ABSTRACT
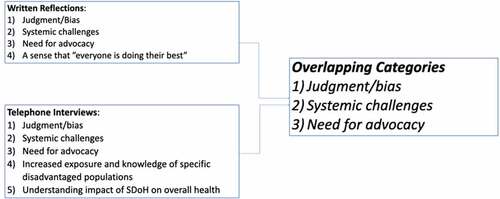
Social Pediatrics is the newest mandatory rotation in the General Pediatrics residency program at the University of Alberta. Evaluation of the residents include a written reflective assignment, asking them to identify assets and disparities that have influenced the health of a child encountered on the rotation. While there are many published papers on reflective writing , few papers are found in the area of how social determinants of health (SDoH) impact an individual’s overall health. This study examines the question: how has exploring SDoH during the Social Pediatrics rotation led to changes in residents’ awareness of their own practice of pediatrics? Grounded theory was used to analyse 35 reflections from residents who had submitted them as a mandatory assignment at the end of their rotation. In addition, 10 semi-structured telephone interviews were conducted to further understand residents’ perceptions. Interviews were transcribed verbatim and analysis of the reflections and interviews was guided by grounded theory using open, axial, and selective coding. Analyses of written reflections revealed the following categories: 1) judgment/bias, 2) systemic challenges, 3) advocacy, and 4) a sense that everyone is doing their best. Interview data reinforced overlapping categories of bias, systemic challenges and advocacy in addition to two new categories: 1) increased exposure and knowledge of specific disadvantaged populations, and 2) understanding impact of SDoH on overall health.
Categories that were generated highlight the importance of residents’ education regarding the role of SDoH on overall health and management plans. They became aware of structural determinants of health working with health-care professionals who were advocates for the communities they worked with. Analysis of residents’ written reflection assignments and follow-up interviews revealed the value of reflective practice in physician development and reinforced the benefit of fostering experiences not typically encountered in traditional clinical learning environments.
Introduction
Social determinants of health (SDoH) have been shown to have a greater impact on one’s overall health than one’s genetics or biology [Citation1]. Yet, it is a topic that until recently, has not been recognized by medical schools as an important concept to include in medical school curricula. In the paper by Denizard-Thompson et al., they comment that ‘an increasing number of US medical schools have begun to recognize the need for health equity curricula that include issues such as access to care, housing instability, and racial/ethnic bias’ [Citation2, pp.2/11]. They also reference papers that recognize that classroom-based experiences without community involvement may not be very beneficial [Citation3]. Gilles Julien, who is considered to be the founder of Social Pediatrics in Canada, describes Social Pediatrics as a model of integrated social medicine [Citation4]. He frames it as a community-based model which respects family cultures and the fundamental rights of children. It combines medicine, law and social sciences to identify needs and take effective action to reduce or eliminate toxic stressors that affect the development of children.
The Royal College of Physicians and Surgeons espouses that physician should function as health advocates and ‘responsibly use their expertise and influence to advance the health and well-being of individual patients, communities, and populations’ [Citation5, pp.11]. A study done at the University of Ottawa medical school had a group of students during the Covid-19 pandemic, follow a social pediatric model for six weeks during clerkship. The control group completed the regular six week core pediatrics rotation. The intervention group had ‘a stronger overall grasp on the CanMEDS roles as compared to the control group. Such roles included those of Communicator, Health Advocate, Medical Expert, Collaborator, Leader/Manager and Professional’ [Citation6, pp.2]. Pediatrics is the newest mandatory rotation added to the General Pediatric residency training program at the University of Alberta. Understanding the social, structural and political-economic determinants of health in the community (poverty, unemployment, food insecurity, early child development, health services, colonialism, etc.) is a necessary foundation to effectively provide recommendations and treatment to individual patients and their families. This foundation also provides residents with a framework and the skills necessary for intervention and advocacy to improve the health of children, families, and communities.
