?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Musculoskeletal conditions such as spinal pain and osteoarthritis are among the leading causes of years lived with disability worldwide. With the COVID-19 pandemic forcing many healthcare providers to change the way in which care for chronic conditions is delivered, telehealth is an alternative to face-to-face consultations that can be used for both assessment and provision of therapy and support.
Objectives
To identify, appraise and synthesise findings from all randomised controlled trials (RCTs) that compared telehealth to face-to-face consultations for patients with any type of musculoskeletal condition.
Methods
Systematic review and meta-analysis. We used the GRADE approach to assess the quality of evidence related to all outcomes. We searched three electronic databases (PubMed, Embase, CENTRAL), clinical trial registries and citing-cited references of included studies.
Results
Five RCTs were includable: one in patients with osteoarthritis of the knee, one in patients with osteoarthritis of the knee or hip in preparation for a total joint arthroscopy and three after total knee replacement. Telehealth was conducted by video in four trials and by phone in one. A total of 402 participants were analysed across the five trials. There were no significant differences in pain outcomes (WOMAC) between telehealth and face-to-face therapy immediate post-intervention (mean difference (MD): 0.12 (95% CI −2.3 to 2.6, p = .92) or two months post-intervention (MD): 1.2, (95% CI: −2.7 to 5.1, p = .55). Similarly, outcomes related to function, quality of life and satisfaction were comparable between the two modes of delivery immediate post-intervention, with no significant differences reported.
Conclusion
There is limited low quality evidence that there is no significant differences between telehealth-based delivery of rehabilitation to patients with osteoarthritis or following knee surgery and face-to-face therapy for pain, function, quality of life and satisfaction. These findings should be should be interpreted with caution due to the small number of included studies and small sample size.
HIGHLIGHTS
Findings based on a small number of trials and very low-quality evidence suggest that there is no difference between telehealth and face-to-face consultation for rehabilitation for adults post-knee surgery.
Outcomes related to pain, function and quality of life were comparable between the two modes of delivery.
There is a significant gap in knowledge relating to cost outcomes, warranting studies that further evaluate cost-effectiveness of telehealth and the subsequent long-term sustainability of telehealth.
Introduction
Musculoskeletal conditions such as spinal pain and osteoarthritis are among the leading causes of years lived with disability worldwide [Citation1]. These often chronic conditions are associated with significant impact on the individual, due to pain and reduced function, and society due to work absenteeism and reduced work productivity. Musculoskeletal conditions are also associated with substantial financial costs [Citation1]. According to 2008/2009 data, in Australia, musculoskeletal conditions accounted for 9% of health care expenditure, making them the fourth most costly health condition, behind cardiovascular, oral health and mental disorders [Citation1]. Treatment is the dominant component of this expenditure which includes hospital admitted patient services (e.g. joint replacements), out of hospital expenses (e.g. outpatient clinics) and pharmaceuticals (e.g. pharmaceutical benefits scheme) [Citation2]. Guideline management for most musculoskeletal conditions begins with advice, condition-specific education and exercise [Citation2, Citation3]. Surgical treatment options such as joint replacement surgery for knee or hip osteoarthritis should only be considered following conservative management and when symptoms are no longer responsive to noninvasive approaches [Citation3]. With the prevalence and treatment costs of musculoskeletal conditions increasing, there is growing recognition for the need to identify effective treatment options that enable timely and equitable access to services irrespective of location, accessibility or public health policies, such as lockdowns or quarantine, in response to COVID-19 [Citation4].
Telehealth is a promising mode of health service delivery that may increase access to health services. Telehealth includes telephone and videoconferencing to provide healthcare at a distance [Citation5], and provides an alternative to face-to-face consultations for both assessment and the provision of healthcare and support. The main benefits of telehealth for both patients and health care professionals are access and convenience [Citation5]. Several systematic reviews have evaluated the effectiveness of telehealth for the assessment and management of musculoskeletal conditions [Citation6–8]. These reviews suggest telehealth is effective for improving function for people with osteoarthritis and following joint replacements (hip and knee arthroplasty) [Citation8, Citation9]. For chronic low back pain moderate quality evidence suggests that telehealth is not superior to minimal interventions (i.e. patient education) for reducing pain, disability or function in the short or medium term [Citation7]. Compared to control, three trials found telehealth to be superior for improving quality-of-life in people with back pain of any duration (ranging between immediate post- and 12 months post-intervention) [Citation7]. These findings, however, have several limitations related to their recency, quality and quantity of studies included and none have evaluated the cost-effectiveness of telehealth in comparison to standard face-to-face consultations.
With the recent COVID pandemic, telehealth has been a pivotal tool facilitating medical treatment when in-person contact was restricted. Given the current rapid increase in telehealth delivery, an updated, comprehensive systematic review that synthesises estimates of treatment effectiveness from randomised controlled trials (RCTs) is warranted to inform and guide the delivery of physiotherapy healthcare services. Therefore, the aim of this systematic review was to identify evidence for the effectiveness of telerehabilitation for the management of patients with musculoskeletal conditions in terms of pain, function, quality of life, satisfaction and costs as compared to conventional face-to-face rehabilitation. We used the GRADE approach to assess the quality of evidence related to all outcomes.
Methods
This systematic review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Citation10] and the review protocol was developed prospectively. Any deviations from the protocol are reported in the relevant methods section.
