ABSTRACT
With the increasing use of technology in education, online learning has become a common teaching method. How effective online learning is for undergraduate medical education remains unknown. This article’s aim is to evaluate whether online learning when compared to offline learning can improve learning outcomes of undergraduate medical students. Five databases and four key journals of medical education were searched using 10 terms and their Boolean combinations during 2000–2017. The extracted articles on undergraduates’ knowledge and skill outcomes were synthesized using a random effects model for the meta-analysis.16 out of 3,700 published articles were identified. The meta-analyses affirmed a statistically significant difference between online and offline learning for knowledge and skill outcomes based on post-test scores (SMD = 0.81; 95% CI: 0.43, 1.20; p < 0.0001; n = 15). The only comparison result based on retention test scores was also statistically significant (SMD = 4.64; 95% CI: 3.19, 6.09; p < 0.00001). The meta-analyses discovered no significant difference when using pre- and post-test score gains (SMD = 3.03; 95% CI: −0.13, 4.13; p = 0.07; n = 3). There is no evidence that offline learning works better. And compared to offline learning, online learning has advantages to enhance undergraduates’ knowledge and skills, therefore, can be considered as a potential method in undergraduate medical teaching.
Introduction
Today, digital information is everywhere and available to almost everyone. In this era of information technology, medical education is now confronted with novel challenges. On the one hand, the online healthcare information boom is continually challenging medical students to rapidly update and expand their existing body of knowledge. On the other hand, the informatic competency requirements of healthcare technology, such as utilizing electronic healthcare records, learning systems and aided-diagnosis systems, also present a new challenge for medical students to master [Citation1], even for the so-called digital native learners [Citation2].
To prepare qualified doctors for today’s environment in which the internet provides ubiquitous digital information, the teaching methods used for educating and training medical school students should be reconsidered. Offline learning, or traditional classroom teaching, represents teaching in the pre-internet era. Although some forms of information technology have already been utilized to assist instruction, traditional teaching methods required that teaching and learning should take place at the same time and place. Online learning, also called internet-based learning or web-based learning, does not have the time and space limitations, and therefore, makes teaching and learning separable via internet-based information delivery systems. Both online and offline teaching have been widely used in higher education. The use of online learning has vastly increased since 2012, as evidenced by the thriving of massive open online courses (MOOCs) [Citation3]. However, evaluating the effectiveness of online and offline teaching remains difficult. Evaluations have failed to reach consistent conclusions [Citation4,Citation5], resulting in complex decisions when selecting a teaching method for medical education.
The effectiveness of online learning is influenced by many factors. Some factors create barriers for online learning, such as administrative issues, social interaction, academic skills, technical skills, learner motivation, time and support for studies, technical problems, cost and access to the internet [Citation6]. Other factors could result in low-quality online learning, for example an ineffective design and arrangement of multimedia materials [Citation7]. The effective analysis of online and offline teaching in medical education, therefore, should depend on a comprehensive consideration of how they are used across groups. It should all be assessed including the learning goals, design properties of the learning materials, evaluation of learning outcomes, etc.
The first comprehensive systematic review and meta-analysis of online versus offline learning dates back to 2008. Cook et al. [Citation4] selected 76 articles that compared internet and non-internet based interventions and 130 articles containing no-intervention control for health professional learners. Through a meta-analysis, this study concluded that internet-based interventions were associated with positive effects compared to no interventions, but the effects and statistical heterogeneities were generally small compared to offline teaching. Richmond et al. [Citation8] then updated the evidence in this rapidly developing field by subdividing different formats of offline learning and comparing these formats to online learning. They focused their review, as well, on licensed healthcare professionals. However, this more recent evidence still suggests that online learning might be as effective as offline one for training licensed healthcare professionals, but the total effects of the online learning were low and showed no significant difference when compared to offline teaching.
