Abstract
Background
Persistent pain (PP) is a complex mechanism affecting 35% to 51.3% of adults in the United Kingdom and is associated with significant reductions in quality of life. Understanding of PP and how best to treat it has developed over the past 50 years, but there is still a vacuum of research to inform novel applications for self-management. Mindfulness techniques and nature exposure have separately been found to have beneficial effects on general well-being and health. The integration of the two could produce much needed self-management strategies, improving quality of life in this patient group.
Objectives
To determine if nature-based mindfulness (NBM) interventions improve pain and quality of life in adults with PP.
Methods
Systematic literature review. Seven electronic databases were searched to identify quantitative papers investigating nature-based mindfulness and persistent pain. Included articles were appraised using the PEDro tool.
Results
A total of 362 studies were identified. Of these, three were included in the final review. All studies reported statistically significant improvements in self-reported scores for pain (p ≤ 0.001–0.006) and depression (p ≤ 0.001–0.000). Other outcomes, such as stress and fatigue produced mixed results.
Conclusion
Despite showing statistical significance in multiple outcomes, the minimal clinically important difference was not reached across all measures. Heterogeneity of interventions and outcomes, as well as methodological issues of internal and external validity, preclude definitive conclusions. Further research is required, employing explicit mindfulness interventions and outcome measures with greater relevance and specificity, as well as further investigation of theoretical mechanisms.
Introduction
Persistent pain (PP) defines a continual pain experience lasting for more than three months [Citation1]. The specific mechanisms behind PP are complex; however, there are commonly changes in central sensitization, involving increased sensitivity and pain response to sensory input [Citation2]. Risk factors for developing PP are also complex, with socio-demographic, psychological, clinical, and biological factors as potential contributors [Citation3]. PP represents the leading cause of disability and disease burden globally, and its prevalence is escalating [Citation3]. PP can be highly debilitating to the individual and treatment is often multi-faceted and challenging [Citation4]. The condition can have a negative effect on the individual’s quality of life (QOL) [Citation5] with a subsequent impact on family members, friends, and carers [Citation6]. In the United Kingdom (UK) population it is estimated at 35% to 51.3%, with 10.4% to 14.3% of people having PP which is moderately or severely disabling [Citation7]. The COVID-19 pandemic has increased the social threats associated with PP, including isolation, increased stress, and lack of access to treatment [Citation8,Citation9]. Globally, it is reported that for some nations, the burden of pain also consequently increased for those already diagnosed with PP during the pandemic [Citation9].
Historically, management of PP has focused on pharmaceutical treatment, initially relying on opioid-based medications, progressing to the use of other medications, such as non-steroidal anti-inflammatory drugs and antidepressants [Citation10,Citation11]. Recent advances in evidence have, however, precipitated a decrease in opioid-based medications which are no longer advised in primary care, due to a lack of evidence for PP alongside the risk of adverse effects and addiction [Citation1,Citation12]. Although medication continues to be an option within specialist pain management settings, in which opioids can be employed in some limited cases [Citation13], there exists a need for holistic treatment modalities that go beyond shorter-term analgesic prescriptions. PP treatment modalities have evolved alongside developments in pain theory [Citation14], which views pain mechanisms as a protector rather than a marker of tissue damage [Citation15]. This divergence from a purely biomedical model of pain management, of which physiotherapy has played a leading role [Citation16], has led to a range of initiatives such as mindfulness practices [Citation17].
Mindfulness
A commonly held definition of mindfulness is cited as ‘paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally’ [Citation18]. Mindfulness-based interventions (MBIs) are an umbrella term for a range of programs based on these principles of awareness, openness, acceptance, and the processing of attention [Citation19,Citation20]. These concepts have stemmed from mindfulness roots in Eastern Buddhist and Hindu traditions [Citation21]. Mindfulness was introduced into the healthcare context with concepts such as Kabat-Zinn’s 1982 [Citation22] mindfulness stress-based reduction for chronic pain and MBIs are now widespread in Western medicine [Citation23]. However, Western medicine can be defined as being evidence-based and historically examining different mechanisms compared with an Eastern medicine approach [Citation24]. It is important to note therefore that in a healthcare context MBIs often use varied and isolated elements that are not representative of the full context of the original cultural settings [Citation25].
MBIs have been utilized to influence a person’s relationship with their pain rather than eliminating the experience, with the goals of improving their independence and QOL [Citation26]. They have been implicated in the direct reduction of pain intensity, particularly with central sensitization mechanisms [Citation17], possibly by affecting the processing of pain and by reducing anxiety about the future and the past [Citation27,Citation28].
Mindfulness can be present in untrained individuals as an innate characteristic disposition and also as a transient state, with sustained practice linked to increased dispositional mindfulness [Citation29]. Lower levels of dispositional mindfulness are linked with increased susceptibility to rumination and catastrophizing, whereas higher levels are linked with increased self-regulation, engagement in acceptance-based pain strategies, and lower pain in multiple PP populations [Citation30,Citation31]. One mechanism behind this change in pain outcomes is explored in predictive processing theory. Expectations play a large part in perception, to the extent that negative expectations can lead to negative experiences despite positive inputs [Citation32]. These prediction errors should be corrected with new information [Citation33]; however, the process can become maladaptive. In PP, it is these maladaptive predictions that may be responsible for the persistence of pain, and phenomena such as pain sensation without painful stimuli [Citation33]. Mindfulness facets such as attentional control or self-regulation may help people with PP to untie and change these ways of thinking [Citation28,Citation34]. The construct of mindfulness has a multitude of facets discussed in the literature with no current gold standard measure [Citation35]. Five common facets of mindfulness have however been identified across multiple mindfulness measurement tools: observing, describing, acting with awareness, non-judgement of internal experiences, and non-reactivity to internal experiences [Citation36].
There is mixed-quality evidence to support MBIs effectiveness in the treatment of PP [Citation37–39]. They do however have an evidence-based treatment approach in other long-term conditions, such as chronic obstructive pulmonary disease [Citation40], depression [Citation41], substance misuse [Citation42] and fatigue [Citation43], and are recommended to promote self-management strategies in PP [Citation1,Citation44].
Nature-based mindfulness
Within MBIs, nature-based mindfulness (NBM) has emerged as a broad category of interventions stemming from practices such as Shinrin-Yoku, or forest bathing, which utilize the potential benefits of exposure to a forest environment [Citation45]. Proposed mechanisms include a gentle attentive response, encouraging reflection and introspective thinking [Citation46], stress reduction [Citation47], or an evolutionary need for nature for well-being [Citation48]. Nature exposure reduces the effort required to engage in MBIs, particularly for those new to mindfulness [Citation49] and is also associated with the development of dispositional mindfulness [Citation29].
