Abstract
Objective: To assess comparative benefits and harms across three airway management approaches (bag valve mask [BVM], supraglottic airway [SGA], and endotracheal intubation [ETI]) used by prehospital emergency medical services (EMS) to treat patients with trauma, cardiac arrest, or medical emergencies, and how they differ based on techniques and devices, EMS personnel and patient characteristics. Data sources: We searched electronic citation databases (Ovid® MEDLINE®, CINAHL®, the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, and Scopus®) from 1990 to September 2020. Review methods: We followed Agency for Healthcare Research and Quality Effective Health Care Program Methods guidance. Outcomes included mortality, neurological function, return of spontaneous circulation (ROSC), and successful advanced airway insertion. Meta-analyses using profile-likelihood random effects models were conducted, with analyses stratified by study design, emergency type, and age. Results: We included 99 studies involving 630,397 patients. We found few differences in primary outcomes across airway management approaches. For survival, there was no difference for BVM versus ETI or SGA in adult and pediatric patients with cardiac arrest or trauma. For neurological function, there was no difference for BVM versus ETI and SGA versus ETI in pediatric patients with cardiac arrest. There was no difference in BVM versus ETI in adults with cardiac arrest, but improved neurological function with BVM or ETI versus SGA. There was no difference in ROSC for patients with cardiac arrest for BVM versus ETI or SGA in adults and pediatrics, or SGA versus ETI in pediatrics. There was higher frequency of ROSC in adults with SGA versus ETI. For successful advanced airway insertion, there was higher first-pass success with SGA versus ETI for all patients except adult medical patients (no difference), and no difference in overall success using SGA versus ETI in adults. Conclusions: The currently available evidence does not indicate benefits of more invasive airway approaches based on survival, neurological function, ROSC, or successful airway insertion. Strength of evidence was low or moderate; most included studies were observational. This supports the need for high-quality randomized controlled trials to advance clinical practice and EMS education and policy, and improve patient-centered outcomes.
Introduction
Airway management is one of the most important aspects of prehospital emergency care, critical to both immediate survival and patients’ potential for recovery. Of the three techniques routinely used by emergency medical services (EMS)—bag valve mask (BVM), supraglottic airway devices (SGA), and endotracheal intubation (ETI)—ETI has long been considered the gold standard for airway management. Although this is true for highly controlled environments, prehospital airway management success rates for ETI vary considerably and high rates of complications have been attributed to multiple factors (Citation1–5).
The choice of technique and the potential for success depend on the severity of the patient’s condition, the training and skills of the EMS personnel, setting (e.g., distance, level of care), and available equipment. EMS care is regulated by a Scope of Practice which vary from state to state in the United States and across countries, with some more restrictive than others. Thus, training and skills, resources, and scope of practice all influence choices. A key challenge in prehospital airway management is to determine the appropriate approach for individual patients given these factors, in the context of a wide range of practice and policy settings.
Guideline developers and EMS system leaders wish to develop evidence-based recommendations based on research in an environment of expanding options for prehospital airway management. The purpose of this systematic review was to identify and synthesize evidence available to support the development of evidence-based recommendations and guidelines for prehospital airway management in the United States.
Methods
Scope of the Review
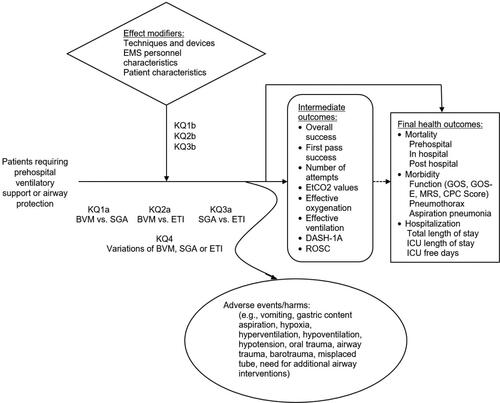
The full review addressed 4 key questions (KQs) () comparing the benefits and harms for patients with trauma, cardiac arrest, or medical emergencies requiring prehospital ventilatory support or airway protection of BVM versus SGA (KQ1), BVM versus ETI (KQ2), SGA versus ETI (KQ3), and variations of any one of the three included airway interventions (KQ4). This review also considered how the benefits and harms for the three airway interventions differed across the following factors:
Figure 1. Analytic framework. BVM = bag valve mask; CPC Score = Cerebral Performance Category Score; DASH-1A = Definitive Airway Sans Hypoxia on First Attempt; EMS = emergency medical services; ETI = endotracheal intubation; GOS = Glasgow Outcome Scale; GOS-E = Glasgow Outcome Scale Extended: Hypoxia/Hypotension on First Attempt; ICU = intensive care unit; KQ = Key Question; MRS = modified Rankin Scale; ROSC = return of spontaneous circulation; SGA = supraglottic airway.
Specific techniques including modifications and devices used for each airway management approach,
Characteristics of the EMS personnel (e.g., training, certification, and expertise), and
Patient characteristics (e.g., demographics, type and severity of illness or injury, and location/environment).
This review followed methods suggested in the Agency for Healthcare Research and Quality (AHRQ) Methods Guide for Effectiveness and Comparative Effectiveness Reviews (Citation6). This article includes results from KQs 1–3; a subsequent publication will report results from KQ4. Detailed methods are available in the full evidence report [AHRQ Airway Report; https://effectivehealthcare.ahrq.gov/products/prehospital-airway-management/research].
Data Sources and Searches
Searches were conducted by a research librarian in Ovid MEDLINE, CINAHL, the Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus from January 1990 through September 2020. These were supplemented by reference lists from relevant systematic reviews and a Federal Register notice requesting unpublished data (Appendix A).