Accordingly, the current meta-analysis was designed to contribute additional evidence from a new perspective in the comparison of the intervention effects of online learning versus offline learning. In contrast to previously published reviews, our analysis narrowed the target participants to undergraduate medical students and excluded postgraduates and professionals like nurses, pharmacists, veterinarians, etc. The reason why we concentrate on this specific group is that different from postgraduates’ self-motivated and clinic practice-orientated learning, undergraduate medical students are mainly driven by common core curricula and examinations stipulated by the universities’ teaching committee, which reversely, brings a sharp gap when evaluating teaching methods on these two groups of students, respectively, [Citation9]. Moreover, our study design concentrated on knowledge and skill outcomes but distinguished among different statistical methods used when generating comparison results. By testing whether online learning worked better than offline one for medical undergraduate education, this review also intended to preliminarily explore the potential factors across these two teaching methods that might cause differences in effectiveness. Identifying such differences could have implications for further research and improvements in educational practices.
Methods
Study design
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines and recommendations from the Cochrane Handbook were followed [Citation10,Citation11]. There were no requirements for an ethical review of this paper since no human participants were involved.
The objective of this systematic review was to assess how online learning compared to offline learning for teaching the medical education knowledge and skills.
Literature sources and searches
The Web of Science, Medline, Embase, PubMed and Scopus were searched for the following terms in the title and abstract: (online learn* OR web-based OR internet OR m-learning OR mobile OR distance) AND (medical edu*) AND (student* OR undergraduat* OR universit*). Four key journals of medical education, Medical Teacher, Academic Medicine, Medical Education and BMC Medical Education, were manually searched for relevant articles.
We used a search start date of January 2000 and an end date of December 2017. Because digital technologies have undergone dramatic changes since the internet first appeared in 1991 [Citation12] and internet-based hard facilities and soft applications in education have been widely accepted by schools and students starting in the 21st century [Citation13], we therefore restricted the start date to after the year 2000. The search was reconducted on May 1st, 2019.
Inclusion criteria
The included studies should meet the following criteria in adherence to the participant, intervention, comparison and outcome (PICO) search in the field of evidence-based medicine:
Participants: medical undergraduate students.
Interventions: online learning, including e-learning, m-learning, MOOCs and distance learning by video.
Comparisons: offline learning, especially referring to face-to-face teaching in a classroom, seminars, watching video lectures together in the classroom and reading text-based documents or books only.
Outcomes: knowledge and skill outcomes measured by objective assessment instruments. The mean score and standard deviations of post-test, pre- and post-test gains, or retention tests for experimental and control groups were available.
Data screening and extraction
The titles of the retrieved articles were first screened by a reviewer (P) based on the inclusion criteria. Duplicates and studies that were superficially unassociated with the comparison of online learning and offline learning were excluded. Then, the abstracts of the remaining articles were independently screened by two reviewers (P and W) based on the criteria. Any articles that seemed to be dubious based on the abstract screening were further examined by reading the full text. In the full-text screening phase, the two reviewers again worked independently to review every article against the criteria. Any conflicts between the two reviewers were resolved by consensus.
Quality assessment
The quality of methodology used in each article was evaluated based on the Medical Education Research Study Quality Instrument (MERSQI) [Citation14].
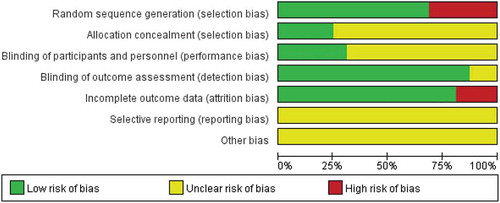
The risk of bias was assessed according to the Cochrane collaboration risk of bias assessment tool [Citation11], which contains random sequence generation (selection bias), allocation concealment (selection bias), blinding of participant and personnel (performance bias), blinding of outcome assessment (detection bias) and incomplete outcome data (attrition bias). For each of these items, the judgment of ‘low risk of bias,’ ‘unclear risk of bias’ and ‘high risk of bias’ was given with necessary supporting statements for each article.