There is cogent evidence linking NBM with positive health outcomes, with statistically significant improvements found in psychological, physiological and interpersonal measures in a recent systematic literature review and meta-analysis [Citation20]. Given the importance of positive top-down protective factors [Citation50], and the mechanisms by which natural environments could improve health outcomes linked to PP conditions such as reducing inflammation and levels of cortisol and lessening anxiety, the effectiveness of NBM as a treatment adjunct for PP is a pertinent question [Citation51,Citation52]. Furthermore, this accessible intervention may help to reduce health inequalities by providing an alternative to green exercise or group based green activities that may be limited by both mobility and fatigue levels for some PP populations.
Systematic literature reviews (SLR) exist examining NBM [Citation20] and MBI for PP [Citation26,Citation38,Citation39], as well as a non-systematic review exploring nature exposure and possible mechanisms for effects in PP [Citation53]; however, there is no SLR combining NBM with PP. The aim of this review therefore is to determine if NBM interventions improve pain and QOL in adults with PP.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used when conducting this SLR [Citation54].
Search strategy
The search strategy and terms () were developed in consultation with a subject librarian and were drawn from background research of the literature concerning PP and NBM. The electronic databases used for the systematic search were AMED, CINAHL, SportDiscus and PsycINFO, Medline (via the EBSCO search engine), Cochrane Library, and Embase. These databases provide resources appropriate to allied health, physical and psychological therapies [Citation55]. Snowballing was used to highlight further missed articles adding rigor to the search strategy [Citation56]. Preliminary reading into NBM identified appropriate terminology, leading to a predicted heterogeneity of outcome measures (OMs) and comparators; therefore, these parameters were left open for the purpose of the search strategy.
Table 1. PICO And search terms.
Inclusion/exclusion criteria
Inclusion and exclusion criteria () were agreed upon a priori. There was no historical limit placed upon the findings, due to mindfulness being a relatively new concept in Western medicine [Citation57,Citation58] To increase the number of possible papers, the terms included conditions such as fibromyalgia which are characterized by PP. Outcome measures were not specified as outlined in the search strategy but were judged by group discussion during screening. Papers were screened at title and abstract as well as at full text by all individuals working initially in two pairs and then discussed and agreed upon collectively.
Table 2. Inclusion/exclusion criteria with justification.
Ethics
Ethically approved as low risk by scrutiny committee [Citation59]
Data extraction
A data extraction table was designed following a recent SLR on MBIs for PP [Citation38] and used for the included papers. Each included paper was assigned to a separate reviewer for extraction of data and the results were then discussed and verified collectively.
Quality appraisal
The Physiotherapy Evidence Database (PEDro) scale was used to appraise the quality of each paper. Despite potential issues highlighted with validity when used as an overall score [Citation60], it has been shown to have ‘fair’ to ‘good’ reliability [Citation61]. After discussion, the tool was also chosen in comparison to more complex tools due to its simplicity of use and increased chance of inter-rater reliability within the review team.
Results
Identification of studies
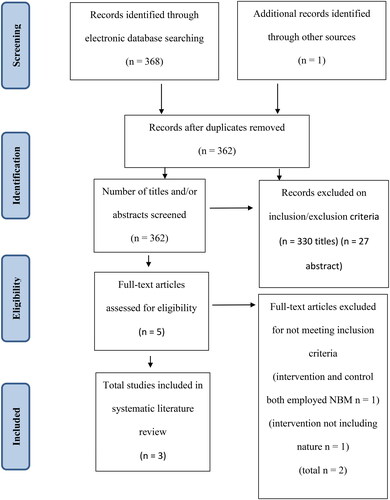
The initial database search yielded 368 articles, with one additional article found through snowballing, after removal of duplications (n = 7). Of these, 330 studies were excluded based on title, 27 on abstract, and two upon reading the full text, leaving three papers that met the inclusion criteria ().
Quality appraisal
Summaries of the critical appraisal process are shown in as a PEDro score. All three studies were of at least ‘fair’ methodological quality. Two studies scored 6/10 indicating ‘good’ quality, and one study scored 5/10. Specific methodological challenges are highlighted within the discussion.
Table 3. PEDro Scores.
Participant characteristics
The three studies were published between 2016 and 2021 with a total of 266 participants. Sample sizes ranged from 33 to 169 participants. The studies were carried out in South Korea [Citation62,Citation63] and Catalonia [Citation64]. The study types were a pragmatic randomized control trial [Citation64], a randomized control trial [Citation62], and a non-randomized control trial [Citation63].
Two of the studies considered people with chronic widespread pain (CWP) [Citation62,Citation63] and one with fibromyalgia [Citation64]. The average age ranged from 37.5 to 54.1 years. The participants in two of the studies [Citation62,Citation63] were recruited from the workforce of a public organization in Seoul, with the former excluding people requiring pain medication daily and participants over 65 years of age, whilst the latter excludes those not in full-time employment and women who have begun menopausal transition. The third study [Citation64] recruited participants from a specialized unit within a hospital with demographic characteristics showing high levels of comorbidity, an older age group, predominantly female and with multiple years lived with illness, with the exclusion of people with severe mental disorders and neurogenerative conditions.
Interventions
The studies used different interventions, and none of them used an active control, although all three studies used a forest as their nature setting. One study [Citation63] had participants spent two days in a forest setting combining guided mindfulness-based meditation with exercise, music therapy, forest activities, and social activities. Half an hour of the second day was spent engaged in mindfulness-based meditation and a total of eleven hours were spent in the forest. The control group was under instructions to carry out normal weekend activities, with a caveat of avoiding nature-based activities. One study [Citation64] used a 12-week intervention of treatment as usual plus weekly 2-h sessions made up of nature-based mindfulness training and other interventions such as pain neuroscience education, exercise therapy, cognitive behavioral therapy, mindfulness training, and nature activity. The control group received a 12-week control of treatment as usual (education and pharmacological treatment). The third [Citation62] used a single 4-h mindfulness-based mandala-coloring session in nature as an intervention, described as supervised coloring-in of a pre-drawn mandala while encouraging participants’ awareness of their emotions and surroundings. The control arm completed a 4-h urban bus tour.
Outcome measures
All three studies assessed outcome measures at the start and end of the intervention, and the 12-week study [Citation64] also assessed mid-way. None of the studies carried out follow-up assessments. Two studies [Citation62,Citation64] included power calculations. Between-group baseline differences were calculated in each paper. Effect sizes and p-values were given for the outcome measures in the selected studies but confidence intervals were only provided by one study [Citation64]. All the studies gained informed consent from participants and reported no conflict of interest.
