ABSTRACT
Purpose. Suicide is a major cause of preventable death worldwide. Adequate training in risk assessment and intervention is key to suicide prevention. The use of simulation (role plays, simulated patients, virtual reality…) for practical training is a promising tool in mental health. The purpose of this study was to assess the effectiveness of simulation training in suicide risk assessment and intervention for healthcare professionals and gatekeepers. Methods. We conducted a systematic review in Medline and PsycINFO up to 31 July 2021 of randomized controlled trials (RCTs), non-randomized controlled trials, and pre/post-test studies. RCTs were furthermore included in a meta-analysis. We assessed the methodological quality of all studies with the Medical Education Research Study Quality Instrument, and the Cochrane Risk of Bias tool 2.0 for RCTs. Primary outcomes were changes in Kirkpatrick criteria: attitudes, skills, knowledge, behaviors, and patient outcomes. Results. We included 96 articles representing 43,656 participants. Most pre/post-test (n = 65) and non-randomized controlled (n = 14) studies showed significant improvement in attitudes, skills, knowledge, and behaviors. The meta-analysis of 11 RCTs showed positive changes in attitudes immediately after training and at 2–4 months post-training; in self-perceived skills at 6 months post-training; but not in factual knowledge. Studies assessing benefits for patients are still limited. Conclusions. The heterogeneity of methodological designs, interventions, and trained populations combined with a limited number of RCTs and studies on patients’ outcomes limit the strength of the evidence. However, preliminary findings suggest that simulation is promising for practical training in suicidal crisis intervention and should be further studied.
Introduction
Background
More than 700 000 people die from suicide worldwide each year, and ten to twenty times more people attempt suicide [Citation1]. Suicide prevention relies on various levels of collective and individual interventions [Citation2] targeting at risk individuals (e.g., training healthcare professionals in the treatment of depression and suicidal patients), including restricting access to suicide means, and school-based programs, among others [Citation3]. Another axis of prevention relies on gatekeepers, i.e., individuals who are not healthcare professionals but may interact with those at risk of suicide and help them seek treatment [Citation4]. Recent studies report a significant decrease in suicide attempts in populations where gatekeepers were trained [Citation5]. Meta-analyses have confirmed the overall effectiveness of preventative interventions on both completed and attempted suicide and a positive effect of combined interventions [Citation6].
Suicide prevention is impeded by false and sometimes detrimental ideas even among healthcare professionals; for example, that suicide cannot be prevented or that asking about suicide may plant suicidal ideas in the patient’s mind [Citation7]. Negative attitudes and stigma toward suicidal patients are high even among healthcare professionals [Citation8]. Yet, it has been shown that a high number of people had met a physician prior to their death by suicide, up to 10% on the day of their death and 60% in the previous month [Citation9]. These numbers highlight dramatically unmet needs as well as a critical opportunity for intervention in suicide prevention.
Fortunately, studies suggest that adequate training may address these needs. In a study including 196 healthcare professionals, 60% reported a lack of intervention skills and the need for specialized training in suicide [Citation10]. Without adequate training, clinicians are fearful to ask about suicidal ideation [Citation11] and mental healthcare providers are more avoidant, uncomfortable, and anxious facing a suicidal patient [Citation12]. Reluctance to ask about suicide and perceived lack of skills among general practitioners were associated with lower frequency of suicide risk [Citation7]. Conversely, previous training on suicide risk assessment was associated with more screening for suicidal ideations among depressed patients [Citation7], improved knowledge, attitudes and confidence to deal with suicide, and reduced stigma and taboo among healthcare professionals [Citation13,Citation14]. Furthermore, several studies have shown a significant decrease in suicide rates when healthcare professionals received training on suicide prevention and depression [Citation15–17].
An important question is how to best train both health professionals and gatekeepers for suicide risk assessment and intervention. Indeed, interviewing someone in a suicidal crisis is not easy [Citation18]. The suicidal person may feel ashamed of their suicidal ideas, may fear the consequences of disclosing such ideas (hospitalization, stigma, children custody, etc.), or may feel professionals are not competent enough to help them. In these circumstances, information focusing on factual knowledge about suicidal behaviors (e.g., epidemiology and risk factors) as done in many training programs (whether initial or continuing) may be important but very insufficient. To enhance skills and confidence to carry out suicidal risk assessments and implement crisis interventions, it is crucial to provide more practical training alongside. However, only a few studies have assessed the effectiveness of suicide training according to the educational format and differences have been shown between, for example, lecture and simulation-based-education in terms of effective learning [Citation19].
First developed in the sixties, simulation-based-education is defined as a set of ‘techniques that creates a situation or environment to allow persons to experience a representation of a real event for the purpose of practice, learning, evaluation, testing, or to gain understanding of systems or human actions’ [Citation20]. In the case of health assessment, the experiential learning component provides the opportunity to interact with simulated patient, to reflect emotionally and practically, before embedding learning through facilitator-led peer discussions in debriefing. The debriefing session is about creating a caring and trusting environment to think about learning objectives and identify areas of improvement [Citation21]. The benefits of medical simulation-based-education are widely recognized in terms of reducing medical errors, improving medical practices and patient safety, as well as learner satisfaction and engagement [Citation22–25].
In mental health, several techniques have been developed to recreate clinical environments () demonstrating the considerable potential for developing simulation practice further. The development of simulation-based-education in mental health was late compared to other specialties due to several controversies while calls have been made to further integrate this modality into mental health education [Citation26]. Authenticity of psychiatric simulations have been questioned, alongside the ability of simulated patients to correctly portray the complexity of mental disorders, or the nature of empathy toward a ‘false’ patient compared to the singular experience of each person with a mental disorder [Citation27–29]. Moreover, some studies have reported induction of psychological symptoms for simulated patients without previous training, while involvement of real patients can be more complex and hazardous than in other specialties. However, an increasing number of experimentations over the past decade and recent meta-analysis have supported the use of simulation-based-education in mental health for medical doctors [Citation30] and nurses [Citation29] in a wide range of psychiatric disorders.
Table 1. Definitions.
To our knowledge, no systematic review or meta-analysis has been conducted on simulation-based-education relating to suicide risk assessment and crisis intervention training. Here, we reviewed studies conducted with both healthcare professionals and gatekeepers, considering their different but complementary roles and training background in suicide prevention.
