Abstract
Objective
Emergency medical services (EMS) workforce demographics in the United States do not reflect the diversity of the population served. Despite some efforts by professional organizations to create a more representative workforce, little has changed in the last decade. This scoping review aims to summarize existing literature on the demographic composition, recruitment, retention, and workplace experience of underrepresented groups within EMS.
Methods
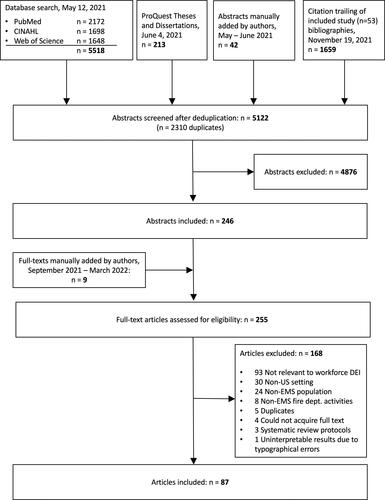
Peer-reviewed studies were obtained from a search of PubMed, CINAHL, Web of Science, ProQuest Thesis and Dissertations, and non-peer-reviewed (“gray”) literature from 1960 to present. Abstracts and included full-text articles were screened by two independent reviewers trained on inclusion/exclusion criteria. Studies were included if they pertained to the demographics, training, hiring, retention, promotion, compensation, or workplace experience of underrepresented groups in United States EMS by race, ethnicity, sexual orientation, or gender. Studies of non-EMS fire department activities were excluded. Disputes were resolved by two authors. A single reviewer screened the gray literature. Data extraction was performed using a standardized electronic form. Results were summarized qualitatively.
Results
We identified 87 relevant full-text articles from the peer-reviewed literature and 250 items of gray literature. Primary themes emerging from peer-reviewed literature included workplace experience (n = 48), demographics (n = 12), workforce entry and exit (n = 8), education and testing (n = 7), compensation and benefits (n = 5), and leadership, mentorship, and promotion (n = 4). Most articles focused on sex/gender comparisons (65/87, 75%), followed by race/ethnicity comparisons (42/87, 48%). Few articles examined sexual orientation (3/87, 3%). One study focused on telecommunicators and three included EMS physicians. Most studies (n = 60, 69%) were published in the last decade. In the gray literature, media articles (216/250, 86%) demonstrated significant industry discourse surrounding these primary themes.
Conclusions
Existing EMS workforce research demonstrates continued underrepresentation of women and nonwhite personnel. Additionally, these studies raise concerns for pervasive negative workplace experiences including sexual harassment and factors that negatively affect recruitment and retention, including bias in candidate testing, a gender pay gap, and unequal promotion opportunities. Additional research is needed to elucidate recruitment and retention program efficacy, the demographic composition of EMS leadership, and the prevalence of racial harassment and discrimination in this workforce.
Introduction
The diversity of the emergency medical services (EMS) workforce is not reflective of the population of the United States (US) and is not projected to change significantly in the near future (Citation1). A workforce that is reflective of the increasing diversity of communities in which health care professionals serve is critical to delivering high-quality, patient-centered care (Citation2). As such, many areas of health care, including EMS, have embraced the call to develop more diverse and inclusive workforces (Citation3–6).
The benefits of an inclusive and representative workforce have been demonstrated in multiple health care sectors. Clinicians from underrepresented racial and ethnic backgrounds are more likely to work in underserved communities, resulting in improved access to care, patient satisfaction, and outcomes (Citation2). The racial and gender concordance of patients and their health care professionals may influence treatments, patient-clinician communication, and patient perceptions of the care they receive (Citation7–9). Diversity and cultural competence in medicine have also been considered important in improving patient safety (Citation10, Citation11). Finally, diverse teams are better able to creatively approach challenges by bringing multiple perspectives to problem solving (Citation12).
There has been a call from EMS leaders in both government and health care to increase workforce diversity in the industry (Citation5); however, a comprehensive review of current EMS workforce composition and the experiences of underrepresented workers in this field is lacking. Understanding the workforce experiences of underrepresented groups is crucial for developing strategies to improve the recruitment and retention of diverse clinicians. Thus, we sought to identify gaps in the literature and provide a summary of existing knowledge to aid in the development of such recruitment and retention strategies. The objectives of this scoping review were to identify, summarize, and contextualize existing literature on the demographic composition, recruitment, retention, promotion, compensation, training, and workplace experiences of underrepresented groups within EMS in the US.
Methods
Study Protocol
The scoping review followed the approach described by Arksey and O’Malley in 2005 (Citation13) and refined by Levac et al. in 2010 (Citation14). The authors followed the PRISMA Extension for Scoping Reviews checklist (Citation15) [Supplement 1]. The study protocol was prospectively registered in Open Science Framework Registries Network (doi: 10.17605/OSF.IO/EDSAH).
Inclusion and Exclusion Criteria
Given the significant variability between international EMS systems, inclusion and exclusion criteria were selected to reflect US-based EMS (). Studies were included if they pertained to the demographics, training, hiring, retention, promotion, compensation, or workplace experience of underrepresented groups in US EMS by race, ethnicity, sexual orientation, or gender.
Table 1. Inclusion/exclusion criteria.
Search Strategy
Supplement 2 contains the detailed search strategy. Peer-reviewed studies were obtained from PubMed, CINAHL, and Web of Science Core Collection with the assistance of a medical research librarian (MVI). The search was last completed on 12 May 2021. Theses and dissertations were obtained from ProQuest Thesis and Dissertations (last searched 04 June 2021). Additional “gray literature,” including relevant reports, news, and editorials, was obtained from a manual search by the lead author (JSR) of Google, EMS professional and regulatory organization websites, and industry media sites (i.e., JEMS, EMS1, EMSWorld) throughout May-June 2021. Citation trailing was conducted to identify articles that cited or were cited by each of the included articles. A few additional abstracts and full-text studies were manually located during article screening and the grey literature search and were added to the screening pool.
Data Extraction
Reviewers were trained a priori to apply the inclusion/exclusion criteria () via a selection of prescreened abstracts. Peer-reviewed studies and theses/dissertations were screened for inclusion using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org). Two independent reviewers screened each title and abstract, with disagreements resolved by the lead author (JSR) in consultation with the senior author (APJ). The full text of each article passing abstract screening was then screened by two independent reviewers, with disagreements similarly resolved by the lead or senior author as recommended by Levac et al. (Citation14). When voting to include an article after reviewing its full text, authors were asked to extract relevant data via a Google Form, which was tested by the authors (JSR, APJ, AF, AH) prior to use on a selection of likely-inclusion articles to ensure functionality and appropriate data capture. Articles voted for inclusion but not extracted by the voting authors were later extracted via this Google Form by the lead author.
Data Charting and Synthesis
Extracted data were verified from the original studies by the lead author during charting. Data were charted by the lead author similarly to the method described by Arksey and O’Malley (Citation13). Briefly, data extracted from articles were entered into a spreadsheet that included key study identifiers, population, relevant demographic subgroup terminology and proportions, methodology, and relevant outcomes or conclusions. Evidence quality was informally assessed by charting the methodology and sample sizes of included items; however, in accordance with the scoping methodology, a formal quality assessment was not conducted (Citation13). Studies were then categorized by theme and their charted data were compared and summarized by the lead author. Gray literature was analyzed according to the themes identified in the peer-reviewed literature to contextualize findings within industry discourse on these topics. As recommended by Levac et al. (Citation14), expert consultation was sought from authors experienced in scoping review methodology and qualitative EMS research (DIP and RPC).
Terminology
Recently, there have been calls to use more precise and inclusive demographic language in biomedical research (Citation16). However, to assist in the critical interpretation of the literature presented in this review, when referencing studies we have used their own demographic language .
Results
Our search of the peer-reviewed literature yielded a total of 5,122 abstracts after deduplication. Reviewers agreed on the inclusion of 246/5122 (5%) abstracts for full-text screening, with nine additional full-text articles added. The authors agreed on 87/255 (34%) for inclusion ().