Findings
All studies measured pain, fatigue, and psychological factors employing a range of instruments. Based on a statistical significance threshold of p. < 0.05 [Citation65] all studies reported statistically significant reductions in pain experience and depression in the intervention group in contrast to the control group. All papers included at least one measure for physical or psychological outcomes and all but one [Citation64] included a physiological marker.
Pain
All three papers found a statistically significant decrease in pain following treatment with large effect sizes. Two studies found a significant improvement in Visual Analog Scale (VAS) pain scores, (p ≤ 0.001, d = 5.62) [Citation64] and (p = 0.001, np2 = 0.19) [Citation63]. The third study found a significant decrease in the number of tender points (p = 0.006, np2 = 0.205) [Citation62].
Fatigue
Two studies measured fatigue. One study found statistically significant improvements (p ≤ 0.001) with a large effect size (d = 0.93) in fatigue using a VAS measure [Citation64] while the other did not find improvement, using the Fatigue Severity Scale (p = 0.133) [Citation62]
Depression
All three studies found statistically significant reductions in depression with large effect sizes, although the outcome measures varied. Outcome measures used were the Beck Depression Inventory (BDI) (p = 0.001, np2 = 0.16) [Citation63], the depressive symptom on the Stress Response Inventory-Modified Form (SRI-MF) (p = 0.001, np2 = 0.309) [Citation62] and the Hospital Anxiety and Depression Scale (HADS) for anxiety (p ≤ 0.001, d = 1.59) and depression (p ≤ 0.001, d = 1.45) [Citation64].
Stress
Two studies measured stress. Statistically significant improvements were seen in with total stress levels as measured by the Stress Response Inventory Modified Form (SRI-MF) (p. 0.001, np2 = 0.300); however, improvements did not reach significance in anger (p. 0.011) and somatization symptoms (p. 0.016) [Citation62]. No significant changes were seen using the perceived stress scale [Citation64].
Quality of life
Two studies employed quality of life measures and found some outcomes to be statistically significant with large effect sizes. One study found a significant change in the Euro Quality-of-Life Visual Analogue Scale (p = 0.000, np2 = 0.21) [Citation63]. Significant reductions (p < 0.001, d = 1.83) were found in the revised fibromyalgia impact questionnaire (FIQR), as well as the Short Form 36 Heath Survey Questionnaire physical functioning component (p ≤ 0.001, d = 1.59) [Citation64].
This study also separated the results of the Cognitive Emotional Regulation Questionnaire (CERQ), finding significant (all p ≤ 0.001) improvements in three out of nine sub-sections with a large effect size; refocusing (d = 0.99), planning (d = 0.83), positive reappraisal (d = 1.42) and one showing medium effect size, perspective (d = 0.71) [Citation64]
Two studies identified physiological biomarkers. A significant reduction in salivary cortisol was found with a large effect size (p = 0.001, np2 = 0.238) [Citation62]. Statistically significant positive differences with large effect sizes were found in measures of heart rate variability; electrocardiogram standard deviation of normal to normal (p ≤ 0.001, np2 = 0.34) and total power (p ≤ 0.001, np2 = 0.23), although heart rate did not decrease. They also found an increase in natural killer (NK) cell activity (p ≤ 0.002, np2 = 0.15) [Citation63].
Discussion
This review aimed to ascertain if NBM interventions could improve QOL and pain in adults with PP. The selected studies found that NBM reduces pain by a large effect size compared to an inactive control, and this is a superior benefit to that found in previous reviews of both NBIs and MBIs. All studies showed a significant improvement in depression and QOL indicators in the intervention group in contrast to control. Two studies demonstrated clinically significant improvements in the measurement of biomarkers [Citation62,Citation63]. The methodological quality of the included studies was ranked as high for two studies and moderate for one although there are limitations to the included studies in regard to the risk of bias, heterogeneity in outcomes and lack of follow-up, the length and type of interventions and populations studied.
Randomization and blinding
Two studies randomized participants [Citation62,Citation64]. One study [Citation63] did not randomly allocate participants, although this was in part mitigated by similar demographic characteristics of the two groups, with effort made to achieve parity of age and gender, indicating that systematic bias was minimized [Citation65]. The study’s source of funding raises the risk of unintended or unconscious bias, which randomization helps protect against [Citation66].
The risk of bias could be inferred in all papers due to lack of allocation concealment, blinding of the therapists administering the interventions and of the assessors [Citation63,Citation64]. This should be qualified, however, given that the blinding of participants and therapists in behavioral interventions may not be plausible [Citation67,Citation68], and sham therapy was unrealistic given the nature of interventions [Citation69]. Although it is not possible to disguise a nature setting, sham mindfulness has been used in other studies enabling participant blinding [Citation28]. There were no significant differences in baseline measurements of participant demographics, apart from one study, with differences in sleep and age across groups [Citation63].
Outcomes and measurement
A shortcoming of all three studies is the lack of follow-up outcomes, limiting the transferability to clinical practice. Final measurements were taken directly post-intervention in all cases. Hilton [Citation38] recommends 6-to-12-month follow-up measurements for studies of PP which could help to ensure validity in measuring interventions in complex long-term conditions in which beneficial effects may be transient [Citation65]. Although all studies reported significant reductions in self-reported parameters, the heterogeneity of OMs limits the results’ synthesizability [Citation70]. The disparity in OMs is a finding shared by previous SLRs of PP and MBIs, in which recommendations were made for a standardized criteria for assessing treatment effect [Citation17,Citation38].
Further limitations exist within the application of significant findings to practice as only one study [Citation64] study considered clinical implications of their outcome measure, with analysis of the number needed to treat (NNT), which shows the number of patients to be treated to have a clinical impact on one patient [Citation71]. Although of clinical significance, this differs from the patient-focused minimally clinically important difference (MCID). An MCID is a measure of the smallest difference that could be meaningful to a patient within a particular outcome measure [Citation72]. MCID values are studied for some of the primary outcomes such as VAS pain although far from being standardised, there is considerable heterogeneity when applying them to PP [Citation73]. Consideration of findings within the context of MCID would aid clinical interpretation although this would require clear reflection to apply clinically [Citation73]
Pain
The findings are promising for the application of NBM in PP management. However, they could be facilitated by reduced stress levels from confounding variables such as participants having time away from their usual lives or feeling that their pain has been acknowledged; a powerful tool in the management of PP and associated conditions [Citation74]. This is a difficulty of using multifactorial interventions, affecting the reliability and validity of the findings [Citation75]. Pain and well-being are subjective experiences, with many OMs available to measure these [Citation76]. MTPS and VAS-Pain were used to measure pain; concurrent validity has not been identified between these two OMs therefore establishing consistency between them is difficult. Although MTPS has been found to be sensitive and specific in the diagnosis of fibromyalgia [Citation77], research indicating its effectiveness as an OM for the PP population is lacking. VAS-pain has been shown to be reliable, responsive, and sensitive to the PP population [Citation78]. Breivik [Citation79] recommends the utilization of multi-modal OMs for PP, arguing the validity of VAS is reduced by a failure to capture the condition’s complexity, something employed to the credit of all three studies.