Many Canadian pediatric residency training programs now have a Social Pediatrics rotation, as a mandatory or an elective rotation. Other programs aim to have the objectives met by incorporating these concepts throughout other rotations. Our mandatory four-week rotation has been designed to provide focused training on community engagement, SDoH, advocacy, public health, health policy, and social justice. The rotation provides a community service learning opportunity for pediatric residents to gain a better appreciation of the environment in which their patients live, learn and grow; and how the environment affects patient health and accessibility to health services. The Social Pediatrics rotation aims to place residents in clinics or community programs that will give them exposure to the following seven populations that have unique needs and barriers to care: 1) adolescents, 2) inner city youth, 3) children in care, 4) child protection services, 5) indigenous children, 6) rural communities, and 7) new Canadians. Unlike other rotations in the residency program, the evaluation process involves a final written reflective assignment asking the resident to map and assess the assets and disparities that have influenced the health and life of a child they encountered on the rotation.
Reflective writing is becoming more common in medical school curricula, especially in North America. Chen and Forbes’ [Citation7] review showed that reflective writing in medical education leads to many positive effects, including an increase in empathy towards patients. Another study examined an online curriculum on care delivery in the medical home. This was offered to third-year pediatric residents who were asked reflective questions [Citation7]. The residents identified their need to improve their understanding of SDoH and systems issues to allow for better care for their patients and families. R.B. Levine et al. [Citation8] looked at written reflections by internal medicine residents, who revealed the process led to deeper reflection and a desire to improve.
A paper by Plant et al. examined reflection in the clinical setting by pediatric residents and faculty. They found that although clinical reflection occurred, ‘they did not always explicitly identify it as reflection or reflect in growth-promoting ways’ [Citation9, pp. S75]. A study by van den Heuvel et al. evaluated a social pediatrics elective for medical students through reflective writing. The most common theme that emerged was learners commenting on social determinants of health. The authors concluded transformative learning occurred through students’ new experiences with interacting with patients in their home communities and environments [Citation10]. Although there are published papers on written reflections during medical school and some during residency training, limited research exists in the area of Social Pediatrics and the interplay between the social determinants of health (SDoH) and their impact on a patient’s ability to access care and the health-care team providing that care. Intentionally reflecting on the SDoH and their impact on a child’s health may increase health-care practitioners’ awareness of factors that influence their practice. The aim of our study was to collate and analyze general pediatrics residents’ written reflective assignments from a Social Pediatrics rotation to describe how exploring SDoH impacts resident’s awareness of their own practice.
Methods
Study design
Citation11] was used for this study. In this qualitative design, the researcher generates a theory or uncover relationships and behavior as well as studies social processes. Ontologically grounded theory is rooted in sociological theories, such as pragmatism and symbolic interactionism. Grounded theory assumes that the objective reality is complex, overlapping, contradictory and that knowledge is developed retrospectively. Additionally, grounded theory also examines interactions and actions, and that the reality is intersubjective based on interactions and shared meanings. Epistemologically, it is rooted in positivism and constructionism. We have followed the positivist approach of Strauss and Corbin (1998), which states that objective reality should not be impacted by the researchers’ interpretations of it [Citation11]. This means that we analysed our data objectively by making sure that the researches’ biases,feelings, and thoughts did not weave into the data. In this approach the phenomenon under investigation is ‘grounded’ in the databy using various sources and methods of data generation from study participants. Grounded theory approach was used as it enabled us to gain in-depth knowledge of how SDoH impacts postgraduate trainees while providing care to patients.
Study participants
Study participants were residents in an accredited Canadian Pediatrics Residency Program between 2016 and 2020 who had completed a 4 week Social Pediatrics rotation during their second year of training. This rotation was self-scheduled by the residents who were given a list of possible placements they may participate in, a diverse range of clinical experiences they are not routinely exposed to or made aware of during other rotations. One of our authors is the preceptor overseeing the rotation making sure schedules and objectives are reviewed. The resident also discusses their final written assignment with their preceptor one or two days after it has been submitted. In addition, following initial data analysis of reflection assignments (n = 35) and using purposeful sampling, a subset of these residents participated in follow-up telephone interviews (n = 10). This study was approved by the Health Research Ethics Board (HREB) at the University of Alberta.
Data sources
The primary source of data for the grounded theory analysis were the written reflective assignments submitted by the residents. For these assignments, residents were required to identify a patient who had a significant impact on them during their rotation and, using the SDoH framework, describe and reflect upon both disparities and individual and community assets that influenced the health of that child. Residents also submitted disparities and assets maps as a visual aid to illustrate connections between individuals, their communities and their disparities and assets. In addition, residents were asked to reflect upon the following questions:
1) Were any of your assumptions challenged or validated?