Data synthesis
We classified the identified articles based on the statistical method of outcome, including analysis of variance (ANOVA) on post-test scores, pre- and post-test score gains and delayed retention scores. When an article contained more than one statistical method of outcome, it was clustered repeatedly into a different genre of the meta-analysis. For those articles that included multiple arms but used the same statistical method, we first considered each of the comparisons, respectively, in the meta-analysis. Then, we only included one comparison result under one genre of meta-analysis in each article, because including multiple comparison results from the same article obviously does not meet the criteria of statistical independence [Citation15].
The standard mean difference (SMD) with 95% confidence intervals (CIs) was applied for the overall effect of group comparisons in the meta-analysis. The statistical heterogeneity was calculated using the I2 statistic [Citation16]. For a high heterogeneity value (I2> 50%) [Citation17], the recommended random-effects model was used in the meta-analysis for the pool weighted effect sizes [Citation18]. The effect sizes were interpreted as 0.2 for a small effect, 0.5 for a moderate effect and 0.8 or greater for a large effect [Citation8]. We used Review Manager (RevMan 5.3) [Citation19] to carry out the meta-analyses in this review.
Results
Search results
The flowchart of article inclusion is shown in . A total of 3,680 articles were searched in five databases, and additional 20 articles were retrieved by searching four specific journals. Among them, 1,969 duplicates were removed manually, 1,275 articles were excluded based on title screening, and 389 articles were excluded based on abstract screening against the inclusion criteria. Sixty-seven full articles were then screened. However, 8 of them could not be accessed in the full text, and 43 articles were excluded against the inclusion criteria. Finally, 16 articles were remained for this systematic review.
Methodological quality
The mean (SD, range) of the total score for included articles was 13.5 (1.1, 11–15) of 18 (). All included articles used appropriate data analysis methods. Only two articles sampled from more than one institution [Citation20,Citation21]. Some of the included articles were rated lower than others, due to a lower score in the ‘validity of educational instrument’ domain (mean (SD) score of 1.5 (0.8) out of 3).
Table 1. Methodological quality of included studies.
Risk of bias
The overall risk of bias for all the included articles is shown in , and shows a detailed judgment of the risk of bias for each article. Six domains of bias were evaluated, and no article reported information about the ‘reporting bias’. Very few articles described the randomization process in detail, which possibly could be that authors considered such a description as unnecessary, and opted instead to just use the word ‘randomized.’ The true blinding of participants was nearly impossible to achieve as well because most of researchers had to describe the study for participant recruitment. However, some studies achieved participant blinding by recruiting students in different academic years as experimental and control groups, using a crossover study design or providing randomized materials.
Table 2. Risk of bias.
Synthesis of included articles
The total number of recruited participants in all the comparison results without duplications was 1,789 and the mean and range were 112 and 29–294, respectively (). The included comparisons were conducted in nine countries (USA, UK, Spain, Brazil, Germany, China, Iran, Indonesia and India).
Table 3. Details of included studies.
Sixteen identified articles were clustered by the statistical methods used (), specifically by the number of outcome comparisons. Among them, 13 articles reported only one comparison arm based on one or more statistical method based on ANOVA: 10 articles compared post-test scores [Citation20–Citation29]; 1 article compared pre- and post-test score gains [Citation30]; 1 article compared both post-test scores and pre- and post-test score gains on the same sample [Citation31]; and 1 article compared all post-test scores, pre- and post-test score gains and retention test scores on the same sample [Citation32]. All of comparison results above were included in meta-analysis but assessed under different genres. The remaining 3 articles contained more than one comparison arm but were all based on ANOVAs of post-test scores: 2 articles reported 2 comparisons using 2 different measure instruments [Citation33,Citation34]; and 1 article reported 2 comparison results for 2 different learning goals on the same sample [Citation35]. To ensure statistical independence, we only extracted one comparison result from each article for the meta-analysis. However, it is worth noting that Jordan et al. [Citation30] reported both post-test scores and pre- and post-test score gains. We only used the latter one because the baselines of the two groups were significantly different. Overall, 15 comparison results were extracted for post-test scores, 3 for pre-and post-test score gains and 1 for retention test scores.