Aims
This study aims to assess the effectiveness, in terms of the main Kirkpatrick criteria [Citation32], of simulation training in suicide risk assessment and crisis intervention for healthcare professionals and gatekeepers.
Design
This systematic review and meta-analysis adheres to the principles of the PRISMA (Preferred Reporting Items for Systematic review and Meta-Analysis) statement [Citation33]. The protocol is registered under PROSPERO: CRD42020196136 (Supplemental Digital Appendix 1).
Methods
Search strategy
We searched PubMed and PsycINFO databases for all relevant English and French language studies published from inception to July 31st, 2021. A librarian specialized in mental health at Sainte-Anne hospital library developed the search algorithm (Supplemental Digital Appendix 2).
Eligibility criteria and selection process
We included all single group and single intervention pre-post-test (PPT) studies, non-randomized controlled trials (non-RCTs), and randomized controlled trials (RCTs) which used and assessed simulation training (Supplemental Digital Appendix 3).
The primary outcomes were based on the main Kirkpatrick criteria [Citation32], namely changes in attitudes and knowledge, skills (levels 2a and 2b, that is, what trainees learned), behaviors (level 3, that is, what trainees do differently in their clinical practice) and patient outcomes (level 4, that is, what impact the program has had on public health e.g., reduction of attempted suicides) [Citation34]. We removed the first level of Kirkpatrick criteria (‘reaction of learners’, that is, satisfaction of learners) because almost all studies used post-test only assessment.
Two authors (OR and FJ) independently screened abstracts and retrieved full-text articles that met inclusion criteria using Covidence (Covidence, Melbourne, VIC, Australia). We resolved disagreements by reaching consensus with a third reviewer (M-AP). The corresponding authors were contacted by email if some doubts remained about eligibility or if full texts were not available.
Quality appraisal
All studies had methodological quality assessed using the Medical Education Research Study Quality Instrument (MERSQI) [Citation35]. For RCTs, we used the Risk of Bias tool 2.0 (RoB 2.0; Cochrane) [Citation36]. We also reviewed key features related to effective learning in simulation training (feedback, multiple-learning strategies, controlled environment) [Citation37,Citation38].
Data extraction
Two authors (OR, MAP) then conducted a standardized data extraction on a Microsoft® Excel form (Microsoft Corp., Redmond, WA, USA).
Data analysis
We used RevMan Version 5.4.1 (Cochrane, London, UK) for meta-analysis.
To limit biases, we performed meta-analyses only for RCTs [Citation39], while a narrative analysis was done for PPT and non-RCTs studies on the basis of their individual statistical significance. For each outcome, we compared separately simulation to active (another type of training such as a lecture course) or inactive (no further training, e.g., trainers who have no lectures, no problem-based learning or any other kind of mental health training) comparators at three time-points (Supplemental Digital Appendix 4).
Statistical significance was set a priori at p < 0.05. Clinical significance was based on Cohen’s effect size classification (>0.8: large effect size, 0.5–0.8: medium effect size, <0.5: small effect size) [Citation40].
We assessed the quality of evidence with the Grading of Recommendations Assessment, Development and Evaluation system (GRADE) [Citation41] (Supplemental Digital Appendix 12).
Results
Search results
The search strategy identified 5,094 articles (). Of these, 429 were selected for full-text review. Among them, 96 studies fulfilled the detailed eligibility criteria: 17 RCTs (n = 15,623 participants), 14 non-RCTs (n = 2,546 participants), 65 PPT (n = 25,487) representing a total of 43,656 participants ().
Table 2. Summary of all studies selected.
We included available quantitative data of 11 RCTs for meta-analysis.
Study characteristics
Characteristics of each study are summarized in and detailed in Supplemental Digital Appendices 5, 6, 7. An overview of the scales used to assess each outcome is provided in Supplemental Digital Appendix 8.
Most studies were conducted in the USA (n = 47, 49.0%), and United Kingdom (n = 10, 10.4%). The origin by country of the different studies is reported in the Supplemental Digital Appendix 9. The main type of simulation was roleplay (n = 77 studies). Study quality evaluated by MERSQI scores reached an average of 12.13 out of 18.
Medical Education Research Study Quality (MERSQI) scores are reported on Supplemental Digital Appendix 11.
Risk of bias summary (ROB 2.0) for RCTs is reported on Supplemental Digital Appendix 10. GRADE system found that the quality of evidence is very low due to a high risk of bias in most of studies (Supplemental Digital Appendix 12).
Findings by Kirkpatrick’s criteria
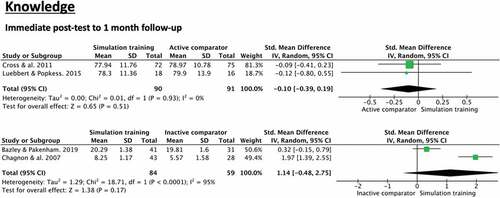
Knowledge
Seven RCTs (n = 1,646) assessed knowledge. Forest-plots of meta-analyses analysis are reported in . The number of studies included in RCTs did not allow the subgroup analysis according to the populations studied (gatekeepers or healthcare professionals). At immediate post-test to one-month follow-up, no significant difference was found when simulation was compared to an active comparator (two studies [Citation42,Citation43] SMD =-0.10, 95% CI −0.39-0.19) or to an inactive comparator (two studies [Citation44,Citation45]; SMD = 1.14, 95% CI −0.48-2.75).
Four non-RCTs assessed knowledge (n = 846). All showed significant improvement in knowledge compared to control condition. Three of them used declarative knowledge questionnaires [Citation46–48] and one assessed perceived knowledge of facts and information about suicide using self-report [Citation49].
Thirty-si PPT studies assessed knowledge (n = 1,275). Twenty-eight studies showed significant improvement of knowledge outcomes from pre- to post-test. Among these studies, one did not report a comparison test for knowledge [Citation50]. Eleven studies evaluated knowledge with a longer follow-up, from 4 weeks to 1 year, but mostly at 3 months. All but two showed significant improvement of knowledge from pre-test to follow up.