The gray literature search yielded 410 items, and 250/410 (61%) were included. Included items were comprised of 216/250 (86%) from industry media sites, 18/250 (7%) from a Google search, 13/250 (5%) from professional organization websites, and 3/250 (1%) manually located while reviewing other items.
General Characteristics of Included Articles
contains a list of included studies by topic, as identified through data charting. Eighty-seven studies were published over 32 years, from 1989 to 2021, with a majority published in since 2012 (60/87, 69%). Most studies included EMTs or paramedics (53/87, 61%) and compared outcomes by sex or gender (65/87, 75%). Nearly half of the studies included outcomes by race or ethnicity (42/87, 48%). Few articles examined outcomes by sexual orientation (3/87, 3%) or specified the inclusion of transgender personnel (1/87, 1%). Most studies were cross-sectional (69/87, 79%), with the most common themes addressing the workplace experience of underrepresented groups (63/87, 72%). Fewer (11/87, 13%) articles addressed themes of recruitment and retention. See Supplement 3 for additional characteristics and detailed summaries of included studies.
Table 2. Included full-text articles by theme.
Workforce Demographics
Workforce demographics were examined in 12/87 (14%) studies (Citation1, Citation17–27). Seven studies examined the demographics of the workforce of EMTs (NREMT) and paramedics (NRP) credentialed by the National Registry of Emergency Medical Technicians, with overall findings in agreement that this workforce is dominated by non-Hispanic White males (Citation1, Citation17–22). These findings were mirrored among studies examining Advanced EMTs and the previous certification level, EMT-Intermediates (Citation18, Citation21). The proportion of females in the NREMT workforce ranged from 27% to 43% across the years (Citation1, Citation17, Citation18) compared to the NRP workforce, which ranged from 20% to 35% (Citation1, Citation17). The nonwhite NREMT workforce increased from 10% in 1999 (19) to 27% in 2017 (1). Lower rates of minority clinicians were noted in the NRP workforce, increasing from 8% in 1999 (19) to 19% in 2017 (Citation1).
Two studies examined the demographics of EMS fellows and physicians (Citation23, Citation24). March et al. found lower proportions of female and minority EMS fellowship faculty compared to emergency medicine residency programs, and 31% and 48% of fellowship programs reported zero female or minority faculty, respectively (Citation23). Although a larger proportion of EMS fellows were female compared to emergency medicine residents (56% vs. 38%), there was a lower proportion of minority EMS fellows compared to minority emergency medicine residents (13% vs. 37%) (Citation23).
Within the gray literature (27/250, 11%), we found numerous reports from state, local, and federal governments (16/27, 59%) providing similar data on the underrepresentation of female and nonwhite individuals within the EMS workforce, in addition to several media articles covering the lack of current workforce diversity at both local and national levels (7/27, 26%) [Supplement 4]. No studies or reports examined the demographics of the EMS workforce by sexual orientation, nor reported the percentage of the workforce identifying as transgender.
Recruitment and Retention
Workforce Entry and Exit
Eight of 87 studies (9%) evaluated workforce entry and exit for underrepresented groups in EMS (Citation1, Citation20, Citation24, Citation28–32). Crowe et al. examined the gender of new nationally certified EMS clinicians from 2008 to 2017 and found an increase in female NREMT recruitment from 28% to 35%, but only a 2% increase in female NRPs (21% to 23%) (Citation1). Over the same period, the proportion of new minority NREMTs and NRPs increased from 22% to 27% and 13% to 19%, respectively. Most of this change was driven by an increase in Hispanic clinicians, with a greater rate of change among female Hispanic clinicians. The percentage of Black clinicians remained constant at 5% of NREMTs and 3% of NRPs (Citation1).
A small 2020 study qualitatively investigated the vocational choice of male African American and Latino paramedic students. The author identified three metanarratives of career choice among these men of color: the need for external sources of information about the profession, ongoing support for their interest from mentors and family, and external validation in their career choice (Citation28).
The sole study examining EMS workforce exit among underrepresented groups found a greater proportion of females and minorities left the nationally certified workforce compared to their overall proportion within this population (Citation29).
Lastly, one article examined diversity and inclusion initiatives via a survey of 47 fire chiefs in 2018; 49% of respondents reported that their fire departments had diversity and inclusion program leaders. A greater proportion of departments with such leaders publicly communicated their diversity goals and had greater numbers of diversity programs than those without (Citation30).
No articles examined EMS clinicians’ workforce entry or exit by sexual orientation.
Within the gray literature (57/250, 23%), a multitude of industry media articles (44/57, 77%) covered diversity recruitment initiatives at EMS agencies and fire departments around the country, with the City of Saint Paul, Minnesota, EMS Academy "Freedom House" receiving particular attention (8/57, 14%). However, no reports or studies were found that empirically reviewed the nature of existing programs nor examined the efficacy or outcomes of such programs. Other media articles covered cases of alleged racial, gender, or sexual orientation discrimination in hiring or termination (8/57, 14%) [Supplement 4].
Education and Testing
Differences in education and testing of underrepresented groups were examined in 7/87 studies (8%) (Citation33–39). Two studies examined the national demographics of EMS educators and found that, similar to the clinician workforce, a majority of educators (Citation33) and training officers (Citation34) were non-Hispanic White males.
Three articles (Citation35–37) examined completion of the standardized NREMT and NRP exams by sex or gender. A retrospective cohort analysis of all candidates attempting initial paramedic certification in 2002 found that male gender was associated with higher odds of passing the paramedic exam compared to female gender (Citation35). Two analyses of EMT candidates unsuccessful in their initial certification exam concurred that female candidates were less likely to reattempt examination (Citation36, Citation37). Powell et al. found that sex was not a significant predictor of retesting among paramedic candidates unsuccessful on their first attempts, although more females than males did not retest (16% vs. 13%) (Citation37).
Two articles examined completion of the NREMT and NRP cognitive exams by race or ethnicity (Citation35, Citation36). Dickison et al. found that among all candidates attempting initial paramedic certification in 2002, Black race was associated with a decreased odds of passing the exam in comparison to White race (OR 0.37, 95% CI 0.31–0.45) (Citation35). An analysis of NREMT candidates who failed their first examination attempts between 2007 and 2012 found that race/ethnicity did not appear to play a substantial role in retesting behavior (Citation36).
No articles examined the education and testing of EMS students or clinicians by sexual orientation.
Within the gray literature (13/250, 5%), media articles provided education related to diversity and inclusion (10/13, 77%), and covered lawsuits alleging racial or gender bias in fire department candidate testing (2/13, 15%), while a position paper from the National Association of EMS Educators argued for increased diversity in EMS education and the teaching of cultural competency in curricula [Supplement 4].
Compensation and Benefits
Compensation or benefits were evaluated in 5/87 studies (6%) (Citation24, Citation40–43). In two national samples of EMTs and paramedics, female respondents reported lower annual pay than their male counterparts (Citation40, Citation41). For paramedics, estimates of this difference ranged from $4,000–$5,000 (40) to $7,000–$11,000 in a larger survey (Citation41), while among EMTs, the difference was more pronounced, with females reporting annual pay of between $10,000 and $15,000 less than males (Citation41). A small survey of women EMS physicians found that 39% of respondents reported experiencing pay or promotional discrimination during their careers (Citation24).
Three articles examined compensation by race, largely focusing on paramedics; none found significant differences in the pay of minorities compared to White EMS clinicians (Citation40–42).
No studies examined compensation by sexual orientation.
One article discussed maternity benefits available to female firefighters, finding that a large proportion of departments lacked maternity leave (20%) or pregnancy policies (24%) (Citation43). No studies were found that examined other types of benefits, nor that examined benefits by race, ethnicity, or sexual orientation.