Inclusion and exclusion criteria
Study designs
We included RCTs of any design (i.e. individual, cluster, factorial, crossover). All other primary study types (e.g. controlled nonrandomised studies, qualitative studies and observational studies) and reviews, were excluded.
Population
Studies were included if their populations of interest comprised individuals of any age or gender, diagnosed with any type of musculoskeletal condition. This included post-operative rehabilitation.
Interventions
Therapy interventions involving a synchronous telehealth component (i.e. involving real-time communication) via either phone or video, were included. Studies examining novel treatments for rehabilitation (i.e. experimental interventions for musculoskeletal care that were considered outside of standard care), as well as asynchronous data transfer (e.g. E-mail), virtual reality software, automated feedback, web-based modules or specialised online apps were excluded. Studies were included if they involved care provision by a physiotherapist (physical therapist) or occupational therapist. Studies which involved patients consulting a specialist (i.e. orthopaedic surgeon), were excluded. The focus of this review was on primary health care providers in the community.
Comparators
We included studies with a comparable (i.e. similar or equivalent frequency and duration of therapy) face-to-face comparator or telehealth comparator (i.e. video intervention with telephone comparator). Any comparator that involved a wait-list control or clinically inequivalent active comparator was excluded, as these interventions were considered too dissimilar to the telehealth interventions investigated.
Outcomes
The primary outcomes were pain and function scores, and secondary outcomes were quality of life, patient satisfaction and costs of therapy. Outcomes were grouped by time points, i.e. immediate post-intervention, and short-term impact (two months post-intervention). See Appendix A for scales used to measure outcomes of interest.
Search strategy
Electronic databases, including PubMed (via MEDLINE), Embase (via Embase) and CENTRAL (via the Cochrane Library) were searched for potentially relevant primary studies from inception until 18 November 2020. The search string was translated for use in other databases using the Polyglot Search Translator [Citation17]. Complete search strategies are provided in Appendix B. The searches were deliberately broad, as the present review was conducted as part of a series of systematic reviews on the effectiveness of telehealth compared to face-to-face for healthcare provision in primary care and allied care.
Other searches
In addition, a backward and forward citation search of the included studies was undertaken using the Scopus database on the 15 December 2020 to identify any further relevant studies. Clinical registries (clinicaltrials.gov and WHO ICTRP) were searched on 25 March 2021. Search strategies are provided in Appendix B.
Restriction on publication type
No restrictions by language or publication date were applied. Only published trials that were available in the full text were considered for inclusion. Studies published as abstract only (e.g. conference abstract) with no additional results information available (e.g. from a clinical trial registry record) were excluded.
Screening and data extraction
Paired authors (NK, HG, RP, MC, AMS, JC, PG) independently reviewed all titles and abstracts identified by the electronic search against the inclusion criteria. One author (JC) retrieved full-text for includable conditions and two authors (NK, RP) screened the full-texts for inclusion. Disagreements were resolved by consensus or referral to a third author, when necessary. Paired authors (NK, RP, MC) independently extracted data from all eligible trials using three data extraction forms: Table of Characteristics form, Primary and Secondary Outcomes data form and Risk of Bias form. Any discrepancies were resolved by discussion or by reference to a third author (see Box 1).
Box 1 List of extracted information
Methods: Study authors, location, study design, duration of follow-up
Participants: n, age (mean), musculoskeletal condition
Interventions: telehealth care
Comparators: equivalent face-to-face care or telehealth comparator
Primary and secondary outcomes: pain, function, quality of life, patient satisfaction and costs of therapy
Risk of bias
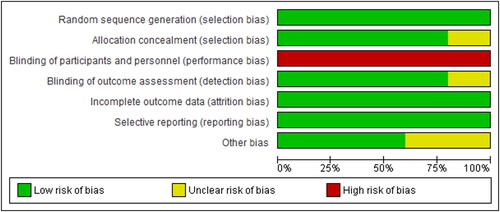
Two authors (NK, MC) independently assessed the risk of bias for each included trial using the Cochrane Collaboration’s Risk of Bias tool 1 [Citation18]. We used Cochrane Risk of Bias Tool 1 rather than Tool 2, as Tool 1 allows for the assessment of biases arising from study funding and conflict of interest (under domain 7, other bias). The following domains were assessed as either ‘high’, ‘low’ or ‘unclear’: method of random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other bias (assessing biases from conflict of interest and funding issues). All disagreements were resolved by consensus.
Assessment of evidence using GRADE (grading of recommendations, assessment, development and evaluations) analysis
Although we had not pre-specified this in the protocol, two authors (NK, ZAM) independently assessed each outcome using the GRADE approach, to provide further understanding around the quality of evidence being evaluated for each comparison and at each time point [Citation19]. Five domains were evaluated: risk of bias, inconsistency, indirectness, imprecision and publication bias. The consensus was sought between authors and reached for each domain’s direction and strength. All RCTs in this review were initially designated as high quality. After evaluating the principal domains, a summarizing degree of the evidence was arrived at (Appendix C)
A summary of GRADE assessments for each outcome are provided in the results. The definitions of the quality levels are presented below:
High
Very confident that the true effect lies close to the estimate of the effect.
Moderate
Moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low
Confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect.
Very low
Very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect [Citation20–22].