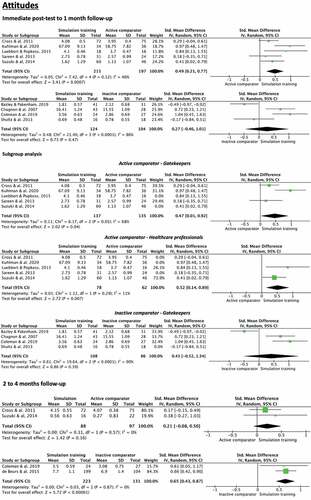
Attitudes
Attitudes comprise ways of approaching patients with suicidal ideas, beliefs, self-efficacy, confidence, and sense of preparedness.
Twelve RCTs (n = 2,000 participants) assessed attitudes. Forest-plots of meta-analyses and subgroups analysis are reported in . At immediate post-test to one-month follow-up, a significant large effect size was found comparing simulation training to an active comparator (five studies [Citation42,Citation43,Citation51–53:] Standardized Mean Difference (SMD) = 0.49, 95% confidence interval (CI) 0.21–0.77) with moderate heterogeneity (I [Citation2] = 46%). No significant difference was found when comparing simulation training to an inactive comparator (four studies [Citation44,Citation45,Citation54,Citation55] SMD = 0.27, 95% CI −0.46-1.01). At 2 to 4-month follow-up, no significant difference was found when comparing simulation training to an active comparator (two studies [Citation42,Citation53] SMD = 0.21, 95% CI −0.08-0.50). However, a significant large effect size was found when comparing simulation training to an inactive comparator (two studies [Citation55,Citation56] SMD = 0.65, 95% CI 0.43–0.87) with low heterogeneity (I [Citation2] = 0%).
Subgroup analysis performed according to the populations trained (gatekeepers or health professionals) at immediate post-test to one-month follow-up showed the same results. Including only studies with gatekeepers, a significant large effect size was found comparing simulation training to an active comparator (three studies [Citation42,Citation51,Citation52] Standardized Mean Difference (SMD) = 0.47, 95% confidence interval (CI) 0.01–0.92) with moderate heterogeneity (I [Citation2] = 68%). Including only studies with healthcare professionals, a significantly large effect size was found comparing simulation training to an active comparator (two studies [Citation43,Citation53] Standardized Mean Difference (SMD) = 0.52, 95% confidence interval (CI) 0.14–0.89) with low heterogeneity (I [Citation2] = 11%). Including only studies with gatekeepers, no significant difference was found when comparing simulation training to an inactive comparator (three studies [Citation44,Citation45,Citation55] SMD = 0.41, 95% CI −0.52-1.34).
Thirteen non-RCT assessed attitudes (n = 2,192). Ten studies showed significant improvement in attitude compared to control condition. Four out of seven [Citation13,Citation46,Citation47,Citation49,Citation57–59] non-RCT evaluating attitudes toward patients with suicidal ideas showed significant improvement, maintained at 3 months for one study [Citation46]. Three out of four [Citation13,Citation48,Citation59,Citation60] non-RCT which evaluated self-confidence showed significant improvement, maintained at 2 months in one study [Citation59] and 5 to 10 months in the other study [Citation48]. Six out of six studies [Citation49,Citation57,Citation61–64] which evaluated self-efficacy showed significant improvement: four studies showed a significant increase compared to an inactive comparator and two studies compared to an active comparator (brief presentations [Citation61] and other didactic learning [Citation62]). Most were gatekeeper trainings, and two were healthcare professional trainings [Citation57,Citation63].
Forty-eight PPT studies assessed attitudes (n = 14,051). Forty-two of them showed significant improvement of attitude outcomes from pre- to post-test. Among them, 19 studies proved still significant improvement after a follow-up of 1 month to 1 year.
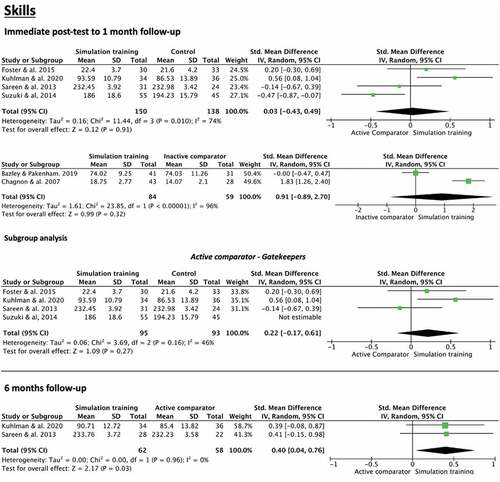
Skills
Eight RCTs (n = 1,097) assessed skills. Forest-plots of meta-analyses and subgroups analysis are reported in . At immediate post-test to one-month follow-up, no significant difference was found when compared to either an active comparator (four studies [Citation51–53,Citation65] SMD = 0.03, 95% CI −0.43-0.49) or an inactive comparator (two studies [Citation44,Citation45] SMD = 0.91, 95% CI −0.89-2.70). Subgroup analysis performed according to the populations trained (gatekeepers only) at immediate post-test to one-month follow-up showed the same results: no significant difference was found when compared to an active comparator (three studies [Citation51,Citation52,Citation65] SMD = 0.22, 95% CI −0.17-0.61). At six-month follow-up, a significant large effect size was found when comparing simulation training to an active comparator (two studies [Citation51,Citation52] SMD = 0.40, 95% CI 0.04–0.76) with low heterogeneity (I [Citation2] = 0%). The first study evaluated the intent to intervene [Citation51] and the second one [Citation52] assessed skills on the Suicide Intervention Response Inventory version 2 (SIRI-2) [Citation66].
Six non-RCT studies assessed skills (n = 625). Four [Citation59–61,Citation64] studies showed significant improvement in skills compared to control condition while two studies [Citation46,Citation63] showed no differences between the two conditions. Four studies [Citation46,Citation59,Citation60,Citation64] used the SIRI-2 to evaluate skills, one used three items that assessed the likelihood that participants will use the suicide-specific skills taught in the training [Citation61], and one evaluated five self-rated specific communication skill items [Citation54].