Although all of included articles assessed knowledge or skill outcomes in medical education, there was no overlap among them. It is also worth noting that 2 articles assessed knowledge or skill outcomes that are not that specific to medical education: scientific writing [Citation20] and oral case presentation [Citation21].
The intervention durations also varied among the included articles, ranging from about 20 min to an academic semester (around 18 weeks). And one article did not report the duration.
The formats of online learning used were also various in the studies. The simplest format consisted of a CD-/DVD-based video lecture that was recorded from a live class and then uploaded to the internet, and the most advanced format was a platform that allowed students to receive static learning resources and facilitated interaction with teachers, classmates and courseware for responsive feedback.
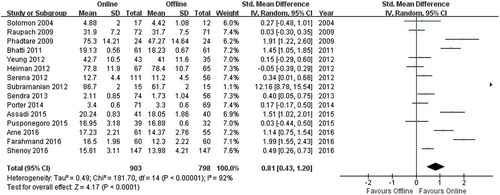
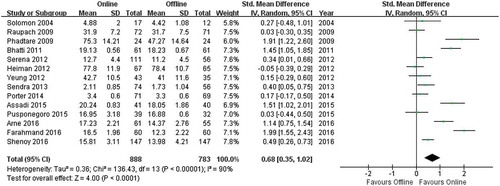
Meta-analysis based on post-test scores
shows the two groups were significantly different (Z = 4.17; p < 0.0001), with the online learning group having higher post-test scores (SMD = 0.81; 95% CI: 0.43, 1.20).
Subramanian et al. [Citation32] reported a larger SMD than the other articles, and this value could contribute heavily to the summary effect in the meta-analysis. To avoid a potential determinative influence from this single article, we conducted a separate meta-analysis on the post-test scores without this study (). There was still a significant difference (Z = 4.00, p < 0.0001) between the online learning and offline learning groups, favoring online learning (SMD = 0.68; 95% CI: 0.35, 1.02).
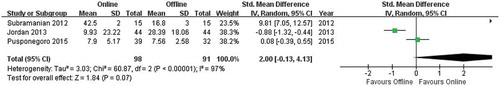
Meta-analysis based on pre- and post-test score gains
Although there was no significant difference between the groups (Z = 1.84; p = 0.07), but the gains in online learning groups trended higher (SMD = 2.00; 95% CI: −0.13, 4.13, ).
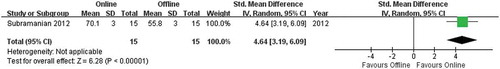
Meta-analysis based on retention test scores
The article of Subramanian et al. [Citation32] was the only study to compare retention test scores. Online learning (70.1 ± 3%) was more effective than offline learning (55.8 ± 3%) with a statistically significant difference (SMD = 4.64; 95% CI: 3.19, 6.09; p < 0.00001, ).
Discussion
In this review, reliable evidences from 2000 to 2017 were scrutinized and synthesized to answer the question: does online learning work better than offline learning for undergraduate medical students? We screened 1,731 unduplicated articles and eventually identified 16 articles that meeting the inclusion criteria. By comparing post-test scores, pre- and post-test score gains and retention test scores, we identified 7 articles that reported no significant difference between the two teaching methods and 9 articles that reported significant improvement in the online learning groups. Whether we included the article of Subramanian et al. [Citation32] or not, the changes in post-test scores indicated that online learning for medical education might be more effective than offline learning when assessed based on the outcomes of knowledge and skills. The examination of the effects on pre- and post-test score gains showed little difference between these two methods. The article of Subramanian et al. [Citation32] was the only study to use a delayed retention test, which showed online learning was better than offline learning. Overall, it suggested that online learning is at least as effective as offline learning, however we still need more research evidences to draw any firm conclusion on the comparison of online versus offline learning, since experimental designs of the included articles varied in terms of participants, learning goals, intervention durations, and forms of online learning, etc.