Study Selection
Two investigators independently reviewed titles, abstracts, and full-text articles using pre-defined eligibility criteria (Appendix A). Disagreements regarding study inclusion were resolved by consensus of the investigators, or by a third investigator when required. Populations included adult and pediatric patients requiring ventilatory support or airway protection treated in the prehospital setting by EMS personnel (paramedic, emergency medical technician at any level of training, emergency medical responder, nurse, physician, etc.). Eligible airway interventions included the use of BVM, SGA, or ETI. Only studies that included comparative data were included. International studies published in English were eligible for inclusion. Randomized controlled trials (RCT), controlled clinical trials (CCT), comparative observational studies, and case-control studies in the prehospital setting were eligible for inclusion. Reviews, case reports, and case series were not included.
The primary outcomes were survival, morbidity (especially neurologic function), and length of stay, focusing on outcomes measured within 30 days of the event requiring airway management. Secondary outcomes included success rates of advanced airway placement (SGA and ETI only), effective ventilation, definitive airway without hypoxia/hypotension on first attempt (DASH-1A), return of spontaneous circulation (ROSC), arterial or venous blood gases obtained on ED arrival, and harms ().
Data Abstraction and Quality Rating
One investigator abstracted details about each study’s design, patient population, setting, interventions, analysis, follow-up, and results. A second investigator reviewed the abstracted data for accuracy. Two investigators independently assessed the quality using predefined criteria in accordance with the AHRQ Methods Guide (Citation6) specifically Cochrane Risk of Bias (ROB) for RCTs (Citation7) and U.S. Preventive Services Task Force (Citation8) for observational studies. Disagreements in quality ratings were resolved by consensus of the investigators, or by a third investigator when required. Authors of any included paper who were part of the research team did not participate in review of their own publications.
Data Synthesis
Data were synthesized separately for each KQ by outcome. We prioritized the following patient-centered outcomes for meta-analyses: survival in-hospital or at one-month post-incident; neurological function at discharge or one-month post-incident; ROSC; and, for KQ3 (SGA vs. ETI), successful advanced airway insertion. When pooling these outcomes was not appropriate, findings were summarized qualitatively. These qualitative assessments did not impact the conclusions reported here, and are described in the full report available online [ARQ Airway Report; https://effectivehealthcare.ahrq.gov/products/prehospital-airway-management/research].
Findings regarding harms from qualitative synthesis are summarized for each KQ in this article.
Definitions
A number of included studies reported on samples with mixed emergency types and mixed ages. In consultation with topic experts, the following assumptions were adopted. Studies in which >85% of the participants included cardiac arrest patients were categorized as such at the study level. Studies or subgroups were categorized as pediatric based on each study’s age-based definition. Studies in which <10% of included patients were pediatric were categorized as adult at the study level. Studies for which age distribution was not explicitly defined were categorized as “mixed-age” at the study level. For meta-analysis, included studies were categorized as either RCTs or observational, based on the characteristics of the individual studies.
There was considerable variation in how provider training and experience were reported in the included studies. For this project, we categorized providers as “ETI-capable, ETI-not capable, and mixed” (a team including both ETI capabilities). ETI-capable providers were classified as those who could perform endotracheal intubaton in the prehospital environment. For EMS providers in the U.S., this included paramedic and more advanced providers (e.g., “critical care paramedic” (no universal definition for this), flight nurse, nurse practitioner/physician assistant, or physician). For EMS providers outside the U.S., this was classified based on the information in the study. If the information was not provided, it was taken from other articles from the reference country or the governmental/agency website listing the provider skill set.
Meta-analyses
Meta-analyses were stratified first by study design (RCTs or observational studies), and then by emergency type (cardiac arrest, trauma, medical) and population age (adult, pediatric, mixed-age). All meta-analysis outcomes were reported as favoring one of the two compared approaches, or no difference. Risk ratios (RR) were used as the effect measure, and reported with 95% confidence intervals (CIs). Studies were combined using random effects models based on profile-likelihood (Citation9). Statistical heterogeneity was assessed using the χ2 test, and the magnitude of heterogeneity using the I2 statistic (Citation10). When available, intention to treat and propensity score matched results for RCTs and observational studies, respectively, were prioritized. Sensitivity analyses were conducted using other data (e.g., data from per-protocol, or as treated analysis for RCTs and results using all data from observational studies), or by excluding outlier studies (see full report for details [AHRQ Airway Report; https://effectivehealthcare.ahrq.gov/products/prehospital-airway-management/research]). All analyses were performed by using STATA®16.1 (StataCorp, College Station, TX).
Strength of Evidence
The strength of evidence (SOE) for each KQ was initially assessed by one researcher for each clinical outcome as low, moderate, high, or insufficient as per the AHRQ Methods Guide (Citation6) (Appendix A). RCTs and observational studies were not combined in the pooled estimates, and are reported separately by study design. However, SOE assessments were based on the entire body of evidence (RCTs and observational studies). For overall SOE ratings, RCTs with low or moderate risk of bias were prioritized over observational studies. In addition, if findings from observational studies conflicted with those of RCTs, the conclusion and final SOE were based on findings from the RCTs.
ROB ratings were provided based on outcomes used in studies. Therefore, some studies were given an overall rating of low, moderate, or high ROB, whereas other studies were given multiple ROB ratings specific to different outcomes. Study-specific ratings can be found in Appendix G of the full report [AHRQ Airway Report; https://effectivehealthcare.ahrq.gov/products/prehospital-airway-management/research].
Results
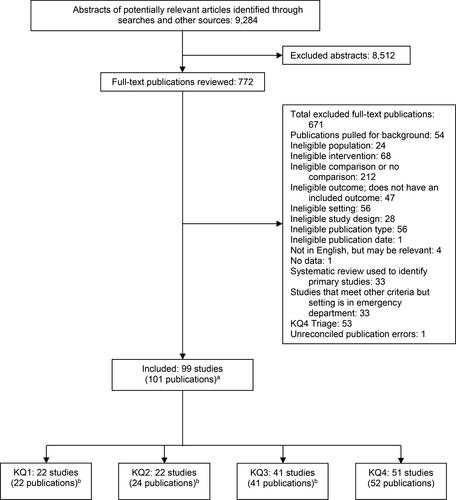
A total of 9,284 abstracts and 772 full-text articles were reviewed (). Of the 99 included studies from 101 publications (N=630,397), 22 were RCTs, 20 were prospective and 50 retrospective observational studies, and 7 used before/after study designs. Most studies were conducted in the U.S. and Canada, followed by Europe, then Asia. Most studies enrolled adults and patients with cardiac arrest; care was most often provided by ETI-capable or mixed EMS personnel levels, using ground transport in urban or mixed prehospital settings.