Thirteen PPT studies assessed skills (n = 10,596). Eleven studies showed significant improvement in skills from pre- to post-test. Five studies [Citation4,Citation67–70] evaluated skills at 1-month follow-up, 3-months follow-up and 6-months follow-up, and showed significant improvement in skills from pre-test to follow-up.
Behaviors
Six RCTs (n = 2,447) assessed changes in behaviors but the variety of measures did not allow meta-analyses. Three studies found significant improvement of behaviors for simulation training compared to control condition [Citation44,Citation55,Citation71]. Coleman et al. (2019) showed that college students were more likely to refer peers for help 2 months after training using virtual reality compared to no further training (Intervention: mean = 0.88 (Standard Deviation = 1.4); Inactive comparator: 0.30 (0.54), p < 0.05). Gould et al. (2013) showed that hotline counselors were more likely to increase calls duration (27.1 (18.7) vs. 24.4 (17.1), p < 0.01) and identify signs of suicide risk (8.4 (3.9) vs. 7.2 (3.5), p < 0.0001) at six to 18 months after a training using role-plays compared to no further training. However, this study found no significant increase in asking about suicide plans. Bazley & Pakenham (2019) showed significant increases in preventative behaviors at one-month for the intervention condition (17.66 (3.21)) compared to an inactive comparator (16.39 (2.28), p = 0.00)).
Six non-RCT studies assessed behaviors (n = 1,585). Four studies [Citation17,Citation48,Citation58,Citation62] showed significant improvement in behaviors compared to control condition while the other two [Citation49,Citation59] showed no significant differences between the two conditions. Chauliac et al. (2016) compared role-plays to no further training for 106 caregivers in 310 nursing homes for 1 year [Citation58]. They found a significant improvement in management of suicidal crises compared to inactive comparator, with more psychological therapies and interventions (28 (77.8) vs. 15 (45.5), p < 0.006), and more contracts made with patients (4 (11.1) vs. 0 (0), p < 0.05). They also found a significant improvement for almost all measures of a recommendation list that could influence suicide prevention (suicide risk factors, assessment tools, restricted access to means). However, they found no difference for attitudes and detection of suicidal crises. Coleman and Del Quest (2015) highlighted a significantly increased frequency of asking about suicide at six-months follow-up (3.8 (0.7) vs. 2.6 (1.1), p < 0.01) but no difference on number of youths referred (4.6 (0.7) vs. 3.8 (1.2), p = 0.13) [Citation62]. Fallucco et al. (2012) showed a significant improvement in using a depression screening tool (50% vs. 19%; p = 0.001) and having diagnosed at least one adolescent with depression in the past 3 months (96% vs. 78%; p = 0.013) [Citation48]. Roskar et al. (2010) found a significant increase in antidepressants prescription rates (mean difference = 1.05, bias-corrected and accelerated 95% CI = 0.47, 1.80, bias = 0.01, Standard error = 0.36) [Citation17].
Eight PPT studies assessed behaviors (n = 11,155). Three studies showed significant improvement of behaviors [Citation70,Citation72,Citation73] from pre-test to follow-up, while four studies showed no significant differences from pre-test to follow-up [Citation31,Citation74–76] and one did not provide comparative results before and after training [Citation77].
Among studies that found positive behavior improvements, Rallis et al. (2018) studied youth services staff’ behaviors at 3 months from a training using role-plays. They collected the number of suicidal students identified and the number of suicidal students referred for help reported by participants at baseline and three-month follow-up. They found a significant increase in the number of students referred (Pre-test: 0.14 (0.42); three-months: 0.31 (0.60) p < 0.002) but not in those identified (Pre-test: 0.23 (0.60); three-months: 0.33 (0.61) p < 0.110).
Ewell Foster et al. (2017) evaluated behavioral change in participants following a training using role-plays. At 6 to 9 months post-training, they found a significant increase in the identification of at-risk youths (Pre-test: 1.04 (1.07); follow-up: 1.43 (1.51) p = 0.000), in frequency of asking about suicide (Pre-test: 3.11 (1.40); follow-up: M 3.56 (1.32) p = 0.000), and in helping behaviors (Pre-test: 3.76 (1.35); follow-up: 3.78 (1.53) p = 0.02). However, they found no significant difference in frequency of referring youth (Pre-test: 1.00 (1.29); follow-up: 1.76 (1.97), ns).
Patient outcomes
Three RCTs (n = 13,401) assessed patient outcomes, two found significant results [Citation71,Citation78], while one did not show significant differences between the two conditions [Citation1,Citation79]°-. Wasserman et al. (2015) compared the incidences of suicide attempts and severe suicidal ideation among students after school staff were trained either with role-plays or with posters [Citation78]. There was no difference at three-months post-training, but a significant decrease with simulation at 12-months post-training of the incidence of suicide attempts (Odd Ratio (OR) = 0.45, 95% CI 0.24–0.85, p < 0.014) and of severe suicidal ideation (OR 0.50, 95% CI 0.27–0.92, p < 0.025). Gould et al. (2013) evaluated the effects of a suicide hotline counselors’ training using role-plays, on callers’ behavioral changes at 6-, 12- and 18-months post-training [Citation71]. They found that callers felt significantly less depressed, less overwhelmed, less suicidal, and more hopeful during the call compared to inactive comparator. Three months after a training including role-plays, De Beurs et al. (2016) did not find an improvement in the frequency of self-reported suicide attempts and satisfaction of patients about treatment and relationship with therapist [Citation79].
One non-RCT [Citation17] assessed patient outcomes (n = 354). It evaluated the number of suicides in regions where general practitioners followed or not a course including role-plays. No significant differences between groups were found.
Two PPT studies assessed patient outcomes (n = 587). The first one [Citation80] only reported descriptive percentages without comparison test. However, results suggest an increase in the detection of suicidal ideation from 14% to 21% in patients presenting to the emergency department studied within 4 years of the implementation of the training. Medical staff reported feeling more comfortable questioning suicidal ideation and looking for protective and risk factors. The second one [Citation81] found no significant difference from pre- to post-test on annual suicide rates after having trained healthcare professionals with role-plays.