Statistical analysis
Review Manager 5.4 was used to calculate the effect of interventions [Citation23]. A meta-analysis was conducted where data were sufficient to pool (i.e. 2 or more trials reporting on the same outcome). For all outcomes (i.e. pain, function, quality of life), the results are presented as mean differences or standardised mean differences. We used a random effects model, in anticipation of considerable heterogeneity. Statistical heterogeneity was assessed using the I2 statistic.
The individual was used as the unit of analysis, where possible. However, where data on the number of individuals with primary and secondary outcomes of interest was not available, we extracted the information as it was presented (e.g. mean scores for the differences between groups). We did not contact investigators or study sponsors to provide missing data.
A funnel plot was not created, as fewer than 10 studies were included in the analysis. Subgroup analyses were conducted according to duration of follow-up.
As none of the included studies were graded at ‘high’ risk of bias in three or more domains, a pre-specified sensitivity analysis assessing the impact of excluding trials rated at high risk of bias for three or more domains, was not conducted.
Results
Search results
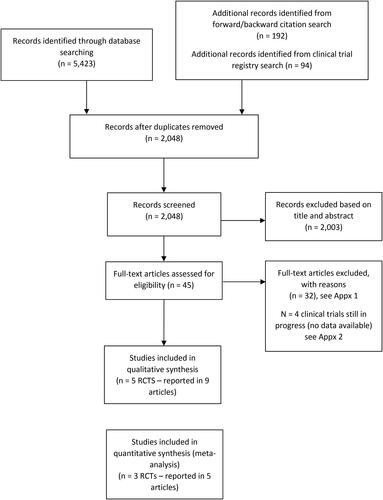
The electronic search retrieved 5423 references, supplemented with 192 references from forward and backward citations of the included studies and 94 records identified from the clinical trial registry search, resulting in 2048 records to screen after deduplication. Screening these on title and abstract excluded 1719 references, leaving 329 articles for which we obtained full-text. Screening of these full texts excluded another 316 which left five RCTs (reported in nine articles) for inclusion in this systematic review (see ). Reasons for exclusions are reported in Appendix D. We identified four potentially relevant clinical trials that are currently in progress, these are listed in Appendix E.
Figure 1. A PRISMA flow diagram that summarises the screening process. It shows the number of articles found at different stages of the systematic review search, and the total number included in the review.
Characteristics of the five included trials are presented in . A total of 402 participants were analysed across the five trials. Three trials were conducted in Canada [Citation24–27, Citation31, Citation32], and one each in Australia [Citation29, Citation30] and Nigeria [Citation28]. Four trials focused on patient rehabilitation (or prehabilitation) in preparation for knee arthroplasty as a result of significant osteoarthritis [Citation25–32]. One trial included a mixed population of people with hip and knee osteoarthritis who were awaiting joint replacement surgery [Citation24]. In all trials, rehabilitation comprised prescribed exercise programs delivered by physiotherapists. All five trials compared conventional therapy in clinic settings (face-to-face) versus the home or clinic-based treatment rooms for telehealth interventions; no trial compared the different modes of telehealth delivery. Telehealth was conducted by video in four trials [Citation24–27, Citation29–32], and by phone in one trial [Citation28].
Table 1. Characteristics of included studies.
Risk of bias
Overall, the included trials were mostly of low or unclear risk of bias. In particular, random sequence generation, incomplete outcome data and selective reporting were at low risk of bias for 100% of the trials. Due to the nature of the interventions (telephone or video vs. face-to-face), blinding of the patients and health care providers was not possible, resulting in a high risk of performance bias for all trials. Allocation concealment, blinding of outcome assessment and other biases were generally at low risk of bias, however, some trials were rated at unclear risk of bias, due to nonreporting ().
Primary outcomes
Pain outcomes – WOMAC pain
Three trials reported data on this outcome – two were able to be meta-analysed [Citation24, Citation25] (), and one narratively summarised [Citation29, Citation30].
Figure 3. Forest plot comparing telehealth vs. face-to-face therapy on pain outcomes using the WOMAC for musculoskeletal conditions.
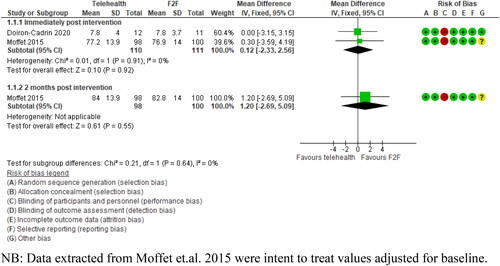
There were no significant differences in pain outcomes between telehealth and face-to-face therapy immediate post-intervention (221 participants, mean difference (MD): 0.12 (95% CI −2.33 to 2.56, p = .92) or two months post-intervention (198 participants, MD: 1.2, 95% CI −2.69 to 5.09, p = .55). The quality of evidence for both pain outcomes (immediate post-intervention and two months post-intervention) was very low (downgraded due to indirectness and imprecision).
Russell et al. (2011) explored the impact of telehealth on WOMAC pain scores, however, reported mean differences pre- and post-rehabilitation for intervention groups. Following the intervention, the telehealth group achieved outcomes comparable to those of the conventional rehabilitation group in the WOMAC pain subscale with no significant differences observed. Mean differences before and after treatment were reported as 2.97 (SD: 2.31) in telehealth vs. 2.19 (SD: 1.76) in face-to-face groups.