2) Did you gain any significant insights about yourself (cognitive and/or emotional)?
3) How might your experience change your practice of medicine?
Following initial analysis of the written assignments, semi-structured telephone interviews lasting 35–60 minutes were conducted with a subset of study participants. All residents who had taken the course were invited to take part in the interviews. It is vital to note that we stopped collecting data because we had reached saturation. A point where we were not hearing any new information from our study participants. We developed an interview guide that was piloted with a resident on this study who had taken the Social Pediatrics rotation in previous years. Residents were asked to recall their overall experience with the Social Pediatrics rotation, elaborate on the patient interaction discussed in their written reflection and, if applicable, further discuss themes identified in their written reflection. These were performed by a resident (KC) and a qualitative researcher (MR). The first three interviews were done together for training purposes, and subsequent interviews were completed by KC.
Data analysis
Three clinicians (KC, MC, JW) and one qualitative expert (MR) independently read the residents’ reflections. Finally, the principal investigator (BI), who is the Social Pediatrics rotation coordinator, also read and coded the data to confirm the identified categories and to ensure relevant information was not missed.
For our telephone interviews, two clinicians (KC, BI) and one qualitative expert (MR) read and analyzed the data. An iterative process of reading and coding each writing assignment and interview transcripts was used until categories reached saturation. Our analysis was guided by grounded theory and by employing the following three steps: 1) Open Coding: Reflections and interviews were analyzed by describing common instances found throughout the data. In this phase, we were involved in breaking our data into segments that reflected particular meanings. 2) Axial Coding: Once we were able to get familiar with our data and got a better understanding of which types of common codes were relevant to students in their social rotations, we then started labeling and assembling these codes into broad categories through constant comparison. 3) Selective Coding: In this phase of our analysis, our categories were integrated and refined into larger abstract schema. During selective coding, decisions were made regarding data saturation. Saturation is a point at which during data analysis no new information appears to be arising from the data being analysed [Citation12]. Saturation of categories was achieved through a search for repeated instances of categories, increased elaboration of identified categories, ongoing data review, and subsequent data collection, as needed.
Trustworthiness
One of the first steps to ensure trustworthiness is by determining methodological congruence. This means evaluating the fit between the various components of the study design. For example, does the method fit with the research question? Does the type of strategy for data generation fit with the chosen method? Finally, is the analysis congruent with the strategy [Citation13]. Furthermore, we used memos as one way to demonstrate trustworthiness by showing evidence of thoughts and creating an audit trail for study transferability. Throughout our study, we focused on developing appropriate codes that fit the data and the reflexive process of cross-checking new codes consistently to ensure reliability. To help minimize the effects of researchers’ presumptions, informal meetings (peer debriefing) were regularly conducted to discuss our thoughts, feelings and emotions while analyzing the data. By having regular meetings, it allowed us to step back from the data and determine whether we were bringing our own preferences into the analysis. We used memos during the analysis to keep track of decisions made in regard to coding and abstraction [Citation13].
Results
We analyzed 35 written reflections from second-year pediatrics residents who completed their Social Pediatrics rotation as part of their General Pediatrics residency at the University of Alberta. From those residents, 10 were recruited via theoretical sampling for a subsequent telephone interview. Of those, the majority remained in residency at the time of interview (PGY3 – 1, PGY4- 6, PGY5- 1) and one was a staff pediatrician.
Based on our analysis, the written reflections revealed four saturating categories: 1) judgment/bias, 2) systemic challenges, 3) need for advocacy and 4) the sense that everyone is doing their best. As with the written reflections, the telephone interviews resulted in the three similar categories of judgment/bias, systemic challenges, and advocacy saturating, along with the additional two categories: 1) exposures to new populations and locations; and increased knowledge of specific disadvantaged populations; and 2) understanding the impact of SDoH on overall health (). includes direct quotes taken from written reflections and interviews, which highlight each of the saturated categories as listed below.
Table 1. Findings: Saturated Categories from Reflections and Interviews
Category 1: Judgment/Bias
Residents expressed experiencing direct bias towards their patients and their families in a variety of situations. Some residents noted biases wherein they assumed patients would be doing poorly based on the contexts in which they were seeing them. Interestingly, a number of implicit biases were evident in the residents’ reflections (). These were directed towards patients, their family members or their environments. The residents also described implicit biases regarding certain families’ ability to cope with the challenges of having a sick child.