In the gray literature, one media article (1/250, <1%) covered a case of sexual orientation discrimination in which a paramedic was denied benefits for a same-sex partner [Supplement 4].
Leadership, Mentorship, and Promotion
Four of 87 studies (5%) examined leadership, mentorship, and promotion in EMS by sex/gender (Citation24, Citation31, Citation44) or race/ethnicity (Citation32). A small 1991 survey of volunteer agencies found that fewer women than men had served as clinical or operational officers (21% vs. 42%) and women were less likely to have officer positions when compared to men with the same level of experience (Citation44). A larger nationwide survey of firefighters in 2015 found that more women than men felt promotions were not decided upon fairly (41% vs. 16%) and felt gender was a barrier to their career development (44% vs. 5%) (Citation31).
One article examined mentorship; this 2019 survey of female EMS physicians found that, among the 48% of respondents who reported receiving mentorship, a minority reported female mentorship, which was usually from a remote rather than local mentor (41% vs. 15%) (Citation24).
One study examined promotion by race/ethnicity, finding that minority firefighters were more likely to hold low, non-officer/chief ranks compared to their White counterparts in a national sample (Citation32).
No studies were reviewed that examined leadership, mentorship, or promotion by sexual orientation.
In the gray literature (26/250, 10%), numerous industry media articles discussed leadership “firsts” (9/26, 35%) largely related to sex/gender, such as the hiring of first female fire chiefs, firsthand accounts from women leaders in EMS (6/26, 23%), and cases of gender discrimination in promotion (7/26, 27%). Discourse on leadership from nonwhite or LGBTQI persons was largely absent. [Supplement 4]
Workplace Experience and Occupational Wellbeing
Stress, Burnout, Job Satisfaction, and Absenteeism
Nineteen of 87 articles (22%) examined various facets of occupational wellbeing in underrepresented groups. Thirteen articles examined occupational stress (Citation45–51) or burnout (Citation51–57), four examined job satisfaction (Citation58–61), and two examined absenteeism (Citation62, Citation63).
Of three studies (Citation45–47) examining occupational stress by sex or gender among large NREMT and NRP cohorts, two found possible increased stress among female personnel (Citation45, Citation46) while the third (Citation47) and three smaller studies (Citation48–50) found similar stress between sex/gender groups. Six articles examined burnout among EMTs or paramedics by sex or gender with varying results (Citation52–57). Three of four studies examining job satisfaction found no differences by sex or gender (Citation58–60), including in one large National Registry cohort (Citation58). The two articles examining absenteeism both found greater absenteeism among female EMS workers (Citation62, Citation63).
Five (Citation47, Citation51, Citation52, Citation55, Citation57) of six studies (Citation47, Citation51, Citation52, Citation55–57) examining occupational stress or burnout by race/ethnicity found that nonwhite personnel had similar or lower indicators of occupational stress or burnout compared to White peers. The sole article examining job satisfaction by race/ethnicity found no between-group differences (Citation61). The single study of absenteeism by race found no difference in missed workdays between White versus minority personnel in a large National Registry cohort (Citation62).
One study examined occupational wellbeing by sexual orientation; the authors found no difference in rates of compassion fatigue between personnel identifying as heterosexual, homosexual, or other sexual orientation (Citation56).
No gray literature items were found that directly related to occupational wellbeing by sex/gender, race/ethnicity, or sexual orientation.
Mental Health
Fifteen of 87 studies (17%) examined mental health among underrepresented groups in EMS, including suicidality (Citation64–71), post-traumatic stress disorder (PTSD) (Citation66, Citation72–74), and depression or anxiety (Citation32, Citation47, Citation50, Citation75).
Suicidality
Eight studies examined suicidality by sex or gender (Citation64–70), race/ethnicity (Citation65, Citation68–71), or sexual orientation (Citation65). Three studies examining the prevalence of suicidality among female firefighters found that a large proportion reported had experienced suicidal ideation during their career (Citation64, Citation65) or lifetime (Citation66). Two studies comparing rates of suicidality by sex or gender found no significant differences in the reported history of career suicidality by sex (Citation68) and no significant gender differences in deaths due to suicide among EMS personnel between 1999 and 2013 (Citation69). In contrast, a 2018 analysis of firefighters found female gender was associated with greater suicidality (Citation70).
Among the five studies comparing various measures of suicidality by race or ethnicity, four found no association (Citation65, Citation69–71); nonwhite respondents in these studies were predominately Black or Latino However, a 2015 survey of firefighters found that those identifying as Native American or Alaska Native were significantly more likely than White peers to report experiencing suicide ideation, plans, attempts, and non-suicidal self-injury during their careers (Citation68).
A study of women firefighters found no association between suicidality and sexual orientation (Citation65).
In the gray literature (3/250, 1%), media articles discussed instances and experiences of suicidality (2/3, 67%) [Supplement 4].
PTSD
Two small studies examining PTSD among cohorts of women firefighters found similar rates of probable PTSD (19–20%) (Citation66, Citation72). Stanley et al. (2019) noted that greater social support from supervisors was a significant predictor of lower PTSD severity scores (Citation72). A 2007 thesis—the only study that directly compared PTSD symptomatology by gender—found women EMTs and paramedics in the Appalachian region reported higher mean scores for PTSD symptoms than men (Citation73). A 2019 analysis of women firefighters compared their observed PTSD prevalence (20%) to previously published rates among male firefighters ranging from 4 to 22% and posited that female firefighters may be at higher risk of PTSD (Citation66).
No studies compared rates of PTSD by race/ethnicity or sexual orientation.
Depression and Anxiety
A small survey of female firefighters found that 22% of career and 39% of volunteer respondents scored in the range of concern for depression (using the Center for Epidemiologic Studies Depression Scale Revised-10) and a greater proportion of female career firefighters scored in the range of concern for depression than females in the general population (Citation75). However, a larger survey of NREMTs and NRPs found that female respondents were less likely to score as depressed (using the Depression Anxiety Stress Scale-21) compared to male peers (Citation47).
Regarding depression by race or ethnicity, the latter study found that minority respondents were less likely to score as depressed when compared to non-minority peers (Citation47). A more detailed analysis among male career firefighters between 2007 and 12 found that minority firefighters based in minority-dominated communities had the lowest prevalence of lifetime depression diagnosis (4%), while minority firefighters in White-dominated communities had the highest (10%) when compared to White firefighters in either type of community (Citation32). Bentley et al. in 2013 also examined anxiety (via the Depression Anxiety Stress Scale-21) and found similar rates of anxiety by sex and race (Citation47).
No studies examined depression or anxiety by sexual orientation.
In the gray literature (2/250, 1%), a media article described a clinician’s experiences with anxiety and depression [Supplement 4].
Health Behaviors
Eleven of 87 studies (13%) examined health behaviors among underrepresented groups in EMS, including the use of alcohol (Citation32, Citation75–81) and tobacco products (Citation32, Citation62, Citation80–83).
Hazardous Alcohol Use
Alcohol use by sex/gender (Citation75–81) or race/ethnicity (Citation32, Citation76, Citation80, Citation81) was examined in eight studies, seven among firefighters (Citation32, Citation75–80) and one among EMTs and paramedics (Citation81). A study using the Alcohol Use Disorders Identification Test-C in firefighters found high rates of concerning use among women (64–68%), which was comparable to men (63%) (Citation77). A second study using the same instrument also found similar average scores between males and females, but with both group’s means below the range of concern (Citation76). Studies using the CAGE Questionnaire found lower but varying rates of potentially hazardous use among female firefighters (Citation78–80). Five studies examined binge drinking among firefighters by sex or gender, with four finding high rates among females (Citation75, Citation78–80). The sole study of alcohol use among EMTs and paramedics found that female personnel drank fewer alcoholic beverages per day compared to males (Citation81).
Three studies among firefighters found minority personnel reported similar or less hazardous drinking behavior compared to White peers (Citation32, Citation77, Citation81).
No studies were found that examined alcohol use by sexual orientation.