Function outcomes – WOMAC function
Three studies reported data on this outcome – two were able to be meta-analysed [Citation24, Citation25], and the remaining one summarised narratively [Citation29] ().
Figure 4. Forest plot comparing telehealth vs. face-to-face therapy on function outcomes using the WOMAC for musculoskeletal conditions.
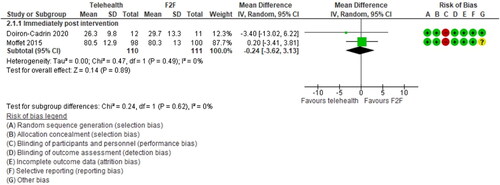
There were no significant differences in function outcomes between telehealth and face-to-face therapy immediate post-intervention (221 participants, mean difference: −0.24, 95% CI −3.62 to 3.13, p = .89). The quality of evidence for function outcomes was very low (downgraded due to indirectness and imprecision).
At two months post-intervention, Moffet et al. reported no significant differences between telehealth and face-to-face therapy for function outcomes (198 participants, mean difference: 1.0, 95% CI −2.61 to 4.61, p = .59).
Russell et al. (2011) reported that both the telehealth and the face-to-face groups had clinically important improvements in the WOMAC function scale (within-group change, i.e. comparing baseline to post-intervention), however, the differences between the two groups were not significant. Mean differences pre- and post-intervention for each group were reported as 3.52 (SD: 2.35) for telehealth and 2.45 (SD: 1.84) for conventional rehabilitation.
Secondary outcome
Quality of life (overall)
Moffet et al. (2015) reported an overall quality of life score using the KOOs scale. There were no significant differences between groups at the post-intervention time point: mean difference = 2.60 (95% CI: −2.67 to 7.87, p = .33) or the two-month follow-up: mean difference = 0.50 (95% CI: −4.77 to 5.77, p = .85). The quality of evidence for both qualities of life outcomes (immediate post-intervention and two months post-intervention) was very low (downgraded due to indirectness and imprecision).
Quality of life – physical component
Two trials reported data on quality-of-life outcomes, separated into physical and mental components and could be pooled (Doiron-Cadrin et al. 2020, Odole and Ojo 2014) ( and ).
Figure 5. Forest plot comparing telehealth vs. face-to-face therapy on Quality of Life physical composite outcomes using the SF-36 and the WHO QoL-Bref scales.
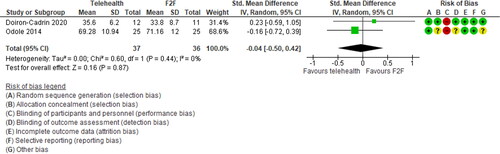
Figure 6. Forest plot comparing telehealth vs. face-to-face therapy on Quality of Life mental composite outcomes using the SF-36 and the WHO QoL-Bref scales.
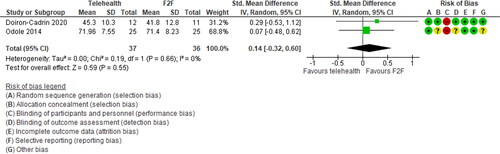
Two trials provided relevant data on the quality of life – physical composite outcome (total participants, n = 73). There was no difference between telehealth and face-to-face groups; standardised mean difference was: −0.04 (95% CI: −0.5 to 0.42, p = .87). The quality of evidence for the quality of life - physical outcome was very low (downgraded due to indirectness and imprecision).
Quality of life – mental component
For the quality of the life-mental component score, we identified two trials, involving a total of 73 participants. We did not find evidence of a difference between the two treatments in this comparison, standardised mean difference was 0.14 (95% CI: −0.32 to 0.6, p = .55). The quality of evidence for the quality of life-mental outcome was very low (downgraded due to indirectness and imprecision).
Satisfaction
Patient’s satisfaction with the mode of therapy received was evaluated in two studies: Moffet et al. 2017 and Tousignant et al. (2011) [Citation26, Citation32]. Moffet et al. (2017) reported that two months post-intervention, there were no reported significant differences in satisfaction between groups relating specifically to the delivery of services (telehealth: n = 78, mean 84.6 (SD: 11.9), p = .38 vs. F2F: n = 96, mean 85.8 (SD: 13.3), p = .38) [Citation26]. Similarly, Tousignant et al. (2011) reported that immediate post-intervention, there was no clear evidence of a significant difference in perceived satisfaction with the services delivered between groups p = .721 (telehealth: n = 22, mean 86 (SD: 15.2) vs. F2F: n = 20, mean 84 (SD: 18.1)) [Citation32]. The quality of evidence for satisfaction outcomes (immediate post-intervention and two months post-intervention) was very low (downgraded due to indirectness and imprecision).
Costs
One trial reported on the costs of in-home rehabilitation post-TKA via telehealth compared to conventional face-to-face therapy, using a real total cost analysis [Citation27]. The mean total cost of total treatment from the perspective of the healthcare system (including all received and cancelled treatments) was significantly lower in the telehealth group than the face-to-face group (CAD$1,224 (SD: 241) telehealth vs. CAD$1,487 (SD: $553), MD: −263, 95% CI: −382 to −143, p = <.001)(Years costed: 2008–2013). Similarly, the reported mean cost per single treatment for the telehealth group was significantly lower CAD $80.99 (SD: 26.60) compared to CAD $93.08 (SD: 35.70) for the face-to-face group (p = .008).