Quality of life and wellbeing
FIQR and CERQ are valid and reliable outcome measures for fibromyalgia populations, although these may be difficult to generalize to other populations [Citation80,Citation81]. The Stress Response Inventory was found to be valid and reliable; however, it was not assessed in the PP population [Citation82]. One study did use a modified version; however, the development paper is not available in English so cannot be assessed [Citation62,Citation83]. The use of subjective outcome measures also presents challenges with floor and ceiling effects. This is especially pertinent as mobility issues are common in fibromyalgia and other PP conditions [Citation84].
The other outcome measured in all three studies was depression, using varied OMs. There is conflicting research into the validity of HADS in persistent pain especially outside of an inpatient environment [Citation85,Citation86]. The BDI and SRI-MF have been validated for their use in identifying depression, although the BDI has been found to be unsuitable for PP populations [Citation87,Citation88].
Lastly, the use of biomarkers can be effective measures if they reflect diagnostic accuracy in a target condition [Citation89]. Reductions in cortisol levels add to the validity of findings [Citation62] given the link between PP and stress levels and findings of heightened cortisol levels in the PP population [Citation51,Citation90,Citation91]. The increase of NKC activity found by [Citation63] is less significant, given findings that indicate NKC activity is not significantly altered in PP conditions [Citation92].
Mindfulness measures
No study assessed dispositional or state mindfulness. The concept of measuring behaviors associated with improved outcomes in PP is established in research. For example, self-compassion levels are associated with improved functioning [Citation93]. One study [Citation64] did measure and find changes in emotional regulation within the CERQ subsections of refocusing, planning, positive affect, and perspective which could be considered within the construct of self-regulation. There could be multiple benefits to measuring state or dispositional mindfulness as well as specific facets in NBM studies, both at baseline and after treatment. First, it would help improve understanding of the mechanisms behind NBM in treating PP, by providing evidence of whether changes in mindfulness traits are reflected in the patient’s well-being and pain experience. Second, taking baseline measures would help ensure experiment groups are similar. Third, it could contribute to the understanding of what makes people more or less likely to respond to NBM, utilizing similar statistical analysis as in [Citation64]. Finally, measuring changes in mindfulness can help resolve some of the difficulties of heterogenous NBM interventions, by providing evidence of changes in the level of mindfulness traits in response to treatment.
There is however no gold standard outcome measure for mindfulness and there are many instruments available. The Mindful Attention Awareness Scale (MAAS) [Citation94] measures dispositional mindfulness and is cited as one of the most commonly used in research [Citation95], which may ease implementation into studies and decrease heterogeneity. It has also been shown to have internal reliability in the PP population [Citation96]. The Five Facet Mindfulness Questionnaire (FFMMQ) [Citation36] is also much used due to its development from analysis of multiple tools and is suggested to provide superior analysis at a facet level, as opposed to the general measure of the MAAS [Citation35]. This measure has also been validated in PP although this should be interpreted with caution as a modified form was used [Citation97]. The use of both has been advocated for a more comprehensive measurement [Citation31]. More recently, the Philadelphia Mindfulness Scale (PMS) [Citation98] has been validated in a PP population and has been advocated for in MBI research [Citation99]. In terms of state mindfulness measures, research is emergent and therefore less validated clinically although the Toronto Mindfulness Scale (TMS) [Citation100] and the State Mindfulness Scale (SMS) [Citation101] are the leading tools [Citation102].
Data analyses
A withdrawal rate of 11.7% in the intervention group in one study [Citation64] could cast doubt on the findings’ significance, due to the risk of attrition bias whereby a systematic difference in an unknown variable in participants may be influencing the outcome rather than the hypothesized variable [Citation103]. The authors did however compare baseline characteristics of dropouts versus non-dropouts, no significant differences were found, which decreases the suspicion of systematic attrition. However, reasons for dropouts were not explored, although this is recommended in order to fully understand any bias [Citation104]. The withdrawal rate from the intervention group only may indicate that the intervention was not tolerated by or acceptable for the intended population [Citation105] with implications for its utilization in clinical practice. However, the dropout rate was not large enough to affect the calculated sample size so there is a decreased risk of a type 2 error in which a false negative finding is concluded due to inadequate sample size and therefore power [Citation106]. The authors did also perform an intention-to-treat analysis (ITT), whereby all participants are analyzed in the group they were allocated to, helping to produce a less biased estimate of the intervention’s efficacy by preserving the randomization effect against confounding variables within groups [Citation107]. They also used the last observation carried forward method to input missing data, where the last known value is used [Citation108]. This is a commonly advocated approach although bias may be introduced due to missing data not being random in nature [Citation108].
One study [Citation63] had three dropouts from the control arm. The study recruited patients with the promise of receiving NBM treatment and therefore this could be a potential result of selection bias where participants’ knowledge of and belief in the study’s aims may result in bias. The study was however already underpowered and this along with a lack of management for missing outcome data the risk of a type 2 error.
Types of intervention
All studies used different forms of NBM and whilst there is no unequivocal definition of mindfulness [Citation109], all studies used ‘attention’ and ‘awareness’ when describing their intervention, words that have been corroborated by Nilsson and Kazemi [Citation110] in their work to thematize mindfulness. All three studies acknowledge that combining NBM with other treatments prevents isolation of the effects of NBM. Of the NBIs in two studies [Citation63,Citation64], only Shinrin-Yoku and nature photography in the former, and mindfulness-based meditation in the latter, could constitute NBM [Citation111,Citation112]. The inclusion of physical activity, which has well-evidenced benefits for PP [Citation113,Citation114], prescribed to intervention groups only, furthers this limitation. One study [Citation64] provided some insight using intra-session assessment of individual activities and found Shinrin-Yoku resulted in significant improvements in a range of factors including pain, stress, and fatigue. However, these results were taken from measuring the short-term impact of activities, with potential cross-over effects of previous activities, and based on only 37 participants, without information on their characteristics.