Tobacco Use
Two studies and one thesis examining cigarette smoking among EMTs and paramedics by sex or gender found greater cigarette smoking behavior among female EMS personnel compared to males (Citation62, Citation81, Citation82).
Three studies examining cigarette smoking by race/ethnicity found that nonwhite/minority EMS personnel reported similar smoking behavior compared to White peers (Citation62, Citation80, Citation81). Two studies examining rates of smokeless tobacco use among firefighters by race/ethnicity found decreased odds of current use among minority personnel compared to White peers (Citation32, Citation83).
No studies were found that examined tobacco use by sexual orientation.
Harassment and Bullying
Harassment or bullying of underrepresented groups among EMTs and paramedics (Citation84, Citation85), firefighters (Citation31, Citation64, Citation86–88), and female EMS physicians (Citation24) was examined in 8/87 (9%) of studies.
Fullerton et al. found no differences in bullying by gender among EMTs and paramedics in New Mexico (Citation84), while a larger study of NREMTs and NRPs reported females had greater odds of experiencing frequent workplace incivility compared to males but found no difference between rates of workplace incivility by race/ethnicity (Citation85).
Four articles specifically queried respondents on their experiences of sexual harassment, with all finding high rates among women EMS personnel, including firefighters and EMS physicians (Citation24, Citation64, Citation86, Citation87). No articles specifically examined sexual harassment among non-firefighter female EMTs or paramedics.
Two studies described experiences of harassment or bullying through an intersectional lens of race and gender among firefighters with differing results (Citation87, Citation88). A mixed-methods study of Black women firefighters recruited in 1992 found a pattern of negative workplace interactions, varying from openly racist or sexist hostility to more subtle or silent exclusion, differential training, treatment, or supervision, and lack of support (Citation88). A differing 2019 survey did not specify overall rates of bullying or harassment but found there was no difference in the severity of discrimination or harassment by race/ethnicity (Citation87).
No studies were found that examined harassment or bullying by sexual orientation.
In the gray literature (80/250, 32%), numerous media articles examined harassment or bullying. Topics included relevant lawsuits or other legal actions (50/80, 63%), sexual harassment (33/80, 41%), and racist harassment (14/80, 18%) [Supplement 4]. A 2019 report from the US Fire Administration cited a 1995 survey, which found that 88% of career and 83% of volunteer women firefighters had been subjected to one or more types of sexual harassment at some point in their careers (Citation89). This report concluded that the culture of the fire service needed to change to be more inclusive of women and provided proposed strategies for such change (Citation89).
Occupational Violence
Eight of 87 studies (9%) examined occupational violence by sex or gender (Citation24, Citation86, Citation87, Citation90–94). Two studies examined rates of occupational violence in samples of women firefighters and found that in 1990, 17% reported having experienced “acts of violence” to person or property by coworkers or their spouses (Citation86) and in 2019, 5% reported having experienced assaults because of their gender (Citation87). In a sample of female EMS physicians in 2019, 23% and 7% reported having experienced workplace physical or sexual assault, respectively (Citation24).
Two national studies of EMTs and paramedics found that females may have a greater risk of occupational violence (Citation90, Citation91), while two smaller regional surveys of EMTs and paramedics did not find differences in overall rates of workplace violence by sex or gender (Citation93, Citation94). However, one of these studies, a survey of Detroit-area EMS workers, found that women were more likely to be assaulted by EMS coworkers compared to male peers (Citation94).
The sole study examining occupational violence by race or ethnicity, a survey of patient-initiated violence toward NREMTs and NRPs, did not find an association between race and rates of physical or verbal assault (Citation91).
No studies examined sexual assault among firefighters, EMTs, or paramedics. No studies examined occupational violence by sexual orientation.
Within the gray literature (8/250, 3%), media articles (7/8, 88%) covered cases of sexual assault in EMS workplaces [Supplement 4]. A 2019 National Association of EMTs survey found much higher rates of occupational violence than those reported above, but a greater proportion of men than women reported having been physically or verbally assaulted (Citation95). However, women respondents reported feeling somewhat less safe at work than men (57% vs. 64%) and were less likely than men to report violence to their agency (Citation95).
Occupational Injuries
Seven of 87 studies (8%) examined various facets of occupational injury among EMTs and paramedics by sex or gender (Citation96–102). A survey of workplace injuries among NREMTs and NRPs from 1999–2005 estimated that females had a greater prevalence of workplace injury (11% vs. 9% for males) and 45% increased odds of injury in the prior 12 months (Citation96). Two retrospective cohort studies using case data from the Bureau of Labor Statistics found that female EMTs and paramedics accounted for a disproportionate share of EMS occupational injuries (Citation97, Citation98). Despite comprising approximately 27% of the workforce in 2003–08, females accounted for 45% of overall reported EMS occupational injuries in 2003–07 (97) and 53% of reported transportation-related EMS occupational injuries in 2006–08 (98). Lastly, a small 2017 qualitative study examining the role of gender in safety behaviors among female firefighters and paramedics nationally hypothesized that female gender might improve safety through various behaviors, including consideration of risks and benefits and improved injury reporting (Citation102).
No studies were found that examined occupational injuries by race/ethnicity or sexual orientation.
A 2019 US Fire Administration report using Bureau of Labor Statistics data from 2011 found that women firefighters have a 1.8-fold higher risk of occupational illness or injury (Citation89).
Gender in the Workplace
Two small studies (2/87, 2%) examined general ways in which gender functions in the EMS workplace (Citation103, Citation104).
A 1998 mixed-methods study of EMTs and paramedics in Louisiana found that most respondents (74% of males and 90% of females) reported no work-partner gender preference. However, the authors also noted that a variety of gendered perceptions were prevalent, such as perceptions of physical strength and men’s versus women’s ability to play authoritative roles in the EMS environment. Lastly, they noted several structural factors affecting gendered experiences of the work environment, such as living quarters not conducive to mixed-gender crews and policies prohibiting an ambulance from operating with two female paramedics (Citation103).
A 2016 sociology dissertation extensively discussed intersections of work, gender, and emotional labor among 30 paramedics on the West Coast. A key exploration focused on the idea of heroism and the way in which certain work done by paramedics (such as caregiving tasks) was not viewed as “heroic” given a feminized conception of such “emotional” labor, despite being an important aspect of their occupational identity (Citation104).
The relevant gray literature (4/250, 2%) was dominated by opinion pieces in which EMS personnel discussed their views on gender and EMS culture (3/4, 75%) [Supplement 4].
Discussion
Workforce Demographics
Diversity in the EMS workforce remains a significant challenge. Women and nonwhite personnel continue to be underrepresented in EMS training, education, and the workforce, irrespective of training level. Research on LGBTQI personnel is largely absent. This lack of diversity mirrors the experience of other health care disciplines, including physicians and nurses (Citation105, Citation106).
Recruitment
Recruitment of women and Hispanic EMS personnel at the EMT level has increased. However, recruitment of Black personnel continues to lag. Furthermore, women and nonwhite clinicians who are recruited face challenges in both the pre-hiring and education phases of their careers. Although recent data are lacking, a majority of EMS educators in 2003–04 and a majority of training officers in 2011 were non-Hispanic White males. Women and Black candidates may be less likely to pass the National Registry paramedic cognitive exam compared to men and White candidates, respectively, raising concern for potential bias in these exams. Additionally, the finding that women may be less likely to reattempt the National Registry EMT cognitive exam after an initial unsuccessful attempt points toward systemic barriers to entry. Additional barriers may include unequal pay compared to colleagues who are men or societal pressures to place family ahead of career. In the fire service, there have been at least two high-profile lawsuits at major departments alleging racial or gender discrimination in pre-hiring testing. Overall, these results raise the concern for systemic barriers to EMS certification for both women and Black candidates.