Discussion
This systematic review of five RCTs suggests that there is no difference in effectiveness between telehealth rehabilitation for knee and hip osteoarthritis compared to conventional in-person rehabilitation delivered face-to-face. Outcomes related to pain, function and quality of life were comparable between the two modes of delivery. Overall, these findings are based on a small number of trials and very low-quality evidence (downgraded for indirectness and imprecision). This suggests that the evidence available is very uncertain about the effectiveness of telehealth on pain, function, quality of life and costs and these findings should be interpreted with caution.
Our review provides an up-to-date, high-quality synthesis of the effectiveness of telehealth as a treatment option for musculoskeletal conditions. While the finding of our review generally align with those of Cottrell et al. (2017) Pietrzak et al. (2013), Dario et al. (2017) and Pastora-Bernal et al. (2017), the methods used in these previous reviews (specifically, inclusion of cohort studies) are likely to influence the estimates of treatment effect and strength of conclusions made by these reviews. By synthesising RCTs alone and through applying the GRADE criteria the findings of this review cast much greater uncertainty over the effectiveness of telehealth compared to face-to-face consultations for musculoskeletal conditions. Our review also identified and analysed two recent publications that were not considered in previously published reviews. Further high-quality trials with large sample sizes are required to improve the certainty of evidence and therefore our confidence in the effectiveness of telehealth for managing musculoskeletal conditions. Accurate reporting of both the size of the effect of an intervention on an outcome and the certainty of evidence is critically important as it is this information that is then used by clinicians, healthcare services and governments to inform practice and guide the allocation of already scarce funds and resources.
The COVID-19 pandemic has forced many healthcare providers to change the way in which care is delivered. Findings of this review suggest no difference between telehealth and face-to-face consultation for rehabilitation for adults post-knee surgery, and further evaluation may be an alternative mode of delivery for patients with musculoskeletal conditions. However, from a practical and policy perspective there is a need for increased guidance, recommendations and training for physiotherapists around the optimal delivery of telehealth interventions [Citation33, Citation34]. In response to this demand, professional organisations and governing bodies including the Australian Health Practitioner Regulation Agency (AHPRA) and the Australian Physiotherapy Association have developed guidelines to assist with the delivery of telehealth interventions, facilitated education and training in its use [Citation35, Citation36]. The pandemic and the need for alternative treatment approaches have also incited responsive changes to remuneration for healthcare providers, with telehealth consultations eligible for rebates through public and private insurance. Such measures have resulted in the rapid uptake of telehealth and demonstrate the ability of both patients and health professional to adjust to alternative models of care delivery. However, significant barriers limiting the widespread utilisation of telehealth both nationally and internationally remain. These include patients’ preferences and barriers to the use of telehealth (e.g. age, level of education, level of computer literacy), clinician skills (e.g. technological self-efficacy, knowledge and skills), organisation/systems (e.g. lack of infrastructure and equipment, reimbursement) and technological factors (e.g. consumer-grade technology, internet quality) [Citation34].
The strengths of this review lie in the robustness of the systematic review methods. It included only randomised trials, which are the least biased and most reliable forms of evidence to assess treatment effectiveness. Furthermore, our search strategy was comprehensive, including searches of multiple databases, trial registries, forward and backward citation searches to ensure a complete overview of the relevant literature. This review is also the first to include a well-defined, systematic process for rating the quality of evidence across studies, using the GRADE approach. The limitations of this review include the small number of includable trials all with relatively small sample sizes which increases the potential for selection bias. As a result, the findings of this review should be interpreted with caution. The small number of trials included is likely attributed to the very specific inclusion criteria, which limited included studies to those assessing services considered ‘usual care’ and those comparing the delivery of identical or similar therapies to the telehealth and face-to-face groups. This excluded several trials which utilised web-based communication, apps, asynchronous data transfer with the use of sensors and other equipment and virtual reality software. Furthermore, there was significant variation in how telehealth was delivered in included studies in terms of the types of interventions provided, sample sizes, the duration of interventions, follow-up times and reporting of results. It is also important to consider the limitations on the generalisability of our findings to the management of a broad scope of musculoskeletal conditions. There are several barriers that limit the development of high-quality studies comparing telehealth and face-to-face rehabilitation for musculoskeletal conditions. These include, among others, heterogeneity in the types of health professionals that provide therapeutic care for MSK conditions (i.e. physiotherapists, chiropractors, GPs, etc.), and the resulting variation in prescribed therapies. This leads to subsequent differences across clinical trials in both the components of interventions and in their delivery, which impacts the analysis of effects [Citation37]. All of the studies eligible for inclusion in this review related to rehabilitation as applied to hip and knee arthroplasty and as such may not be applicable to other musculoskeletal conditions. Results should be interpreted with caution.
There is a need for further high-quality trials to determine the effectiveness, acceptability and feasibility of telehealth interventions for the management of musculoskeletal conditions. Future trials should aim to recruit larger sample sizes and follow participants over longer follow-up periods. There is also a significant gap in knowledge relating to cost outcomes, warranting studies that further evaluate cost-effectiveness of this treatment approach and the subsequent long-term sustainability of telehealth. This research also has important implications in facilitating its uptake and in guiding the optimal delivery of telehealth and its integration into health services.