Although the overall finding indicated that online learning worked as well as offline learning, it didn’t imply that online learning is an effective teaching method for every student in every learning context. We note the effects of online learning reported in the article of Subramanian et al. [Citation32] stood out against the results in the other 15 articles. Through a comprehensive evaluation, we determined that the format of online learning used by Subramanian’s team, StepStone Interactive Medical Software, might have played a key role in that study, since the rich feedback and guidance, matched task difficulties to students’ developmental level [Citation36] and case-based teaching strategies designed for online learning might improve the outcomes of online learning. For online learning that consisted mainly of static, non-interactive learning resources that largely resembled offline learning, usually no significant difference was found when compared to offline learning. In addition, the knowledge and skills taught in the included studies actually only covered a small part of the learning goals in medical education. It is highly possible that online learning might not work better than offline learning for the topics that remain to be studied. Moreover, the objective assessment instruments used in the articles might not be able to evaluate the advanced capacities acquired by undergraduate medical students. Given that the objective assessments filled with multiple choice questions were more appropriate for the assessment of low-level learning goals, online learning, therefore, might only be as effective as offline learning when the learning goals are simple. Similarly, type of curriculum, usually associating largely with learning goals, might also affect the effectiveness of online and offline learning; however, it is known that undergraduate medical courses emphasized mainly on basic knowledge and skills, we still cannot speculate whether online works better than offline learning across various curriculum types before new evidence emerges. Besides above, the effectiveness could also be influenced by characteristics of students themselves, such as gender, learning style [Citation37], attitude [Citation38], satisfaction [Citation39] and level of engagement [Citation40].
The rapid growth of online learning in higher education has also benefited from the potential cost savings for limitless students [Citation41]. The undergraduates who participated in the included studies were passively arranged into an experimental or control group, and they did not have to figure out how to pay for the teaching they received, which is not realistic. A recent study, conducted in a large for-profit university with an undergraduate enrollment of more than 100,000, estimated the effects of online learning and face-to-face instruction on students’ achievement and progress. As a result, students got lower grades for both the course taken online and the courses that followed [Citation42]. Therefore, the choice of teaching method should also be made after comprehensive thought of human economic behaviors in the real world.
To some extent, online learning might not compete with some aspects of offline learning, like interactive knowledge building between teacher and students. Such limitations could create opportunities for students to obtain self-learning abilities through information technology, such as information literacy and metacognition controlling [Citation43].
The effectiveness of online learning varied, which is as or more effective than offline learning for some target knowledge and skills and also the students. To avoid the potential limitations of online learning in undergraduate medical education, it might be worthwhile to combine the advantages of online and offline teaching methods, called blended learning [Citation44]. Despite the uncertainties of online learning, it should be allowed in undergraduate medical education, but to maximize the benefits, a combination of online and offline learning might be the most effective.
Limitations
There are still some limitations of this study. First, the small number of included studies. Although we actually used a relatively broad search strategy, but when narrowed down based on the inclusion criteria, only 16 articles were eventually identified and the total number of participants was 1,789, including 947 in online learning groups and 842 in offline learning groups. It should also be emphasized that the meta-analyses did not differentiate knowledge outcomes from skill outcomes [Citation45] but regarded these two categories of outcomes as equal. What was discriminated were the statistical methods. Second, the different statistical heterogeneities of the meta-analyses with and without the article of Subramanian et al. [Citation32] complicated conclusions about the effectiveness of online versus offline learning.
Further research
Despite some outstanding questions, the findings of this review offer supporting evidence on the effectiveness of online learning in undergraduate medical education. Further research is needed to clarify the effects of online learning and the conditions under which it can be effectively used. Whether online learning works as a direct or mediated factor in improving achievement needs to be assessed, as do what design and delivery strategies for online learning works in practice. How the advantages of online learning can be used to amplify other teaching methods for undergraduate medical students also needs to be studied. The design of the assessment instruments and curriculum types used for online learning requires further study. It is possible that students do acquire knowledge and skills through online learning that cannot obtain through offline learning, and this knowledge could compensate for the loss of knowledge and skills identified by questionnaires for offline learning.