Approaches to addressing disparities in medical education, including pipeline programs and innovative admissions practices, have resulted in marginal improvements in recruitment of nonwhite clinicians (Citation105, Citation107). Structural racism and stereotyping are proposed factors limiting the success of such programs and likely also affect EMS. Additionally, the unintended creation of exclusionary environments through implicit and explicit bias, especially involving Black men, threatens efforts to increase diversity, equity, and inclusion (Citation108).
Retention
Attrition among women and nonwhite EMS personnel may be higher than among men and White personnel. We hypothesize that lack of pay parity is one driver of attrition among women. The gender pay gap across industries has persisted despite improvements over the past decades (Citation109), and EMS has not been spared. Female EMS professionals earned between $4,000 and $15,000 less annually than males, according to data from 1999 to 2008. This disparity is particularly pronounced at the EMT compared to paramedic level. The 1999–2008 data from NREMT did not suggest a race or ethnicity-based pay gap between White versus minority personnel, although the limited resolution of the minority category in these data makes it difficult to extrapolate this conclusion to particular racial or ethnic groups. Other compensation and benefits such as maternity leave remain poorly studied in EMS.
Another key driver of attrition may be opportunities for advancement. Women and nonwhite individuals are likely to experience disparities in recruitment and selection for leadership positions. Industry media coverage of leadership “firsts” and overall workforce demographics suggest a paucity of women leadership in EMS. However, formal data are lacking. Limited data hypothesize that nonwhite firefighters may be less likely to hold leadership ranks, while data on nonwhite leadership in non-fire EMS appear to be absent.
Workplace experience is a third likely driver of attrition, with occupational safety, including exposure to harassment and violence, being of particular concern. Sexual harassment is highly prevalent among women firefighters, although the prevalence may have decreased since the 1990s, and limited recent data suggest a similarly high prevalence among female EMS physicians. Women in EMS may also be more likely to experience workplace violence and injury.
Despite extensive coverage of relevant lawsuits in the media and discussion in industry opinion pieces, empirical data are absent on sexual harassment among non-firefighter EMTs and paramedics. Furthermore, despite media coverage of racist incidents and relevant lawsuits, empirical data on racial harassment and bullying in EMS were not found in this review.
Recommendations
Structured and innovative efforts to increase diversity, equity, and inclusion in EMS must include deliberate actions to comprehend and address deeply rooted barriers such as structural racism, racial and gender stereotyping, and implicit bias. EMS organizations seeking to increase diversity should develop strategic plans that include a needs assessment to evaluate the representativeness of their own workforce in relation to the community served, as well as the creation of diversity and inclusion leadership positions. Such leaders should design and implement programs based on these needs assessments to improve the recruitment, retention, and workplace experience of underrepresented groups, including women, nonwhite personnel, and LGBTQI personnel.
Furthermore, a formalization of efforts to study the efficacy of and implement such recruitment and retention programs is needed. While our review did not identify any literature to support specific approaches, there are reports of programs that have shown some success and warrant further research (Citation110, Citation111). Future efforts should account for the workplace and societal experiences of underrepresented groups, including systemic barriers to entry. After recruitment, the pre-hiring, education, and testing processes should reflect the varying needs of potential candidates. There should be careful consideration of the potential for stereotype threat with respect to women and nonwhite individuals during the development and use of standardized testing.
Retention of EMS personnel is likely closely tied to workplace experience, fair compensation, and opportunities for advancement. All EMS entities should proactively review their compensation to ensure pay parity among professionals of equal experience, regardless of race, gender, or sexual orientation. Additionally, well-delineated job-protected policies and procedures for family and medical leave—maternity leave in particular—should become an integral part of high-performing EMS entities. Lastly, such entities should examine internal practices for promotion and recruitment into leadership positions, to ensure the process is transparent, equitable, and reflects the diversity of the community served.
Progress has been made in preventing harassment, bullying, and discrimination in the EMS workplace, but significant effort is still needed to eradicate them. This scoping review reveals that research in prevention methodology is lacking, particularly in the mechanisms of reporting, investigating, and implementing strategies to prevent sexual harassment, bullying, and discrimination against women EMS clinicians. A transparent, zero-tolerance environment should accompany robust reporting mechanisms that are non-punitive and non-retaliatory. Recruitment of underrepresented personnel into leadership positions is a culture-affecting factor that we hypothesize may reduce negative behaviors toward underrepresented EMS clinicians and thus may improve retention.
Limitations
This scoping review is inherently limited by the existing literature that was reviewed, and by the scoping methodology. As the aim of a scoping review is to be broadly inclusive (Citation13), a formal quality assessment was not conducted, which limits the strength of conclusions based on our findings.
There are additional characteristics within the workforce that were not assessed in this review, such as diversity in nationality, socioeconomic status, language, religion, ability, and age. Such characteristics likely influence the workplace experience in an intersectional manner unexplored here.
Studies were inconsistent in their use of demographic terminologies such as race, ethnicity, sex, and gender. This complicates the interpretation of our findings for diverse populations. Given that gender (socially constructed and enacted roles and behaviors within a dynamic cultural context) is generally of more relevance to studies of the workforce than one’s sex (chromosomes or sex organs) (Citation112), we recommend the term gender be used in place of sex for future demographic data capture of the EMS workforce. Similarly, race and ethnicity refer to socially constructed aspects of identity and heritage that may overlap or be exclusive, depending on the individual. Combining race and ethnicity or using dichotomized variables (e.g., minority vs. non-minority) hinders the accurate representation of experiences among included populations or, in the case of gender, excludes those identifying as transgender or non-binary. In doing so, we do a disservice to our colleagues by obfuscating their experiences and thus perpetuating systemic inequities. We recommend that future researchers in the field use the best practices outlined recently by Nahmias et al. for operationalizing demographic variables: ensuring that demographic variables are self-reported and, “[including] at least a nonbinary gender variable and a more inclusive than Hispanic/Latino and not-Hispanic/Latino ethnicity category,” at a minimum (Citation16).
Conclusion
The existing literature demonstrates continued underrepresentation of women and nonwhite personnel in the EMS workforce. Additionally, these studies raise concerns for pervasive negative workplace experiences including sexual harassment and factors that negatively affect recruitment and retention, including bias in candidate testing, a gender pay gap, and unequal promotion opportunities. Additional research is needed to elucidate recruitment and retention program efficacy, the demographic composition of EMS leadership, and the prevalence of racial harassment and discrimination in this workforce.
Supplemental Material
Download Zip (2 MB)Acknowledgments
Thank you to the NAEMSP Diversity, Equity, and Inclusion Committee for their vision and support of this project.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Crowe RP, Krebs W, Cash RE, Rivard MK, Lincoln EW, Panchal AR. Females and minority racial/ethnic groups remain underrepresented in emergency medical services: a ten-year assessment, 2008–2017. Prehosp Emerg Care. 2020;24(2):180–7. doi:10.1080/10903127.2019.1634167.
- Institute of Medicine (US) Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Healthcare Workforce. In the nation’s compelling interest: ensuring diversity in the health-care workforce. Smedley B, Stith Butler A, Bristow L, eds. Washington (DC): National Academies Press (US); 2004.
- Stanford FC. The importance of diversity and inclusion in the healthcare workforce. J Natl Med Assoc. 2020;112(3):247–9. doi:10.1016/j.jnma.2020.03.014.
- Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine (US). The future of nursing: leading change, advancing health. Washington (DC): National Academies Press (US); 2011.
- EMS Agenda 2050 Technical Expert Panel. EMS agenda 2050: a people-centered vision for the future of emergency medical services. Report No.: DOT HS 812 664. Washington (DC): National Highway Traffic Safety Administration; 2019.
- Chapman SA, Lindler V, Kaiser JA, Nielsen CS. EMS workforce for the 21st century: a national assessment. Washington (DC): National Highway Traffic Safety Administration; 2008.