External validity
Within the PP population in Western healthcare, there exists a disproportionately high number of older adults, those racialized as black and minority ethnic communities, and in areas of higher economic deprivation [Citation115,Citation116]. There is a marked overlap with these populations regarding reduced access to quality green space, especially in the light of widening inequalities due to COVID-19 [Citation117]. This may prevent generalization of interventions to these populations and further exacerbate these inequalities. The results of the studies carried out in Korea [Citation62,Citation63] may not generalize to Western culture as concepts of nature depend upon contextual social and cultural constructs, for example, differences between European and Asian countries [Citation118]. Practices such as Shinrin-Yoku have been reported as well accepted by participants of a Western culture [Citation119]. However, further research is needed into diverse populations [Citation120], including the at-risk PP populations identified above.
Only CWP/fibromyalgia was studied so there are questions about generalizability to other PP conditions. However, although each PP condition, as well as each person, has varied contributing factors, there are many key features of PP which are likely to be common to all PP conditions, increasing generalisability [Citation121]. However, the CWP studies [Citation62,Citation63] only included people in employment, and one [Citation62] excluded people using daily pain medication. These restrictions mean that the findings may not apply to people with higher levels of pain or disability.
Other individual characteristics of the studies may also impact the generalisability of this research; 40% (n = 97) of the participants were from South Korea [Citation62,Citation63], were 99% female [Citation64], and recruitment was from a particularly distinct group of workers [Citation62,Citation63]. Age ranged from 37 to 54 years, which may make it difficult to generalize to the older or younger adult population. This is perhaps an oversight when figures show up to 86% of OAs experience PP [Citation122,Citation123]. Finally, In terms of clinical application, there is little agreement about MCID figures for chronic pain [Citation73]. Their lack of use in the studies makes the stated results hard to interpret for clinical use.
Limitations of this study
Grey literature was not searched and hand searching was not undertaken. In addition, only English-language studies were included. A more thorough risk of bias tool could have been utilized when appraising the studies such as the Cochrane risk of bias tool; however, this tool was considered and the PEDro tool was chosen to promote higher levels of inter-rater reliability. Individual completion of the PEDro appraisal tool prior to group appraisal would have reduced bias; however, any disparities were discussed and agreed upon.
Conclusion
This review finds promising improvements in pain and QOL outcomes in adults with PP across three studies of moderate to high quality with a large effect size, delivered without significant adverse effects. This supports previous evidence showing that nature-based interventions and MBI can improve outcomes for PP patients. Two studies [Citation62,Citation63] provide interesting information regarding the use of short-term NBM in less severe PP populations, and the range of outcome measures in the final study provides potential insight into the mechanisms of NBM. [Citation64]
Although the significance and effect sizes of benefits were encouraging, considerable methodological issues undermine the validity of results, as well as a small number of eligible studies. Heterogeneous OMs and difficulties capturing PP outcomes due to the complexity of pain processing lessen certainty in results. The clinical usefulness of results is also undermined by a lack of information on long-term outcomes, MCID interpretation, and limited generalisability of specialized participant characteristics, which may exacerbate existing inequalities. The inability to isolate NBM interventions reduces the impact of the results as a causal relationship between NBM and the outcomes cannot be explicitly implied. A definitive conclusion is therefore not possible and future research is recommended.
Future research
Future research recommendations include adequately powered studies with participants from clinically relevant and diverse populations, such as those with higher levels of pain and disability and from diverse ethnic and socio-economic backgrounds. The development of standardized categories for the mindfulness and the nature aspects of NBM would aid future analyses. Studies should be designed to allow isolation of the NBM variable for causal analysis and active controls used, ideally of a currently recommended non-pharmacological treatment or comparison of MBI with NBM.
Measurement of dispositional and state mindfulness should be considered, with measures of both general mindfulness and facet-level mindfulness. Measurement tools to consider that have some level of validation for PP include the MAAS, FFMMQ, or PMS for dispositional mindfulness and SMS or TMS for state mindfulness. This may aid the current understanding of theoretical mechanisms of action for NBM. Follow-up measures should be taken at six to twelve months and MCID for PP further developed and used to help clinical interpretation. Future research should attempt to estimate the cost of delivering NBM and ensuring that it occurs in a suitable natural environment that is accessible and equitable.
To further improve internal validity, future studies should ensure random allocation and assessor blinding, as well as accounting for loss to follow-up. Placebo effects should be minimized by avoiding the use of a single therapist for a long intervention, and selection bias reduced by avoidance of convenience sampling.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- NICE. Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain. NICE Guideline NG193 [Internet]. Available from: https://www.nice.org.uk/guidance/ng193.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl): S2–S15. doi: 10.1016/j.pain.2010.09.030.
- Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–e283. doi: 10.1016/j.bja.2019.03.023.
- Carville S, Constanti M, Kosky N, et al. Chronic pain (primary and secondary) in over 16s: summary of NICE guidance. BMJ. 2021;373:n895. doi: 10.1136/bmj.n895.
- Hadi MA, McHugh GA, Closs SJ. Impact of chronic pain on patients’ quality of life: a comparative mixed-methods study. J Patient Exp. 2019;6(2):133–141. doi: 10.1177/2374373518786013.
- Dueñas M, Ojeda B, Salazar A, et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–467.
- Fayaz A, Croft P, Langford RM, et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016;6(6):e010364. doi: 10.1136/bmjopen-2015-010364.
- Karos K, McParland JL, Bunzli S, et al. The social threats of COVID-19 for people with chronic pain. Pain. 2020;161(10):2229–2235. doi: 10.1097/j.pain.0000000000002004.
- Shanthanna H, Nelson AM, Kissoon N, et al. The COVID-19 pandemic and its consequences for chronic pain: a narrative review. Anaesthesia. 2022;77(9):1039–1050. doi: 10.1111/anae.15801.
- Wilson IR. Management of chronic pain through pain management programmes. Br Med Bull. 2017;124(1):55–64. doi: 10.1093/bmb/ldx032.
- Meldrum ML. A capsule history of pain management. JAMA. 2003;290(18):2470–2475. doi: 10.1001/jama.290.18.2470.
- British Medical Association. Chronic pain: supporting safer prescribing of opioid analgesics. London British Medical Association. 2017; [cited 29 Jan 24]. Available from: analgesics-chronic-pain.pdf(bma.org.uk).
- Faculty of Pain Medicine of the Royal College of Anaesthetists. Opioids for long term pain. London Faculty of Pain Medicine. 2023; [cited 17 Jan 24]. Available from: Opioids for long term pain | Faculty of Pain Medicine (fpm.ac.uk.)
- Carnes D, Homer KE, Miles CL, et al. Effective delivery styles and content for self-management interventions for chronic musculoskeletal pain: a systematic literature review. Clin J Pain. 2012;28(4):344–354. doi: 10.1097/AJP.0b013e31822ed2f3.
- Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–813. doi: 10.1016/j.jpain.2015.05.005.
- Semmons J. The role of physiotherapy in the management of chronic pain. Anaes Inte Care Med. 2016;17:445–447.
- Pardos-Gascón EM, Narambuena L, Leal-Costa C, et al. Psychological therapy in chronic pain: differential efficacy between mindfulness-based cognitive therapy and cognitive behavioral therapy. J Clin Med. 2021;10(16):3544. doi: 10.3390/jcm10163544.
- Kabat-Zinn J. Wherever you go there you are: mindfulness meditation in everyday life. New York (NY): Hyperion; 1994.
- Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006.
- Djernis D, Lerstrup I, Poulsen D, et al. A systematic review and meta-analysis of nature-based mindfulness: effects of moving mindfulness training into an outdoor natural setting. Int J Environ Res Pub Health. 2019;16(17):3202.
- Hickey WS. The Routledge handbook of religion, medicine, and health. New York: Routledge; 2022. p. 83–97; Chapter 6, Mind Cure and mindfulness-based interventions (MBIs).
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psych. 1982;4(1):33–47.
- Goldberg SB, Riordan KM, Sun S, et al. The empirical status of mindfulness-based interventions: a systematic review of 44 meta-analyses of randomized controlled trials. Perspsychsci. 2022;17(1):108–130.
- Zhang M, Moalin M, Haenen GRMM. Connecting West and East. Int J Mol Sci. 2019;11(9):2333.
- Kirmayer LJ. Mindfulness in cultural context. Transcult Psych. 2015;52(4):447–469.
- Majeed MH, Ali AA, Sudak DM. Mindfulness-based interventions for chronic pain: evidence and applications. Asian J Psychiatr. 2018;32:79–83.
- Gu J, Strauss C, Bond R, et al. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12.
- Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31(14):5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011.
- Schutte N, Malouff J. Mindfulness and connectedness to nature: a meta-analytic investigation. Pers Ind Diff. 2018;127:10–14.
- Zeidan F, Salomons T, Farris SR, et al. Neural mechanisms supporting the relationship between dispositional mindfulness and pain. Pain. 2018;159(12):2477–2485. doi: 10.1097/j.pain.0000000000001344.
- Schütze R, Rees C, Preece M, et al. Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain. 2010;148(1):120–127. doi: 10.1016/j.pain.2009.10.030.
- Kube T, Rozenkrantz L, Rief W, et al. Understanding persistent physical symptoms: conceptual integration of psychological expectation models and predictive processing accounts. Clin Psych Rev. 2020;2020:76.
- Kiverstein J, Kirchhoff MD, Thacker M. An embodied predictive processing theory of pain experience. Rev Philos Psychol. 2022;13:973–998.
- Bissell D, Ziadni M, Sturgeon J. Perceived injustice in chronic pain: an examination through the lens of predictive processing. Pain Mgt. 2018;8(2):129–138.
- Karl JA, Fischer R. Revisiting the five-facet structure of mindfulness. Meas Instrum Soc Sci. 2020;2(1):3. doi: 10.1186/s42409-020-00014-3.
- Baer RA, Smith GT, Hopkins J, et al. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504.
- Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, et al. Does mindfulness meditation improve chronic pain? A systematic review. Curr Opin Obstet Gynecol. 2017;29(6):359–366. doi: 10.1097/GCO.0000000000000417.
- Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2.
- Marikar Bawa FL, Mercer SW, Atherton RJ, et al. Does mindfulness improve outcomes in patients with chronic pain? Systematic review and meta-analysis. Br J Gen Pract. 2015;65(635):e387–e400. doi: 10.3399/bjgp15X685297.
- Farver-Vestergaard I, O’Toole MS, O’Connor M, et al. Mindfulness-based cognitive therapy in COPD: a cluster randomised controlled trial. Eur Respir J. 2018;51(2):1702082. doi: 10.1183/13993003.02082-2017.
- Vasile D, Vasiliu O, Mangalagiu A, et al. Mindfulness-based cognitive therapy for major depressive disorder – a literature review. Eur Psychiatry. 2021;64:S494–S494.
- Mumba MN, Findlay LJ, Snow DE. Treatment options for opioid use disorders: a review of the relevant literature. J Addict Nurs. 2018;29(3):221–225. doi: 10.1097/JAN.0000000000000241.
- Ulrichsen KM, Kaufmann T, Dørum ES, et al. Clinical utility of mindfulness training in the treatment of fatigue after stroke, traumatic brain injury and multiple sclerosis: a systematic literature review and meta-analysis. Front Psychol. 2016;7:912. doi: 10.3389/fpsyg.2016.00912.
- British Pain Society. Frequently asked questions. London: The British Pain Society. 2022; [cited 2022 Apr 26]. Available from: https://www.britishpainsociety.org/people-with-pain/frequently-asked-questions/.
- Wen Y, Yan Q, Pan Y, et al. Medical empirical research on forest bathing (Shinrin-yoku): a systematic review. Envi Health Prev Med. 2019;24(1):70.
- Kaplan R, Kaplan S. The experience of nature: a psychological perspective. Cambridge (UK): Cambridge University Press; 1989.
- Ulrich RS. Aesthetic and affective response to natural environment. Behav and Nat Env. 1983;(6):85–125.
- Kellert SR, Wilson EO. The biophilia hypothesis. Washington (DC): Island Press; 1993.
- Kaplan S. Meditation, restoration, and the management of mental fatigue. Env and Behav. 2001;33:480–506.
- Friston K, Frith C. A Duet for one. Conscious Cogn. 2015;36:390–405. doi: 10.1016/j.concog.2014.12.003.
- Lumley MA, Cohen JL, Borszcz GS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. 2011;67(9):942–968. doi: 10.1002/jclp.20816.
- Stier-Jarmer M, Throner V, Kirschneck M, et al. The psychological and physical effects of forests on human health: a systematic review of systematic reviews and meta-analyses. Int J Environ Res Public Health. 2021;18:1–39.
- Stanhope J, Breed MF, Weinstein P. Exposure to greenspaces could reduce the high global burden of pain. Environ Res. 2020;187:109641. doi: 10.1016/j.envres.2020.109641.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005.
- Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6(1):245. doi: 10.1186/s13643-017-0644-y.
- Moule P, Hek G. Making sense of research : an introduction for health and social care practitioners. United Kingdom: SAGE; 2011.
- Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Cont Budd. 2011;12(1):281–306.
- Hyland T. On the contemporary applications of mindfulness: some implications for education. Jrnl Philos Edu. 2015;49:170–186.