Figure 2. Literature flow diagram. KQ = Key Question. aSome included publications are counted in multiple sections. bEvans, 2016 was counted as two trials.
Summary of Overall Results
The overall results are summarized as follows and in . Detailed results are presented in the individual KQ sections. Sufficient evidence was not available to address all outcomes and all patient characteristics, provider characteristics, and variations in techniques that were specified a priori.
Table 1. Overview of conclusions: comparison by emergency types and age groups
Survival measured in-hospital or at 1-month post incident:
No difference in outcomes across all three comparisons in adult/mixed-age and pediatric patients with cardiac arrest.
No difference when BVM was compared with ETI in adult patients with trauma.
Neurological function measured by the Cerebral Performance Category (CPC), Pediatric CPC, or modified Rankin Scale (mRS) in-hospital or at 1-month post incident:
When BVM was compared with SGA, outcomes favored BVM in adult patients with cardiac arrest.
When SGA was compared with ETI, outcomes measured by the CPC favored ETI in adult patients with cardiac arrest; there was no difference in outcomes measured by the mRS in this group.
When BVM was compared with ETI, there was no difference in outcomes in adult patients with cardiac arrest.
When ETI was compared with BVM or SGA, there was no difference in outcomes in pediatric patients with cardiac arrest.
Return of spontaneous circulation (ROSC) (prehospital, sustained, or overall):
When BVM was compared with SGA or ETI, there was no difference in outcomes in adult patients with cardiac arrest.
When SGA was compared with ETI, outcomes favored SGA in adult patients with cardiac arrest.
When ETI was compared with BVM or SGA, there was no difference in outcomes in pediatric patients with cardiac arrest.
Successful advanced airway insertion when SGA is compared with ETI:
First-pass success favored SGA in adult patients with cardiac arrest and with mixed emergency types, and in pediatric patients with cardiac arrest; no difference was noted in adult patients with medical emergencies.
No difference in overall airway insertion success in adult patients with cardiac arrest, medical emergencies, or mixed emergency types.
Key Question 1: What Are the Comparative Benefits and Harms of BVM versus SGA for Patients Requiring Prehospital Ventilatory Support or Airway Protection?
Twenty-two studies (n = 70,718) provided data to compare BVM versus SGA in survival (patients with cardiac arrest or trauma), neurological function (cardiac arrest), and ROSC (cardiac arrest) (Citation11–31). Meta-analysis indicated no significant difference in survival measured in-hospital or at one-month post-incident in adult/mixed-age (14 studies; SOE: Low) and pediatric (2 studies; SOE: Low) patients with cardiac arrest (). While the primary analysis of observational studies enrolling adults favored BVM, sensitivity analyses excluding high ROB studies suggested no difference between these two methods, similar to the primary results from the RCTs.
There was insufficient evidence to assess comparative benefits and harms in trauma patients, as only one observational study was eligible for inclusion, resulting in no conclusion ().
Data for neurological function, measured by the Cerebral Performance Category (CPC) or Pediatric CPC at discharge or 1-month post-incident favored BVM over SGA in adults in RCTs and observational studies (9 studies; SOE: Low), although sensitivity analyses excluding high ROB indicated no difference in observational studies. Evidence was insufficient to make conclusions about effects of BVM versus SGA on pediatric patients for neurological function ().
Rates of ROSC (pre-hospital, sustained, or overall) were not significantly different between BVM and SGA for adults with cardiac arrest (12 studies; SOE: Low); there was insufficient evidence to support a conclusion for pediatric patients ().
A qualitative analysis of four studies (2 RCTs and 2 observational) indicated no difference in the majority of reported harms between BVM and SGA (SOE: Moderate) (Citation14, Citation17, Citation21, Citation25). One study reported lower rates of aspiration pneumonia within 72 hours with use of BVM versus SGA (5% vs. 33%) (Citation17).
Key Question 2: What Are the Comparative Benefits and Harms of BVM versus ETI for Patients Requiring Prehospital Ventilatory Support or Airway Protection?
Twenty-two studies (n = 106,325) provided data to compare BVM versus ETI in survival (patients with cardiac arrest or trauma), neurological function (cardiac arrest), and ROSC (cardiac arrest) (Citation11, Citation13, Citation15–17, Citation19, Citation20, Citation22–24, Citation27, Citation29–41). Meta-analysis indicated no significant difference in survival measured in-hospital or at 1-month post-incident in adult/mixed age (10 studies; SOE: Moderate) and pediatric cardiac arrest patients (3 studies; SOE: Low), and in adult/mixed-age trauma patients (3 studies: SOE: Low) (). There was insufficient evidence to support a conclusion for pediatric trauma patients.
For neurological function, measured by the CPC or Pediatric CPC in-hospital or at 1-month post-incident, there was no significant difference in adult (7 studies; SOE: Moderate) and pediatric (2 studies; SOE: Low) patients with cardiac arrest ().
There was no significant difference in rates of ROSC (pre-hospital, sustained, or overall) in adult (10 studies; SOE: Low) and pediatric (1 study; SOE: Low) patients with cardiac arrest ().
A qualitative analysis of five studies (2 RCTs, 1 CCT, and 2 observational) indicated no difference in the majority of reported harms between BVM and ETI (Citation17, Citation32–36, Citation38). One study reported a lower rate of regurgitation for ETI compared with BVM; 7.7% difference (95% CI 4.9 to 10.4), p < 0.001 (Citation33).