In addition to realizing biases towards certain patients, there were circumstances wherein residents felt biases directed towards themselves. This was expressed (quotes in ) with reference to both clinical situations and educational events that residents attended. Most frequently residents commented on biases they felt in the form of racism. They also identified the importance of being aware of, and challenging biases, most notably their own and those of their colleagues. Furthermore, some acknowledged the need to actively prevent these biases from affecting their work and patient care.
Category 2: Systemic challenges
Within the written reflections and interviews, residents frequently commented on systemic limitations that impacted their patients. In general, they identified access to care as a major barrier, in addition to a sense that the healthcare system was failing their patients. Limitations in certain geographical locations, such as rural and First Nations reserve communities, were most often identified as having increased barriers to care. Even when geographical location is not a barrier, many residents identified that certain disadvantaged populations experienced challenges in accessing services due to various logistical challenges, such as not having personal identification, fixed addresses or even a telephone for communication of appointments.
Experiencing a shortage of resources also arose as a systemic challenge that residents faced in caring for their patients. Specifically, many residents noted that resources for mental health and help for substance users were particularly challenging to access. Many residents felt as though the healthcare system was failing certain patients especially those in foster care. The feeling that the system was failing these children, came up frequently.They also felt that a lack of focus in preventative health led to more disparties in , the general system as a whole.
Category 3: Need for advocacy
Residents reported numerous experiences wherein they witnessed advocacy or expressed increased recognition for the need to advocate for individual patients. Similarly, residents reflected on the importance of advocating for patients in such a way that aligns with the patient and family’s goals through patient-centered care. What’s more, some residents expressed that their experiences throughout their Social Pediatrics rotation sparked increased desire to advocate for patients in their future career.
Category 4: Everyone is doing their best
Residents frequently highlighted that throughout their Social Pediatrics rotations they were exposed to patients, families and health-care providers who, despite many challenges, were doing their best to provide care. Many people expressed parents’ efforts as an asset to their patients’ overall health, often despite their own challenges. In addition to this, residents described challenges in providing care in clinics or contexts wherein patients frequently have more complex social circumstances. They described that sometimes it is not realistic to make perfect management plans that are ‘by the book,’ but that some degree of compromise is necessary.
Category 5: Increased exposure and knowledge of specific populations and locations
Our study participants reported ‘eye opening’ exposures to new communities during their rotation, specifically reserve communities, and outreach clinics in rural centres as far as 800 km away from Edmonton. Given that Edmonton has a large encatchment area, the rotation gave residents a chance to see the communities that many of their patients live in. Other residents commented () on the unique experiences that were part of the Social Pediatrics rotation including opportunities for intentional exposure to specific population groups. These included new immigrants to Canada, children in foster care, high-risk youth, and adolescent mothers.
Many residents identified that these exposures to specific marginalized populations and remote locations developed their approach to history-taking, specifically targeting social determinants of health in addition to more traditional review of systems. What’s more, residents commented that their experiences gave them increased confidence to have what are often perceived as difficult conversations regarding more sensitive subjects, such as finances, trauma and abuse. They also displayed awareness of asking questions to ensure the management plan is suitable for the patient and their family.
Residents also identified that their rotation gave them increased knowledge of community resources and how to access them. They emphasized the importance of not only being aware of resources, but also learning how to access them and support patients in doing so.
Category 6: Increased understanding of SDoH on overall health
Residents frequently commented on an expanded understanding of SDoH and how these impacted the care of their patients. Many residents discussed the importance of the environment in which their patients shaped their care, including family structure, living circumstances and finances. In addition to the aforementioned factors, exposure to adverse childhood experiences (ACEs) in the children or their family members was commented upon as a source of adversity (). The residents expressed that although they were aware of the importance of living environments on health prior to their Social Pediatrics rotation, having a firsthand look into the lives of their patients reiterated this and made it more meaningful. Perhaps as equally as important as an increased awareness of SDoH, residents expressed how these must be accounted for in providing patient-centered care.
Discussion
This is the first study to our knowledge to explore learning around the social determinants of health, its influence on access to care, and the health-care team providing that care through reflective writing. The four saturating categories that were generated from the written reflections were judgment and bias, systemic challenges, need for advocacy, and a sense that everyone is doing their best. The telephone interviews revealed the first three categories (bias, systemic challenges, advocacy) with overlapping saturation, along with two new categories: an increased exposure and knowledge of disadvantaged populations, and understanding the impact of SDoH on overall health.