Conclusion
Although not all of the included research studies reported that using online learning methods in medical education was more effective than offline learning, none of the included studies concluded that online learning was less effective than offline methods, regardless of the statistical method used. We need to recognize that online learning has its own advantages for enhancing students’ learning and should be considered a potential teaching method in medical education. To guarantee the effectiveness of online learning, the design principles of digital learning materials, learning goals and students’ preferences and characteristics should be rigorously evaluated.
Ethics approval
Not applicable.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Triola MM, Friedman E, Cimino C, et al. Health information technology and the medical school curriculum. Am J Manag Care. 2010;16(12Suppl HIT):54–13.
- Thompson P. The digital natives as learners: technology use patterns and approaches to learning. Comput Educ. 2013;65(7):12–33.
- Daniel J. Making sense of MOOCs: musings in a maze of myth, paradox and possibility. Open EducRes. 2013;2012(3):18.
- Cook DA, Levinson AJ, Garside S, et al. Internet-based learning in the health professions: a meta-analysis. Jama. 2008;300(10):1181.
- Bartley SJ, Golek JH. Evaluating the cost effectiveness of online and face-to-face instruction. J Educ Technol Soc. 2004;7(4):167–175.
- Muilenburg LY, Berge ZL. Student barriers to online learning: a factor analytic study. Distance Educ. 2005;26(1):29–48.
- Mayer RE. Multimedia learning. Psychol Learn Motiv. 2002;41(1):85–139.
- Richmond H, Copsey B, Hall AM, et al. A systematic review and meta-analysis of online versus alternative methods for training licensed health care professionals to deliver clinical interventions. BMC Med Educ. 2017;17(1):227.
- Davis J, Chryssafidou E, Zamora J, et al. Computer-based teaching is as good as face to face lecture-based teaching of evidence based medicine: a randomised controlled trial. Med Teach. 2007;7(1):23.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Epidemiol Biostat Public Health. 2009;6(4):e1–e34.
- Higgins JPGS, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [cited 2011 Mar]. Available from: http://handbook.cochrane.org In: The Cochrane Collaboration; 2011.
- Demers E, Lev B. A Rude awakening: internet shakeout in 2000. Rev Account Stud. 2001;6(2–3):331–359.
- Cattagni A, Farris E. Internet access in U.S. Public schools and classrooms: 1994-2000. Educ Stat Q. 2001;3(4):85.
- Reed DA, Cook DA, Beckman TJ, et al. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–1009.
- Brydges R, Manzone J, Shanks D, et al. Self-regulated learning in simulation-based training: a systematic review and meta-analysis. Med Educ. 2015;49(4):368–378.
- Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Br Med J. 2003;327(7414):557–560.
- Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. Jama. 2011;306(9):978.
- Cook DA. Randomized controlled trials and meta-analysis in medical education: what role do they play? Med Teach. 2012;34(6):468–473.
- Review Manager (RevMan) [computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014.
- Phadtare A, Bahmani A, Shah A, et al. Scientific writing: a randomized controlled trial comparing standard and on-line instruction. BMC Med Educ. 2009;9(1):1–9.
- Heiman HL, Uchida T, Adams C, et al. E-learning and deliberate practice for oral case presentation skills: A randomized trial. Med Teach. 2012;34(12):820–826.
- Bhatti I, Jones K, Richardson L, et al. E-learning vs lecture: which is the best approach to surgical teaching? Colorectal DisOff J Ass Coloproctol. 2011;13(4):459–462.
- Chao SH, Brett B, Wiecha JM, et al. Use of an online curriculum to teach delirium to fourth‐year medical students: a comparison with lecture format. J Am Geriatr Soc. 2012;60(7):1328–1332.