Conclusions
Overall, based on five RCTs, the delivery of rehabilitation via a telehealth to patients prior to or following knee surgery appears to be equivalent to therapy delivered face-to-face. These findings are based on very low-quality evidence and should be interpreted with caution. To provide a better indication of the impact of telehealth, further high-quality primary trials are warranted in the musculoskeletal domain.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Natalia Krzyzaniak
Natalia Krzyzaniak Post-doctoral research fellow at the Centre for Research Excellence in Minimising Antibiotic Resistance in the Community (CRE-MARC), working towards the development of strategies decreasing the use of antibiotics in residential aged care facilities.
Magnolia Cardona
Magnolia Cardona Associate Professor Magnolia Cardona is a health services researcher with a passion for ensuring high quality care of disadvantaged populations. Her work over the past few years has focused on the identification and reduction of overtreatment of older patients near the end of life.
Ruwani Peiris
Ruwani Peiris Research assistant at the Institute for Evidence Based Healthcare.
Zoe A. Michaleff
Zoe Michaleff Honorary Adjunct Assistant Professor. She has a strong interest in research methods and the evidence-based diagnosis, prognosis and sustainable management of musculoskeletal conditions across the life course.
Hannah Greenwood
Hannah Greenwood Research assistant at the Institute for Evidence Based Healthcare. She has a background in psychology and main research interest areas are public mental health, nondrug interventions, over-diagnosis and research automation.
Justin Clark
Justin Clark Senior Research Information Specialist at the Centre for Research and Evidence Based Practice (CREBP) at Bond University. His work focuses on locating and retrieving information in a way that minimises workloads for research teams. He has been working on developing tools and methods for the automation of systematic reviews.
Anna Mae Scott
Anna Mae Scott Assistant Professor/Senior Research Fellow at the Centre for Research Excellence in Minimising Antibiotic Resistance in the Community (CRE-MARC). Her research primarily focuses on evidence generation and methodological development in two aspects of robust health policy decision-making: evidence syntheses (e.g. systematic reviews) needed to make sound, evidence-informed decisions; and the involvement of community members in those decisions.
Paul Glasziou
Paul Glasziou Professor of Evidence-Based Practice at Bond University and the Director of the Institute for Evidence Based Healthcare. His key interests include identifying and removing the barriers to using high quality research in everyday clinical practice.
References
- Australian Institute of Health and Welfare. Health-care expenditure on arthritis and other musculoskeletal conditions 2008–09. Canberra: AIHW; 2014.
- NSW Agency for Clinical Innovation. Management of people with acute low back pain: model of care. In: Health N, editor. Chatswood; 2016.
- Australian Commission on Safety and Quality in Health Care. Osteoarthritis of the knee clinical care standard. Sydney: ACSQHC; 2017.
- James SL, Geleijnse JM. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858.
- Fisk M, Livingstone A, Pit SW. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020;22(6):e19264–e19264.
- Cottrell MA, Galea OA, O'Leary SP, et al. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017;31(5):625–638.
- Dario AB, Moreti Cabral A, Almeida L, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342–1351.
- Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, et al. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017;19(4):e142.
- Pietrzak E, Cotea C, Pullman S, et al. Self-management and rehabilitation in osteoarthritis: is there a place for internet-based interventions? Telemed J E Health. 2013;19(10):800–805.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Physiopedia. WOMAC Osteoarthritis Index 2021. [cited 2021 Jan 19]. Available from: https://www.physio-pedia.com/WOMAC_Osteoarthritis_Index
- Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384–391.
- Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725.
- World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and generic version of the assessment 1996. [cited 2021 Jan 19]. Available from: https://www.who.int/mental_health/media/en/76.pdf?ua=1
- Roos EM, Lohmander LS. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64–64.
- Gagnon M, Hébert R, Dubé M, et al. Development and validation of the health care satisfaction questionnaire (HCSQ) in elders. J Nurs Meas. 2006;14(3):190–204.
- Clark J, Glasziou P, Del Mar C, et al. A full systematic review was completed in 2 weeks using automation tools: a case study. J Clin Epidemiol. 2020;121:81–90.
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
- Schünemann H, Brożek J, Guyatt G, et al. 2013. [cited 2021 Apr 22]. Available from: https://gdt.gradepro.org/app/handbook/handbook.html#h.svwngs6pm0f2
- Shaker MS, Wallace DV, Golden DBK, et al. Anaphylaxis—A 2020 practice parameter update, systematic review, and grading of recommendations, assessment, development and evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145(4):1082–1123.
- Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394.
- Danielsson L, Noras AM, Waern M, et al. Exercise in the treatment of major depression: a systematic review grading the quality of evidence. Physiother Theory Pract. 2013;29(8):573–585.
- Review Manager (RevMan) [Computer Program]. Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2020.
- Doiron-Cadrin P, Kairy D, Vendittoli PA, et al. Feasibility and preliminary effects of a tele-prehabilitation program and an in-person prehablitation program compared to usual care for total hip or knee arthroplasty candidates: a pilot randomized controlled trial. Disabil Rehabil. 2020;427(7):989–998.
- Moffet H, Tousignant M, Nadeau S, et al. In-Home telerehabilitation compared with face-to-Face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2015;97(14):1129–1141.
- Moffet H, Tousignant M, Nadeau S, et al. Patient satisfaction with in-Home telerehabilitation after total knee arthroplasty: results from a randomized controlled trial. Telemed J E Health. 2017;23(2):80–87.
