et al. General lifestyle interventions on their own seem insufficient to improve the level of physical activity after stroke or TIA: a systematic review. BMC Neurol. 2020;20(1):168.
- Heath G, Parra D, Sarmiento O, et al. Evidence-based intervention in physical activity: lessons from around the world. The Lancet. 2012;380(9838):272–281.
- Ding D, Ramirez Varela A, Bauman AE, et al. Towards better evidence-informed global action: lessons learnt from the lancet series and recent developments in physical activity and public health. Br J Sports Med. 2020;54(8):462–468.
- Sexton E, McLoughlin A, Williams DJ, et al. Systematic review and meta-analysis of the prevalence of cognitive impairment no dementia in the first year post-stroke. Eur Stroke J. 2019;4(2):160–171.
- Kwah LK, Harvey LA, Diong J, et al. Models containing age and NIHSS predict recovery of ambulation and upper limb function six months after stroke: an observational study. J Physiother. 2013;59(3):189–197.
- Veerbeek JM, Van Wegen EE, Harmeling-Van der Wel BC, for the EPOS Investigators, et al. Is accurate prediction of gait in nonambulatory stroke patients possible within 72 hours post stroke?: the EPOS study. Neurorehabil Neural Repair. 2011;25(3):268–274.
- Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50.