Key Question 3: What Are the Comparative Benefits and Harms of SGA versus ETI for Patients Requiring Prehospital Ventilatory Support or Airway Protection?
Forty-one studies (n = 383,953) provided data to compare SGA versus ETI in survival (patients with cardiac arrest or trauma), neurological function (cardiac arrest), ROSC (cardiac arrest), and first-pass and overall successful advanced airway insertion (cardiac arrest, trauma, medical, and mixed emergency types) (Citation11, Citation13, Citation15–17, Citation19, Citation20, Citation22–24, Citation27, Citation29–31, Citation37, Citation42–67). Meta-analysis indicated no significant difference in survival measured in-hospital or at 1-month post-incident in adult/mixed-age (16 studies; SOE: Low) and pediatric (3 studies; SOE: Low) patients with cardiac arrest (). There was insufficient evidence to support a conclusion about patients with trauma.
Neurological function favored ETI over SGA for adult cardiac arrest patients when measured at discharge in studies using the CPC score (11 studies; SOE: Low), but there was no difference at discharge when measured in studies using the mRS (3 studies; SOE: Low). There was no difference between SGA versus ETI in pediatric cardiac arrest patients when measured at discharge by the Pediatric CPC (2 studies; SOE: Low) ().
Rates of ROSC (pre-hospital, sustained, or overall) favored SGA over ETI for adult patients with cardiac arrest (16 studies; SOE: Low) (). These findings were inconsistent between RCTs and observational studies, resulting in low SOE. There was no significant difference for pediatric patients with cardiac arrest (2 studies; SOE: Low).
First-pass insertion success favored SGA over ETI for adult (5 studies; SOE: Low) and pediatric (2 studies; SOE: Low) patients with cardiac arrest, and for adult patients with mixed emergency types (2 studies; SOE: Low) (). There was no significant difference in adult patients with medical emergencies (2 studies; SOE: Low). There was insufficient evidence to support conclusions in adult and pediatric patients with trauma, and in pediatric patients with medical emergencies.
There was no significant difference in overall airway insertion success between SGA versus ETI in adult patients with cardiac arrest (9 studies; SOE: moderate), medical emergencies (3 studies; SOE: Moderate), and mixed emergency types (3 studies; SOE: Moderate) (). There was insufficient evidence to support a conclusion about adult patients with trauma.
A qualitative analysis of seven studies (2 RCTs, 5 observational) indicated no difference between SGA versus ETI for aspiration (2 studies), oral/airway trauma (2 studies), or regurgitation (1 study). SGA was favored over ETI for multiple insertion attempts (1 study); ETI was favored over SGA for inadequate ventilation (1 study) (Citation17, Citation30, Citation45, Citation53, Citation54, Citation60, Citation65). The SOE for each of these harms was moderate.
Discussion
An essential part of prehospital care is airway management, which enables patients to receive adequate oxygenation and ventilation. There are currently three main approaches to airway management: BVM (usually with airway adjuncts such as oropharyngeal airway [OPA] and nasopharyngeal airway [NPA]), SGA, and ETI. While guidelines and best practices exist, individual experiences, policies, and research do not definitively support one airway approach over another. Furthermore, airway management approaches are often used in a complementary fashion so that one serves as a backup when the other is deemed ineffective. Our review quantitatively synthesized results from pairwise comparisons of the three primary approaches for survival in-hospital or at 1-month post-incident, neurological function, ROSC and successful advanced airway insertion. Overall, evidence indicated few differences between airway approaches; when statistically significant differences occurred, they were for specific outcomes/comparisons and did not indicate a pattern favoring one airway over another across multiple outcomes.
For KQ1 (BVM versus SGA), our confidence in the findings is limited, as it often was not clear whether the comparison was BVM versus SGA directly, or BVM versus BVM initially, followed by SGA insertion. Studies did not always clearly identify whether other devices (e.g., OPA and NPA) were used in conjunction with BVM, or describe how BVM was actually performed (e.g., by one- vs. two-person technique). Finally, some studies assessed efficacy of BVM using chest rise and fall, which is not always measured reliably or consistently across providers. More objective measures of ventilation effectiveness, such as waveform capnography or tidal volume measurements, would be useful, as blood gas analysis is not practical in the prehospital setting.
There is a strong possibility that resuscitation time bias influenced results favoring BVM (Citation68). Resuscitation time bias refers to interventions that are applied at varying time points; those applied later are less effective in part due to their delayed application. As BVM typically is the first airway management technique used in the field, effects of successful BVM would be favorably confounded by the shorter time between EMS arrival and airway intervention. This is particularly true for patients presenting with cardiac arrest with favorable features such as being witnessed, receiving bystander CPR, and a shockable initial rhythm. Another contributing factor is hyperventilation, which may occur more frequently with advanced airways (SGA or ETI) than with BVM. Hyperventilation has been shown to adversely impact patient outcomes in part by increasing intrathoracic pressure and decreasing venous return, ultimately leading to decreased cerebral and coronary perfusion pressures (Citation69–73).
For KQ2 (BVM versus ETI), the same caveats apply as identified for KQ1 with respect to study limitations. For example, whether ETI was preceded by BVM or not, the lack of precise details on BVM use and subjective measurement of its effectiveness, as well as resuscitation time bias, potential hyperventilation following ETI, and provider level/experience, all limit conclusions for this question.
For KQ3 (SGA vs. ETI), compared with ETI, SGA had higher first-pass success in specific subgroups. However, no difference was noted in rates of overall insertion success. It is thought that SGAs may not protect against aspiration and thus may not work well for patients with vomitous, fluid, or blood in the airway. While overall rates of aspiration were similar between groups, aspiration may be more common during or after an advanced airway attempt with SGA as compared to ETI. Since the SGA is placed above the glottis, it may also be more difficult for EMS clinicians to hyperventilate with the SGA than with ETI, but our ability to assess this is limited by the lack of ventilation data in the included studies. This is an important topic for future research.