Generated theories for teaching SDoH in residency
The three overlapping categories from the written reflections and interviews (bias, systemic challenges, advocacy) are key concepts one must wrestle with in the pursuit of equitable healthcare, but these topics are not explicitly taught during medical school or residency. The interviews revealed that when residents approached clinic encounters using a social pediatrics lens, they were able to understand the true impact SDoH play on the overall health of a child. The residents acknowledged the importance of checking their own biases and judgment before interacting and assessing patients. Many conscious and unconscious biases in medicine are not just from ones carried over from past life experiences and belief systems, but also ones the learner has unconsciously picked up during their training from fellow trainees and staff physicians whom they may respect. This forms part of a hidden curriculum steeped in the inherent biases of western (some would say colonialist) medical system that affects how we approach and treat people of different demographics and cultures. More and more cases of racial biases in Canada’s healthcare system are now being highlighted in the mainstream media. In 2008, Brian Sinclair, an indigenous man, died in a Winnipeg emergency department while waiting 34 hours for care. Although an inquest and final report completed in 2014 concluded that his death was preventable, Barry Lavallee, a professor at the University of Manitoba and a member of the Brian Sinclair Working group states, ‘The recommendations from the inquest itself did not and will not interrogate racism.’ The working group’s interim report, Out of Sight, concludes Sinclair’s death was a result of racism in the health-care system [Citation14]. A more recent case in the news in 2020 was that of Joyce Echaquan, an indigenous woman in Quebec, who filmed hospital staff taunting her. She died later the same day she filmed the video [Citation15]. A systematic review looking at implicit bias in health-care professionals indicated that implicit bias leads to disparities in healthcare [Citation16].
Residents also came to appreciate the systemic challenges in our healthcare system and the importance of advocacy by working with health-care practitioners who delivered care in locations that do not have the physical or human resources as a tertiary care centre does. On the Government of Canada website for Canada’s Health-Care System [Citation17], fiscal restraint is listed as a challenge for how services are delivered. It is well known that there is a high cost in delivering healthcare to our remote communities and the vast distances that families need to travel in order to access healthcare. The lack of or limited access to quality healthcare is not truly appreciated until one works outside urban center (where most training programs are situated). During the rotation, residents were able to travel to outreach clinics in Northern Alberta (including ones that they needed to fly to) and on First Nations reserves. Similarly, the learners were able to experience firsthand the barriers facing homeless youth when working in a clinic situated in a youth shelter, and the struggles individuals face when they present to a clinic in the inner city. Through these placements they witnessed the importance of addressing health inequities by advocating for those who live in underserved and resource-poor settings. By working with preceptors who worked in these settings, they learned how to advocate for services, supplies, and medications in different ways than they were traditionally used to, i.e., regular healthcare coverage.
The additional categories that were saturated from the interviews confirmed that the main objectives of the rotation were met: the learner was exposed to new populations that they had little to no previous experience with and saw first hand how SDoH impacted the patient-centered care they were able to deliver. This is a crucial finding to highlight. It is well known that trainees most frequently will settle to practice in the community or a community similar to ones they have been already exposed to in their life and/or during their training. If they have not worked with or been exposed to certain populations such a Indigenous families on a reserve, refugee families being seen in a resource poor clinic etc., they do not incorporate or consider these settings into their future careers. A questionnaire-based study by Larkins et al. [Citation18] showed recruiting trainees from underserved groups (lower socio-economic, non-urban status) led to a higher proportion of students who intended to practice in non-rural settings. The University of British Columbia (UBC) has successfully placed increasing numbers of graduated physicians in more northern and remote communities by expanding and distributing medical education. As a result, more undergraduate and graduate trainees were placed in more rural settings. The ‘evidence shows that as students gain exposure to the people and places, as well as the rewards of practice, they are more likely to set up shop there’ [Citation19]. This is the reasoning behind why training programs are advocating for more funding directed to train rural physicians. During their rotation, the residents witnessed the importance of SDoH in the delivery of healthcare and recognized that resources are disproportionately allocated to urban and hospital settings.