- University of the West of England. Research ethics policies, procedures and guidance – Research ethics. Bristol: University of the West of England. 2022; [cited 2022 Dec 20]. Available from: https://www.uwe.ac.uk/research/policies-and-standards/research-ethics/policies-procedures-and-guidance.
- Albanese E, Bütikofer L, Armijo-Olivo S, et al. Construct validity of the Physiotherapy Evidence Database (PEDro) quality scale for randomized trials: item response theory and factor analyses. Res Synth Methods. 2020;11(2):227–236. doi: 10.1002/jrsm.1385.
- Maher CG, Moseley AM, Sherrington C, et al. A description of the trials, reviews, and practice guidelines indexed in the PEDro database. Phys Ther. 2008;88(9):1068–1077. doi: 10.2522/ptj.20080002.
- Choi H, Hahm SC, Jeon YH, et al. The effects of mindfulness-based Mandala coloring, made in nature, on chronic Widespread Musculoskeletal Pain: randomized trial. Healthcare. 2021;9(6):9. doi: 10.3390/healthcare9060642.
- Han JW, Choi H, Jeon YH, et al. The effects of forest therapy on coping with chronic widespread pain: physiological and psychological differences between participants in a forest therapy program and a control group. Int J Environ Res Public Health. 2016;13(3):255.
- Serrat M, Almirall M, Musté M, et al. Effectiveness of a multicomponent treatment for fibromyalgia based on pain neuroscience education, exercise therapy, psychological support, and nature exposure (NAT-FM): a pragmatic randomized controlled trial. J Clin Med. 2020;9(10):3348. doi: 10.3390/jcm9103348.
- Greenhalgh T. How to read a paper : the basics of evidence-based medicine, 5th ed. Hoboken: Wiley; 2014.
- Deaton A, Cartwright N. Understanding and misunderstanding randomized controlled trials. Soc Sci Med. 2018;210:2–21. doi: 10.1016/j.socscimed.2017.12.005.
- Anand R, Norrie J, Bradley JM, et al. Fool’s gold?: Why blinded trials are not always best. BMJ. 2020;368:l6228. doi: 10.1136/bmj.l6228.
- Gewandter JS, Eisenach JC, Gross RA, et al. Checklist for the preparation and review of pain clinical trial publications: a pain-specific supplement to CONSORT. Pain Rep. 2019;4(3):e621. doi: 10.1097/PR9.0000000000000621.
- Armijo-Olivo S, Fuentes J, da Costa BR, et al. Blinding in physical therapy trials and its association with treatment effects: a meta-epidemiological study. Am J Phys Med Rehabil. 2017;96(1):34–44. doi: 10.1097/PHM.0000000000000521.
- Littlewood C, May S. Understanding physiotherapy research. Newcastle Upon Tyne: Cambridge Scholars; 2013.
- Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. Bmj. 1995;310(6977):452–454. doi: 10.1136/bmj.310.6977.452.
- McGlothlin AE, Lewis RJ. Minimal clinically important difference: defining what really matters to patients. JAMA. 2014;312(13):1342–1343. doi: 10.1001/jama.2014.13128.
- Frahm Olsen M, Bjerre E, Hansen MD, et al. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: systematic review of empirical studies. J Clin Epidemiol. 2018;101:87–106.e2. doi: 10.1016/j.jclinepi.2018.05.007.
- Furness P. A qualitative exploration of experiences of physiotherapy among people with fibromyalgia in the United Kingdom. PainRehab. 2019;(48):37–47.
- Pannucci CJ, Wilkins EG. Identifying and avoiding bias in research. Plast Reconstr Surg. 2010;126(2):619–625. doi: 10.1097/PRS.0b013e3181de24bc.
- Vellucci R. Heterogeneity of Chronic Pain. Clin Drug Investig. 2012;32(Suppl 1):3–10. doi: 10.2165/11630030-000000000-00000.
- Boomershine CS. A comprehensive evaluation of standardized assessment tools in the diagnosis of fibromyalgia and in the assessment of fibromyalgia severity. Pain Res Treat. 2012;2012:653714. doi: 10.1155/2012/653714.
- Boonstra AM, Schiphorst Preuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31(2):165–169. doi: 10.1097/MRR.0b013e3282fc0f93.
- Breivik H. Fifty years on the Visual Analogue Scale (VAS) for pain-intensity is still good for acute pain. But multidimensional assessment is needed for chronic pain. Scand J Pain. 2016;11(1):150–152. doi: 10.1016/j.sjpain.2016.02.004.
- Feliu-Soler A, Reche-Camba E, Borràs X, et al. Psychometric properties of the Cognitive Emotion Regulation Questionnaire (CERQ) in patients with fibromyalgia syndrome. Front Psychol. 2017;8:2075. doi: 10.3389/fpsyg.2017.02075.
- Luciano J V, Aguado J, Serrano-Blanco A, et al. Dimensionality, reliability, and validity of the revised fibromyalgia impact questionnaire in two Spanish samples. Arthritis Care Res. 2013;65:1682–1689.
- Koh KB, Park JK, Kim CH, et al. Development of the stress response inventory and its application in clinical practice. Psychosom Med. 2001;63(4):668–678. doi: 10.1097/00006842-200107000-00020.
- Choi S-M, Kang T, Woo J. Development and validation of a modified form of the stress response inventory for workers. J Kor Neurpsych Ass. 2006 45(6):541–553.
- Estévez-López F, Álvarez-Gallardo IC, Segura-Jiménez V, et al. The discordance between subjectively and objectively measured physical function in women with fibromyalgia: association with catastrophizing and self-efficacy cognitions. The al-Ándalus project. Disabil Rehabil. 2018;40(3):329–337. doi: 10.1080/09638288.2016.1258737.
- Coyne JC, van Sonderen E. No further research needed: Abandoning the Hospital and Anxiety Depression Scale (HADS). J Psychosom Res. 2012;72(3):173–174. doi: 10.1016/j.jpsychores.2011.12.003.
- LoMartire R, Äng BO, Gerdle B, et al. Psychometric properties of short form-36 health survey, EuroQol 5-dimensions, and hospital anxiety and depression scale in patients with chronic pain. Pain. 2019;161(1):83–95. doi: 10.1097/j.pain.0000000000001700.
- Lee EH, Lee SJ, Hwang ST, et al. Reliability and validity of the beck depression inventory-ii among Korean adolescents. Psychiatry Investig. 2017;14(1):30–36. doi: 10.4306/pi.2017.14.1.30.
- Harris CA, D'Eon JL. Psychometric properties of the Beck Depression Inventory – second edition (BDI-II) in individuals with chronic pain. Pain. 2008;137(3):609–622. doi: 10.1016/j.pain.2007.10.022.