Most studies reported that ROSC outcomes were improved with SGA versus ETI. Survival and neurological function are influenced by post-resuscitation care, including hospital procedures (e.g., targeted temperature management, cardiac catheterization, and critical care expertise) and shared decision making with family regarding prognosis and withdrawal of life sustaining treatments. Best practices regarding neuroprognostication are evolving, and unfortunately at present patients may be moved too quickly to comfort care, especially following cardiac arrest (Citation74). Therefore, post-resuscitation care differences deserve detailed attention in future airway management comparison studies in cardiac arrest.
Limitations
The most serious limitations of this review were related to the comparatively weak study designs used to compare airway management approaches and the risk of biases that are common challenges in prehospital and emergency care research. While the body of evidence did include randomized clinical trials, the majority of included studies were retrospective observational studies based on analyses of data from national or regional registries or administrative data from a single health system or EMS agency. Observational studies are more susceptible to bias. Indication bias, classifying patients by the treatment received, and survival bias, including only patients who survive a treatment, are variants of selection bias that are likely to occur in observational studies of prehospital care. Furthermore, data on important confounding variables are often limited in large databases, and retrospective analyses may not account for all relevant potential confounders, even with matched propensity score analyses.
Importantly, EMS clinicians acquire skill in all airway procedures over time and with practice. The skillset of the provider with each technique was rarely controlled for in the studies included in this review. It is possible that providers have greater skill with one technique more than another, which introduces another potential source of bias into the body of evidence.
Other limitations are specific to advanced airway management in the prehospital setting. In the field, use of more than one airway is typical with a progression through different approaches as the patient is assessed. The use of multiple airways, and the order and duration of each may affect outcomes, but this information is rarely documented precisely and included in analyses. Another concern is resuscitation time bias (i.e., the intervention is influenced by duration of resuscitation) and the patient’s status and course of treatment preceding airway placement, which may influence both the intervention received and outcomes (Citation68). The preparation time needed for different airway management techniques and the differences in skill and experience may be confounders, and the impact is often difficult to separate from the airway technique itself.
Finally, there is a paucity of data regarding prehospital ventilation; most airway trials to date have not addressed what happens after the airway is secured. Findings regarding ventilation as an outcome are limited by the lack of consistent measurement methods. Better tools are needed to measure ventilation parameters, in particular rate, tidal volume, and airway pressures.
Future Research
Research is needed to clarify whether there are situations in which certain airway approaches are superior, in particular in pediatric populations. Ideally, trials would compare all three airway approaches. Studies should clearly identify devices and airway management methods used (e.g., whether adjuncts were used with BVM [OPA, NPA]) to allow for more accurate and direct comparisons of the different airway methods. Research should incorporate objective measures of success in oxygenation and ventilation (e.g., waveform capnography, video monitoring, in-line ventilation rate, flow, tidal volume, and pressure, etc.). Resuscitation time bias remains an important issue in cardiac arrest studies, and efforts should be made to accurately capture airway intervention times to mitigate this concern. Research also is needed to identify optimal methods to acquire and maintain airway management skills in the prehospital setting. Further studies are also needed with regard to the impact of race and sex on the outcomes of different airway management strategies.
Conclusion
Overall, there is limited evidence to suggest differences in patient-centered outcomes between use of BVM, SGA, and ETI in prehospital airway management. This topic converges vast variation in multiple factors (patient characteristics, emergency types, provider level) in an emergent environment that defies control, thereby limiting the ability to systematically apply and study interventions. The findings from this review are detailed and comprehensive, and can inform policy, practice, education, and future research to improve prehospital airway management and ventilation support to optimize patient outcomes.
Supplemental Material
Download MS Word (35.3 KB)Additional information
Funding
References
- Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, Lapandry C. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87(6):1290–7. doi:10.1097/00000542-199712000-00005.
- Caruana E, Duchateau FX, Cornaglia C, Devaud ML, Pirracchio R. Tracheal intubation related complications in the prehospital setting. Emerg Med J. 2015;32(11):882–7. doi:10.1136/emermed-2013-203372.
- Cook T, Behringer EC, Benger J. Airway management outside the operating room: hazardous and incompletely studied. Curr Opin Anaesthesiol. 2012;25(4):461–9. doi:10.1097/ACO.0b013e32835528b1.
- Garnier M, Bonnet F. Management of anesthetic emergencies and complications outside the operating room. Curr Opin Anaesthesiol. 2014;27(4):437–41. doi:10.1097/ACO.0000000000000088.
- Pepe PE, Roppolo LP, Fowler RL. Prehospital endotracheal intubation: elemental or detrimental? Crit Care. 2015;19:121. doi:10.1186/s13054-015-0808-x.
- Agency for Healthcare Research and Quality. Agency for healthcare research and quality. Future research needs – methods research series, 2010 [accessed 2019 October 12]. https://effectivehealthcare.ahrq.gov/products/future-research-needs-methods/overview.
- Higgins J, Savović J, Page M, Elbers R, Sterne J. Chapter 8: Assessing risk of bias in a randomized trial. In: Cochrane handbook for systematic reviews of interventions version 6 (updated July 2019) [Internet]. Hoboken, NJ: Wiley; Cochrane; 2019. www.training.cochrane.org/handbook.
- United States Preventive Services Task Force. US preventive services task force procedure manual. Rockville, MD: Agency for Healthcare Research and Quality: 2018 [accessed 2019 December 26]. https://www.uspreventiveservicestaskforce.org/Page/Name/procedure-manual.
- Hardy RJ, Thompson SG. A likelihood approach to meta-analysis with random effects. Statist Med. 1996;15(6):619–29. doi:10.1002/(SICI)1097-0258(19960330)15:6<619::AID-SIM188>3.0.CO;2-A.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. doi:10.1002/sim.1186.