- Wallis CJD, Jerath A, Coburn N, Klaassen Z, Luckenbaugh AN, Magee DE, Hird AE, Armstrong K, Ravi B, Esnaola NF, et al. Association of surgeon-patient sex concordance with postoperative outcomes. JAMA Surg. 2022;157(2):146–56. doi:10.1001/jamasurg.2021.6339.
- Chekijian S, Kinsman J, Taylor RA, Ravi S, Parwani V, Ulrich A, Venkatesh A, Agrawal P. Association between patient-physician gender concordance and patient experience scores. Is there gender bias? Am J Emerg Med. 2021;45:476–82. doi:10.1016/j.ajem.2020.09.090.
- Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, Bylund CL. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117–40. doi:10.1007/s40615-017-0350-4.
- Rotenstein LS, Reede JY, Jena AB. Addressing workforce diversity - a quality-improvement framework. N Engl J Med. 2021;384(12):1083–6. doi:10.1056/NEJMp2032224.
- Betancourt JR. Improving quality and achieving equity: the role of cultural competence in reducing racial and ethnic disparities in health care. New York (NY): Commonwealth Fund; 2006.
- Hoever IJ, van Knippenberg D, van Ginkel WP, Barkema HG. Fostering team creativity: perspective taking as key to unlocking diversity’s potential. J Appl Psychol. 2012;97(5):982–96. doi:10.1037/a0029159.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodology. 2005;8(1):19–32. doi:10.1080/1364557032000119616.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi:10.1186/1748-5908-5-69.
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi:10.7326/M18-0850.
- Nahmias J, Zakrison TL, Haut ER, Gurney O, Joseph B, Hendershot K, Ghneim M, Stey A, Hoofnagle MH, Bailey Z, et al. Call to action on the categorization of sex, gender, race, and ethnicity in surgical research. J Am Coll Surg. 2021;233(2):316–9. doi:10.1016/j.jamcollsurg.2021.04.025.
- Bentley MA, Shoben A, Levine R. The demographics and education of emergency medical services (EMS) professionals: a national longitudinal investigation. Prehosp Disaster Med. 2016;31(S1):S18–S29. doi:10.1017/S1049023X16001060.
- Rivard MK, Cash RE, Mercer CB, Chrzan K, Panchal AR. Demography of the national emergency medical services workforce: a description of those providing patient care in the prehospital setting. Prehosp Emerg Care. 2021;25(2):213–20. doi:10.1080/10903127.2020.1737282.
- Brown WE, Dickison PD, Misselbeck WJA, Levine R. Longitudinal emergency medical technician attribute and demographic study (LEADS): an interim report. Prehosp Emerg Care. 2002;6(4):433–9. doi:10.1080/10903120290938085.
- Crowe RP, Levine R, Eggerichs JJ, Bentley MA. A longitudinal description of emergency medical services professionals by race/ethnicity. Prehosp Disaster Med. 2016;31(S1):S30–S69. doi:10.1017/S1049023X16001072.
- Rivard MK, Cash RE, Chrzan K, Panchal AR. Comprehensive description of the advanced emergency medical technician certification level. Prehosp Emerg Care. 2020;24(3):394–400. doi:10.1080/10903127.2019.1639862.
- Cash RE, Rivard MK, Chrzan K, Mercer CB, Camargo CA, Panchal AR. Comparison of volunteer and paid EMS professionals in the United States. Prehosp Emerg Care. 2021;25(2):205–12. doi:10.1080/10903127.2020.1752867.
- March JA, Adams JL, Portela RC, Taylor SE, McManus JG. Characteristics and diversity of ACGME accredited emergency medical services fellowship programs. Prehosp Emerg Care. 2019;23(4):551–9. doi:10.1080/10903127.2018.1544327.
- Staats K, Counts CR, Dyer KS, Stemerman R, Braithwaite S, Luke A, Mercer MP. Characteristics and experiences of women physicians and professionals in NAEMSP. Prehosp Emerg Care. 2022;26(5):689–99. doi:10.1080/10903127.2021.1992051.
- Taylor A. Illinois fire departments with paid personnel: An initial characterization [Thesis]. Macomb (IL): Western Illinois University; 2013.
- Chng CL, Collins J, Eaddy S. A comparison of rural and urban emergency medical system (EMS) personnel: a Texas study. Prehosp Disaster Med. 2001;16(3):159–65. doi:10.1017/S1049023X00025917.
- Thompson AM. Rural emergency medical volunteers and their communities: a demographic comparison. J Community Health. 1993;18(6):379–92. doi:10.1007/BF01323968.
- Lineros JV. An investigation of paramedical vocational interest and choice for Latinos and African American men in Texas community colleges. Community Coll J Res Prac. 2020;44(3):181–210. doi:10.1080/10668926.2019.1565844.
- Cash RE, Crowe RP, Agarwal R, Rodriguez SA, Panchal AR. Exiting the emergency medical services profession and characteristics associated with intent to return to practice. Prehosp Emerg Care. 2018;22(1):28–33. doi:10.1080/10903127.2017.1339749.
- Marimon MO, Santiago KM, Caban-Martinez AJ, Schaefer Solle N, Fonseca M, Dietz N. Diversity and inclusion leaders in US fire departments impact the type and number of diversity and inclusion programs offered. J Occup Environ Med. 2020;62(1):e13–e16. doi:10.1097/JOM.0000000000001780.
- Griffith JC, Roberts DL, Wakeham RT. Bullying at the fire station? Perceptions based on gender, race and sexual orientation. Am Int J Soc Sci. 2016;5:12.
- Poston W, Haddock CK, Jahnke SA, Jitnarin N, Day RS, Daniels ID. Health disparities among racial and ethnic minority firefighters. J Health Dispar Res Prac. 2014;7:25.
- Ruple JA, Frazer GH, Hsieh AB, Bake W, Freel J. The state of EMS education research project. Prehosp Emerg Care. 2005;9(2):203–12. doi:10.1080/10903120590924807.
- Bentley MA, Eggerichs-Purcell JJ, Brown WE, Wagoner R, Gibson GC, Sahni R. A national assessment of the roles and responsibilities of training officers. Prehosp Emerg Care. 2013;17(3):373–8. doi:10.3109/10903127.2013.785618.
- Dickison P, Hostler D, Platt TE, Wang HE. Program accreditation effect on paramedic credentialing examination success rate. Prehosp Emerg Care. 2006;10(2):224–8. doi:10.1080/10903120500541126.
- McKenna KD. Factors that affect reattempting the emergency medical technician cognitive certification examination [Dissertation]. St. Louis (MO): University of Missouri-St. Louis; 2016.
- Powell JR, Cash RE, Rivard MK, Panchal AR. EMS program graduates who did not retest after initial attempt on the national certification exam. Prehosp Emerg Care. 2022;26(5):664–72. doi:10.1080/10903127.2021.1943579.
- Crowe RP, Levine R, Bentley MA. Prehospital helicopter air ambulances part 2: utilization criteria and training. Air Med J. 2015;34(6):337–42. doi:10.1016/j.amj.2015.06.008.
- Rodriguez SA. Paramedic program accreditation and individual performance on the national paramedic certification examination [Dissertation]. Minneapolis (MN): Walden University; 2016.
- Russ-Eft DF, Dickison PD, Levine R. Examining career success of minority and women emergency medical technicians (EMTs): a LEADS project. Hum Resour Dev Q. 2008;19(4):281–98. doi:10.1002/hrdq.1242.
- Studnek JR. Compensation of emergency medical technician (EMT)-basics and paramedics. Prehosp Disaster Med. 2016;31(S1):S87–S95. doi:10.1017/S1049023X16001096.
- Russ-Eft D, Levine R, Fernandez AR. Objective career success among paramedics: interaction effects of location and race. Hum Resource Dev Int. 2014;17(1):10–29. doi:10.1080/13678868.2013.840084.
- Jahnke SA, Poston WSC, Jitnarin N, Haddock CK. Maternal and child health among female firefighters in the US. Maternal Child Health J. 2018;22(6):922–31. doi:10.1007/s10995-018-2468-3.