Discussion
This study systematically reviewed the literature on the use of simulation-based-education for suicide risk assessment and intervention training in order to assess its effectiveness in healthcare professionals or gatekeepers involved in suicide prevention. Results from RCTs, non-RCTs and PPT studies suggest potential benefits in the use of simulation, notably in terms of short-term changes in attitudes (immediate to four-month post-training), and to some extent in improving skills, knowledge, and behaviors. However, only six studies assess changes in patients’ outcomes following simulation training to date and just two of them found a significant improvement in these criteria. It seems too few to draw any strong conclusion, whereas this criterion is precisely the one for which simulation-based education is provided, i.e., a concrete improvement in terms of public health. For example, these studies looked at the number of patients who had suicidal ideation, who had attempted suicide or the rate of completed suicides.
Change in attitudes is critical to improve the quality of relationship, prevent negative countertransference, and subsequently enhance the quality of suicide risk assessment and intervention. Consistent with previous meta-analyses on mental health simulation [Citation29,Citation30], a large effect on attitudes was found immediately at the end of training for simulation as compared to an active comparator, and at two- to four-months post-training as compared to an inactive comparator. The lack of significant difference at immediate post-test in the comparison with an inactive comparator may be related to the weakness of the simulation design in two out of four studies, which used role-plays with no details reported about dedicated time for roleplays among many other learning strategies [Citation44,Citation45]. Conversely, the strength of active comparators in studies assessing attitudes at two- to four-months follow-up may explain the absence of statistical significance: one study used a one-hour lecture with video, booklets and question-and-answer discussion period based on Question-Persuade-Refer training [Citation42] and the other used a lecture [Citation53]. In addition to RCTs, 10 out of 13 non-RCTs (including attitude toward suicidal patients, self-confidence, and self-efficacy) and 42 out of 48 PPT studies reporting statistical significance on attitudes provide further support on the effectiveness of simulation-based education, even if we cannot exclude natural learning effect for PPTs. One clear limitation of attitude measures in the reported studies is the reliance on subjective assessment.
Beyond possible lack of temporal distance for reporting effects on skills at immediate post-test, time devoted to role-play among the relevant studies was either less important, or not specified among several other educational approaches as seen in Suzuki et al. (2014) where role-play is included among lecture, video-modeling, and discussions, with time devoted unspecified. Improvement of skills found at six-months post-training compared to an active comparator but not at immediate post-training may be explained by the delayed effects of training on skills, notably regular personal reinforcement from practicing the skills learned during the training, engaging with Kolb’s Experiential Learning Cycle introduced through simulation. However, of the two studies included in the meta-analysis at 6-month follow-up, one study showed significant improvement of skills at immediate post-training [Citation82]. In this study, role-plays took a large part of the training with each participant taking part into role-plays and general feedback. In addition to RCTs, four positive studies out of five non-RCTs and eleven positive PPT studies tend to support an effect of simulation-based-education on skills. Studies investigating longer follow-ups and using an external assessment of skills are needed.
No significant difference was found in meta-analyses for a change in knowledge following simulation. Beyond the few numbers of studies, another explanation is that simulation-based-education, through experience and reflection, targets more the acquisition of behaviors, skills, and attitudes than theoretical knowledge. This is consistent with a previous review on simulation in psychiatry for nurses [Citation29]. However, 4 non-RCT and 28 out of 36 PPT studies do report significant results. As a matter of fact, many training programs include teaching basic factual knowledge.
Most studies focused on attitudes, skills, and knowledge. Assessment of changes in the learner’s objective behaviors, and of increased patient outcomes are much more limited, possibly due to methodological complexities. Three RCTs showed objective behavioral changes including an improved management of suicidal crises, an increased frequency of asking about suicidal ideas, an increased number of diagnosed depressions and increased rates of antidepressant prescription. Moreover, four out of six non-RCTs also showed positive results, which is promising.
Regarding patient outcomes, two RCTs showed significant positive effects following the training of school staff and of suicide hotline counselors. While these studies are more complex to manage, they are necessary. Simulation training can be a complex training modality to implement, requiring writing authentic scenarios, training facilitators and actors. When working with actors, additional costs, and ethical considerations present. Virtual reality necessitates programming and equipment and software to implement. Clear and robust benefits of simulation over other ‘simpler’ training modalities (such as lectures or videos) are required and while some are evident, those relating to behaviors and patient outcomes are less clear.
Strength and limitations
This is the first systematic review and meta-analysis on simulation training in suicide prevention, providing encouraging results alongside certain limitations. First, despite careful research, some studies may have been missed. Second, only RCTs were included in meta-analyses in order to raise the level of confidence, while results from non-RCTS and PPTs were less detailed. However, only 17 RCTs were found. Six RCTs could not be included in meta-analysis because of different data collection time points, comparators, outcomes measured and missing data. We kept only post-test results to homogeneous measures. Third, because of the limited number of studies, sensitivity analysis, funnel plots, and Egger tests could not be performed given the lack of statistical power [Citation83] which undermined the strength of our conclusions. However, we were able to perform some subgroup analysis when possible, distinguishing trainings targeted for gatekeepers from that for healthcare professionals, thus reaching the same conclusions suggested by the meta-analyses. In the future, variables such as professional activities (general practitioner, psychiatrist, nurse, psychologist), the stage of education (initial versus continuing) or the type of simulation should be analyzed. Fourth, GRADE system found the quality of evidence is very low due to a high risk of bias in most of studies.
Heterogeneity was high across studies. Participants came from very different social and professional backgrounds, and simulation pedagogies and methods varied greatly across studies. In addition, simulation techniques were frequently a small part of the overall training offered, as educators’ attempts to strengthen training programs through the use of simulation. However, this made it challenging to measure the specific effect of simulation compared to other learning strategies, and their interaction. Finally, few studies evaluated the impact in terms of public health (number of suicides and suicidal ideations for example).
Implications
Regarding methodological implications, more research, with an adequate methodological design, is needed to robustly evaluate the benefits of simulation-based education for suicide prevention training, including RCTs, long-term follow-up, and measures of the highest levels of the Kirkpatrick’s criteria, namely change in participants’ behaviors and changes in patient outcomes. Given the few studies that have investigated the direct implications for patients, it would seem particularly interesting, for example, to study the number of suicide attempts and completed suicides in regions where general practitioners or psychiatrists have been trained with simulation-based education compared to a region where general practitioners or psychiatrists have been trained with more conventional training (e.g., lectures). Guidance and recommendations on study design to investigate the effectiveness of simulation training would be helpful.