- Chiang W-C, Hsieh M-J, Chu H-L, Chen AY, Wen S-Y, Yang W-S, Chien Y-C, Wang Y-C, Lee B-C, Wang H-C, et al. The effect of successful intubation on patient outcomes after out-of-hospital cardiac arrest in Taipei. Ann Emerg Med. 2018;71(3):387–96.e2. doi:10.1016/j.annemergmed.2017.08.008.
- Chien L-C, Hsu H-C, Lin C-H, Cheng C-F, Tung Y-C, Hung H-C, Yeh Y-C, Tsai M-C. Use of an intubating laryngeal mask airway on out-of-hospital cardiac arrest patients in a developing emergency medical service system. J Formos Med Assoc. 2012;111(1):24–9. doi:10.1016/j.jfma.2012.01.004.
- Evans CCD, Petersen A, Meier EN, Buick JE, Schreiber M, Kannas D, Austin MA, Resuscitation Outcomes Consortium Investigators. Prehospital traumatic cardiac arrest: management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg. 2016;81(2):285–93. doi:10.1097/TA.0000000000001070.
- Fiala A, Lederer W, Neumayr A, Egger T, Neururer S, Toferer E, Baubin M, Paal P. EMT-led laryngeal tube vs. face-mask ventilation during cardiopulmonary resuscitation - a multicenter prospective randomized trial. Scand J Trauma Resusc Emerg Med. 2017;25(1):104. doi:10.1186/s13049-017-0446-1.
- Hanif MA, Kaji AH, Niemann JT. Advanced airway management does not improve outcome of out-of-hospital cardiac arrest. Acad Emerg Med. 2010;17(9):926–31. doi:10.1111/j.1553-2712.2010.00829.x.
- Hansen ML, Lin A, Eriksson C, Daya M, McNally B, Fu R, Yanez D, Zive D, Newgard C, CARES Surveillance Group. A comparison of pediatric airway management techniques during out-of-hospital cardiac arrest using the CARES database. Resuscitation. 2017;120:51–6. doi:10.1016/j.resuscitation.2017.08.015.
- Hansen M, Wang H, Le N, Lin A, Idris A, Kornegay J, Schmicker R, Daya M. Prospective evaluation of airway management in pediatric out-of-hospital cardiac arrest. Resuscitation. 2020;156:53–60. doi:10.1016/j.resuscitation.2020.08.003.
- Hardy GB, Maddry JK, Ng PC, Savell SC, Arana AA, Kester A, Bebarta VS. Impact of prehospital airway management on combat mortality. Am J Emerg Med. 2018;36(6):1032–5. doi:10.1016/j.ajem.2018.02.007.
- Kang K, Kim T, Ro YS, Kim YJ, Song KJ, Shin SD. Prehospital endotracheal intubation and survival after out-of-hospital cardiac arrest: results from the Korean nationwide registry. Am J Emerg Med. 2016;34(2):128–32. doi:10.1016/j.ajem.2015.09.036.
- Lupton JR, Schmicker RH, Stephens S, Carlson JN, Callaway C, Herren H, Idris AH, Sopko G, Puyana JCJ, Daya MR, et al. Outcomes with the use of bag-valve-mask ventilation during out-of-hospital cardiac arrest in the Pragmatic Airway Resuscitation Trial. Acad Emerg Med. 2020;27(5):366–74. doi:10.1111/acem.13927.
- Maignan M, Koch F-X, Kraemer M, Lehodey B, Viglino D, Monnet M-F, Pham D, Roux C, Genty C, Rolland C, et al. Impact of laryngeal tube use on chest compression fraction during out-of-hospital cardiac arrest. A prospective alternate month study. Resuscitation. 2015;93:113–7. doi:10.1016/j.resuscitation.2015.06.002.
- Nagao T, Kinoshita K, Sakurai A, Yamaguchi J, Furukawa M, Utagawa A, Moriya T, Azuhata T, Tanjoh K. Effects of bag-mask versus advanced airway ventilation for patients undergoing prolonged cardiopulmonary resuscitation in pre-hospital setting. J Emerg Med. 2012;42(2):162–70. doi:10.1016/j.jemermed.2011.02.020.
- Noda E, Zaitsu A, Hashizume M, Takahashi S. Prognosis of patient with cardiopulmonary arrest transported to Kyushu University Hospital. Fukuoka Igaku Zasshi. 2007;98(3):73–81.
- Ohashi-Fukuda N, Fukuda T, Yahagi N. Effect of pre-hospital advanced airway management for out-of-hospital cardiac arrest caused by respiratory disease: a propensity score-matched study. Anaesth Intensive Care. 2017;45(3):375–83. doi:10.1177/0310057X1704500314.
- Roth D, Hafner C, Aufmesser W, Hudabiunigg K, Wutti C, Herkner H, Schreiber W. Safety and feasibility of the laryngeal tube when used by EMTs during out-of-hospital cardiac arrest. Am J Emerg Med. 2015;33(8):1050–5. doi:10.1016/j.ajem.2015.04.048.
- Rumball CJ, MacDonald D. The PTL, Combitube, laryngeal mask, and oral airway: a randomized prehospital comparative study of ventilatory device effectiveness and cost-effectiveness in 470 cases of cardiorespiratory arrest. Prehosp Emerg Care. 1997;1(1):1–10. doi:10.1080/10903129708958776.
- Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83(3):313–9. doi:10.1016/j.resuscitation.2011.10.028.
- Sos K, Study G. Comparison of arterial blood gases of laryngeal mask airway and bag-valve-mask ventilation in out-of-hospital cardiac arrests. Circ J. 2009;73(3):490–6. doi:10.1253/circj.CJ-08-0874.
- Sulzgruber P, Datler P, Sterz F, Poppe M, Lobmeyr E, Keferböck M, Zeiner S, Nürnberger A, Schober A, Hubner P, et al. The impact of airway strategy on the patient outcome after out-of-hospital cardiac arrest: a propensity score matched analysis. Europ Heart J Acute Cardiovasc Care. 2018;7(5):423–31. doi:10.1177/2048872617731894.