- Thompson IA. The sexual division of leadership in volunteer emergency medical service squads. Nonprofit Manage Leadersh. 1995;6(1):55–66. doi:10.1002/nml.4130060106.
- Cash RE, Anderson SE, Lancaster KE, Lu B, Rivard MK, Camargo CA, Panchal AR. Comparing the prevalence of poor sleep and stress metrics in basic versus advanced life support emergency medical services personnel. Prehosp Emerg Care. 2020;24(5):644–56. doi:10.1080/10903127.2020.1758259.
- Blau G, Bentley MA, Eggerichs-Purcell J. Testing the impact of emotional labor on work exhaustion for three distinct emergency medical service (EMS) samples. Career Dev Int. 2012;17(7):626–45. doi:10.1108/13620431211283788.
- Bentley MA, Crawford JM, Wilkins JR, Fernandez AR, Studnek JR. An assessment of depression, anxiety, and stress among nationally certified EMS professionals. Prehosp Emerg Care. 2013;17(3):330–8. doi:10.3109/10903127.2012.761307.
- Cydulka RK, Emerman CL, Shade B, Kubincanek J. Stress levels in EMS personnel: a national survey. Prehosp Disaster Med. 1997;12(2):136–40.
- Cydulka RK, Lyons J, Moy A, Shay K, Hammer J, Mathews J. A follow-up report of occupational stress in urban EMT-paramedics. Ann Emerg Med. 1989;18(11):1151–6. doi:10.1016/S0196-0644(89)80050-2.
- Murphy SA, Beaton RD, Cain K, Pike K. Gender differences in fire fighter job stressors and symptoms of stress. Women Health. 1995;22(2):55–69. doi:10.1300/J013v22n02_04.
- Neale AV. Work stress in emergency medical technicians. J Occup Med. 1991;33:991–7.
- Sporer C. Burnout in emergency medical technicians and paramedics in the USA. Int J Emergency Serv. 2021;10(3):366–89. doi:10.1108/IJES-03-2020-0012.
- Eaddy S. Sensation seeking as it relates to burnout among emergency medical personnel: a statewide study [Thesis]. Denton: University of North Texas; 1997.
- Essex B, Scott LB. Chronic stress and associated coping strategies among volunteer EMS personnel. Prehosp Emerg Care. 2008;12(1):69–75. doi:10.1080/10903120701707955.
- Weiss SJ, Silady MF, Roes B. Effect of individual and work characteristics of EMTs on vital sign changes during shiftwork. Am J Emerg Med. 1996;14(7):640–4. doi:10.1016/S0735-6757(96)90078-9.
- Renkiewicz GK, Hubble MW. Secondary traumatic stress in emergency services systems (STRESS) project: quantifying and predicting compassion fatigue in emergency medical services personnel. Prehosp Emerg Care. 2022;26(5):652–63. doi:10.1080/10903127.2021.1943578.
- Miller A, Unruh L, Liu X, Wharton T, Zhang N. Individual and organizations factors associated with professional quality of life in Florida EMS personnel. Int J Emergency Serv. 2018;7(2):147–60. doi:10.1108/IJES-08-2017-0041.
- Blau G, Bentley M, Eggerichs J, Chapman S, Viswanathan K. Are there differences between male versus female ems professionals on emotional labor and job satisfaction? J Behav Health. 2014;3(2):82–6. doi:10.5455/jbh.20140225061443.
- Bowron JS, Todd KH. Job stressors and job satisfaction in a major metropolitan public EMS service. Prehosp Disaster Med. 1999;14(4):32–5. doi:10.1017/S1049023X00027692.
- Will JB. An analysis of attitudes toward measures of job satisfaction related to identified factors of paramedic education [Dissertation]. Chester (PA): Widener University; 1999.
- Federiuk CS, O'Brien K, Jui J, Schmidt TA. Job satisfaction of paramedics: The effects of gender and type of agency of employment. Ann Emerg Med. 1993;22(4):657–62. doi:10.1016/S0196-0644(05)81843-8.
- Bentley MA. A national assessment of ideal cardiovascular health among emergency medical service professionals [Dissertation]. Columbus: The Ohio State University; 2016.
- Martin SC. Examining the relationship between secondary traumatic stress and sickness absenteeism within 9-1-1 emergency call centers [Thesis]. Seattle (WA): University of Washington; 2016.
- Hom MA, Stanley IH, Spencer-Thomas S, Joiner TE. Women firefighters and workplace harassment: associated suicidality and mental health sequelae. J Nerv Ment Dis. 2017;205(12):910–7. doi:10.1097/NMD.0000000000000759.
- Stanley IH, Hom MA, Spencer-Thomas S, Joiner TE. Suicidal thoughts and behaviors among women firefighters: an examination of associated features and comparison of pre-career and career prevalence rates. J Affective Disorders. 2017;221:107–14. doi:10.1016/j.jad.2017.06.016.
- Noor N, Pao C, Dragomir-Davis M, Tran J, Arbona C. PTSD symptoms and suicidal ideation in US female firefighters. Occup Med. 2019;69:577–85. doi:10.1093/occmed/kqz057.
- Hom MA, Stanley IH, Spencer-Thomas S, Joiner TE. Mental health service use and help-seeking among women firefighters with a career history of suicidality. Psychol Serv. 2018;15(3):316–24. doi:10.1037/ser0000202.
- Stanley IH, Hom MA, Hagan CR, Joiner TE. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J Affect Disord. 2015;187:163–71. doi:10.1016/j.jad.2015.08.007.
- Vigil NH, Beger S, Gochenour KS, Frazier WH, Vadeboncoeur TF, Bobrow BJ. Suicide among the EMS occupation in the United States. West J Emerg Med. 2021;22(2):326–32. doi:10.5811/westjem.2020.10.48742.
- Bartlett BA, Jardin C, Martin C, Tran JK, Buser S, Anestis MD, Vujanovic AA. Posttraumatic stress and suicidality among firefighters: the moderating role of distress tolerance. Cognit Ther Res. 2018;42(4):483–96. doi:10.1007/s10608-018-9892-y.
- Martin CE, Tran JK, Buser SJ. Correlates of suicidality in firefighter/EMS personnel. J Affective Disorders. 2017;208:177–83. doi:10.1016/j.jad.2016.08.078.
- Stanley I, Hom M, Chu C, Dougherty S, Gallyer A, Spencer-Thomas S, Shelef L, Fruchter E, Comtois K, Gutierrez P. Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: a multistudy investigation. Psychol Serv. 2019;16(4):543–55. doi:10.1037/ser0000240.
- Woods GL. Post traumatic stress symptoms and critical incident stress debriefing (CISD) in emergency medical services (EMS) personnel [Thesis]. Johnson City (TN): East Tennessee State University; 2007.
- Mishra S, Goebert D, Char E, Dukes P, Ahmed I. Trauma exposure and symptoms of post-traumatic stress disorder in emergency medical services personnel in Hawaii. Emerg Med J. 2010;27(9):708–11. doi:10.1136/emj.2009.080622.
- Jahnke SA, Poston WSC, Haddock CK, Jitnarin N, Hyder ML, Horvath C. The health of women in the US fire service. BMC Womens Health. 2012;12:39. doi:10.1186/1472-6874-12-39.
- Piazza-Gardner AK, Barry AE, Chaney E, Dodd V, Weiler R, Delisle A. Covariates of alcohol consumption among career firefighters. Occup Med (London). 2014;64(8):580–2. doi:10.1093/occmed/kqu124.
- Gallyer AJ, Dougherty SP, Gai AR, Stanley IH, Hom MA, Rogers ML, Duffy ME, Buchman-Schmitt JM, Spencer-Thomas S, Joiner TE. Problematic alcohol use and suicidal ideation among firefighters: A multi-study investigation of the explanatory roles of perceived burdensomeness and thwarted belongingness. J Affect Disord. 2018;238:281–8. doi:10.1016/j.jad.2018.05.045.