Regarding educational implication, our encouraging results suggest the benefit to implement simulation-based education for all health students as is done for somatic first aids. Moreover, targeting people most likely to be close with person with suicidal idea may be an efficient public health approach.
As suicide prevention rests on the combined efforts of many types of contributors, we included here all types of participants without any limit of professional category. However, the complexity of training should be adapted to the educational level of trainees – a basic requirement in education – and the assessment of effectiveness needs to be adjusted accordingly. For example, as role-plays are more effective with unexperienced people, are well-trained standardized patients required with an advanced mental health professional? Some studies [Citation30,Citation84] suggested that even with experienced professionals, role-plays positively influence attitudes towards suicide. Simulation training may be complementary to other classical training techniques such as lectures, as theoretical knowledge remains necessary (including epidemiology or risk factors). Simulation allows the acquisition of ‘know-how’, experience, and practical skills, which is essential in mental health, notably for crisis situations where training with real patients might not be appropriate.
Conclusion
The present study suggests that simulation-based training may be effective to change attitudes and skills for suicide risk assessment and crisis intervention, with promising preliminary results regarding changes in behaviors and patients’ outcomes. However, numerous limitations must be acknowledged, and many challenges remain. More research of higher methodological quality must be developed.
Supplemental Material
Download MS Word (56.7 MB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10872981.2023.2199469.
Additional information
Funding
References
- World Health Organization. Suicide worldwide in 2019: global health estimates. World Health Organization; 2021. Available from 2021 Sep15; https://apps.who.int/iris/handle/10665/341728
- Hawton K, Pirkis J. Suicide is a complex problem that requires a range of prevention initiatives and methods of evaluation. Br J Psychiatry. 2017;210(6):381–14.
- Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016;3(7):646–659.
- Hawgood J, Woodward A, Quinnett P, et al. Gatekeeper training and minimum standards of competency: essentials for the suicide prevention workforce. Crisis. Published online. 2021 June 30;0227–5910/a000794. DOI:10.1027/0227-5910/a000794.
- Pistone I, Beckman U, Eriksson E, et al. The effects of educational interventions on suicide: a systematic review and meta-analysis. Int J Soc Psychiatry. 2019;65(5):399–412.
- Hofstra E, van Nieuwenhuizen C, Bakker M, et al. Effectiveness of suicide prevention interventions: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2020;63:127–140.
- Bocquier A, Pambrun E, Dumesnil H, et al. Physicians’ characteristics associated with exploring suicide risk among patients with depression: a French panel survey of general practitioner Xia Y, ed. PLoS ONE. 2013;8(12):e80797.
- Saunders KEA, Hawton K, Fortune S, et al. Attitudes and knowledge of clinical staff regarding people who self-harm: a systematic review. J Affect Disord. 2012;139(3):205–216.
- Laanani M, Imbaud C, Tuppin P, et al. Contacts with health services during the year prior to suicide death and prevalent conditions a nationwide study. J Affect Disord. 2020;274:174–182.
- Rothes IA, Henriques MR, Leal JB, et al. Facing a patient who seeks help after a suicide attempt: the difficulties of health professionals. Crisis. 2014;35(2):110–122.
- Quinnett P. The role of clinician fear in interviewing suicidal patients. Crisis. 2019;40(5):355–359.
- Mitchell SM, Taylor NJ, Jahn DR, et al. Suicide-related training, self-efficacy, and mental health care providers’ reactions toward suicidal individuals. Crisis. 2020;41(5):359–366.
- Boukouvalas E, El-Den S, Murphy AL, et al. Exploring health care professionals’ knowledge of, attitudes towards, and confidence in caring for people at risk of suicide: a systematic review. Arch Suicide Res. Published online 2019. 2020;24(sup2):S1–31. DOI:10.1080/13811118.2019.1586608.
- Ramberg IL, Wasserman D. Benefits of implementing an academic training of trainers program to promote knowledge and clarity in work with psychiatric suicidal patients. Arch Suicide Res. 2004;8(4):331–343.
- Rutz W, von Knorring L, Wålinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80(2):151–154.
- Hegerl U, Althaus D, Schmidtke A, et al. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychol Med. 2006;36(9):1225–1233.
- Roskar S, Podlesek A, Zorko M, et al. Effects of training program on recognition and management of depression and suicide risk evaluation for Slovenian primary-care physicians: follow-up study. Croat Med J. 2010;51(3):237–242.
- Shea SC, Barney C. Teaching clinical interviewing skills using role-playing: conveying empathy to performing a suicide assessment: a primer for individual role-playing and scripted group role-playing. Psychiatr Clin North Am. 2015;38(1):147–183.
- Han A, Kim TH, Hong H. A factorial randomized controlled trial to examine separate and combined effects of a simulation-based empathy enhancement program and a lecture-based education program on family caregivers of people with dementia. Aging Mental Health. Published online. 2020 May 19;1–11. DOI:10.1080/13607863.2020.1768214.
- Lopreiato JO. Healthcare simulation dictionary. MD: Agency for Healthcare Research and Quality; 2016.
- Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc J Soc Simul Healthc. 2007;2(2):115–125.
- Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9).
- Gordon CJ, Ryall T, Judd B. Simulation-based assessments in health professional education: a systematic review. J Multidiscip Healthc. 2016 February:69. Published online. Doi:10.2147/JMDH.S92695.
- Sarfati L, Ranchon F, Vantard N, et al. Human-simulation-based learning to prevent medication error: a systematic review. J Eval Clin Pract. 2019;25(1):11–20.
- Zendejas B, Brydges R, Wang AT, et al. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28(8):1078–1089.
- Attoe C, Kowalski C, Fernando A, et al. Integrating mental health simulation into routine health-care education. Lancet Psychiatry. 2016;3(8):702–703.
- Brenner AM. Uses and limitations of simulated patients in psychiatric education. Acad Psychiatry. 2009;33(2):112–119.
- McNaughton N, Ravitz P, Wadell A, et al. Psychiatric education and simulation: a review of the literature. Can J Psychiatry. 2008;53(2):85–93.