- Tousignant M, Moffet H, Nadeau S, et al. Cost analysis of in-home telerehabilitation for post-knee arthroplasty. J Med Internet Res. 2015;17(3):e83.
- Odole AC, Ojo OD. Is telephysiotherapy an option for improved quality of life in patients with osteoarthritis of the knee? Int J Telemed Appl. 2014;2014:903816.
- Russell TG, Buttrum P, Wootton R, et al. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(2):113–120.
- Russell TG, Buttrum P, Wootton R, et al. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. J Telemed Telecare. 2003;9(2):S44–S47.
- Tousignant M, Moffet H, Boissy P, et al. A randomized controlled trial of home telerehabilitation for post-knee arthroplasty. J Telemed Telecare. 2011;17(4):195–198.
- Tousignant M, Boissy P, Moffet H, et al. Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. Telemed J E Health. 2011;17(5):376–382.
- Turolla A, Rossettini G, Viceconti A, et al. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100(8):1260–1264.
- Cottrell MA, Russell TG. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020;48:102193–102193.
- Australian Health Practitioner Regulation Agency. Telehealth guidance for practitioners AHPRA; 2020. [cited 2021 Jan 20]. Available from: https://www.ahpra.gov.au/News/COVID-19/Workforce-resources/Telehealth-guidance-for-practitioners.aspx
- Association AP. Telehealth Guidelines; Response to COVID-19 2020. [cited 2021 Jan 20]. Available from: https://australian.physio/sites/default/files/APATelehealthGuidelinesCOVID190420FA.pdf
- Ward L, Stebbings S, Cherkin D, et al. Components and reporting of yoga interventions for musculoskeletal conditions: a systematic review of randomised controlled trials. Complement Ther Med. 2014;22(5):909–919.
Appendix A
Table A1. Scales used to measure outcomes of interest
Appendix B
Searches
Database searches
PubMed search run 18/11/2020
(“Telemedicine”[Mesh] OR “Videoconferencing”[Mesh] OR Telehealth[tiab] OR Telemedicine[tiab] OR Videoconferencing[tiab] OR ((Telephone[tiab]) AND (Consultation[tiab] OR face-to-face[tiab] OR in-person[tiab])) OR telephone-delivered[tiab])
AND
(“Primary Health Care”[Mesh] OR “General Practice”[Mesh] OR rehabilitation[sh] OR “Outpatients”[Mesh] OR “Speech Therapy”[Mesh] OR Outpatient[tiab] OR “Primary health”[tiab] OR “Primary care”[tiab] OR “General practice”[tiab] OR “General practices”[tiab] OR “General practitioners”[tiab] OR “General practitioner”[tiab] OR “Family practice”[tiab] OR Physician[tiab] OR Physicians[tiab] OR Clinician[tiab] OR Clinicians[tiab] OR Therapist[tiab] OR Nurse[tiab] OR Nurses[tiab] OR Physiotherapist[tiab] OR Rehabilitation[tiab] OR Diabetes[tiab] OR Diabetic[tiab] OR Asthma[tiab] OR Depression[tiab] OR “Ïrritable bowel”[tiab] OR IBS[tiab] OR PTSD[tiab] OR “Chronic fatigue”[tiab])
AND
((Face-to-face[tiab]) OR “Usual care”[tiab] OR Visits[tiab] OR Visit[tiab] OR In-person[tiab] OR “In person”[tiab] OR ((Clinic[tiab] OR Centre[tiab] OR Home[tiab]) AND (Based[tiab] OR Contact[tiab])) OR Conventional[tiab] OR “Practice-based”[tiab] OR “Practice based”[tiab] OR Traditional[tiab] OR “Standard care”[tiab] OR Homecare[tiab] OR ((Routine[tiab] OR Home[tiab]) AND (Care[tiab])))
AND
(“Delivery of Health Care”[Mesh] OR Delivery[tiab] OR Delivered[tiab] OR via[tiab] OR Received[tiab])
AND
(“Treatment Outcome”[Mesh] OR “Patient Satisfaction”[Mesh] OR Therapy[sh] OR Diagnosis[sh] OR “Clinical outcomes”[tiab] OR Treatment[tiab] OR Diagnostic[tiab] OR Efficacy[tiab])
AND
(Randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR randomised[tiab] OR placebo[tiab] OR “drug therapy”[sh] OR randomly[tiab] OR trial[tiab] OR groups[tiab])
NOT
(Animals[Mesh] not (Animals[Mesh] and Humans[Mesh]))
NOT
(“Case Reports”[pt] OR Editorial[pt] OR Letter[pt] OR Meta-Analysis[pt] OR “Observational Study”[pt] OR “Systematic Review”[pt] OR “Case Report”[ti] OR “Case series”[ti] OR Meta-Analysis[ti] OR “Meta Analysis”[ti] OR “Systematic Review”[ti] OR “Systematic Literature Review”[ti] OR “Qualitative study”[ti] OR Protocol[ti])