- Yeung JC, Fung K, Wilson TD. Prospective evaluation of a web-based three-dimensional cranial nerve simulation. J Otolaryngol Head Neck Surg. 2012;41(6):426–436.
- Porter AL, Pitterle ME, Hayney MS. Comparison of online versus classroom delivery of an immunization elective course. Am J Pharm Educ. 2014;78(5):96.
- Assadi T, Mofidi M, Rezai M, et al. The comparison between two methods of basic life support instruction: video self-instruction versus traditional method. Hong Kong J Emerg Med. 2015;22(5):291–296.
- Arne P, Klaus K, Cord S. Self-directed learning can outperform direct instruction in the course of a modern German medical curriculum – results of a mixed methods trial. BMC Med Educ. 2016;16(1):158.
- Farahmand S, Jalili E, Arbab M, et al. Distance learning can be as effective as traditional learning for medical students in the initial assessment of trauma patients. Acta Med Iran. 2016;54(9):600.
- Shenoy SJ, Kuriakose C. Effects of E-learning as a teaching learning method in medical education. J Evol Med Dent Sci. 2016;99(5):7272–7275.
- Jordan J, Jalali A, Clarke S, et al. Asynchronous vs didactic education: it’s too early to throw in the towel on tradition. BMC Med Educ. 2013;13(1):105.
- Pusponegoro HD, Soebadi A, Surya R. Web-based versus conventional training for medical students on infant gross motor screening. Telemed J E Health. 2015;21(12):992.
- Subramanian A, Timberlake M, Mittakanti H, et al. Novel educational approach for medical students: improved retention rates using interactive medical software compared with traditional lecture-based format. J Surg Educ. 2012;69(2):253–256.
- Raupach T, Muenscher C, Anders S, et al. Web-based collaborative training of clinical reasoning: A randomized trial. Med Teach. 2009;31(9):e431.
- Sendra-Portero F, Torales-Chaparro OE, Ruiz-Gómez MJ, et al. A pilot study to evaluate the use of virtual lectures for undergraduate radiology teaching. Eur J Radiol. 2013;82(5):888.
- Solomon DJ, Ferenchick GS, Laird-Fick HS, et al. A randomized trial comparing digital and live lecture formats [ISRCTN40455708. BMC Med Educ. 2004;4(1):1–6.
- Yavner SD, Pusic MV, Kalet AL, et al. Twelve tips for improving the effectiveness of web-based multimedia instruction for clinical learners. Med Teach. 2015;37(3):239–244.
- Terrell SR, Dringus L. An investigation of the effect of learning style on student success in online learning environment. J Educ Technol Syst. 2000;28:3.
- Omar ND, Hassan H, Atan H. Student engagement in online learning: learners attitude toward E-mentoring. Procedia Soc Behav Sci. 2012;67(67):464–475.
- Johnson SD, Aragon SR, Shaik N, et al. Comparative analysis of learner satisfaction and learning outcomes in online and face-to-face learning environments. J Interact Learn Res. 2000;11(1):29–49.
- Robinson CC, Hullinger H. New benchmarks in higher education: student engagement in online learning. J Educ Bus. 2008;84(2):101–109.
- Deming DJ, Goldin C, Katz LF, et al. Can online learning bend the higher education cost curve? Am Econ Rev. 2015;105(5):496–501.
- Bettinger EP, Fox L, Loeb S, et al. Virtual classrooms: how online college courses affect student success. Am Econ Rev. 2017;107(9):2855–2875.
- Friedman CP, Donaldson KM, Vantsevich AV. Educating medical students in the era of ubiquitous information. Med Teach. 2016;38(5):504–509.
- Garrison DR, Vaughan ND. Blended Learning in Higher Education: Framework, Principles, and Guidelines. New York (NY): John Wiley & Sons; 2007; ix–xi.
- Rees EL, Quinn PJ, Davies B, et al. How does peer teaching compare to faculty teaching? A systematic review and meta-analysis. Med Teach. 2015;38(8):829–837.