- Gulliver SB, Zimering RT, Dobani F, Pennington ML, Morissette SB, Kamholz BW, Knight JA, Keane TM, Kimbrel NA, Carpenter TP, et al. Alcohol use and mental health symptoms in female firefighter recruits. Occup Med (Lond). 2019;69(8-9):625–31. doi:10.1093/occmed/kqaa015.
- Haddock CK, Poston WSC, Jahnke SA, Jitnarin N. Alcohol use and problem drinking among women firefighters. Womens Health Issues. 2017;27(6):632–8. doi:10.1016/j.whi.2017.07.003.
- Jitnarin N, Poston WSC, Haddock CK, Jahnke SA. Tobacco use among women firefighters. Womens Health Issues. 2019;29(5):432–9. doi:10.1016/j.whi.2019.05.006.
- Pirrallo RG, Levine R, Dickison PD. Behavioral health risk factors of United States emergency medical technicians: the LEADS project. Prehosp Disaster Med. 2005;20(4):235–42. doi:10.1017/S1049023X00002594.
- Studnek JR, Bentley M, Crawford JM, Fernandez AR. An assessment of key health indicators among emergency medical services professionals. Prehosp Emerg Care. 2010;14(1):14–20. doi:10.3109/10903120903144957.
- Jitnarin N, Haddock CK, Poston WSC, Jahnke S. Smokeless tobacco and dual use among firefighters in the central United States. J Enviro Public Health. 2013;2013:e675426–7. doi:10.1155/2013/675426.
- Fullerton L, Oglesbee S, Weiss SJ, Ernst AA, Mesic V. Assessing the prevalence and predictors of bullying among emergency medical service providers. Prehosp Emerg Care. 2019;23(1):9–14. doi:10.1080/10903127.2018.1470208.
- Cash RE, White-Mills K, Crowe RP, Rivard MK, Panchal AR. Workplace incivility among nationally certified EMS professionals and associations with workforce-reducing factors and organizational culture. Prehosp Emerg Care. 2019;23(3):346–55. doi:10.1080/10903127.2018.1502383.
- Rosell E, Miller K, Barber K. Firefighting women and sexual harassment. Public Personnel Manage. 1995;24(3):339–50. doi:10.1177/009102609502400306.
- Jahnke SA, Haddock CK, Jitnarin N, Kaipust CM, Hollerbach BS, Poston WSC. The prevalence and health impacts of frequent work discrimination and harassment among women firefighters in the US Fire Service. Biomed Res Int. 2019;2019:1–13. doi:10.1155/2019/6740207.
- Yoder JD, Aniakudo P. Outsider within" the firehouse: subordination and difference in the social interactions of African American women firefighters. Gender Soc. 1997;11(3):324–41. doi:10.1177/089124397011003004.
- US Fire Administration. Emerging health and safety issues among women in the fire service. Washington (DC): Federal Emergency Management Agency; 2019.
- Maguire BJ, O'Neill BJ. Emergency medical service personnel’s risk from violence while serving the community. Am J Public Health. 2017;107(11):1770–5. doi:10.2105/AJPH.2017.303989.
- Gormley MA, Crowe RP, Bentley MA, Levine R. A national description of violence toward emergency medical services personnel. Prehosp Emerg Care. 2016;20(4):439–47. doi:10.3109/10903127.2015.1128029.
- Taylor JA, Barnes B, Davis AL, Wright J, Widman S, LeVasseur M. Expecting the unexpected: A mixed methods study of violence to EMS responders in an urban fire department. Am J Ind Med. 2016;59(2):150–63. doi:10.1002/ajim.22550.
- Furin M, Eliseo LJ, Langlois B, Fernandez WG, Mitchell P, Dyer KS. Self-reported provider safety in an urban emergency medical system. West J Emergency Med. 2015;16(3):459–64. doi:10.5811/westjem.2015.2.24124.
- Touriel R, Dunne R, Swor R, Kowalenko T. A pilot study: emergency medical services-related violence in the out-of-hospital setting in southeast Michigan. J Emerg Med. 2021;60(4):554–9. doi:10.1016/j.jemermed.2020.12.007.
- NAEMT EMS Workforce Committee. 2019 National survey on violence against EMS practitioners. Clinton (MS): National Association of Emergency Medical Technicians; 2019.
- Studnek JR, Ferketich A, Crawford JM. On the job illness and injury resulting in lost work time among a national cohort of emergency medical services professionals. Am J Ind Med. 2007;50(12):921–31. doi:10.1002/ajim.20516.
- Maguire BJ, Smith S. Injuries and fatalities among emergency medical technicians and paramedics in the United States. Prehosp Disaster Med. 2013;28(4):376–82. doi:10.1017/S1049023X13003555.
- Maguire BJ. Transportation-related injuries and fatalities among emergency medical technicans and paramedics. Prehosp Disaster Med. 2011;26(5):346–52. doi:10.1017/S1049023X11006601.
- Reichard AA, Marsh SM, Tonozzi TR, Konda S, Gormley MA. Occupational injuries and exposures among emergency medical services workers. Prehosp Emerg Care. 2017;21(4):420–31. doi:10.1080/10903127.2016.1274350.
- Hogya PT, Ellis L. Evaluation of the injury profile of personnel in a busy urban EMS system. Am J Emerg Med. 1990;8(4):308–11. doi:10.1016/0735-6757(90)90081-A.
- Alhazmi RA, Parker RD, Wen S. Needlestick injuries among emergency medical services providers in urban and rural areas. J Community Health. 2018;43(3):518–23. doi:10.1007/s10900-017-0446-0.
- Khan YA, Davis AL, Taylor JA. and lifting: How gender affects safety behaviors in the fire service. J Workplace Behav Health. 2017;32(3):206–25. doi:10.1080/15555240.2017.1358642.
- Gonsoulin S, Palmer CE. Gender issues and partner preferences among a sample of emergency medical technicians. Prehosp Disaster Med. 1998;13(1):34–40. doi:10.1017/S1049023X0003301X.
- McNamara MB. Saving lives; living the dream”: gender and emotional labor among ambulance-based 911 paramedics [Dissertation]. Santa Cruz (CA): University of California Santa Cruz; 2016.
- Association of American Medical Colleges. Diversity in medicine: facts and figures 2019 [Internet]. 2019. [accessed 2022 Jul 25]. Available from: https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018.
- Smiley RA, Ruttinger C, Oliveira CM, Hudson LR, Allgeyer R, Reneau KA, Silvestre JH, Alexander M. The 2020 national nursing workforce survey. J Nurs Regul. 2021;12(1):S1–S96. doi:10.1016/S2155-8256(21)00027-2.
- Boatright DH, Samuels EA, Cramer L, Cross J, Desai M, Latimore D, Gross CP. Association between the liaison committee on medical education’s diversity standards and changes in percentage of medical student sex, race, and ethnicity. JAMA. 2018;320(21):2267–9. doi:10.1001/jama.2018.13705.
- Lewis D, Paulson E. Proceedings of the diversity and inclusion innovation forum: unconscious bias in academic medicine. Washington (DC): George Washington University Faculty Bookshelf; 2017.
- Blau FD, Kahn LM. The gender wage gap: extent, trends, and explanations. J Econ Lit. 2017;55(3):789–865. doi:10.1257/jel.20160995.
- Alameda County Emergency Medical Services. EMScorps. Alameda County EMS. [accessed Sep. 18]. https://ems.acgov.org/CommtyResources/EMScorps.page.
- The Saint Paul Fire Department. EMS Academy. Saint Paul Minnesota. [accessed 2022 Sep 18]. https://www.stpaul.gov/departments/fire-emergency-medical-services/paramedicsems/ems-academy.
- National Institutes of Health: Office of Research on Women’s Health. Sex & Gender [Internet]. [accessed 2022 Jul 29]. Available from: https://orwh.od.nih.gov/sex-gender.