- Piot MA, Attoe C, Billon G, et al. Simulation training in psychiatry for medical education: a review. Front Psychiatry. 2021;12:658967.
- Piot M, Dechartres A, Attoe C, et al. Simulation in psychiatry for medical doctors: a systematic review and meta‐analysis. Med Educ. 2020;54(8):696–708.
- Terpstra S, Beekman A, Abbing J, et al. Suicide prevention gatekeeper training in the Netherlands improves gatekeepers’ knowledge of suicide prevention and their confidence to discuss suicidality, an observational study. BMC Public Health. 2018;18(1):637.
- Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs. San Franscisco: TATA McGraw-Hill; 2006.
- Moher D, Liberati A, Tetzlaff J, et al. The PRISMA group. preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7):e1000097.
- World Health Organization. Evaluating Training in WHO.; 2010. Available from 2021 Sep 20;. https://apps.who.int/iris/bitstream/handle/10665/70552/WHO_HSE_GIP_ITP_2011.2_eng.pdf
- Reed DA, Cook DA, Beckman TJ, et al. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002.
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. Published online. 2019 August 28;l4898. DOI:10.1136/bmj.l4898
- Cook DA, Hamstra SJ, Brydges R, et al. Comparative effectiveness of instructional design features in simulation-based education: systematic review and meta-analysis. Med Teach. 2013;35(1):e867–898.
- Barry Issenberg S, Mcgaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28.
- Cochrane Handbook for Systematic Reviews of Interventions. Available from Sep 16; https://training.cochrane.org/handbook/current
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed ed. New York: Lawrence Erlbaum Associates, Inc; 1988.
- Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. DOI:10.1136/bmj.39489.470347.AD
- Cross WF, Seaburn D, Gibbs D, et al. Does practice make perfect? a randomized control trial of behavioral rehearsal on suicide prevention gatekeeper skills. J Prim Prev. 2011;32(3–4):195–211.
- Luebbert R, Popkess A. The influence of teaching method on performance of suicide assessment in baccalaureate nursing students. J Am Psychiatr Nurses Assoc. 2015;21(2):126–133.
- Bazley R, Pakenham K. Suicide prevention training for Christian faith-based organizations using acceptance and commitment therapy: a pilot controlled trial of the HOLLY program. J Context Behav Sci. 2019;11:6–14.
- Chagnon F, Houle J, Marcoux I, et al. Control-group study of an intervention training program for youth suicide prevention. Suicide Life Threat Behav. 2007;37(2):135–144.
- Shannonhouse LR, Elston N, Lin YWD, et al. Suicide intervention training for counselor trainees: a quasi-experimental study on skill retention. Couns Educ Superv. 2018;57(3):194–210.
- Fallucco EM, Hanson MD, Glowinski AL. Teaching pediatric residents to assess adolescent suicide risk with a standardized patient module. Pediatrics. 2010;125(5):953–959.
- Fallucco EM, Conlon MK, Gale G, et al. Use of a standardized patient paradigm to enhance proficiency in risk assessment for adolescent depression and suicide. J Adolesc Health. 2012;51(1):66–72.
- Kuhlman STW, Walch SE, Bauer KN, et al. Intention to enact and enactment of gatekeeper behaviors for suicide prevention: an application of the theory of planned behavior. Prev Sci off J Soc Prev Res. 2017;18(6):704–715.
- Robinson J, Gook S, Yuen HP, et al. Managing deliberate self-harm in young people: an evaluation of a training program developed for school welfare staff using a longitudinal research design. BMC Psychiatry. 2008;8(1):75.
- Kuhlman STW, Smith PN, Marie L, et al. A pilot randomized controlled trial of the alliance project gatekeeper training for suicide prevention. Arch Suicide Res. Published online. 2020 May 21;1–17. DOI:10.1080/13811118.2020.1767246.
- Sareen J, Isaak C, Bolton SL, et al. Gatekeeper training for suicide prevention in first nations community members: a randomized controlled trial. Depress Anxiety. 2013;30(10):1021–1029.
- Suzuki Y, Kato TA, Sato R, et al. Effectiveness of brief suicide management training programme for medical residents in Japan: a cluster randomized controlled trial. Epidemiol Psychiatr Sci. 2014;23(2):167–176.
- Shultz E. Technology and teaching: suicide risk assessment. Med Educ. 2013;47(11):1132–1133.
- Coleman D, Black N, Ng J, et al. Kognito’s avatar‐based suicide prevention training for college students: results of a randomized controlled trial and a naturalistic evaluation. Suicide Life Threat Behav. 2019;49(6):1735–1745.
- de Beurs DP, de Groot MH, de Keijser J, et al. The effect of an e-learning supported train-the-trainer programme on implementation of suicide guidelines in mental health care. J Affect Disord. 2015;175:446–453.
- Siau CS, Wee LH, Ibrahim N, et al. Gatekeeper suicide training’s effectiveness among Malaysian hospital health professionals: a control group study with a three-month follow-up. J Contin Educ Health Prof. 2018;38(4):227–234.
- Chauliac N, Brochard N, Payet C, et al. How does gatekeeper training improve suicide prevention for elderly people in nursing homes? A controlled study in 24 centres. Eur Psychiatry. 2016;37:56–62.
- Fenwick CD, Vassilas CA, Carter H, et al. Training health professionals in the recognition, assessment and management of suicide risk. Int J Psychiatry Clin Pract. 2004;8(2):117–121.
- Hashimoto N, Takeda H, Fujii Y, et al. Effectiveness of suicide prevention gatekeeper training for university teachers in Japan. Asian J Psychiatr. 2021;60:102661.
- Teo AR, Andrea SB, Sakakibara R, et al. Brief gatekeeper training for suicide prevention in an ethnic minority population: a controlled intervention. BMC Psychiatry. 2016;16(1):211.
- Coleman D, Del Quest A. Science from evaluation: testing hypotheses about differential effects of three youth-focused suicide prevention trainings. Soc Work Public Health. 2015;30(2):117–128.
- Fiedorowicz JG, Franklin EM, Rosenbaum M. A medical interviewing curriculum intervention for medical students’ assessment of suicide risk. Acad Psychiatry. Published online. 2013;4(6):398. DOI:10.1176/appi.ap.11110200.