- Bossuyt PMM. Clinical validity: defining biomarker performance. Scand J Clin Lab Invest Suppl. 2010;242:46–52. doi: 10.3109/00365513.2010.493383.
- Begum N, Taylor JR, Brown C, et al. Morning and evening salivary cortisol levels in patients with chronic widespread pain and those at high risk. Euro J Pain. 2021;26:197–206.
- Timmers I, Quaedflieg CWEM, Hsu C, et al. The interaction between stress and chronic pain through the lens of threat learning. Neurosci Biobehav Rev. 2019;107:641–655. doi: 10.1016/j.neubiorev.2019.10.007.
- Yoon JJ, Song JA, Park SY, et al. Cytotoxic activity and subset populations of peripheral blood natural killer cells in patients with chronic pain. Korean J Pain. 2018;31(1):43–49. doi: 10.3344/kjp.2018.31.1.43.
- Davey A, Chilcot J, Driscoll E, et al. Psychological flexibility, self-compassion and daily functioning in chronic pain. J Cont Behav Sci. 2020;17:79–85.
- Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Perso Soc Psyc. 2003;84:822–848.
- Medvedev ON, Siegert RJ, Feng XJ, et al. Measuring trait mindfulness: how to improve the precision of the mindful attention awareness scale using a Rasch Model. Mindfulness. 2016;7(2):384–395. doi: 10.1007/s12671-015-0454-z.
- McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131(1-2):63–69. doi: 10.1016/j.pain.2006.12.013.
- Veehof MM, ten Klooster PM, Taal E, et al. Psychometric properties of the Dutch Five Facet Mindfulness Questionnaire (FFMQ) in patients with fibromyalgia. Clin Rheumatol. 2011;30(8):1045–1054. doi: 10.1007/s10067-011-1690-9.
- Cardaciotto L, Herbert JD, Forman EM, et al. The assessment of present-moment awareness and acceptance: the Philadelphia Mindfulness Scale. Assessment. 2008;15(2):204–223. doi: 10.1177/1073191107311467.
- Taylor PJ, Bourne K, Eames C, et al. Validating the Philadelphia Mindfulness Scale [PMS] for those with fibromyalgia. MYOPAIN. 2015;23(3-4):155–164. doi: 10.1080/24708593.2017.1314401.
- Lau MA, Bishop SR, Segal ZV, et al. The Toronto mindfulness scale: development and validation. J Clin Psychol. 2006;62(12):1445–1467. doi: 10.1002/jclp.20326.
- Tanay G, Bernstein A. State mindfulness scale (SMS): development and initial validation. Psychol. 2013;25:1289–1299.
- Baer R. Assessment of mindfulness by self-report. Curr Opin Psychol. 2019;28:42–48. doi: 10.1016/j.copsyc.2018.10.015.
- Nunan D, Aronson J, Bankhead C. Catalogue of bias: attrition bias. Evi Bas Med. 2018;23(1):21–22.
- Higgins JPT, Altman DG, Sterne JAC. Cochrane Handbook for systematic reviews of interventions version 5.2.0. Chichester: John Wiley; 2017. Chapter 8, Assessing risk of bias in included studies.
- Elkins MR, Moseley AM. Intention-to-treat analysis. J Physiother. 2015;61(3):165–167. doi: 10.1016/j.jphys.2015.05.013.
- Akobeng AK. Understanding type I and type II errors, statistical power and sample size. Acta Paediatr. 2016;105(6):605–609. doi: 10.1111/apa.13384.
- McCoy CE. Understanding the intention-to-treat principle in randomized controlled trials. West J Emerg Med. 2017;18(6):1075–1078. doi: 10.5811/westjem.2017.8.35985.
- Andrade C. Intent-to-Treat (ITT) vs completer or per-protocol analysis in randomized controlled trials. Ind J Psych Med. 2022;44(4):416–418.
- Hanley AW, Abell N, Osborn DS, et al. Mind the gaps: Are conclusions about mindfulness entirely conclusive? Jour of Counseling & Develop. 2016;94(1):103–113. doi: 10.1002/jcad.12066.
- Nilsson H, Kazemi A. Reconciling and thematizing definitions of mindfulness: the big five of mindfulness. RevGenPsych. 2016;20:183–193.
- Timko Olson ER, Hansen MM, Vermeesch A. Mindfulness and Shinrin-Yoku: potential for Physiological and Psychological Interventions during Uncertain Times. IntJournEnvResPublHealth. 2020;17:9340.
- Peterson C. “Walkabout: looking In, Looking Out”: A mindfulness-based art therapy program. ArtTherapy. 2015;32(2):78–82. doi: 10.1080/07421656.2015.1028008.
- Geneen LJ, Moore RA, Clarke C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4(4): CD011279. doi: 10.1002/14651858.CD011279.pub3.
- Bidonde J, Busch AJ, Webber SC, et al. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev; 2014
- Miaskowski C, Blyth F, Nicosia F, et al. A biopsychosocial model of chronic pain for older adults. Pain Med. 2020;21(9):1793–1805. doi: 10.1093/pm/pnz329.
- Chronic pain in adults. London: Public Health England. 2017; [cited 2022 Apr 22]. Available from: https://www.gov.uk/government/publications/chronic-pain-in-adults-2017.
- Geary RS, Wheeler B, Lovell R, et al. A call to action: improving urban green spaces to reduce health inequalities exacerbated by COVID-19. Prev Med. 2021;145:106425.
- Jordan M, Hinds J. Ecotherapy: theory, research and practice. UK: MacMillan; 2016.
- Markwell N, Gladwin TE. Shinrin-Yoku (Forest bathing) reduces stress and increases people’s positive affect and well-being in comparison with its digital counterpart. Ecopsyc. 2020;12(4):247–256.
- McEwan K, Giles D, Clarke FJ, et al. A pragmatic controlled trial of forest bathing compared with compassionate mind training in the UK: impacts on self-reported wellbeing and heart rate variability. Sustainability. 2021;13(3):1380. doi: 10.3390/su13031380.
- Raffaeli W, Arnaudo E. Pain as a disease: an overview. J Pain Res. 2017;10:2003–2008.
- Domenichiello AF, Ramsden CE. The silent epidemic of chronic pain in older adults. Prog Neuropsychopharmacol Biol Psychiatry. 2019;93:284–290. doi: 10.1016/j.pnpbp.2019.04.006.
- Larsson C, Hansson EE, Sundquist K, et al. Chronic pain in older adults: prevalence, incidence, and risk factors. Scand J Rheumatol. 2017;46(4):317–325. doi: 10.1080/03009742.2016.1218543.