CENTRAL via the Cochrane Library run 18/11/2020
([mh Telemedicine] OR [mh Videoconferencing] OR Telehealth:ti,ab OR Telemedicine:ti,ab OR Videoconferencing:ti,ab OR ((Telephone:ti,ab) AND (Consultation:ti,ab OR “face-to-face”:ti,ab OR “in person”:ti,ab)) OR “telephone delivered”:ti,ab)
AND
([mh “Primary Health Care”] OR [mh “General Practice”] OR [mh Outpatients] OR [mh “Speech Therapy”] OR Outpatient:ti,ab OR “Primary health”:ti,ab OR “Primary care”:ti,ab OR “General practice”:ti,ab OR “General practices”:ti,ab OR “General practitioners”:ti,ab OR “General practitioner”:ti,ab OR “Family practice”:ti,ab OR Physician:ti,ab OR Physicians:ti,ab OR Clinician:ti,ab OR Clinicians:ti,ab OR Therapist:ti,ab OR Nurse:ti,ab OR Nurses:ti,ab OR Physiotherapist:ti,ab OR Rehabilitation:ti,ab OR Diabetes:ti,ab OR Diabetic:ti,ab OR Asthma:ti,ab OR Depression:ti,ab OR “Ïrritable bowel”:ti,ab OR IBS:ti,ab OR PTSD:ti,ab OR “Chronic fatigue”:ti,ab)
AND
((“Face-to-face”:ti,ab) OR “Usual care”:ti,ab OR Visits:ti,ab OR Visit:ti,ab OR “In person”:ti,ab OR ((Clinic:ti,ab OR Centre:ti,ab OR Home:ti,ab) AND (Based:ti,ab OR Contact:ti,ab)) OR Conventional:ti,ab OR “Practice based”:ti,ab OR Traditional:ti,ab OR “Standard care”:ti,ab OR Homecare:ti,ab OR ((Routine:ti,ab OR Home:ti,ab) AND (Care:ti,ab)))
AND
([mh “Delivery of Health Care”] OR Delivery:ti,ab OR Delivered:ti,ab OR via:ti,ab OR Received:ti,ab)
AND
([mh “Treatment Outcome”] OR [mh “Patient Satisfaction”] OR “Clinical outcomes”:ti,ab OR Treatment:ti,ab OR Diagnostic:ti,ab OR Efficacy:ti,ab)
Embase search run 18/11/2020
('Telemedicine’/exp OR 'Videoconferencing’/exp OR Telehealth:ti,ab OR Telemedicine:ti,ab OR Videoconferencing:ti,ab OR ((Telephone:ti,ab) AND (Consultation:ti,ab OR face-to-face:ti,ab OR in-person:ti,ab)) OR telephone-delivered:ti,ab)
AND
('Primary Health Care’/exp OR 'General Practice’/exp OR 'Outpatient’/exp OR 'Speech Therapy’/exp OR Outpatient:ti,ab OR “Primary health”:ti,ab OR “Primary care”:ti,ab OR “General practice”:ti,ab OR “General practices”:ti,ab OR “General practitioners”:ti,ab OR “General practitioner”:ti,ab OR “Family practice”:ti,ab OR Physician:ti,ab OR Physicians:ti,ab OR Clinician:ti,ab OR Clinicians:ti,ab OR Therapist:ti,ab OR Nurse:ti,ab OR Nurses:ti,ab OR Physiotherapist:ti,ab OR Rehabilitation:ti,ab OR Diabetes:ti,ab OR Diabetic:ti,ab OR Asthma:ti,ab OR Depression:ti,ab OR “Ïrritable bowel”:ti,ab OR IBS:ti,ab OR PTSD:ti,ab OR “Chronic fatigue”:ti,ab)
AND
((“Face-to-face”:ti,ab) OR “Usual care”:ti,ab OR Visits:ti,ab OR Visit:ti,ab OR In-person:ti,ab OR “In person”:ti,ab OR ((Clinic:ti,ab OR Centre:ti,ab OR Home:ti,ab) AND (Based:ti,ab OR Contact:ti,ab)) OR Conventional:ti,ab OR Practice-based:ti,ab OR “Practice based”:ti,ab OR Traditional:ti,ab OR “Standard care”:ti,ab OR Homecare:ti,ab OR ((Routine:ti,ab OR Home:ti,ab) AND (Care:ti,ab)))
AND
('health care delivery’/exp OR Delivery:ti,ab OR Delivered:ti,ab OR via:ti,ab OR Received:ti,ab)
AND
('Treatment Outcome’/exp OR 'Patient Satisfaction’/exp OR “Clinical outcomes”:ti,ab OR Treatment:ti,ab OR Diagnostic:ti,ab OR Efficacy:ti,ab)
AND
(random* OR factorial OR crossover OR placebo OR blind OR blinded OR assign OR assigned OR allocate OR allocated OR 'crossover procedure’/exp OR 'double-blind procedure’/exp OR 'randomized controlled trial’/exp OR 'single-blind procedure’/exp NOT ('animal’/exp NOT ('animal’/exp AND 'human’/exp)))
AND [embase]/lim
Clinical registry searches
Searches run 25 March 2021
Clinicaltrials.gov
Intervention field: (Telemedicine OR Videoconferencing OR Telephone OR Telehealth) AND (‘Usual care’ OR ‘Standard care’ OR ‘Face-to-face OR Face-to-face’)
Condition or disease field: musculoskeletal
WHO ICTRP
Telemedicine AND musculoskeletal OR Telehealth AND musculoskeletal OR Videoconferencing AND musculoskeletal
Appendix C
Table C1. Assessment of evidence using GRADE analysis.
Appendix D
Table D1. Table of excluded studies.
Appendix E
Table E1. Potentially relevant ‘in progress’ clinical trials.