Limitations
As with any research study, we identified some limitations to our study. Firstly, our data was collected from a single institution. In future, it may be beneficial to expand similar studies to other pediatrics residency programs and other specialties across the country. Secondly, given that there are approximately 10 residents completing the Social Pediatrics rotation per year, there is limited availability of data to analyze at any given time. This similarly may be addressed by expanding the study to other residency programs. Finally, the principal investigator also leads the Social Pediatrics rotation; the possibility of bias was mitigated by having clinicians and researchers code the data and ensure reflexivity.
Conclusion
During the four-week Social Pediatrics rotation, residents work with underserved populations in their home communities and gain an understanding of the structural and social barriers families face that impact the wellbeing and health-care needs of their children. We believe this is a new and innovative rotation as showcased by the resulting work produced by the residents in their final reflective assignment. The assignments have been rich in content and common categories were generated. These categories can be used not only to reinforce the importance of a social pediatric rotation during pediatric residency training, but one can extrapolate these findings to highlight the importance of social medicine teachings earlier in training and across all disciplines. Advocacy is something that cannot be taught in a classroom setting, one can model behavior and have mentors. Physicians learn and are motivated to advocate for their patients once they start clinical work and notice disparities in care. The learners who participated in this study learned from the health-care professionals they worked with. The staff helped highlight the social determinants of health, which needed to be addressed but also helped to teach the learners about the structural determinants of health, which require us as a society as a whole, to address. Only once we do so, can we then start to address the inequities that exist in our healthcare system in all domains.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Andermann A. Taking action on the social determinants of health in clinical practice: a framework for healthcare professionals. Cmaj. 2016;188(17–18):E474–E483.
- Denizard T. Association of health equity curriculum with medical students’knowledge of social determinants of health and confidence in working with underserved populations. JAMA Network Open March. 2021;4(3):210–10.
- Doobay-Persaud A. Teaching the social determinants of health in undergraduate medical education: a scoping review. J Gernr Intern Med. 2019;34:239–720.
- Canadian Encyclopedia. 2022 https://www.thecanadianencyclopedia.ca/en/article/gilles-Julien. Cited 2022 Feb 8.
- Jr F, Snell L, Sherbino J. CanMEDS 2015 Physician CompetencyFramework. Eds. Ottawa, ON: Royal College of Physicians and Surgeons of Canada. 2015.
- Daccache J, Khoury M, Habibi C, et al. More than Just Soup: use of a Student-LedCOVID-19 Social Pediatrics Initiative to Propose the Integration of Social MedicineElectives in Undergraduate Medical Education. J of Med Educ Curric Dev. 2020: 71–75
- Chen I, Forbes C. Reflective writing and its impact on empathy in medical education: systematic review. J Educ Eval Health Prof. 2014;16(11):20.
- Levine RB, Kern DE, Wright SM. The impact of prompted narrative writing during internship on reflective practice: a qualitative study. Adv Heal Sci Educ. 2008;13(5):723–733.
- Plant J, Li S, Blackenburg R, et al. Reflective practice in the clinical setting: a multiinstitutional qualitative study of pediatric faculty and residents. Acad Med. 2017;92(11S):S75–84.
- van den Heuvel Meta et al, et al. Evaluation of a Social Pediatric Elective: transforming institutional qualitative study of pediatric faculty and residents. Acad Med 53(6) 549–555 doi:10.1177/0009922814526974 .
- Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks: SAGE Publications; 2014.
- Morse JM, Richards L. README FIRST for a user’s guide to qualitative methods. Thousand Oaks: SAGE Publications; 2002.
- Morse JM, Barrett M, Mayan M, et al. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Res. 2007;1(2): 13–22
- CBC. 2017. https://www.cbc.ca/news/canada/manitoba/winnipeg-brian-sinclair-report-1.4295996. Cited 2022 Feb 8.
- https://www.cbc.ca/news/canada/montreal/joyce-echaquan-inquiry-toxicology-1.6042783. Cited 2022 Feb 8.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Government of Canada. Canada’s Health Care System. 2019. https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html. Cited 2021 Nov 24
- Larkins S, Michielsen K, Iputo J, et al. Impact of selection strategies on representation of underserved populations and intention to practise: international findings. Med Educ. 2015;49(1):60–72.
- Fleming P, Mari-Lynne S. Rural physician supply and retention: factors in the Canadian context. Can J Rural Med. 2018;23(1):15–20.