- Pasco S, Wallack C, Sartin RM, et al. The impact of experiential exercises on communication and relational skills in a suicide prevention gatekeeper-training program for college resident advisors. J Am Coll Health J ACH. 2012;60(2):134–140.
- Foster A, Chaudhary N, Murphy J, et al. The use of simulation to teach suicide risk assessment to health profession trainees-rationale, methodology, and a proof of concept demonstration with a virtual patient. Acad Psychiatry J Am Assoc Dir Psychiatr Resid Train Assoc Acad Psychiatry. 2015;39(6):620–629.
- Bonnelle RANK. THE suicide intervention response inventory: a revision and validation. Death Stud. 1997;21(1):59–81.
- Hashimoto N, Suzuki Y, Kato TA, et al. Effectiveness of suicide prevention gatekeeper-training for university administrative staff in Japan. Psychiatry Clin Neurosci. 2016;70(1):62–70.
- Kubo H, Urata H, Katsuki R, et al. Development of MHFA-based 2-h educational program for early intervention in depression among office workers: a single-arm pilot trial Hashimoto Ked. PLOS ONE. 2018;13(12):e0208114. DOI:10.1371/journal.pone.0208114
- Rimkevičienė J, Skruibis P, Padroštytė G. Effectiveness of applied suicide intervention skills training (ASIST) in Lithuania. Death Stud. Published online. 2020 December 30;46(8):1–7. DOI:10.1080/07481187.2020.1867254
- Smith-Millman M, Bernstein L, Link N, et al. Effectiveness of an online suicide prevention program for college faculty and students. J Am Coll Health J ACH. Published online. 2020 August 19;1–8. DOI:10.1080/07448481.2020.1804389.
- Gould MS, Cross W, Pisani AR, et al. Impact of applied suicide intervention skills training on the national suicide prevention lifeline. Suicide Life Threat Behav. 2013;43(6):676–691.
- Ewell Foster CJ, Burnside AN, Smith PK, et al. Response, and referral of suicidal youth following applied suicide intervention skills training. Suicide Life Threat Behav. 2017;47(3):297–308.
- Rallis BA, Esposito-Smythers C, Disabato DJ, et al. A brief peer gatekeeper suicide prevention training: results of an open pilot trial. J Clin Psychol. 2018;74(7):1106–1116.
- Robinson-Link N, Hoover S, Bernstein L, et al. Is gatekeeper training enough for suicide prevention? Sch Ment Health Multidiscip Res Pract J. Published online. 2019;12(2):239–249. DOI:10.1007/s12310-019-09345-x.
- Sale E, Hendricks M, Weil V, et al. Counseling on Access to lethal means (CALM): an evaluation of a suicide prevention means restriction training program for mental health providers. Community Ment Health J. 2018;54(3):293–301.
- Osteen PJ, Lacasse JR, Woods MN, et al. Training youth services staff to identify, assess, and intervene when working with youth at high risk for suicide. Child Youth Serv Rev. 2018;86:308–315.
- Oordt MS, Jobes DA, Fonseca VP, et al. Training mental health professionals to assess and manage suicidal behavior: can provider confidence and practice behaviors be altered? Suicide Life Threat Behav. 2009;39(1):21–32.
- Wasserman D, Hoven CW, Wasserman C. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. 2015;385(9977):9.
- de Beurs DP, Hooiveld M, Kerkhof AJFM, et al. Trends in suicidal behaviour in Dutch general practice, 1983-2013. Ned Tijdschr Geneeskd. 2016;160:D745.
- McAuliffe N, Perry L. Making it safer: a health centre’s strategy for suicide prevention. Psychiatr Q. 2007;78(4):295–307.
- Morriss R, Gask L, Webb R, et al. The effects on suicide rates of an educational intervention for front-line health professionals with suicidal patients (the STORM Project). Psychol Med. 2005;35(7):957–960.
- Kuhlman STW. A randomized controlled trial of the alliance project gatekeeper training for suicide prevention: effects of training on gatekeeper behaviors. ProQuest Inf & Learn. 2020. Available from: http://sirius.parisdescartes.fr/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2020-04054-023&lang=fr&site=ehost-live
- Cuijpers P, Griffin JW, Furukawa TA. The lack of statistical power of subgroup analyses in meta-analyses: a cautionary note. Epidemiol Psychiatr Sci. 2021;30:e78.
- Gryglewicz K, Monahan MF, Chen JI, et al. Examining the effects of role play practice in enhancing clinical skills to assess and manage suicide risk. J Ment Health. 2020;29(5):549–557.
- Lewis KL, Bohnert CA, Gammon WL, et al. The Association of Standardized Patient Educators (ASPE) Standards of Best Practice (SOBP). Adv Simul (Lond). 2017;2:10.
- Williams B, Reddy P, Marshall S, Beovich B, McKarney L. Simulation and mental health outcomes: a scoping review. Adv Simul. 2017;2:2. DOI:10.1186/s41077-016-0035-9
- King J, Hill K, Gleason A. All the world’s a stage: evaluating psychiatry role-playbased learning for medical students. Australas Psychiatry Bull R Aust N Z CollPsychiatr 2015;23(1):76–9.
- Hodges B, Hanson M, McNaughton N, Regehr G. Creating, monitoring, and improving a psychiatry OSCE. Acad Psychiatry. 2002;26(3):134–161.
- Pantziaras I, Fors U, Ekblad S. Training with virtual patients in transcultural psychiatry: do the learners actually learn? J Med Internet Res. 2015;17(2):e46.
- Galletly C, Burton C. Improving medical student attitudes towards people with schizophrenia. Aust N Z J Psychiatry. 2011;45(6):473–476.
- Rabheru K, Wiens A, Ramprasad B, Bourgon L, Antochi R, Hamstra SJ. Comparison of traditional didactic seminar to high-fidelity simulation for teaching electroconvulsive therapy technique to psychiatry trainees. J ECT. 2013;29(4):291–296.
- Hodges BD, Hollenberg E, McNaughton N, Hanson MD, Regehr G. The psychiatry OSCE: a 20-year retrospective. Acad Psychiatry. 2014;38:26–34. DOI:10.1007/s40596-013-0012-8