- Wang HE, Schmicker RH, Daya MR, Stephens SW, Idris AH, Carlson JN, Colella MR, Herren H, Hansen M, Richmond NJ, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2018;320(8):769–78. doi:10.1001/jama.2018.7044.
- Yanagawa Y, Sakamoto T. Analysis of prehospital care for cardiac arrest in an urban setting in Japan. J Emerg Med. 2010;38(3):340–5. doi:10.1016/j.jemermed.2008.04.037.
- Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M, Cooper DJ, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg. 2010;252(6):959–65. doi:10.1097/SLA.0b013e3181efc15f.
- Jabre P, Penaloza A, Pinero D, Duchateau F-X, Borron SW, Javaudin F, Richard O, de Longueville D, Bouilleau G, Devaud M-L, et al. Effect of bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after out-of-hospital cardiorespiratory arrest: a randomized clinical trial. JAMA. 2018;319(8):779–87. doi:10.1001/jama.2018.0156.
- Malinverni S, Bartiaux M, Cavallotto F, De Longueville D, Mols P, Gorlicki J, Adnet F. Does endotracheal intubation increases chest compression fraction in out of hospital cardiac arrest: a substudy of the CAAM trial. Resuscitation. 2019;137:35–40. doi:10.1016/j.resuscitation.2019.01.032.
- Gausche M, Lewis RJ, Stratton SJ, Haynes BE, Gunter CS, Goodrich SM, Poore PD, McCollough MD, Henderson DP, Pratt FD, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. see comment erratum appears. JAMA. 2000;283(6):783–90. doi:10.1001/jama.283.6.783.
- Gausche-Hill M, Lewis RJ, Gunter CS, Henderson DP, Haynes BE, Stratton SJ. Design and implementation of a controlled trial of pediatric endotracheal intubation in the out-of-hospital setting. Ann Emerg Med. 2000;36(4):356–65. doi:10.1067/mem.2000.109447.
- Takei Y, Enami M, Yachida T, Ohta K, Inaba H. Tracheal intubation by paramedics under limited indication criteria may improve the short-term outcome of out-of-hospital cardiac arrests with noncardiac origin. J Anesth. 2010;24(5):716–25. doi:10.1007/s00540-010-0974-6.
- Cooper A, DiScala C, Foltin G, Tunik M, Markenson D, Welborn C. Prehospital endotracheal intubation for severe head injury in children: a reappraisal. Semin Pediatr Surg. 2001;10(1):3–6. doi:10.1053/spsu.2001.19379.
- Eckstein M, Chan L, Schneir A, Palmer R. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma. 2000;48(4):643–8. doi:10.1097/00005373-200004000-00010.
- Stockinger ZT, McSwain NE, Jr. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56(3):531–6.
- Yuksen C, Phattharapornjaroen P, Kreethep W, Suwanmano C, Jenpanitpong C, Nonnongku R, Sittichanbuncha Y, Sawanyawisuth K. Bag-valve mask versus endotracheal intubation in out-of-hospital cardiac arrest on return of spontaneous circulation: a national database study. Open Access Emerg Med. 2020;12:43–6. doi:10.2147/OAEM.S229356.
- Bartlett RL, Martin SD, McMahon JM, Jr, Schafermeyer RW, Vukich DJ, Hornung CA. A field comparison of the pharyngeotracheal lumen airway and the endotracheal tube. J Trauma. 1992;32(3):280–4. doi:10.1097/00005373-199203000-00002.
- Becker TK, Berning AW, Prabhu A, Callaway CW, Guyette FX, Martin-Gill C. An assessment of ventilation and perfusion markers in out-of-hospital cardiac arrest patients receiving mechanical CPR with endotracheal or supraglottic airways. Resuscitation. 2018;122:61–4. doi:10.1016/j.resuscitation.2017.11.054.
- Behrens N-H, Fischer M, Krieger T, Monaco K, Wnent J, Seewald S, Gräsner J-T, Bernhard M. Effect of airway management strategies during resuscitation from out-of-hospital cardiac arrest on clinical outcome: a registry-based analysis. Resuscitation. 2020;152:157–64. doi:10.1016/j.resuscitation.2020.04.015.
- Benger JR, Kirby K, Black S, Brett SJ, Clout M, Lazaroo MJ, Nolan JP, Reeves BC, Robinson M, Scott LJ, et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: the AIRWAYS-2 randomized clinical trial. JAMA. 2018;320(8):779–91. doi:10.1001/jama.2018.11597.
- Cady CE, Pirrallo RG. The effect of Combitube use on paramedic experience in endotracheal intubation. Am J Emerg Med. 2005;23(7):868–71. doi:10.1016/j.ajem.2005.07.013.
- Davis DP, Peay J, Sise MJ, Vilke BM, Kennedy F, Eastman AB, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58(5):933–9.
- Duckett J, Fell P, Han K, Kimber C, Taylor C. Introduction of the I-gel supraglottic airway device for prehospital airway management in a UK ambulance service. Emerg Med J. 2014;31(6):505–7. doi:10.1136/emermed-2012-202126.
- Edwards T, Williams J, Cottee M. Influence of prehospital airway management on neurological outcome in patients transferred to a heart attack centre following out-of-hospital cardiac arrest. Emerg Med Australas. 2019;31(1):76–82. doi:10.1111/1742-6723.13107.
- Frascone RJ, Russi C, Lick C, Conterato M, Wewerka SS, Griffith KR, Myers L, Conners J, Salzman JG. Comparison of prehospital insertion success rates and time to insertion between standard endotracheal intubation and a supraglottic airway. Resuscitation. 2011;82(12):1529–36. doi:10.1016/j.resuscitation.2011.07.009.
- Fukuda T, Sekiguchi H, Taira T, Hashizume N, Kitamura Y, Terada T, Ohashi-Fukuda N, Kukita I. Type of advanced airway and survival after pediatric out-of-hospital cardiac arrest. Resuscitation. 2020;150:145–53. doi:10.1016/j.resuscitation.2020.02.005.
- Gamberini L, Giugni A, Ranieri S, Meconi T, Coniglio C, Gordini G, Bardi T. Early-onset ventilator-associated pneumonia in severe traumatic brain injury: is there a relationship with prehospital airway management? J Emerg Med. 2019;56(6):657–65. doi:10.1016/j.jemermed.2019.02.005.
- Gahan K, Studnek JR, Vandeventer S. King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resuscitation. 2011;82(12):1525–8. doi:10.1016/j.resuscitation.2011.06.036.
- Hankins DG, Carruthers N, Frascone RJ, Long LA, Campion BC. Complication rates for the esophageal obturator airway and endotracheal tube in the prehospital setting. Prehosp Disaster Med. 1993;8(2):117–21. doi:10.1017/s1049023x00040176.
- Hiltunen P, Jantti H, Silfvast T, Kuisma M, Kurola J, Group FPs, for the FINNRESUSCI Prehospital Study Group. Airway management in out-of-hospital cardiac arrest in Finland: current practices and outcomes. Scand J Trauma Resusc Emerg Med. 2016;24(1):49. doi:10.1186/s13049-016-0235-2.
- Jarman AF, Hopkins CL, Hansen JN, Brown JR, Burk C, Youngquist ST. Advanced airway type and its association with chest compression interruptions during out-of-hospital cardiac arrest resuscitation attempts. Prehosp Emerg Care. 2017;21(5):628–35. doi:10.1080/10903127.2017.1308611.
- Jarvis JL, Wampler D, Wang HE. Association of patient age with first pass success in out-of-hospital advanced airway management. Resuscitation. 2019;141:136–43. doi:10.1016/j.resuscitation.2019.06.002.
- Kajino K, Iwami T, Kitamura T, Daya M, Ong M, Nishiuchi T, Hayashi Y, Sakai T, Shimazu T, Hiraide A, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care. 2011;15(5):R236. doi:10.1186/cc10483.
- McCall MJ, Reeves M, Skinner M, Ginifer C, Myles P, Dalwood N. Paramedic tracheal intubation using the intubating laryngeal mask airway. Prehosp Emerg Care. 2008;12(1):30–4. doi:10.1080/10903120701709803.
- McMahan S, Ornato JP, Racht EM, Cameron J. Multi-agency, prehospital evaluation of the pharyngeo-tracheal lumen (PTL) airway. Prehosp Disaster Med. 1992;7(1):13–8. doi:10.1017/s1049023x00039145.
- McMullan J, Gerecht R, Bonomo J, Robb R, McNally B, Donnelly J, Wang HE, CARES Surveillance Group. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85(5):617–22. doi:10.1016/j.resuscitation.2014.02.007.
- Nwanne T, Jarvis J, Barton D, Donnelly JP, Wang HE. Advanced airway management success rates in a national cohort of emergency medical services agencies. Resuscitation. 2020;146:43–9. doi:10.1016/j.resuscitation.2019.11.006.
- Rabitsch W, Schellongowski P, Staudinger T, Hofbauer R, Dufek V, Eder B, Raab H, Thell R, Schuster E, Frass M, et al. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Resuscitation. 2003;57(1):27–32. doi:10.1016/S0300-9572(02)00435-5.
- Rumball C, Macdonald D, Barber P, Wong H, Smecher C. Endotracheal intubation and esophageal tracheal Combitube insertion by regular ambulance attendants: a comparative trial. Prehosp Emerg Care. 2004;8(1):15–22. doi:10.1080/312703002764.
- Steuerwald MT, Braude DA, Petersen TR, Peterson K, Torres MA. Preliminary report: comparing aspiration rates between prehospital patients managed with extraglottic airway devices and endotracheal intubation. Air Med J. 2018;37(4):240–3. doi:10.1016/j.amj.2018.04.004.
- Tanabe S, Ogawa T, Akahane M, Koike S, Horiguchi H, Yasunaga H, Mizoguchi T, Hatanaka T, Yokota H, Imamura T, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J Emerg Med. 2013;44(2):389–97. doi:10.1016/j.jemermed.2012.02.026.
- Wang HE, Szydlo D, Stouffer JA, Lin S, Carlson JN, Vaillancourt C, Sears G, Verbeek RP, Fowler R, Idris AH, ROC Investigators, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation. 2012;83(9):1061–6. doi:10.1016/j.resuscitation.2012.05.018.
- Andersen LW, Grossestreuer AV, Donnino MW. "Resuscitation time bias" - A unique challenge for observational cardiac arrest research. Resuscitation. 2018;125:79–82. doi:10.1016/j.resuscitation.2018.02.006.
- Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9 Suppl):S345–S51.
- Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, von Briesen C, Sparks CW, Conrad CJ, Provo TA, Lurie KG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109(16):1960–5. doi:10.1161/01.CIR.0000126594.79136.61.
- Davis DP, Dunford JV, Poste JC, Ochs M, Holbrook T, Fortlage D, et al. The impact of hypoxia and hyperventilation on outcome after paramedic rapid sequence intubation of severely head-injured patients. J Trauma. 2004;57(1):1–8.
- Gaither JB, Spaite DW, Bobrow BJ, Denninghoff KR, Stolz U, Beskind DL, Meislin HW. Balancing the potential risks and benefits of out-of-hospital intubation in traumatic brain injury: the intubation/hyperventilation effect. Ann Emerg Med. 2012;60(6):732–6. doi:10.1016/j.annemergmed.2012.06.017.
- Pepe PE, Lurie KG, Wigginton JG, Raedler C, Idris AH. Detrimental hemodynamic effects of assisted ventilation in hemorrhagic states. Crit Care Med. 2004;32(9 Suppl):S414–S20.
- Elmer J, Torres C, Aufderheide TP, Austin MA, Callaway CW, Golan E, Herren H, Jasti J, Kudenchuk PJ, Scales DC, et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation. 2016;102:127–35. doi:10.1016/j.resuscitation.2016.01.016.
